ABSTRACT
Background: While empirical support for the ICD-11 distinction between posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD) is growing, empirical research into the ICD-11 model of CPTSD in military populations is scarce and inconsistent.
Objective: To replicate a study from our own group identifying distinct classes based on CPTSD symptoms using the International Trauma Questionnaire (ITQ) and to identify predictors and functional outcomes associated with a potential distinction between PTSD and CPTSD.
Method: Formerly deployed treatment-seeking Danish soldiers (N = 294) completed the ITQ and self-report measures of traumatic life events prior to treatment. Latent profile analysis (LPA) was used to extract classes based on CPTSD symptoms.
Results: LPA revealed four classes; (1) high CPTSD symptoms (‘CPTSD’, 28.7%); (2) high PTSD symptoms and lower DSO symptoms (‘PTSD’, 23.5%); (3) high DSO symptoms (‘DSO’, 17.3%); and (4) low symptoms (‘Low Symptoms’, 30.5%). In comparison to the PTSD-class, CPTSD-class membership was not predicted by traumatic events in adult life and in childhood. The CPTSD class was more often single/divorced/widowed compared to the PTSD class. Moreover, the CPTSD class more often used psychotropic medicine compared to the DSO-class and Low Symptoms-class.
Conclusion: Using the ITQ, this study yields empirical support for the ICD-11 model of CPTSD within a clinical sample of veterans. The results replicate findings from our previous study that also identified distinct profiles of ICD-11 PTSD and CPTSD.
KEYWORDS: ICD-11, posttraumatic stress disorder (PTSD) and complex posttraumatic stress disorder (CPTSD), military veterans, treatment-seeking persons, latent profile analysis
HIGHLIGHTS
The study identified separate classes representing CPTSD, PTSD, DSO and Low Symptoms in treatment-seeking military veterans based on the International Trauma Questionnaire.
CPTSD is a more debilitating condition than PTSD.
Findings replicate a previous LPA study of treatment-seeking Danish veterans.
Abstract
Antecedentes: Si bien, el soporte empírico de la clasificación de la CIE-11 para la distinción entre el trastorno de estrés postraumático (TEPT) y TEPT complejo (TEPTC) está creciendo, la investigación empírica sobre el modelo del TEPTC según la CIE-11 en poblaciones militares es escasa e inconsistente.
Objetivo: Replicar un estudio de nuestro propio grupo identificando distintas clases basadas en los síntomas del TEPTC utilizando el Cuestionario Internacional de Trauma (ITQ por sus siglas en inglés) e identificar los predictores y las consecuencias funcionales asociadas a una posible distinción entre TEPT y TEPTC.
Método: Los soldados daneses que estuvieron en despliegue y en búsqueda de tratamiento (N= 294) completaron el cuestionario de la ITQ y medidas de auto-reporte en relación a eventos traumáticos a lo largo de la vida antes del tratamiento. Se utilizó el análisis de perfil latente (APL) para extraer clases basadas en los síntomas del TEPTC.
Resultados: El APL reveló cuatro clases; (1) síntomas elevados de TEPTC (‘TEPTC’, 28.7%); (2) síntomas elevados de TEPT y síntomas más bajos de Alteraciones en la Auto-Organización (DSO por sus siglas en inglés) (‘TEPT’, 23.5%); (3) síntomas elevados de DSO (‘DSO’, 17.3%); y (4) síntomas bajos (‘Síntomas bajos’, 30.5%). En comparación con la clase de TEPT, la afiliación a la clase del TEPTC no estuvo predicha por eventos traumáticos en la adultez y en la infancia. La clase TEPTC era más frecuentemente soltero/divorciado/viudo, en comparación con la clase TEPT. Además, la clase TEPTC utilizó con mayor frecuencia medicamentos psicotrópicos en comparación con la clase DSO y la clase de Síntomas bajos.
Conclusiones: Utilizando el cuestionario ITQ, este estudio proporciona apoyo empírico para el modelo de TEPTC de la CIE-11 dentro de una muestra clínica de veteranos. Los resultados replican los hallazgos de nuestro estudio anterior, que tambien identificó distintos perfiles de TEPT y TEPTC según la clasificación de la CIE-11.
PALABRAS CLAVE: CIE-11, Trastorno de Estrés Postraumático (TEPT) y Trastorno de Estrés Postraumático Complejo (TEPTC), veteranos militares, personas en búsqueda de tratamiento, análisis de perfil latente
Abstract
背景: 尽管对ICD-11区分创伤后应激障碍 (PTSD) 与复杂性创伤后应激障碍 (CPTSD) 的实证支持越来越多, 对军人群体中CPTSD的ICD-11模型的实证研究很少且不一致。
目的: 重复我们自己小组的一项研究, 根据使用国际创伤问卷调查 (ITQ) 测量的CPTSD症状识别不同的类别, 并确定与PTSD和CPTSD潜在区别相关的预测因素和功能结果。
方法: 退伍寻求治疗的丹麦士兵 (N = 294) 在治疗之前完成了ITQ和自我报告创伤生活事件的测量。潜在剖面分析 (LPA) 用来选取基于CPTSD症状的类别。
结果: LPA揭示了四个类别: (1) 高CPTSD症状类 (‘ CPTSD’, 28.7%); (2) 高PTSD症状和低DSO症状类 (‘ PTSD’, 23.5%); (3) 高DSO症状类 (‘ DSO’, 17.3%); (4) 低症状类 (‘低症状’, 30.5%) 。与PTSD类相比, 成年和童年期的创伤事件并未预测CPTSD类成员身份。与PTSD类相比, CPTSD类更常为单身/离婚/丧偶。此外, 与DSO类和低症状类相比, CPTSD类更经常使用精神药物。
结论: 使用ITQ, 本研究为退伍军人临床样本中的CPTSD的ICD-11模型提供了实证支持。结果重复了我们先前研究的发现, 也确定了ICD-11 PTSD和CPTSD的不同剖面。
关键词: ICD-11, 创伤后应激障碍 (PTSD) 和复杂性创伤后应激障碍 (CPTSD), 退伍军人, 寻求治疗者, 潜在剖面分析
1. Introduction
Posttraumatic stress disorder (PTSD) is a common mental disorder in military populations following deployment to war zones (Forbes et al., 2019). Among Danish soldiers deployed to Afghanistan, self-reported rate of probable PTSD has been estimated to 10% 2.5 years after homecoming (Madsen, Andersen, & Karstoft, 2016). While trauma exposure during deployment is expected to contribute to PTSD-development (Palic et al., 2016), several non-deployment stressors may also heighten risk of mental health problems. Importantly, adverse childhood experiences (ACE) have repeatedly been found to increase the risk of mental health problems following deployment (Cabrera, Hoge, Bliese, Castro, & Messer, 2007). Moreover, presence of ACE has been linked to PTSD severity as well as the presence of what is sometimes called symptoms of complex PTSD (Brewin et al., 2017).
The latest version of the WHO International Classification of Diseases 11th version (ICD-11; World Health Organization, 2018) includes two ‘sibling disorders’ within the section on Disorders Specifically Associated with Stress: PTSD and a new diagnosis of complex PTSD (CPTSD). The ICD-11 model of PTSD includes symptoms reflecting (1) re-experiencing of the trauma in the present, (2) avoidance of traumatic reminders, and (3) a persistent sense of threat. CPTSD retains the core symptoms of PTSD plus additional symptoms that identify ‘disturbances in self-organization’ (DSO): (1) affective dysregulation, (2) negative self-concept, and (3) disturbances in relationships. ICD-11 CPTSD has been scrutinized in a growing number of empirical studies, most commonly using mixture models, such as latent class and latent profile analysis (LCA/LPA). Across a range of trauma-exposed individuals, research evidence is largely supportive of the ICD-11 distinction between PTSD and CPTSD in both clinical (Böttche et al., 2018; Karatzias et al., 2017; Kazlauskas, Gegieckaite, Hyland, Zelviene, & Cloitre, 2018) and community samples (Knefel, Garvert, Cloitre, & Lueger-Schuster, 2015; Palic et al., 2016).
However, findings are inconclusive with regards to the distinction of PTSD and CPTSD in military samples (Mordeno, Nalipay, & Mordeno, 2019; Murphy et al., 2020; Palic et al., 2016; Wolf et al., 2015). While a study on the ICD-11 model of PTSD and CPTSD in 323 trauma-exposed U.S. veterans found that PTSD and CPTSD are not clearly distinct constructs (Wolf et al., 2015), more recent studies of Israeli veterans (Palic et al., 2016), Filipino combat-exposed soldiers (Mordeno et al., 2019), and UK veterans (Murphy et al., 2020) found support for the distinction between PTSD and CPTSD. Recently, our research group applied LPA in a large treatment-seeking sample of Danish veterans (N = 1.541; Folke et al., 2019) and found evidence for distinct PTSD and CPTSD symptom profiles. Further, we identified groups of low symptoms, low DSO-symptoms, elevated hyperarousal-symptoms, and high DSO-symptoms. ACE were found to be a significant risk factor for CPTSD, and CPTSD-class members were more likely to live alone and use psychotropic medication compared to the PTSD-class (Folke et al., 2019). A major limitation of this study, however, was that it used a proxy measure of ICD-11 PTSD and DSO-symptoms.
To date, no studies have explored symptom profiles using mixture models based on the ICD-11 PTSD and CPTSD scale (i.e. the International Trauma Questionnaire (ITQ); Cloitre et al., 2018) in military samples. Addressing this gap in the literature will determine the applicability of the PTSD/CPTSD distinction in military samples and pave the way for research on the potential need for targeted treatment of CPTSD.
Here, we present a replication of Folke et al. (2019) and aim to identify distinct symptom profiles of PTSD and CPTSD using the ITQ in a new sample of previously deployed treatment-seeking soldiers. In accordance with Folke et al. (2019) we hypothesize (1) that separate classes representing PTSD and CPTSD will be found, (2) that more traumatic life events, particularly in childhood, will predict membership of a CPTSD class, and (3) that a potential distinction between PTSD and CPTSD will be associated with sociodemographic and functional outcomes.
2. Methods
2.1. Participants
Previously deployed soldiers were recruited from the Military Psychology Department (MPD) of the Danish Defence between 25 October 2019 and 2 November 2020. In the MPD, previously deployed soldiers, whether still employed by the defence or not, can refer themselves for treatment. All who, at an intake session, are assessed to have mental health problems related to their deployment will be offered treatment. For this study, we included everyone who completed the on-line initial assessment questionnaire and were referred on to treatment (N = 294), i.e. who had mental health problems related to their deployment experiences. We therefore had no missing data.
2.2. Measures
PTSD and CPTSD symptoms were assessed with the Danish version of the ITQ (Danish translation by Hansen et al., 2017). Six items assessed PTSD-symptoms, and six items assessed DSO-symptoms. Cronbach’s alpha for the PTSD-subscale was 0.89 and for the DSO-subscale 0.88.
We created a measure of childhood trauma (ACE) by summing three items concerning childhood trauma; witnessing violence in the family, physical punishment, and sexual abuse in the Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000). The remaining items were summed to arrive at a total measure of adult life trauma. We Z-transformed the total scores to arrive at comparable estimates. Further, age, gender, marital status, psychotropic medicine use, and occupational status (employed vs. unemployed vs. sickness benefits) were included as covariates in the models (see Folke et al. (2019)).
2.3. Statistical analyses
Classes were identified by LPA as implemented in MPlus version 8.2 (Muthén & Muthén, 1998). The procedure for model selection in LPA is described in detail in Folke et al. (2019). Briefly, we ran a series of models with increasing number of classes and selected the final model based on fit indices (Akaike and Bayesian), likelihood ratio tests (Lo-Mendel-Rubin (LMR-LRT) and bootstrapped (BLRT)), interpretability, class sizes and parsimony. To test predictors of class membership and evaluate potential class differences across covariates, we applied a 3-step method where class formation and covariate estimation was done successively while accounting for the probabilistic nature of class assignment (Vermunt, 2010).
3. Results
3.1. Descriptives
Descriptives can be seen in Table 1. Based on ITQ 15.3% and 30.3% fulfilled the criteria for PTSD and CPTSD, respectively.
Table 1.
Sample descriptives of Danish veterans referred on to treatment in the Military Psychology Department of the Danish Defence (n = 294)
| Variable | Mean (SD)/Number (%) |
|---|---|
| Age (Mean (SD)) | 39.7 (9.8) |
| Gender (male) | 272 (92.5%) |
| Civilian status (single/divorced/widowed) | 69 (23.5%) |
| Employment | |
| – Unemployed | 14 (4.8%) |
| – Receiving sickness benefits | 39 (13.3%) |
| Currently using psychotropic medicine | 70 (23.8%) |
| Has experienced childhood trauma | 84 (28.6%) |
| Has experienced at least one adult life trauma | 294 (100%) |
| Has been exposed to combat | 230 (78.2%) |
| PTSD according to ICD-11 criteria | 45 (15.3%) |
| CPTSD according to ICD-11 criteria | 89 (30.3%) |
3.2. Model results
Table 2 shows fit indices of models with 1–6 classes. While reductions in fit indices are seen throughout, they become very small with the addition of classes five and six. The LMR-LRT test becomes insignificant with the addition of the third class while the BLRT remains significant with addition of each new class up to six classes. Class sizes are reasonable for all models. All models up to the 6-class model are interpretable, however, in the 5- and 6-class models, some groups share very great resemblance and these models are therefore not considered parsimonious. Based on all information, the 4-class model was selected as the best-fitting, most parsimonious representation of the data (entropy was 0.92).
Table 2.
Latent class models, fit indices, likelihood ratio tests and class proportions
| AIC | BIC | SSA-BIC | LMR-LrT | BLRT | Class proportions (%) | |
|---|---|---|---|---|---|---|
| 1 class | 12453 | 12541 | 12466 | |||
| 2 classes | 11272 | 11408 | 11291 | <0.0001 | <0.0001 | 48/52 |
| 3 classes | 11009 | 11193 | 11035 | 0.115 | <0.0001 | 38/23/39 |
| 4 classes | 10755 | 10987 | 10788 | 0.108 | <0.0001 | 17/30/29/23 |
| 5 classes | 10686 | 10966 | 10724 | 0.425 | <0.0001 | 24/13/22/28/13 |
| 6 classes | 10618 | 10946 | 10664 | 0.460 | <0.0001 | 17/12/12/15/16/28 |
AIC = Akaike information criteria, BIC = Bayesian Information Criteria, SSA-BIC = Sample-size adjusted BIC, LMR-LRT = Lo-Mendell-Rubin Likelihood Ratio Test, BLRT = Bootstrapped Likelihood Ratio Test.
Class characteristics (Figure 1) show that 30.5% of the participants had low symptoms across both symptom groups (‘Low symptoms’), while 17.3% had low PTSD-symptoms but elevated DSO-symptoms (‘DSO’). An additional 23.5% showed a pattern of high PTSD-symptom level and lower DSO-symptom level, particularly low for the two negative self-concept items (‘PTSD’). Finally, 28.7% had high symptom-level across PTSD as well as DSO-symptoms (‘CPTSD’).
Figure 1.
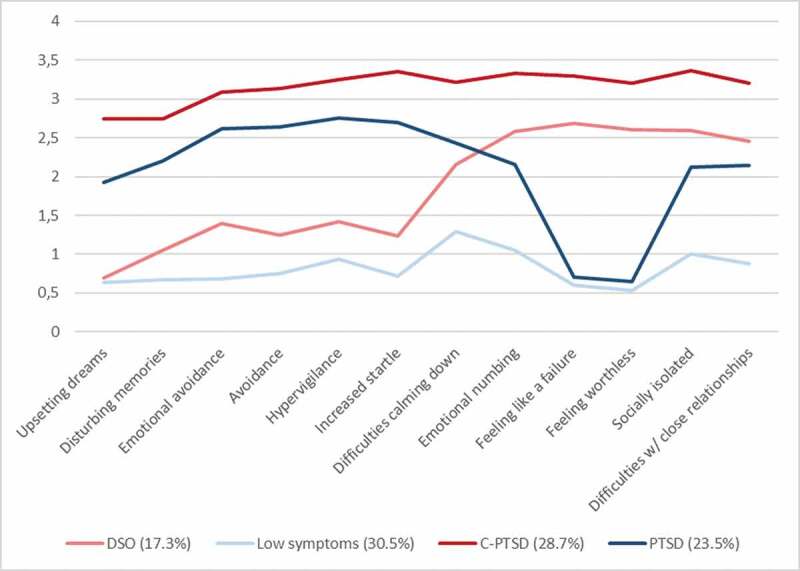
Plot of the 4-class model
3.3. Prediction of class membership and difference in outcomes between classes
In the multinomial regression analysis with class membership as dependent variable and CPTSD as reference, age was predictive of membership of all classes (Table 3): Higher age made membership of the Low Symptoms and DSO-classes less likely (Low symptoms: OR = 0.69 (0.51–0.93), p= .014, DSO: OR = 0.50 (0.35–0.72), p< .001) and membership of the PTSD-class more likely (OR = 1.56 (1.17–2.08), p= .042) in comparison to the CPTSD-class. Further, more traumatic events in adult life made membership of the Low Symptoms-class less likely in comparison to the CPTSD-class (OR = 0.56 (0.41–0.76), p< .001). ACE was not significantly related with membership in any class.
Table 3.
Multinomial regression analysis with class membership as the dependent variable with CPTSD class as reference. Results are presented as odds ratios with 95% confidence intervals
| Age | Childhood traumatic events (ACE) |
Adult life traumatic events | |
|---|---|---|---|
| Low symptoms | 0.69* (0.51–0.93) |
1.12 (0.84–1.48) |
0.56*** (0.41–0.76) |
| DSO | 0.50*** (0.35–0.72) |
0.84 (0.56–1.26) |
0.81 (0.56–1.18) |
| PTSD | 1.56* (1.17–2.08) |
1.17 (0.89–1.55) |
0.77 (0.60–1.00) |
* p< 0.05, ** p< 0.01, *** p< 0.001.
Figure 2 shows the proportion of relevant covariates across classes: single/divorced/widowed, psychotropic medication users, unemployed and those receiving sickness benefits. Overall comparisons reveal differences between classes in marital status (χ2(df = 3) = 10.4, p = .016) as well as in psychotropic medicine use (χ2(df = 3) = 27.4, p < .001), but not in employment status. Specifically, more individuals in the CPTSD-class were single/divorced/widowed than in the PTSD and the Low Symptoms-classes, and more individuals in the DSO-class were single/divorced/widowed than in the PTSD-class. More individuals in the CPTSD-class reported current psychotropic medicine use than in the Low Symptoms and DSO-classes, and more individuals in the PTSD-class reported current psychotropic medicine use than in the Low Symptoms and DSO-classes.
Figure 2.
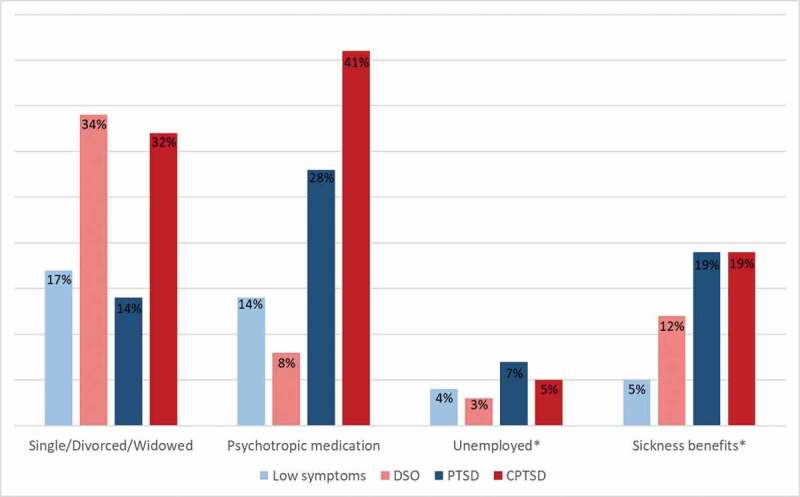
Proportion of individuals in each class who are single/divorced/widowed, uses psychotropic medication, are unemployed or receives sickness benefits
Notes: *Unemployed and sickness benefits are coded as a three-category variable (unemployed, sickness benefits, in some way occupied (work, student, etc.)).
4. Discussion
In line with Folke et al. (2019), this study identified classes that were clearly delineated based on the presence or absence of PTSD and DSO symptoms. In more detail, we identified four groups: (1) high CPTSD symptoms (‘CPTSD’, 28.7%), (2) high PTSD and relatively lower DSO symptoms (‘PTSD’, 23.5%), (3) high DSO symptoms (‘DSO’, 17.3%); and (4) low symptoms (‘Low Symptoms’, 30.5%). Neither childhood nor adult life trauma could predict PTSD or CPTSD class membership. Membership of more symptomatic classes was associated with negative functional outcomes.
The identified model with 4 classes deviates from the 6-class model in Folke et al. (2019). This might very likely reflect the larger sample size in our previous study, in that the extracted number of classes in LPA is somewhat sample size-dependent (Brewin et al., 2017). Previous studies in clinical samples (Karatzias et al., 2017; Kazlauskas et al., 2018) have typically identified 3 classes (PTSD, CPTSD, and Low symptoms), while studies in larger and more heterogeneous clinical and community samples (Böttche et al., 2018; Knefel et al., 2015; Palic et al., 2016) have typically reported 4 or more classes. The four identified classes in this study clearly mirror four of the classes of Folke et al. (2019) and hence, it replicates the finding of a PTSD-class, a CPTSD-class, a DSO-class, and a low symptoms-class. Further, the prevalence of the CPTSD class (28.7%) is much in line with the prevalence of CPTSD as defined by the ITQ, while the PTSD-prevalence is lower when defined by the ITQ-criteria (15.3%) as compared to the PTSD-class identified by LPA (23.5%).
In our 2019-study, we found that less ACE increased the likelihood membership of PTSD-class membership compared to CPTSD-class membership. This was not replicated in the current study, which could be a result of our smaller sample size. Moreover, ACE was measured with the TLEQ, which does not include emotional abuse and emotional neglect during childhood; specific types of ACE that have previously shown high predictive power (Karatzias et al., 2017; Knefel et al., 2015). Only age was a significant factor in predicting class membership across the PTSD and CPTSD-class.
As in our previous study, we found clear differences in functional outcomes across classes: The CPTSD class was more often single/divorced/widowed compared to the PTSD class. Moreover, the CPTSD class more often used psychotropic medicine compared to the DSO-class and Low Symptoms-class. No overall difference between classes in employment and sickness benefits was found. The difference in functional impairment across classes illustrates the usefulness of the PTSD/CPTSD-distinction in military samples.
4.1. Limitations
We did not consider diagnostic comorbidities such as depression, anxiety or substance use. Future research should explore the comorbidities nature and type associated with each disorder. It is unknown how well the findings apply to female military veterans. Further, larger sample sizes may be needed to identify all relevant symptom profiles and covariates.
5. Conclusions
Using the ITQ, we replicated findings from our previous LPA study of treatment-seeking veterans identifying two distinct classes of individuals with symptom profiles consistent with the ICD-11 PTSD and CPTSD, an additional DSO-only class as well as a Low symptoms-class. CPTSD seems to be a more debilitating condition than PTSD, as seen by more severe functional outcomes, which has implications for treatment planning.
6. Implications for clinicians and future research
The continued empirical support for ICD-11 CPTSD should encourage clinicians to screen for DSO symptomatology, and emphasizes the need for treatment interventions specifically tailored to address these symptoms. New modular treatment approaches for CPTSD have been suggested (Karatzias & Cloitre, 2019). Future studies should investigate the effects of these treatments on PTSD and DSO symptoms.
Acknowledgments
We thank all veterans who filled out the questionnaires prior to treatment start at the Military Psychology Department within the Danish Defence.
Funding Statement
This work was not supported by any funding.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability
Due to privacy and data protection regulations of the Danish Defence, data from the current study cannot be shared.
Ethical approval
In Denmark, studies that do not include interventions or human biological material should not be subjected to the National Committee on Health Research Ethics. All participants provided informed consent.
References
- Böttche, M., Ehring, T., Krüger-Gottschalk, A., Rau, H., Schäfer, I., Schellong, J., … Knaevelsrud, C. (2018). Testing the ICD-11 proposal for complex PTSD in trauma-exposed adults: Factor structure and symptom profiles. European Journal of Psychotraumatology, 9(1), 1512264. doi: 10.1080/20008198.2018.1512264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin, C. R., Cloitre, M., Hyland, P., Shevlin, M., Maercker, A., Bryant, R. A., … Reed, G. M. (2017). A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clinical Psychology Review, 58, 1–7. doi: 10.1016/j.cpr.2017.09.001 [DOI] [PubMed] [Google Scholar]
- Cabrera, O. A., Hoge, C. W., Bliese, P. D., Castro, C. A., & Messer, S. C. (2007). Childhood adversity and combat as predictors of depression and post-traumatic stress in deployed troops. American Journal of Preventive Medicine, 33(2), 77–82. doi: 10.1016/j.amepre.2007.03.019 [DOI] [PubMed] [Google Scholar]
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. doi: 10.1111/acps.12956 [DOI] [PubMed] [Google Scholar]
- Folke, S., Nielsen, A. B. S., Andersen, S. B., Karatzias, T., & Karstoft, K. I. (2019). ICD-11 PTSD and complex PTSD in treatment-seeking Danish veterans: A latent profile analysis. European Journal of Psychotraumatology, 10(1), 1686806. doi: 10.1080/20008198.2019.1686806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes, D., Pedlar, D., Adler, A. B., Bennett, C., Bryant, R., Busuttil, W., … Wessely, S. (2019). Treatment of military-related post-traumatic stress disorder: Challenges, innovations, and the way forward. International Review of Psychiatry, 1–16. doi: 10.1080/09540261.2019.1595545 [DOI] [PubMed] [Google Scholar]
- Hansen, M., Hyland, P., Karstoft, K.-I., Vaegter, H. B., Bramsen, R. H., Nielsen, A. B. S., … Andersen, T. E. (2017). Does size really matter? A multisite study assessing the latent structure of the proposed ICD-11 and DSM-5 diagnostic criteria for PTSD. European Journal of Psychotraumatology, 8(sup7), 1398002. doi: 10.1080/20008198.2017.1398002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karatzias, T., & Cloitre, M. (2019). Treating adults with complex posttraumatic stress disorder using a modular approach to treatment: Rationale, evidence, and directions for future research. Journal of Traumatic Stress, 32(6), 870–876. doi: 10.1002/jts.22457 [DOI] [PubMed] [Google Scholar]
- Karatzias, T., Shevlin, M., Fyvie, C., Hyland, P., Efthymiadou, E., Wilson, D., … Cloitre, M. (2017). Evidence of distinct profiles of Posttraumatic Stress Disorder (PTSD) and Complex Posttraumatic Stress Disorder (CPTSD) based on the new ICD-11 Trauma Questionnaire (ICD-TQ). Journal of Affective Disorders, 207, 181–187. doi: 10.1016/j.jad.2016.09.032 [DOI] [PubMed] [Google Scholar]
- Kazlauskas, E., Gegieckaite, G., Hyland, P., Zelviene, P., & Cloitre, M. (2018). The structure of ICD-11 PTSD and complex PTSD in Lithuanian mental health services. European Journal of Psychotraumatology, 9(1), 1414559. doi: 10.1080/20008198.2017.1414559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knefel, M., Garvert, D. W., Cloitre, M., & Lueger-Schuster, B. (2015). Update to an evaluation of ICD-11 PTSD and complex PTSD criteria in a sample of adult survivors of childhood institutional abuse by Knefel & Lueger-Schuster (2013): A latent profile analysis. European Journal of Psychotraumatology, 6(1), 25290. doi: 10.3402/ejpt.v6.25290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubany, E. S., Leisen, M. B., Kaplan, A. S., Watson, S. B., Haynes, S. N., Owens, J. A., & Burns, K. (2000). Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment, 12(2), 210–224. doi: 10.1037/1040-3590.12.2.210 [DOI] [PubMed] [Google Scholar]
- Madsen, T., Andersen, S. B., & Karstoft, K.-I. (2016). Are posttraumatic stress symptoms related to mental health service use? A prospective study of Danish soldiers deployed to Afghanistan. The Journal of Clinical Psychiatry, 77(10), 1226–1232. doi: 10.4088/JCP.15m10088 [DOI] [PubMed] [Google Scholar]
- Mordeno, I. G., Nalipay, M. J. N., & Mordeno, E. R. (2019). The factor structure of complex PTSD in combat-exposed Filipino soldiers. Psychiatry Research, 278, 65–69. doi: 10.1016/j.psychres.2019.05.035 [DOI] [PubMed] [Google Scholar]
- Murphy, D., Shevlin, M., Pearson, E., Greenberg, N., Wessely, S., Busuttil, W., & Karatzias, T. (2020). A validation study of the International Trauma Questionnaire to assess post-traumatic stress disorder in treatment-seeking veterans. The British Journal of Psychiatry, 216(3), 132–137. doi: 10.1192/bjp.2020.9 [DOI] [PubMed] [Google Scholar]
- Muthén, L. K., & Muthén, B. (1998). Mplus user’s guide (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Palic, S., Zerach, G., Shevlin, M., Zeligman, Z., Elklit, A., & Solomon, Z. (2016). Evidence of complex posttraumatic stress disorder (CPTSD) across populations with prolonged trauma of varying interpersonal intensity and ages of exposure. Psychiatry Research, 246, 692–699. doi: 10.1016/j.psychres.2016.10.062 [DOI] [PubMed] [Google Scholar]
- Vermunt, J. K. (2010). Latent class modeling with covariates: Two improved three-step approaches. Political Analysis, 18(4), 450–469. doi: 10.1093/pan/mpq025 [DOI] [Google Scholar]
- Wolf, E. J., Miller, M. W., Kilpatrick, D., Resnick, H. S., Badour, C. L., Marx, B. P., … Friedman, M. J. (2015). ICD–11 Complex PTSD in U.S. National and Veteran Samples: Prevalence and structural associations with PTSD. Clinical Psychological Science, 3(2), 215–229. doi: 10.1177/2167702614545480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2018). International classification of diseases for mortality and morbidity statistics (11th ed.). Retrieved from https://icd.who.int/browse11/l-m/en [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to privacy and data protection regulations of the Danish Defence, data from the current study cannot be shared.


