Abstract
Objective
The objective of this systematic review was to investigate the quality and outcome of studies into artificial intelligence techniques, analysis, and effect in dentistry.
Materials and Methods
Using the MeSH keywords: artificial intelligence (AI), dentistry, AI in dentistry, neural networks and dentistry, machine learning, AI dental imaging, and AI treatment recommendations and dentistry. Two investigators performed an electronic search in 5 databases: PubMed/MEDLINE (National Library of Medicine), Scopus (Elsevier), ScienceDirect databases (Elsevier), Web of Science (Clarivate Analytics), and the Cochrane Collaboration (Wiley). The English language articles reporting on AI in different dental specialties were screened for eligibility. Thirty-two full-text articles were selected and systematically analyzed according to a predefined inclusion criterion. These articles were analyzed as per a specific research question, and the relevant data based on article general characteristics, study and control groups, assessment methods, outcomes, and quality assessment were extracted.
Results
The initial search identified 175 articles related to AI in dentistry based on the title and abstracts. The full text of 38 articles was assessed for eligibility to exclude studies not fulfilling the inclusion criteria. Six articles not related to AI in dentistry were excluded. Thirty-two articles were included in the systematic review. It was revealed that AI provides accurate patient management, dental diagnosis, prediction, and decision making. Artificial intelligence appeared as a reliable modality to enhance future implications in the various fields of dentistry, i.e., diagnostic dentistry, patient management, head and neck cancer, restorative dentistry, prosthetic dental sciences, orthodontics, radiology, and periodontics.
Conclusion
The included studies describe that AI is a reliable tool to make dental care smooth, better, time-saving, and economical for practitioners. AI benefits them in fulfilling patient demand and expectations. The dentists can use AI to ensure quality treatment, better oral health care outcome, and achieve precision. AI can help to predict failures in clinical scenarios and depict reliable solutions. However, AI is increasing the scope of state-of-the-art models in dentistry but is still under development. Further studies are required to assess the clinical performance of AI techniques in dentistry.
1. Introduction
Artificial intelligence (AI) is a general term which refers to perform the task of human beings with the help of machine and technology. According to “Barr and Feigenbaum,” AI is the part of computer science concerned with designing an intelligent computer system that exhibits characteristics we associate with intelligence in human behavior-understanding language, learning, reasoning, problem solving, and many more [1]. There are subcategories of AI, which is machine learning and its allied fields like deep learning, cognitive computing, natural language processing, robotics, expert systems, and fuzzy logic. Machine learning is a subgroup of AI which enhances automated learning ability without being distinctly programmed. Its primary goal is to allow automated learning without human arbitration. AI models predict future events with the present set of observations [2]. The schematic presentation of AI and a human intelligence model is shown in Figures 1 and 2.
Figure 1.
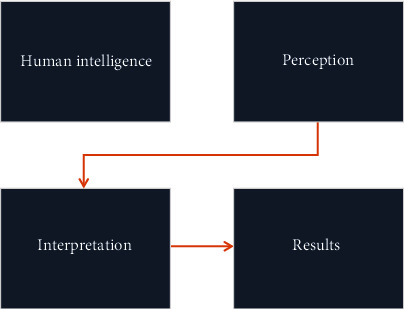
Schematic illustration of human intelligence networking.
Figure 2.
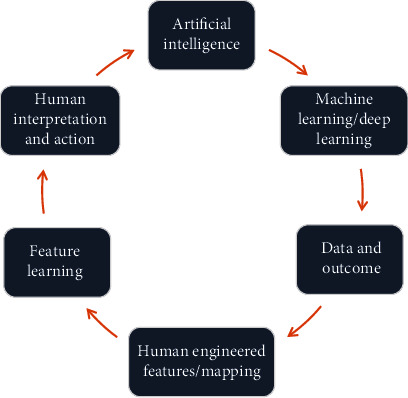
Schematic illustration of artificial intelligence model.
AI, similar to other fields, is transforming as an emerging field of dentistry. AI can perform a number of simple tasks in the dental clinic with greater precision, less staffing, and fewer errors than human counterparts; from booking and coordinating regular appointments to assisting the clinical diagnosis and treatment planning, AI can handle all [3]. The AI application showed high accuracy, sensitivity, specificity, and precision in detection and classification of malocclusion in orthodontics [4]. AI can automatically detect and classify dental restorations on panoramic radiographs along with assistance in the detection of dental and maxillofacial abnormalities such as periodontal diseases, root caries, bony lesions, i.e., BRONJ (bisphosphonate-related osteonecrosis of the jaw) associated with dental extraction, and facial defects [3, 5].
A popular field in machine learning is “deep learning,” where multilayered (deep) neural networks are used to learn hierarchical features in the data. Deep learning refers to the process of data (e.g., images) and corresponding labels (e.g., “carious tooth,” or “specific area on an image where a caries lesion is present”) being repetitively passed through the neural network during training, with the model parameters (so-called weights) being iteratively adjusted to improve the model's accuracy [1]. A deep learning-based convolutional neural network (CNN) algorithm considerably performed well in detecting dental caries in periapical radiographs [6]. It also successfully helped in detecting and classifying impacted supernumerary teeth in patients with fully erupted maxillary permanent incisors on panoramic radiographs [7]. The fully deep, fine-tuned mask R-CNN model performed well in automated tooth segmentation on panoramic images [8]. Additionally, it was also used for detecting apical lesions on panoramic radiographs [9].
Recently, an investigation showed that artificial neural networks (ANNs) could act as a second opinion to locate the apical foreman on radiographs and to enhance the accuracy of working length determination by radiography [10]. In another in vitro study, ANN also aided in the determination of shade, light-curing unit, and composite Vickers hardness ratio of bottom to top composites [11]. AI technology is found useful in assisting debonding probability of composite restorations in restorative dentistry [12].
Furthermore, an automated robotic system can fulfill the requirements of typical dental operations with accurate, safe, and three-dimensional (3D) tooth preparation [13, 14]. The AI convolutional neural network (CNN) can be utilized for classifying dental arches and designing removable partial dentures [15]. AI can analyze the impact of orthognathic treatment on facial attractiveness and age appearance. It offers a new feature that permits scoring of facial attractiveness and apparent age objectively and reproducibly [16]. Automated integration of facial and intraoral images of anterior teeth benefits dentists to analyze the shape and position of maxillary anterior teeth [17].
In a nutshell, the last decade has seen a surged with breakthrough in advancement of technology associated with artificial intelligence. However, it is still uncertain how information available in the literature regarding AI can assist in diagnosis, planning, and management of dental diseases. Therefore, to understand the current trends of AI in dentistry and its application, a systematic review was carried out on studies which have discussed different modalities of artificial intelligence, its application, and outcome in dentistry.
2. Materials and Methods
2.1. Focused Question
This systematic review was conducted using PRISMA (Preferred Reported Items for Systematic Review and Meta-analysis) guidelines. Our intended question was “Which artificial intelligence techniques are practiced in dentistry, and how AI is improving the diagnosis, clinical decision making, and outcome of dental treatment?” The question was constructed according to the Participants Intervention Comparison Outcome and Study (PICOS) strategy [18].
Population: patient/simulator faciodental images (two-dimensional image (2D), three-dimensional (3D), radiographs (periapical, bitewing, orthopantomography, and cone-beam computed tomography), CAD/CAM (computer-aided design and computer-aided manufacturing). Virtual dental models.
Intervention: AI techniques (deep learning, natural language processing, and robotics) applied in diagnosis, management, and predicting prognosis of dental treatment.
Comparison: automatic algorithm, testing models, image analysis, and rater opinions.
Outcome: analysis of AI performance, accuracy/precision, sensitivity, rating, CDS: clinical decision support, AUC: area under the curve, and AI applicability in different dental specialties.
Study design type: for this review, we considered both observational (case control and cohort) and interventional (trials) based studies, published in the English language.
2.2. Eligibility Criteria
The subsequent articles were reviewed for inclusion criteria: (1) original articles relevant to AI in dentistry, (2) clinical trials, (3) nonclinical trials, (4) observational studies, and (5) English language articles, whereas review articles, letters to editors, commentaries, grey literature, case reports, and articles with less than 10 participants or specimen were excluded.
2.3. Search Methodology
The medical subject heading (MeSH) terms are artificial intelligence (AI), dentistry, AI in dentistry, neural networks and dentistry, machine learning, AI dental imaging, and AI treatment recommendations; electronic search was carried out with PubMed/MEDLINE, ScienceDirect, Scopus, Web of Science, and Cochrane Collaboration databases. The articles published in the years 2000 to 2020 were targeted. The duration of data extraction was between 10 and 12 weeks. The last search was performed in the month of January 2020. Two calibrated reviewers (N.A. and W.Q.) performed the search. Disagreements and discrepancies were resolved by consensus, and a third examiner (F.Z.) was consulted. All the titles and abstracts were read thoroughly from the articles searched primarily, and nonrelevant studies were excluded. The relevant articles were enlisted and scrutinized for any similar studies which matched our inclusion criteria. For extraction of pertinent results, we read full texts of the included studies and the findings were recorded.
2.4. Quality Assessment of Included Studies
Quality assessment of included articles was carried out according to the standard parameters described in the Cochrane Handbook for Systematic Reviews of Interventions (v5.1.0) [19]. The parameters were patient randomization, blinding procedure, withdrawal/dropout reported; statistical analysis was used and stated clearly, execution of sample size estimation, multiple variables measurement, clear inclusion and exclusion criteria, comprehensible examiner reliability tested and clearly report all expected outcomes. The quality of each study was further classified into low, medium, and high risk of bias. The same 2 review authors autonomously sort out the search to amplify the number of studies recovered. The reviewers surveyed every selected article for the predefined consideration criteria and directed impartial appraisals, and any ambiguity was settled by discussion and agreement or by consultation with a third reviewer (F.Z.).
The Newcastle-Ottawa quality assessment scale (NOS) for case-control studies [20] was used for further analysis of the included articles. The analysis was based on the three core quality analysis parameters: case and group (selection, definition, and representativeness), comparability (comparison of case and control groups; analysis and control of confounding variable), and exposure (outcome assessment, i.e., analysis of golden percentage estimation in patients by different examiners; evaluation of study outcome related to different teeth measurements clinically; use of a universal assessment method for both control and case groups; dropout rate of patients in the included studies). A star system was adopted for rating the included studies. Each item in selection and outcome category received a maximum of 01 star while 02 stars were assigned for comparability if sufficiently reported. Each study total scored from 1 to 8 stars. Due to heterogeneity of the outcome and variables in selected studies, the research team was not able to conduct meta-analysis in the current review.
3. Results
3.1. Search Results
The primary search identified 175 articles based on key terms. Following those, 41 duplicates were removed, and 134 articles were screened based on title and abstracts. The search was further narrow down, and 96 irrelevant articles were excluded. The remaining 38 full-text articles were assessed for eligibility. Additionally, 6 full-text articles were further excluded. The 32 relevant articles were finally included and analyzed in the review. The PRISMA flow diagram for the literature search strategy is described in Figure 3. The excluded studies, in addition to their reasons for exclusion, are mentioned in Table 1.
Figure 3.
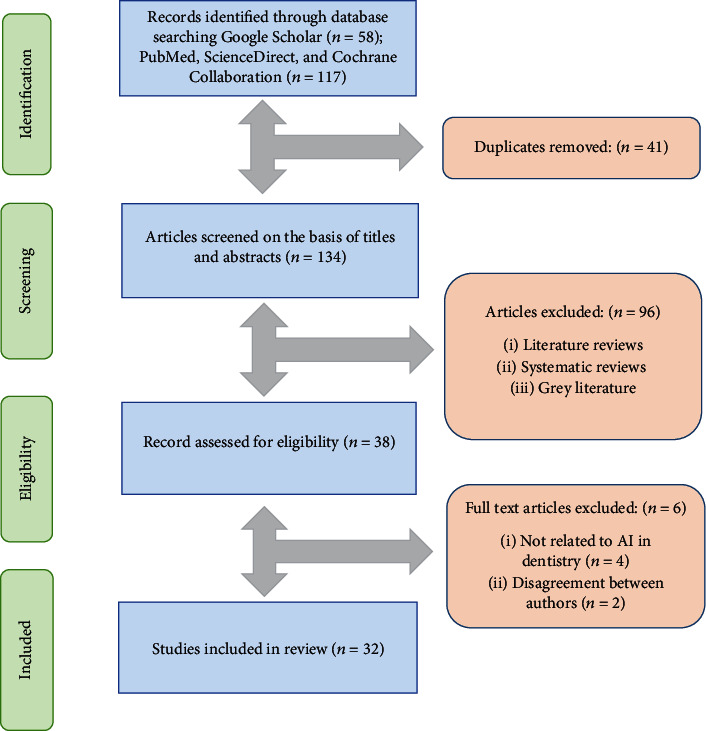
The PRISMA flow diagram for literature search performed in this study.
Table 1.
Methodological list of studies excluded from this review and reasons for exclusion (n = 5).
| Author and year | Reason of exclusion |
|---|---|
| Gould [21] 2002 | Disagreement between authors |
| Van der Meer et al. [22] 2016 | Not AI, it was related to 3D printing guides |
| Vera et al. [23] 2013 | AI-related to dental biotechnology |
| Leeson [24] 2020 | Disagreement between authors |
| Rekow [25] 2020 | Not AI, it was related to digital dentistry |
| McCracken et al. [26] 2000 | Not AI, it was related to computer-assisted learning program |
AI: artificial intelligence.
3.2. General Characteristics of Included Studies
The general characteristics of the included studies are summarized in Table 2. The data were extracted from articles about the proposed study design: the authors' ID, year of publication, study and control groups, area of application in dentistry, assessment methods, follow-up period, and outcome of the study.
Table 2.
Characteristics of selected studies (n = 33).
| Author and year | Study design | Groups | Application | Assessment method | Follow-up period | Outcome | |
|---|---|---|---|---|---|---|---|
| Study | Control | ||||||
| Abdalla-Aslan et al. [5] 2020 | Cohort study | Machine learning computer vision algorithms | NA | OD | Automatic algorithm was used to detection and classification restoration while vector machine algorithm with error-correcting output codes was applied for cross-validation | NA | Machine learning demonstrated excellent performance in detecting and classifying dental restorations on panoramic images |
| Bouchahma et al. [6] 2019 | Clinical trial | CNN | NM | OD and endodontics | Prediction of three types of treatments; fluoride, filling, and root canal treatments. The model was trained to learn on dataset of 200 X-ray images of patients' teeth collected | NM | DL overall accuracy was 87%. The best prediction was the fluoride treatment with 98%, followed by RCT detection 88% and filling 77% |
| Kuwada et al. [7] 2020 | Clinical trial | DetectNet, AlexNet, and VGG-16 | NM | OD | 400 images were randomly selected as training data, and 100 as validating and testing data. The remaining 50 images were used as new testing data. Recall, precision, and F-measure were used for detection of impacted teeth | NM | DetectNet and AlexNet appear to have potential use in classifying the presence of impacted supernumerary teeth in the maxillary incisor region on PR, while VGG-16 showed lower values |
| Lee et al. [8] 2020 | Clinical trial | CNN on 20 automated 20 tooth segments | Oral radiologist manually performed individual tooth annotation on the PA | OD and forensic dentistry | 846 images with tooth annotations from 30 PA were used for training, and 20 as the validation and test sets. A fully deep learning method using the mask R-CNN model was implemented through a fine-tuning process to detect and localize the tooth structures | NM | It achieved high performance for automation of tooth segmentation on dental panoramic images. The proposed method might be applied in the first step of diagnosis automation and in forensic identification |
| Ekert et al. [9] 2019 | Clinical trial | CNN to detect AL | Six independent examiners detect AL | Endodontics and OD | NN was trained and validated via 10 times repeated group shuffling. Results were compared with the majority vote of 6 examiners who detected ALs on an ordinal scale | NM | A moderately deep CNN showed satisfying discriminatory ability to detect ALs on panoramic radiographs |
| Saghiri et al. [10] 2012 | Clinical trial | ANN | Endodontist's opinion | Endodontics | Working length was determined and confirmed radiographically by endodontists and compared with ANN, and stereomicroscope as a gold standard after tooth extraction in cadaver | NM | ANN was more accurate than endodontists' determinations when compared with measurements by using the stereomicroscope |
| Arisu et al. [11] 2018 | Clinical trial | ANN | NM | Restorative dentistry | Obtained measurements and data were fed to an ANN to establish the correlation between the inputs; composite shade curing units and outputs; tooth number | NM | ANN showed that the light-curing units and composite parameter had the most significant effect on the bottom to top Vickers hardness ratio of the composites |
| Yamaguchi et al. [12] 2019 | Clinical trial | 12 dislodge CAD/CAM composite resin crowns with DL | 12 trouble-free CAD/CAM composite resin crowns | Restorative dentistry | Convolution neural network (CNN) technique was used to predict debonding of composite crowns using 2D images captured from 3D stereolithography models | NM | Deep learning with CNN model showed good performance in terms of dislodgement predictability of composite crowns through 3D stereolithography models |
| Otani et al. [13] 2015 | Experimental study | Ten veneer preparation with a robotic arm | Ten conventional veneers prepared by a clinician | Restorative dentistry | Accuracy and precision of veneer preparation were compared for all sites and separately for each tooth surface (facial, finish line, incisal) through 3D images and computation | NM | The robotic arm was able to prepare the tooth model as accurately as the control. However, a better finish line accuracy and precision was showed by the robotic arm |
| Wang et al. [14] 2014 | Experimental study | Automatic laser ablation system for tooth crown preparation | NM | Prosthodontics | A layer-by-layer ablation method is developed to control the laser focus during the crown preparation | NM | The movement range and the resolution of the robotic system meet the satisfying requirements of typical dental operations for clinical crown preparation |
| Takahashi et al. [15] 2020 | Experimental study | CNN | NM | Prosthodontics and OD | 1184 images of dental arches were classified into four arch types. A CNN method to classify images was developed using tensor flow and Kera's deep learning libraries | NM | The results of this study suggest that dental arches can be classified and predicted using a CNN |
| Patcas et al. [16] 2019 | Cohort study | CNN was applied in posttreatment photographs of 146 orthognathic patients | Pretreatment photographs of 146 patients | Orthodontics | CNN-based technique was used to compare facial attractiveness and apparent age of patients through pre- and posttreatment photographs | NA | Artificial intelligence can be used to detect facial attractiveness scores and apparent age in orthognathic surgery patients |
| Li et al. [17] 2020 | Clinical trial | 50 oral images and 274 anterior through automated photo integrating system | Manual segmentation system | Esthetic dentistry | The facial and intraoral key points were detected by an automatic algorithm and compared with manual segmentation on standard photographs | NM | The proposed automated system can eliminate the need for dentists to employ a laborious image integration process and has potential for broad applicability in the field of esthetic dentistry |
| Li et al. [44] 2015 | Experimental study | BPNN and GA neural network | Traditional neural network | Esthetic dentistry | The weighs and threshold values of GA and BPNN were compared for assistance in tooth color matching in dentistry | NM | GA and BP have practical application and can make teeth color matching objective and accurate |
| Edinger [30] 2004 | Clinical trial | ROSY, a robot-like electronic simulator | NM | Prosthodontics | Accuracy of the simulator was measured for all directions in space by registering eccentric jaw positions on both sides of 10 subjects | NM | Its accuracy may render it suitable for clinical applications |
| Meissner et al. [31] 2006 | Clinical trial | Automated smart ultrasonic calculus detection system | NM | Periodontics | The detection device is based on a conventional dental piezoelectric ultrasonic hand piece with a conventional scaler insert | NM | It was able to distinguish between different tooth surfaces in vitro independently from tip movements |
| Meissner et al. [32] 2005 | Clinical trial | A novel calculus recognition device applied on 70 extracted teeth | NM | Periodontics | Impulse generator, coupled to a conventional piezo-driven ultrasonic scaler, sends signals to the cementum via the tip of an ultrasound device | NM | This system is able to function correctly, independent of the lateral forces and the tip angle of the instrument |
| Devito et al. [33] 2008 | Clinical trial | Multilayer perceptron neural network | Twenty-five dental specialists with 20 years' experience | OD | Evaluation of proximal caries on radiographic through ANN | NM | AI improves the radiographic diagnosis of proximal caries by 39.4% |
| Kositbowornchai et al. [34] 2006 | Clinical trial | Learning vector quantization (LQV, NN) | NM | Restorative dentistry and OD | Tooth sections and microscopic examinations were used to confirm the actual dental caries status | NM | AI plays a useful and supporting in making dental caries diagnosis |
| Patcas et al. [35] 2019 | Clinical trial | Ten images evaluated by CNN model | Ten images were analyzed by laypeople, orthodontists, and oral surgeon on a visual analogue scale | Orthodontics | Decision on profile and frontal images of cleft patients were compared between CNN technique and conventional rater group to evaluate facial attractiveness | NM | AI can be a helpful tool to describe facial attractiveness and overall analysis were comparable with the rater groups |
| Lee et al. [36] 2018 | Clinical trial | CNN | Four calibrated board-certified dentists | OD and restorative dentistry | A pretrained GoogleNet Inception v3 CNN network was used for preprocessing and transfer learning | NM | CNN provides considerably good performance in detecting dental caries in PR |
| Vranckx et al. [37] 2020 | Clinical trial | CNN and ResNet-101 | Manual measurements by 2 observers | OD | CNN and ResNet-101 jointly predicted the molar segmentation maps and an estimate of the orientation lines | NM | Fast, accurate, and consistent automated measurement of molar angulations on dental PR |
| Lee et al. [38] 2020 | Clinical trial | Fifty cases of class2 TMJOA | Fifty cases of normal TMJ | OMFS | The condylar head was classified into 2 categories and tested by making 300 images | NM | AI can be used to support clinicians with diagnosis and decision making for treatments of TMJOA |
| Hung et al. [39] 2019 | Clinical study | Machine learning method ANN was used on bitewing radiograph | Training group consisting of conventional radiograph analysis | Gerontology | Support vector machine (ANN) was used to detect root caries on radiograph by determining AUC | NM | Support vector machine showed 97.1% accuracy, 95.1% precision, 99.6% sensitivity, and 94.3% specificity for root caries detection |
| Cui et al. [27] 2020 | Cohort study | CDS model applied to 3559 patient records | Two prosthodontists' opinion | OMFS | CDS model was used to predict the outcome of teeth extraction through electronic dental records | NA | The machine learning CDS was an efficient tool to predict teeth extraction outcome |
| Sornam and Prabhakaran [40] 2019 | Clinical study | LB-ABC with BPNN | BPNN classifier | Restorative dentistry | The BPNN classifier is compared with the LB-ABC-based BPNN classifier for dental caries classification | NM | The learning rate generated by the LB-ABC for the BPNN classifier achieved the best training and testing accuracy of 99.16% |
| Setzer et al. [41] 2020 | Clinical study | Evaluation of periapical lesion by DL method | Rating by OMF radiologist, an endodontist, and a senior graduate student | Endodontics | The CBCT segmentation was assessed by DL, CNN detection | NM | DL algorithm trained in a limited CBCT environment showed excellent results in lesion detection accuracy |
| Cantu et al. [42] 2020 | Clinical study | Caries detection on bitewing radiograph with DL | Opinion of four experienced dentists | OD, OR | CNN (U-Net) and Intersection-over-Union were used to detect caries on radiographs | NM | The deep neural network was accurate than dentists |
| Aliaga et al. [45] 2020 | Experimental study | Automatic computation and intelligent image segmentation of 370 radiographs | Expert dentist opinion | OD, OMFS | Automatic computation for analysis of mandibular indices and osteoporosis detection | NM | Automatic computation of mandibular indices and intelligent image segmentation was an efficient and reliable approach for early osteoporosis detection |
| Kim et al. [28] 2018 | Case-control study | Machine learning prediction models for BRONJ after extraction in 125 patients with drug use | Conventional methods, serum CTX level | OMFS/OM | Five machine learning methods such as logistic regression model, decision tree, support vector machine, ANN, and random forest were applied to predict BRONJ at extraction sites | NA | Machine learning showed superior performance in predicting BRONJ compared with serum CTX level and drug holiday period |
| Dumast et al. [29] 2018 | Case-control study | 17 tested OA subjects evaluated with deep CNN on 3D images | 17 age and sex-matched control subjects without OA | OMFS | Deep neural network classifier of 3D condylar morphology (ShapeVariationAnalyzer, SVA), and a flexible web-based system for data storage, computation and integration (DSCI) of high dimensional imaging, clinical, and biological data | NA | Deep neural network is a useful tool for classification of TMJOA |
| Sorkhabi and Khajeh [43] 2019 | Clinical trial | 3D deep CNN and CBCT | Postextraction clinical parameter measurements | OD and implant dentistry | 3D CNN method was used to measure alveolar bone density on CBCT images | 6 months | 3D deep CNN technique can accurately classify alveolar bone. Pattern, which is helpful in dental implant placement and diagnosis |
NA: not applicable; NM: not mentioned; OMFS: oral and maxillofacial surgery; OM: oral medicine; OP: oral pathology; OR: oral radiology; OD: oral diagnosis; AL: apical lesion; CNN: convolutional neural networks; ANN: artificial neural networks; 3D: three dimensional; DL: deep learning; CAL: computer-assisted learning; CAD/CAM: computer-aided design/computer-aided manufacturing; 2D: two dimensional; TMJOA: temporomandibular joint osteoarthritis; OA: osteoarthritis; BPNN: back-propagation neural networks; CDS: clinical decision support systems; BRONJ: bisphosphonate-related osteonecrosis of the jaw; LB-ABC: logit-based artificial bee colony optimization algorithm; VGG-16: Visual Geometry Group; PA: periapical radiograph; CBCT: cone-beam computerized tomography; GA: genetic algorithm; serum CTX: serum C-terminal telopeptide; AUC: area under the curve.
The included studies were ranged from the year 2000 to 2020. The studies were from four categories: cohort study [5, 16, 27], case control [28, 29], clinical trials [6–12, 17, 30–43], and experimental trials [13–15, 44, 45]. The follow-up period was mentioned in one study [43]. The various techniques of artificial intelligence was applied in the field oral and maxillofacial surgery [27–29, 38, 45], oral medicine [28], oral radiology [42], esthetic dentistry [17, 44], restorative dentistry [11–13, 34, 36, 40], endodontics [6, 9, 10, 41], oral diagnosis [5–9, 15, 33, 34, 36, 37, 42, 43, 45], orthodontics and orthognathic surgery [16, 35], forensic dentistry [8], gerodontology [39], implantology [43], periodontics [31, 32], and prosthodontics [14, 15, 30].
3.3. General Outcomes of Included Studies
The different modalities of artificial intelligence showed favorable outcomes. The deep learning with CNN's performed well in predicting the debonding probability of CAD/CAM crowns from 3D models [12], and it functioned considerably well in detecting apical lesion and dental caries in periapical (PA) and panoramic radiography [9, 36, 40, 42]. In addition to this, it has been proved to be accurate in predicting the treatment of dental decay based on radiographic images [6].
AI also has been proved to assist dentists in implant treatment starting from diagnosis to surgery by proficient and certain radiological evaluation [43]. Further, AI aided in the detection and classification of impacted supernumerary teeth, in the maxillary incisor region on periapical radiographs [7]. Along with AI, automation of tooth segmentation can be achieved through dental panoramic images [8].
CNN has been used to classify dental arches, and multilayer CNN also improves the radiographic diagnosis of proximal caries [33]. Machine learning computer algorithmic tool also facilitates detecting and classifying dental restoration in panoramic images [5]. ANN has been used to determine accurate working length on radiographs [10]. Likewise, a neural network and web-based system was able to assists in characterization of TMJ health and temporomandibular joint osteoarthritis (TMJOA) at clinical, imaging, and biological levels [29, 30, 38]. Furthermore, the computer color matching (CCM) technique provides an accurate color matching of dental restorations, together with the automatic laser ablation system for clinical crown preparation [14, 44]. Overall, the above methods if introduced into routine practice can be helpful in diagnosis and treating dental diseases.
3.4. Results of Quality Assessment
According to the standards described in the Cochrane Handbook for Systematic Reviews of Interventions (v5.1.0) [19], the following findings were recorded. Out of the 32 studies [5–17, 27–45] assessed, 1 study employed blinding [6]. In 5 studies, randomizations [5, 7, 34, 37, 39] were performed. The dropout rate was mentioned in 31 studies [5–11, 13–17, 27–45]. The study variables were analyzed for accuracy in 30 studies [5–13, 15–17, 27–29, 37, 39–45]. Sample size was mentioned in 31 studies [5–17, 27–33, 35–45]. The inclusion and exclusion criteria were clearly mentioned in 30 studies [5–15, 17, 27–37, 39–45]. The examiner reliability was also applied in 30 studies [5–13, 15–17, 27–31, 33–45]. Additionally, the outcome of study was prespecified in 28 studies [5–10, 13–17, 27–33, 35–37, 39–45]. The quality of 25 studies was rated as low [5–10, 13, 15, 17, 27–29, 31–33, 39–45, 33–35–37], whereas 7 studies were rated as having a moderate risk of biasness [11, 12, 14, 16, 30, 34, 38]. The quality assessment of the included studies is shown in Table 3.
Table 3.
Methodological quality assessment results of the included studies (n = 33).
| Author and year | Randomization | Blinding | Withdrawal/dropout mentioned | Variables measured many times | Sample size estimation | Inclusion/exclusion criteria clear | Examiner reliability tested | Expected outcomes prespecified | Quality of study/bias risk |
|---|---|---|---|---|---|---|---|---|---|
| Abdalla-Aslan et al. [5] 2020 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Bouchahma et al. [6] 2019 | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Kuwada et al. [7] 2020 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Lee et al. [8] 2020 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Ekert et al. [9] 2019 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Saghiri et al. [10] 2012 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Arisu et al. [11] 2018 | No | No | Yes | Yes | Yes | Yes | Yes | No | Moderate |
| Yamaguchi et al. [12] 2019 | No | No | Unclear | Yes | Yes | Yes | Yes | No | Moderate |
| Otani et al. [13] 2015 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Wang et al. [14] 2014 | Unclear | Unclear | Yes | No | Yes | Yes | No | Yes | Moderate |
| Takahashi et al. [15] 2020 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Patcas et al. [16] 2019 | No | No | Yes | Yes | Yes | Unclear | Yes | Yes | Moderate |
| Li et al. [17] 2020 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Li et al. [44] 2015 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Edinger [30] 2004 | Unclear | Unclear | Yes | Yes | Yes | Yes | No | Yes | Moderate |
| Meissner et al. [31] 2006 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Meissner et al. [32] 2005 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Devito et al. [33] 2008 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Kositbowornchai et al. [34] 2006 | Yes | No | Yes | Yes | No | Yes | Yes | No | Moderate |
| Patcas et al. [35] 2019 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Lee et al. [36] 2018 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Vranckx et al. [37] 2020 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Lee et al. [38] 2020 | No | No | Yes | No | Yes | No | Yes | No | Moderate |
| Hung et al. [39] 2019 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Cui et al. [27] 2020 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Sornam and Prabhakaran [40] 2019 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Setzer et al. [41] 2020 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Cantu et al. [42] 2020 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Aliaga et al. [45] 2020 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Kim et al. [28] 2018 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Dumast et al. [29] 2018 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Sorkhabi and Khajeh [43] 2019 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
∗A study was graded to have a low risk of bias if it yielded 6 or more “yes” answers to the 9 questions, moderate risk if it yielded 3 to 5 “yes” answers, and high risk if it yielded 2 “yes” answers or less.
Furthermore, “the quality assessment of selected studies on NOS [20] was ranging from 4 to 8 stars.” A mean score of 7 was achieved for the included studies, as mentioned in Table 4. Thirty-one studies fall in the moderate bias category [5–17, 27–29, 31–45] while 1 study had a high risk of biasness [30].
Table 4.
Newcastle-Ottawa scale based quality assessment of selected studies (n = 33).
| Author and year | Selection | Compatibility | Exposure | Newcastle-Ottawa quality (total) |
|---|---|---|---|---|
| Abdalla-Aslan et al. [5] 2020 | ∗∗∗ | ∗ | ∗∗∗ | 7 |
| Bouchahma et al. [6] 2019 | ∗∗∗∗ | ∗ | ∗∗∗ | 7 |
| Kuwada et al. [7] 2020 | ∗∗∗ | ∗ | ∗∗∗ | 7 |
| Lee et al. [8] 2020 | ∗∗∗ | ∗ | ∗∗ | 6 |
| Ekert et al. [9] 2019 | ∗∗∗ | ∗ | ∗∗∗∗ | 8 |
| Saghiri et al. [10] 2012 | ∗∗∗ | ∗ | ∗∗∗ | 7 |
| Arisu et al. [11] 2018 | ∗∗ | ∗ | ∗∗∗ | 6 |
| Yamaguchi et al. [12] 2019 | ∗∗∗ | ∗ | ∗∗∗∗ | 8 |
| Otani et al. [13] 2015 | ∗∗ | ∗∗ | ∗∗∗ | 7 |
| Wang et al. [14] 2014 | ∗∗ | ∗ | ∗∗∗ | 6 |
| Takahashi et al. [15] 2020 | ∗∗∗ | ∗∗ | ∗∗ | 7 |
| Patcas et al. [16] 2019 | ∗∗∗ | ∗ | ∗∗ | 6 |
| Li et al. [17] 2020 | ∗∗∗∗ | ∗ | ∗∗∗ | 8 |
| Li et al. [44] 2015 | ∗∗∗ | ∗ | ∗∗∗∗ | 8 |
| Edinger [30] 2004 | ∗ | ∗ | ∗∗ | 4 |
| Meissner et al. [31] 2006 | ∗∗ | ∗ | ∗∗∗ | 6 |
| Meissner et al. [32] 2005 | ∗∗∗ | ∗ | ∗∗ | 6 |
| Devito et al. [33] 2008 | ∗∗∗ | ∗ | ∗∗∗∗ | 7 |
| Kositbowornchai et al. [34] 2006 | ∗∗∗ | ∗ | ∗∗ | 6 |
| Patcas et al. [35] 2019 | ∗∗∗ | ∗ | ∗∗∗ | 7 |
| Lee et al. [36] 2018 | ∗∗∗ | ∗ | ∗∗ | 6 |
| Vranckx et al. [37] 2020 | ∗∗∗ | ∗ | ∗∗∗ | 7 |
| Lee et al. [38] 2020 | ∗∗ | ∗ | ∗∗∗ | 8 |
| Hung et al. [39] 2019 | ∗∗∗ | ∗ | ∗∗∗ | 7 |
| Cui et al. [27] 2020 | ∗∗∗ | ∗ | ∗∗ | 6 |
| Sornam and Prabhakaran [40] 2019 | ∗∗∗ | ∗ | ∗∗∗ | 7 |
| Setzer et al. [41] 2020 | ∗∗∗ | ∗ | ∗∗∗ | 7 |
| Cantu et al. [42] 2020 | ∗∗∗∗ | ∗ | ∗∗∗ | 8 |
| Aliaga et al. [45] 2020 | ∗∗∗ | ∗ | ∗∗ | 6 |
| Kim et al. [28] 2018 | ∗∗∗ | ∗ | ∗∗∗ | 7 |
| Dumast et al. [29] 2018 | ∗∗∗ | ∗ | ∗∗∗ | 7 |
| Sorkhabi and Khajeh [43] 2019 | ∗∗∗ | ∗ | ∗∗∗ | 7 |
∗A study can be awarded a maximum of 1 star for each numbered item within the selection and exposure categories. A maximum of 2 stars can be given for comparability. Each study can be awarded a total of 9 stars. A study was rated to have a low risk of biasness if it received the maximum allowed number of 9 “stars” while moderate risk if it received 8, 7, or 6 “stars” and high risk if it received 5 “stars” or less.
4. Discussion
The AI digital systems have unquestionably changed the direction of dentistry [46]. The AI modalities: machine learning, deep learning, cognitive computing, computer vision (recognizes the content in photos and videos), and natural language processing (to both analyze and generate human speech with the help of machines), are promising and practiced in dentistry [47]. Along the advent of AI better restoration, options are available with longer shelf life and superior esthetics and function [12, 13]. AI models are bringing greater efficiency and accuracy, capitalizing on the interest, capabilities, and skills of those involved [48]. Effective and efficient interprofessional and clinician-patient interactions have evolved using these new ways, with AI students have new ways of learning through research and the data collected can be efficiently utilized for forensic and epidemiological uses [49, 50]. Extensive research has been carried out on the application, benefits, and comparison of AI with human skills around the globe. The purpose of this systematic review was to investigate the quality and outcome of studies into artificial intelligence techniques, analysis, and its effect in dentistry.
Among the studies reviewed, it was revealed the application of artificial intelligence in dentistry is ample. Studies have found that the implications of AI in practice will facilitate dentists at every step. For instance, a neural network is beneficial in screening for oral cancer and precancer conditions, diagnosing bisphosphonate-related osteonecrosis before surgical removal of teeth and evaluating cervical lymph node metastasis of carcinoma after comparing it with magnetic resonance imaging [21, 28]. Furthermore, the computer color matching (CCM) technique provides an accurate color matching of dental restorations, together with the automatic laser ablation system for clinical crown preparation [14, 44]. The methodology used varied among the studies as to how the data were collected and analyzed and the AI technique developed. Therefore, a comparison of the studies was difficult.
The AI models suggested a positive impact in assisting dental diagnostics. Therefore, it can assist dentists in achieving correct interpretations of dental anomalies and minimizing human error. This review suggests that computer-based neural network plays a supporting role to dental practitioners, in decision making and minimizing errors during execution of dental treatment planning.
Furthermore, the current review proposes AI, a reliable technology for appraising the depth of dental caries, apical lesion diagnosis, working length determination, classification of dental arches, tooth segmentation, TMJ osteoarthritis, and early detection of early osteoporosis in jaws on panoramic radiographs [6, 8–10, 15, 36, 38, 45]. Rekow used a machine-learning algorithm to detect and classify dental restorations on panoramic images [25]. Kuwada et al. revealed that “DetectNet and AlexNet” appeared potentially useful in classifying the presence of impacted supernumerary teeth in the maxillary incisor region on panoramic radiographs [7]. Drevenstedt et al. used voice commands for recording patients' history and data, making suggestions during an ongoing dental procedure, scheduling patients' appointment, reminders for routine checkups, and necessary dental consultations [51]. The artificial neural network (ANN) models using bitewing photographs showed 97.1% accuracy for the dental caries diagnosis, 95.1% precision, a specificity of 94.3%, and a sensitivity ranging from 85% to 99.6% [42]. Sornam and Prabhakaran depicted an accuracy ranging from 85 to 100% using the AI model, “back-propagation neural networks” (BPNN) in dental caries classification [40]. However, comparisons among the studies were difficult because of differences in the methods used.
Despite the fact that the outcome of reviewed studies is auspicious, this study has few limitations. For example, the quality assessment of the literature conceded that there is a possibility of bias. The complexity of a particular system or mechanism, cost, and equipment of each setup need to be considered, including the training required for each AI model. Further research, exposure, and implementation are required. The worthwhile outcomes are not achieved yet due to the unavailability of accurate and sufficient data. In short, challenges exist both in technical and ethical aspects.
Nonetheless, in the future, the AI-based comprehensive care system will analyze big data including faciodental images and other records. AI models will provide reliable information and refined the clinical decision-making process. Infect AI is expected to establish high-quality patient care, innovative research, and state-of-the-art development in dentistry. Artificial intelligence and machine learning will aid to automation of aesthetic evaluation, smile design, and oral rehabilitation. By far, a change is not easy to adapt, but gradually, the application of AI in dental practice will become a necessity and might drive patient's demand too. AI has the proven ability to rationalize and take actions in the best manner of achieving a specific goal; this automated model can easily execute tasks, from simple to complex in nature.
5. Conclusions
At present, AI has been used vastly in dentistry. It has the potential to revolutionize oral health care by assisting in addressing the weaknesses grimly criticized in conventional dental care.
Based on the findings of this systematic review, it was concluded that
AI techniques assist dental practitioners in numerous ways, from decreasing the chairside time, saving extra steps, achieving excellent infection control, and providing quality treatment with accuracy and precision
AI can be successfully used for patient diagnosis, clinical decision making, and prediction of dental failures. Hence, it is a reliable modality for future application in oral diagnosis, oral and maxillofacial surgery, restorative dentistry, prosthodontics, orthodontics, endodontics, forensic dentistry, radiology, and periodontics
However, AI is increasing the scope of state-of-the-art models in dentistry but is still under development. Further studies are required to assess the clinical performance of AI techniques in dentistry
Acknowledgments
The authors thank Mr. Muhammad Hashim and Dr. Zohaib Khurshid for guidance and help regarding English language editing and ideas on Figures 1 and 2 in this study. We are also grateful to University Sains Malaysia, Jouf University, Kingdom of Saudi Arabia, and Altamash Institute of Dental Medicine, Pakistan, for the support and facilitation in this study.
Contributor Information
Mohamad Syahrizal Bin Halim, Email: drsyah@usm.my.
Mohammad Khursheed Alam, Email: dralam@gmail.com.
Data Availability
The raw data used to support the findings of this study are included within the article.
Conflicts of Interest
The authors declare no conflict of interest.
Authors' Contributions
NA, FZ, and WQ planned and designed the present work, and MSA was responsible for realizing the work. NA, MSA, FZ, and WQ were responsible for the data acquisition and analysis. NA, MSH, and AM drafted and revised the manuscript. NA, MKA, MSH, and AM approved the final version of the manuscript. All authors read and approved the final manuscript. MSH and MKA contributed equally to this work and are corresponding authors.
References
- 1.Barr A., Feigenbaum E. A., Cohen P. R. The Handbook of Artificial Intelligence. 1-3. Los Altos, CA: William Kaufmann Inc.; 1981. [Google Scholar]
- 2.Schwendicke F., Samek W., Krois J. Artificial intelligence in dentistry: chances and challenges. Journal of Dental Research. 2020;99(7):769–774. doi: 10.1177/0022034520915714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen Y. W., Stanley K., Att W. Artificial intelligence in dentistry: current applications and future perspectives. Quintessence International. 2020;51(3):248–257. doi: 10.3290/j.qi.a43952. [DOI] [PubMed] [Google Scholar]
- 4.Cozzani M., Sadri D., Nucci L., Jamilian P., Pirhadirad A. P., Jamilian A. The effect of Alexander, Gianelly, Roth, and MBT bracket systems on anterior retraction: a 3-dimensional finite element study. Clinical Oral Investigations. 2020;24(3):1351–1357. doi: 10.1007/s00784-019-03016-6. [DOI] [PubMed] [Google Scholar]
- 5.Abdalla-Aslan R., Yeshua T., Kabla D., Leichter I., Nadler C. An artificial intelligence system using machine-learning for automatic detection and classification of dental restorations in panoramic radiography. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology. 2020;130(5):593–602. doi: 10.1016/j.oooo.2020.05.012. [DOI] [PubMed] [Google Scholar]
- 6.Bouchahma M., Ben Hammouda S., Kouki S., Alshemaili M., Samara K. An automatic dental decay treatment prediction using a deep convolutional neural network on X-ray images. 2019 IEEE/ACS 16th International Conference on Computer Systems and Applications (AICCSA); 2019; Abu Dhabi, United Arab Emirates. pp. 1–4. [DOI] [Google Scholar]
- 7.Kuwada C., Ariji Y., Fukuda M., et al. Deep learning systems for detecting and classifying the presence of impacted supernumerary teeth in the maxillary incisor region on panoramic radiographs. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology. 2020;130(4):464–469. doi: 10.1016/j.oooo.2020.04.813. [DOI] [PubMed] [Google Scholar]
- 8.Lee J. H., Han S. S., Kim Y. H., Lee C., Kim I. Application of a fully deep convolutional neural network to the automation of tooth segmentation on panoramic radiographs. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology. 2020;129(6):635–642. doi: 10.1016/j.oooo.2019.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Ekert T., Krois J., Meinhold L., et al. Deep learning for the radiographic detection of apical lesions. Journal of endodontics. 2019;45(7):917–922.e5. doi: 10.1016/j.joen.2019.03.016. [DOI] [PubMed] [Google Scholar]
- 10.Saghiri M. A., Garcia-Godoy F., Gutmann J. L., Lotfi M., Asgar K. The reliability of artificial neural network in locating minor apical foramen: a cadaver study. Journal of Endodontia. 2012;38(8):1130–1134. doi: 10.1016/j.joen.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Deniz Arısu H., Eligüzeloglu Dalkilic E., Alkan F., Erol S., Uctasli M. B., Cebi A. Use of artificial neural network in determination of shade, light curing unit, and composite parameters’ effect on bottom/top Vickers hardness ratio of composites. BioMed Research International. 2018;2018:9. doi: 10.1155/2018/4856707.4856707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yamaguchi S., Lee C., Karaer O., Ban S., Mine A., Imazato S. Predicting the debonding of CAD/CAM composite resin crowns with AI. Journal of Dental Research. 2019;98(11):1234–1238. doi: 10.1177/0022034519867641. [DOI] [PubMed] [Google Scholar]
- 13.Otani T., Raigrodski A. J., Mancl L., Kanuma I., Rosen J. In vitro evaluation of accuracy and precision of automated robotic tooth preparation system for porcelain laminate veneers. The Journal of Prosthetic Dentistry. 2015;114(2):229–235. doi: 10.1016/j.prosdent.2015.02.021. [DOI] [PubMed] [Google Scholar]
- 14.Wang L., Wang D., Zhang Y., Ma L., Sun Y., Lv P. An automatic robotic system for three-dimensional tooth crown preparation using a picosecond laser. Lasers in Surgery and Medicine. 2014;46(7):573–581. doi: 10.1002/lsm.22274. [DOI] [PubMed] [Google Scholar]
- 15.Takahashi J., Nozaki K., Gonda T., Ikebe K. A system for designing removable partial dentures using artificial intelligence. Part 1. Classification of partially edentulous arches using a convolutional neural network. Journal of Prosthodontic Research. 2021;65(1):115–118. doi: 10.2186/jpr.JPOR_2019_354. [DOI] [PubMed] [Google Scholar]
- 16.Patcas R., Bernini D. A. J., Volokitin A., Agustsson E., Rothe R., Timofte R. Applying artificial intelligence to assess the impact of orthognathic treatment on facial attractiveness and estimated age. International Journal of Oral and Maxillofacial Surgery. 2019;48(1):77–83. doi: 10.1016/j.ijom.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 17.Li M., Xu X., Punithakumar K., Le L. H., Kaipatur N., Shi B. Automated integration of facial and intra-oral images of anterior teeth. Computers in Biology and Medicine. 2020;122, article 103794 doi: 10.1016/j.compbiomed.2020.103794. [DOI] [PubMed] [Google Scholar]
- 18.Moher D., Liberati A., Tetzlaff J. A., Altman D. G., PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine. 2009;151(4):264–9, W64. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 19.Higgins J. P., Green S. Cochrane Handbook for Systematic Reviews of Interventions. Vol. 4. John Wiley & Sons; 2011. [Google Scholar]
- 20.Wells G. A., Shea B., O’Connell D. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. Ottawa, ON, Canada: Ottawa Hospital Research Institute; 2011. [Google Scholar]
- 21.Gould A. R. Early detection of oral premalignant disease and oral cancer: refining the process. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 2002;94(4):397–398. doi: 10.1067/moe.2002.128527. [DOI] [PubMed] [Google Scholar]
- 22.Van der Meer W. J., Vissink A., Ng Y. L., Gulabivala K. 3D computer aided treatment planning in endodontics. Journal of Dentistry. 2016;45:67–72. doi: 10.1016/j.jdent.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 23.Vera V., Corchado E., Redondo R., Sedano J., Garcia A. E. Applying soft computing techniques to optimise a dental milling process. Neurocomputing. 2013;109(109):94–104. doi: 10.1016/j.neucom.2012.04.033. [DOI] [Google Scholar]
- 24.Leeson D. The digital factory in both the modern dental lab and clinic. Dental Materials. 2020;36(1):43–52. doi: 10.1016/j.dental.2019.10.010. [DOI] [PubMed] [Google Scholar]
- 25.Rekow E. D. Digital dentistry: the new state of the art -- is it disruptive or destructive? Dental Materials. 2020;36(1):9–24. doi: 10.1016/j.dental.2019.08.103. [DOI] [PubMed] [Google Scholar]
- 26.McCracken G. I., Nunn J. H., Hobson R. S., Stephenson J. J., Jepson N. J. Evaluation of a computer- assisted learning package on the management of traumatised incisors by general dental practitioners. Endodontics & Dental Traumatology. 2000;16(1):40–42. doi: 10.1034/j.1600-9657.2000.016001040.x. [DOI] [PubMed] [Google Scholar]
- 27.Cui Q., Chen Q., Liu P., Liu D., Wen Z. Clinical decision support model for tooth extraction therapy derived from electronic dental records. The Journal of Prosthetic Dentistry. 2020;20:S0022–S3913. doi: 10.1016/j.prosdent.2020.04.010. [DOI] [PubMed] [Google Scholar]
- 28.Kim D. W., Kim H., Nam W., Kim H. J., Cha I. H. Machine learning to predict the occurrence of bisphosphonate-related osteonecrosis of the jaw associated with dental extraction: a preliminary report. Bone. 2018;116:207–214. doi: 10.1016/j.bone.2018.04.020. [DOI] [PubMed] [Google Scholar]
- 29.de Dumast P., Mirabel C., Cevidanes L., et al. A web-based system for neural network based classification in temporomandibular joint osteoarthritis. Computerized Medical Imaging and Graphics. 2018;67:45–54. doi: 10.1016/j.compmedimag.2018.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Edinger D. H. Accuracy of a robotic system for the reproduction of condylar movements: a preliminary report. Quintessence International. 2004;35(7):519–523. [PubMed] [Google Scholar]
- 31.Meissner G., Oehme B., Strackeljan J., Kocher T. In vitro calculus detection with a moved smart ultrasonic device. Journal of Clinical Periodontology. 2006;33(2):130–134. doi: 10.1111/j.1600-051X.2005.00863.x. [DOI] [PubMed] [Google Scholar]
- 32.Meissner G., Oehme B., Strackeljan J., Kocher T. Influence of handling-relevant factors on the behaviour of a novel calculus-detection device. Journal of clinical periodontology. 2005;32(3):323–328. doi: 10.1111/j.1600-051X.2005.00679.x. [DOI] [PubMed] [Google Scholar]
- 33.Devito K. L., de Souza Barbosa F., Filho W. N. F. An artificial multilayer perceptron neural network for diagnosis of proximal dental caries. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 2008;106(6):879–884. doi: 10.1016/j.tripleo.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 34.Kositbowornchai S., Siriteptawee S., Plermkamon S., Bureerat S., Chetchotsak D. An artificial neural network for detection of simulated dental caries. International Journal of Computer Assisted Radiology and Surgery. 2006;1(2):91–96. doi: 10.1007/s11548-006-0040-x. [DOI] [Google Scholar]
- 35.Patcas R., Timofte R., Volokitin A., et al. Facial attractiveness of cleft patients: a direct comparison between artificial-intelligence-based scoring and conventional rater groups. European journal of orthodontics. 2019;41(4):428–433. doi: 10.1093/ejo/cjz007. [DOI] [PubMed] [Google Scholar]
- 36.Lee J. H., Kim D. H., Jeong S. N., Choi S. H. Detection and diagnosis of dental caries using a deep learning-based convolutional neural network algorithm. Journal of Dentistry. 2018;77:106–111. doi: 10.1016/j.jdent.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 37.Vranckx M., Van Gerven A., Willems H., et al. Artificial intelligence (AI)-driven molar angulation measurements to predict third molar eruption on panoramic radiographs. International Journal of Environmental Research and Public Health. 2020;17(10):p. 3716. doi: 10.3390/ijerph17103716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee K. S., Kwak H. J., Oh J. M., et al. Automated detection of TMJ osteoarthritis based on artificial intelligence. Journal of Dental Research. 2020;99(12):1363–1367. doi: 10.1177/0022034520936950. [DOI] [PubMed] [Google Scholar]
- 39.Hung M., Voss M. W., Rosales M. N., et al. Application of machine learning for diagnostic prediction of root caries. Gerodontology. 2019;36(4):395–404. doi: 10.1111/ger.12432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sornam M., Prabhakaran M. Integrated Intelligent Computing, Communication and Security. Vol. 771. Singapore: Springer; 2019. Logit-based artificial bee colony optimization (LB-ABC) approach for dental caries classification using a back propagation neural network; pp. 79–91. [DOI] [Google Scholar]
- 41.Setzer F. C., Shi K. J., Zhang Z., et al. Artificial intelligence for the computer-aided detection of periapical lesions in cone-beam computed tomographic images. Journal of Endodontia. 2020;46(7):987–993. doi: 10.1016/j.joen.2020.03.025. [DOI] [PubMed] [Google Scholar]
- 42.Cantu A. G., Gehrung S., Krois J., et al. Detecting caries lesions of different radiographic extension on bitewings using deep learning. Journal of Dentistry. 2020;100, article 103425 doi: 10.1016/j.jdent.2020.103425. [DOI] [PubMed] [Google Scholar]
- 43.Sorkhabi M. M., Saadat Khajeh M. Classification of alveolar bone density using 3-D deep convolutional neural network in the cone-beam CT images: a 6-month clinical study. Measurement. 2019;148, article 106945 doi: 10.1016/j.measurement.2019.106945. [DOI] [Google Scholar]
- 44.Li H., Lai L., Chen L., Lu C., Cai Q. The prediction in computer color matching of dentistry based on GA+BP neural network. Computational and Mathematical Methods in Medicine. 2015;2015:7. doi: 10.1155/2015/816719.816719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Aliaga I., Vera V., Vera M., García E., Pedrera M., Pajares G. Automatic computation of mandibular indices in dental panoramic radiographs for early osteoporosis detection. Artificial Intelligence in Medicine. 2020;103, article 101816 doi: 10.1016/j.artmed.2020.101816. [DOI] [PubMed] [Google Scholar]
- 46.Grischke J., Johannsmeier L., Eich L., Griga L., Haddadin S. Dentronics: towards robotics and artificial intelligence in dentistry. Dental Materials. 2020;36(6):765–778. doi: 10.1016/j.dental.2020.03.021. [DOI] [PubMed] [Google Scholar]
- 47.Khanna S. S., Dhaimade P. A. Artificial intelligence: transforming dentistry today. Indian Journal Of Basic And Applied Medical Research. 2017;6(3):161–167. [Google Scholar]
- 48.Joda T., Bornstein M. M., Jung R. E., Ferrari M., Waltimo T., Zitzmann N. U. Recent trends and future direction of dental research in the digital era. International Journal of Environmental Research and Public Health. 2020;17(6):p. 1987. doi: 10.3390/ijerph17061987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shan T., Tay F. R., Gu L. Application of artificial intelligence in dentistry. Journal of Dental Research. 2021;100(3):232–244. doi: 10.1177/0022034520969115. [DOI] [PubMed] [Google Scholar]
- 50.Schwendicke F., Singh T., Lee J. H., et al. Artificial intelligence in dental research: checklist for authors, reviewers, readers. Journal of Dentistry. 2021;107, article 103610 doi: 10.1016/j.jdent.2021.103610. [DOI] [Google Scholar]
- 51.Drevenstedt G., Mcdonald J., Drevenstedt L. The role of voice-activated technology in today's dental practice. Journal of the American Dental Association (1939) 2005;136(2):157–161. doi: 10.14219/jada.archive.2005.0135. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data used to support the findings of this study are included within the article.


