Abstract
Acute graft-versus-host disease (aGVHD) is a rare complication after liver transplantation that characterized by high mortality. We presented a case of aGVHD after orthotopic liver transplantation (OLT) for hepatocellular carcinoma (HCC). The patient suffered from fever, oral ulcer, rashes and diarrhea and had a co-infection with Cytomegalovirus (CMV). Short tandem repeat (STR) analysis for cluster of differentiation (CD3) cells and skin biopsy indicated aGVHD. His regimens included high dose of steroids, ruxolitinib, basiliximab, local liver radiotherapy and antibiotics prophylaxis, with the withdrawal of tacrolimus and MMF. Unfortunately, he developed an acute rejection followed by cytomegalovirus infection and lung infection. Soon afterwards he was sent to “isolation ward” due to high suspicion for clinical coronavirus disease 2019 (COVID-19). Fortunately, He was excluded from COVID-19 after nucleic acid and antibody tests. Though closely contact with other COVID-19 patients for a month, the patient was not affected with COVID-19 through his careful protective measures. Finally, the patient recovered after antiviral and antifungal treatment. To our knowledge, this is the first case report of a patient recovered from aGVHD as a close contact.
Keywords: Orthotopic live transplantation, aGVHD, COVID-19, Close contact
1. Introduction
Acute graft-versus-host-disease (aGVHD) is a rare and lethal complication occurred in 0.5%–2% of the patients after live transplantation [[1], [2], [3], [4]]. Its mortality rate has been reported up to 75%–100% [2,5,6]. Immunocompetent donor lymphocytes engraft and proliferate in the recipient's bone marrow and initiate an immunological attack against the target organs such as skin, liver, gastrointestinal tract, and bone marrow, leading to typical symptoms in these organs [7,8]. However, clinical manifestations like fever, rash, diarrhea, and pancytopenia are often mistakenly attributed to underlying diseases, drug reactions or viral infections, delaying the diagnosis and treatment of aGVHD [[9], [10], [11]]. Here, we showed a patient who recovered from aGVHD after live transplantation, even as a close contact during the COVID-19 outbreak.
2. Case report
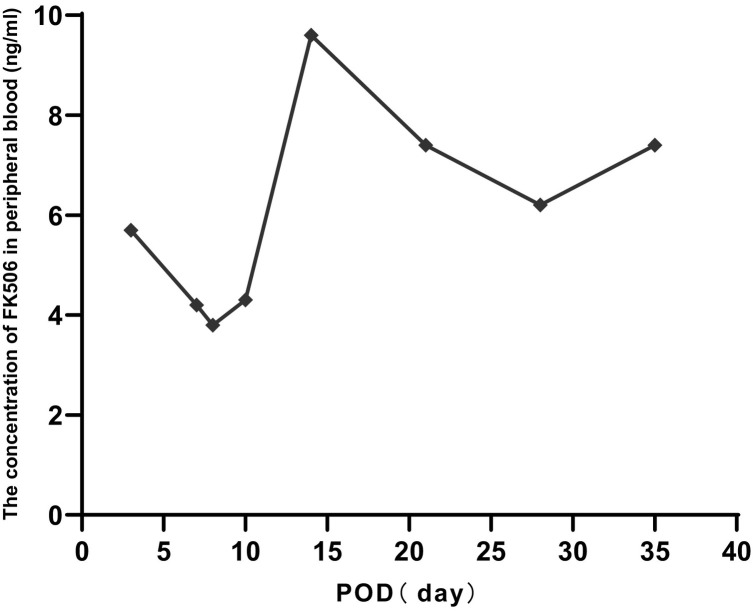
A 61- year-old diabetic man underwent OLT in our facility for hepatocellular carcinoma secondary to hepatitis B virus (HBV) cirrhosis in October 2019. He had a history of liver tumor resection and TACE before OLT. Postoperative immunosuppressive regimens were tacrolimus (trough concentration level showed in Fig. 1 ), methylprednisolone (decreased from a large dose of 500 mg/d to a maintenance dose of 8 mg/d on day 7) and mycophenolate mofetil (MMF; 1 mg/day). His postoperative recovery was uneventful and discharged on postoperative day (POD) 14 with intact liver function.
Fig. 1.
Changes in the concentration of FK506 in peripheral blood trunk.
However, he presented with an oral ulcer on POD 16, whose routine blood and liver function examination were normal. On POD 28, he developed a maculopapular skin rash on his bilateral tights and subsequently involving the trunk (Fig. 2 ), accompanied by diarrhea. Laboratory tests showed increased IL-2 receptors(5978 pg/ml), TNF-a (12.4 pg/ml) and IL-10 (80.1 pg/ml), and normal liver function and routine blood. Skin biopsy on POD 32 indicated that mild hyperkeratosis, vacuolar degeneration of basal layer of epithelium, lymphocyte infiltrations in the epidermis and dermis (Fig. 3 ) and bone marrow swear showed marrow dysplasia. STR analysis revealed 4.82% lymphocyte macrochimerism in peripheral blood. These findings were consistent with GVHD.
Fig. 2.
Scattered maculopapular rash on the patient's trunk and pigmentation of the patient's skin after the resolution of the rash.
Fig. 3.
Biopsy of skin rash on POD 32. Mild hyperkeratosis and vacuolar degeneration can be seen in the basal layer of epithelium, and lymphocyte infiltrations can be seen in the epidermis and dermis.
The process of patient's therapy was showed in Fig. 4 . He discontinued the tacrolimus and MMF and was treated with methylprednisolone (500 mg for 3 days and tapered to 8 mg within three weeks) on POD 38. Ruxolitinib (5 mg/d), basiliximab (20 mg) and local liver low dose radiotherapy (350 cGy/d for 2 times) were administered subsequently. The skin rash began to retreat a week after the treatment and diarrhea recovered. Unfortunately, on POD 63, the patient developed acute rejection with elevated ALT and Total bilirubin (Fig. 5 ) and was treated with methylprednisolone (500 mg/d for 3 days), plasma exchange and anti-human T lymphocyte globulin (ATG). On POD 75, he suffered from fever (37.8 °C)with Cytomegalovirus-positive in peripheral blood. After which, the CT imaging indicated multiple ground-glass imaging and nodular consolidation in his left lung (Fig. 6 ). He was misdiagnosed as “clinical COVID-19” after consultation by the “Wuhan expert group” due to imperfect knowledge of the disease at that time and was sent to “isolation ward”, staying with COVID-19 patients for one month. Eventually, he was excluded from COVID-19 by nucleic acid and antibody tests and discharged after antiviral and antifungal treatment. During the one-year follow-up period, the patient was readmitted with herpes zoster virus infection 11 months after OLT and was discharged after antiviral treatment.
Fig. 4.
Symptoms and treatment process for GVHD and acute rejection.
Fig. 5.
Changes in liver function after aGVHD.
Fig. 6.

Lung CT. Multiple ground-glass imaging and nodular consolidation in his left lung.
3. Discussion
aGVHD, usually developing 3 to 5 weeks after OLT, is an infrequent complication, but associated with an extremely high mortality rate [7,12]. aGVHD happens in two forms. The first form is antibody-mediated. The donor lymphocytes recognize recipients' RBC antigens due to an ABO blood type mismatch, resulting in hemolytic anemia. The second form is a cellular immune response. The development of aGVHD can be summarized into three phases: (1) the activation of the APCs; (2) donor-derived T lymphocytes engraft and proliferated in the host tissue; (3) target tissue destruction [7,8,13]. The classical “cytokine storm” participate in the development of GVHD [14]. Some studies found that TNF-α, IL-2 and INF-γ may act as biomarkers for aGVHD and are associated with the degree of the disease [15,16]. The reported risk factors for aGVHD include donor-recipient age difference greater than 20 years, younger donor age, recipient age over 50 years, closely matched HLA, hepatocellular carcinoma, autoimmune hepatitis and glucose intolerance [[17], [18], [19], [20]]. In this case, the patient had increased cytokine (TNF-α, IL-10) and IL-2 receptors. The donor age was 19 years old, and the patient was a 61-year-old diabetic man with hepatocellular carcinoma, according to the contributing factors aforementioned.
The diagnosis of aGVHD after OLT is depended on the clinical features, T-lymphocyte macrochimerism and biopsy-proven histologic evidence [21,22]. aGVHD often involves the skin, gastrointestinal tract, and bone marrow. The clinical manifestations are usually nonspecific (skin rash, diarrhea, fever, and pancytopenia) with normal liver function and are often confused with infection or drug adverse effects [20]. Skin rash is erythematous, maculopapular and may develop any part of the body with subtle and nonpruritic symptoms [23]. Typical skin histologic features are vacuolar alteration, dyskeratosis, and lymphocyte infiltration [24]. Patients with severe diarrhea should be performed endoscopic biopsies. aGVHD is implied by showing increased crypt epithelial apoptosis, crypt loss and soakage of neutrophilic [25,26]. It has been assessed that approximately 10 [9]–1010 donor lymphocytes remain in the portal tracts and the parenchyma of the donor liver graft after flushing with preservation solution [27,28]. These cells can exist in the first weeks after OLT [29,30]. Confirmation of aGVHD is made by showing more than 1% lymphocyte macrochimerism in recipient tissues [7]. Pancytopenia may be an element of characteristic manifestations. However, blood examination was normal in this case.
The optimal treatment modality for aGVHD remains debatable given the rarity of the disease. Corticosteroids are the first-line therapy for aGvHD after hematopoietic stem cell transplantation [31]. However, aGVHD after LT seemed to respond poorly to the high-dose steroids alone. Some kinds of literature have demonstrated a good response to the combination with decrease/discontinue/increase in or substitution of the immunosuppressive medications [[32], [33], [34], [35]], intravenous immunoglobulin, antimicrobial prophylaxis, anti-T cell antibodies, anti-B cell antibodies [17,[36], [37], [38], [39]]. Other second-line regimens, including IL-2 inhibitors (basiliximab), CD2-blockers (alefacept) and TNF-α antagonists (infliximab), appear to be promising for steroid-resistant patients with aGVHD after LT [12]. In our case, the patient was given a combined treatment of steroids, IL-2 antagonists, ruxolitinib, basiliximab and local liver radiotherapy and responded well to this regimen. Although the patient was encountered with acute rejection and close contact with COVID-19 infectors, he was recovered eventually due to proper clinical management and rigorous preventive measure, without suffering from liver failure or systematic infection. He had continued liver dysfunction during the one-year follow-up period, which we attributed to liver damage caused by acute rejection and local liver radiotherapy.
In conclusion, we herein presented a case of a 61-year-old man who recovered from aGVHD even as a close contact during the COVID19 outbreak. Low lymphocyte macrochimerism (4.82%) in the skin and lack of the presentation of pancytopenia reflected mild aGVHD and a good prognosis of this patient, although the interval from his primary diagnosis to the treatment was 10 days. High-dose steroids combined with IL-2 antagonists and local liver radiotherapy appear to be a promising approach for aGVHD. However, the dose of radiotherapy needs further study to avoid liver injury. Ceasing immunosuppressive agents seems not to be a good decision. In addition, prophylactic antibacterial, antifungal and antiviral therapy may improve prognosis.
Declaration of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
We sincerely thank all of the patients and the staff in the department.
References
- 1.Murali A.R., Chandra S., Stewart Z., et al. Graft versus host disease after liver transplantation in adults [J] Transplantation. 2016;100(12):2661–2670. doi: 10.1097/TP.0000000000001406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taylor A.L., Gibbs P., Bradley J.A. Acute graft versus host disease following liver transplantation: the enemy within [J] Am. J. Transplant. 2015;4(4):466–474. doi: 10.1111/j.1600-6143.2004.00406.x. [DOI] [PubMed] [Google Scholar]
- 3.Smith D.M., Agura E., Netto G., et al. Liver transplant-associated graft-versus-host disease [J] Transplantation. 2003;75(1):118–126. doi: 10.1097/00007890-200301150-00022. [DOI] [PubMed] [Google Scholar]
- 4.Zhi-Yong Guo, Xiao-Shun, et al. Graft-verse-host disease after liver transplantation:a report of two cases and review of literature [J] World J. Gastroenterol. 2008;06:164–169. doi: 10.3748/wjg.14.974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen X.B., Yang J., Xu M.Q., et al. Unsuccessful treatment of four patients with acute graft-vs-host disease after liver transplantation [J] World J. Gastroenterol. 2012;18(1):84–89. doi: 10.3748/wjg.v18.i1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perri R., Assi M., Talwalkar J., et al. Graft vs. host disease after liver transplantation: a new approach is needed [J] Liver Transpl. 2010:13(8). doi: 10.1002/lt.21203. [DOI] [PubMed] [Google Scholar]
- 7.Smith E.P. Hematologic disorders after solid organ transplantation [J] Hematology. 2010;2010(1):281–286. doi: 10.1182/asheducation-2010.1.281. [DOI] [PubMed] [Google Scholar]
- 8.Zacharias N., Gallichio M.H., Conti D.J. Graft-versus-host disease after living-unrelated kidney transplantation [J] Case Rep. Transplant. 2014;2014(2):971426. doi: 10.1155/2014/971426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sun B., Zhao C., Xia Y., et al. Late onset of severe graft-versus-host disease following liver transplantation [J] Transpl. Immunol. 2006;16(3–4):250–253. doi: 10.1016/j.trim.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Lehner F., Becker T., Sybrecht L., et al. Successful outcome of acute graft-versus-host disease in a liver allograft recipient by withdrawal of immunosuppression [J] Transplantation. 2002;73(2):307–310. doi: 10.1097/00007890-200201270-00030. [DOI] [PubMed] [Google Scholar]
- 11.Schrager J.J., Vnencak-Jones C.L., Graber S.E., et al. Use of short tandem repeats for DNA fingerprinting to rapidly diagnose graft-versus-host disease in solid organ transplant patients [J] Transplantation. 2006;81(1):21–25. doi: 10.1097/01.tp.0000190431.94252.3f. [DOI] [PubMed] [Google Scholar]
- 12.Murali, Arvind R., Blazar, et al. Graft versus host disease after liver transplantation in adults: a case series, review of literature, and an approach to management [J] Transplantation. 2016;100(12):2661–2670. doi: 10.1097/TP.0000000000001406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferrara J.L.M., Levine J.E., Reddy P., et al. Graft-versus-host disease [J] Lancet. 2009;373(9674):1550–1561. doi: 10.1016/S0140-6736(09)60237-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Antin J.H., Ferrara J.L.M. Cytokine dysregulation and acute graft-versus-host disease [J] Blood. 1993;80(12):2964–2968. [PubMed] [Google Scholar]
- 15.Lin M.T., Storer B., Martin P.J., et al. Relation of an interleukin-10 promoter polymorphism to graft-versus-host disease and survival after hematopoietic-cell transplantation [J] N. Engl. J. Med. 2003;349(23):2201. doi: 10.1056/NEJMoa022060. [DOI] [PubMed] [Google Scholar]
- 16.Dickinson A.M., Charron D. Non-HLA immunogenetics in hematopoietic stem cell transplantation [J] Curr. Opin. Immunol. 2005;17(5):517–525. doi: 10.1016/j.coi.2005.07.017. [DOI] [PubMed] [Google Scholar]
- 17.Chen M.A., Bai, et al. Acute graft-vs-host disease after liver transplantation in a patient presenting with neurogenic symptoms as the single primary manifestation: a case report [J] Transplant. Proc. 2018;50(10):4028–4032. doi: 10.1016/j.transproceed.2018.05.013. [DOI] [PubMed] [Google Scholar]
- 18.Zhao X.F., Lin D.D., Li N., et al. Diagnosis and treatment of acute graft-versus-host disease after liver transplantation: a report of 11cases [J] Transpl. Immunol. 2020;62:101307. doi: 10.1016/j.trim.2020.101307. [DOI] [PubMed] [Google Scholar]
- 19.Elfeki M.A., Genco P.V., Pungpapong S., et al. Proceedings of the 2015 American Transplant Congress, F. 2015. Graft-versus-host disease after orthotopic liver transplantation: Multivariate analysis of risk factors. [DOI] [PubMed] [Google Scholar]
- 20.Murali A.R., Chandra S., Stewart Z., et al. Graft versus host disease after liver transplantation in adults: a case series, review of literature, and an approach to management [J] Transplantation. 2016;100(12):1. doi: 10.1097/TP.0000000000001406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Darrellj, Triulzi, Michaela, et al. Microchimerism, GVHD, and tolerance in solid organ transplantation [J] Transfusion. 2001;41(3):419–426. doi: 10.1046/j.1537-2995.2001.41030419.x. [DOI] [PubMed] [Google Scholar]
- 22.Rogulj I.M., Deeg J., Lee S.J. Acute graft versus host disease after orthotopic liver transplantation [J] J. Hematol. Oncol. 2012;5(1):1–6. doi: 10.1186/1756-8722-5-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Advani S.D., Nellore A., Hadjivassiliou G., et al. Two cases and a review of graft-versus-host disease and the role of hepatitis C treatment in liver transplant patients [J] Prog. Transplant. (Aliso Viejo, Calif) 2018;28(3) doi: 10.1177/1526924818781558. 1526924818781558. [DOI] [PubMed] [Google Scholar]
- 24.Rodrigues K.S., Oliveira-Ribeiro C., Gomes S.D.A.F., et al. Cutaneous graft-versus-host disease: diagnosis and treatment [J] Am. J. Clin. Dermatol. 2017;19(12):1–18. doi: 10.1007/s40257-017-0306-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ross W.A., Ghosh S., Dekovich A.A., et al. Endoscopic biopsy diagnosis of acute gastrointestinal graft-versus-host disease: rectosigmoid biopsies are more sensitive than upper gastrointestinal biopsies [J] Am. J. Gastroenterol. 2008;103(4):982–989. doi: 10.1111/j.1572-0241.2007.01639.x. [DOI] [PubMed] [Google Scholar]
- 26.Thompson B., Salzman D., Steinhauer J., et al. Prospective endoscopic evaluation for gastrointestinal graft-versus-host disease: determination of the best diagnostic approach [J] Bone Marrow Transplant. 2006;38(5):371–376. doi: 10.1038/sj.bmt.1705453. [DOI] [PubMed] [Google Scholar]
- 27.Domiati-Saad R., Klintmalm G.B., Netto G., et al. Acute graft versus host disease after liver transplantation: patterns of lymphocyte chimerism [J] 2005;5(12):2968–2973. doi: 10.1111/j.1600-6143.2005.01110.x. [DOI] [PubMed] [Google Scholar]
- 28.Norris S., Collins C., Doherty D.G., et al. Resident human hepatic lymphocytes are phenotypically different from circulating lymphocytes [J] J. Hepatol. 1998;28(1):84–90. doi: 10.1016/s0168-8278(98)80206-7. [DOI] [PubMed] [Google Scholar]
- 29.Meves A., El-Azhary R.A., Talwalkar J.A., et al. Acute graft-versus-host disease after liver transplantation diagnosed by fluorescent in situ hybridization testing of skin biopsy specimens [J] J. Am. Acad. Dermatol. 2006;55(4):642–646. doi: 10.1016/j.jaad.2006.04.073. [DOI] [PubMed] [Google Scholar]
- 30.Taylor A.L., Gibbs P., Sudhindran S., et al. Monitoring systemic donor lymphocyte macrochimerism to aid the diagnosis of graft-versus-host disease after liver transplantation [J] Transplantation. 2004;77(3):441–446. doi: 10.1097/01.TP.0000103721.29729.FE. [DOI] [PubMed] [Google Scholar]
- 31.Martin P.J., Schoch G., Fisher L., et al. A retrospective analysis of therapy for acute graft-versus-host disease: secondary treatment [J] Blood. 1990;77(8):1821–1828. [PubMed] [Google Scholar]
- 32.Marubayashi S., Matsuzaka C., Takeda A., et al. Fatal generalized acute graft-versus-host disease in a liver transplant recipient [J] Transplantation. 1990;50(4):709–711. doi: 10.1097/00007890-199010000-00036. [DOI] [PubMed] [Google Scholar]
- 33.Chinnakotla S., Smith D.M., Domiati-Saad R., et al. Acute graft-versus-host disease after liver transplantation: role of withdrawal of immunosuppression in therapeutic management [J] Liver Transpl. 2010:13(1). doi: 10.1002/lt.20982. [DOI] [PubMed] [Google Scholar]
- 34.Hahn A.B., Baliga P. Rapid method for the analysis of peripheral chimerism in suspected graft-versus-host disease after liver transplantation [J] Liver Transpl. 2000;6(2):180–184. doi: 10.1002/lt.500060214. [DOI] [PubMed] [Google Scholar]
- 35.Comenzo R.L., Malachowski M.E., Rohrer R.J., et al. Anomalous ABO phenotype in a child after an ABO-incompatible liver transplantation [J] N. Engl. J. Med. 1992;326(13):867–870. doi: 10.1056/NEJM199203263261305. [DOI] [PubMed] [Google Scholar]
- 36.Gao P.J., Leng X.S., Wang D., et al. Graft versus host disease after liver transplantation: a case report [J] Front. Med. China. 2010;4(004):469–472. doi: 10.1007/s11684-010-0120-8. [DOI] [PubMed] [Google Scholar]
- 37.Walling H.W., Voigt M.D., Stone M.S. Lichenoid graft vs. host disease following liver transplantation [J] J. Cutan. Pathol. 2010;31(2):179–184. doi: 10.1111/j.0303-6987.2004.00146.x. [DOI] [PubMed] [Google Scholar]
- 38.Wu Z., Shi W. Rash as the first manifestation of acute graft-versus-host disease after orthotopic liver transplantation [J] Eur. J. Dermatol. 2011;21(6):997–998. doi: 10.1684/ejd.2011.1506. [DOI] [PubMed] [Google Scholar]
- 39.Kriss M., Feliciano J., Fryer J., et al. Haploidentical hematopoietic stem cell transplantation for graft-versus-host disease after liver transplantation [J] Blood. 2011;118(12):3448–3449. doi: 10.1182/blood-2011-05-353714. [DOI] [PubMed] [Google Scholar]