Abstract
Introduction
With the COVID-19 vaccine rollout is well underway now beginning in children ages 12 and over, it is unknown what percent of parents plan to vaccinate their children against COVID-19.
Method
The purpose of this descriptive correlational study was to examine parents’ attitudes, beliefs, and behaviors in administering a COVID-19 vaccine.
Results
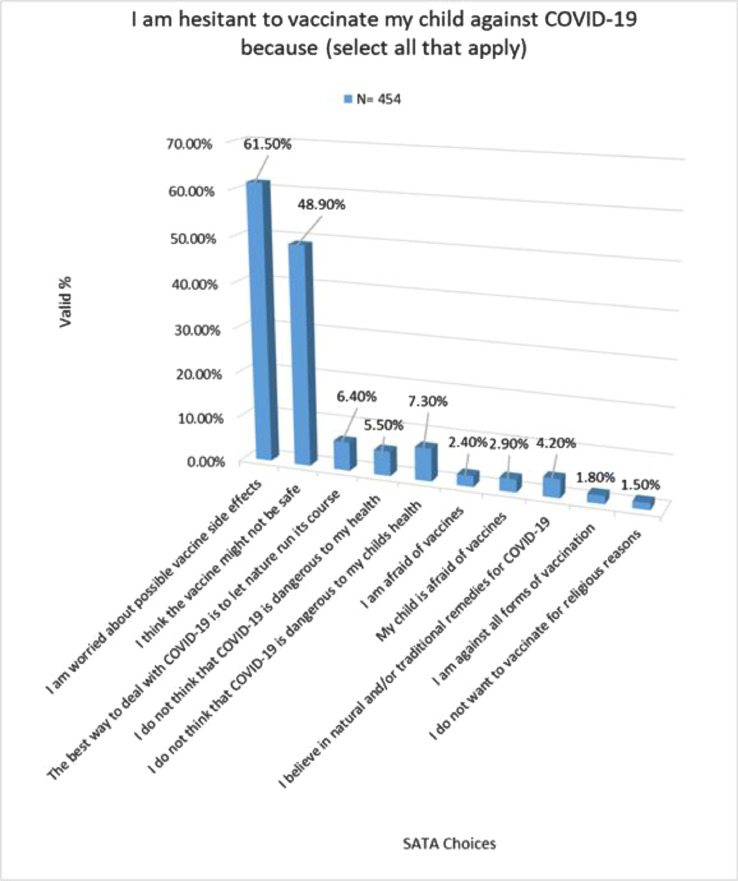
Only 21.93% of the subjects reported overall VH. Half of parents (49.45%) say they want the COVID vaccine for their child, and 44.17% plan to vaccinate against COVID once the vaccine becomes available to them. Concern for vaccine side effects (61.5%) and vaccine safety (48.96%) were significant factors that increased VH. In addition, there was a significant correlation between parents who were planning to vaccinate their child against the flu and being less VH about a COVID-19 vaccine for their child.
Discussion
This is the first known study to describe parental perceptions’ of COVID-19 VH and identify factors that increase VH for parents.
KEY WORDS: COVID-19, vaccine hesitancy, parent-perceptions, vaccinations
INTRODUCTION
Vaccines have long been a hot-button issue. It has been well-established and recognized that vaccination is one of the most important public health interventions which curbs the spread of viral illness, protects vulnerable populations and the public alike from disease, and ultimately saves lives (Callender, 2016). However, it is also well-known that various levels of hesitancy exist in different populations toward receiving vaccinations for a multitude of reasons. According to recently published research, 1 in 5 parents are vaccine-hesitant against the COVID-19 vaccine (Santibanez et al., 2020). COVID-19, also known as severe acute respiratory syndrome coronavirus 2 or more generally known to the public as the coronavirus, was identified in January of 2020 before spreading globally to over 170 countries (World Health Organization, 2020).
More than 2 million pediatric cases of COVID-19 have been reported, and more than 200 children have died, with a disproportionate rate in children in minority communities. Although a majority of the pediatric population seems relatively unaffected by the disease, there are many other factors that need to be considered, such as subpopulations of high-risk children, the true attributable risk for severe disease from COVID-19 (e.g., coinfection), and the role children play in community-based viral transmission (Cruz & Zeichner, 2020).
Children are beginning to be vaccinated, and the (Jenco, 2021) has called for the expansion of vaccine trials to include children (AAP.org). Both Pfizer and Moderna have completed enrollment for studies of children aged ≥ 12 years and expect to release the data over the summer. The Pfizer vaccine is already cleared for use starting in children aged ≥ 16 years. The Moderna vaccine is currently cleared for people aged ≥ 18 years. This means teenagers can now start being vaccinated.
Vaccine hesitancy (VH) is defined as “a behavior, influenced by a number of factors including issues of confidence (do not trust a vaccine or a provider), complacency (do not perceive a need for a vaccine or do not value the vaccine), and convenience (access).” (World Health Organization, 2012). To be proactive about the potential for VH, possible objections to the vaccine need to be identified and examined. VH is not seen equally across settings or communities. In many settings, parents or informal caregivers are provided with, or given access to, a variety of information and sources regarding vaccination. Alternatively, in other settings, there can be a lack of information and communication between provider and caregiver, resulting in a significant barrier to improving vaccination uptake and national coverage. Because parents are the drivers and users of their child's health care, it is also important to consider how personal beliefs, values, and lifestyle affect a person's ability to understand and trust the validity of the information being provided and therefore inform decisions surrounding childhood vaccines.
The purpose of this descriptive correlational study was to examine factors associated with parent-perceived vaccine decision making around a novel COVID-19 vaccine and compare this to parent-perceived vaccine decision making around the influenza vaccine. We wanted to achieve this by understanding factors that impact or influence parent-perceived vaccine decision making. Results from this research can help to inform best practices (such as methods of communication, messaging of the vaccine side effect, etc.) for addressing potential barriers to vaccinating children against COVID-19.
Background/Literature Review
Despite immunizations protecting children from serious illnesses, there remains a growing unacceptance of vaccinating children. Research has shown that there are various reasons for this which are multifaceted and not entirely well understood (Opel et al., 2011). COVID-19’s influence on vaccination behaviors is ongoing. Children were initially thought to be “spared” or asymptomatic carriers of the disease. We now know that this is not the case. In fact, the prevalence of unvaccinated children against the flu has increased in 2019 from previous years. Research by Santibanez and colleagues (2020) first reported on VH among parents of children during the COVID outbreak. Although their research focused on a variety of vaccine concerns related to various childhood immunizations, it specifically examined why fewer children received the flu vaccine in 2019 (during a pandemic). Ultimately, Santibanez's (2020) research showed that children with vaccine-hesitant parents were 26% less likely to receive a flu shot than children whose parents expressed no concerns. That said, not every parent who had reservations skipped the vaccine—34% to 47% of those children eventually were vaccinated, despite their parents’ doubts (Santibanez et al., 2020) .
The study performed by Ames et al. (2017), revealed that parents wanted more information in general, preferred to receive balanced information about vaccine benefits and harm, have difficulty discerning between validated information and biased information regarding vaccination, and viewed health care workers as an important source of information with certain expectations about the communication that would take place during the appointment. In another study by Kempe et al. (2020), an educational level lower than a bachelor's degree and household income of 400% of the federal poverty level predicted hesitancy for both routine childhood and influenza vaccines.
Children, particularly those aged < 6 years, maybe asymptomatic carriers and carry a higher viral load of COVID-19, meaning they can potentially spread it more easily than adults. Although vaccine administration has now begun in the United States, even with a safe vaccine for children, what are parents’ perceptions of a COVID vaccine for their children? This original research is the first known study to examine parents’ perceptions and intentions of vaccinating their child against the coronavirus.
For these reasons, it is an especially delicate time for parents to hesitate about vaccinating their children. Understanding factors that impact VH are critical in identifying potential areas or gaps to better address VH on both a patient level and a policy and public health level with regard to acquiring herd immunity.
Theoretical Framework
The Health Belief Model was used to guide this study. To prepare for the administration of children with a COVID-19 vaccine, it is important to assess the public and health communities regarding their readiness to implement and receive these vaccinations (Schaffer DeRoo, Pudalov, & Fu, 2020). The Health Belief Model suggests that people's beliefs about health problems, perceived benefits of action and barriers to action, and self-efficacy explain engagement (or lack of engagement) in health-promoting behavior.
Applying this model to our research, VH is the proxy to measure parental engagement (or lack of engagement) with their perceptions of administering a COVID-19 vaccine to children. A stimulus, or cue to action, must also be present to trigger the health-promoting behavior; for this research, the stimulus is the COVID-19 pandemic.
METHODS
The purpose of this descriptive correlational study was to examine factors associated with parent-perceived vaccine decision making around a COVID-19 vaccine and compare this to parent-perceived vaccine decision making around the influenza vaccine. We wanted to achieve this by understanding factors that impact or influence parent-perceived vaccine decision making.
Briefly, the Parental Attitudes About Childhood Vaccines (PACV) was a web-based survey that reads at a sixth-grade level and can be completed in less than 5 min. It contains 15 items under three domains (behavior, safety and efficacy, and general attitudes). In addition, for this study, we adapted elements of the PACV survey to COVID-specific questions. Furthermore, demographic items (parental age, parental educational level, marital status, race) were also included in the survey. Item scores were summed in an unweighted fashion to obtain a total raw score (percentage).
Odds ratios were calculated using logistic regression to isolate the adjusted effects of (1) immunization behavior, (2) vaccine safety and efficacy beliefs, (3) general attitudes and trust, and (4) demographics on the likelihood of intent to vaccinate for flu and COVID. Intent to vaccinate was generated from dichotomized survey questions “I plan to vaccinate my child against flu this season (or have already done so)” and “I plan to have my child vaccinated with a covid-19 vaccine if one becomes available.” All statistical analyses were performed using Stata (version 16.1; StataCorp, College Station, TX).
Results from this research can help to inform further research to develop or improve on immunization communication education strategies for parents regarding the administration of the COVID-19 vaccine to children.
Sample
English-literate parents of school-age children aged between 1 and 18 years were included. Participants’ children did not have to have been vaccinated before. Children who were terminally ill (under hospice care) or had other life-threatening comorbidities such as cancer were excluded from the study, as these conditions impact the administration of regularly scheduled vaccines.
Power Analysis
G*Power version 3.1.9.6 was used to conduct power analysis. The nonparametric Kendall tau-b-test was performed using SPSS (version 24; IBM, Armonk, NY) to examine correlations between variables. Statistical significance was concluded if p <.05. A power analysis was run a priori to determine the appropriate sample size. According to a survey performed by the Pew Research Center (2020), 49% would not get the coronavirus vaccine, and 32% of the population were identified as vaccine-hesitant . Therefore, assuming a type I error at 0.05 and a type II error at 0.7, a sample size of 38 participants was needed to show a statistical significance on the basis of the results of a power analysis.
Instruments
A web-based parental survey was administered using the PACV, and a COVID VH survey was adapted from the PACV. The PACV, developed by Opel and colleagues (2011), was one of the first validated survey tools to measure parental attitudes of VH. This tool, tested for construct validity and reliability, is an eight-item survey encompassing eight domains: immunization behavior, beliefs about vaccine safety and efficacy, attitudes, and trust. The COVID VH questionnaire, adapted from the PACV, was used; this is a 10-item Likert scale encompassing similar domains as the PACV but specifically directed toward the COVID vaccine. Parental demographic information was obtained in a 10-item questionnaire.
Procedure
Following Human Subjects and Institutional Review Board approval from the Massachusetts General Hospital, data were obtained from voluntary participation from parents of children (aged 1–18 years) recruited through social media who met the inclusion criteria. An invitation to participate in this study was posted on parent community groups and other social media posts. The snowball method was used for survey distribution online. No incentives were offered to participants, and survey responses were kept anonymous. Informed consent was requested on the introductory web page before survey enrollment. Confidentiality of information was assured. Participants were permitted to terminate participation in the survey at any time.
RESULTS
Among the 427 participants who responded, most parents were married (89.7%) and not Hispanic or Latino (81.1%). Similar results for the children were found, with 79.4% of children reporting not Hispanic or Latino (Table 1 ). Interestingly, much of the study population reported having a child at home with a chronic condition (74.9%). Other motivations for VH were minimally reported, including a general fear of vaccines (2.4%), being against all forms of vaccines (1.8%), and religious reasons (1.5%).
TABLE 1.
Parent and child demographics
| Demographic characteristics | Percentages (%) |
|---|---|
| Marital status | |
| Married | 89.7 |
| Divorced | 3.1 |
| Single | 3.4 |
| Other | 3.7 |
| Race of parents | |
| Hispanic or Latino | 2.9 |
| Not Hispanic or Latino | 81.1 |
| Other | 12 |
| Prefer not to answer | 4 |
| Race of children | |
| Hispanic or Latino | 4.6 |
| Not Hispanic or Latino | 79.4 |
| Other | 12 |
| Prefer not to answer | 4 |
| Parents have a child at home with a chronic condition | |
| Yes | 25.1 |
| No | 74.9 |
| Parent ethnicity | |
| White/Caucasian | 91.4 |
| Asian | 1.1 |
| Black or African American | 0.6 |
| Native Hawaiian and other Pacific Islander | 0.3 |
| Two or more races | 2 |
| Prefer not to answer | 4.6 |
| Ethnicity of children | |
| White/Caucasian | 84.9 |
| Asian | 0.9 |
| Black or African American | 1.2 |
| Two or more races | 8.4 |
| Prefer not to answer | 4.7 |
| Education level of parents | |
| Less than high school | 0.6 |
| High school or equivalent | 5.5 |
| Associate degree | 5.7 |
| Bachelor's degree | 35.1 |
| Master's degree | 37.9 |
| Doctoral degree | 15.2 |
| Insurance | |
| Yes | 98.3 |
| No | 1.7 |
| Number of children in home | |
| Yes | 75.7 |
| No | 24.3 |
| Age of children in home | |
| < 1 year | 9 |
| 12–35 months | 14.1 |
| 4–8 years | 34.1 |
| 8–12 years | 25.1 |
| 13–18 years | 23.6 |
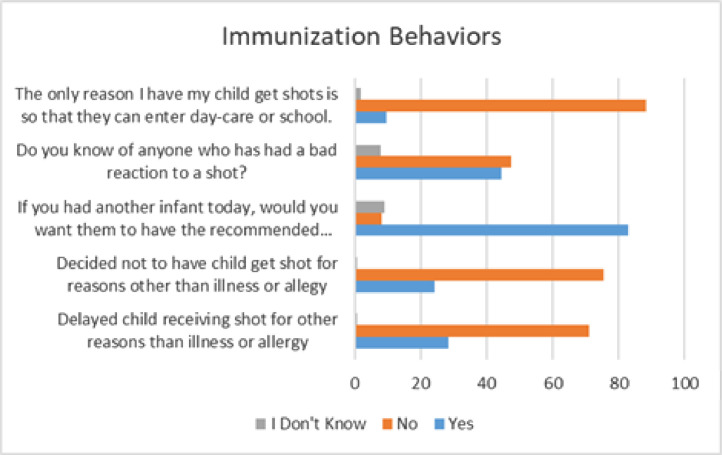
Parental immunization behaviors overall did not demonstrate increased VH as a larger percentage of respondents answered “no” to immunization behaviors. Only 21.93% of the subjects reported overall VH, and 93.03% reported that their child is up-to-date with all their vaccines. Although nearly half (46.94%) of respondents are less hesitant toward the flu vaccine than the COVID vaccine, most parents (81.61%) report that they have already or plan to vaccinate their child against flu this season. Although 44% of parents have a positive attitude toward the COVID vaccine, 69.53% of parents report more hesitancy to this vaccine than previous vaccinations (Figure 1 ). Half of parents (49.45%) say they want the COVID vaccine for their child, and 44.17% plan to vaccinate against COVID once the vaccine becomes available to them (Figure 2 and Table 2) .
FIGURE 1.
Immunization behaviors
This figure appears in color online at www.jpedhc.org.
FIGURE 2.
Parent-perceived vaccine hesitancy against the COVID-19 vaccine. SATA, STAT version 16, 2020
This figure appears in color online at www.jpedhc.org.
TABLE 2.
Results of correlation between parental vaccine hesitancy for flu vaccine and vaccine hesitancy for COVID vaccine
| Frequency (%) |
||||||
|---|---|---|---|---|---|---|
| Statement | 1 | 2 | 3 | 4 | 5 | Total |
| I plan to vaccinate my child against the flu this season (or have already done so). | 11.3 | 3.6 | 3.9 | 16.3 | 64.9 | 100.0 |
| I am less hesitant to vaccinate my child against the flu this season than COVID-19. | 22.9 | 10.2 | 20.1 | 20.7 | 26.2 | 100.0 |
| Regarding the COVID-19 vaccine, I have less hesitancy than with previous vaccinations. | 34.2 | 35.3 | 21.2 | 4.7 | 4.7 | 100.0 |
Results of Correlation Between Parental VH for Flu Vaccine and VH for COVID Vaccine
There was a significant correlation between how the participants responded to “I plan to vaccinate my child against the flu this season (or have already done so)” and “I am less hesitant to vaccinate my child against the flu this season than COVID-19” (p < .001). There was also a significant correlation between how the participants responded to “I plan to vaccinate my child against the flu this season (or have already done so)” and “Regarding the COVID-19 vaccine, I have less hesitancy than with previous vaccinations” (p < .001; Table 2).
Results of Parents’ Overall VH
Among all the participants, 46.9% reported that they either strongly agreed or agreed with this statement: I am less hesitant to vaccinate my child against the flu this season than COVID-19. Only 21.93% of the subjects reported overall VH, and 93.03% report that their child is up-to-date with all their vaccines. Although nearly half (46.94%) are less hesitant toward the flu vaccine than the COVID vaccine, the majority of parents (81.61%) report that they have already or plan to vaccinate their child against flu this season. Although 44% of parents have a positive attitude toward the covid vaccine, 69.53% of parents report more hesitancy to the COVID vaccine than previous vaccinations. Half of parents (49.45%) say they want the COVID vaccine for their child and 44.17% plan to vaccinate against COVID once the vaccine becomes available to them (data not shown).
Several reported immunization behaviors were shown to influence the likelihood of flu and covid vaccination (TABLE 3, TABLE 4, TABLE 5, TABLE 6 ). Having reportedly decided against a vaccine for reasons other than illness or allergy reduced the likelihood of flu vaccination while agreeing that wanting all the recommended shots for another infant increased the likelihood. Of note, believing it is the role of the parent to question shots and increased overall VH reduced the predicted likelihood of both flu and COVID vaccination.
TABLE 3.
Immunization behavior and intent to vaccinate
| Intent to vaccinate | p value | OR (95% CI) |
|---|---|---|
| Flu | ||
| Delayed child's shots for a reason other than illness or allergy | .693 | 1.162 (0.550–2.455) |
| Decided against shot for a reason other than illness or allergy | .000 | 0.198 (0.090–0.414) |
| Sure, following recommended shot schedule is good for the child | .860 | 1.073 (0.488–2.361) |
| It is role of parent to question shots | .000 | 0.275 (0.147–0.512) |
| If had another infant today, would want all recommended shots | .000 | 4.177 (2.054–0.849) |
| Overall hesitancy about childhood shots | .000 | 0.247 (0.123–0.494) |
| COVID | ||
| Delayed child's shots for a reason other than illness or allergy | .363 | 0.700 (0.325–1.507) |
| Decided against shot for a reason other than illness or allergy | .406 | 0.682 (0.277–1.680) |
| Sure, following recommended shot schedule is good for the child | .552 | 1.472 (0.411–5.272) |
| It is role of parent to question shots | .001 | 0.435 (0.268–0.705) |
| If had another infant today, would want all recommended shots | .192 | 1.99 (0.706–5.635) |
| Overall hesitancy about childhood shots | .012 | 0.328 (0.138–0.779) |
Note. CI, confidence interval; OR, odds ratio.
TABLE 4.
Vaccine safety and efficacy beliefs and intent to vaccinate
| Intent to vaccinate | p value | OR (95% CI) |
|---|---|---|
| Flu | ||
| Children get more shots than are good for them | .001 | 0.233 (0.102–0.532) |
| Many illnesses shots prevent are severe | .220 | 1.792 (0.705–4.557) |
| Better to develop immunity by getting sick | .019 | 0.294 (0.106–0.814) |
| Better for children to get fewer vaccines at the same time | .011 | 0.342 (0.151–0.778) |
| Concerned for serious side effect | .000 | 0.107 (0.039–0.294) |
| Concerned childhood shots not safe | .796 | 0.853 (0.255–2.847) |
| Concerned shot might not prevent disease | .452 | 1.369 (0.604–3.103) |
| Know anyone with bad reaction | .304 | 0.656 (0.295–1.462) |
| COVID | ||
| Children get more shots than are good for them | .587 | 0.786 (0.338–1.830) |
| Many illnesses shots prevent are severe | 1.000 | 2.12 (0.865–5.23) |
| Better to develop immunity by getting sick | .248 | 0.533 (0.183–1.549) |
| Better for children to get few vaccines at the same time | .000 | 0.365 (0.217–0.613) |
| Concerned for serious side effect | .000 | 0.270 (0.158–0.461) |
| Concerned childhood shots not safe | .058 | 0.319 (0.098–1.040) |
| Concerned shot might not prevent disease | .749 | 0.902 (0.480–1.694) |
| Know anyone with a bad reaction | .607 | 1.151 (0.672–1.972) |
Note. CI, confidence interval; OR, odds ratio.
TABLE 5.
General attitudes and trust and intent to vaccinate
| Intent to vaccinate | p value | OR (95% CI) |
|---|---|---|
| Flu | ||
| Get shots so child can enter daycare or school | .177 | 0.396 (0.103–1.516) |
| Trust information about shots | .003 | 12.239 (2.380–62.925) |
| Able to openly discuss concerns with doctor | .318 | 0.642 (0.269–1.529) |
| Child is up-to-date on all vaccines | .000 | 31.382 (5.819–169.239) |
| COVID | ||
| Get shots so child can enter daycare or school | .013 | 0.070 (0.008–0.569) |
| Trust information about shots | .000 | 6.120 (3.223–11.622) |
| Able to openly discuss concerns with doctor | .365 | 0.761 (0.422–1.373) |
| Child is up-to-date on all vaccines | .387 | 2.031 (0.407–10.138) |
Note. CI, confidence interval; OR, odds ratio.
TABLE 6.
COVID-specific general attitudes and intent for COVID vaccination
| Intent to vaccinate | p value | OR (95% CI) |
|---|---|---|
| Positive attitude toward COVID vaccine for child | .333 | 0.746 (0.413–1.348) |
| COVID high-risk people at home | .654 | 1.185 (0.563–2.497) |
| High-risk child (chronic condition) | .000 | 3.464 (1.912–6.278) |
| Concern for COVID infection for child or self | .110 | 0.631 (0.359–1.109) |
| Concerned COVID vaccine might not prevent disease | .000 | 0.089 (0.050–0.158) |
Note. CI, confidence interval; OR, odds ratio.
Trusting information about vaccines showed a significant increase in the likelihood in both flu and COVID vaccination intent. Although being up-to-date with all childhood vaccines increased the likelihood of flu vaccination, it did not significantly increase the likelihood of COVID vaccine intent (Table 4).
DISCUSSION
VH has been found to be a major barrier to achieving herd immunity. A recent study showed that depending on varying biological, environmental, and socio-behavioral factors, the threshold for COVID-19 herd immunity may be between 55% and 82% of the population (cite Journal of the American Medical Association article 2020). For herd immunity, we need to consider vaccination in our younger population. In addition, a flu outbreak during a time of a COVID pandemic has the potential to be devastating.
The results of this study showed that parental VH is more pronounced with the flu vaccine than with the COVID vaccine. This study also showed that parents who did plan to vaccinate their children against the flu did have less VH against also giving their child the COVID vaccine. Vaccine availability does not necessarily guarantee enough population vaccination because previous research indicates that vaccine compliance remains variable and inconsistent.
On the surface, a pandemic might suggest a reason to increase vaccination rates and change overall behaviors related to VH. For example, our research showed a significant correlation (p <.001) between parents who plan to vaccinate against the flu this season and having less VH against the influenza vaccine than the COVID-19 vaccine. This may suggest that the COVID pandemic has lessened VH against the influenza vaccine; it could also suggest that parents are more hesitant to have their child receive a novel COVID-19 vaccine.
In addition, parents whose children had previously received the influenza vaccination reported a higher likelihood of future vaccination because of the pandemic, whereas those whose children had not received the vaccination reported a decreased likelihood or intention to vaccinate their child against COVID-19. These findings are similar to research by Sokol and Grummon (2020), who suggested that the COVID-19 pandemic has led to increasing polarization of parents’ vaccination behaviors, whereby parents who previously did not vaccinate their children reported becoming even less likely to vaccinate their children during the pandemic.
Successful inoculation against this disease will require widespread education campaigns regarding vaccine safety and efficacy and health policies that address parental VH for the COVID vaccine. Without herd immunity, high-risk individuals would remain vulnerable to the COVID-19 virus (Schaffer DeRoo et al., 2020). Objections to the COVID vaccine need to be identified and examined. As was the case with our study, significant parental concerns included vaccine safety or misinformation surrounding vaccination in general.
A recent study by Kempe and colleagues (2020) reported that although U.S. parents are hesitant to vaccinate their children with routine immunizations because of safety concerns, parents who hesitate to have their children vaccinated for influenza do so with concerns about a low level of vaccine effectiveness. Similarly, Nyhan and Reifler (2015) found through a cross-sectional survey of a nationally representative sample that in terms of the influenza vaccine, providing corrective factual information to debunk myths such as that the flu vaccine causes the flu can lead to varied responses of whether the individuals intend to receive the vaccine or not. This aligns with prior research that information provided to disprove myths can be counterproductive (Nyhan & Reifler, 2015). It is also important to consider when trying to educate the public about vaccines what techniques are used, including educating with facts before debunking myths and always having the target audience in mind (Dubé, Gagnon, & Vivion, 2020).
Study Limitations
One limitation of the study is that parents were surveyed from November of 2020 to January of 2021 during the height of the pandemic. As such, the results may not be generalizable to later in the pandemic. Although this study's participants were randomly recruited from web-based parents’ social networks, they were predominately a White, English-speaking, insured, college-educated population living in the suburbs. Although the survey was translated into Spanish, no Spanish-speaking participants participated. It is understood that racially and ethnically diverse populations may have a different perspective about the safety of the COVID vaccine, which should be addressed in future studies.
In addition, it is important to address the collinearity of the study. In all real-world data, there is some degree of collinearity between predictor variables. In this study, this was addressed in two ways: increasing the sample size and transforming the predictor variables using simple regression between highly correlated variables and calculating the odds ratio of correlated variables.
Conclusions
Future studies should assess a broader and diverse parent population to fully understand the impact of VH. Despite these limitations, our results suggest that the COVID-19 vaccine rollout is just expanding to the adolescent population. It is important to better understand what parents identify as barriers to potentially vaccinating their children against COVID-19. Addressing parental VH is key in establishing broad community vaccination against COVID-19. This is the first known study to identify parents’ attitudes, beliefs, and behaviors around administering the COVID vaccine to their children.
Understanding the influence of this pandemic not only on vaccination behaviors related to the COVID vaccine but also how this affects vaccination behaviors of other vaccines is important. This research helps to better inform nurse practitioners and other health care providers about parental vaccine decision making around COVID-19 vaccination. Future research should focus on better understanding how to increase vaccine uptake during this COVID-19 pandemic.
Biographies
Kristine M. Ruggiero, Assistant Professor of Nursing, MGH Institute of Health Professions, Boston, MA; Nurse Practitioner/Nurse Scientist, Boston Children's Hospital, Waltham, MA; Nurse Faculty at Boston Nursing Institute, Waltham, MA.
John Wong, Associate Professor of Nursing, MGH Institute of Health Professions, Waltham, MA.
Casey Fryer Sweeney, Nurse Practitioner, Mass General Brigham Urgent Care, Boston, MA.
Alicia Avola, Graduate Student, MGH Institute of Health Professions, Boston, MA.
Andria Auger, Graduate Student, MGH Institute of Health Professions, Boston, MA.
Madeline Macaluso, Graduate Student, MGH Institute of Health Professions, Boston, MA.
Patricia Reidy, Professor and Associate Dean of Academic Affairs, MGH Institute of Health Professions, Boston, MA.
Footnotes
This work was supported by a COVID-19 grant from the MGH Institute of Health Professions, Boston, MA.
Conflicts of interest: None to report.
SUPPLEMENTARY MATERIALS
Parental Attitudes About Childhood Vaccines (PACV) survey tool can be found at https://doi.org/10.1016/j.pedhc.2021.04.005.
SUPPLEMENTARY TABLE 1.
Questions of the PACV survey, by category (adapted from Opel et al., 2011 [13])
| Immunization behavior |
| Have you ever delayed having your child get a shot for reasons other than illness or allergy? |
| Have you ever decided not to have your child get a shot for reasons other than illness or allergy? |
| How sure are you that following the recommended shot schedule is a good idea for your child? |
| Do you agree with the following statement? It is my role as a parent to question shots |
| If you had another infant today, would you want him/her to get all the recommended shots? |
| Overall, how hesitant about childhood shots would you consider yourself to be? |
| Beliefs about vaccine safety and efficacy |
| Do you agree with the following beliefs about vaccine safety and efficacy? |
| Children get more shots than are good for them |
| Many of the illnesses that shots prevent are severe |
| It is better for my child to develop immunity by getting sick than by getting a shot |
| It is better for children to get fewer vaccines at the same time |
| How concerned are you that your child might have a serious side effect from a shot? |
| How concerned are you that any one of the childhood shots might not be safe? |
| How concerned are you that a shot might not prevent the disease? |
| Do you know of anyone who has had a bad reaction to a shot? |
| General attitudes and trust |
| Which of the following statements reflect your general attitude and trust toward vaccines? |
| The only reason I have my child get shots is so that they can enter daycare or school |
| I trust the information I receive about shots |
| I can openly discuss my concerns about shots with my child's doctor |
| All things considered, how much do you trust your child's doctor? |
SUPPLEMENTARY TABLE 2.
COVID vaccine hesitancy questionnaire (adapted from Opel et al., 2011 [13])
| Please indicate your response with a checkmark (√) in the appropriate box, using the scale below: 1 = strongly disagree 2 = disagree 3 = neither agree nor disagree 4 = agree 5 = strongly agree |
| 1. I want a COVID vaccine for my child? |
| 2. What are parents’ attitudes toward a possible vaccine for COVID? |
| 3. My child is up-to-date on all their other vaccines. |
| 4. Regarding the COVID vaccine, I have less hesitancy than with previous vaccinations? |
| 5. Live with people at home who are considered at high risk for COVID? |
| 6. Is your child considered at higher risk (chronic condition)? |
| 7. Level of concern about COVID? |
| 8. How concerned are you that a COVID shot might not prevent the disease? |
| 9. How concerned are you that your child might have a serious side effect from a COVID shot? |
SUPPLEMENTARY TABLE 3.
Parent/child demographic questionnaire
| Questions |
| 1. Do parents have a child at home at with a chronic condition? |
| 2. Marital status of parent? |
| 3. Race/ethnicity of parents |
| 4. What is the education level of the parents? |
| 5. How would you identify the type of setting they live in (rural, urban, apartment, house)? |
| 6. Is there more than one child living at home? |
| 7. Age of children living at home: |
| < 1 year |
| 12–36 months |
| 36–48 months |
| 4–8 years |
| 8–12 years |
| 13–18 years |
References
- Callender D. Vaccine hesitancy: More than a movement. Human Vaccines & Immunotherapeutics. 2016;12(9):2464–2468. doi: 10.1080/21645515.2016.1178434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz A.T., Zeichner S.L. COVID-19 in children: Initial characterization of the pediatric disease. Pediatrics. 2020;145 doi: 10.1542/peds.2020-0834. [DOI] [PubMed] [Google Scholar]
- Dubé E., Gagnon D., Vivion M. Optimizing communication material to address vaccine hesitancy. Canada Communicable Disease Report. 2020;46:48–52. doi: 10.14745/ccdr.v46i23a05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenco Melissa, AAP News Eligible teens should receive the covid vaccine. Eligible teens should receive the covid vaccine. 2021 https://www.aappublications.org/news/2021/04/19/pediatric-covid-cases-041921 In this issue. [Google Scholar]
- Kempe A., Saville A.W., Albertin C., Zimet G., Breck A., Helmkamp L.…Szilagyi P.G. Parental hesitancy about routine childhood and influenza vaccinations: A national survey. Pediatrics. 2020;146 doi: 10.1542/peds.2019-3852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyhan B., Reifler J. Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine. 2015;33:459–464. doi: 10.1016/j.vaccine.2014.11.017. [DOI] [PubMed] [Google Scholar]
- Opel D.J., Mangione-Smith R., Taylor J.A., Korfiatis C., Wiese C., Catz S., Martin D.P. Development of a survey to identify vaccine-hesitant parents: The parent attitudes about childhood vaccines survey. Human Vaccines. 2011;7:419–425. doi: 10.4161/hv.7.4.14120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center . 2020. Intent to get a COVID-19 vaccine rises to 60% as confidence in research and development process increases.https://www.pewresearch.org/science/2020/12/03/intent-to-get-a-covid-19-vaccine-rises-to-60-as-confidence-in-research-and-development-process-increases/ Retrieved from. [Google Scholar]
- Santibanez T., Nguyen K., Greby S., Fisher A., Scanlon P., Bhatt A.…Singleton J. Parental Vaccine Hesitancy and Childhood Influenza Vaccination. Pediatrics. 2020;146 doi: 10.1542/peds.2020-007609. e2020007609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaffer DeRoo S., Pudalov N.J., Fu L.Y. Planning for a COVID-19 vaccination program. Journal of the American Medical Association. 2020;323:2458–2459. doi: 10.1001/jama.2020.8711. [DOI] [PubMed] [Google Scholar]
- Sokol R.L., Grummon A.H. COVID-19 and parent intention to vaccinate their children against influenza. Pediatrics. 2020;146:1–5. doi: 10.1542/peds.2020-022871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2012. SAGE working group dealing with vaccine hesitancy.http://www.who.int/immunization/sage/sage_wg_vaccine_hesitancy_apr12/en/ Retrieved from. [Google Scholar]
- World Health Organization . 2020. Coronavirus disease (COVID-19) situation report-167.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200705-covid-19-sitrep-167.pdf?sfvrsn=17e7e3df_4 Retrieved from. [Google Scholar]