Abstract
Objective
To evaluate physician perceptions and attitudes toward telemedicine use at a tertiary care academic institution in northeast Florida during the coronavirus disease 2019 pandemic.
Patients and Methods
An anonymous 38-question cross-sectional survey was developed using Qualtrics survey software (Qualtrics) and e-mailed to all staff physicians from all specialty disciplines at Mayo Clinic in Florida. The survey was open from August 17, 2020, through September 1, 2020. Collected data included general demographic characteristics and employment information, attitude and experience with telemedicine use before and during the coronavirus disease 2019 pandemic, perception of patients’ experience, and the effect of telemedicine on burnout.
Results
The survey was distributed to 529 eligible physicians at our institution, with 103 physicians responding (20%). The distribution of specialties was 22% primary care specialties, 41% other internal medicine subspecialties, and 18% surgical specialties. Collectively, 63% found comparable quality of care when provided virtually (vs in-person) whereas 80% perceived telemedicine as cost-effective. A total of 76% of physicians felt that telemedicine increased flexibility and control over patient care activities, with 36% reporting improved work-life balance and 30% reporting improved burnout symptoms. Overall, 42% preferred using telemedicine over in-person visits when possible.
Conclusion
Physicians generally had positive attitudes regarding the adoption of telemedicine and perceived that the quality of health care delivery as generally comparable to in-person care. Future studies are needed to explore attitudes regarding telemedicine after the pandemic and how this virtual technology may be further used to improve physicians’ professional and personal well-being.
Abbreviations and Acronyms: COVID-19, coronavirus disease 2019
Telemedicine includes the use of telecommunication technology to provide health care remotely.1 In 2020, the recent coronavirus disease 2019 (COVID-19) pandemic had various implications on health care delivery. This resulted in a need to adjust and provide quality care to patients while limiting potential exposure to the virus for both patients and health care professionals.2,3 During the pandemic, physicians have used videoconferencing or virtual communication software, video visits, telephone visits, and electronic written visits or e-consultations, with the potential advantages of providing comparable quality care while social distancing.2,3 Because of the pandemic, telemedicine has seen exponential growth and widespread adoption,4 consisting of more than 90% of visits in some clinics.5,6 Telemedicine has been used in almost every specialty, including procedural specialties.5,7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 Further, especially since the beginning of the COVID-19 pandemic, telemedicine use has increased internationally.18, 19, 20, 21
Although various forms of telemedicine, including phone calls and electronic messaging, have been used extensively in our clinic for years, the COVID-19 pandemic has led to the implementation and successful use of audiovisual technologies for patient care visits across the Mayo Clinic enterprise. These visits occur via commonly used commercial software, as these platforms are secure, Health Insurance Portability and Accountability Act compliant, and accessible to the general public.
Previous limited evidence suggested telemedicine to provide a generally effective, comparable, and satisfactory quality of care and sometimes with better clinical outcomes for certain conditions22; however, there is a paucity of larger studies on perception and attitude regarding patient-physician interactions, satisfaction with services, and the ease and comfort of using telemedicine, preference for face-to-face communication, technology infrastructure support, and insurance coverage,23 especially in physicians with limited experience using telemedicine technology before the COVID-19 pandemic. Reports from our institution reporting on patients treated virtually for possible and confirmed COVID-19 suggest that patients recognize telemedicine as a key component of receiving health care throughout the pandemic.24,25
Further, few studies have analyzed whether physicianwell-being and burnout are affected by the adoption of telemedicine, as telemedicine theoretically provides more flexibility in terms of physician time and geographical location while performing virtual visits.5 Up to the onset of the pandemic, Hartzband and Groopman26 pointed out that medicine had been at a crisis point regarding burnout. Increased flexibility from telemedicine supporting physician autonomy may enhance the experience of intrinsic motivation that staves off “amotivation” and burnout. Given this, we aim to address these gaps in the literature and provide insight into physician perceptions of telemedicine at Mayo Clinic in Florida.
Patients and Methods
This study included conducting a 38-question, 5-domain anonymous survey that was developed through expert panel consensus informed by certain elements from existing evidence and models, including the unified theory of acceptance and use of technology,27 Technology Acceptance Model 2,28 and diffusion of innovation frameworks.29,30 The survey was conducted using Qualtrics survey software (Qualtrics). A list of all staff physicians at the Jacksonville campus of Mayo Clinic as of August 1, 2020 was obtained. The survey was distributed via e-mail to all staff physicians. Anonymous links and Quick Response codes were sent to all physicians. All specialties were included; however, traditional nonclinical specialties including diagnostic radiology, pathology, and nonclinical physician research were excluded from the survey to minimize outliers and positive skewing. The survey remained open for 2 weeks from August 17, 2020, through September 1, 2020, and results were collected in Qualtrics. Participation was optional and voluntary. Our study was deemed exempt by the Mayo Clinic Institutional Review Board. For the purposes of our study, telemedicine was defined as the use of commercially available audiovisual software programs for videoconferencing with patients for scheduled consultations or return visits. Other commonly used forms of telemedicine, such as e-consultations or phone calls, were excluded given the widespread use of these before COVID-19. The survey included general demographic characteristics and professional information as well as 5 distinctive domains: (1) overall experience with telemedicine use before and during COVID-19, (2) future adaptability to using telemedicine, (3) perception about patients’ experience, (4) and the effect of telemedicine on burnout, and (5) narrative reflections and accounts of experience of barriers of facilitators to using telemedicine. All questions were Likert-like scale questions with the exception of narrative reflections domain (typed entry). Variables of interest included current academic position based on time practicing at our institution (associate consultant, senior associate consultant, and consultant, with the rank of consultant being achieved after 3 years), specialty, years in practice following residency, current clinical full-time equivalent, age, sex, frequency of telemedicine use before COVID-19, length of period of using telemedicine technology. A copy of the survey is included in Supplemental Table 1 (available online at http://www.mcpiqojournal.org).
Physician subspecialties were grouped into the following categories: primary care (community internal medicine and family medicine), internal medicine subspecialties (ie, pulmonology, hematology, and gastroenterology), surgery and surgical subspecialties (ie, orthopedic surgery, ophthalmology, vascular surgery, and neurosurgery), dermatology, rehabilitation, and radiation oncology.
Descriptive statistics were performed for all questions. Comparisons of the 5 specific domains of interest—“I am open to using telemedicine routinely in the future for consultations,” “I am open to using telemedicine routinely in the future for return visits,” “Assuming both are equally appropriate, I prefer to use telemedicine over face-to-face visits,” “What role has telemedicine played in your experience of burnout,” and “Overall, my work-life balance has been improved with telemedicine”—were made using the Wilcoxon rank sum test (current position), the Spearman test of correlation (years of practice following residency and age), or the Kruskal-Wallis rank sum test (specialty). P values of less than .05 were considered as statistically significant. All statistical tests were 2-sided. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Inc.).
Results
The survey was distributed to 529 physicians at our institution, with a total of 115 physicians providing responses to the survey. There were 12 incomplete survey responses or surveys that were submitted in error, leaving 103 responses for analysis. Thus, the response rate was approximately 19.5% of physicians in eligible specialties.
Approximately 78% of physicians were consultants, indicating that they have worked within the institution for at least 3 years. Of the 103 respondents, approximately 22% were in primary care specialties, 41% were in internal medicine subspecialties, and 18% were in surgery or surgical subspecialties. Years in practice following residency were fairly evenly distributed from less than 5 to more than 30. Before the COVID-19 pandemic, 72% of physicians had not used telemedicine before. A summary of physician characteristics and previous experiences with telemedicine is provided in Table 1.
Table 1.
Physician Characteristics and Previous Experience With Telemedicine
| Characteristic | No. (%) of physicians |
|---|---|
| Current position (n=103) | |
| Associate consultant | 1 (1.0) |
| Senior associate consultant | 22 (21.4) |
| Consultant | 80 (77.7) |
| Specialty (n=103) | |
| Primary care | 23 (22.3) |
| Internal medicine subspecialties | 42 (40.8) |
| Surgery and surgical subspecialties | 18 (17.5) |
| Neurology | 9 (8.7) |
| Radiation oncology | 5 (4.9) |
| Physical medicine and rehabilitation | 4 (3.9) |
| Dermatology | 2 (1.9) |
| Years in practice following residency (n=103) | |
| <5 | 12 (11.7) |
| 5-10 | 29 (28.2) |
| 11-20 | 23 (22.3) |
| 21-30 | 27 (26.2) |
| >30 | 12 (11.7) |
| Current clinical FTE (n=102) | |
| <0.20 | 1 (1.0) |
| 0.20-0.40 | 1 (1.0) |
| 0.41-0.60 | 4 (3.9) |
| 0.61-0.80 | 8 (7.8) |
| 0.81-1.00 | 88 (86.3) |
| Age (n=103) | |
| 31-40 y | 32 (31.1) |
| 41-50 y | 30 (29.1) |
| 51-60 y | 23 (22.3) |
| >60 y | 18 (17.5) |
| Sex (n=102) | |
| Female | 33 (32.0) |
| Male | 69 (67.0) |
| How often did you use telemedicine before COVID-19? (n=103) | |
| Never | 74 (71.8) |
| Occasionally (1-12 times per year) | 10 (9.7) |
| Frequently (>1 time per month or >12 times per year) | 19 (18.4) |
| How many years have you been using telemedicine technology for any type of consults or return visits? (n=103) | |
| 0-1 y | 93 (90.3) |
| 2-3 y | 4 (3.9) |
| >3 y | 6 (5.8) |
COVID-19, coronavirus disease 2019; FTE, full-time equivalent.
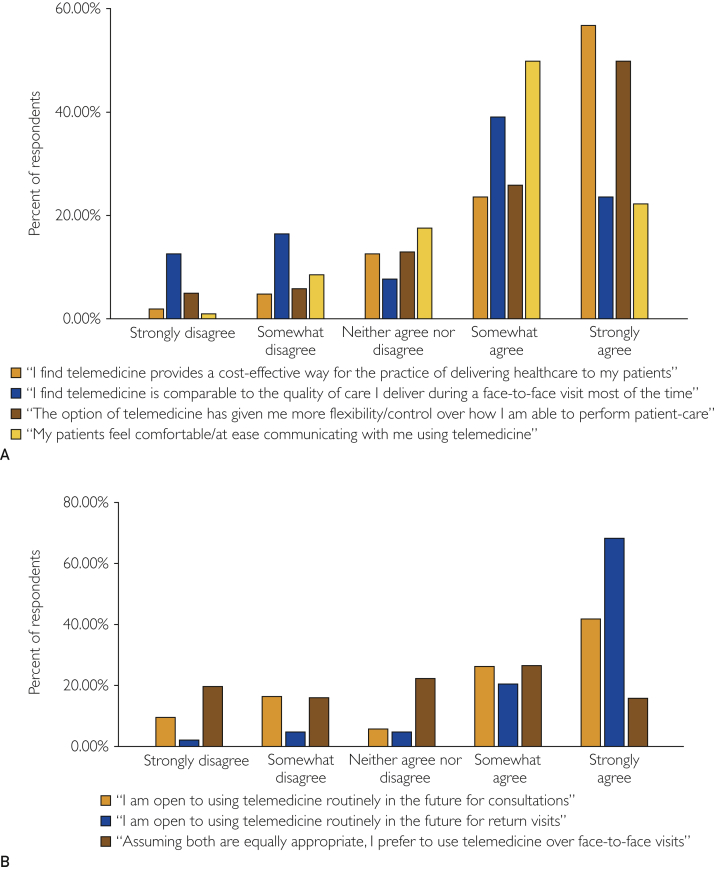
A summary of responses for each question of the survey is provided in Table 2 and in Figure 1. Specifically, approximately 63% of respondents agreed or strongly agreed that the quality of care delivered using telemedicine was comparable to face-to-face visits and approximately 80% of respondents either agreed or strongly agreed that telemedicine is a cost-effective way to deliver health care. Approximately 76% of physicians felt that telemedicine has increased flexibility and control over how the physician performs patient care activities.
Table 2.
Physician Perceptions and Attitudes Toward Telemedicine
| Responses | n | No. (%) of physicians |
|---|---|---|
| I find telemedicine has been easy to navigate and use | 101 | |
| Strongly disagree | 2 (2.0) | |
| Somewhat disagree | 3 (3.0) | |
| Neither agree not disagree | 9 (8.9) | |
| Somewhat agree | 33 (32.7) | |
| Strongly agree | 54 (53.5) | |
| I feel skilled at using telemedicine | 103 | |
| Strongly disagree | 3 (2.9) | |
| Somewhat disagree | 3 (2.9) | |
| Neither agree not disagree | 7 (6.8) | |
| Somewhat agree | 46 (44.7) | |
| Strongly agree | 44 (42.7) | |
| I find it easy to solve technological errors during a telemedicine visit | 102 | |
| Strongly disagree | 6 (5.9) | |
| Somewhat disagree | 27 (26.5) | |
| Neither agree not disagree | 24 (23.5) | |
| Somewhat agree | 36 (35.3) | |
| Strongly agree | 9 (8.8) | |
| I find telemedicine provides a cost-effective way for the practice of delivering healthcare to my patients | 102 | |
| Strongly disagree | 2 (2.0) | |
| Somewhat disagree | 5 (4.9) | |
| Neither agree not disagree | 13 (12.7) | |
| Somewhat agree | 24 (23.5) | |
| Strongly agree | 58 (56.9) | |
| I find telemedicine is comparable to the quality of care I deliver during a face-to-face visit most of the time | 102 | |
| Strongly disagree | 13 (12.7) | |
| Somewhat disagree | 17 (16.7) | |
| Neither agree not disagree | 8 (7.8) | |
| Somewhat agree | 40 (39.2) | |
| Strongly agree | 24 (23.5) | |
| I feel comfortable/at ease communicating with my patients using telemedicine | 103 | |
| Strongly disagree | 4 (3.9) | |
| Somewhat disagree | 5 (4.9) | |
| Neither agree not disagree | 10 (9.7) | |
| Somewhat agree | 20 (19.4) | |
| Strongly agree | 64 (62.1) | |
| I feel I have sufficient IT support for telemedicine visits in my practice | 102 | |
| Strongly disagree | 3 (2.9) | |
| Somewhat disagree | 17 (16.7) | |
| Neither agree not disagree | 17 (16.7) | |
| Somewhat agree | 35 (34.3) | |
| Strongly agree | 30 (29.4) | |
| The option of telemedicine has given me more flexibility/control over how I am able to perform patient-care activities | 100 | |
| Strongly disagree | 5 (5.0) | |
| Somewhat disagree | 6 (6.0) | |
| Neither agree not disagree | 13 (13.0) | |
| Somewhat agree | 26 (26.0) | |
| Strongly agree | 50 (50.0) | |
| The telemedicine system in my practice needs technological improvements | 103 | |
| Strongly disagree | 6 (5.8) | |
| Somewhat disagree | 12 (11.7) | |
| Neither agree not disagree | 27 (26.2) | |
| Somewhat agree | 49 (47.6) | |
| Strongly agree | 9 (8.7) | |
| I am open to using telemedicine routinely in the future for consultations | 103 | |
| Strongly disagree | 10 (9.7) | |
| Somewhat disagree | 17 (16.5) | |
| Neither agree not disagree | 6 (5.8) | |
| Somewhat agree | 27 (26.2) | |
| Strongly agree | 43 (41.7) | |
| I am open to using telemedicine routinely in the future for return visits | 103 | |
| Strongly disagree | 2 (1.9) | |
| Somewhat disagree | 5 (4.9) | |
| Neither agree not disagree | 5 (4.9) | |
| Somewhat agree | 21 (20.4) | |
| Strongly agree | 70 (68.0) | |
| Learning to use telemedicine has positively affected my professional growth | 103 | |
| Strongly disagree | 5 (4.9) | |
| Somewhat disagree | 5 (4.9) | |
| Neither agree not disagree | 26 (25.2) | |
| Somewhat agree | 28 (27.2) | |
| Strongly agree | 39 (37.9) | |
| Assuming both are equally appropriate, I prefer to use telemedicine over face-to-face visits | 102 | |
| Strongly disagree | 20 (19.6) | |
| Somewhat disagree | 16 (15.7) | |
| Neither agree not disagree | 23 (22.5) | |
| Somewhat agree | 27 (26.5) | |
| Strongly agree | 16 (15.7) | |
| I plan to obtain continued medical education (CME) credits to enhance my knowledge of telemedicine | 103 | |
| Strongly disagree | 10 (9.7) | |
| Somewhat disagree | 21 (20.4) | |
| Neither agree not disagree | 44 (42.7) | |
| Somewhat agree | 18 (17.5) | |
| Strongly agree | 10 (9.7) | |
| My patients find telemedicine easy to navigate and use | 101 | |
| Strongly disagree | 4 (4.0) | |
| Somewhat disagree | 20 (19.8) | |
| Neither agree not disagree | 21 (20.8) | |
| Somewhat agree | 48 (47.5) | |
| Strongly agree | 8 (7.9) | |
| My patients find it easy to solve technological errors during a telemedicine visit | 100 | |
| Strongly disagree | 12 (12.0) | |
| Somewhat disagree | 36 (36.0) | |
| Neither agree not disagree | 26 (26.0) | |
| Somewhat agree | 25 (25.0) | |
| Strongly agree | 1 (1.0) | |
| My patients find using telemedicine for consultations to be more cost-effective than face-to-face visits | 102 | |
| Strongly disagree | 1 (1.0) | |
| Somewhat disagree | 7 (6.9) | |
| Neither agree not disagree | 35 (34.3) | |
| Somewhat agree | 35 (34.3) | |
| Strongly agree | 24 (23.5) | |
| My patients find using telemedicine for return visits to be more cost-effective than face-to-face visits | 100 | |
| Strongly disagree | 1 (1.0) | |
| Somewhat disagree | 4 (4.0) | |
| Neither agree not disagree | 25 (25.0) | |
| Somewhat agree | 42 (42.0) | |
| Strongly agree | 28 (28.0) | |
| My patients find telemedicine comparable to the quality of care they receive during a face-to-face visit | 101 | |
| Strongly disagree | 3 (3.0) | |
| Somewhat disagree | 16 (15.8) | |
| Neither agree not disagree | 30 (29.7) | |
| Somewhat agree | 41 (40.6) | |
| Strongly agree | 11 (10.9) | |
| My patients feel comfortable/at ease communicating with me using telemedicine | 102 | |
| Strongly disagree | 1 (1.0) | |
| Somewhat disagree | 9 (8.8) | |
| Neither agree not disagree | 18 (17.6) | |
| Somewhat agree | 51 (50.0) | |
| Strongly agree | 23 (22.5) | |
| My patients find using telemedicine to be time saving | 102 | |
| Strongly disagree | 0 (0.0) | |
| Somewhat disagree | 2 (2.0) | |
| Neither agree not disagree | 16 (15.7) | |
| Somewhat agree | 33 (32.4) | |
| Strongly agree | 51 (50.0) |
Figure 1.
Survey results regarding physician perceptions and applicability of telemedicine. A, Physician attitudes toward the quality and possible advantages of telemedicine. B, Openness of respondents to using telemedicine after the coronavirus disease 2019 pandemic.
Overall, physicians feel that they have adequate technological support and feel skilled at using telemedicine, with 87% of respondents feeling skilled at using telemedicine and 55% agreeing that patients find telemedicine easy to use.
Physicians also feel that patients like telemedicine visits. Approximately 51% of physicians agree that patients find quality of care with telemedicine to be comparable to the quality of care during a face-to-face visit, and 73% agree that patients are at ease with communicating over telemedicine.
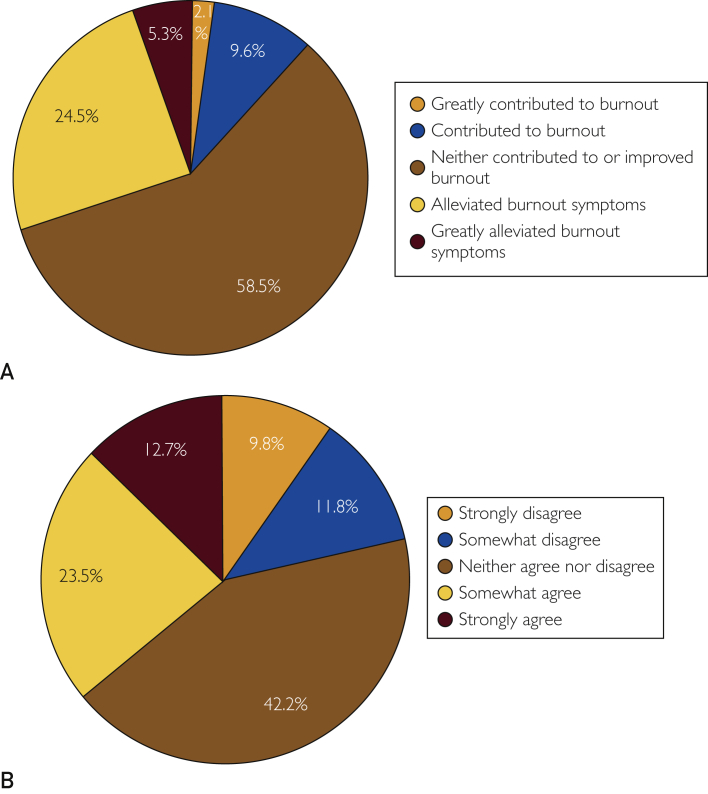
In regard to burnout, approximately 30% of respondents felt that telemedicine alleviated symptoms of burnout and 36% agreed that work-life balance has improved with the use of telemedicine (Table 3; Figure 2). Primary care physicians were statistically more likely to have burnout symptoms alleviated by telemedicine (P=.006) and improved work-life balance (P<.001) with telemedicine than internal medicine subspecialties, surgical subspecialties, or other specialties (Supplemental Tables 2-5, available online at http://www.mcpiqojournal.org). There were no significant differences for these questions when comparing position (P=.61 and P=.62, respectively), years in practice (P=.69 and P=.38, respectively), or age (P=.51 and P=.28, respectively).
Table 3.
Physician Burnout and the Influence of Telemedicine
| Variable | n | No. (%) of physicians |
|---|---|---|
| Before COVID-19—I feel burned out from my work | 102 | |
| Never | 11 (10.8) | |
| A few times per year | 29 (28.4) | |
| Once a month | 17 (16.7) | |
| A few times per month | 25 (24.5) | |
| A few times per week | 13 (12.7) | |
| Every day | 7 (6.9) | |
| During COVID-19—I feel burned out from my work | 102 | |
| Never | 17 (16.7) | |
| A few times per year | 23 (22.5) | |
| Once a month | 12 (11.8) | |
| A few times per month | 29 (28.4) | |
| A few times per week | 8 (7.8) | |
| Every day | 13 (12.7) | |
| What role has telemedicine played in your experience of burnout | 94 | |
| Greatly contributed to burnout | 2 (2.1) | |
| Contributed to burnout | 9 (9.6) | |
| Neither contributed to or improved burnout | 55 (58.5) | |
| Alleviated burnout symptoms | 23 (24.5) | |
| Greatly alleviated burnout symptoms | 5 (5.3) | |
| Overall, my work-life balance has been improved with telemedicine | 102 | |
| Strongly disagree | 10 (9.8) | |
| Somewhat disagree | 12 (11.8) | |
| Neither agree nor disagree | 43 (42.2) | |
| Somewhat agree | 24 (23.5) | |
| Strongly agree | 13 (12.7) |
COVID-19, coronavirus disease 2019.
Figure 2.
Responses regarding physician burnout and the influence of telemedicine. A, “What role has telemedicine played in your experience of burnout?” B, “Overall, my work-life balance has been improved with telemedicine.”
There was no difference between consultants and senior associate consultants (P=.50), years in practice (P=.28), younger or older physicians (P=.56), or specialty group (P=.14) for openness to using telemedicine in the future for consultations. Similarly, there were no statistically significant differences among the same groups for telemedicine use for return visits (P=.9, P=.19, P=.39, and P=.058, respectively).
Overall, 68% of physicians are open to using telemedicine in the future for consultations and 88% of physicians are open to using telemedicine routinely in the future for follow-up visits or appointments. Assuming all other factors are equal and there is no detriment to patient care, approximately 42% of physicians prefer to use telemedicine over face-to-face visits, with 22% of physicians reporting neutral feelings.
Discussion
Our data suggest that physicians have adapted to the implementation of telemedicine technology for clinical consultations and follow-ups. In our study, most respondent physicians felt skilled at using the technology. Interestingly, almost all physicians were open to using telemedicine routinely for follow-up visits after the resolution of the pandemic, with just under half of respondents preferring telemedicine over face-to-face visits. The findings from this work are similar to other previously reported data on the adoption of telemedicine use. For example, Gillman-Wells et al9 found that 70% of plastic surgeons surveyed in the United Kingdom embraced the use of telemedicine. Qualitative surveys by Srinivasan et al31 of personnel at Stanford University’s general primary care clinics found that respondents strongly believed that video visits should be an ongoing part of medical practice after the pandemic.
The generally favorable reviews of telemedicine and physician willingness to adapt the technology is likely secondary to multiple reasons, including cost-effectiveness of care, time-savings to both the physician and patients, and increased flexibility of scheduling telemedicine visits, which may all contribute to improved physician quality of life. Additionally, our results suggest that telemedicine is associated with decreased cost and more time-savings for patients, especially those who are required to travel for care. This is necessarily balanced against concerns regarding quality of care and the lack of physical examination inherent of video consultations, although physicians in our study largely feel that the quality of care is similar.
Perceived cost-effectiveness of telemedicine compared to traditional in-person care is one of the primary reasons cited for the positive attitudes toward telemedicine, with 80% of physicians agreeing that telemedicine is a cost-effective way to deliver care. To quantify this, a study by Demaerschalk et al32 evaluating postoperative visit costs found that patients who used video telemedicine services saved an average of $888 per return visit, increasing to $1501 when accounting for travel and accommodations. The authors report a savings of $256 per visit even for those patients who did not need accommodations. Furthermore, a study from the pediatric cardiology service at Coimbra University Hospital Center analyzed telemedicine use in Portugal since 1998 and estimated that approximately €1.1 million (∼$1.3 million) in the health system and approximately €419 (∼$500) per patient have been saved since adopting telemedicine.20
Additionally, there is substantial time-savings for both physicians and patients with the adoption of telemedicine, with approximately 75% of respondents agreeing that telemedicine use has improved flexibility. For physicians, the perceived improvement in flexibility is likely multifaceted but most likely because of time-savings and flexibility with scheduling. First, telemedicine visits can be performed anywhere, such as in the office setting or a secure home setting, which may afford greater flexibility for physicians who may be balancing increasing demands both at work and at home, especially during the pandemic. Second, video visits may be easier to reschedule as opposed to in-person visits, in which patients frequently travel and have limited flexibility to reschedule. Third, video consultations and returns may limit some of the time-consuming logistics of the clinic, such as waiting to room or check in patients or walking from clinic room to clinic room. Regardless, more research is needed to quantify the time-savings and identify the factors that contribute.
Time-savings is also seen with patients. In a meta-analysis by Chaudhry et al,8 patients receiving either telemedicine or in-person visits for orthopedic care found that telemedicine improved time-savings for patients, both when including travel time (180 minutes) and when excluding travel time (17 minutes).
Despite the benefits many physicians experienced with telemedicine implementation, approximately one-third of physicians surveyed do not believe that telemedicine is comparable to face-to-face visits. One of the leading concerns is regarding the potential disparities in quality of care for telemedicine as compared with that for in-person visits. Although telemedicine can be largely cost-effective and saves time, this comes at a cost of losing the ability to perform an adequate physical examination, something that is vital to practice and adequate care of patients. Additionally, the physician-patient relationship is largely reliant on personal communications, such as “small talk,” which is largely eliminated when using telemedicine software. As telemedicine is more widely used now than at the time of the study, further survey studies will be vital to understand physician concerns and the relative importance of these concerns.
Perhaps the most often cited concern regarding telemedicine is the feeling of being unable to provide comparable care virtually. Zhang et al5 looked at this very question at the Memorial Sloan Kettering Cancer Center during the COVID-19 pandemic. They found that 92% of radiation oncology visits were conducted via telemedicine during the peak of the pandemic. Seventy-one percent of respondents reported that there was no difference in the ability to treat cancer appropriately, with 55% having no difference in overall visit quality.5
To support the finding that quality of care is equivalent with telemedicine visits, a study from Stanford’s ClickWell Care clinic evaluated ordering patterns for telemedicine visits or in-person visits. Interestingly, there were no differences in laboratory tests ordered, imaging tests ordered, or prescriptions ordered between virtual and in-person visits for 17 of the most common diagnoses, although there were overall more laboratory and imaging tests ordered following in-person visits for any diagnosis, likely reflecting general medical examinations.33
Another primary concern with the use of telemedicine is the lack of physical examinations. The physical examination remains a critical component of follow-up care, especially when evaluating for adverse effects of therapy or in patients with physical limitations.34 Despite the lack of physical examinations available during telemedicine visits, some clinicians are working to develop examinations suited for telemedicine and in-person use, such as the neurosurgical spine examination that has been adopted for telemedicine use.10 A study by Piche et al35 found that overall, virtual spine examinations for low back pain may be comparable to in-person examinations and patients are overall satisfied with virtual evaluations. Laskowski et al36 have developed a specific set of guidelines to enhance the evaluation of the musculoskeletal system as well.
Patient satisfaction with telemedicine is critically important, as the cost- and time-savings are meaningless if patients do not feel they are receiving similar high-quality care. Although our study did not survey patients directly, approximately 75% of physicians felt that patients are at ease communicating over telemedicine, with half agreeing that patients find the technology easy to use and the quality of care is comparable to face-to-face visits. Similar studies of providers in the National Health Service in the United Kingdom found that approximately 73% of respondents felt that patients understood the medical conditions and recommendations when given over the phone, and 70% of respondents felt that video conferencing adds to patient care.37 In the meta-analysis by Chaudhry et al,8 there were no differences in surgeon satisfaction or patient-reported outcome measures when comparing telemedicine or in-person visits.8 Previous studies have also reported patient satisfaction with telemedicine at a large health system in California.38
One of the promises of telemedicine is to reduce burnout by allowing physicians to have more flexibility over their schedule. For instance, physicians may be able to see patients virtually while improving work-life balance at home. Furthermore, telemedicine may decrease commuting time, freeing up time for sleep, family time, and other social events, which all are primary factors for burnout.16 Our data suggest that approximately one-third of physicians experience either improved work-life balance or improved symptoms of burnout due to telemedicine, although these statistics are confounded by the other stressors associated with the COVID-19 pandemic. Further study is needed to fully assess whether, and how, burnout can be reduced by more widespread adoption of telemedicine after the pandemic.
Looking ahead, telemedicine will likely be an important component of clinic in the post-COVID world. To help compensate for the lack of physical presence during virtual visits, virtual reality has been suggested as a way to enhance the feeling of physical presence during the examination.39 Additionally, telemedicine can be used preferentially in populations that have expressed interest in, or particularly benefit from, telemedicine. For example, patients with anxiety and depression tend to prefer telemedicine visits and have more frequent visits in the virtual setting according to 1 analysis.33 Another potential benefit of telemedicine is to improve access to routine and preventive health care for underrepresented groups, such as underrepresented minorities or patients in rural communities, that may not be able to cover the expense or time of travel to clinic for routine follow-up. Furthering this, telemedicine can also be used to offer clinical trial participation to these underrepresented populations, as intensive follow-up protocols and toxicity management can be performed virtually.
Even though our data suggest that physicians have overall positive perceptions and attitudes regarding telemedicine, our study is not without limitations. First, our study is survey based, with the typical limitations of survey-based evaluations, including complete responses and a low response rate. Furthermore, there is a relatively small sample size of some of the subgroups that were examined when making comparisons of survey responses, which results in a lack of sufficient power to detect significant differences. Therefore, the possibility of a type II error (ie, a false-negative finding) is important to consider. Additionally, this work provides a thorough and important representation of physician attitudes and reflections, including the effect of technology on burnout and well-being—something that has not been addressed widely before,40 especially during times of crises like the COVID-19 pandemic.
At approximately the same time as our study, the COVID-19 Healthcare Coalition, of which Mayo Clinic is a participant, surveyed more than 1500 providers regarding the use of telemedicine. In their study, approximately 68% of patients were motivated to increase the use of telemedicine (68% in our study) and 55% found that telemedicine improved satisfaction with work (36% in our study had improved work-life balance).41,42 Taken together, our study and the study by the COVID-19 Healthcare Coalition support the notion that telemedicine is an important component of medicine delivery. Additional research is needed to identify whether these attitudes persist in the post–COVID-19 clinical environment.
Future research could explore the sustainability of telemedicine, cost benefit of telemedicine, and potential causal relationships between telemedicine and burnout prevention. We acknowledge that many patients do not have access to, or knowledge of, the technology required for telemedicine. Further research can investigate methods to improve this health care delivery to potentially underserved patients.
Conclusion
This survey analysis found that physicians generally had positive attitudes regarding the adoption of telemedicine and felt that the quality of care is generally comparable with that delivered during in-person visits. Importantly, most physicians are open to using telemedicine after the pandemic for consultations and routine follow-ups. Additionally, approximately one-third of physicians reported an improved work-life balance or improvement in subjective burnout symptoms with telemedicine. Future studies are needed to explore attitudes regarding telemedicine after the pandemic and how the technology can be used to improve physician well-being.
Footnotes
Potential Competing Interests: The authors report no competing interests.
Supplemental material can be found online at: http://www.mcpiqojournal.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
Supplemental Online Material
References
- 1.Wootton R. Recent advances: telemedicine. BMJ. 2001;323(7312):557–560. doi: 10.1136/bmj.323.7312.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barnett M.L., Ray K.N., Souza J., Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA. 2018;320(20):2147–2149. doi: 10.1001/jama.2018.12354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehrotra A., Jena A.B., Busch A.B., Souza J., Uscher-Pines L., Landon B.E. Utilization of telemedicine among rural medicare beneficiaries. JAMA. 2016;315(18):2015–2016. doi: 10.1001/jama.2016.2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miner H., Fatehi A., Ring D., Reichenberg J.S. Clinician telemedicine perceptions during the COVID-19 pandemic. Telemed J E Health. 2021;27(5):508–512. doi: 10.1089/tmj.2020.0295. [DOI] [PubMed] [Google Scholar]
- 5.Zhang H., Cha E.E., Lynch K. Radiation oncologist perceptions of telemedicine from consultation to treatment planning: a mixed-methods study. Int J Radiat Oncol Biol Phys. 2020;108(2):421–429. doi: 10.1016/j.ijrobp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peden C.J., Mohan S., Pagan V. Telemedicine and COVID-19: an observational study of rapid scale up in a US academic medical system. J Gen Intern Med. 2020;35(9):2823–2825. doi: 10.1007/s11606-020-05917-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arimany-Manso J., Pujol R.M., García-Patos V., Saigí U., Martin-Fumadó C. Medicolegal aspects of teledermatology. Actas Dermosifiliogr (Engl Ed) 2020;111(10):815–821. doi: 10.1016/j.ad.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chaudhry H., Nadeem S., Mundi R. How satisfied are patients and surgeons with telemedicine in orthopaedic care during the COVID-19 pandemic? A systematic review and meta-analysis. Clin Orthop Relat Res. 2021;479(1):47–56. doi: 10.1097/CORR.0000000000001494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gillman-Wells C.C., Sankar T.K., Vadodaria S. COVID-19 reducing the risks: telemedicine is the new norm for surgical consultations and communications. Aesthetic Plast Surg. 2021;45(1):343–348. doi: 10.1007/s00266-020-01907-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goyal D.K.C., Divi S.N., Schroeder G.D. Development of a telemedicine neurological examination for spine surgery: a pilot trial. Clin Spine Surg. 2020;33(9):355–369. doi: 10.1097/BSD.0000000000001066. [DOI] [PubMed] [Google Scholar]
- 11.Guido-Estrada N., Crawford J. Embracing telemedicine: the silver lining of a pandemic. Pediatr Neurol. 2020;113:13–14. doi: 10.1016/j.pediatrneurol.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lew S.Q., Wallace E.L., Srivatana V. Telehealth for home dialysis in COVID-19 and beyond: a perspective from the American Society of Nephrology COVID-19 Home Dialysis Subcommittee. Am J Kidney Dis. 2021;77(1):142–148. doi: 10.1053/j.ajkd.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moon H.S., Wang T.T., Rajasekaran K., Brewster R., Shanti R.M., Panchal N. Optimizing telemedicine encounters for oral and maxillofacial surgeons during the COVID-19 pandemic. Oral Surg Oral Med Oral Pathol Oral Radiol. 2021;131(2):166–172. doi: 10.1016/j.oooo.2020.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pareek P., Vishnoi J.R., Kombathula S.H., Vyas R.K., Misra S. Teleoncology: the youngest pillar of oncology. JCO Glob Oncol. 2020;6:1455–1460. doi: 10.1200/GO.20.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh A.K., Kasle D.A., Jiang R. A review of telemedicine applications in otorhinolaryngology: considerations during the coronavirus disease of 2019 pandemic. Laryngoscope. 2021;131(4):744–759. doi: 10.1002/lary.29131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vogt E.L., Mahmoud H., Elhaj O. Telepsychiatry: implications for psychiatrist burnout and well-being. Psychiatr Serv. 2019;70(5):422–424. doi: 10.1176/appi.ps.201800465. [DOI] [PubMed] [Google Scholar]
- 17.Ziadé N., Hmamouchi I., El Kibbi L. The impact of COVID-19 pandemic on rheumatology practice: a cross-sectional multinational study. Clin Rheumatol. 2020;39(11):3205–3213. doi: 10.1007/s10067-020-05428-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jafarzadeh-Esfehani R., Mirzaei Fard M., Habibi Hatam-Ghale F. Telemedicine and computer-based technologies during coronavirus disease 2019 infection; a chance to educate and diagnose. Arch Iran Med. 2020;23(8):561–563. doi: 10.34172/aim.2020.60. [DOI] [PubMed] [Google Scholar]
- 19.Kim A.Y., Choi W.S. Considerations on the implementation of the telemedicine system encountered with stakeholders’ resistance in COVID-19 pandemic. Telemed J E Health. 2021;27(5):475–480. doi: 10.1089/tmj.2020.0293. [DOI] [PubMed] [Google Scholar]
- 20.Maia M.R., Castela E., Pires A., Lapão L.V. How to develop a sustainable telemedicine service? A Pediatric Telecardiology Service 20 years on—an exploratory study. BMC Health Serv Res. 2019;19(1):681. doi: 10.1186/s12913-019-4511-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malhotra N., Sakthivel P., Gupta N., Nischal N., Ish P. Telemedicine: a new normal in COVID era; perspective from a developing nation. [published online ahead of print September 2, 2020]. Postgrad Med J. [DOI] [PubMed]
- 22.Ekeland A.G., Bowes A., Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform. 2010;79(11):736–771. doi: 10.1016/j.ijmedinf.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 23.Kruse C.S., Krowski N., Rodriguez B., Tran L., Vela J., Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crane S.J., Ganesh R., Post J.A., Jacobson N.A. Telemedicine consultations and follow-up of patients with COVID-19. Mayo Clin Proc. 2020;95(9S):S33–S34. doi: 10.1016/j.mayocp.2020.06.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jethwa T., Ton A., Paredes Molina C.S. Establishing Mayo Clinic’s coronavirus disease 2019 virtual clinic: a preliminary communication. Telemed J E Health. 2020;26(11):1419–1423. doi: 10.1089/tmj.2020.0145. [DOI] [PubMed] [Google Scholar]
- 26.Hartzband P., Groopman J. Physician burnout, interrupted. N Engl J Med. 2020;382(26):2485–2487. doi: 10.1056/NEJMp2003149. [DOI] [PubMed] [Google Scholar]
- 27.Venkatesh V., Thong J.Y.L., Xu X. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Q. 2012;36(1):157–178. [Google Scholar]
- 28.Venkatesh V., Davis F.D. A theoretical extension of the technology acceptance model: four longitudinal field studies. Manag Sci. 2000;46(2):186–204. [Google Scholar]
- 29.Rogers E. 5th ed. Simon & Schuster; New York: 2003. Diffusion of Innovations. [Google Scholar]
- 30.Berwick D.M. Disseminating innovations in health care. JAMA. 2003;289(15):1969–1975. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- 31.Srinivasan M., Asch S., Vilendrer S. Qualitative assessment of rapid system transformation to primary care video visits at an academic medical center. Ann Intern Med. 2020;173(7):527–535. doi: 10.7326/M20-1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Demaerschalk B.M., Cassivi S.D., Blegen R.N. Health economic analysis of postoperative video telemedicine visits to patients’ homes. Telemed J E Health. 2021;27(6):635–640. doi: 10.1089/tmj.2020.0257. [DOI] [PubMed] [Google Scholar]
- 33.Norden J.G., Wang J.X., Desai S.A., Cheung L. Utilizing a novel unified healthcare model to compare practice patterns between telemedicine and in-person visits. Digit Health. 2020;6 doi: 10.1177/2055207620958528. 2055207620958528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Finazzi T., Papachristofilou A., Zimmermann F. “Connection failed”: a word of caution on telemedicine in radiation oncology. Int J Radiat Oncol Biol Phys. 2020;108(2):435–437. doi: 10.1016/j.ijrobp.2020.06.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Piche J., Butt B.B., Ahmady A., Patel R., Aleem I. Physical examination of the spine using telemedicine: a systematic review. https://doi.org/10.1177/2192568220960423 [published online ahead of print September 22, 2020]. Global Spine J. [DOI] [PMC free article] [PubMed]
- 36.Laskowski E.R., Johnson S.E., Shelerud R.A. The telemedicine musculoskeletal examination [published correction appears in Mayo Clin Proc. 2020;95(10):2299] Mayo Clin Proc. 2020;95(8):1715–1731. doi: 10.1016/j.mayocp.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elawady A., Khalil A., Assaf O., Toure S., Cassidy C. Telemedicine during COVID-19: a survey of Health Care Professionals’ perceptions. Monaldi Arch Chest Dis. 2020;90(4) doi: 10.4081/monaldi.2020.1528. [DOI] [PubMed] [Google Scholar]
- 38.Reed M.E., Huang J., Parikh R. Patient-provider video telemedicine integrated with clinical care: patient experiences. Ann Intern Med. 2019;171(3):222–224. doi: 10.7326/M18-3081. [DOI] [PubMed] [Google Scholar]
- 39.Riva G., Gamberini L. Virtual reality in telemedicine. Telemed J E Health. 2000;6(3):327–340. doi: 10.1089/153056200750040183. [DOI] [PubMed] [Google Scholar]
- 40.Talaee N., Varahram M., Jamaati H. Stress and burnout in health care workers during COVID-19 pandemic: validation of a questionnaire. https://doi.org/10.1007/s10389-020-01313-z [published online ahead of print June 6, 2020]. Z Gesundh Wiss. [DOI] [PMC free article] [PubMed]
- 41.COVID-19 healthcare coalition surveys physicians on telehealth impact during COVID-19. ATA (American Telemed Association) website. www.americantelemed.org/covid-19/telehealth-impact-physician-survey/ Accessed September 15, 2020.
- 42.Telehealth impact: physician survey analysis. COVID-19 Healthcare Coalition website. c19hcc.org/telehealth/physician-survey-analysis/ Accessed September 15, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.