Abstract
Background
The purpose of this study was to compare shoulder outcomes and function after humeral shaft fractures treated with plates and screws vs. antegrade nailing.
Methods
A group of 27 patients treated with plates and a group of 30 patients (previously published) who had undergone antegrade locked intramedullary nailing, all with acute humeral shaft fractures, were retrospectively compared. Final shoulder range of motion (ROM), full shoulder ROM recovery rate, functional outcomes, residual pain, complications, and elbow flexion-extension range were also analyzed.
Results
There were a total of 57 patients: 27 cases in the plate (P) group and 30 in the nail (N) group (average age, 41.9 years).There were 66.7% men in group N and 63.0% in group P. The average age was 38 years (interquartile range [IQR] 28) in group N and 37 years (IQR 55) in group P. There were no differences in follow-up between groups, which averaged 28 months (IQR 7) in group P and 30 months (IQR 2) in group N (P = .385). There was no difference in both groups in elbow flexion-extension. Group P had a full shoulder ROM (66.6% vs. 40.0%; P = .02) and excellent Rodríguez-Merchán scoring (66% vs. 40.0%; P < .01), which was significantly higher than in group N. In group P, the Constant score was 95 (IQR 9).
Conclusions
Treatment with plates in this comparative study led to a better ROM in the shoulder and fewer complications. Loss of shoulder motion may be expected after humeral shaft osteosynthesis. However, the functional scores and the healing index can be good and excellent with both techniques.
Keywords: Plates vs. nail, Shoulder outcomes, Humeral shaft fractures, Fracture fixation, Internal fixation, Plates, Nailing, Shoulder range of motion
The treatment of humeral shaft fractures is still controversial. In most of these fractures, treatment is nonsurgical. But in those cases where surgery is indicated, the election between rigid nails and plates with screws is difficult. Multiple studies on this topic have been published, but they usually conclude that there are no differences in outcomes by comparison. In addition, few investigations focus on the analysis of the final function in the affected shoulder. The comparisons of outcomes between nails and plates usually do not objectively report the shoulder range of motion (ROM).1,4 The mostly used functional scores generally underestimate the movement loss, as it is feasible to achieve an “excellent” score, even when the patient loss is 30° of anterior flexion.5,6,14
In our previously published series treated with antegrade locked nails, a decrease of shoulder ROM, beyond good functional scores, was observed. Apart from this, the riskiest variable associated with the loss of ROM was the presence of some milliliters of subacromial impingement. Therefore, is it possible to obtain better shoulder outcomes with plates?
The objective of this study was to compare the functional outcomes in patients with humeral shaft fractures treated with plates and screws with a series of patients treated with nails, with a special focus on final shoulder ROM and complications.
Materials and methods
This study was approved by our institutional ethics committee.
This is a retrospective comparative study. Participants were identified in our health record database. The patients included were older than 18 and treated with 4.5-mm plates and screws for acute humeral shaft fractures between 2014 and 2017, with a minimum follow-up of 2 years. Patients who had undergone a previous surgery in the same shoulder, arm, or elbow were excluded. Twenty-nine patients met the criteria, but one did not have complete follow-up data, and one was excluded because of a chronic neurologic lesion. This group was analyzed and compared with a previously published series of 30 patients treated with nails.15
The surgical indication was for displaced fractures.
Preoperative and final follow-up X-rays were evaluated.
Fractures were classified as per the Arbeitsgemeinschaft für Osteosynthesefragen classification (AO).14 Fracture healing status and final shoulder ROM, including forward elevation, external rotation, and internal rotation, were evaluated. The patients were also assessed by the Rodríguez-Merchán criteria,17 which simultaneously evaluates shoulder and elbow ROM. Subjective data, such as pain, were also considered on a graded scale: none, occasional, pain with activity, and variable pain. General subjective disability was rated as none, minimal, moderate, and severe. The final scores were qualified as excellent, good, fair, and poor, using the lowest score of each item for the final result.
Shoulder forward elevation and external rotation were measured with a manual goniometer. Internal rotation was determined by the highest spinal level reached by the thumb, graded as follows: T7, excellent; T12, good; L5, fair; and <L5, poor.
In the plate (P) group, the Constant score was used as well.
The following variables were compared: gender, age, fracture type as per the AO classification, full shoulder ROM, Rodríguez-Merchán score, complications, and associated injuries.
A full ROM was considered with shoulder flexion of 180°, external rotation of 90°, and internal rotation with the thumb reaching T7 or higher.
The anterolateral or posterior approach was used for all cases in the P group. The surgical approach was determined as per the location of the fracture. The anterolateral approach was used for midshaft and proximal shaft fractures, whereas the posterior approach was used for more distal diaphyseal fractures.
All nail surgeries were performed with the patient in a beach-chair position by an anterolateral acromial approach, dissection between the anterior and middle deltoid, and a longitudinal incision through the supraspinatus tendon.
Statistical analysis
The variables were presented for median and interquartile range (IQR) for numerical variables and absolute values with their percentages for categorical variables. The comparison between numerical variables was analyzed with the Wilcoxon rank sum test, and the Fisher exact test was used for the categorical variables. Logistic regression was used for the multivariate analysis. A value of P < .05 was considered significant. Data were analyzed with STATA/MP 14 version package.
Results
There were a total of 57 patients, 27 cases in the P group and 30 in the nail (N) group. The demographic characteristics were similar in both groups. Sixty-six percent of the patients treated with a nail and 63% of those treated with plates were men. The average age was 38 years (Interquartile rank [IQR] 28) in group N and 37 years (IQR 55) in group P (Table I).
Table I.
Comparative demographics baseline data.
| Demographic variables | Plate (n = 27) | Nail (n = 30) | P value |
|---|---|---|---|
| Sex, male, n (%) | 17 (63.0%) | 20 (66.7%) | .788 |
| Age in yr, median (IQR) | 37 (55) | 38 (28) | .791 |
| Fractures characteristics | |||
| Side, n (%) | .528 | ||
| Right | 11 (40.7%) | 13 (43.3%) | |
| Left | 16 (59.3%) | 17 (56.7%) | |
| Associated injuries, n (%) | 0 | 8 (26.7%) | .004 |
| Fracture type | .163 | ||
| A | 16 (59.3%) | 22 (73.3%) | .021 |
| B | 7 (25.9%) | 7 (23.3%) | .400 |
| C | 4 (14.8%) | 1 (3.33%) | .196 |
IQR, interquartile range.
Bold values indicate statistical significance.
There were no differences in follow-up between groups, which averaged 28 months (IQR 7) in group P and 30 months (IQR 2) in group N (P = .385). All fractures were healed in the P group and 28 of 30 in the N group (93%; P = .273).
There were no differences between groups in the elbow flexion-extension range and type of fractures (Table I).
The P group had a greater percentage of patients who reached 100% of shoulder ROM (66.6% vs. 40.0%; P = .02). As per the Rodríguez-Merchán criteria in the P group, 18 patients achieved excellent results (66%), 7 good (26%), and 2 obtained poor outcomes (8%). On the other hand, in the N group, the Rodríguez-Merchán score was 12 patients excellent (40%), 7 good (23%), 6 regular (20%), and 5 poor (16.6%).
The Constant score in the P group was 95 (IQR 9).
There were fewer complications in the P group, but this variable was not statistically significant (7.4% vs. 20.0%; P = .163). These complications included 2 postsurgical infections that were treated with surgery and endovenous antibiotics.
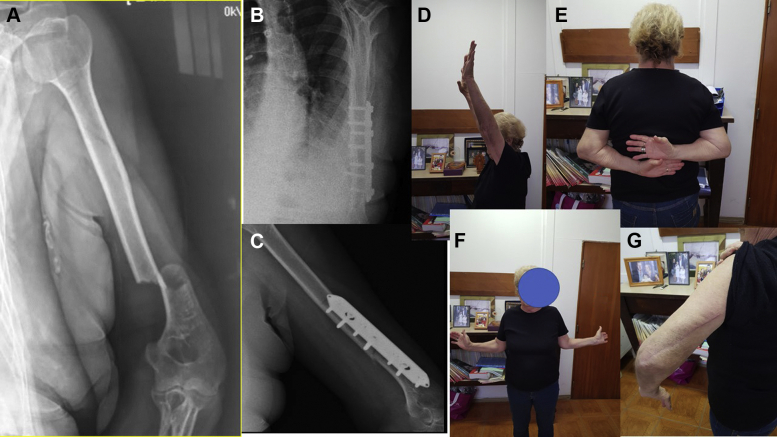
The N group reported subacromial nail impingement (1-2 mm of protrusion) in 8 patients (26%), 5 complications including 2 cases of nonunion, 1 case of radial neuroapraxia, 1 granuloma and 1 tuberosity fracture15 (Table II, Fig. 1).
Table II.
Comparative results.
| Variable | P group | N group | P value |
|---|---|---|---|
| Healing rate (%) | 27 (100%) | 28 (93.3%) | 0.273 |
| Complications (%) | 2 (7.4%) | 5 (20.0%) | 0.163 |
| Full shoulder ROM 100%, n (%) | 18 (66.6%) | 12 (40%) | 0.021 |
| Foward elevation median (IQR) | 180° (RIQ 20°) | 170° (RIQ 40°) | 0.046 |
| External rotation median (IQR) | 90° (RIQ 10) | 85° (RIQ 20) | 0.196 |
| Internal rotation vertebrae level, n (%) | 0.004 | ||
| D7 | 14 (51.9%) | 16 (53.3%) | |
| D10 | 7 (25.9%) | -(0%) | |
| D12 | 5 (18.5%) | 6 (20%) | |
| L5 | -(0%) | 6 (20%) | |
| S1 | 1 (3.7%) | 2 (6.7%) | |
| Elbow extension, median(RIQ) | 0° (RIQ 5°) | 0° (RIQ 5°) | 0.451 |
| Elbow flexion, median(IQR) | 140° (RIQ 15°) | 137.5° (RIQ 10) | 0.311 |
| Pain n (%) | 1 (3.7%) | 5 (16.7%) | 0.122 |
| Rodriguez-Merchán score | 0.005 | ||
| Excellent | 18 (67%) | 12 (40.0%) | |
| Good | 7 (26%) | 7 (23%) | |
| Fair | -(0%) | 6 (20%) | |
| Poor | 2 (7%) | 5 (16%) |
IQR, interquartile range.
Bold values indicate statistical significance.
Figure 1.
A 78-year-old patient. (A) X-ray showing fracture type. (B and C) X-rays showing healed fracture. (D, E, and F) Final shoulder ROM. (G) Posterior approach. ROM, range of motion.
Treatment method, fracture type, and age were included in the multivariate analysis. It was observed that the chance to achieve a complete shoulder ROM was 6.50 times greater in patients treated with plates than those treated with nails (odds ratio, 6.50; confidence interval, 1.40-26.58; P = .010; Table III).
Table III.
Variables association with full shoulder ROM. Logistic regression model.
| Variables association with full shoulder ROM | OR∗ | CI 95% | P value |
|---|---|---|---|
| Type of treatment | |||
| Nails | 1.00 | - | - |
| Plate | 6.50 | 1.56-27.09 | .010 |
| Fracture type | |||
| A | 1.00 | - | - |
| B† | 1.16 | 0.26-5.11 | .846 |
| C‡ | 2.81 | 0.23-34.15 | .417 |
| Age | 0.95 | 0.92-0.98 | .002 |
CI, confidence interval; IQR, interquartile range; OR, odds ratio; ROM, range of motion.
Odds ratio adjusted to the other variables included in the model.
Compare A vs. B.
Compare A vs. C.
Discussion
In the present study, we observed a clear difference in favor of the P group concerning the final rates of shoulder ROM.
The treatment of humeral shaft fractures remains controversial. The evidence is not clear in reference to outcomes and complications between methods. Comparative series and meta-analysis usually make little reference to the final shoulder function and objective measurement of ROM. In our opinion, the decrease in shoulder mobility is usually underestimated because of the scoring used.1,4, 5, 6,8,14,18
In a previously published series of patients treated with nails, we identified a percentage of patients who had lost some mobility grades despite the good general scoring.15 This was related mainly to nail subacromial impingement. After that evaluation, we decided to make osteosynthesis with plates and screws for humeral shaft fractures. In the present study, we performed a comparison between methods with special attention to the final shoulder function.
In the P group, we obtained better functional outcomes. The average shoulder elevation was 169° with plates vs. 157° with nails (P = .046). Internal rotation was significantly better in the P group (P = .004). On the other hand, the average external rotation was better in the P group (83° plate vs. 75° nail), but this difference was not significant (P = .196). As per the Rodríguez-Merchán criteria, we found a difference regarding the percentage of excellent results: 66% in patients treated with plates and 40% with nails (P = .021).
Concerning shoulder mobility, it is difficult to compare the literature because the studies typically do not report details of the final ROM with absolute values (in degrees).
Gracitelli et al11 compared nails and plates with the mini invasive plate osteosynthesis technique. They concluded that there are no differences between groups. In this article, the University of California, Los Angeles score was used in the comparison, so the final function can be underestimated because it gives a maximum score with 150° of anterior flexion and does not include shoulder rotations. In addition, they have not reported the final range in grades. This is why we did not consider the shoulder evaluation to be complete and objective. We decided to use the Rodríguez-Merchán score, which grants the excellent score only with a full ROM. We also divided the cases between those that achieved and did not achieve full ROM.
Regarding complications, in a meta-analysis, Wen et al21 reports that in multiple comparative studies between both methods, no significant differences were found.
In our series treated with plates, we had 2 infections: a superficial infection treated with antibiotics and a deep infection treated with debridement and antibiotics.
In another meta-analysis, Heineman et al9 did not find significant differences between implants in the total rate of complications, nonunion, infection, nerve injury, or revision surgeries.
With regards to the functional results and the risk of suffering shoulder movement restriction, the aforementioned meta-analysis has shown (in the same way as the present study) that open reduction and plate fixation yielded superior results over the group treated with intramedullary nails, and no significant difference between mini invasive plate osteosynthesis and nail groups was found. Other meta-analyses suggested that the plates could reduce the incidence of shoulder deficit.13
Some studies have related the decrease of shoulder function in cases treated with intramedullary nails to a nerve injury, accidental proximal nail migration, rotator cuff injury, capsulitis, and other factors.2,10,16
The current literature remains inconclusive when comparing surgery complications between plates and nails.10 Treatment with the humeral nail has been associated with a higher incidence of shoulder impingement, pain, and hardware removal.3,12,20 On the other hand, open reduction and internal fixation through an anterolateral or posterior approach requires significant soft-tissue dissection and local vascularization damage, which could decrease the potential of healing, with a higher risk of deep infection and iatrogenic nerve injury.7,11,19
We acknowledge as limitations those of any retrospective study: the number of cases and different fracture types. But, we find some strengths, such as the control group with a special focus on the final shoulder function, long-term follow-up, and having the same surgical team. We consider that our findings add information to the knowledge about final clinical results in these fractures.
Conclusion
In this comparative study, treatment with plates led to a better ROM in the shoulder and fewer complications. However, functional scores and healing rates can be good and excellent with both techniques. A loss of shoulder motion may be expected after humeral shaft osteosynthesis. Prospective studies are necessary with a long-term follow-up to strengthen these findings.
Disclaimers
Funding: No funding was disclosed by the author(s).
Conflicts of interest: The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional Ethical Committee approval was received from the Comite de Etica, Hospital Militar Central, HGRL 601-HMC, Acta folio 6- 2020.
References
- 1.Benegas E., Ferreira Neto A.A., Gracitelli M.E., Malavolta E.A., Assunção J.H., Prada Fde S., Bolliger Neto R., Mattar R., Jr. Shoulder function after surgical treatment of displaced fractures of the humeral shaft: a randomized trial comparing antegrade intramedullary nailing with minimally invasive plate osteosynthesis. J Shoulder Elbow Surg. 2014;23:767–774. doi: 10.1016/j.jse.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 2.Bhandari M., Devereaux P.J., McKee M.D., Schemitsch E.H. Compression plating versus intramedullary nailing of humeral shaft fractures--a meta-analysis. Acta Orthop. 2006;77:279–284. doi: 10.1080/17453670610046037. [DOI] [PubMed] [Google Scholar]
- 3.Chapman J.R., Henley M.B., Agel J., Benca P.J. Randomized prospective study of humeral shaft fracture fixation: intramedullary nails versus plates. J Orthop Trauma. 2000;14:162–166. doi: 10.1097/00005131-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Cheng H.R., Lin J. Prospective randomized comparative study of antegrade and retrograde locked nailing for middle humeral shaft fracture. J Trauma. 2008;65:94–102. doi: 10.1097/TA.0b013e31812eed7f. [DOI] [PubMed] [Google Scholar]
- 5.Constant C.R., Murley A.H. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987:160–164. [PubMed] [Google Scholar]
- 6.Ellman H., Hanker G., Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68:1136–1144. [PubMed] [Google Scholar]
- 7.Fan Y., Li Y.W., Zhang H.B., Liu J.F., Han X.M., Chang X., Weng X.S., Lin J., Zhang B.Z. Management of humeral shaft fractures with intramedullary Interlocking nail versus locking compression plate. Orthopedics. 2015;38:e825–e829. doi: 10.3928/01477447-20150902-62. [DOI] [PubMed] [Google Scholar]
- 8.Farouk O., Krettek C., Miclau T., Schandelmaier P., Guy P., Tscherne H. Minimally invasive plate osteosynthesis and vascularity: preliminary results of a cadaver injection study. Injury. 1997;28:A7–A12. doi: 10.1016/s0020-1383(97)90110-8. [DOI] [PubMed] [Google Scholar]
- 9.Heineman D.J., Poolman R.W., Nork S.E., Ponsen K.J., Bhandari M. Plate fixation or intramedullary fixation of humeral shaft fractures. Acta Orthop. 2010;81:216–223. doi: 10.3109/17453671003635884. Erratum in: Acta Orthop. 2010 Oct;81(5):647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hohmann E., Glatt V., Tetsworth K. Minimally invasive plating versus either open reduction and plate fixation or intramedullary nailing of humeral shaft fractures: a systematic review and meta-analysis of randomized controlled trials. J Shoulder Elbow Surg. 2016;25:1634–1642. doi: 10.1016/j.jse.2016.05.014. [DOI] [PubMed] [Google Scholar]
- 11.Lee T., Yoon J. Newly designed minimally invasive plating of a humerus shaft fracture; a different introduction of the plate. Int Orthop. 2016;40:2597–2602. doi: 10.1007/s00264-015-3097-8. [DOI] [PubMed] [Google Scholar]
- 12.Matsunaga F.T., Tamaoki M.J., Matsumoto M.H., Netto N.A., Faloppa F., Belloti J.C. Minimally invasive osteosynthesis with a Bridge plate versus a functional Brace for humeral shaft fractures: a randomized controlled trial. J Bone Joint Surg Am. 2017;99:583–592. doi: 10.2106/JBJS.16.00628. [DOI] [PubMed] [Google Scholar]
- 13.McCormack R.G., Brien D., Buckley R.E., McKee M.D., Powell J., Schemitsch E.H. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomized trial. J Bone Joint Surg Br. 2000;82:336–339. doi: 10.1302/0301-620x.82b3.9675. [DOI] [PubMed] [Google Scholar]
- 14.Muller M.E., Perren S.M., Allg€ower M. 3rd ed. Springer-Verlag; Berlin: 1995. Manual of internal fixation: Techniques recommended by the AO-ASIF group. [Google Scholar]
- 15.Patino J.M. Treatment of humeral shaft fractures using antegrade nailing: functional outcome in the shoulder. J Shoulder Elbow Surg. 2015;24:1302–1306. doi: 10.1016/j.jse.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 16.Raghavendra S., Bhalodiya H.P. Internal fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail: a prospective study. Indian J Orthop. 2007;41:214–218. doi: 10.4103/0019-5413.33685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rodríguez-Merchán E.C. Compression plating versus hackethal nailing in closed humeral shaft fractures failing nonoperative reduction. J Orthop Trauma. 1995;9:194–197. doi: 10.1097/00005131-199506000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Rommens P.M., Kuechle R., Bord T., Lewens T., Engelmann R., Blum J. Humeral nailing revisited. Injury. 2008;39:1319–1328. doi: 10.1016/j.injury.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 19.Verdano M.A., Pellegrini A., Schiavi P., Somenzi L., Concari G., Ceccarelli F. Humeral shaft fractures treated with antegrade intramedullary nailing: what are the consequences for the rotator cuff? Int Orthop. 2013;37:2001–2007. doi: 10.1007/s00264-013-2007-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang X., Chen Z., Shao Y., Ma Y., Fu D., Xia Q. A meta-analysis of plate fixation versus intramedullary nailing for humeral shaft fractures. J Orthop Sci. 2013;18:388–397. doi: 10.1007/s00776-013-0355-8. [DOI] [PubMed] [Google Scholar]
- 21.Wen H., Zhu S., Li C., Chen Z., Yang H., Xu Y. Antegrade intramedullary nail versus plate fixation in the treatment of humeral shaft fractures: an update meta-analysis. Medicine (Baltimore) 2019;98:e17952. doi: 10.1097/MD.0000000000017952. [DOI] [PMC free article] [PubMed] [Google Scholar]