Abstract
Background
The irreparability of rotator cuff repair is generally determined during surgery. We have been performing partial repairs for rotator cuff tears that are deemed irreparable with primary repair. The aim of this study is to report, for the first time, the long-term postoperative outcome of our partial repair method and to clarify the criteria for the irreparability of primary repair.
Methods
The UCLA score, radiographic findings, and magnetic resonance imaging findings of 156 shoulders that underwent rotator cuff repair (primary repair, 126 shoulders; partial repair, 30 shoulders) were retrospectively evaluated at preoperative and >10-year postoperative follow-up (mean evaluation time, 11.5 ± 1.0 years). Osteoarthritic (OA) changes were evaluated by radiographic findings, and the cuff integrity (Sugaya classification) and fatty infiltration (Goutallier classification) were evaluated by magnetic resonance imaging findings. These evaluations were compared between a primary repair group and partial repair group.
Results
Although no significant difference was observed between preoperative and postoperative findings for the UCLA score, the strength of forward flexion was significantly lower at 10 years postoperatively in the partial repair group. Preoperative image evaluation showed no significant difference in OA changes between the 2 groups; however, fatty infiltration showed significantly greater progression in the partial repair group than the primary repair group. At >10-year postoperative follow-up, the OA changes, cuff integrity, and fatty infiltration showed significantly greater progression in the partial repair group compared to the primary repair group. Although the long-term outcome of the partial repair group was inferior to that of the primary repair group in imaging evaluations, good functional outcome of the shoulder joint was maintained.
Conclusion
Our results suggested that partial repair could be an effective treatment option for irreparable rotator cuff tear. In terms of the feasibility of primary repair, the cutoff value for preoperative fatty infiltration was stage 2; thus, we believe that primary repair should be performed for cases with stage 2 fatty infiltration or lower, and partial repair should be performed for cases with stage 3 fatty infiltration or higher. However, manual workers and athletes with stage 3 fatty infiltration or higher should be advised in advance that mild muscle weakness may remain after surgery.
Keywords: Massive Rotator cuff tear, Irreparable Rotator cuff tear, Partial repair, Osteoarthritis, Cuff integrity, Fatty infiltration
Rotator cuff tear is a common disorder that causes chronic pain and decreased function of the shoulder, and the effectiveness of surgical treatment for rotator cuff tears is widely accepted and well established. In recent years, clinical outcomes with >10-year postoperative follow-up after rotator cuff repair have been reported, and some have reported that 80% to 91% of cases exhibited good or excellent results.1,7,14 The prospect of maintaining a long-term effect of the surgery is an important issue for consideration and provides useful information for the practicing surgeon.
The size of the tear is known to greatly affect the postoperative outcome of surgical treatment,16 and some cases are not only affected in terms of clinical results but also involve difficulties in performing primary repairs. Warner et al30 defined cases that are believed to be irreparable with primary repair as “the inability to achieve a direct repair of the native tendon to the humerus despite mobilizing the soft tissues,” wherein up to 30% of rotator cuff tears were considered difficult to achieve primary repair due to massive tears or severe contractures. Moreover, Chung et al6 also reported a failure rate of approximately 40% for those with tear sizes over 5 cm or with 2 or more tendon tears. Conservative therapy, partial repair, tendon transfer, and more recently reverse total shoulder arthroplasty are performed for massive tears that are considered difficult to repair; however, there is no consensus on how to determine the feasibility of primary repair based on preoperative findings. Goutallier et al used CT scans to assess the degree of fatty degeneration for rotator cuff muscles in a spectrum of 5 stages, ranging from Stage 0 to Stage 415. This classification is commonly used, and stages 3 and 4 are generally considered irreparable; however, there are reports of good short-term clinical outcomes after surgery3 and questions remain on the effectiveness of the evaluation method. We have been performing partial repairs using the mini-open deltoid splitting approach for cases that are deemed irreparable with primary repair. Partial repair was originally introduced by Burkhart et al in 1993 as a treatment option for irreparable rotator cuff tears based on a “suspension bridge" analogy.4,5
The aim of this study is to report, for the first time, the long-term postoperative outcome of partial repairs for massive rotator cuff tears, and to clarify the imaging-based criteria for determining the feasibility of primary repair. Therefore, we investigated the long-term postoperative outcomes of partial repairs, and we then compared their clinical outcomes and imaging findings with those who were able to undergo primary repair. We believe that the results of this study will enable a more accurate treatment protocol for massive rotator cuff tears based on preoperative imaging findings and will also lead to further improvement in postoperative results.
Materials and methods
Study population
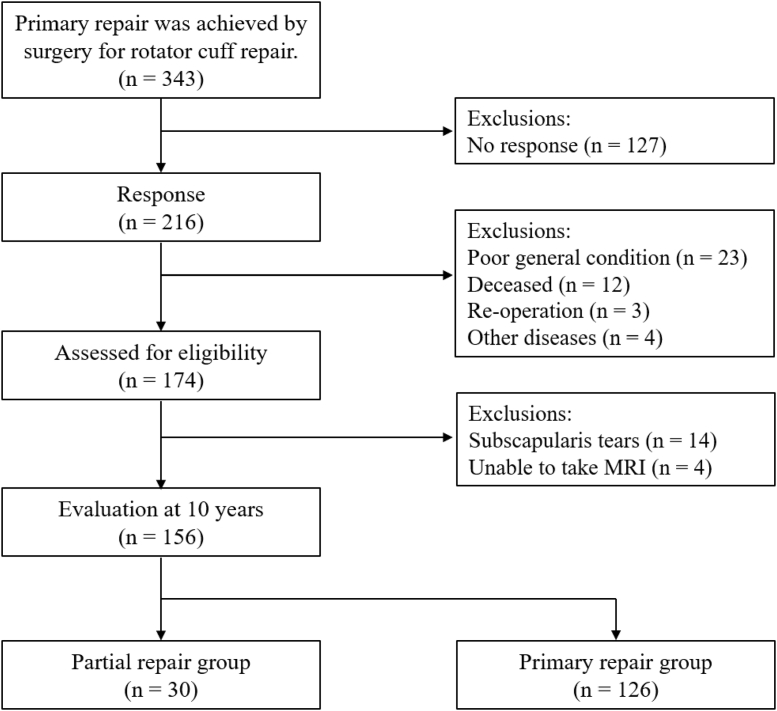
From March 1998 to May 2006, 343 shoulders in 339 patients underwent primary rotator cuff repair at our institution (Fig. 1). The mean age at surgery was 60.6 years (SD ± 9.0 years). All patients with >10-year postoperative follow-up after rotator cuff repair were requested by mail to schedule a follow-up visit. Responses to the letter were received for 216 shoulders, and no response was received for the remaining 127 shoulders. The following patients were excluded from this study: poor general condition (23 shoulders), deceased patients (12 shoulders; responses were provided by family members), and patients who underwent reoperation within the previous 10 years (3 shoulders), patients who developed shoulder disorder due to cerebral infarction or trauma (4 shoulders). We were able to investigate 174 shoulders in 170 patients. Subscapularis tears that required sutures to the lesser tuberosity were found in 14 shoulders from the records of intraoperative findings, and these cases were excluded. One hundred sixty shoulders in 157 patients were able to attend a follow-up evaluation. Of these 160 shoulders, 156 shoulders were included in this study after excluding 4 shoulders for those unable to undergo magnetic resonance imaging (MRI) (claustrophobia, 2 shoulders; after implanted pacemaker, 2 shoulders). The mean age at surgery was 60.7 years (SD ± 7.3 years). The mean follow-up period was 11.5 years (SD ± 1.0 year). Eighty-five shoulders were male and 71 shoulders were female, of which 103 were right shoulders and 53 were left shoulders. Tear sizes based on preoperative MRI were assessed based on the DeOrio and Cofield classification system, and the results were as follows: 28 small tears (<1 cm in length), 94 medium tears (1-3 cm), 15 large tears (3-5cm), and 19 massive tears (>5 cm).
Figure 1.
Flow diagram of the study recruitment process.
All surgical procedures were performed by the same orthopedic shoulder surgeon (Y.H.). Our surgical indications were patients with no underlying disease and those who wished to undergo surgery after appropriate informed consent. We aimed to perform suture repair to the greater tuberosity footprint in all cases during surgery and to suture more proximally in cases where it is impossible. In all cases, the tendon stump was sutured into the bone groove, regardless of where it was sutured. The rotator cuff was classified into 126 shoulders with coverage of the greater tuberosity footprint in the primary repair group (male, 68 shoulders; female, 60 shoulders; mean age at surgery, 60.7 ± 7.3 years) and 30 shoulders with coverage proximal to the footprint in the partial repair group (male, 18 shoulders; female, 12 shoulders; mean age at surgery, 60.8 ± 6.8 years) based on intraoperative findings. There were no significant differences in demographics between the 2 groups (age: P = .94, gender: P = .50).
The research protocol of this retrospective study was approved by the Ethics Committee of the North Alps Medical Center Azumi Hospital (reference number: 774), and informed consent was obtained for all patients.
Surgical procedure and postoperative rehabilitation
All surgical procedures were performed using the mini-open deltoid splitting approach.17 A 3-cm skin incision was made from the midpoint of the anterior margin of the acromion toward the axilla, and the anterior deltoid muscle was split in the direction of the fiber. The degenerated coracoacromial ligament was resected and acromioplasty was performed according to Neer.24 The degenerated rotator cuff tendon was resected, and musclotendinous units were sufficiently mobilized to extract the stump. The suture site was positioned at 0° shoulder abduction without inducing excessive tension on the repaired rotator cuff. A bony groove was constructed at the greater tuberosity footprint for cases without excessive tension on the stump (primary repair group) and at the footprint proximal to the chondral surface of the humeral head for cases with severe tension (partial repair group), and transosseous sutures were used for the repair.
There were some differences in protocols that were implemented for postoperative therapy in the primary and partial repair groups. In the primary repair group, the affected limb was fixed at 70° abduction and 30° horizontal flexion using an abduction pillow at 2 weeks postoperatively. The fixation of the affected limb was completed at 3 weeks postoperatively. In the partial repair group, at the affected limb was fixed at 90° abduction and 30° horizontal flexion using a shoulder abduction orthosis, and the abduction angle was then gradually decreased. The fixation of the affected limb was completed at 4 weeks postoperatively. Both groups underwent physical therapy with active flexion and extension exercises of the elbow joint, relaxation of the shoulder muscles, and passive range of motion training of the shoulder joint in all directions on the day after the operation. Active range of motion training was performed after fixation with an orthosis. Muscle strengthening training for the extrinsic muscles was initiated at 2 to 3 months postoperatively, and light work was allowed. Engagement in heavy physical labor and sports were allowed without restriction at 6 months postoperatively.
Clinical evaluation
Clinical evaluations were conducted by the same evaluator (N.I.) both preoperatively and at >10-year postoperative follow-up. The University of California Los Angeles (UCLA) shoulder score was used for evaluations.11 The preoperative and 10-year postoperative total UCLA score was compared between the primary repair group and partial repair group.
Evaluation using image findings
Imaging findings of the shoulder were obtained by radiography and MRI, and these were taken preoperatively and during re-examination at >10 years postoperatively.
Radiographs were taken in anterior-posterior projection with the shoulder positioned in external rotation, internal rotation, and elevation. The degree of OA changes were evaluated by radiographs using the Samilson and Prieto classification system, comprised the following 4 categories: 0 = normal, 1 = mild (osteophytes < 3 mm on the humeral head), 2 = moderate (osteophytes between 3 mm and 7 mm on the humeral head or the glenoid rim), and 3 = severe (osteophytes >7 mm with or without articular incongruity).26
A GP Flex Coil with a 1.0-Tunit (Signa Horizon Lx1.0 T; GE Healthcare, Waukesha, WI, USA) was used in the same setting for MRI. Spin echo proton-weighted sequences (repetition time: 3000 ms, echo time: 7.4 ms, matrix: 256×192), spin echo T2-weighted sequences (repetition time: 3000 ms, echo time: 90 ms, matrix: 256×192), and gradient echo T2∗-weighted sequences (repetition time: 440 ms, echo time: 20 ms, flip angle: 30°) were used to obtain the MRI findings for each patient with a 4-mm slice thickness and 1-mm interslice gap.
Cuff integrity was evaluated according to the Sugaya classification27 and categorized into the following types: type I, repaired cuff appears to have sufficient thickness compared to normal cuff with homogenously low intensity on each image; type II, sufficient thickness compared with normal cuff associated with partial high intensity area; type III, insufficient thickness with less than half the thickness when compared with normal cuff, but without discontinuity; type IV, presence of a minor discontinuity in only one or two slices on both oblique coronal and sagittal images; type V, major discontinuity in more than 2 slices on both oblique coronal and sagittal images.
The evaluation of fatty infiltration in the rotator cuff muscle was performed by MRI according to the method described by Goutallier et al.12 The rotator cuff muscle that was evaluated was the supraspinatus muscle belly.
All imaging findings were evaluated by a shoulder surgeon (T.M.) with over 10 years of experience who was uninformed of the clinical evaluation for each patient. Cuff integrity was evaluated on MRI findings during re-examination at 10 years postoperatively, and the degree of OA was evaluated on radiographic findings and fatty infiltration on MRI findings during re-examination at >10 years postoperatively. These findings were compared between the primary and partial repair groups.
Statistical analysis
We calculated the sample size using G∗ power 3.1 software (Heinrich Heine University, Duesseldorf, Germany), and the results showed that 52 subjects (26 subjects each) were required for our study (effect size = 0.8, α = 0.05, power = 0.8). The Shapiro-Wilk test was used to verify normality of distributions. The paired or unpaired t test was used to compare the UCLA score. Categorical variables (degree of OA, cuff integrity, and fatty infiltration) were compared using χ2 tests. ROC analysis was performed to determine the preoperative fatty infiltration and feasibility of primary repair, for which a cutoff value was selected to evaluate the sensitivity, specificity, and odds ratio at 95% CI. The cutoff value was defined as the sum of the highest sensitivity and specificity values. SPSS version 16 software (IBM, Armonk, NY, USA) was used for statistical analysis with a significance level set to less than 1%.
Results
Clinical evaluation
Comparing the preoperative and 10-year postoperative UCLA scores, both groups showed significant improvement after surgery (Table I). In a comparison of each item, all items except active forward flexion were significantly improved at 10-year postoperatively (P < .001).
Table I.
Comparison of UCLA scores between 2 groups.
| UCLA score | Primary repair (n = 126) | Partial repair (n = 30) | P value |
|---|---|---|---|
| Preoperative | |||
| Total score | 21.0 ± 3.59 | 20.1 ± 3.57 | .18 |
| Pain | 4.68 ± 2.26 | 4.26 ± 2.50 | .38 |
| Function | 7.49 ± 1.57 | 7.23 ± 1.69 | .42 |
| Active forward flexion | 4.57 ± 0.69 | 4.45 ± 0.77 | .41 |
| Length of forward flexion | 4.32 ± 0.66 | 3.97 ± 0.75 | .02 |
| 10 years postoperative | |||
| Total score | 32.7 ± 3.11 | 31.9 ± 3.35 | .22 |
| Pain | 9.05 ± 1.67 | 9.27 ± 1.31 | .48 |
| Function | 9.64 ± 0.98 | 9.15 ± 1.42 | .06 |
| Active forward flexion | 4.73 ± 0.45 | 4.55 ± 0.94 | .11 |
| Length of forward flexion | 4.88 ± 0.45 | 4.58 ± 0.83 | .007 |
| Satisfaction of patient | 4.38 ± 0.73 | 4.34 ± 0.71 | .81 |
The preoperative UCLA score was 21.1 points (SD ± 3.6 points) in the primary repair group and 20.0 points (SD ± 3.6 points) in the partial repair group. There was no significant difference between the 2 groups in terms of the total UCLA score and UCLA score for each item (Table II).
Table II.
Comparison of UCLA scores before and after surgery.
| UCLA score | Preoperative | 10 years postoperative | P value |
|---|---|---|---|
| Primary repair (n = 126) | |||
| Total score | 21.0 ± 3.59 | 32.7 ± 3.11 | <.001 |
| Pain | 4.68 ± 2.26 | 9.05 ± 1.67 | <.001 |
| Function | 7.49 ± 1.57 | 9.64 ± 0.98 | <.001 |
| Active forward flexion | 4.57 ± 0.69 | 4.73 ± 0.45 | .03 |
| Length of forward flexion | 4.32 ± 0.66 | 4.88 ± 0.45 | <.001 |
| Partial repair (n = 30) | |||
| Total score | 20.1 ± 3.57 | 31.9 ± 3.35 | <.001 |
| Pain | 4.26 ± 2.50 | 9.27 ± 1.31 | <.001 |
| Function | 7.23 ± 1.69 | 9.15 ± 1.42 | <.001 |
| Active forward flexion | 4.45 ± 0.77 | 4.55 ± 0.94 | .65 |
| Length of forward flexion | 3.97 ± 0.75 | 4.58 ± 0.83 | <.001 |
At >10-year postoperative follow-up, the UCLA score was 32.7 points (SD ± 3.1 points) in the primary repair group and 31.8 points (SD ± 3.4 points) in the partial repair group, showing no significant difference between the 2 groups. In a comparison of each item, the strength of forward flexion item was significantly lower in the partial repair group (P < .001).
Evaluation using radiographs
There was no significant difference in the degree of preoperative OA between the primary and partial repair groups. During re-examination at >10 years postoperatively, significantly more OA progression was observed in the partial repair group than in the primary repair group (P < .001) (Table III). In both groups, no severe stage 3 OA was observed preoperatively or at >10 years postoperatively.
Table III.
Comparison of radiographic osteoarthritis classification.
| Osteoarthritis staging (Samilson and Prieto classification) | Primary repair (n) | Partial repair (n) | P value |
|---|---|---|---|
| Preoperative | .069 | ||
| Stage 0 | 75 | 14 | |
| Stage 1 | 50 | 14 | |
| Stage 2 | 1 | 2 | |
| Stage 3 | 0 | 0 | |
| 10 years postoperative | <.001 | ||
| Stage 0 | 29 | 1 | |
| Stage 1 | 72 | 14 | |
| Stage 2 | 25 | 15 | |
| Stage 3 | 0 | 0 |
MRI findings: evaluation of cuff integrity
The cuff integrity during re-examination at >10 years postoperatively was of poor quality, with significantly more cases classified as type IV and V in the partial repair group than in the primary repair group (P < .001) (Table IV). Cases classified as type IV and V suspected of re-tear were 37 (29%) in the primary repair group and 21 (70%) in the partial repair group. In the partial repair group, there were almost no cases classified as type I and II.
Table IV.
Comparison of the cuff integrity on MRI at 10 years postoperatively.
| Cuff integrity (Sugaya classification) | Primary repair (n) | Partial repair (n) | P value |
|---|---|---|---|
| Pre-operative | |||
| Type I | 35 | 2 | <.001 |
| Type II | 22 | 0 | |
| Type III | 32 | 7 | |
| Type IV | 12 | 8 | |
| Type V | 25 | 13 |
MRI findings: evaluation of fatty infiltration
The degree of fatty infiltration of the supraspinatus muscle was significantly more severe in the partial repair group than the primary repair group before surgery (P < .001). The results of ROC analysis are as follows: cutoff value, stage 2; area under the curve, 0.694; sensitivity, 0.864; specificity, 0.442; odds ratio, 5.00 (95% CI 0.585-0.803); P value < .001 (Fig. 2). The percentage of stage 3 fatty infiltration or higher prior to surgery was 12% in the primary repair group and 33% in the partial repair group. The percentage of stage 3 fatty infiltration or higher was 44% in the primary repair group and 90% in the partial repair group during re-evaluation at >10 years postoperatively. There were many cases in which the latter was significantly more severe than the former (P < .001) (Table V).
Figure 2.
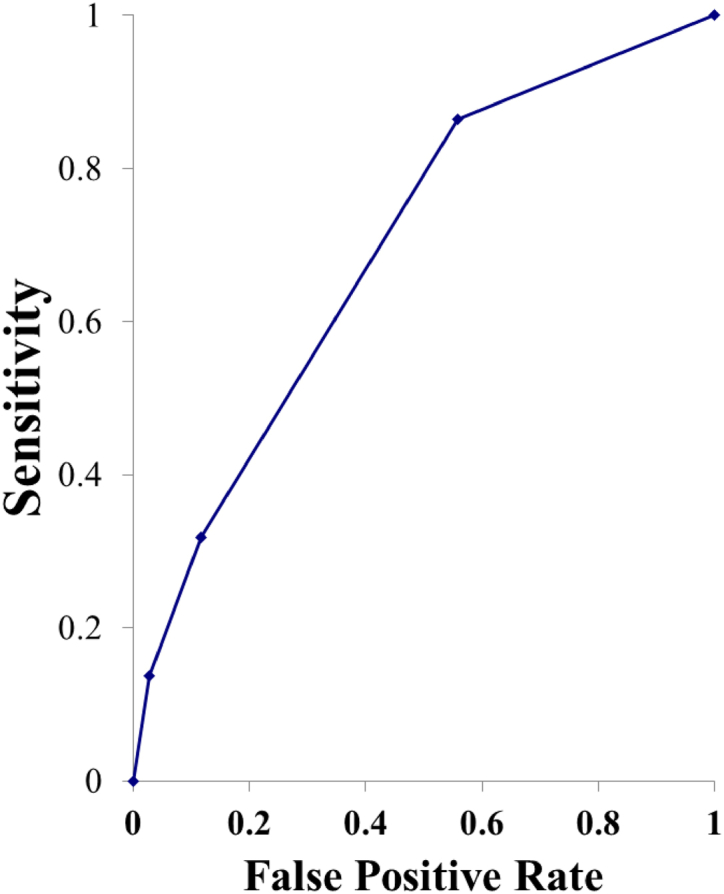
Receiver operating characteristic (ROC) curve of preoperative fatty infiltration.
Table V.
Comparison of fatty infiltration on MRI.
| Fatty infiltration of supraspinatus muscle belly (Goutallier classification) | Primary repair (n) | Partial repair (n) | P value |
|---|---|---|---|
| Preoperative | |||
| Stage 0 | 0 | 0 | <.001 |
| Stage 1 | 57 | 4 | |
| Stage 2 | 54 | 19 | |
| Stage 3 | 14 | 1 | |
| Stage 4 | 1 | 6 | |
| 10 years postoperative | |||
| Stage 0 | 0 | 0 | <.001 |
| Stage 1 | 19 | 1 | |
| Stage 2 | 51 | 2 | |
| Stage 3 | 33 | 14 | |
| Stage 4 | 23 | 13 |
Complications
No intraoperative or postoperative complications were observed in either group. In addition, no cases of infection or contracture were observed after surgery that required joint mobilization.
Discussion
Surgical treatment is commonly practiced for rotator cuff tears that are refractory to conservative treatment, and some reports show good or superior results at >10 years postoperatively.1,7,14 In recent years, long-term results of massive rotator cuff tears have also been reported, demonstrating that clinically satisfactory results have been maintained.9,25,31 However, in these reports, the rotator cuff was anatomically repaired by surgery even for massive tears, and primary repair may have been feasible. Thus, the long-term postoperative outcome for a “true irreparable rotator cuff tear” remains unknown.
Partial repairs have been reported by various authors to improve postoperative shoulder function.13,20 Although Galasso et al13 reported good results at 7 years postoperatively, others have only reported short-term outcomes. To the best of our knowledge, there are no reports on the long-term outcomes of partial repairs with over 10 years of follow-up. We believe this study is the first to report the long-term outcomes of partial repairs with >10-year postoperative follow-up. Moreover, there was no significant difference between the primary and partial repair groups when comparing the UCLA score at >10 years postoperatively. Iagulli et al reported similar results at 2 years postoperative follow-up18 and suggested that shoulder joint function could be maintained even in the long-term postoperative period.
In terms of OA changes following rotator cuff repair, we previously reported that the shoulder showed OA progression on the operative side at 11.1 years postoperatively.22 However, since the non-operative side also showed OA progression, we considered that aging may also have an effect on OA changes. Although the 2 groups showed no significant difference preoperatively, both the partial and primary repair groups showed significantly greater OA progression at >10 years postoperatively. This result suggested that since there was no difference in clinical outcomes, OA progression could potentially be suppressed by performing primary repair, even if its effect on shoulder joint function remains unknown.
Cuff integrity has been gaining attention as a method of evaluation for re-tear cases in recent years. In this study, the percentage of type IV and V that indicates a re-tear was 29% in the primary repair group and 70% in the partial repair group. There are many reports on long-term postoperative re-tears in the literature with varying incidence rates, including that of massive tears (38-94%).9,29,31 Berth et al reported a re-tear rate of 52% after partial repair at 7 years postoperatively, and our results at >10 years postoperatively showed an even higher incidence of 70%. We found that the cuff integrity of the partial repair group was considerably inferior to that of the primary repair group at >10 years postoperatively.
Regarding the fatty infiltration of the supraspinatus muscle, Collin et al reported that fatty infiltration showed progression at 10 years postoperatively in tears of the supraspinatus muscle belly alone.10 Moreover, another study by Collin et al reported that 42% of cases demonstrated progression of fatty infiltration in the supraspinatus at 20 years after massive tears.8 In a previous study, we reported that no progression of fatty infiltration was observed in the supraspinatus for small and medium-sized tears at >10 years postoperatively.23 In this study, significantly more severe cases were observed in the partial repair group both preoperatively and postoperatively, and the percentage of stage 3 fatty infiltration of or higher was 44% in the primary repair group and 90% in the partial repair group during re-examination at >10 years postoperatively. This result suggests a postoperative progression of fatty infiltration in rotator cuff repair cases that could potentially progress further in the partial repair group compared to the primary repair group.
There are 2 notable points in this study. The first is that clinical results were good despite the severe cuff integrity and fat infiltration of the supraspinatus muscle in the partial repair group at 10 years postoperatively. Burkhart et al reported the importance of reconstructing the transverse force couple2 and suspension bridge system4,5 for “irreparable rotator cuff tears.” In order to achieve these 2 methods of reconstruction, we have performed cuff repairs using the transosseous suture technique. Therefore, even if the cuff integrity and fat infiltration of the supraspinatus muscle deteriorated at >10 years postoperatively, we suspect that the function of the shoulder joint would be maintained for a long period of time. On the other hand, this study also clarified that several points should be noted on partial repair, which shows long-term effectiveness for “irreparable rotator cuff tears.” In examining each item of the UCLA score in detail, there is no significant difference in most of the items preoperatively and >10 years postoperatively; however, the strength of forward flexion was significantly lower in the partial repair group during re-examination at >10 years postoperatively. For this reason, surgical procedures should be carefully selected for some manual workers and athletes, but partial repairs provide good shoulder function for the majority of patients.
The second notable point is that the ROC analysis showed the cutoff value for preoperative fatty infiltration was stage 2 regarding the feasibility of primary repair. Although the cuff integrity at >10 years postoperatively was distributed in all stages in the primary repair group, there were almost no type 1 and 2 cases in the partial repair group. Moreover, most cases exhibiting fatty infiltration of the supraspinatus muscle in the partial repair group were stage 3 or higher at >10 years postoperatively. These results indicate that if the fatty infiltration is stage 3 or higher before the operation, the primary repair becomes difficult. Furthermore, even the long-term results of the imaging findings can become poor, and the stage 2 fatty infiltration indicates the boundary for predicting primary repair. In terms of the feasibility of primary repair, recent reports have suggested predictive factors such as chronic pseudoparalysis, tear size, acromiohumeral distance, tangent sign, fatty infiltration of the supraspinatus, and tendon involvement.19,21,28 Although these reports mention the feasibility of primary repair, they do not mention the long-term postoperative outcomes. Our results show that it is possible to preoperatively examine the surgical procedure by predicting the feasibility of primary repair. In the future, we will perform primary repair for cases with stage 2 fatty infiltration or lower and partial repairs for cases with stage 3 fatty infiltration or higher. However, we believe that manual workers and athletes with stage 3 fatty infiltration or higher should be advised in advance that mild muscle weakness may remain after surgery.
There are several limitations to this study. First, this study was conducted by a single institution with a small patient sample size. In this study, surgical outcomes of procedures conducted by the same operator were investigated to ensure consistency in the feasibility of primary repair. Future studies may benefit from a multicenter study with a larger sample size. Second, the study does not show early postoperative outcomes for patients who underwent surgery. Although the importance of maintaining long-term postoperative function was considered in this study, it may be necessary to examine short-term postoperative results. Thirdly, we used the Samilson and Prieto classification for the evaluation of OA changes, and we did not use the Hamada classification that is specific to cuff tear arthropathy. Since there were no cases with severe OA that were observed in this study, the Samilson and Prieto classification was used in order to detect more sensitive changes. Fourth, although we believe that the use of multiple scoring systems such as the Constant score and ASES score is ideal for assessing the shoulder function score, we were only able to perform an assessment using the UCLA score. The UCLA score was used in order to compare scores with evaluations that were performed 10 years ago. Fifth, our cases used an abduction pillow after surgery. Currently, there are various opinions on the use of abduction pillows, and the effects of their use warrant further investigation for future studies. Finally, our study did not compare partial repair with other procedures in cases of irreparable rotator cuff tears. We believe we have shown the effectiveness of partial repair, but a comparison with other procedures should be conducted in the future.
Conclusions
In this study, we reported the long-term outcome of partial repair for irreparable rotator cuff tears for the first time. The >10-year postoperative outcome of those who underwent partial repair was inferior to those who underwent primary repair in terms of OA changes, cuff integrity, and fat infiltration; however, good function of the shoulder joint was maintained. From this result, partial repairs could be considered an effective treatment option for irreparable rotator cuff tears. In addition, we believe that the stage 2 fatty infiltration of the infraspinatus prior to surgery is a boundary that determines whether a primary repair for massive rotator cuff tear is feasible. In the future, we plan to perform primary repairs for cases with stage 2 fatty infiltration or lower, and partial repair for cases with stage 3 fatty infiltration or higher. Therefore, for cases with stage 3 fatty infiltration or higher, it is necessary to predict the possibility of those that can achieve only a partial repair.
Disclaimers:
Funding: No funding was disclosed by the author(s).
Conflicts of interest: The authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
This study was approved by the Institutional Review Board of Azumi General Hospital Ethics Committee (study number: 774). This committee consists of the following members: Chairperson and Assistant Director, Shigeo Kawachi; Director of Psychiatry, Hisashi Kitou; Secretary General, Kazuhiko Nishijou; Chief Pharmacist, Shigeru Yokoyama; Director of Nursing Service Department, Yasuko Oota; External Committee, Kiyotoshi Maruyama; External Committee, Masahiko Takizawa.
Footnotes
This study was approved by the Institutional Review Board of Azumi General Hospital Ethics Committee (study number: 774).
References
- 1.Adamson G., Tibone J.E. Ten-year assessment of primary rotator cuff repairs. J Shoulder Elbow Surg. 1993;2:57–63. doi: 10.1016/1058-2746(93)90001-W. [DOI] [PubMed] [Google Scholar]
- 2.Burkhart S.S. Arthroscopic treatment of massive rotator cuff tears. Clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991;267:45–56. [PubMed] [Google Scholar]
- 3.Burkhart S.S., Barth J.R., Richards D.P., Zlatkin M.B., Larsen M. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy. 2007;23:347–354. doi: 10.1016/j.arthro.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 4.Burkhart S.S., Esch J.C., Jolson R.S. The rotator crescent and rotator cable: an anatomic description of the shoulder's "suspension bridge". Arthroscopy. 1993;9:611–616. doi: 10.1016/s0749-8063(05)80496-7. [DOI] [PubMed] [Google Scholar]
- 5.Burkhart S.S., Nottage W.M., Ogilvie-Harris D.J., Kohn H.S., Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994;10:363–370. doi: 10.1016/s0749-8063(05)80186-0. [DOI] [PubMed] [Google Scholar]
- 6.Chung S.W., Kim J.Y., Kim M.H., Kim S.H., Oh J.H. Arthroscopic repair of massive rotator cuff tears: outcome and analysis of factors associated with healing failure or poor postoperative function. Am J Sports Med. 2013;41:1674–1683. doi: 10.1177/0363546513485719. [DOI] [PubMed] [Google Scholar]
- 7.Cofield R.H., Parvizi J., Hoffmeyer P.J., Lanzer W.L., Ilstrup D.M., Rowland C.M. Surgical repair of chronic rotator cuff tears: a prospective long-term study. J Bone Joint Surg Am. 2001;83:71–77. doi: 10.2106/00004623-200101000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Collin P., Betz M., Herve A., Walch G., Mansat P., Favard L. Clinical and structural outcome 20 years after repair of massive rotator cuff tears. J Shoulder Elbow Surg. 2020;29:521–526. doi: 10.1016/j.jse.2019.07.031. [DOI] [PubMed] [Google Scholar]
- 9.Collin P., Colmar M., Thomazeau H., Mansat P., Boileau P., Valenti P. Clinical and MRI Outcomes 10 Years After Repair of Massive Posterosuperior Rotator Cuff Tears. J Bone Joint Surg Am. 2018;100:1854–1863. doi: 10.2106/JBJS.17.01190. [DOI] [PubMed] [Google Scholar]
- 10.Collin P., Kempf J.F., Molé D., Meyer N., Agout C., Saffarini M. Ten-year multicenter clinical and MRI evaluation of isolated supraspinatus repairs. J Bone Joint Surg Am. 2017;99:1355–1364. doi: 10.2106/JBJS.16.01267. [DOI] [PubMed] [Google Scholar]
- 11.Ellman H., Hanker G., Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68:1136–1144. [PubMed] [Google Scholar]
- 12.Fuchs B., Weishaupt D., Zanetti M., Hodler J., Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8:599–605. doi: 10.1016/s1058-2746(99)90097-6. [DOI] [PubMed] [Google Scholar]
- 13.Galasso O., Riccelli D.A., De Gori M., De Benedetto M., Orlando N., Gasparini G. Quality of life and functional results of arthroscopic partial repair of irreparable rotator cuff tears. Arthroscopy. 2017;33:261–268. doi: 10.1016/j.arthro.2016.06.024. [DOI] [PubMed] [Google Scholar]
- 14.Galatz L.M., Griggs S., Cameron B.D., Iannotti J.P. Prospective longitudinal analysis of postoperative shoulder function: a ten year follow-up study of full-thickness rotator cuff tears. J Bone Joint Surg Am. 2001;83:1052–1056. [PubMed] [Google Scholar]
- 15.Goutallier D., Postel J.M., Bernageau J., Lavau L., Voisin M.C. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. [PubMed] [Google Scholar]
- 16.Harryman D.T., 2nd, Mack L.A., Wang K.Y., Jackins S.E., Richardson M.L., Matsen F.A., 3rd Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73:982–989. [PubMed] [Google Scholar]
- 17.Hata Y., Saitoh S., Murakami N., Seki H., Nakatsuchi Y., Takaoka K. A less invasive surgery for rotator cuff tear: mini-open repair. J Shoulder Elbow Surg. 2001;10:11–16. doi: 10.1067/mse.2001.110514. [DOI] [PubMed] [Google Scholar]
- 18.Iagulli N.D., Field L.D., Hobgood E.R., Ramsey J.R., Savoie F.H., 3rd Comparison of partial versus complete arthroscopic repair of massive rotator cuff tears. Am J Sports Med. 2012;40:1022–1026. doi: 10.1177/0363546512438763. [DOI] [PubMed] [Google Scholar]
- 19.Kim I.B., Jung D.W., Suh K.T. Prediction of the Irreparability of Rotator Cuff Tears. Arthroscopy. 2018;34:2076–2084. doi: 10.1016/j.arthro.2018.02.033. [DOI] [PubMed] [Google Scholar]
- 20.Kim S.J., Lee I.S., Kim S.H., Lee W.Y., Chun Y.M. Arthroscopic partial repair of irreparable large to massive rotator cuff tears. Arthroscopy. 2012;28:761–768. doi: 10.1016/j.arthro.2011.11.018. [DOI] [PubMed] [Google Scholar]
- 21.Kissenberth M.J., Rulewicz G.J., Hamilton S.C., Bruch H.E., Hawkins R.J. A positive tangent sign predicts the repairability of rotator cuff tears. J Shoulder Elbow Surg. 2014;23:1023–1027. doi: 10.1016/j.jse.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 22.Matsuba T., Hata Y., Ishigaki N., Nakamura K., Kato H. Osteoarthritis progression of the shoulder: a long-term follow-up after mini-open rotator cuff repair. J Orthop Surg (Hong Kong) 2018;26 doi: 10.1177/2309499018768106. 2309499018768106. [DOI] [PubMed] [Google Scholar]
- 23.Matsuba T., Hata Y., Ishigaki N., Nakamura K., Murakami N., Kobayashi H. Long-term clinical and imaging outcomes after primary repair of small- to medium-sized rotator cuff tears. J Orthop Surg (Hong Kong) 2019;27 doi: 10.1177/2309499019883985. 2309499019883985. [DOI] [PubMed] [Google Scholar]
- 24.Neer C.S., 2nd Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. 1972;54:41–50. [PubMed] [Google Scholar]
- 25.Paxton E.S., Teefey S.A., Dahiya N., Keener J.D., Yamaguchi K., Galatz L.M. Clinical and radiographic outcomes of failed repairs of large or massive rotator cuff tears: minimum ten-year follow-up. J Bone Joint Surg Am. 2013;95:627–632. doi: 10.2106/JBJS.L.00255. [DOI] [PubMed] [Google Scholar]
- 26.Samilson R.L., Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65:456–460. [PubMed] [Google Scholar]
- 27.Sugaya H., Maeda K., Matsuki K., Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21:1307–1316. doi: 10.1016/j.arthro.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 28.Sugihara T., Nakagawa T., Tsuchiya M., Ishizuki M. Prediction of primary reparability of massive tears of the rotator cuff on preoperative magnetic resonance imaging. J Shoulder Elbow Surg. 2003;12:222–225. doi: 10.1016/s1058-2746(02)86888-4. [DOI] [PubMed] [Google Scholar]
- 29.Vastamäki M., Lohman M., Borgmästars N. Rotator cuff integrity correlates with clinical and functional results at a minimum 16 years after open repair. Clin Orthop Relat Res. 2013;471:554–561. doi: 10.1007/s11999-012-2494-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Warner J.J. Management of massive irreparable rotator cuff tears: the role of tendon transfer. Instr Course Lect. 2001;50:63–71. [PubMed] [Google Scholar]
- 31.Zumstein M.A., Jost B., Hempel J., Hodler J., Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2008;90:2423–2431. doi: 10.2106/JBJS.G.00677. [DOI] [PubMed] [Google Scholar]