Abstract
Background
Reverse shoulder arthroplasty is becoming an increasingly common surgical procedure in Hong Kong, as well as in many other countries worldwide. The aim of this study is to describe the glenoid anatomy in the Southern Chinese population. We are interested to know whether commercially available glenoid implants are suitable for this population and whether there are any steps or precautions we can take during surgery to optimize the clinical outcome for these patients.
Method
A total of 244 shoulders of Southern Chinese patients were analyzed using 2-dimensional computed tomography, formatted to align along the scapular axis. The anatomic parameters analyzed included the shape, axial configuration, maximum width, maximum height, version, and presence of bone defect.
Results
In our study, 76.6% of glenoids were pear-shaped, 23.0% were elliptical, and only 0.4% were inverted pear in shape. Of all glenoids, 95.1% of glenoids had posterior-prominent axial configuration, whereas 4.9% had neutral axial configuration. The mean maximum glenoid height for both genders was 33.8 mm, whereas the mean maximum glenoid height was 32.2 mm for women and 36.6 mm for men. The mean maximum glenoid width for both genders was 25.8 mm, whereas the mean maximum glenoid width was 24.8 mm for women and 27.3 mm for men. The differences in measurements between genders were statistically significant. Of all glenoids, 46.3% of the glenoids were retroverted, whereas 53.7% of the glenoids were anteverted. The mean version for both genders was 0.77 degrees anteversion. The mean version was 1.16 degrees anteversion for women and 0.10 degrees anteversion for men. Of the 244 glenoids, 4 had bone defects. In our study, 39.8% of patients had mean maximum glenoid widths that were less than 25 mm, which is the smallest size available for most conventional glenoid baseplates.
Conclusion
A significant portion of the Southern Chinese population has glenoid widths that are smaller than the smallest commercially available glenoid baseplates. Understanding the glenoid anatomy is crucial in the case of reverse shoulder arthroplasty, as it has significant implications in implant design, operative planning, and surgical outcomes.
Keywords: Glenoid anatomy, Glenoid morphology, 2D-CT, Reverse shoulder arthroplasty, Hong Kong, Southern Chinese
The anatomy of the glenoid, particularly in the Caucasian and African-American population, has been well-documented in numerous cadaveric and radiologic studies.2,3,6,9,21,25,27,28,41,43 The anatomic parameters of interest, especially in reverse shoulder arthroplasties, include the shape, height, width, version, and presence of bone defect in the glenoid.
Previous studies have noted some differences in the glenoid anatomy between different populations of patients. For example, Churchill et al6 reported that glenoids of Caucasian patients tend to be more retroverted compared with those of African-American patients. These studies also described significant differences in the glenoid anatomy between genders.2,6,27,28 The version of the glenoid also varied between patients with healthy glenoids and those with shoulder pathology such as rotator cuff tears, glenohumeral joint arthritis, and chronic dislocations of the shoulder.8,15,31
It is useful to know these anatomic parameters when planning for reverse shoulder arthroplasties. As the glenoid is notorious for having limited bone stock, understanding its anatomy can allow us to better position the glenoid component so as to achieve maximal bone purchase during its fixation.31 A poorly positioned glenoid component has often been linked to suboptimal functional outcome and increased risk of glenoid component-related complications such as loosening.11,13,14,18,20,22,40,48 Studies about the glenoid anatomy and the biomechanics of the glenohumeral joint have also contributed to the evolution of the glenoid component design over the years, which may translate to better surgical outcomes for patients undergoing this procedure.1,5,16,22,26,32,34,36,43,44
The aim of this study is to describe the glenoid anatomy in the Southern Chinese population, which we currently serve. We are interested to see how the anatomic parameters of the glenoids in this population compare with those analyzed in previous studies and its clinical implication.
Methods
This is a retrospective study including all patients who were admitted to our district hospital from 2012 to 2019 for shoulder injuries and had plain 2-dimensional (2D) computed tomography (CT) scans of the shoulder done. Skeletally immature patients, patients with fractures involving the glenoid or scapula, infection, and tumors involving the glenoid or scapula, as well as those with significant glenohumeral arthritis were excluded from the study. The 2D CT scans were formatted to align with the axis of the scapula (along the medial border of the scapular body and trans-scapular axis) using the Osirix software (Fig. 1).
Figure 1.
CT reformatted using Osirix software. Orange line: medial scapular body. Blue line: trans-scapular axis. Purple line: Center of best fit circle/point with widest glenoid width. CT, computed tomography.
The glenoid shape was classified into 3 types based on the ratio of the glenoid width at the superior third to the inferior third of the glenoid, measured on the sagittal view of the CT scan. The 3 types of glenoid shape were pear (ratio < 0.8), elliptical (ratio 0.8-1.2), and inverted pear (ratio > 1.2) (Fig. 2).
Figure 2.
Glenoid shape.
The axial configuration of the glenoid was classified into 3 types: posterior-prominent, neutral, and anterior-prominent (Fig. 3). The axial cut used to determine the axial configuration of the glenoid was at the level of the center of the best-fit circle.
Figure 3.
Axial configuration of the glenoid.
The maximum glenoid width was the distance from the most anterior to most posterior points of the glenoid on the axial view. The maximum glenoid height was the distance from the most superior to the most inferior points of the glenoid on the coronal view.
The glenoid version was calculated using the trans-scapular axis as reference, at the level of the center of the best-fit circle. The version was 90 degrees minus the anterior angle between the trans-scapular axis and a line connecting the most anterior and posterior points of the glenoid surface (Fig. 4).15,49
Figure 4.
Glenoid version.
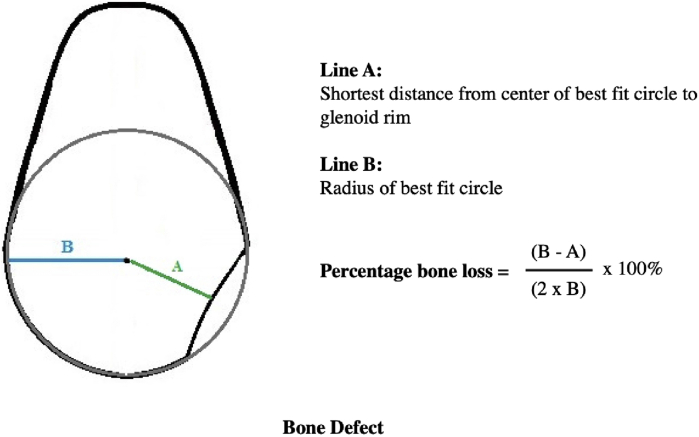
Presence of bone defect was noted and quantified using the “best-fit circle” method (Fig. 5).37,49
Figure 5.
Calculation of bone defect.
The measurements were first made by the same observer twice, months apart. A second observer was invited to measure the parameters again. The average of all 3 measurements was taken. Interclass correlation coefficients were 0.95 for intraobserver agreement and 0.94 for interobserver agreement.
The data collected were analyzed using the IBM SPSS Statistics program (IBM, Armonk, NY, USA). We defined a P-value of <0.05 as statistically significant. Analyses of the shape, axial configuration, and type of version between both genders were performed using frequency tables and the Pearson Chi-square test. We applied the independent-sample T-test for analyses of the glenoid heights, glenoid widths, and the degrees of version for both genders. A frequency table was constructed to document the presence of bone defect.
Ethics review and approval were obtained for this study, granted by the Joint Chinese University of Hong Kong-New Territories East Cluster Clinical Research Ethics Committee on April 2020.
Results
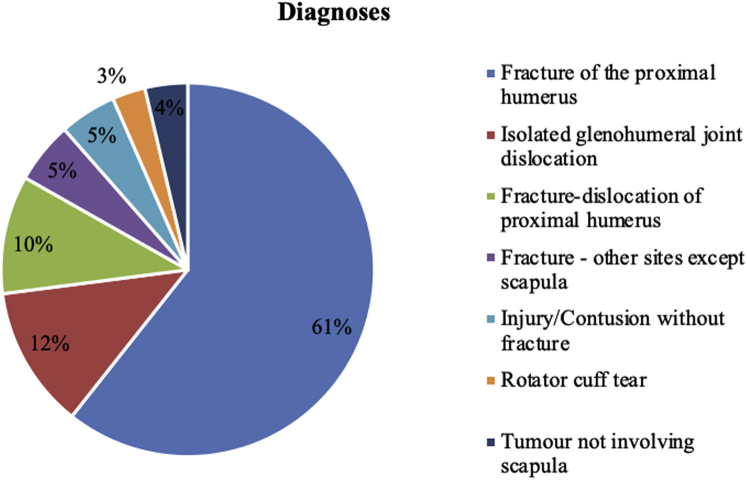
A total of 244 patients were included in this study; of which, 150 were women and 94 were men. The mean age for the female patients was 69.1 years, whereas the mean age for the male patients was 55.2 years. The overall mean age was 64.0 years (range 16-97 years) (Fig. 6). All of these patients had CT scans performed owing to “shoulder injury” as the indication and were then found to have different diagnoses afterward (Fig. 7).
Figure 6.
Age distribution of study population.
Figure 7.
Indications for 2D CT scans of the shoulder by diagnoses. CT, computed tomography; 2D, 2-dimensional.
Of the glenoids, 76.6% (n = 187) of glenoids were pear-shaped, whereas 23.0% (n = 56) were elliptical. Only 0.4% (n = 1) of glenoids were inverted pear in shape.
Of the glenoids, 95.1% (n = 232) of glenoids had posterior-prominent axial configuration, whereas 4.9% (n = 12) had neutral axial configuration. None of the glenoids had anterior-prominent axial configuration.
The mean maximum glenoid height for both genders was 33.8 mm. The mean maximum glenoid height was 32.2 mm for women and 36.6 mm for men. The difference in means was statistically significant between genders (P = .000) (Table I) (Fig. 8).
Table I.
Data analyses for glenoid height, glenoid width, and glenoid version for both genders
| Gender | Mean maximum glenoid height | Standard deviation |
| Both | 33.8 | 3.180 |
| Male | 36.6 | 2.659 |
| Female | 32.2 | 2.165 |
| Difference between genders is statistically significant (P < .05) | ||
| Gender |
Mean maximum glenoid width |
Standard deviation |
| Both | 25.8 | 2.423 |
| Male | 27.3 | 2.258 |
| Female | 24.8 | 2.017 |
| Difference between genders is statistically significant (P < .05) | ||
| Gender |
Mean version |
Standard deviation |
| Both | +0.77 | 6.569 |
| Male | +0.10 | 6.206 |
| Female | +1.16 | 6.741 |
| Difference between genders is not statistically significant (P = .225) | ||
Figure 8.
Distribution of glenoid height for both genders.
The mean maximum glenoid width for both genders was 25.8 mm. The mean maximum glenoid width was 24.8 mm for women and 27.3 mm for men. Again, the difference in means was statistically significant between genders (P = .000) (Table I) (Fig. 9).
Figure 9.
Distribution of glenoid width for both genders.
Of the 244 glenoids, 113 (46.3%) were retroverted, whereas 131 (53.7%) were anteverted. The mean version for both genders was 0.77 degrees anteversion. The mean version for women was 1.16 degrees anteversion and for men was 0.10 degrees anteversion. The difference in versions was not statistically significant between genders (P = .225) (Table I).
Of the 244 glenoids, only 4 had bone defects (1.6%).
Discussion
We compared our data with those reported in previous cadaveric and radiologic studies. Most of the studies, especially the earlier studies, were on Caucasian and African-American patients.2, 3, 4,6,7,9,12,21,25,27, 28, 29, 30,41,43,47
Similar to these studies, we found most glenoids in our study were pear-shaped, whereas the remaining was elliptical.3,21,43 None of the studies mentioned an “inverted pear”–shaped glenoid. The solitary inverted pear–shaped glenoid in our study was a result of significant bone loss at the glenoid. The pear-shaped glenoid would be most favorable in reverse shoulder arthroplasties, as majority of the bone stock is concentrated at the inferior third of the glenoid, which corresponds to the ideal position of the baseplate.10,11,17,35,42 Inferior placement of the baseplate is important to avoid impingement over the scapula by the humeral tray.10,11,17,35,42 In our population, it is usually difficult to accommodate all 4 screws for fixation of the baseplates onto the smaller glenoids. A pear shape would be most ideal in such situations as its largest width is at the inferior part of the glenoid, which allows for maximal contact surface area of the baseplate at its ideal position. In the case of “inverted pear”–shaped glenoids, strategies to improve the bone stock at the inferior third of the glenoid, such as bone grafting, may need to be considered.33,37 In some circumstances, the baseplate may need to be fixed at a less-than-optimal position to obtain the best bone purchase and stable fixation. In this case, we may need to rely on the modular offset design of the glenosphere to achieve an optimal inferior shift or tilt.
Previous studies did not take into account the axial configuration of the glenoid or how it affects preoperative planning in the case of reverse shoulder arthroplasty.2, 3, 4,6,7,9,12,21,25,27, 28, 29, 30,41,43,47 Conventionally, the baseplate is thought to be best placed at anatomical center of the glenoid. However, we found that majority of our patients have posterior-prominent glenoids. Putting the glenoid baseplate at the anatomical center may lead to risk of posterior cortex blowout and result in shorter lengths of the central peg and posterior screws, especially for those with small glenoid widths to begin with. Jha et al23 recommended for the baseplate to be positioned more anteriorly on the axial plane in their Japanese female patients for this very reason. Preoperative assessment of the axial configuration of the glenoid is essential in helping us decide the optimal location of the baseplate in this plane, as well as to help plan the trajectory and length of the central peg and screws to be used. A custom-made patient-specific guide for screw insertion can also be considered for patients with significant bone loss or abnormal anatomy.
The definitions for the mean maximum glenoid heights and widths were similar across the different studies that used CT scans for analyses.2,4,28, 29, 30,43,47 However, in the case of analyzing 2D CT scans, a significant limitation in obtaining accurate measurements lie in the scapular rotation, which is affected by the positioning of the patient on the CT table. To overcome this, some authors have recommended the use of 3-dimensional (3D) CT radiographs for preoperative planning, though this resource may not be readily available across different orthopedic centers.19,39,46 Another option is to reformat the 2D CT scans so that it is aligned to the scapular axis (along the medial border of the scapular body and trans-scapular axis).45
It is worth noting that 97 (39.8%) of the patients in our study had mean maximum glenoid widths that were less than 25 mm. The size options for conventional glenoid baseplates are quite limited, with 25 mm being the smallest size available for most systems. Most systems also allow insertion of up to 4 peripheral screws. For the 39.8% of patients from our study, the size of the commercially available glenoid baseplates is too large and may result in risk of glenoid baseplate overhang in the anterior-posterior dimension as well as render insertion of all 4 peripheral screws, especially the anterior and posterior screws, difficult if not impossible.23,24 This may result in weaker fixation of the baseplate to the glenoid, leading to poorer clinical outcome.38 The development and use of custom-made patient-specific implants may be considered in such cases of patients with particularly small glenoid widths.
As reverse shoulder arthroplasty is becoming increasingly popular over the years, there has been a rise in the number of anatomic studies on the Asian population. Many of the existing studies’ discussions and conclusions raised similar concerns that currently available glenoid implants may not be suited for the smaller sized Asian population.2,4,23,24,29,30 Table II is a summary of the data compiled from these studies involving different populations, for comparison with the measurements in our study.2,4,6,7,12,21,25,27, 28, 29, 30,43,47
Table II.
Comparison of glenoid height and glenoid width across different studies
| Study | Number of glenoids studied | Type of study | Country | Race/Ethnicity | Mean glenoid height |
Mean glenoid width∗ |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| Both genders | Male | Female | Both genders | Male | Female | |||||
| Churchill et al.6 | 144 | Cadaveric | America | Caucasian | 37.4 | 32.5 | 28.1 | 23.8 | ||
| Churchill et al.6 | 200 | Cadaveric | America | African American | 37.6 | 32.7 | 27.6 | 23.4 | ||
| Iannotti et al.19 | 140 | Cadaveric | America | 39 | 29 | |||||
| Kwon et al.23 | 12 | Cadaveric | America | 37.8 | 26.8 | |||||
| Kwon et al.23 | 12 | CT scan | America | 39.1 | 25.2 | |||||
| Mallon et al.25 | 28 | Cadaveric | America | 38 | 36.2 | 28.3 | 23.6 | |||
| Mathews et al.26 | 18 | Cadaveric and CT scan | Switzerland | Swiss | 36.6 | 39.5 | 34.8 | 27.8 | 30.3 | 26.2 |
| El-Din et al.11 | 160 | Cadaveric | Egypt | Egyptian | 39 | 28.2 | ||||
| Coskun et al.7 | 90 | Cadaveric | Turkey | Turkish | 36.3 | 24.6 | ||||
| Cabezas et al.2 | 92 | CT scan | America | North American | 35.8 | 38.4 | 33.3 | 28 | 30.5 | 25.6 |
| Mizuno et al.28 | 100 | CT scan | Japan | French | 35.4 | 37.3 | 33.5 | 26.7 | 28.7 | 24.7 |
| Cabezas et al.2 | 58 | CT scan | South Korea | East Asian | 33.4 | 34.3 | 31.9 | 25.7 | 25.7 | 23.7 |
| Mizuno et al.28 | 100 | CT scan | Japan | Japanese | 33.3 | 35.3 | 31.4 | 25.5 | 27.4 | 23.5 |
| Meshram et al.27 | 200 | CT scan | India | Indian | 33.9 | 36.1 | 31.7 | 24.2 | 25.8 | 22.6 |
| Cheung et al.4 | 70 | CT scan | Hong Kong | Southern Chinese | 37.4 | 39.1 | 34.4 | 28.6 | 30.2 | 25.8 |
| Yang et al.44 | 56 | CT scan | China | Chinese | 35.8 | 27.3 | ||||
| This study | 244 | CT scan | Hong Kong | Southern Chinese | 33.8 | 36.6 | 32.2 | 25.8 | 27.3 | 24.8 |
CT, computed tomography.
∗ for studies that recorded mean superior and inferior glenoid widths, the inferior glenoid widths, which have larger measurements, are included in this table.
The glenoids in our study were more anteverted, as most of the aforementioned studies described mean versions that were retroverted. One exception is a study conducted by Friedman et al,15 which reported a mean of 2 degrees anteversion when analyzing the 2D CT scans of 63 healthy glenoids. Werner et al46 compared the measurements of glenoid version on reformatted 2D CT scans with measurements from 3D CT scans and found that the versions from the 2D CT scans were more anteverted than the 3D measurements. They then concluded that the measurement of the glenoid version on reformatted 2D CT scans was less accurate compared with that of 3D measurements.19,39,46 We should thus keep in mind the possible discrepancy in the version measured on the 2D CT scans compared with the actual glenoid when preparing for surgery. This makes intraoperative assessment of the glenoid version all the more essential.
The glenoid version affects our orientation of the glenoid component during shoulder arthroplasties. Studies by Farron et al,13 Shapiro et al,40 and Yian et al48 have suggested that retroverted glenoids are associated with poorer functional outcomes and early loosening of the glenoid components. For glenoids with retroversions of more than 10 degrees, Farron et al13 recommended intraoperative correction of the version.
All 4 glenoids that were documented to have bone defects in our study were related to history of shoulder dislocations. It is important to take note of any bone loss when preparing for reverse shoulder arthroplasty as it is crucial in the fixation and positioning of the glenoid component.37 Bone grafting may be considered in select cases to optimize surgical outcome.33
Although preoperative CT scans of the shoulder can give us a general idea about the glenoid morphology to aid in our surgical planning, there are some measures that we can take intraoperatively to improve on our glenoid implant fixation. Meticulous clearance of the glenoid rim, including soft tissue and labrum, can help us assess the exact size and configuration of the glenoid. Direct visualization of the glenoid, careful intraoperative assessment using finger palpation along the glenoid neck and X-ray guidance can help us confirm the ideal trajectory during insertion of the screws and central peg of the baseplate.
There are several weaknesses to our study. First, we made the assumption that patients who had 2D CT scans of the shoulder performed on admission to our unit because of shoulder injury were representative of the normal population. We think it is a fair assumption to make, as it would be highly difficult for us to obtain ethics board approval for a study that exposes the normal asymptomatic population to radiation. We hope that having a sizeable sample size and random sampling based on clinical admission is sufficient in representing the population we are interested in. In addition, we think that the patients who were included in our study were particularly relevant to the study, as these were the patients who may potentially benefit from reverse shoulder arthroplasty for their conditions. In fact, 17 of these patients did end up having reverse shoulder arthroplasties performed.
Second, our analyses of the axial configuration were qualitative in nature. We did not have a quantitative measure to evaluate the extent of the posterior-prominence, which may be more informative.
Third, we mentioned the limitations of 2D CT scans in measuring glenoid parameters compared with 3D CT scans, especially in the case of the glenoid version. It should also be noted that 55 (22.5%) of the patients in our study had anterior dislocations or fracture dislocations of the shoulder joint. This may result in a bias in the calculation of the version, as patients with anterior glenoid versions may be more prone to such dislocations.
Conclusion
A significant portion of the Southern Chinese population has glenoid widths that are smaller than the smallest commercially available glenoid baseplates.
Understanding the glenoid anatomy is crucial in the case of reverse shoulder arthroplasty, as it has significant implications in implant design, operative planning, and surgical outcomes.
Disclaimers:
Funding: No funding was disclosed by the author(s).
Conflicts of interest: The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Approval was obtained from the Joint Chinese University of Hong Kong-New Territories East Cluster Clinical Research Ethics Committee on 31 March 2020 (CREC reference number: 2020.070).
References
- 1.Anglin C., Wyss U.P., Pichora D.R. Mechanical testing of shoulder prostheses and recommendations for glenoid design. J Shoulder Elbow Surg. 2000;9:323–331. doi: 10.1067/mse.2000.105451. [DOI] [PubMed] [Google Scholar]
- 2.Cabezas A.F., Krebes K., Hussey M.M., Santoni B.G., Kim H.S., Frankle M.A. Morphologic variability of the shoulder between the populations of North American and East Asian. Clin Orthoped Surg. 2016;8:280–287. doi: 10.4055/cios.2016.8.3.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chechroun A.J., Hawkins C., Kummer F.J., Zuckerman J.D. Fit of current glenoid component designs: an anatomic cadaver study. J Shoulder Elbow Surg. 2002;11:614–617. doi: 10.1067/mse.2002.126009. [DOI] [PubMed] [Google Scholar]
- 4.Cheung Y.L.A., Lie W.H.C., Chow H.L., Chan W.L., Wong K.H.K., Woo S.B. Are the Current Size Options of Glenoid Baseplates for Reverse Shoulder Arthroplasty Sufficient for our Local Population? J Orthopaedics, Trauma Rehabil. 2016;21:30–34. doi: 10.1016/j.jotr.2015.11.002. [DOI] [Google Scholar]
- 5.Churchill R.S., Boorman R.S., Fehringer E.V., Matsen F.A., 3rd Glenoid cementing may generate sufficient heat to endanger the surrounding bone. Clin Orthop Relat Res. 2004:76–79. doi: 10.1097/00003086-200402000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Churchill R.S., Brems J.J., Kotschi H. Glenoid size, inclination, and version: an anatomic study. J Shoulder Elbow Surg. 2001;10:327–332. doi: 10.1067/mse.2001.115269. [DOI] [PubMed] [Google Scholar]
- 7.Coskun N., Karaali K., Cevikol C., Demirel B.M., Sindel M. Anatomical basics and variations of the scapula in Turkish adults. Saudi Med J. 2006;27:1320–1325. [PubMed] [Google Scholar]
- 8.Couteau B., Mansat P., Mansat M., Darmana R., Egan J. In vivo characterization of glenoid with use of computed tomography. J Shoulder Elbow Surg. 2001;10:116–122. doi: 10.1067/mse.2001.112884. [DOI] [PubMed] [Google Scholar]
- 9.Cyprien J.M., Vasey H.M., Burdet A., Bonvin J.C., Kritsikis N., Vuagnat P. Humeral retroversion and glenohumeral relationship in the normal shoulder and in recurrent anterior dislocation (scapulometry) Clin Orthop Relat Res. 1983:8–17. [PubMed] [Google Scholar]
- 10.De Wilde L.F., Poncet D., Middernacht B., Ekelund A. Prosthetic overhang is the most effective way to prevent scapular conflict in a reverse total shoulder prosthesis. Acta Orthop. 2010;81:719–726. doi: 10.3109/17453674.2010.538354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duethman N.C., Aibinder W.R., Nguyen N.T.V., Sanchez-Sotelo J. The influence of glenoid component position on scapular notching: a detailed radiographic analysis at midterm follow-up. J Shoulder Elbow Surg. 2020;4:144–150. doi: 10.1016/j.jses.2019.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El-Din W.A., Ali M.H. A morphometric study of the patterns and variations of the acromion and glenoid cavity of the scapulae in Egyptian population. J Clin Diagn Res. 2015;9:Ac08–Ac11. doi: 10.7860/JCDR/2015/14362.6386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farron A., Terrier A., Buchler P. Risks of loosening of a prosthetic glenoid implanted in retroversion. J Shoulder Elbow Surg. 2006;15:521–526. doi: 10.1016/j.jse.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Franta A.K., Lenters T.R., Mounce D., Neradilek B., Matsen F.A., 3rd The complex characteristics of 282 unsatisfactory shoulder arthroplasties. J Shoulder Elbow Surg. 2007;16:555–562. doi: 10.1016/j.jse.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 15.Friedman R.J., Hawthorne K.B., Genez B.M. The use of computerized tomography in the measurement of glenoid version. J Bone Joint Surg Am. 1992;74:1032–1037. [PubMed] [Google Scholar]
- 16.Gartsman G.M., Elkousy H.A., Warnock K.M., Edwards T.B., O’Connor D.P. Radiographic comparison of pegged and keeled glenoid components. J Shoulder Elbow Surg. 2005;14:252–257. doi: 10.1016/j.jse.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 17.Gutierrez S., Levy J.C., Frankle M.A., Cuff D., Keller T.S., Pupello D.R., Lee W.E., 3rd Evaluation of abduction range of motion and avoidance of inferior scapular impingement in a reverse shoulder model. J Shoulder Elbow Surg. 2008;17:608–615. doi: 10.1016/j.jse.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 18.Hasan S.S., Leith J.M., Campbell B., Kapil R., Smith K.L., Matsen F.A., 3rd Characteristics of unsatisfactory shoulder arthroplasties. J Shoulder Elbow Surg. 2002;11:431–441. doi: 10.1067/mse.2002.125806. [DOI] [PubMed] [Google Scholar]
- 19.Hoenecke H.R., Hermida J.C., Flores-Hernandez C., D’Lima D.D. Accuracy of CT-based measurements of glenoid version for total shoulder arthroplasty. J Shoulder Elbow Surg. 2009;19:166–171. doi: 10.1016/j.jse.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 20.Hopkins A.R., Hansen U.N., Amis A.A., Emery R. The effects of glenoid component alignment variations on cement mantle stresses in total shoulder arthroplasty. J Shoulder Elbow Surg. 2004;13:669–675. doi: 10.1016/S1058274604001399. [DOI] [PubMed] [Google Scholar]
- 21.Iannotti J.P., Gabriel J.P., Schneck S.L., Evans B.G., Misra S. The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J Bone Joint Surg Am. 1992;74:491–500. [PubMed] [Google Scholar]
- 22.Ianotti J.P., Spencer E.E., Winter U., Deffenbaugh D., Williams G. Prosthetic positioning in total shoulder arthroplasty. J Shoulder Elbow Surg. 2005;14:111S–121S. doi: 10.1016/j.jse.2004.09.026. [DOI] [PubMed] [Google Scholar]
- 23.Jha S.C., Fukuta S., Wada K., Higasino K., Amari-Kita R., Tsutsui T. Optimising baseplate position in reverse total shoulder arthroplasty in small-sized Japanese females: technical notes and literature review. J Med Invest. 2016;63:8–14. doi: 10.2152/jmi.63.8. [DOI] [PubMed] [Google Scholar]
- 24.Ji J.H., Jeong J.Y., Song H.S., Ok J.H., Yang S.J., Jeon B.K. Early clinical results of reverse total shoulder arthroplasty in the Korean population. J Shoulder Elbow Surg. 2013;22:1102–1107. doi: 10.1016/j.jse.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 25.Kwon Y.W., Powell K.A., Yum J.K., Brems J.J., Iannotti J.P. Use of three-dimensional computed tomography for the analysis of the glenoid anatomy. J Shoulder Elbow Surg. 2005;14:85–90. doi: 10.1016/j.jse.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 26.Lazarus M.D., Jensen K.L., Southworth C., Matsen F.A., 3rd The radio-graphic evaluation of keeled and pegged glenoid component insertion. J Bone Joint Surg Am. 2002;84:1174–1182. doi: 10.2106/00004623-200207000-00013. [DOI] [PubMed] [Google Scholar]
- 27.Mallon W.J., Brown H.R., Vogler J.B., III, Martinez S. Radiographic and geometric anatomy of the scapula. Clin Orthop Relat Res. 1992:142–154. [PubMed] [Google Scholar]
- 28.Mathews S., Burkhard M., Serrano N., Link K., Häusler M., Frater N. Glenoid morphology in light of anatomical and reverse total shoulder arthroplasty: a dissection-based and 3D-CT-based study in male and female body donors. BMC Musculoskelet Disord. 2017;18:9. doi: 10.1186/s12891-016-1373-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meshram P., Pawaskar A., Kekatpure A. 3D CT scan-based study of glenoid morphology in Indian population: Clinical relevance in design of reverse total shoulder arthroplasty. J Clin Orthopaedics Trauma. 2020;11:S604–S609. doi: 10.1016/j.jcot.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mizuno N., Nonaka S., Ozaki R. Three-dimensional assessment of the normal Japanese glenoid and comparison with the normal French glenoid. Orthop Traumatol Surg Res OTSR. 2017;103:1271–1275. doi: 10.1016/j.otsr.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 31.Mullaji A.B., Beddow F.H., Lamb G.H. CT measurement of glenoid erosion in arthritis. J Bone Joint Surg Br. 1994;76:384–388. [PubMed] [Google Scholar]
- 32.Murphy L.A., Prendergast P.J., Resch H. Structural analysis of an offset-keel design glenoid component compared with a center-keel design. J Shoulder Elbow Surg. 2001;10:568–579. doi: 10.1067/mse.2001.118630. [DOI] [PubMed] [Google Scholar]
- 33.Norris T.R. Glenoid Bone Loss in Reverse Shoulder Arthroplasty Treated with Bone Graft Techniques. Am J Orthop (Belle Mead Nj) 2018;47 doi: 10.12788/ajo.2018.0016. [DOI] [PubMed] [Google Scholar]
- 34.Nuttall D., Haines J.F. Trail. II. A study of the micromovement of pegged and keeled glenoid components compared using radio-stereometric analysis. J Shoulder Elbow Surg. 2007;16:S65–S70. doi: 10.1016/j.jse.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 35.Nyffeler R.W., Wener C.M., Gerber C. Biomechanical relevance of glenoid component positioning in the reverse Delta III total shoulder prosthesis. J Shoulder Elbow Surg. 2005;14:524–528. doi: 10.1016/j.jse.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 36.Orr T.E., Carter D.R., Schurman D.J. Stress analyses of glenoid component designs. Clin Orthop Relat Res. 1988:217–224. [PubMed] [Google Scholar]
- 37.Provencher M.T., Bhatia S., Ghodadra N.S., Grumet R.C., Bach B.R., Jr., Dewing C.B. Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Joint Surg Am. 2010;92:133–151. doi: 10.2106/JBJS.J.00906. [DOI] [PubMed] [Google Scholar]
- 38.Roche C., DiGeorgio C., Yegres J., VanDeven J., Stroud N., Flurin P.H. Impact of screw length and screw quantity on reverse total shoulder arthroplasty glenoid fixation for 2 different sizes of glenoid baseplates. J Shoulder Elbow Surg. 2019;3:296–303. doi: 10.1016/j.jses.2019.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Scalise J.J., Codsi M.J., Bryan J., Brems J.J., Iannotti J.P. The influence of three-dimensional computed tomography images of the shoulder in preoperative planning for total shoulder arthroplasty. J Bone Joint Surg Am. 2008;90:2438–2445. doi: 10.2106/JBJS.G.01341. [DOI] [PubMed] [Google Scholar]
- 40.Shapiro T.A., McGarry M.H., Gupta R., Lee Y.S., Lee T.Q. Biomechanical effects of glenoid retroversion in total shoulder arthroplasty. J Shoulder Elbow Surg. 2007;16:S90–S95. doi: 10.1016/j.jse.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 41.Sharkey N.A., Marder R.A. The rotator cuff opposes superior translation of the humeral head. Am J Sports Med. 1995;23:270–275. doi: 10.1177/036354659502300303. [DOI] [PubMed] [Google Scholar]
- 42.Simovitch R.W., Zumstein M.A., Lohri E., Helmy N., Gerber C. Predictors of scapular notching in patients managed with Delta III reverse total shoulder replacement. J Bone Joint Surg Am. 2007;89:588–600. doi: 10.2106/JBJS.F.00226. [DOI] [PubMed] [Google Scholar]
- 43.Strauss E.J., Roche C., Flurin P.H., Wright T., Zuckerman J.D. The glenoid in shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:819–833. doi: 10.1016/j.jse.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 44.Szabo I., Buscayret F., Edwards T.B., Nemoz C., Boileau P., Walch G. Radiographic comparison of flat-back and convex-back glenoid components in total shoulder arthroplasty. J Shoulder Elbow Surg. 2005;14:636–642. doi: 10.1016/j.jse.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 45.van de Bunt F., Pearl M.L., Lee E.K., Peng L., Didomenico P. Glenoid version by CT scan: an analysis of clinical measurement error and introduction of a protocol to reduce variability. Skeletal Radiol. 2015;44:1627–1635. doi: 10.1007/s00256-015-2207-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Werner B.S., Hudek R., Burkhart K.J., Gohlke F. The influence of three-dimensional planning on decision-making in total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1477–1483. doi: 10.1016/j.jse.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 47.Yang Y., Zuo J., Liu T., Shao P., Wu H., Gao Z. Glenoid morphology and the safe zone for protecting the suprascapular nerve during baseplate fixation in reverse shoulder arthroplasty. Int Orthop. 2018;42:587–593. doi: 10.1007/s00264-017-3646-4. [DOI] [PubMed] [Google Scholar]
- 48.Yian E.H., Werner C.M., Nyffeler R.W., Pfirrmann C.W., Ramappa A., Sukthankar A. Radiographic and computed tomography analysis of cemented pegged polyethylene glenoid components in total shoulder replacement. J Bone Joint Surg Am. 2005;87:1928–1936. doi: 10.2106/JBJS.D.02675. [DOI] [PubMed] [Google Scholar]
- 49.Yun G., Kang Y., Joong M.A., Lee E. A Comprehensive Review of Shoulder CT Morphometry: What Surgeons Want to Know. J Korean Soc Radiol. 2018;78:265–278. doi: 10.3348/jksr.2018.78.4.265. [DOI] [Google Scholar]