Abstract
There is some confusion in the terminology used when referring to MIS (Minimal invasive surgery) or percutaneous surgery. The correct term to describe these procedures should be percutaneous (made through the skin) and MIS should be reserved for procedures whose extent is between percutaneous and open surgery (e.g. osteosynthesis). Minimal incision surgery may be distinguished in first, second and third generation minimal incision surgery techniques.
First generation MIS hallux valgus surgery is mainly connected with the Isham procedure; an intraarticular oblique and incomplete osteotomy of the head of the first metatarsal without fixation.
The Bösch osteotomy and the SERI are classified as second generation MIS hallux surgery. They are both transverse subcapital osteotomies fixed with a percutaneous medial K-wire inserted into the medullary canal. For all these procedures, intraoperative fluoroscopic control is necessary.
Open hallux valgus surgery can be divided into proximal, diaphyseal and distal osteotomies of the first metatarsal. Reviewing the available literature suggests minimally invasive and percutaneous hallux valgus correction leads to similar clinical and radiological results to those for open chevron or SCARF osteotomies. First generation minimally invasive techniques are primarily recommended for minor deformities. In second generation minimally invasive hallux valgus surgery, up to 61% malunion of the metatarsal head is reported. Once surgeons are past the learning curve, third generation minimally invasive chevron osteotomies can present similar clinical and radiological outcomes to open surgeries. Specific cadaveric training is mandatory for any surgeon considering performing minimally invasive surgical techniques.
Cite this article: EFORT Open Rev 2021;6:432-438. DOI: 10.1302/2058-5241.6.210029
Keywords: MIS, open hallux valgus surgery, percutaneous surgery
Hallux valgus is one of the most common pathologies of the lower extremity. Nix et al1 performed a systematic review and meta-analysis on the prevalence of hallux valgus. In 78 reviewed papers the pooled prevalence estimated for hallux valgus was 23% in adults aged 18–65 years (male: 8.5%, female: 26.3%) and 35.7% in adults aged over 65 years (male: 16%, female: 36%). The earliest reports of surgical hallux valgus correction with resection of the metatarsal head date back to the 19th century.2 Reverdin, in 1881,3 was the first to describe an open subcapital closing wedge for the correction of hallux valgus deformity. It later became more popular as the Hohmann procedure4 and many years later when used in a minimal surgery fashion as the Isham osteotomy.5
From the beginning of the use of osteotomies for the treatment of hallux valgus deformities, surgeons distinguished between distal, diaphyseal and proximal osteotomies. While the Hohmann,4 the Wilson,6 the Mitchell7 and the Chevron/Austin8 osteotomies were representatives of the distal type of osteotomy, the Ludloff,9 crescentic Mann osteotomy10 and proximal Chevron11 were representatives of the proximal osteotomies. The SCARF is a diaphyseal osteotomy. In 1974, Helal counted over 150 different techniques which appeared in the literature.12
Roger Mann13 and Wanivenhaus14 both established algorithms according to the severity of the deformity for the correction of hallux valgus deformity. In 1945, Polokoff reported a system of subdermal surgery as the first attempt for minimal incision hallux valgus surgery.15 By the 1960s, power-operated burrs and shavers became available.16 With these small power instruments older techniques like the Reverdin or Hohmann procedures were manageable via tiny incisions and were renamed Isham, Bösch osteotomy,5,17 or SERI.18 (Simple, Effective, Rapid, Inexpensive)
There is some confusion in the terminology used to refer to MIS (Minimal invasive surgery) or percutaneous surgery. The correct term to describe these procedures should be percutaneous (made through the skin) and MIS should be reserved for procedures situated in extent between percutaneous and open surgery (e.g. osteosynthesis).19 Minimal incision surgery may be distinguished as first, second and third generation minimal incision surgery techniques.
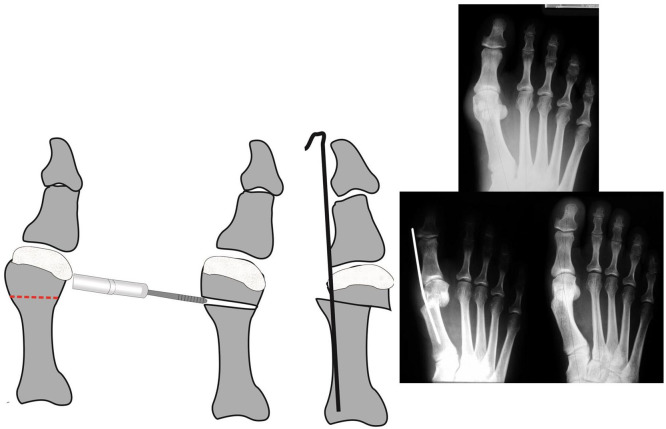
First generation MIS hallux valgus surgery is mainly connected with the Isham procedure (Fig. 1); an intraarticular oblique and incomplete osteotomy of the head of the first metatarsal. The principle of this technique dates back to the Reverdin osteotomy from the 19th century.19 A correction of the IM (Intermetatarsal) angle will not be achieved. This technique is performed with fluoroscopic control without fixation.
Fig. 1.
The Isham–Reverdin osteotomy.
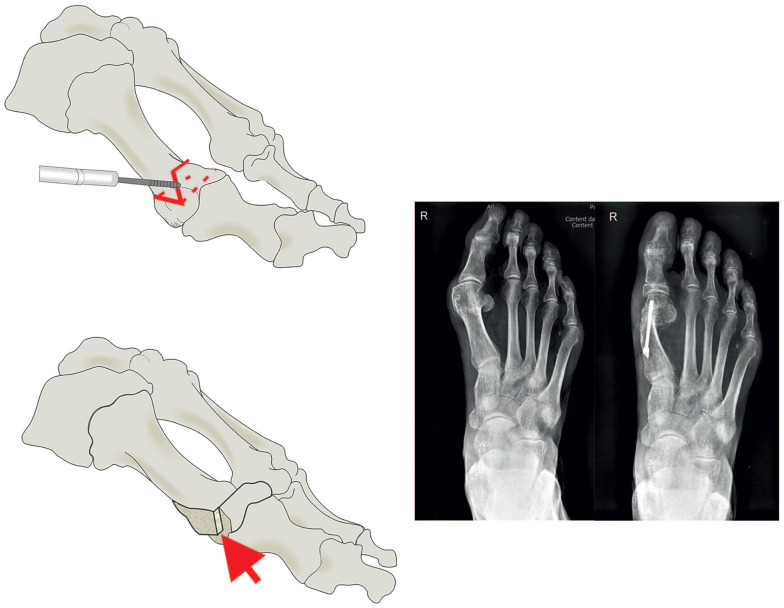
The Bösch osteotomy (Fig. 2)17,20 and the SERI18 are the examples of second generation MIS hallux surgery. They are both transverse subcapital osteotomies fixed with a percutaneous medial K-wire inserted into the medullary canal and represent a modification of the Hohmann osteotomy first described in 1923.4 While the Bösch osteotomy is a percutaneous osteotomy with a 2 mm burr, the SERI osteotomy is performed through a small incision with an oscillating saw. No additional soft tissue release is performed. For both procedures, intraoperative fluoroscopic control is necessary.
Fig. 2.
Bösch osteotomy. Case: 25-year-old female preoperatively, four weeks and one year after surgery.
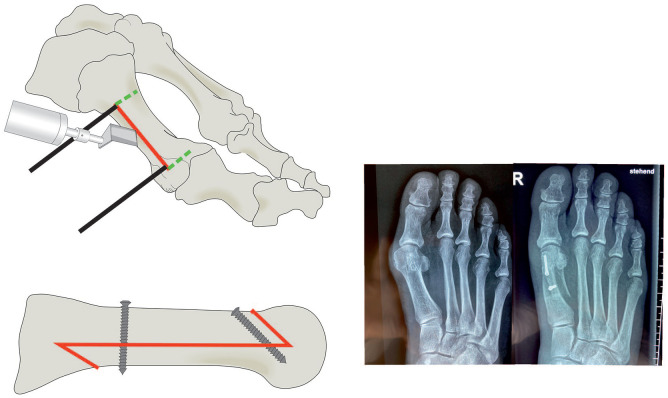
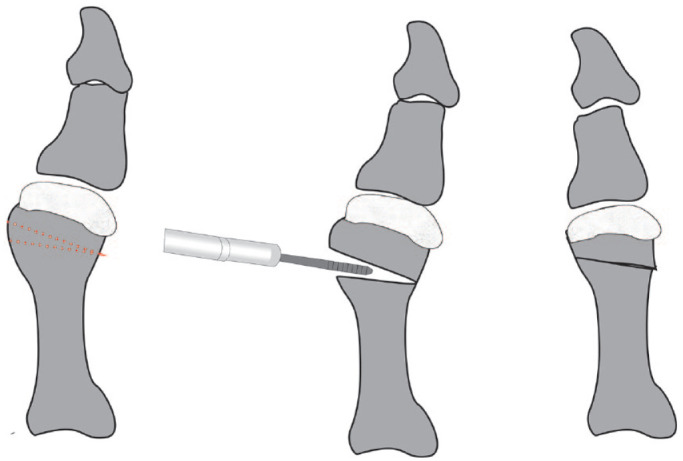
The third generation MIS hallux valgus correction osteotomies have evolved from the Chevron type osteotomies (Fig. 3).8,19 The osteotomy is performed percutaneously with a 2 mm burr under fluoroscopic control. The translation of the metatarsal head is achieved by placing a periosteal elevator through the portal into the diaphysis of the proximal fragment and levering the distal fragment laterally. One or two Herbert-type screws are used to gain extra stability, which allows faster rehabilitation.
Fig. 3.
MIS (Minimal invasive surgery) Chevron osteotomy: 65-year-old female preoperatively and six weeks after surgery.
Source: Case courtesy of G. Kaufmann.
Open hallux valgus surgery can be divided into osteotomies performed on the proximal, diaphyseal and distal regions of the first metatarsal. Since most of the MIS and percutaneous hallux valgus correction is described on the distal metatarsal, for this article I have also discussed distal and diaphyseal osteotomies for comparison.
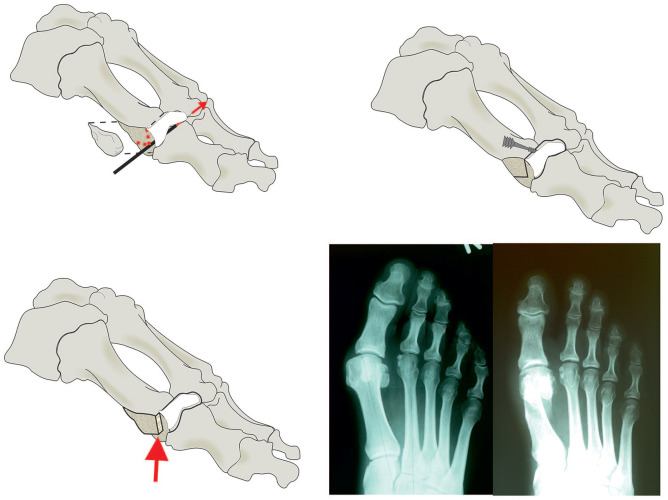
According to the hallux valgus treatment algorithm of the Austrian Foot and Ankle Society,14 the most common internationally used osteotomies in this area of the metatarsal are the Kramer, the Chevron/Austin (Fig. 4), and the SCARF osteotomy (Fig. 5).
Fig. 4.
Austin/Chevron osteotomy. Case: 53-year-old female preoperatively and two years after surgery.
Fig. 5.
SCARF osteotomy. Case: 57-year-old female preoperatively and four weeks after surgery.
Reverdin3 and Barker21 were the first to describe distal medial closing wedge metatarsal osteotomies for hallux valgus correction. In 1921, this procedure was popularized by Hohmann.4 The downside of the original technique was the necessity of a cast and the resulting shortening of the metatarsal. To compensate for these undesired effects, Kramer22 modified the original technique with a lateral translation osteotomy and added a Kirschner-wire fixation. This procedure is still in use.23,24 In the Kramer osteotomy, a dorsomedial skin incision is used, and the periosteum is elevated circumferentially from the metatarsal neck and, using a power saw, transverse subcapital osteotomy is performed and the distal fragment is shifted laterally. The hallux is held in a minimal overcorrection position and a percutaneous Kirschner-wire from the tip of the first toe, medial to the displaced head into the shaft of the first metatarsal which is retained for six weeks.
In 1962, Austin performed his first horizontally directed ‘V’ osteotomy.8 In the initial report by Austin and Leventen no fixation was mentioned. They suggested that the shape of the osteotomy and impaction of the cancellous capital fragment upon the shaft of the first metatarsal provided sufficient stability to forego fixation. Over the decades research on K-wire fixation and screw fixation with various types of screws has been published.25,26
A skin incision is made at the medial aspect of the first MTP(Metatarsophalangeal) joint. The metatarsal head is then exposed, and Hohmann retractors are placed dorsal and plantar just extraarticular of the first metatarsophalangeal joint. The medial eminence is now minimally shaved to achieve a even surface. A 1.0 mm, Kirschner-wire is placed minimally dorsal to the centre of the exposed medial eminence. This wire is generally inclined 20° from medial to lateral, aiming at the head of the fourth metatarsal. Using a saw guide, two cuts at an angle between 60° and 80° are then made with an oscillating power saw. The distal fragment is translated laterally and fixed with a screw. In general, a lateral soft tissue release is added either transarticularly or via a second incision over the first webspace.
The SCARF osteotomy was first described by Burutaran27 in 1976, followed by American podiatrists.28,29 Borrelli and Weil30 and Barouk31 then popularized this technique worldwide. Using a straight midline incision, the metatarsal is exposed. A lateral soft tissue release is performed. After placing two K-wires to mark the two edges of the Z-type osteotomy, the osteotomy is performed by using a power oscillating saw. After lateral translation of the plantar fragment fixation is achieved by using two Herbert-type screws.
Results
First generation MIS
Bauer et al32 presented a multicentre study of the distal percutaneous metatarsal osteotomy according to Isham with a mean follow-up of 13 months (12–24 months). The AOFAS score (American Orthopaedic Foot and Ankle Society) improved from 52 points on average preoperatively, to 93 points at follow-up. The median range of motion reduced from 90° preoperatively to 75°, which is an average of 17% loss of motion. Neither nonunion, AVN 8avascular necrosis) or malunion of the capital fragment were reported.
Biz et al33 performed, between 2010 and 2012, a consecutive series of the combined Akin and Reverdin–Isham osteotomies on 80 patients. Complete healing was achieved by three months. Complications occurred in 25 patients (31.25%) including access portal burns during surgery, loss of range of motion in 16 patients and recurrence of deformity in five cases.
Second generation MIS
Bösch et al17 presented their preliminary results with the SCOT (Subcapital Metatarsal First Osteotomy) technique. The average follow-up was 16 months (range 8–32 months). Range of motion of the MTP-1 joint decreased in 31.5% of the patients. The incidence of pin tract infection of the temporary K-wire was 9%. In a follow-up study in 200017 the incidence of infection was reduced. Evaluation of the hallux valgus and intermetatarsal angle at follow-up revealed pathologic values on average (19° HV hallux valgus) angle and 10° IM angle). Portaluri34 published, in 2000, a series of the Bösch technique in 143 patients with 182 operated feet with similar results.
Magnan et al,20 in 2005, reported on 118 consecutive percutaneous distal metatarsal osteotomies at an average of 35.9 months follow-up. Significant correction of all radiological parameters was reported. Quite interesting was the incidence of malalignment of the metatarsal head. In 61%, either plantar or dorsal displacement of the capital fragment was noted.
In a series by Iannò et al35 significant correction of hallux valgus and intermetatarsal angle was noted. But an overall complication rate of 29.4% with recurrence of deformity in 18.8% lead the authors to the conclusion that caution should be exercised when using this technique. Enan and colleagues36 reported 55.6% of either dorsal or plantar displacement of the distal fragment.
Giannini et al18 presented a series of 641 patients with 1000 osteotomies. Contrary to the above-mentioned results, he reported no nonunion and only eight cases of dorsal malalignment out of 1000 osteotomies.
Poggio at al37 reviewed a series of MIS Kramer (Bösch) and SCARF osteotomies to evaluate the costs. Patients in the Kramer group made significantly more visits (especially emergency room visits, due to the higher number of complications) and the economic cost of follow-up was greater. They concluded that the MIS Kramer osteotomy had a significantly higher care burden and was therefore less cost-effective. The analysis of these data has resulted in the abandonment of the Kramer osteotomy technique.
Third generation MIS
Vernois and Redfern38 reported the results of 100 feet treated with a percutaneous Chevron osteotomy. Radiological analysis revealed a correction of the intermetatarsal angle from 14.5° to 5.5° at the last follow-up. The mean hallux valgus angle was corrected from 33.7° preoperatively to 7.3° at the last follow-up. Patient-reported satisfaction rate was 95% good/excellent results.
Jowett and Bedi39 reviewed the learning curve of the first 120 minimally invasive Chevron osteotomies by dividing the population into group A (first 60) and group B (consecutive 60). Patient satisfaction and radiological correction were better in group B, but results were statistically not significant. There was a learning curve, but results were promising and comparable to open hallux valgus surgery.
Kaufmann et al40 published, in 2020, a series of 19 minimally invasive Chevron osteotomies assessed at six and 12 weeks, 9 months, and five years postoperatively. The K-wire used for fixation had to be removed in 16 of the 19 cases.
Lucas y Hernandez et al41 presented a series of 38 patients who underwent 45 extraarticular reverse-L Chevron (PERC) osteotomies. With a mean follow-up of 59.1 months (45.9 to 75.2), the AOFAS score increased from 62.5 (range, 30 to 80) preoperatively to 97.1 (range, 75 to 100). There was a statistically significant decrease in the hallux valgus angle and the intermetatarsal angle. With a mean preoperative hallux valgus and intermetatarsal angle of 26 degrees and 11 degrees, respectively, these patients presented mainly mild deformities.
A series of 25 minimally invasive Chevron/Akin osteotomies was reviewed by Lee et al.42 Six patients required removal of the screws because of prominence of the screws under the skin. Significant improvements in the hallux valgus angle and the intermetatarsal angle were observed at final follow-up (P < .05).
Comparative studies open hallux surgery vs. minimal incision hallux valgus surgery
Lee et al42 compared percutaneous Chevron/Akin (PECA) and open SCARF/Akin osteotomies. Both groups showed significantly improved clinical and radiological results. The PECA group showed significantly lower pain level (visual analogue scale) in the early postoperative phase. No serious complications were observed in either group.
Kaufmann et al40 published, in 2020, a randomized controlled study of minimally invasive distal metatarsal chevron osteotomy and open chevron with five-year follow-up. No significant differences were seen between the two groups within five years postoperatively in terms of clinical outcomes (VAS, AOFAS, satisfaction), radiographic outcomes, joint degeneration, or range of motion.
A retrospective cohort study of 49 minimally invasive versus and 32 open distal Chevron osteotomies was reviewed by Brogan et al.43 Clinical and radiologic postoperative scores in all domains were substantially improved in both groups but there was no statistically significant difference in improvement of any domain between open and MIS groups. There were no significant differences in complications between the two groups.
A comparative study of 31 feet treated with the Bösch osteotomy and 33 feet treated with a Chevron osteotomy was presented by Radwan and Mansour.44 The mean operative time was shorter in the Bösch group (50.86 minutes versus 58 minutes). Both osteotomies yielded similar clinical and radiological results.
Mafulli et al45 compared a group of 36 SCARF osteotomies with a group of 36 Bösch osteotomies. They also noted significantly shorter surgical time with the Bösch osteotomy and comparable clinical and radiological results.
In a cost-comparison study by Poggio et al,37 the minimally invasive Kramer osteotomy presented significantly higher care burdens, complication rates and associated costs during the first year of follow-up.
Conclusion
When reviewing the available literature, minimally invasive and percutaneous hallux valgus correction lead to similar clinical and radiological results as the open chevron or SCARF osteotomies. First generation minimally invasive techniques are primarily recommended for minor deformities since they are performed without translation of the capital fragment and therefore avoid the potential of reduction of the intermetatarsal angle. They similarly avoid the potential risk of joint incongruency. In second generation minimally invasive hallux valgus surgery, Magnan et al20 and Enan et al36 reported 61% and 55.6% malunion of the metatarsal head. Poggio et al37 investigated the cost-effectiveness of the MIS Kramer (Bösch) osteotomy compared to the SCARF osteotomy and demonstrated significantly higher cost burden of the MIS Kramer (Bösch) osteotomy and therefore abandoned the technique. Third generation minimally invasive Chevron osteotomies present similar clinical and radiological outcomes. Once the surgeons were past the learning curve the complication rate was similar to open chevron or SCARF. The benefit is the size of the incision; the disadvantage being the length of radiation exposure. Redfern and Perera46 pointed out that specific cadaveric training is mandatory for any surgeon considering performing minimally invasive surgical techniques, and this training is vital to avoid unnecessary complications and to minimize the surgeon’s learning curve.
Footnotes
ICMJE Conflict of interest statement: The author declares no conflict of interest relevant to this work.
OA licence text: This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res 2010;3:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hueter C. Kapitel 5. Leipzig: Klinik der Gelenkkrankheiten mit Einschluss der Orthopädie, 1870:345–346. [Google Scholar]
- 3. Reverdin J. De la deviation en dehors du gros orl (hallux valgus) et son traitement chirurgical. Trans Int Med Congress 1881;2:408–412. [Google Scholar]
- 4. Hohmann G. Symptomatische oder physiologische Behandlung des Hallux valgus. Munch Med Wochenschr 1921;33:1042–1045. [Google Scholar]
- 5. Isham SA. The Reverdin–Isham procedure for the correction of hallux abducto valgus: a distal metatarsal osteotomy procedure. Clin Podiatr Med Surg 1991;8:81–94. [PubMed] [Google Scholar]
- 6. Wilson DW. Treatment of hallux valgus and bunions. Br J Hosp Med 1980;24:548–549. [PubMed] [Google Scholar]
- 7. Mitchell CL, Fleming JL, Allen R, Glenney C, Sanford GA. Osteotomy-bunionectomy for hallux valgus. J Bone Joint Surg Am 1958;40-A:41–58. [PubMed] [Google Scholar]
- 8. Austin DW, Leventen EO. A new osteotomy for hallux valgus: a horizontally directed ‘V’ displacement osteotomy of the metatarsal head for hallux valgus and primus varus. Clin Orthop Relat Res 1981;157:25–30. [PubMed] [Google Scholar]
- 9. Weinfeld AB. The Ludloffs osteotomy for correction of hallux valgus: a historic procedure re-invented. In: Osteotomies of the hindfoot and forefoot. 2nd International Spring Meeting (AFCP) Bordeaux, 4 May 2000. [Google Scholar]
- 10. Mann RA, Rudicel S, Graves SC. Repair of hallux valgus with a distal soft-tissue procedure and proximal metatarsal osteotomy: a long-term follow-up. J Bone Joint Surg Am 1992;74:124–129. [PubMed] [Google Scholar]
- 11. Easley ME, Kiebzak GM, Davis WH, Anderson RB. Prospective, randomized comparison of proximal crescentic and proximal chevron osteotomies for correction of hallux valgus deformity. Foot Ankle Int 1996;17:307–316. [DOI] [PubMed] [Google Scholar]
- 12. Helal B. Surgery for adolescent hallux valgus. Clin Orthop Relat Res 1981;157:50–63. [PubMed] [Google Scholar]
- 13. Mann RA. Decision-making in bunion surgery. Instr Course Lect 1990;39:3–13. [PubMed] [Google Scholar]
- 14. Wanivenhaus A, Bock P, Gruber F, et al. Deformity-associated treatment of the hallux valgus complex. Orthopade 2009;38:1117–1126. [DOI] [PubMed] [Google Scholar]
- 15. Polokoff M. Raspostectomy: reduction of exostoses and hypertrophied condyles with files and rasps. J Am Podiatry Assoc 1962;52:599–602. [PubMed] [Google Scholar]
- 16. Chalk DE, Sammarco GJ. Minimum incision surgery. Foot Ankle 1992;13:157–160. [DOI] [PubMed] [Google Scholar]
- 17. Bösch P, Markowski HP, Rannicher V. Technik und erste Ergebnisse der subkutanen distalen Metatarsale-I-Osteotomie. Orthop Prax 1990;26:51–56. [Google Scholar]
- 18. Giannini S, Faldini C, Nanni M, Di Martino A, Luciani D, Vannini F. A minimally invasive technique for surgical treatment of hallux valgus: simple, effective, rapid, inexpensive (SERI). Int Orthop 2013;37:1805–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Del Vecchio JJ, Ghioldi ME. Evolution of minimally invasive surgery in hallux valgus. Foot Ankle Clin 2020;25:79–95. [DOI] [PubMed] [Google Scholar]
- 20. Magnan B, Pezzè L, Rossi N, Bartolozzi P. Percutaneous distal metatarsal osteotomy for correction of hallux valgus. J Bone Joint Surg Am 2005;87:1191–1199. [DOI] [PubMed] [Google Scholar]
- 21. Barker A. An operation for hallux valgus. Lancet 1884;123:655. [Google Scholar]
- 22. Kramer J. Die Kramer Osteotomie zur Behandlung des Hallux valgus und des digitus quintus varus. Oper Orthop Traumatol 1990;2:29–38. [Google Scholar]
- 23. Trnka HJ, Hofmann S, Wiesauer H, Kaider A, Salzer M, Ritschl P. Kramer versus Austin osteotomy: two distal metatarsal osteotomies for correction of hallux valgus deformities. Orthopedics 2004;5:110–116. [Google Scholar]
- 24. Schulze C, Böhme N, Hacke C, Gutcke A, Bergschmidt P. Kramer and chevron osteotomy for hallux valgus deformity: retrospective comparison of functional and radiological results. Z Orthop Unfall 2019;157:29–34. [DOI] [PubMed] [Google Scholar]
- 25. Trnka HJ, Zembsch A, Easley ME, Salzer M, Ritschl P, Myerson MS. The chevron osteotomy for correction of hallux valgus: comparison of findings after two and five years of follow-up. J Bone Joint Surg Am 2000;82:1373–1378. [PubMed] [Google Scholar]
- 26. Hofstaetter SG, Schuh R, Trieb K, Trnka HJ. Modified chevron osteotomy with lateral release and screw fixation for treatment of severe hallux deformity. Z Orthop Unfall 2012;150:594–600. [DOI] [PubMed] [Google Scholar]
- 27. Burutaran JM. Hallux valgus y cortedad anatomica del primer metatarsano (correction quinrugica). Actual Med Chir Pied 1976;XIII:261–266. [Google Scholar]
- 28. Gudas CJ. Compression screw fixation in proximal first metatarsal osteotomies for metatarsus primus varus: initial observations. J Foot Surg 1979;18:10–15. [PubMed] [Google Scholar]
- 29. Schwartz N, Groves ER. Long-term follow-up of internal threaded Kirschner-wire fixation of the SCARF bunionectomy. J Foot Surg 1987;26:313–316. [PubMed] [Google Scholar]
- 30. Borrelli AH, Weil LS. Modified SCARF bunionectomy: our experience in more than one thousand cases. J Foot Ankle Surg 1991;30:609–612. [Google Scholar]
- 31. Barouk LS. New osteotomies in the forefoot and their therapeutic role. In: Valtin B, ed. Forefoot surgery. Paris: Expansion Scientifique Française, 1997:49–76. [Google Scholar]
- 32. Bauer T, de Lavigne C, Biau D, De Prado M, Isham S, Laffenétre O. Percutaneous hallux valgus surgery: a prospective multicenter study of 189 cases. Orthop Clin North Am 2009;40:505–514, ix. [DOI] [PubMed] [Google Scholar]
- 33. Biz C, Crimì A, Fantoni I, Tagliapietra J, Ruggieri P. Functional and radiographic outcomes of minimally invasive intramedullary nail device (MIIND) for moderate to severe hallux valgus. Foot Ankle Int 2020. doi: 10.1177/1071100720969676 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 34. Portaluri M. Hallux valgus correction by the method of Bösch: a clinical evaluation. Foot Ankle Clin 2000;5:499–511, vi. [PubMed] [Google Scholar]
- 35. Iannò B, Familiari F, De Gori M, Galasso O, Ranuccio F, Gasparini G. Midterm results and complications after minimally invasive distal metatarsal osteotomy for treatment of hallux valgus. Foot Ankle Int 2013;34:969–977. [DOI] [PubMed] [Google Scholar]
- 36. Enan A, Abo-Hegy M, Seif H. Early results of distal metatarsal osteotomy through minimally invasive approach for mild-to-moderate hallux valgus. Acta Orthop Belg 2010;76:526–535. [PubMed] [Google Scholar]
- 37. Poggio D, Melo R, Botello J, Polo C, Fernández de Retana P, Asunción J. Comparison of postoperative costs of two surgical techniques for hallux valgus (Kramer vs. SCARF). Foot Ankle Surg 2015;21:37–41. [DOI] [PubMed] [Google Scholar]
- 38. Vernois J, Redfern DJ. Percutaneous surgery for severe hallux valgus. Foot Ankle Clin 2016;21:479–493. [DOI] [PubMed] [Google Scholar]
- 39. Jowett CRJ, Bedi HS. Preliminary results and learning curve of the minimally invasive chevron akin operation for hallux valgus. J Foot Ankle Surg 2017;56:445–452. [DOI] [PubMed] [Google Scholar]
- 40. Kaufmann G, Mörtlbauer L, Hofer-Picout P, Dammerer D, Ban M, Liebensteiner M. Five-year follow-up of minimally invasive distal metatarsal chevron osteotomy in comparison with the open technique: a randomized controlled trial. J Bone Joint Surg Am 2020;102:873–879. [DOI] [PubMed] [Google Scholar]
- 41. Lucas y, Hernandez J, Golanó P, Roshan-Zamir S, Darcel V, Chauveaux D, Laffenêtre O. Treatment of moderate hallux valgus by percutaneous, extra-articular reverse-L chevron (PERC) osteotomy. Bone Joint J 2016;98-B:365–373 [DOI] [PubMed] [Google Scholar]
- 42. Lee M, Walsh J, Smith MM, Ling J, Wines A, Lam P. Hallux valgus correction comparing percutaneous chevron/Akin (PECA) and open SCARF/Akin osteotomies. Foot Ankle Int 2017;38:838–846. [DOI] [PubMed] [Google Scholar]
- 43. Brogan K, Lindisfarne E, Akehurst H, Farook U, Shrier W, Palmer S. Minimally invasive and open distal chevron osteotomy for mild to moderate hallux valgus. Foot Ankle Int 2016;37:1197–1204. [DOI] [PubMed] [Google Scholar]
- 44. Radwan YA, Mansour AM. Percutaneous distal metatarsal osteotomy versus distal chevron osteotomy for correction of mild-to-moderate hallux valgus deformity. Arch Orthop Trauma Surg 2012;132:1539–1546. [DOI] [PubMed] [Google Scholar]
- 45. Maffulli N, Longo UG, Oliva F, Denaro V, Coppola C. Bosch osteotomy and Scarf osteotomy for hallux valgus correction. Orthop Clin North Am 2009;40:515–524, ix–x. [DOI] [PubMed] [Google Scholar]
- 46. Redfern D, Perera AM. Minimally invasive osteotomies. Foot Ankle Clin 2014;19:181–189. [DOI] [PubMed] [Google Scholar]