Abstract
Ankle sprains are mainly benign lesions, but if not well addressed can evolve into permanent disability. A non-treated lateral, syndesmotic or medial ankle instability can evolve into ankle osteoarthritis. For this reason, diagnosis and treatment of these entities is of extreme importance.
In general, acute instabilities undergo conservative treatment, while chronic instabilities are better addressed with surgical treatment. It is important to identify which acute instabilities are better treated with early surgical treatment.
Syndesmosis injuries are frequently overlooked and represent a cause for persistent pain in ankle sprains. Unstable syndesmotic lesions are always managed by surgery.
Non-treated deltoid ligament ruptures can evolve into a progressive valgus deformity of the hindfoot, due to its links with the spring ligament complex. This concept would give new importance to the diagnosis and treatment of acute medial ligament lesions.
Multi-ligament lesions are usually unstable and are better treated with early surgery. A high suspicion rate is required, especially for combined syndesmotic and medial lesions or lateral and medial lesions.
Ankle arthroscopy is a powerful tool for both diagnostic and treatment purposes. It is becoming mandatory in the management of ankle instabilities and multiple arthroscopic lateral/syndesmotic/medial repair techniques are emerging.
Cite this article: EFORT Open Rev 2021;6:420-431. DOI: 10.1302/2058-5241.6.210017
Keywords: ankle instability, ankle sprains, arthroscopy, deltoid ligament lesion, lateral instability, medial instability, syndesmosis instability, syndesmotic instability
Introduction
Ankle instability is a clinical condition closely related with the traumatic event commonly known as ankle sprain, usually a supination trauma. This event is extremely frequent, being one of the top causes of Emergency Room visits and frequently related to sports. In most cases, the ankle sprain is a benign situation that heals completely after an uneventfully course but up to 30% of cases will develop permanent complications.1 Ankle instability is one of these complications. The term instability implies a dysfunction of the ligaments. It can be acute or chronic and results from a traumatic event, and is therefore related with a ligament rupture. The ankle has three main set of ligaments: the lateral, the medial and the syndesmotic ligaments.
Lateral instability
The anatomy of the ankle joint makes it weak in supination. Supination trauma stresses the lateral ligament, putting it at risk, so the rupture of the lateral ligament is the most frequent lesion of the ankle.2 Some of these patients will develop chronic ankle instability (CAI), making this situation an important and frequent condition.1
Anatomy
Consensus
The lateral ankle ligament has three bundles: anterior talo-fibular ligament (ATFL); calcaneo-fibular ligament (CFL) and posterior talo-fibular ligament (PTFL). The ATFL and PTFL are mainly horizontal, bounding the anterior and posterior faces of the distal fibula with the talus giving some sagittal stability in different positions of the ankle joint but also, and mainly, rotational stability. The CFL is mainly a vertical structure with its insertions on the anterior distal part of the fibula and the lateral calcaneus. It is mainly a coronal plane stabilizer.
Controversy
Some authors describe two (or three) fascicules of the ATFL, mainly a proximal and a distal one with a visible separation between the fascicules, the distal being apparently stronger than the proximal. The distal fascicule shares the fibular footprint with CFL and with some arciform fibres connecting the two ligaments, suggesting that the distal fascicule of the ATFL and the CFL are the same anatomic structure.3 This is the anatomic support for the idea that the repair of the AFTL will produce an indirect re-insertion of the CFL.
In the same way, there might be some connections between the proximal fascicule of the ATFL and the anterior inferior tibiofibular ligament (AITFL), part of the syndesmotic ligament, sharing the same footprint on the fibula. This might explain the relationship between the anterolateral impingement syndrome and micro-instability.4 The improper healing of the AITFL causes the meniscoid and the partial rupture of the ATFL causes the micro-instability.
Biomechanics
Consensus
The incompetence of the lateral ligament complex will impair the sagittal, coronal and transverse joint stability producing a tendency to varus tilt and anterior translation of the talus. Due the bony configuration of the ankle, this is also the weakest point in terms of stability. This impairs the normal function of the joint. Nevertheless, not all instabilities act in the same way.
Controversy
Although the idea of ankle instability as a homogeneous condition is still present, in terms of biomechanics there are clearly some sub-groups. Freeman, in 1965, proposed the term functional instability as an alternative to mechanical instability.5 Functional instability is proposed to result from functional insufficiencies such as strength deficits, impaired proprioception and impaired neuromuscular or postural control.6 Hertel6 proposed a model involving mechanical and functional insufficiencies that is widely accepted. In this model, mechanical and functional insufficiencies are not mutually exclusive, and recurrent sprain occurs when both conditions are present. At this point a patient is considered to have mechanical instability when there is documented increased laxity on the symptomatic ankle (when compared with the other side) either on the clinical examination, stress X-rays or stress sonography. Patients in whom this laxity cannot be documented are considered to have functional instability.5,7
This is the most known and accepted model, despite the fact that some patients do not fit into it. Hiller proposed an evolution of the Hertel model, with three different types of CAI patients: ‘mechanical instability’, ‘perceived instability’ and ‘recurrent sprains’.8 This group differentiation, in terms of biomechanical behaviour, should cover all types of CAI. Nevertheless, there are some cases that do not fit completely into these groups, like the recently described micro-instability.4,9
Clinical features and classification
Consensus
Acute ankle instability occurs after a traumatic supination trauma. It presents with pain and tenderness on the ATFL, peri-malleolar swelling and effusion, ecchymosis and gait impairment. Usually, the severity of this condition is classified into three grades, but there is no consensus regarding the characteristics of each grade, making it difficult to establish a prognosis based on current classification systems.10 History of a previous sprain may predispose to chronicity, but we still lack the clinical signs to predict the evolution to CAI.11 On physical examination, the more important sign is the anterior drawer sign with a sensitivity of 73–96% and a specificity of 84–97% to detect a compromised ATFL.12 The importance of other signs is still controversial.13
Chronic ankle instability (CAI) has been defined as ‘repetitive bouts of lateral ankle instability resulting in numerous ankle sprains’.8 The most commonly cited characteristics of CAI include giving way of the ankle, mechanical instability, pain and swelling, loss of strength, recurrent sprain and functional instability.
The clinical picture might be grouped into the following presentations:
✓ A first acute sprain followed by pain
✓ Repetitive sprains with symptom-free intervals
✓ Repetitive sprains with pain between them
It is not uncommon for patients to report progressive pain between the sprains, which tells the clinician that the prognosis is deteriorating. Terada et al defined individuals with CAI according to the presence of a previous history of an acute lateral ankle sprain which caused swelling, pain, and temporary loss of function for at least one day; and repeated episodes of ‘giving way’ for six months and/or recurrent ankle sprains and/or perceived ankle instability.14
Controversy
Clinically, the anterior drawer sign is a standard test to identify ankle instability. Other classical signs such as the sulcus or the varus tilt test may not be that helpful. The main goal of the anterior drawer test is to define the insufficiency of the ATFL (in the sagittal plane) which is always the first ruptured ligament, and the varus tilt will detect insufficiency of the CFL (in the coronal plane). These are single-plane tests, which may not be ideal for multiple-plane lesions. For instance, the fact that the medial ligament is intact limits the pure anterior translation of the talus. If we add a rotational momentum (exactly as the lesion is produced) the ATFL insufficiency becomes more evident, because the lateral side would give in and the deltoid ligament would act as the fulcrum.15
Another grey area is the definition, time wise, of chronicity. It is difficult to draw the line and define the precise moment when an instability becomes chronic. The rationale behind chronicity is when the body ceases its attempt to heal a lesion. The time when it happens varies from case to case and we do not have a tool that can give us the answer so we can use a broad timeframe, usually from three to six months.
There is no consensus on a classification of ankle sprains that is widely accepted. As all classification, it should orientate the treatment options, give a notion of prognosis and allow a normalization of speech, so everybody knows what a grade III means. This is yet to be achieved. What we have now is a classification into three grades (I to III) and this graduation can be pathophysiologic (strain, partial rupture, complete rupture), anatomic (one ligament to three ligaments ruptured) or clinical (minor symptoms to unable to stand). Ideally, we should be able to identify which cases are more prone to develop CAI. These cases may benefit from early surgical treatment, to avoid the economic burden of absence from work or to shorten return to sport.
There is no classification of CAI, besides the biomechanical distinction mentioned above (mechanical versus functional), and not even this differentiation is agreed on. Also, there are some clinical categories that have been proposed such as micro-instability that do not fit into any of the previous ones. There is some work to be done on this field.
Imaging
Consensus
For acute events, a radiogram should be taken, according to the Ottawa criteria, to exclude fractures and, in severe cases, an ultrasound (US) can be done to identify complete ruptures, which may have implications in terms of treatment and follow-up. A few days after the accident and in severe cases, magnetic resonance imaging (MRI) is the most helpful exam, showing the extent of the ligament lesion and the presence of concomitant lesions. MRI can also be helpful in the pre-operative workup.16
Controversy
The use of stress radiographs, very popular in the past, is falling out of favour. Some authors doubt their benefit for the decision-making algorithm and the results can be misleading.12 The benefit of the use of radiographs in the chronic phase is not clear. Some features that can be identified on a radiogram (varus heel, cavus foot or short medial malleolus) have been reported as triggering or worsening factors for CAI, but there is no evidence of this relationship. Nevertheless, most surgeons have the tendency of correcting a varus heel when doing a CAI repair.17
Ultrasounds can be helpful in the acute phase but MRI is a more powerful exam in the late acute and chronic phase. Nevertheless, the US is a dynamic exam and can give some important information such as the amount of translation between bones. On the other hand, it does depend on the examiner and the way it is done. The use of MRI in the acute phase should be made with care because the extent of the lesions may be exacerbated by this imaging technique. On the other hand, in patients with chronic status, some of the concomitant lesions may not be detected. Some new imaging techniques such as weight-bearing CT can be useful,18 especially in a chronic setting, but their applicability is yet to be defined.
Non-operative treatment
Consensus
An acute ankle sprain should receive a functional treatment that includes a rigid brace that allows dorsi-plantar flexion and blocks varus-valgus stress, as well as early physiotherapy for CAI prevention.19 The outcomes of non-operative treatment for CAI are usually considered poor. Most surgeons would consider this kind of treatment only to prevent recurrences and especially in a post-operative context to improve the outcome.
Controversy
There is some evidence of good results with neuromuscular training functional instability treatment, especially during training or after surgery. The rationale behind this method is related to the thought that deficient sensory input from damaged ankle ligament receptors contributes to sensorimotor deficits in those with CAI. Targeting other viable sensory receptors may then enhance sensorimotor control in these patients. This is called sensory-targeted ankle rehabilitation strategies (STARS) on patient- and clinician-oriented outcomes in those with CAI. This method has been described as a valid treatment to address this condition with success.20 Nevertheless, self-reported functional deficits, worse single-limb balance, and number of previous ankle sprains are important characteristics that can impair the probability of treatment success.21 Although there are positive reports, the efficacy of this method needs further validation.
The classical algorithm of treatment decision on CAI would say that mechanical instability is treated with surgery (but as we have seen there might be some room for conservative treatment) and functional instability with physiotherapy. However, some surgeons would advocate surgery, even on mechanically stable ankles, after a period of three to six months of non-surgical treatment.16
Surgical treatment
Consensus
The gold standard for the surgical treatment of CAI is the Brostrom–Gould operation.16 First described by Brostrom in 1966, it consists of a direct re-insertion of the torn ligament on the fibula, usually using some kind of suture anchors. Later, Gould added a reinforcement using the extensor retinaculum that is mobilized and attached to the fibula over the ligament re-insertion, increasing the strength of the repair. The aim is to reproduce the normal anatomy. It is easy to preform, reproducible and has been extensively used, with numerous articles of literature confirming its efficacy.22–24 Nevertheless, when the remaining tissue does not permit a confident repair, the ligaments should be replaced and reconstructed, usually using some kind of graft replacing the original anatomy (more frequently a hamstring autograft).25
Several other surgical techniques have been proposed to treat CAI. A group of techniques called ‘tenodesis’ gained some popularity in the past. It consisted of using usually the Peroneus brevis tendon (totally or partial) to create loops with different configurations (depending on the author) to stabilize the lateral aspect of the ankle and subtalar joint. These techniques have several drawbacks: sacrifice of the main dynamic stabilizer of the ankle, altered biomechanics with a tendency to stiffness, being an extensive operation with difficult rehabilitation, among other reasons.22 Because of their poor results these techniques should be abandoned.
In summary, we have two types of CAI repair: An anatomic direct repair using the remaining ligaments and the extensor retinaculum or a replacement of the ligaments using a tendon graft reproducing the normal orientation. With the advent of ankle arthroscopy, several arthroscopic techniques have been described for ankle instability repair. We also know that ankle sprains are frequently combined with concomitant intra-articular lesions,26,27 and most of these lesions can be diagnosed and treated trough arthroscopic means. For these reasons, it is becoming mandatory to scope the ankle while treating CAI.
Controversy
If all CAI repairs should include a routine ankle arthroscopy, an arthroscopic method of CAI repair would be a good idea. The senior author developed an arthroscopic repair technique for CAI, that was published in 2009,28 trying to reproduce the Brostrom–Gould principles. This operation included the implantation of a suture anchor above the footprint of the ATFL and passing the suture through an accessory portal made on top of the extensor retinaculum. The sutures are passed through the retinaculum and the remaining ligament. The purpose is fixing the ligament stump and extensor retinaculum to the fibula and compressing against the footprint (Fig. 1 and Fig. 2). The author has nearly 20 years’ experience with this method with good results, at least as good as open techniques, with less morbidity. Since that first publication, several other authors have reported good outcomes of arthroscopic repair techniques, reproducing open surgery principles. These results were also confirmed by independent authors and validated by meta-analysis and systematic reviews.23
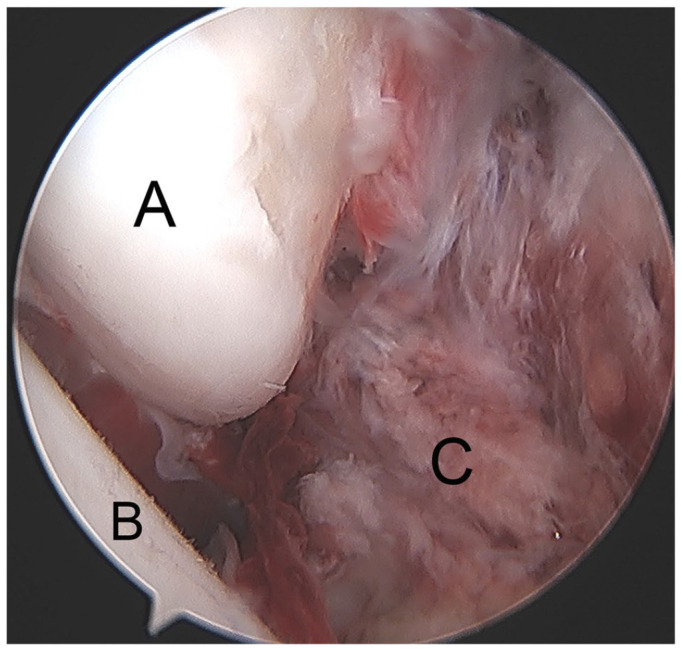
Fig. 1.
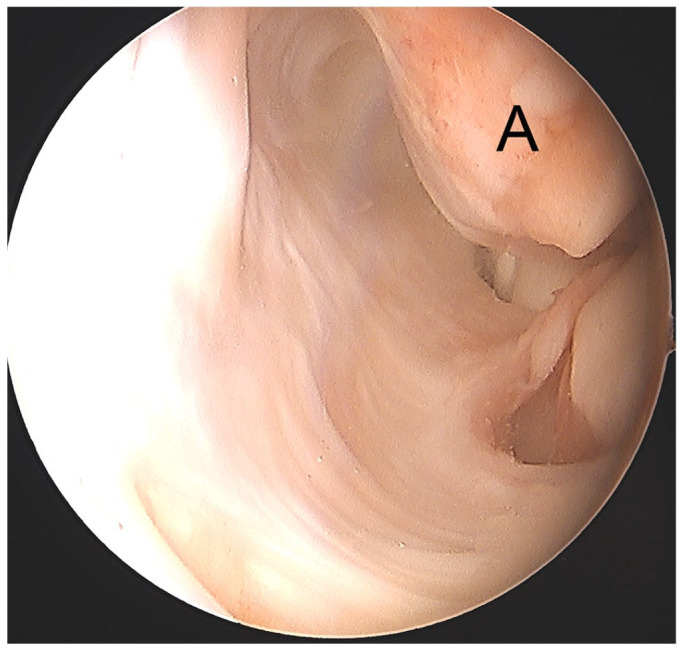
Right ankle arthroscopy: chronic avulsion of the lateral ligament complex (A – distal fibular tip).
Fig. 2.
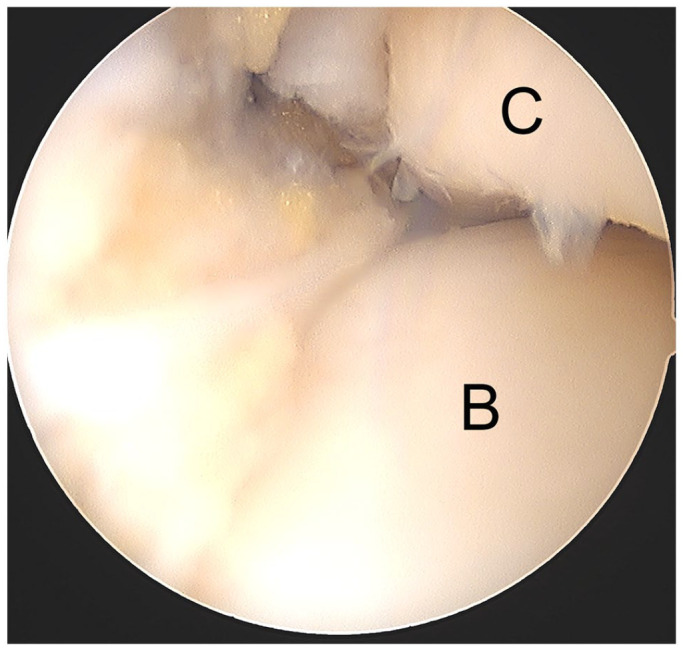
Right ankle arthroscopy: re-attachment of the lateral ligament complex after the author’s arthro-Brostrom procedure (B – talus; C – tibial plafond).
It is the authors’ opinion that there are two kind of surgical treatment for CAI:
One where the surgeon reproduces the normal anatomy either by re-insertion of the ligament or replacement with a tendon graft.
Another where the surgeon creates a situation that allows the ligament to heal with its normal length and tensile conditions. The purpose is to make a kind of functional crutch to the ligament.
Nowadays we have the means to use these principles (anatomic or functional crutch) and apply them either with an open surgery, a percutaneous procedure or an arthroscopic operation. In the Brostrom–Gould procedure we have both principles. The re-insertion of the ligament is an anatomic repair and the reinforcement with the extensor retinaculum acts as the functional crutch or seatbelt. Some of the arthroscopic procedures described will rely on the tensioning and insertion of the extensor retinaculum on the fibula to achieve the repair and consequent healing of the ligament.
The ligament reconstruction with tendon graft is also an anatomic repair, being crucial that the graft has the same orientation, insertion and tension of the natural ligaments. This can be done open, percutaneously or arthroscopically. This will be strictly anatomic and can be used in patients with poor ligament quality. As endoscopic skill became more universal, the ability to perform this procedure with the arthroscope is possible and reproducible with less aggression to the patients. The short-term clinical outcomes are better,29 with no significant difference in complication rate,29,30 so we can predict that in the future the recommended method for surgical treatment of CAI will be arthroscopic.
Recently, the use of an artificial ligament (fibertape) as checkrein or a seatbelt to augment the repair and shorten the recovery time has been proposed. The idea may sound appealing but still needs further validation. It can also be used in situations where direct repair with the tissue available locally may not be possible. It can also be used as an alternative to the tendon graft in ligament reconstruction. As it is an artificial ligament, there is the risk of over tightness and rigidity and it should not be placed in an intra-articular position.
In high-level athletes and for acute grade III lesions there is a trend for early surgery on mechanical instabilities.16
Post-operative follow-up
Consensus
Practitioners agree that after surgery patients will need physiotherapy to accelerate recovery and improve functional results. The return to normal activity, including sport activities, may occur around four months post-operatively.
Controversy
The need for immobilization after surgery is still a question open to debate. Some will use a cast immobilization for a period as long as three weeks, others (like the authors) advocate only the use of a soft dressing. The non-weight-bearing period also varies from surgeon to surgeon, with the authors authorizing full weight-bearing as tolerated around six weeks post-operatively. Also, consensus had not been reached on the timing to start mobilization and physiotherapy.
The authors’ post-operative care includes a soft dressing, allowing immediate mobilization, within three weeks of discharge of the operated ankle. The beginning of physiotherapy is at two weeks post-operatively and the return to sports or heavy work around four months.
Syndesmosis instability
Isolated syndesmosis injuries, commonly referred to as high ankle sprains, are relatively uncommon.31 They are usually associated with other lesions of the lateral ankle ligaments and are present in up to 20% of all ankle sprains32,33 and about 5% will need surgery.34 These lesions can be associated with important morbidity and delayed return to sports, compared to an isolated lateral ankle sprain,31,35,36 representing a challenge for both physician and athlete. This section will consider syndesmotic lesions, with or without associated ankle ligamentous injuries, excluding association with ankle fractures.
Anatomy
The syndesmosis is an essential stabilizer of the ankle joint and consists of a complex ligamentous structure with three different portions: the anterior inferior tibiofibular ligament (AITFL); the interosseous ligament (IOL); and the posterior inferior tibiofibular and the transverse ligaments (PITFL and TL). The posterior syndesmosis plays the most important role providing 40–45% of the resistance to diastasis, while the AITFL provides around 35%.37 Major injuries of two of the syndesmosis components represent a loss of more than 50% of resistance to diastasis37 and may result in instability.
Clinical features
Typically, syndesmosis injuries result from a forced external rotation of the foot on a dorsiflexed ankle.38 Hyperdorsiflexion and inversion with external rotation are also possible mechanisms of injury. The incidence is higher in contact sports38 and sports where the foot is locked in a boot such as skiing or ice hockey.35 They are frequently overlooked on the emergency room and up to 20% are missed on the first visit.39 Misdiagnosis or late diagnosis are associated with poorer outcomes but the lesion itself is associated with high morbidity, activity-related pain, poor functional outcomes, instability, stiffness and heterotopic ossification.40,41
Clinical examination
Consensus
A considerable number of clinical tests for syndesmosis injuries have been described: external rotation stress test, Cotton test, dorsiflexion-compression test, squeeze test, crossed-leg test, fibular translation and AITFL palpation. The external rotation test shows good interrater reliability compared to others.42
Controversy
Nonetheless, the reports on clinical tests show conflicting results. While some present unsatisfactory predictive positive values43 and low sensitivity,44 others show highly significant relation between clinical and MRI findings.45 Due to the questionable reliability and accuracy of clinical examination, if there is clinical suspicion of a syndesmosis lesion, especially an unstable lesion, additional imaging and/or arthroscopy are mandated for accurate diagnosis and treatment.
Imaging and diagnosis
Consensus
Standard radiographs are part of ankle trauma evaluation, especially for fracture exclusion, applying the Ottawa criteria. Identification of a complete syndesmotic disruption on X-ray is feasible, but plain radiographs may have little value for subtle lesions.
Controversy
Radiographic diagnosis of syndesmosis ruptures traditionally will imply some measurements made on plain radiographs:
Increased tibiofibular clear space (TFCS), measured 10 mm proximally to the tibial plafond, on anteroposterior (AP) or mortise view, more than 6 mm (most reliable indicator of syndesmosis lesion).
- Reduced tibiofibular overlap (TFO)
- AP view less than 6 mm
- Mortise view less than 1 mm
Enlarged medial clear space (MCS) between talus and medial malleolus – indicates medial collateral ligament lesion.
However, these radiologic measurements show poor reproducibility, with 82% of sensibility and 75% of specificity for TFCS and 36% and 78% for TFO. Furthermore, results fail to correlate with MRI findings.46 Even with a syndesmosis ligament rupture the tibiofibular distance can remain intact. Stress radiographs, using the Télos apparatus, with forced external rotation or gravity, can detect latent diastasis in case of full syndesmosis tear but exhibit low reliability.43,46 Computerized tomography (CT) scan is a useful tool to assess tibiofibular diastasis, fibular rotation and joint asymmetry, but shows low sensitivity.47 MRI is an essential tool, showing very high sensitivity and specificity in identification of syndesmotic injuries.47
There are few reports on the use of weight-bearing CT scan18 and its clinical role is still not clear. Dynamic ultrasound is a promising technique but is very examiner dependent, has a steep learning curve and low reproducibility. Ultimately, a syndesmotic lesion can be definitely confirmed by ankle arthroscopy, with a dynamic evaluation that can detect subtle displacement in multiple planes and also guide the surgeon to obtain an anatomic reduction.
Ankle arthroscopy has been the gold standard diagnostic tool for syndesmotic ligament rupture, but a current report show that MRI has similar accuracy47 without the invasiveness of a surgical procedure.
Classification
Consensus
There are numerous classifications proposed for syndesmotic lesions, usually classifying the lesion into three grades. The 2016 ESSKA-AFAS consensus on syndesmotic injuries43 recommended distinguishing, on acute lesions, between stable and unstable. A stable lesion is characterized by an AITFL lesion, with or without IOL, with a competent deltoid ligament. An unstable lesion usually combines with deltoid ligament lesion and is divided into latent or frank diastasis. The latent diastasis combines the AITFL rupture with or without IOL and deltoid ligament rupture. In frank diastasis all the syndesmotic and deltoid ligaments are ruptured. The definition of stability is essential to guide us through the treatment algorithm and a proper classification method is lacking.
Treatment
Consensus
There is consensus that a stable lesion (classic grade I) can be treated with conservative measures, including a non-weight-bearing period followed by protected partial weight-bearing (with walking boot) and a rehabilitation protocol. Progress through these phases is determined by symptom severity and individual response to treatment. An unstable lesion (classic grade III) should always be surgical to avoid long-term disability and chronic instability.
Ankle arthroscopy remains essential for diagnosis and treatment and it is vital to decide which lesions are to be repaired. Numerous instability assessment methods have been described, usually with accessory tools that measure the syndesmosis gap (e.g. 3.5 mm shaver canula or a metallic tools) (Fig. 3). Passage of a 3 mm spherical probe during external rotation indicates very high likelihood of rupture of both the AITFL and the IOL,48 against previous reports classifying unstable lesions when diastasis was greater than 2 mm. Additionally, half of these lesions can present with concomitant intra-articular pathologies (osteochondral lesions, other ligamentous rupture or loose bodies) with 19% needing additional treatment,49 reinforcing the role of arthroscopy not only for diagnosis but also for concomitant treatment. It is also an excellent tool to evaluate anatomic reduction and residual diastasis.
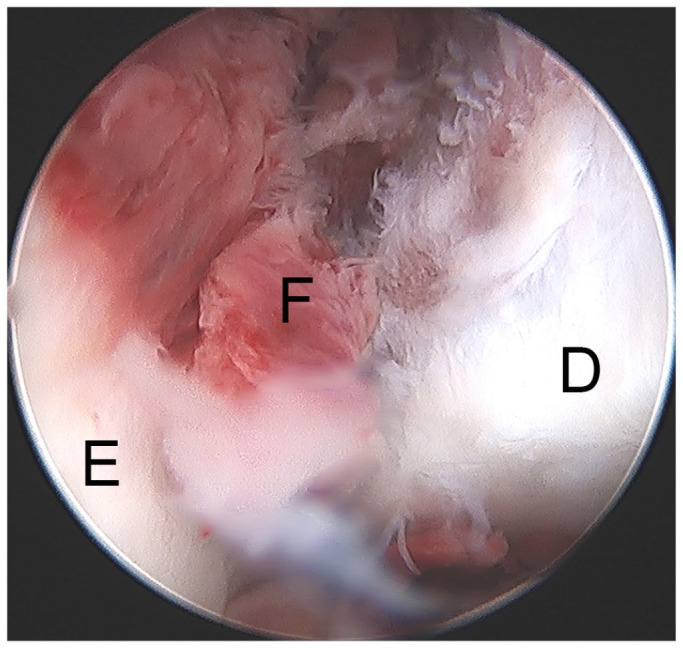
Fig. 3.
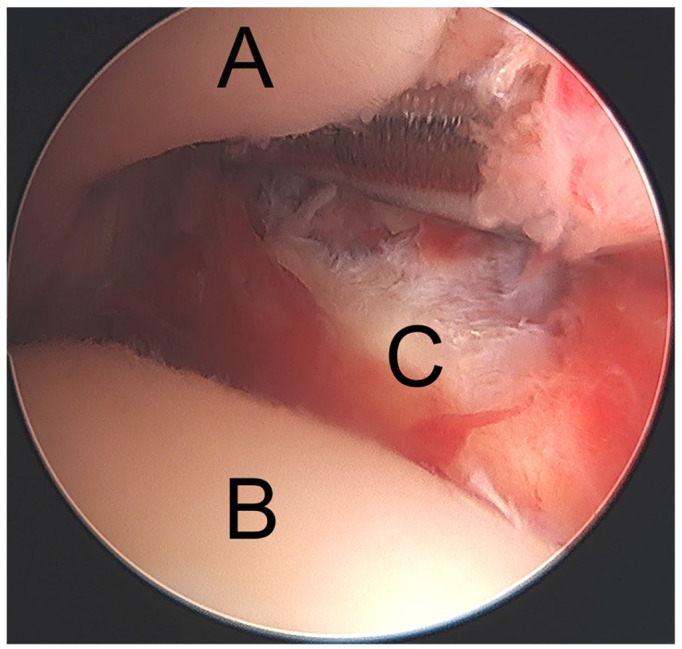
Left ankle arthroscopy: syndesmosis lesion diagnosis using a 4.5 mm shaver cannula that can penetrate through the syndesmotic space (A – tibial plafond; B – talus; C – fibula).
Controversy
The controversy in the treatment decision algorithm remains on how to distinguish between a stable and an unstable lesion, especially on subtle or latent unstable lesions (classic grade II). As previously said, an association with a Deltoid ligament lesion is highly predictive of an unstable injury.45
The surgical options vary between a rigid fixation, with screws, and a dynamic fixation with suture-button-like materials. Screws have been the gold standard procedure for decades but have some associated complications such as screw loosening or breakage. Moreover, some surgeons advocate screw removal, with the inherent risk of instability recurrence. Dynamic fixation was created to solve some of these problems, letting some physiologic syndesmotic movement occur, permitting early weight-bearing, reducing the risk of breakage and the need for implant removal.
Clinical outcomes appear to be better at two and five years for suture-button patients with less osteoarthritis50,51 and with fewer complications and reoperations.52 A recent meta-analysis on biomechanical comparison between fixation options shows superior strength for screw fixation but similar load and rotation to failure compared to flexible systems.53 Suture-button constructions provide some degree of micro-motion, thus mimicking physiologic mobility which can be helpful for ligament healing.53 The flexible implants also provide a little more forgiveness for implant malposition, a not so rare complication for syndesmotic screws.52,54 To avoid rotational instability, AITFL augmentation with suture-tape materials has been described55 for use in high-level athletes and active patients with ligamentous laxity, connective tissue disorders and history of joint instability.55,56
The authors routinely use arthroscopy for syndesmosis lesions treatment and, in terms of fixation, favour the use of suture-button options except in contact sports athletes for whom a mixed technique with a screw and a suture-button is used. The screw will give a more solid temporary fixation. After an early removal of the screw, a more flexible fixation remains with the suture-button system.
As seen before, for acute lesions, ankle arthroscopy can be an important tool for diagnostic purposes and to check the final reduction after surgery, but the repair can be achieved without any direct approach to the joint. On the other hand, for chronic lesions, it is essential to conduct a meticulous debridement of the inferior tibiofibular joint to allow complete reduction of the articulation. This can be done arthroscopically. In terms of fixation, the principles are the same but a more solid option should be chosen, with double screws or double suture-button construct or mixed options. Some authors describe techniques with tendon graft, but these options are usually unnecessary.
Medial instability
Isolated deltoid ligament injuries account for about 3–4% of all ankle ligament injuries,57 and usually result from an eversion trauma. As in lateral instability, if not correctly addressed, a deltoid lesion can evolve into chronic medial ankle instability. This section will focus mainly on isolated lesions, although deltoid lesions have a close and important relation with other ligamentous lesions, especially with syndesmotic ruptures.
Anatomy
Consensus
The deltoid ligament complex spreads fan-shaped over the medial part of the ankle joint. It plays an essential role in terms of stability against valgus and rotational forces. It is clearly divided into two layers (deep and superficial).58
Controversy
Some authors describe six distinct components of the deltoid ligament, four superficial and two deep ligaments. The superficial ligaments (tibiospring ligament [TSL], tibionavicular ligament [TNL], superficial posterior tibiotalar ligament [STTL] and tibiocalcaneal ligament [TCL]) confer stability both to the ankle and subtalar joints, while the deep components (deep posterior tibiotalar ligament [PTTL] and anterior tibiotalar ligament [ATTL]) are shorter and thicker and cross only the ankle joint.58
The anterior superficial deltoid (TSL) inserts on the spring ligament originating a single functional unit to provide medial ankle stability and support to the medial arch of the foot. For some, the TSL and the spring ligament are the same structure. This notion is important in understanding the physiopathology of medial instability and some chronic conditions such as the acquired flat foot.
Clinical features
Consensus
The main causes of isolated deltoid ligament lesions are pronation (eversion) and external rotation forces on the ankle. When combined with other ligament lesions, deltoid rupture can be caused by other trauma mechanisms, like the common supination trauma. Clinical suspicion must be raised on physical examination. The patient will have pain and tenderness, local swelling and ecchymosis on the anteromedial part of the ankle. Weight-bearing may be impossible. Clinical signs such as the drawer test or talar tilt test can be used, usually only after some days due to acute pain.
Controversy
If not correctly treated, some of these patients will evolve chronic medial ligament instability, whereas an accurate diagnosis might be challenging. In these cases, a feeling of instability might be present (‘medial giving way’), specially on irregular terrain. Tenderness at the medial gutter of the ankle joint must arouse suspicion. A flat foot with prominence of the medial malleolus, pronounced hindfoot valgus (with concomitant lateral pain from subfibular impingement) and pronation of the affected foot can be observed, but the deformity can be actively corrected (for instance, with the heel-rise test).58 With this test, we can differentiate these cases from the typical adult acquired flat foot (AAFF) or tibialis posterior tendon dysfunction (TPTD).
Nevertheless, it has been questioned whether AAFF is caused by lesion or insufficiency of the tibialis posterior tendon, because in numerous cases the tendon is found intact. Some authors believe that the index event that produces AAFF is the lesion/insufficiency of the spring ligament.59 It is our conviction that the cause of flatfoot deformity is the incompetence of the functional unit composed by the anterior superficial deltoid and the spring ligament. This notion would give a new importance to the diagnosis and treatment of acute medial ligament lesions.
Imaging
Consensus
Similar to other ligamentous injures, radiographs are essential to exclude fractures. Widening of the medial ankle clear space can be found. US is an important tool for an initial screening of a suspected acute deltoid ligament rupture.
Controversy
In the acute phase, stress radiographs, like gravitational X-rays, were a very popular tool in the past, but they are falling into disuse because of the lack of additional information and the potential to further damage the injured structures.58,60 In the chronic medial ankle instability, standard weight-bearing radiographs can show segmental deformities and associated lesions (such as osteochondral lesions (OCL), bony impingements, osteoarthritic changes). Contralateral comparison may be essential for more subtle injuries.
In both acute and chronic medial ankle instability MRI is an important tool to characterize the extent and location of the rupture, and to identify concomitant lesions and affection of adjacent ligaments or tendons. It can help in pre-operative planning and impact on the treatment protocol. However, as in other ligamentous deficits, MRI is less reliable in detecting ligament rupture/insufficiency compared to arthroscopic assessment,60 especially due to the dynamic assessment of the biomechanics. Weight-bearing CT has been frequently reported as an important asset to the study of flatfoot deformity. It can also play a role in chronic medial ligament instability assessment.18
Non-operative treatment
Consensus
The large majority of acute ruptures of the deltoid can be treated conservatively.
Controversy
Due to the medial ligament dimension, anatomic and histologic features and bony morphology of the joint, the deltoid ligament has an inherent capacity to heal. The problem emerges when there is incompetent healing. This would be more frequent with an associated syndesmotic rupture. The modalities of conservative treatment vary from skilful neglect to cast immobilization from four to six weeks. The option with the greatest consensus is an early functional treatment associated with six weeks bracing to avoid eversion (similar to the treatment for lateral ligament ruptures). Without specific treatment some patients will develop chronic instability with pain and progressive valgus deformity of the hindfoot, especially in patients with simultaneous spring ligament injury, that is, patients with important anterior superficial deltoid rupture.
Surgical treatment
Consensus
As in other ankle ligamentous lesions, arthroscopy plays an important role both with diagnostic or therapeutic purposes, as arthroscopy is the most reliable diagnostic method and is recommended for treatment of the majority of intra-articular lesions. It is also important to assess talar reduction after syndesmotic fixation, where sometimes there is a deltoid deep bundle interposition that is causing malposition (Fig. 4). So, the use of arthroscopy during the surgical treatment of these patients can be extremely helpful.
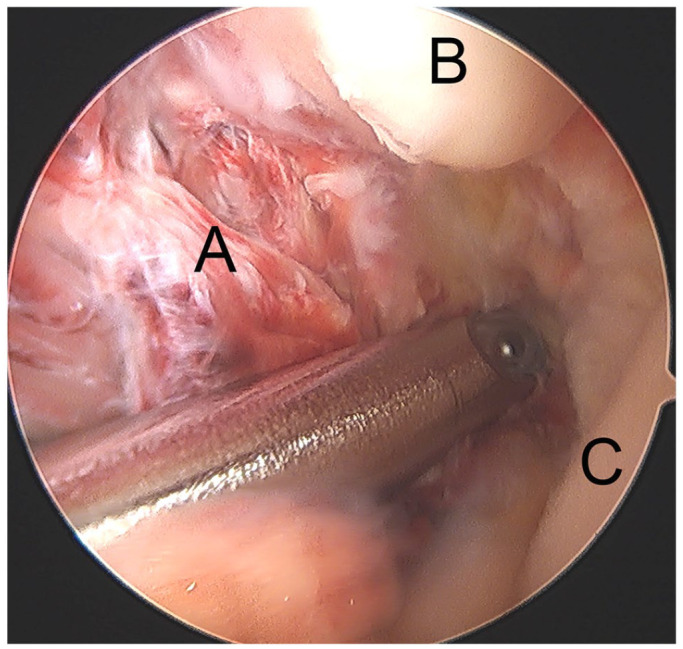
Fig. 4.
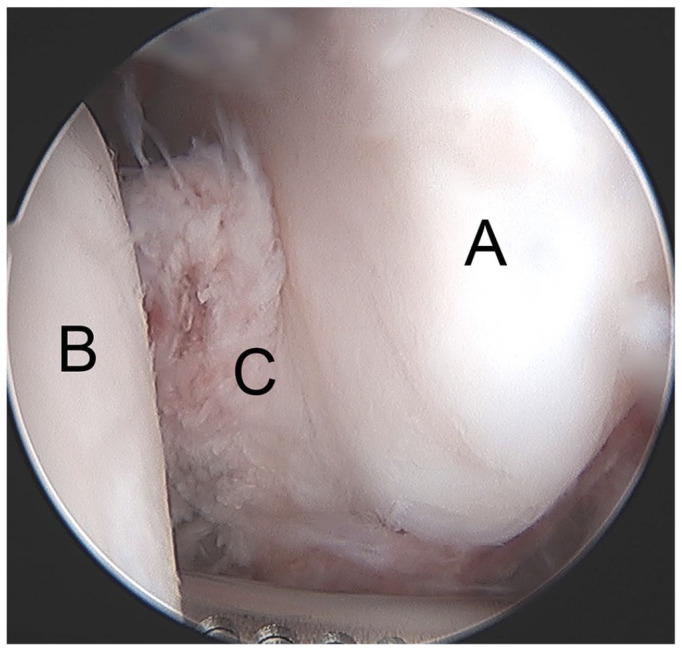
Right ankle arthroscopy: a deltoid ligament acute rupture (C) with interposition between the talus (B) and medial malleolus (A). This is one of the causes of inadequate reduction of bimalleolar equivalent fractures (A – tibial plafond; B – talus; C – fibula).
Controversy
Surgical repair should be considered in combined injuries, such as to the deltoid ligament and the spring ligament with or without involvement of the tibialis posterior tendon, or with the syndesmotic ligament in the acute phase (Fig. 5 and Fig. 6). The open surgery techniques for deltoid ligament repair are well documented. Most surgeons carry out a direct suture of the ligament, individualizing each layer, and, if necessary, augmenting with suture anchors.
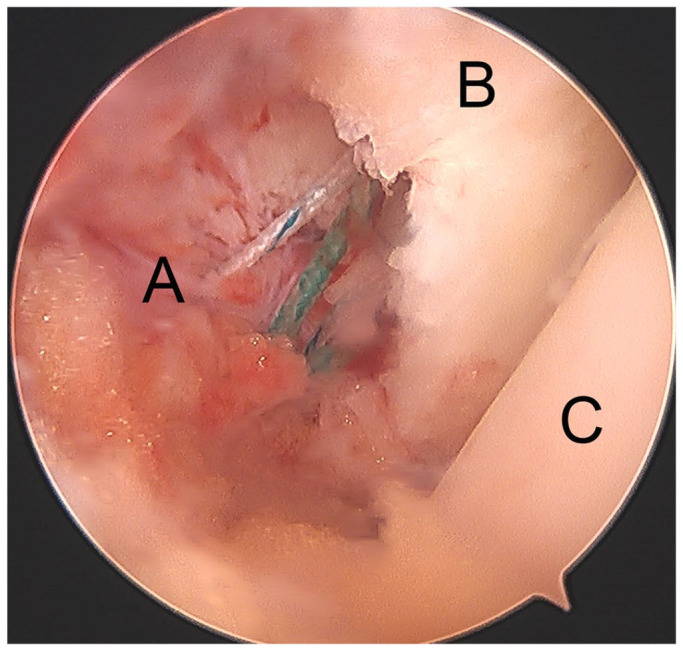
Fig. 5.
Right ankle arthroscopy: multiple ligamentar lesion with and acute deltoid rupture (C) and syndesmosis rupture (see Fig. 6). (A – medial malleolus; B – talus; C – Deltoid ligament).
Fig. 6.
Right ankle arthroscopy: syndesmosis disruption (F – front view of the syndesmosis). (tibial plafond; E – fibula; F syndesmosis).
Hintermann61 classified the deltoid ligament lesion into three types, depending on the anatomic location on the anterior bundles of the ligament:
Type I – Injuries at the proximal part of the deltoid
Type II – Injuries at the intermediate part of the deltoid
Type III – Injuries at the distal part of the deltoid and spring ligaments
Depending on the type of lesion, Hintermann61 proposed three slightly different techniques. For type I lesions, a suture anchor is placed on the medial malleolus where the detached ligament is re-inserted (both tibionavicular and tibiospring ligaments are re-tensioned). For type II lesions, the deep part of the ligament is fixed to the medial malleolus and the superficial part is fixed distally to the superior edge of the navicular tuberosity. In type III lesions, a bony anchor is used to fix the detached deltoid and spring ligaments to the navicular tuberosity.
In revision cases or when quality of the remaining ligament is insufficient, a reconstruction using a free tendon graft can be considered. As an alternative, augmentation with artificial ligament (fibertapes) is gaining popularity,62 as in lateral instability, but requires further scientific validation. When there is a fixed deformity (hindfoot valgus or forefoot abduction) additional procedures should be considered: a medial sliding calcaneal osteotomy or a lateral calcaneal lengthening osteotomy.
With the advent and benefits of ankle arthroscopy, descriptions of deltoid ligament arthroscopic repairs are beginning to appear in the literature.63,64 The senior author developed a technique inspired by the arthroscopic Brostrom procedure used for repair of lateral ankle instability. A suture anchor is placed on the anterior face of the medial malleolus using arthroscopic means and the sutures are passed through an accessory portal, grabbing the extensor retinaculum and the remaining ligament, in the same way as is done for the lateral ligament (Fig. 7 and Fig. 8). The rationale behind this technique is to take advantage of the natural ability of the ligament to heal and create a functional crutch that allows the ligament to heal with the normal tension and length and, also, to focus on the more important part of the repair, which is the restoration of a normal anterior superficial deltoid/spring ligament complex.
Fig. 7.
Left ankle arthroscopy: acute deltoid rupture of the anteromedial bundle (A) with a wide space between the talus (C) and the medial malleolus (B).
Fig. 8.
Left ankle arthroscopy: the result of the arthroscopic repair with anchor and correction of the medial clear space (A – deltoid ligament; B – medial malleolus; C – talus).
Conclusion
Ankle ligamentous lesions, due to their incidence, are important conditions. Although most cases are benign, a group of patients will have chronic complaints. Lateral ligament ruptures form the large majority of cases due mainly to the bony anatomy of the joint, but the other ligaments should not be overlooked or minimized, especially in the case of combined lesions. Ligaments have an inherent ability to heal but, if not treated correctly, the healing may be incompetent in terms of length and strength creating a ligament insufficiency – instability. Acute isolated lesions are treated with conservative means. Athletes and patients with risk factors may benefit from early surgery. Combined lesions are candidates for surgery. Chronic cases should be operated. The major challenge is to identify, in the acute phase, the patients who will evolve chronic instability and consider early surgery. This kind of lesion frequently has concomitant intra-articular lesions that need simultaneous treatment. Ankle arthroscopy plays an important role in the treatment of ankle instability (lateral, medial and syndesmotic) due to its diagnostic power and usefulness to treat concomitant lesions. Arthroscopic instability repair is becoming more popular with promising results in terms of outcomes, reproducibility and low morbidity. Instability of all three sets of ankle ligament groups, if left untreated, will eventually develop into ankle arthritis.
Footnotes
ICMJE Conflict of interest statement: NCR reports consultancy for Arthrex, payment for lectures including service on speakers’ bureaus for Arthrex and Stryker, and payment for development of educational presentations from Arthrex, Stryker and Sociedade Portuguesa de Medicina Desportiva, all outside the submitted work.
JC declares no conflict of interest relevant to this work.
OA licence text: This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. van Rijn RM, van Os AG, Bernsen RMD, Luijsterburg PA, Koes BW, Bierma-Zeinstra SMA. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med 2008;121:324–331.e6. [DOI] [PubMed] [Google Scholar]
- 2. Fong DTP, Hong Y, Chan LK, Yung PSH, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med 2007;37:73–94. [DOI] [PubMed] [Google Scholar]
- 3. Peters JW, Trevino SG, Renstrom PA. Current topic review chronic lateral ankle instability. Foot Ankle 1991;12:182–191. [DOI] [PubMed] [Google Scholar]
- 4. Molinier F, Benoist J, Colin F, et al. Does antero-lateral ankle impingement exist? Orthop Traumatol Surg Res 2017;103:S249–S252. [DOI] [PubMed] [Google Scholar]
- 5. Freeman MA. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br 1965;47:669–677. [PubMed] [Google Scholar]
- 6. Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train 2002;37:364–375. [PMC free article] [PubMed] [Google Scholar]
- 7. Lohrer H, Nauck T, Gehring D, Wissler S, Braag B, Gollhofer A. Differences between mechanically stable and unstable chronic ankle instability subgroups when examined by arthrometer and FAAM-G. J Orthop Surg Res 2015;10:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hiller CE, Kilbreath SL, Refshauge KM. Chronic ankle instability: evolution of the model. J Athl Train 2011;46:133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vega J, Peña F, Golanó P. Minor or occult ankle instability as a cause of anterolateral pain after ankle sprain. Knee Surg Sports Traumatol Arthrosc 2016;24:1116–1123. [DOI] [PubMed] [Google Scholar]
- 10. Pourkazemi F, Hiller CE, Raymond J, Nightingale EJ, Refshauge KM. Predictors of chronic ankle instability after an index lateral ankle sprain: a systematic review. J Sci Med Sport 2014;17:568–573. [DOI] [PubMed] [Google Scholar]
- 11. Thompson JY, Byrne C, Williams MA, Keene DJ, Schlussel MM, Lamb SE. Prognostic factors for recovery following acute lateral ankle ligament sprain: a systematic review. BMC Musculoskelet Disord 2017;18:421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gribble PA. Evaluating and differentiating ankle instability. J Athl Train 2019;54:617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rosen AB, Ko J, Brown CN. Diagnostic accuracy of instrumented and manual talar tilt tests in chronic ankle instability populations. Scand J Med Sci Sports 2015;25:e214–e221. [DOI] [PubMed] [Google Scholar]
- 14. Terada M, Bowker S, Hiller CE, Thomas AC, Pietrosimone B, Gribble PA. Quantifying levels of function between different subgroups of chronic ankle instability. Scand J Med Sci Sports 2017;27:650–660. [DOI] [PubMed] [Google Scholar]
- 15. Guerra-Pinto F, Côrte-Real N, Mota Gomes T, et al. Rotational instability after anterior talofibular and calcaneofibular ligament section: the experimental basis for the ankle pivot test. J Foot Ankle Surg 2018;57:1087–1091. [DOI] [PubMed] [Google Scholar]
- 16. Michels F, Pereira H, Calder J, et al. ; ESSKA-AFAS Ankle Instability Group. Searching for consensus in the approach to patients with chronic lateral ankle instability: ask the expert. Knee Surg Sports Traumatol Arthrosc 2018;26:2095–2102. [DOI] [PubMed] [Google Scholar]
- 17. Bosman HA, Robinson AHN. Treatment of ankle instability with an associated cavus deformity. Foot Ankle Clin 2013;18:643–657. [DOI] [PubMed] [Google Scholar]
- 18. Conti MS, Ellis SJ. Weight-bearing CT scans in foot and ankle surgery. J Am Acad Orthop Surg 2020;28:e595–e603. [DOI] [PubMed] [Google Scholar]
- 19. Doherty C, Bleakley C, Delahunt E, Holden S. Treatment and prevention of acute and recurrent ankle sprain: an overview of systematic reviews with meta-analysis. Br J Sports Med 2017;51:113–125. [DOI] [PubMed] [Google Scholar]
- 20. McKeon PO, Wikstrom EA. Sensory-targeted ankle rehabilitation strategies for chronic ankle instability. Med Sci Sports Exerc 2016;48:776–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wikstrom EA, McKeon PO. Predicting balance improvements following STARS treatments in chronic ankle instability participants. J Sci Med Sport 2017;20:356–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cao Y, Hong Y, Xu Y, Zhu Y, Xu X. Surgical management of chronic lateral ankle instability: a meta-analysis. J Orthop Surg Res 2018;13:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Guelfi M, Zamperetti M, Pantalone A, Usuelli FG, Salini V, Oliva XM. Open and arthroscopic lateral ligament repair for treatment of chronic ankle instability: a systematic review. Foot Ankle Surg 2018;24:11–18. [DOI] [PubMed] [Google Scholar]
- 24. Lu A, Wang X, Huang D, et al. The effectiveness of lateral ankle ligament reconstruction when treating chronic ankle instability: a systematic review and meta-analysis. Injury 2020;51:1726–1732. [DOI] [PubMed] [Google Scholar]
- 25. Brambilla L, Bianchi A, Malerba F, Loppini M, Martinelli N. Lateral ankle ligament anatomic reconstruction for chronic ankle instability: allograft or autograft? A systematic review. Foot Ankle Surg 2020;26:85–93. [DOI] [PubMed] [Google Scholar]
- 26. Komenda GA, Ferkel RD. Arthroscopic findings associated with the unstable ankle. Foot Ankle Int 1999;20:708–713. [DOI] [PubMed] [Google Scholar]
- 27. Hintermann B, Boss A, Schäfer D. Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med 2002;30:402–409. [DOI] [PubMed] [Google Scholar]
- 28. Corte-Real NM, Moreira RM. Arthroscopic repair of chronic lateral ankle instability. Foot Ankle Int 2009;30:213–217. [DOI] [PubMed] [Google Scholar]
- 29. Brown AJ, Shimozono Y, Hurley ET, Kennedy JG. Arthroscopic versus open repair of lateral ankle ligament for chronic lateral ankle instability: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 2020;28:1611–1618. [DOI] [PubMed] [Google Scholar]
- 30. Zhi X, Lv Z, Zhang C, Kong C, Wei S, Xu F. Does arthroscopic repair show superiority over open repair of lateral ankle ligament for chronic lateral ankle instability: a systematic review and meta-analysis. J Orthop Surg Res 2020;15:355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lubberts B, D’Hooghe P, Bengtsson H, DiGiovanni CW, Calder J, Ekstrand J. Epidemiology and return to play following isolated syndesmotic injuries of the ankle: a prospective cohort study of 3677 male professional footballers in the UEFA Elite Club Injury Study. Br J Sports Med 2019;53:959–964. [DOI] [PubMed] [Google Scholar]
- 32. McCollum GA, van den Bekerom MPJ, Kerkhoffs GMMJ, Calder JDF, van Dijk CN. Syndesmosis and deltoid ligament injuries in the athlete. Knee Surg Sports Traumatol Arthrosc 2013;21:1328–1337. [DOI] [PubMed] [Google Scholar]
- 33. Roemer FW, Jomaah N, Niu J, et al. Ligamentous injuries and the risk of associated tissue damage in acute ankle sprains in athletes: a cross-sectional MRI study. Am J Sports Med 2014;42:1549–1557. [DOI] [PubMed] [Google Scholar]
- 34. Mulcahey MK, Bernhardson AS, Murphy CP, et al. The epidemiology of ankle injuries identified at the National Football League Combine, 2009–2015. Orthop J Sports Med 2018;6:2325967118786227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wright RW, Barile RJ, Surprenant DA, Matava MJ. Ankle syndesmosis sprains in national hockey league players. Am J Sports Med 2004;32:1941–1945. [DOI] [PubMed] [Google Scholar]
- 36. Vancolen SY, Nadeem I, Horner NS, Johal H, Alolabi B, Khan M. Return to sport after ankle syndesmotic injury: a systematic review. Sports Health 2019;11:116–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ogilvie-Harris DJ, Reed SC, Hedman TP. Disruption of the ankle syndesmosis: biomechanical study of the ligamentous restraints. Arthroscopy 1994;10:558–560. [DOI] [PubMed] [Google Scholar]
- 38. Delahunt E, Farrell G, Boylan A, et al. Mechanisms of acute ankle syndesmosis ligament injuries in professional male rugby union players: a systematic visual video analysis. Br J Sports Med. 2020. doi: 10.1136/bjsports-2020-102281 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 39. Tourné Y, Molinier F, Andrieu M, Porta J, Barbier G. Diagnosis and treatment of tibiofibular syndesmosis lesions. Orthop Traumatol Surg Res 2019;105:S275–S286. [DOI] [PubMed] [Google Scholar]
- 40. Taylor DC, Englehardt DL, Bassett FH, III. Syndesmosis sprains of the ankle: the influence of heterotopic ossification. Am J Sports Med 1992;20:146–150. [DOI] [PubMed] [Google Scholar]
- 41. Kent S, Yeo G, Marsland D, et al. Delayed stabilisation of dynamically unstable syndesmotic injuries results in worse functional outcomes. Knee Surg Sports Traumatol Arthrosc 2020;28:3347–3353. [DOI] [PubMed] [Google Scholar]
- 42. Alonso A, Khoury L, Adams R. Clinical tests for ankle syndesmosis injury: reliability and prediction of return to function. J Orthop Sports Phys Ther 1998;27:276–284. [DOI] [PubMed] [Google Scholar]
- 43. van Dijk CN, Longo UG, Loppini M, et al. Classification and diagnosis of acute isolated syndesmotic injuries: ESSKA-AFAS consensus and guidelines. Knee Surg Sports Traumatol Arthrosc 2016;24:1200–1216. [DOI] [PubMed] [Google Scholar]
- 44. de César PC, Ávila EM, de Abreu MR. Comparison of magnetic resonance imaging to physical examination for syndesmotic injury after lateral ankle sprain. Foot Ankle Int 2011;32:1110–1114. [DOI] [PubMed] [Google Scholar]
- 45. Calder JD, Bamford R, Petrie A, McCollum GA. Stable versus unstable grade II high ankle sprains: a prospective study predicting the need for surgical stabilization and time to return to sports. Arthroscopy 2016;32:634–642. [DOI] [PubMed] [Google Scholar]
- 46. Anand Prakash A. Syndesmotic stability: is there a radiological normal? A systematic review. Foot Ankle Surg 2018;24:174–184. [DOI] [PubMed] [Google Scholar]
- 47. Chun DI, Cho JH, Min TH, et al. Diagnostic accuracy of radiologic methods for ankle syndesmosis injury: a systematic review and meta-analysis. J Clin Med 2019;8:968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Guyton GP, DeFontes K, III, Barr CR, Parks BG, Camire LM. Arthroscopic correlates of subtle syndesmotic injury. Foot Ankle Int 2017;38:502–506. [DOI] [PubMed] [Google Scholar]
- 49. Rellensmann K, Behzadi C, Usseglio J, et al. Acute, isolated and unstable syndesmotic injuries are frequently associated with intra-articular pathologies. Knee Surgery, Sport Traumatol Arthrosc, 2020. 10.1007/s00167-020-06141-y [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 50. Ræder BW, Figved W, Madsen JE, Frihagen F, Jacobsen SB, Andersen MR. Better outcome for suture button compared with single syndesmotic screw for syndesmosis injury: five-year results of a randomized controlled trial. Bone Joint J 2020;102-B:212–219. [DOI] [PubMed] [Google Scholar]
- 51. Gan K, Xu D, Hu K, Wu W, Shen Y. Dynamic fixation is superior in terms of clinical outcomes to static fixation in managing distal tibiofibular syndesmosis injury. Knee Surg Sports Traumatol Arthrosc 2020;28:270–280. [DOI] [PubMed] [Google Scholar]
- 52. Grassi A, Samuelsson K, D’Hooghe P, et al. Dynamic stabilization of syndesmosis injuries reduces complications and reoperations as compared with screw fixation: a meta-analysis of randomized controlled trials. Am J Sports Med 2020;48:1000–1013. [DOI] [PubMed] [Google Scholar]
- 53. Lee JS, Curnutte B, Pan K, Liu J, Ebraheim NA. Biomechanical comparison of suture-button, bioabsorbable screw, and metal screw for ankle syndesmotic repair: a meta-analysis. Foot Ankle Surg 2019;2020:6–11. [DOI] [PubMed] [Google Scholar]
- 54. Sanders D, Schneider P, Taylor M, Tieszer C, Lawendy AR; Canadian Orthopaedic Trauma Society. Improved reduction of the tibiofibular syndesmosis with TightRope compared with screw fixation: results of a randomized controlled study. J Orthop Trauma 2019;33:531–537. [DOI] [PubMed] [Google Scholar]
- 55. Regauer M, Mackay G, Lange M, Kammerlander C, Böcker W. Syndesmotic InternalBraceTM for anatomic distal tibiofibular ligament augmentation. World J Orthop 2017;8:301–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kwon JY, Stenquist D, Ye M, et al. Anterior syndesmotic augmentation technique using nonabsorbable suture-tape for acute and chronic syndesmotic instability. Foot Ankle Int 2020;41:1307–1315. [DOI] [PubMed] [Google Scholar]
- 57. Ribbans WJ, Garde A. Tibialis posterior tendon and deltoid and spring ligament injuries in the elite athlete. Foot Ankle Clin 2013;18:255–291. [DOI] [PubMed] [Google Scholar]
- 58. Lötscher P, Lang TH, Zwicky L, Hintermann B, Knupp M. Osteoligamentous injuries of the medial ankle joint. Eur J Trauma Emerg Surg 2015;41:615–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Monteagudo M, Maceira E. Posterior tibial tendoscopy. Foot Ankle Clin 2015;20:1–13. [DOI] [PubMed] [Google Scholar]
- 60. Alshalawi S, Galhoum AE, Alrashidi Y, et al. Medial ankle instability: the deltoid dilemma. Foot Ankle Clin 2018;23:639–657. [DOI] [PubMed] [Google Scholar]
- 61. Hintermann B. Medial ankle instability. Foot Ankle Clin 2003;8:723–738. [DOI] [PubMed] [Google Scholar]
- 62. Pellegrini MJ, Torres N, Cuchacovich NR, Huertas P, Muñoz G, Carcuro GM. Chronic deltoid ligament insufficiency repair with Internal Brace™ augmentation. Foot Ankle Surg 2019;25:812–818. [DOI] [PubMed] [Google Scholar]
- 63. Kim JG, Gwak HC, Lee MJ, et al. Arthroscopic deltoid repair: a technical tip. J Foot Ankle Surg 2017;56:1253–1256. [DOI] [PubMed] [Google Scholar]
- 64. Acevedo JI, Kreulen C, Cedeno AA, Baumfeld D, Nery C, Mangone PG. Technique for arthroscopic deltoid ligament repair with description of safe zones. Foot Ankle Int 2020;41:605–611. [DOI] [PubMed] [Google Scholar]


