Abstract
Objectives
To investigate the perceptions, attitudes, behaviours and potential barriers to effective obesity care in the UK using data collected from people with obesity (PwO) and healthcare professionals (HCPs) in the Awareness, Care, and Treatment In Obesity maNagement–International Observation (ACTION-IO) study.
Design
UK’s PwO (body mass index of ≥30 kg/m2 based on self-reported height and weight) and HCPs who manage patients with obesity completed an online survey.
Results
In the UK, 1500 PwO and 306 HCPs completed the survey. Among the 47% of PwO who discussed weight with an HCP in the past 5 years, it took a mean of 9 years from the start of their struggles with weight until a discussion occurred. HCPs reported that PwO initiated 35% of weight-related discussions; PwO reported that they initiated 47% of discussions. Most PwO (85%) assumed full responsibility for their own weight loss. The presence of obesity-related comorbidities was cited by 76% of HCPs as a top criterion for initiating weight management conversations. The perception of lack of interest (72%) and motivation (61%) in losing weight was reported as top reasons by HCPs for not discussing weight with a patient. Sixty-five per cent of PwO liked their HCP bringing up weight during appointments. PwO reported complex and varied emotions following a weight loss conversation with an HCP, including supported (36%), hopeful (31%), motivated (23%) and embarrassed (17%). Follow-up appointments were scheduled for 19% of PwO after a weight discussion despite 62% wanting follow-up.
Conclusions
The current narrative around obesity requires a paradigm shift in the UK to address the delay between PwO struggling with their weight and discussing weight with their HCP. Perceptions of lack of patient interest and motivation in weight management must be challenged along with the blame culture of individual responsibility that is prevalent throughout society. While PwO may welcome weight-related conversations with an HCP, they evoke complex feelings, demonstrating the need for sensitivity and respect in these conversations.
Trial registration number
Keywords: general medicine (see internal medicine), public health, epidemiology, medical education & training
Strengths and limitations of this study.
Strengths include the scientific rigour in the study design and implementation.
The large number of UK respondents and the ability to directly compare the UK data to the equivalent global dataset is an additional strength.
Limitations of this study include possible response bias from the population sampled and recall bias.
Background
The causes of obesity are complex and multifaceted, encompassing biological, genetic, environmental, economic, social and psychological factors.1–3 The chronic and relapsing nature of obesity is associated with many serious physical and psychological comorbidities, reduced quality of life and increased healthcare costs.2 4–8 The WHO has recognised obesity as a disease, and the National Institute for Health and Care Excellence provides guidance on its assessment and treatment.9 More recently, it has been recognised as a risk factor for severity of COVID-19 infection.5 6 The prevalence of overweight and obesity among adults in the UK has been increasing and was 63% in 2018.7 This increase is thought to be primarily caused by people’s latent biological susceptibility interacting with a changing environment that includes more sedentary lifestyles and increased dietary abundance.1 The prevalence of adiposity in the UK population is approaching similar levels to those reported in the US (71%), Chile (74%) and Mexico (75%), which are among the highest recorded adult overweight and obesity levels in the world.8 The number of people with obesity (PwO) in the UK continues to rise, and severe and complex obesity (body mass index (BMI) ≥40 kg/m2) increased from less than 1% of the total population in 1993 to nearly 4% in 2017.10 The UK-wide National Health Service (NHS) costs attributable to overweight and obesity are projected to reach £9.7 billion by 2050, with wider societal costs estimated to reach £49.9 billion per year.11 The significant increase in the prevalence of obesity has not been matched by a proportionate expansion of continuing education on the biological basis and clinical management of obesity and training provision for healthcare professionals (HCPs), irrespective of their discipline.12 Moreover, little effort has been made to address weight stigma and societal effects of weight bias, which continue to be experienced in a consistently negative way by those who have excess weight or obesity. Current evidence demonstrates that weight stigma is widespread in the UK,13 that weight stigma is experienced in many settings14 15 and that experience of stigma is associated with negative psychosocial outcomes, increased eating, reduced engagement with physical activity and weight gain.16
The variability of causal pathways of weight gain is inherently unsuited to a ‘one size fits all’ treatment approach.1 There is a range of existing guidance to support practice and care throughout the obesity care pathway in the UK.9 17 However, the extent and range of the provision of weight management services is inconsistent and geographically dependent.18 The obesity care pathway has an important role within the whole systems approach to tackling obesity, as outlined in the Foresight’s report,1 and endorsed in the Department of Health and Social Care’s (DHSC) Call to Action19 and the Public Health England’s paper on a whole systems approach to obesity.20 The DHSC clinical policy outlines a tiered system of obesity care with a focus on public health and community advice in tier 1; primary care, community interventions and pharmacotherapy in tier 2; multi-disciplinary weight management service in tier 3 and secondary care and bariatric surgery in tier 4.21
Despite its wide global prevalence, obesity remains poorly understood by the general public and HCPs, and this contributes to the high levels of stigma associated with obesity.22 Society is continually informed through intense media coverage that obesity is simple and easily manipulated.23 This attitude contributes to greater perceptions of individual responsibility, contrary to evidence that suggests that many factors outside a person’s control influence obesity.22 23 To improve the quality and accessibility of obesity care, a better understanding of the disease and the gaps between current and optimal obesity management strategies is required. The Awareness, Care, and Treatment In Obesity maNagement–International Observation (ACTION-IO) study assessed the perceptions, attitudes and behaviours of PwO and HCPs.24 The global dataset24 revealed a need to increase understanding of obesity and improve education concerning its aetiology. The aim of this subanalysis was to identify the perceptions, attitudes, behaviours and potential barriers to effective obesity care in the UK.
Methods
Study design and participants
The ACTION-IO study was a cross-sectional, non-interventional study that collected data via an online survey in Australia, Chile, Israel, Italy, Japan, Mexico, Saudi Arabia, South Korea, Spain, the UK and the United Arab Emirates. The full methods for the ACTION-IO study have been reported previously.24 Eligible PwO in the UK were 18 years or older, with a current BMI of at least 30 kg/m2 based on self-reported height and weight. The PwO sample was targeted for demographic representativeness based on gender, age, income, race/ethnicity and region. Therefore, PwO were excluded if they declined to provide any of these variables. Respondents were also excluded for non-obesity reasons, for high BMI or for dramatic weight loss, that is, if they were pregnant, participated in intense fitness or body building programmes, or had significant, unintentional weight loss in the past 6 months. Eligible UK’s HCPs were in practice for 2 years or more, with at least 70% of their time spent in direct patient care, and who had seen 100 or more patients in the past month, at least 10 of whom had a BMI of at least 30 kg/m2. HCPs specialising in general, plastic or bariatric surgery were excluded. Respondents were recruited via online panel companies (via email) to whom they had given permission to be contacted for research purposes, and completed the survey in English. All respondents provided electronic informed consent prior to initiation of the screening questions and survey. Preceding participation, PwO were only informed of the purpose of the study, and were blinded to the specific study goals.
Survey development and procedures
The study was designed by an international steering committee of obesity experts (representing primary care, endocrinology and psychology, and including three medical doctors employed by Novo Nordisk), with support from KJT Group (Honeoye Falls, New York, USA), and based on the ACTION US and Canada questionnaires.25 26 KJT Group managed the acquisition and analysis of data; UK responses were collected between September 2018 and October 2018. Questionnaire items were carefully phrased and presented in identical order for each respondent. Items in a list were displayed in alphabetical, categorical, chronological or random order as relevant for each response. Respondents accessed the survey using a unique web link, details regarding the digital fingerprinting system used to assess unique site visitors has been previously described.24 To prevent duplicate survey entries, unique site visitors were recorded via a user ID that was passed along the unique web link that respondents used to access the site. The system checked every respondent entering the survey against previous user IDs logged in its database. Respondents who began the survey and suspended were able to re-enter the survey while it was still open and finish the survey where they left off. Respondents who had already received a terminal status (complete, over-quota or terminate) were blocked from re-entering the survey. Following closure of the survey, no users were able to gain access. The user ID and data of suspended respondents were stored until the survey was closed and were then eliminated from the data analysis. The study was conducted in accordance with the Guidelines for Good Pharmacoepidemiology Practices.27
To ensure representativeness to the general population, the final PwO sample was weighted to demographic targets within each country for age, gender, income, race/ethnicity and region. The HCP data were not weighted. Only data from those who completed the survey were included in the analyses.
Patient and public involvement
No patients or members of the public were involved in the design or conduct of the study. A patient representative was involved in the analysis and interpretation of the UK data and is an author on this article. She will also be involved in disseminating these findings to a wider audience.
Results
Demographics
A total of 69 676 PwO and 2508 HCPs, in the UK, were invited. The response rate to the survey was 14% (9786/69 676) for PwO and 35% (886/2508) for HCPs, as expected for this type of study and in line with the target sample size.24 Of those who completed the screening questions, the eligibility rate was 22% (2146/9779) for PwO and 53% (387/737) for HCPs. The final UK sample for the ACTION-IO survey was 1500 PwO and 306 HCPs, of whom 156 were primary care professionals (PCPs) and 150 were secondary care professionals (SCPs) (table 1). Some differences were observed in the survey outcomes between PCPs and SCPs, which will be reported in full at a later date.
Table 1.
Sample demographics and characteristics
| UK’s PwO (n=1500) | HCPs (n=306) | |
| Recruitment and qualification* | ||
| Total survey invitations sent | 69 676 | 2508 |
| Respondents | 9786 | 886 |
| Respondents who completed screening questions | 9779 | 737 |
| Respondents who qualified | 2146 | 387 |
| Respondents who qualified and completed validated survey | 1500 | 306 |
| Age, years (range) | 55.7 (19–88) | 48.9 (28–68) |
| Gender, n (%) | ||
| Male | 687 (45.8%) | 225 (73.5%) |
| Female | 811 (54.1%) | 81 (26.5%) |
| Other | 2 (0.1%) | – |
| BMI classification, n (%) | ||
| Respondents† | 1500 (100%) | 236 (77.1%) |
| Underweight or healthy range (<25 kg/m2) | – | 152 (64.4%) |
| Overweight (25–29.9 kg/m2) | – | 72 (30.5%) |
| Obesity Class I (30–34.9 kg/m2) | 883 (56.2%) | 7 (3.0%) |
| Obesity Class II (35–39.9 kg/m2) | 333 (22.4%) | 2 (0.9%) |
| Obesity Class III (≥40 kg/m2) | 284 (21.4%) | 3 (1.3%) |
| Number of comorbidities, n (%) | ||
| 0 | 264 (16.9%) | – |
| 1 | 360 (25.0%) | – |
| 2 | 330 (22.2%) | – |
| 3 | 257 (16.0%) | – |
| ≥4 | 289 (20.0%) | – |
| HCP category, n (%) | 306 (100%) | |
| PCP | – | 156 (51.0%) |
| SCP | – | 150 (49.1%) |
| Endocrinologist | – | 43 (14.1%) |
| Cardiologist | – | 51 (16.7%) |
| Obstetrician–gynaecologist | – | 16 (5.2%) |
| Other | – | 40 (13.1%) |
| Obesity specialist,‡ n (%) | ||
| Yes | – | 162 (52.9%) |
| No | – | 144 (47.1%) |
All ‘n’ sizes for PwO are from unweighted data. Demographic percentages (age and gender) are also from unweighted data. All non-demographic percentage results are for PwO weighted data. HCP data were not weighted; therefore, n sizes and percentages are all unweighted data.
*Participation rate (those who completed the screener) was 99.9% for PwO and 84.7% for HCPs; completion rate was 100% for PwO and 85.8% for HCPs.
†Disclosure of height and weight was optional for HCPs. The percentages for the BMI categories were calculated using the number of respondents to this question as the denominator.
‡A physician who meets at least one of the following criteria: at least 50% of their patients are seen for obesity/weight management; or has advanced/formal training in treatment of obesity/weight management beyond medical school; or considers themselves to be an expert in obesity/weight loss management or works in an obesity service clinic.24
BMI, body mass index; HCP, healthcare professional; PCP, primary care professional; PwO, people with obesity; SCP, secondary care professional.
Pre-consultation and initiation of weight management discussion
People with obesity
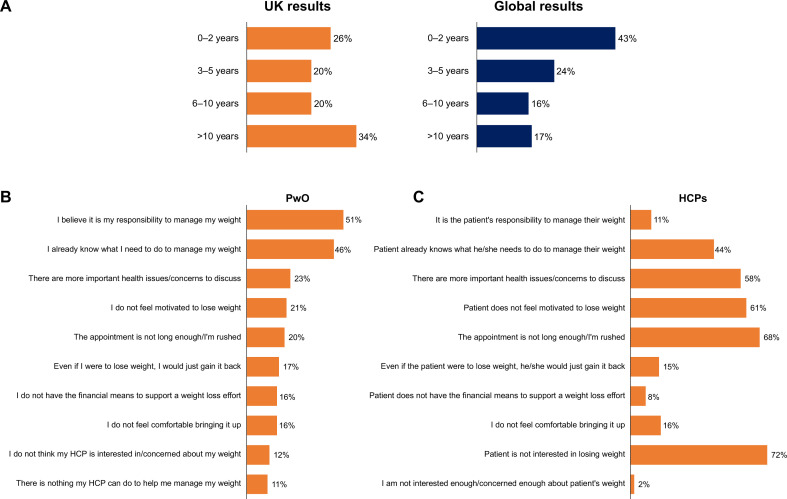
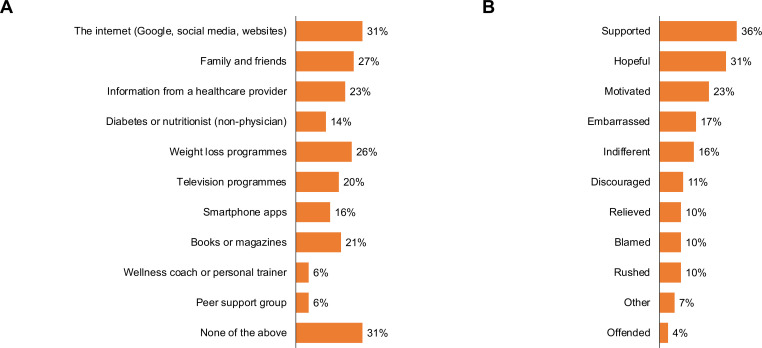
Only about half (47%) of all PwO had discussed excess weight or losing weight with an HCP in the past 5 years. It took a median of 6 years and mean of 9 years (range: 0.0–56.0 years; IQR: 13 years) between the time when PwO said that they first started struggling with excess weight or obesity and when they first had a weight management conversation with an HCP (figure 1A). In comparison, globally it took a median of 3 years and a mean of 6 years (range: 0.0–68.0 years; IQR: 8 years (figure 1A)).24 Forty-seven per cent of PwO who discussed weight with an HCP reported that they initiated the conversation themselves. When PwO were asked to name the top five reasons why they may not discuss weight management with their HCP, the most common reason was the belief that it was their own responsibility to manage their weight (51% of PwO) (figure 1B). Indeed, when asked whether they agreed with the statement ‘my weight loss is completely my responsibility’, 85% of PwO agreed with the statement. Thirty-four per cent of PwO said that they were motivated to lose weight, and 36% provided a neutral response (neither agreed nor disagreed that they were motivated). Only 4% of PwO reported an indifference to losing weight as a reason for not discussing managing their weight with an HCP. Sixty-five per cent of PwO who previously had a weight conversation with their HCP liked that their HCP discussed their weight with them, and 58% who not previously had a conversation would have liked their HCP to bring up weight during their appointments. Most PwO (81%) believed that obesity has a large impact on overall health, similar to other chronic diseases such as diabetes (82%), stroke (88%), cancer (82%) or chronic obstructive pulmonary disease (COPD; 84%). The internet was cited as a source of information used by 31% of PwO for managing weight (figure 2A). Other sources of information were reported as family and friends (27%), weight loss programmes (26%), information from an HCP (23%) and media (books/magazines: 21%, television programmes: 20%) (figure 2A).
Figure 1.
Number of years between when struggle with weight began and first discussed with an HCP and PwO/HCP reasons for not discussing weight management. (A) Approximate number of years reported by the UK and global PwO (ACTION-IO study steering committee, personal communication) between the beginning of their struggle with weight and first discussion with an HCP. Calculated at respondent level from questions, ‘Approximately how old were you when you first remember struggling with excess weight or obesity?’ and ‘Approximately how old were you when a healthcare provider first discussed your excess weight or recommended that you lose weight?’. (B) Reasons reported by the UK’s PwO for not discussing managing their weight with an HCP. (C) Reasons reported by the UK’s HCPs for not discussing weight management with their patients. ACTION-IO, Awareness, Care, and Treatment In Obesity maNagement–International Observation; HCP, healthcare professional; PwO, people with obesity.
Figure 2.
Sources of information and feelings after a weight discussion. (A) Sources of information most frequently used by the UK’s PwO for managing weight (reported by PwO). (B) Feelings reported by the UK’s PwO after their most recent weight or weight loss discussion with an HCP in the past 5 years. HCP, healthcare professional; PwO, people with obesity.
Healthcare professionals
Those HCPs who discussed weight with their patients reported that 35% of the time the patient initiated the conversation. Compared with PwO (85%), a smaller proportion of HCPs (33%) placed the responsibility for weight loss on PwO. Only 13% of HCPs thought that their patients were motivated to lose weight, and 42% provided a neutral response (neither agreed nor disagreed that their patients were motivated). The most commonly selected reason for not discussing weight management with a patient (selected by 72% of HCPs) was the perception that the patient was not interested in losing weight, and 61% of HCPs selected lack of patient motivation (figure 1C). Other reasons provided for not discussing obesity with a patient were that the appointments were not long enough and that they felt rushed (selected by 68% of HCPs), and that more important health issues/concerns were an impediment to discussing obesity with a patient (selected by 58% of HCPs). In addition, almost one-third of HCPs (31%) reported that the good health of a patient and the absence of weight-related comorbidities would be a reason for not discussing weight management. The most important criterion for initiating weight management conversations with a patient was the presence of obesity-related comorbidities, cited by 76% of HCPs. Only 68% of the UK’s HCPs (vs 76% of global HCPs24) recognised the impact of obesity on health, and it was rated as less serious than diabetes, cancer, stroke or COPD by 40%, 65%, 62% and 43% of the UK’s HCPs, respectively.
Consultation
People with obesity
Eighty-one per cent of the PwO who had discussed weight with an HCP had had a discussion with a PCP, 42% with a nurse, 18% with a dietitian/nutritionist and 17% with a diabetes educator. PwO reported a complex mixture of feelings following a weight loss conversation with an HCP (figure 2B). PwO cited a combination of feelings such as supported 36%, hopeful 31%, motivated 23%, embarrassed 17%, indifferent 16%, discouraged 11%, relieved 10%, blamed 10%, rushed 10%, offended 4% and confused 4% (figure 2B).
Healthcare professionals
Fifty-nine per cent of HCPs reported that they were extremely or very comfortable discussing weight, 30% were neither comfortable nor uncomfortable and 11% were a little or not at all comfortable discussing weight. On average, HCPs reported that they spent 10 min interacting with their patients when discussing weight (range: 1–20 min).
Consultation outcomes and follow-up
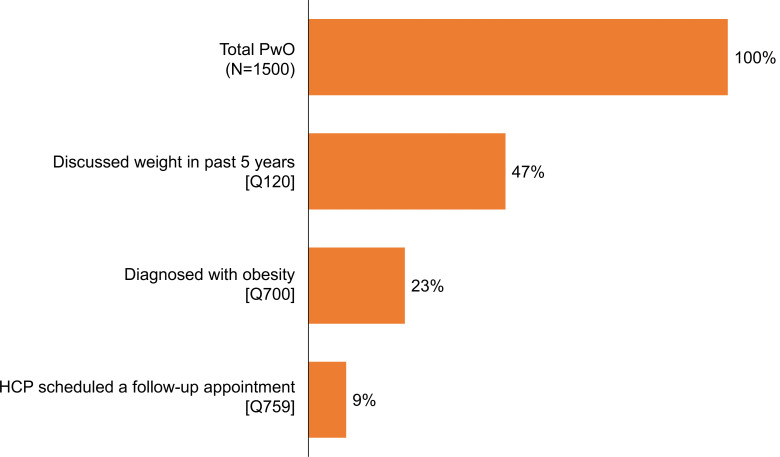
People with obesity
Among the 47% of PwO who had discussed their weight with an HCP in the past 5 years, 49% reported that they had been diagnosed with obesity in the past by an HCP (24% of all PwO, figure 3). Only 19% of PwO who had discussed their weight with an HCP had a follow-up appointment scheduled (9% of all PwO) (figure 3). However, 62% of PwO would have liked a follow-up appointment and 96% reported attending or planning to attend a follow-up appointment if scheduled. The most frequent methods for managing weight tried by PwO were general improvements in eating habits/reducing calories (reported by 61% of PwO) and general increases in physical activity (55%), which were reported at a greater frequency than by global PwO (51% and 39% for general eating habits and physical activity, respectively; ACTION-IO study steering committee, personal communication). Bariatric surgery and behavioural therapy referral rates were reported in small numbers by the UK’s PwO (1% and 2%, respectively). Visits to a nutritionist/dietician and obesity specialist were reported less frequently by the UK’s PwO than global PwO (nutritionist/dietician: 11% UK, 24% global; obesity specialist: 2% UK, 9% global; ACTION-IO study steering committee, personal communication).
Figure 3.
Obesity diagnoses and follow-up appointments with an HCP. Proportion of the UK’s PwO who discussed weight or weight loss with an HCP in the past 5 years and the frequency of obesity diagnoses and follow-up appointments. HCP, healthcare professional; PwO, people with obesity.
Healthcare professionals
On average, HCPs scheduled follow-up appointments with 33% of their patients for obesity and 46% of HCPs said that patients kept these follow-up appointments always or most of the time. HCPs most frequently recommended general improvements in eating habits/reducing calories (reported by 61% of HCPs) and general increases in physical activity (65%). Referrals to obesity specialists were recommended less frequently by UK HCPs (12%) compared with the global dataset (23%).24
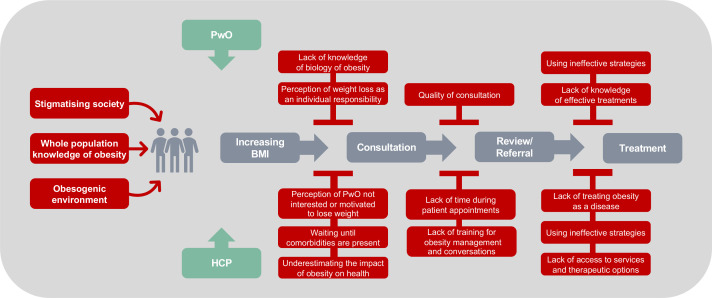
Discussion
PwO are faced with biological predispositions, and societal and environmental conditions that contribute to obesity, weight stigma and discrimination. Obesity prevention and management are key health priorities and require a whole systems approach. However, the national response for obesity focuses on individual responsibility regarding nutrition and lack of physical activity. In this study, multiple barriers to effective weight management were identified, which are summarised in figure 4 and discussed below.
Figure 4.
A conceptual model of the obesity treatment pathway and barriers to obesity care in the UK. BMI, body mass index; HCP, healthcare professional; PwO, people with obesity.
Initiation of weight management discussion with HCPs
Fewer than half of PwO in the UK (47%) had a discussion with an HCP about their weight in the past 5 years, despite HCPs being the gateway to weight management care in the NHS. Moreover, for the PwO who did have a weight discussion, it took a mean of 9 years after they first started struggling with their weight before having the discussion (compared with 6 years globally).24 This delay is particularly important as it may create an opportunity for significant obesity-related complications to develop. This long delay may also reflect a higher degree of obesity stigma in the UK28 and a culture of individual responsibility for obesity.29 30 Indeed, a focus on individual responsibility is reflected in UK government policy on obesity.31 Reducing the time gap by initiating earlier weight management discussions may be an effective strategy for improving obesity treatment and preventing the development of comorbidities.
From the PwO perspective, a delay in seeking help could be linked to the high percentage (85%) of PwO who perceived their weight loss as completely their responsibility. From the HCP perspective, a delay in discussing obesity with a patient could be linked to reported perceptions that the patient was not interested or motivated in losing weight, consistent with previous research.32 33 Other impediments to the discussion were HCPs’ views that there were more important health issues to discuss and that a weight management discussion is only required when weight-related comorbidities are present, as supported by other studies.33 34 Moreover, HCPs in the UK underestimated the effect of obesity on health to a greater extent than the UK’s PwO and global HCPs.24 For PwO, this will likely require a change in the narrative around obesity to lessen focus on individual responsibility, and for HCPs a need to increase the understanding of the health consequences of obesity and the desire of PwO for help and support. The internet, media, and family and friends formed a substantial source of information for PwO for managing weight. We need to change this from personal responsibility to recognising the aetiology of obesity and its implications for PwO.
Consultation
Primary care is the gateway to obesity treatment, and most weight management discussions were held with a primary care physician or nurse. While many PwO welcomed weight discussions with HCPs, they also reported experiencing complex and varied emotions after these discussions. It is important to acknowledge the complexity of the experience for PwO. Studies have previously reported patients feeling that their obesity had been ignored, dismissed, distorted or attributed as the explanation of all their health problems by HCPs.35–37 Negative experiences can contribute to depression, anxiety, low self-esteem and body dissatisfaction.38 39 Dissatisfactory conversations with an HCP may discourage PwO from seeking further weight management help in the future and reinforce feelings of personal responsibility for weight management. The attitudes of health professionals towards obesity and its management have been generally reported to be negative, and knowledge and skills in managing obesity have been noted to be inconsistent.40–45 Even well-intended acts can cause offence and humiliation,46 and PwO often experience their weight in profoundly negative ways as a result of the pervasive stigmatisation of obesity. Patient experiences are valid indications of the strengths and shortcomings of the services they receive.47 It is important to ensure that the narrative around obesity resonates with the lived experiences of those affected by it and encourages patients to engage with an HCP.47 HCPs in turn should aim to provide compassionate care that is free of bias and use supportive communication and language to facilitate successful and meaningful conversations.47
HCPs often have limited time and resources, and lack of time has previously been reported as a barrier to discussing obesity.48 49 More HCPs in the UK (68%) than globally (54%) indicated that the limited appointment time would be a factor in not having a weight loss conversation.24 This may be a reflection of the average primary care consultation time in the UK, which is 10 min and considerably shorter than in many other countries.50 51 Other potential barriers described in the literature have included uncertainty about appropriate language,48 concerns about compromising rapport9 and concerns discussing a potentially upsetting and stigmatising topic.22 50 52 However, in this study, relatively few HCPs reported discomfort with weight discussions.
Consultation outcomes and follow-up
Obesity diagnoses, follow-up appointments and referrals to specialists were infrequently reported by PwO, which could incorrectly reinforce the feeling of individual responsibility. Indeed, methods for managing weight reported by PwO, which relied largely on general improvements in eating habits and physical activity, suggest a lack of knowledge of effective treatment methods and/or a consequence of the availability of therapeutic options (see below).
The data from HCPs on the frequency of follow-up appointments and methods for obesity management largely aligned with the data from PwO. Barriers to effective weight management cited in the literature have included lack of effective and individualised treatment and/or referral options.40 41 50 53 Weight management services in the UK exist as part of fragmented health and social care systems, which are geographically dependent.49 54 55 The range of services and treatments, including pharmacotherapy and bariatric surgery, is limited in the UK, which may restrict HCPs in what they can offer patients. Indeed, HCPs report insufficient management options and scepticism about their efficacy.56 57 This is further compounded by limited consultation times for the UK’s general practitioners.50 51 The limited availability of weight management services, effective treatments and coherent, joined-up strategies in the UK health system are significant barriers to providing effective obesity care.55
Strengths and limitations
Strengths of this study include scientific rigour in the study design (including carefully phrased and ordered questions to prevent biased responses, blinded purpose of the survey for PwO and determination of eligibility by initial screening questions to eradicate bias during recruitment) and implementation (including stratified sampling to provide a representative cohort of the general population and rigorous data analysis). Other strengths include the large number of UK’s PwO and HCP respondents and the ability to directly compare the UK data to the equivalent global dataset. Limitations include the cross-sectional design and reliance on accurate reporting from the PwO and HCP respondents, which could be perceived as recall bias. The self-reported height and weight could underestimate the BMI of the PwO. A higher proportion of HCPs than might be expected self-identified as obesity specialists using the broad criteria specified in table 1. The low response rates could affect sample representativeness and is a known limitation for this type of study. Response bias from the population sampled cannot be ruled out. However, the PwO sample was representative of the demographics of the general population.
Conclusion
This study demonstrates the need to change the narrative around obesity, with less stigmatising focus on individual responsibility, for the government, commissioners, general public, PwO and HCPs. The findings identified areas that prevent PwO from seeking help and receiving appropriate care. In addition, the attitudes of HCPs prevent them from offering the support PwO require for obesity management. The consultation about weight with an HCP is the gateway to treatment in the NHS and improving the frequency and quality of PwO–HCP conversations is essential. Sufficient time should be given to HCPs to approach the topic of overweight and obesity sensitively and effectively. The current survey did not have high numbers of people with a BMI of over 40 kg/m2; further research is required to understand whether people with higher BMIs have distinct experiences in the management of their obesity.
To conclude, a whole systems approach is required to address and eliminate weight bias and stigmatisation, to change the narrative around obesity in the UK, and to improve provision of NHS services. Educating the whole population, including PwO and HCPs, about the aetiology and psychology of obesity and the interaction with the obesogenic environment should help to ensure that patients access and receive quality care and effective weight treatment and management. Changing the narrative around obesity will allow for a more effective delivery framework for health service providers and greater access to effective treatment pathways and weight management services for PwO.
Supplementary Material
Acknowledgments
We thank the participants of the study. Medical editorial assistance was provided by Anna Bacon from Articulate Science, and was funded by Novo Nordisk.
Footnotes
Contributors: CAH and JCGH are members of the ACTION-IO study steering committee and contributed to the design of the study. CAH, ALA, HK, BMM, HMP, AV and JCGH participated in the interpretation of data, and drafting and revision of the manuscript. All authors reviewed and approved the final, submitted version.
Funding: This work and ACTION-IO was supported by Novo Nordisk. ALA is funded by the Medical Research Council through grant MC_UU_00006/6.
Competing interests: CAH reports financial support from Novo Nordisk to attend an obesity conference during the conduct of the study, grants from the Rona Marsden Fund at Fakenham Medical Practice and personal fees from Orexigen Therapeutics, Consilient Health, Nestlé, Ethicon and Alva outside the submitted work. ALA reports grants from UKRI Medical Research Council and National Institute for Health Research, and non-financial support from WW (formerly Weight Watchers). HK is an employee of Novo Nordisk and owns shares in Novo Nordisk. BMM reports grants paid to her institution from Novo Nordisk and personal fees (consultancy and advisory board) from Novo Nordisk, Boehringer Ingelheim and Orexigen Therapeutics; and has received speaker fees for Eli Lilly, Novo Nordisk, Boehringer Ingelheim, Janssen, MSD and Sanofi. HMP reports grants from the National Institute for Health Research and Public Health England and an honorarium from Novo Nordisk (educational grant) outside the submitted work. AV acted as a speaker for Obesity Empowerment Network and is a board member of the Clinical Advisory Committee on the All Wales Obesity Strategy. JCGH reports fees (honoraria) paid to the University of Liverpool from Novo Nordisk, Orexigen and Boehringer Ingelheim during the conduct of the study.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. De-identified participant data will be made available for this article on a specialised SAS data platform. Datasets from Novo Nordisk will be available permanently after completion of data analysis. Access to data can be made through a request proposal form and the access criteria can be found online (novonordisk-trials.com). Data will be shared with bona fide researchers submitting a research proposal requesting access to data. Data use is subject to approval by the independent review board.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The National Health Service Health Research Authority (Central Research Ethics Committee, London) advised that ethical approval was not needed in the UK.
References
- 1.Foresight . Tackling obesities: future choices, 2007. Available: https://www.gov.uk/government/collections/tackling-obesities-future-choices [Accessed 15 Jan 2020]. [DOI] [PubMed]
- 2.Bray GA, Kim KK, Wilding JPH, et al. Obesity: a chronic relapsing progressive disease process. A position statement of the world obesity Federation. Obes Rev 2017;18:715–23. 10.1111/obr.12551 [DOI] [PubMed] [Google Scholar]
- 3.Ralston J, Brinsden H, Buse K, et al. Time for a new obesity narrative. Lancet 2018;392:1384–6. 10.1016/S0140-6736(18)32537-6 [DOI] [PubMed] [Google Scholar]
- 4.Ghanemi A, Yoshioka M, St-Amand J. Broken energy homeostasis and obesity pathogenesis: the surrounding concepts. J Clin Med 2018;7:453. 10.3390/jcm7110453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kassir R. Risk of COVID-19 for patients with obesity. Obes Rev 2020;21:e13034. 10.1111/obr.13034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 - COVID-NET, 14 States, March 1-30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:458–64. 10.15585/mmwr.mm6915e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NHS Digital . Health survey for England 2018. overweight and obesity in adults and children. Available: http://healthsurvey.hscic.gov.uk/media/81625/HSE18-Adult-Child-Obesity-rep.pdf [Accessed Jun 2020].
- 8.The Organization for Economic Cooperation and Development (OECD) . Overweight or obese population (indicator), 2019. Available: https://data.oecd.org/healthrisk/overweight-or-obese-population.htm [Accessed Jun 2020].
- 9.National Institute of Health and Care Excellence (NICE) . Obesity: identification, assessment and management, 2014. Available: https://www.nice.org.uk/guidance/cg189/resources/obesity-identification-assessment-andmanagement-pdf-35109821097925 [Accessed 28 Nov 2019]. [PubMed]
- 10.NHS Digital . Statistics on obesity, physical activity and diet, England, 2019. Available: https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/statistics-on-obesity-physical-activity-and-diet-england-2019/part-3-adult-obesity [Accessed 2 Dec 2019].
- 11.Public Health England . Health matters: obesity and the food environment, 2017. Available: https://www.gov.uk/government/publications/health-matters-obesity-and-the-food-environment/health-matters-obesity-and-the-food-environment-2 [Accessed Apr 2020].
- 12.Royal College of Physicians . The training of health professionals for the prevention and treatment of overweight and obesity, 2010. Available: https://www.rcplondon.ac.uk/news/rcp-report-concludes-all-health-professionals-need-obesity-training [Accessed 3 Dec 2019].
- 13.Flint SW, Hudson J, Lavallee D. UK adults' implicit and explicit attitudes towards obesity: a cross-sectional study. BMC Obes 2015;2:31. 10.1186/s40608-015-0064-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flint SW, Čadek M, Codreanu SC, et al. Obesity discrimination in the recruitment process: "you're not hired!". Front Psychol 2016;7:647. 10.3389/fpsyg.2016.00647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flint SW, Reale S. Weight stigma in frequent exercisers: overt, demeaning and condescending. J Health Psychol 2018;23:710–9. 10.1177/1359105316656232 [DOI] [PubMed] [Google Scholar]
- 16.Vartanian LR, Novak SA. Internalized societal attitudes moderate the impact of weight stigma on avoidance of exercise. Obesity 2011;19:757–62. 10.1038/oby.2010.234 [DOI] [PubMed] [Google Scholar]
- 17.Department of Health, Obesity and Food Policy Branch . Developing a specification for lifestyle weight management services. best practice guidance for tier 2 services. 2013. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/142723/Weight_Management_Service_Spec_FINAL_with_IRB.pdf [Accessed Apr 2020].
- 18.Public Health England . National mapping of weight management services: provision of tier 2 and tier 3 services in England, 2015. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/484115/Final_Weight_Management_Mapping_Report.pdf [Accessed 17 Jan 2020].
- 19.Department of Health and Social Care . Healthy lives healthy people: a call to action on obesity in England, 2011. Available: https://www.gov.uk/government/publications/healthy-lives-healthy-people-a-call-to-action-on-obesity-in-england [Accessed Apr 2020].
- 20.Public Health England . Whole systems approach to obesity. A guide to support local approaches to promoting a healthy weight, 2019. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/820783/Whole_systems_approach_to_obesity_guide.pdf [Accessed Jun 2020].
- 21.Public Health England and NHS England . Report of the Working group into: joined up clinical pathways for obesity, 2014. Available: https://www.england.nhs.uk/wp-content/uploads/2014/03/owg-join-clinc-path.pdf [Accessed Apr 2020].
- 22.Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health 2010;100:1019–28. 10.2105/AJPH.2009.159491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stanford FC, Tauqeer Z, Kyle TK. Media and its influence on obesity. Curr Obes Rep 2018;7:186–92. 10.1007/s13679-018-0304-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Caterson ID, Alfadda AA, Auerbach P, et al. Gaps to bridge: misalignment between perception, reality and actions in obesity. Diabetes Obes Metab 2019;21:1914–24. 10.1111/dom.13752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the national ACTION study. Obesity 2018;26:61–9. 10.1002/oby.22054 [DOI] [PubMed] [Google Scholar]
- 26.Sharma AM, Bélanger A, Carson V, et al. Perceptions of barriers to effective obesity management in Canada: results from the ACTION study. Clin Obes 2019;9:e12329. 10.1111/cob.12329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.International Society for Pharmacoepidemiology (ISPE) . Guidelines for Good Pharmacoepidemiology Practices (GPP). Available: https://www.pharmacoepi.org/resources/policies/guidelines-08027/ [Accessed 15 Jan 2020].
- 28.Kyle TK, Nadglowski J, Salas RX, et al. A comparative analysis of explicit weight bias in the UK and eight other countries. Obes Facts 2018;11(Suppl 1):1–364. abstract S1.3. [Google Scholar]
- 29.Carof S. Is There a ‘National Body’? How National Cultures Shape the ‘Fat’ Body and the Food Practices. Stud Ethn Natl 2017;17:57–67. 10.1111/sena.12219 [DOI] [Google Scholar]
- 30.O'Keeffe M, Flint SW, Watts K, et al. Knowledge gaps and weight stigma shape attitudes toward obesity. Lancet Diabetes Endocrinol 2020;8:363–5. 10.1016/S2213-8587(20)30073-5 [DOI] [PubMed] [Google Scholar]
- 31.Theis DRZ, White M. Is obesity policy in England fit for purpose? Analysis of government strategies and policies, 1992-2020. Milbank Q 2021;99:126–70. 10.1111/1468-0009.12498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Visser F, Hiddink G, Koelen M, et al. Longitudinal changes in GPs' task perceptions, self-efficacy, barriers and practices of nutrition education and treatment of overweight. Fam Pract 2008;25(Suppl 1):i105–11. 10.1093/fampra/cmn078 [DOI] [PubMed] [Google Scholar]
- 33.Tham M, Young D. The role of the General Practitioner in weight management in primary care--a cross sectional study in General Practice. BMC Fam Pract 2008;9:66. 10.1186/1471-2296-9-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scott JG, Cohen D, DiCicco-Bloom B, et al. Speaking of weight: how patients and primary care clinicians initiate weight loss counseling. Prev Med 2004;38:819–27. 10.1016/j.ypmed.2004.01.001 [DOI] [PubMed] [Google Scholar]
- 35.Merrill E, Grassley J. Women's stories of their experiences as overweight patients. J Adv Nurs 2008;64:139–46. 10.1111/j.1365-2648.2008.04794.x [DOI] [PubMed] [Google Scholar]
- 36.Thomas SL, Hyde J, Karunaratne A, et al. Being 'fat' in today's world: a qualitative study of the lived experiences of people with obesity in Australia. Health Expect 2008;11:321–30. 10.1111/j.1369-7625.2008.00490.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brown HL. Providers' Familiarity with guidelines for weight gain during pregnancy impacts counseling and compliance in obese women. J Womens Health 2017;26:1139–40. 10.1089/jwh.2017.6545 [DOI] [PubMed] [Google Scholar]
- 38.Tuthill A, Slawik H, O'Rahilly S, et al. Psychiatric co-morbidities in patients attending specialist obesity services in the UK. QJM 2006;99:317–25. 10.1093/qjmed/hcl041 [DOI] [PubMed] [Google Scholar]
- 39.Hill AJ, Williams J. Psychological health in a non-clinical sample of obese women. Int J Obes Relat Metab Disord 1998;22:578–83. 10.1038/sj.ijo.0800631 [DOI] [PubMed] [Google Scholar]
- 40.Brown I, Stride C, Psarou A, et al. Management of obesity in primary care: nurses' practices, beliefs and attitudes. J Adv Nurs 2007;59:329–41. 10.1111/j.1365-2648.2007.04297.x [DOI] [PubMed] [Google Scholar]
- 41.Leverence RR, Williams RL, Sussman A, et al. Obesity counseling and guidelines in primary care: a qualitative study. Am J Prev Med 2007;32:334–9. 10.1016/j.amepre.2006.12.008 [DOI] [PubMed] [Google Scholar]
- 42.Blane DN, Macdonald S, Morrison D, et al. The role of primary care in adult weight management: qualitative interviews with key stakeholders in weight management services. BMC Health Serv Res 2017;17:764. 10.1186/s12913-017-2729-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dewhurst A, Peters S, Devereux-Fitzgerald A, et al. Physicians' views and experiences of discussing weight management within routine clinical consultations: a thematic synthesis. Patient Educ Couns 2017;100:897–908. 10.1016/j.pec.2016.12.017 [DOI] [PubMed] [Google Scholar]
- 44.Henderson E. Obesity in primary care: a qualitative synthesis of patient and practitioner perspectives on roles and responsibilities. Br J Gen Pract 2015;65:e240–7. 10.3399/bjgp15X684397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.World Health Organization . Obesity: preventing and managing the global epidemic. Report of a WHO consultation, 2000. Available: https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ [Accessed Apr 2020]. [PubMed]
- 46.Malterud K, Thesen J. When the helper humiliates the patient: a qualitative study about unintended intimidations. Scand J Public Health 2008;36:92–8. 10.1177/1403494807085358 [DOI] [PubMed] [Google Scholar]
- 47.Ananthakumar T, Jones NR, Hinton L, et al. Clinical encounters about obesity: systematic review of patients' perspectives. Clin Obes 2020;10:e12347. 10.1111/cob.12347 [DOI] [PubMed] [Google Scholar]
- 48.Speer SA, McPhillips R. Initiating discussions about weight in a non-weight-specific setting: what can we learn about the interactional consequences of different communication practices from an examination of clinical consultations? Br J Health Psychol 2018;23:888–907. 10.1111/bjhp.12322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gadsby EW, Peckham S, Coleman A, et al. Commissioning for health improvement following the 2012 health and social care reforms in England: what has changed? BMC Public Health 2017;17:211. 10.1186/s12889-017-4122-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McGowan BM. A practical guide to engaging individuals with obesity. Obes Facts 2016;9:182–92. 10.1159/000445193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Martin S, Davies E, Gershlick B. Under pressure. What the Commonwealth Fund’s 2015 international survey of general practitioners means for the UK, 2016. Available: https://www.health.org.uk/sites/default/files/UnderPressure.pdf [Accessed 1 Dec 2019].
- 52.Swift JA, Choi E, Puhl RM, et al. Talking about obesity with clients: preferred terms and communication styles of U.K. pre-registration dieticians, doctors, and nurses. Patient Educ Couns 2013;91:186–91. 10.1016/j.pec.2012.12.008 [DOI] [PubMed] [Google Scholar]
- 53.Ogden J, Flanagan Z. Beliefs about the causes and solutions to obesity: a comparison of GPs and lay people. Patient Educ Couns 2008;71:72–8. 10.1016/j.pec.2007.11.022 [DOI] [PubMed] [Google Scholar]
- 54.Public Health England . Spend and outcome tool (SPOT), 2017. Available: https://www.gov.uk/government/publications/spend-and-outcome-tool-spot [Accessed Apr 2020].
- 55.Public Health England . National mapping of weight management services: provision of tier 2 and tier 3 services in England, 2015. Available: https://www.gov.uk/government/publications/weight-management-services-national-mapping [Accessed 17 Jan 2020].
- 56.Campbell K, Engel H, Timperio A, et al. Obesity management: Australian general practitioners' attitudes and practices. Obes Res 2000;8:459–66. 10.1038/oby.2000.57 [DOI] [PubMed] [Google Scholar]
- 57.Claridge R, Gray L, Stubbe M, et al. General practitioner opinion of weight management interventions in New Zealand. J Prim Health Care 2014;6:212–20. 10.1071/HC14212 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. De-identified participant data will be made available for this article on a specialised SAS data platform. Datasets from Novo Nordisk will be available permanently after completion of data analysis. Access to data can be made through a request proposal form and the access criteria can be found online (novonordisk-trials.com). Data will be shared with bona fide researchers submitting a research proposal requesting access to data. Data use is subject to approval by the independent review board.