Abstract
Background
Multiple treatment modalities have been developed to treat atrophic acne scars with varying degrees of success. Post‐inflammatory hyperpigmentation (PIH) after acne scar treatments remain a major concern in Asian patients. Fractional radiofrequency (FRF) has been used in many dermatological skin conditions including acne scars.
Aims
To determine the efficacy and safety of FRF nanoneedle system in the treatment of acne scars in Asians.
Methods
This is a prospective, evaluator‐blinded study with 25 subjects diagnosed with moderate to severe acne scarring. All subjects received 3 monthly treatments of the FRF nanoneedle system on both cheeks. Primary outcome was the clinical improvement of acne scars graded by 2 blinded dermatologists at baseline, 1‐, 3‐, and 6‐month follow‐ups. Objective scar volume analysis was done using ultraviolet A (UVA) light video camera. Subjects’ self‐assessment, pain score, and adverse events were also recorded.
Results
Twenty‐three out of 25 subjects completed the study and attended all follow‐up. Clinical improvement of acne scars was observed as early as 1‐month follow‐up. Objective evaluation of acne scar volume decreased significantly on all follow‐up compared to baseline (P < .005). Majority of the subjects (48%) reported marked improvement in their acne scars. Adverse events such as pain, erythema, burning sensation, edema, scab formation, and PIH were mild and temporary.
Conclusions
FRF nanoneedle system is a safe and effective treatment for acne scars in Asians. However, despite the significant changes in the scar volume, caution should be used to avoid excessive coagulation resulting in PIH.
Keywords: acne scar, fractional radiofrequency, nanoneedle
1. INTRODUCTION
Acne scar is a permanent complication of acne vulgaris which can cause significant psychological distress, poor self‐esteem, and social isolation. 1 Atrophic acne scars are the most common type, and its pathogenesis is related to the inflammatory mediators and enzymatic degradation of collagen fibers and subcutaneous fat. 2 Today, multiple treatment modalities have been developed to treat this condition with varying degrees of success. 2 PIH as a result of acne scar treatment is still a major concern in Asian patients. 3
Ablative lasers are considered the gold standard for treating acne scars because of its excellent results; however, it became a less popular option because of its side effects and longer recovery time. 4 Nonablative lasers have faster recovery time and less side effects, but more sessions are needed to achieve better scar improvement. 4 Fractional laser resurfacing (FLR) has been proven to be effective in the treatment of facial wrinkles, photoaging as well as acne scarring, but the common complication is PIH especially in Fitzpatrick skin type IV. 5
Nonablative RF (monopolar, bipolar, and fractional) uses electric current to produce focal thermal damage to the dermis; therefore, it is associated with fewer complications and faster recovery time. 6 FRF uses an array of electrodes or microneedles to create fractional thermal wounds which is delivered directly into the deep reticular dermis. 7 This technology causes volumetric heating of the dermal structures with little to no heat damage to the epidermis, resulting in neoelastogenesis and neocollagenesis. 8 Previous clinical studies have demonstrated its efficacy in treating various skin conditions including striae, irregular texture, rhytides, hyperpigmentation, skin laxity, and acne scars. 9 , 10 , 11 , 12 , 13
The objective of this study was to determine the efficacy and safety of FRF nanoneedle system in the treatment of atrophic acne scars in Asians.
2. METHODS
This was a prospective, single‐center, and evaluator‐blinded study. A total of twenty‐five subjects, male or female, at least 18 years old, diagnosed with moderate to severe acne scarring that is present for more than 6 months were included in the study. Acne scar severity was graded based on the Goodman and Baron Qualitative Global Scarring Grading System. 14 Exclusion criteria included subjects with active inflammatory acne, history of allergy to topical anesthesia, photosensitive dermatosis, skin infection, and regular smoking habit.
All subjects received three monthly treatments of FRF nanoneedle system (Venus Viva™, Venus Concept Inc, Toronto, Canada) for the treatment of atrophic acne scars. The hand piece has 160 pins/tip with a maximum energy of 62 mJ/pin, and each pin is 150 x 20 microns in size. Preoperatively, topical anesthetic cream (EMLA®, APP Pharmaceuticals, Schaumburg, Illinois) was applied for 1 hour prior to the treatment. Subjects were treated on both cheeks using a parameter setting of 260 volts with a pulse duration of 30 milliseconds (msec). The initial pass was done in an oblique pattern, followed by the second pass over the same area in a reverse oblique pattern. Postoperatively, the subjects were instructed to apply cold compress to the treated area. Petrolatum ointment was applied four times daily for 1 week until the crusting had completely healed. Sun avoidance and protection were also emphasized.
The primary outcome of the study was the clinical improvement of acne scars graded using the quartile scale: 0 = no improvement, 1 = minimal improvement (0‐25%), 2 = moderate improvement (26‐50%), 3 = marked improvement (51‐75%), and 4 = excellent improvement (76‐100%). Subjective evaluation of the photographs was graded by 2 blinded dermatologists at baseline, 1‐, 3‐, and 6‐month follow‐ups. All clinical photographs were taken with identical camera settings, lighting, and positioning using a Canon PowerShot G9 stand‐off camera (OMNIA imaging System, Canfield Scientific Inc, Fairfield, NJ).
In addition, acne scar volume was objectively evaluated using an UVA‐light video camera (Visioscan® VC 98, Courage‐Khazaka with an analysis software (Surface Evaluation of the Living Skin; SELS) at baseline, 1‐, 3‐, and 6‐month follow‐ups. Subjects’ self‐assessment was also evaluated using the same quartile grading scale and were recorded on every follow‐up. Pain score after each treatment was rated using a visual analogue scale (VAS) from 1 to 10. Adverse events such as facial erythema, burning sensation, edema, scab formation, pigmentary changes, scarring, pinpoint bleeding, and purpura were also recorded.
Descriptive analysis was used for the demographic data. Cumulative acne scar volume was compared using the Wilcoxon signed rank test, and the p‐value less than 0.05 was considered statistically significant. The statistical analysis was performed using a statistical software (SPSS version 19.0; SPSS Inc).
This study was approved by the ethics committee of the Siriraj Institutional Review Board. Written informed consent was obtained from all participants prior to their enrollment in the study.
3. RESULTS
Out of the 25 subjects recruited, 23 (92%) completed the study protocol and were included in the final analysis. Two subjects were withdrawn from the study because they could not attend the follow‐up visits. Among the 23 subjects included, there were 9 males (39%) and 14 females (61%) with a mean age of 30.6 years. Most subjects had Fitzpatrick skin types III to IV. The median of acne scar duration was 7.5 years, with a range of 1‐15 years. Based on the Goodman and Baron Qualitative Global Scarring Grading System, 47% had moderate acne scar severity while 53% had severe acne scar severity.
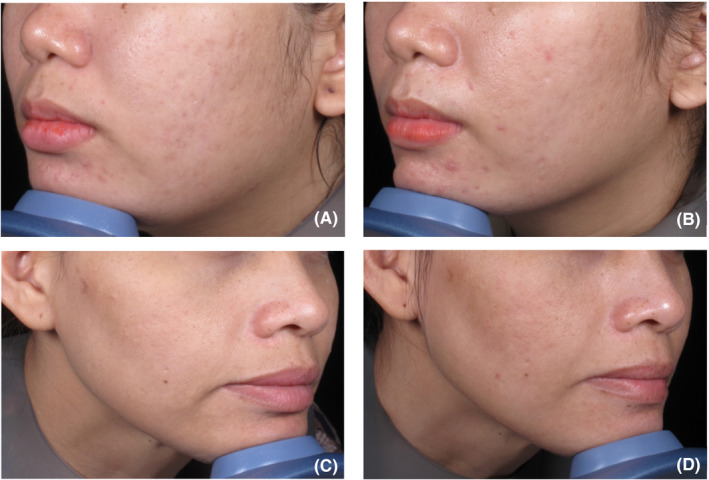
Subjective evaluation of the acne scar improvement using the quartile scale was presented in Figure 1. As early as 1‐month follow‐up, 78% already had minimal improvement (0%‐25%) when compared to the baseline. On the 3‐month follow‐up, majority (39%) had moderate improvement (26%‐50%) while on 6‐month follow‐up, most of the patients had excellent (30%) and marked (30%) improvement. The clinical improvement of the acne scars after FRF nanoneedle treatment is shown in Figure 2.
Figure 1.
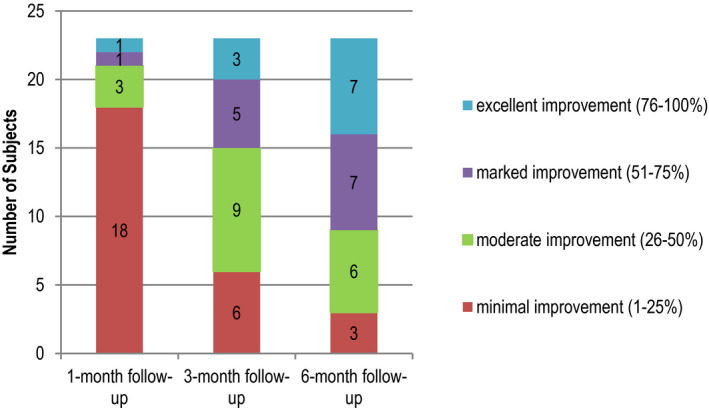
Subjective evaluation of acne scars by comparative evaluation of photographs from baseline to follow‐ups
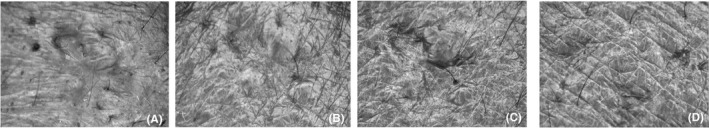
Figure 2.

Clinical improvement of acne scars after fractional radiofrequency nanoneedle treatment from A, baseline, B, 1‐mo follow‐up, C, 3‐mo follow‐up, and D, 6‐mo follow‐up
Objective evaluation of the acne scar volume using a UVA‐light video camera was analyzed by the SELS software. In Figure 3, the acne scar volume decreased significantly on all follow‐up when compared to the baseline (P < .005). The improvement of the atrophic acne scar using a UVA‐light video camera is shown on Figure 4.
Figure 3.
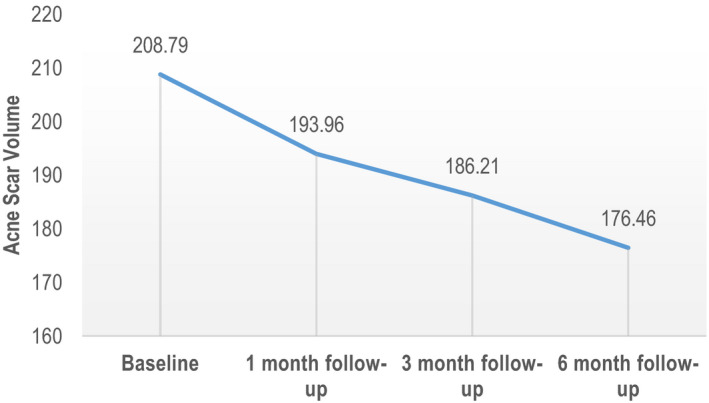
Acne scar volume evaluation using UVA‐light video camera showed significant reduction when compared from baseline
Figure 4.
Clinical improvement in the atrophic acne scar was demonstrated in the photographs using a UVA‐light video camera from A, baseline, B, 1‐mo follow‐up, C, 3‐mo follow‐up, and D, 6‐mo follow‐up
Subjects’ self‐assessment was also recorded on the 1‐, 3‐, and 6‐month follow‐ups. During the 1‐ and 3‐month follow‐ups, majority (78%, 48%) reported minimal improvement. However, on the 6‐month follow‐up, most of the subjects (48%) reported marked improvement in their acne scars (Figure 5).
Figure 5.
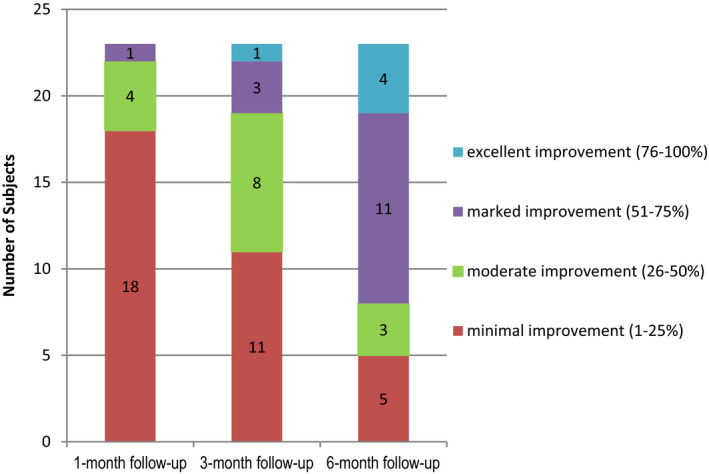
Subjects’ self‐assessment on the improvement of acne scars at baseline and follow‐ups
All subjects had adverse event of pain, facial erythema, and scab formation as presented in Table 1. The average pain score was 6.5 out of 10. Other adverse events were burning sensation, mild edema, and PIH. All of the adverse events resolved spontaneously within 7 days except for the PIH. Three out of 23 subjects demonstrated PIH (13%), 2 cases were mild and 1 case was moderate. Two of them reported PIH after the 3rd treatment, and it lasted up to 6 months. The other subject reported 2 episodes of PIH that occurred before the 2nd treatment session which resolved spontaneously and before the 3rd treatment that lasted until the 3‐month follow‐up.
Table 1.
Adverse events in this study and its duration
| Number of affected patients/ total number of patients (%) | Duration | |
|---|---|---|
| Pain | 23/23 (100%) | 1‐2 h |
| Facial erythema | 23/23 (100%) | 1‐5 d |
| Burning sensation | 14/23 (60.8%) | 2‐24 h |
| Edema | 19/23 (82.6%) | 1‐3 d |
| Scab formation | 23/23 (100%) | 3‐7 d |
| Hyperpigmentation |
3/23 (13%) (mild: 2, moderate: 1) |
3‐6 mo |
In addition, 2 out of 23 subjects (8.7%) had noticeable improvement in facial contouring at 6‐month follow‐up (Figure 6).
Figure 6.
Clinical photographs comparing the improvement of facial contouring at the jaw lines from A, baseline to B, 6‐mo follow‐up and at the marionette lines from C, baseline to D, 6‐mo follow‐up
4. DISCUSSION
Ablative laser resurfacing has been proven to be an effective treatment of atrophic acne scars, but the potential risk of PIH is very high especially in Asians. 15 Recently, FRF has been a popular treatment option to improve skin laxity, wrinkles, and acne scarring because of its ability to preserve the epidermis leading to rapid recovery time and less adverse effects. 16 Many studies were conducted to evaluate the efficacy of FRF in the treatment of acne scars with good results. 12 , 17 , 18
Our study demonstrated the continued improvement of acne scar volume over time when compared to the baseline (P < .005). FRF microneedle system was reported to upregulate the TGFß expression, which stimulates dermal fibroblast activation and collagen formation leading to acne scar improvement. 19 Biopsy specimens taken 3 months after bipolar FRF showed marked improvement in acne scars which were characterized by a decrease in dermal pilosebaceous units and perivascular inflammatory cell infiltrates with an increase in elastin content and collagen deposition in the upper dermis. 20
In our study, the subject assessment scores were better on a later follow‐up period (6‐month follow‐up) and this was consistent with another study. 18
The average pain score in our study was 6.5 out of 10. A split‐face study comparing the invasive FRF (with needle) and noninvasive FRF was done, and interestingly, the invasive FRF produced a lower pain score. 21 The authors concluded that the variation in pain could be related to the differences in the way the two FRF methods contact the skin. 21 Invasive FRF only contacts the skin with the needles while the noninvasive FRF has the entire treatment head as its contact area. 21
The treatment of acne scars with FRF appears to be safe and effective because it avoids the downtime by creating a triangular beam of thermal energy directly into the dermis with minimal epidermal damage. 22 Most common adverse events in FRF were pain, edema, and erythema, which were similar with the findings in our study. 22 PIH was reported in 6.5% after using combined FRF and fractional laser treatment for acne scars in Asians. 23 A study using FRF microneedle system as the sole treatment for acne scars had PIH in 3.85% of cases. 24 Goel and colleague treated acne scars in Fitzpatrick skin type IV‐V with the same device used in our study—FRF nanoneedle system. 12 They customized the treatment per subject based on the depth of the acne scar lesion using a range of parameters (220‐270 volts, 10‐30 ms pulse width, 80 pins/tip, and multiple passes for deeper scar) and no PIH was reported. 12 Our study reported a higher percentage of PIH (13%) because we used the same parameter (260 volts, 30 ms pulse width, 160 pins/tip, and double pass) on all subjects regardless of their skin type and acne scar depth. The relatively long pulse duration together with the double pass treatment increased the coagulation ratio of tissue which may have affected the epidermal melanocytes leading to PIH. Bipolar FRF using high to moderate energy (60 and 100 mJ/pin) setting for acne scars in Asians reported PIH of 13.5%‐17.5%. 25 Higher energy density can cause more epidermal ablation and deeper coagulation leading to PIH. 25 Adjusting the treatment parameters should be considered to reduce the chances of having PIH especially in darker skin types.
In our study, we also discovered that 8.7% of our subjects had improvement in their facial contouring noted during the 6‐month follow‐up. This finding supports the benefit of FRF in the improvement of skin laxity. 26
Our study was limited by a small sample size and a dropout rate of 8% due to lost of follow‐up. Therefore, we recommend larger trials in the future with a control group and also longer a follow‐up period to further evaluate the longevity of the treatment results.
5. CONCLUSION
The FRF nanoneedle system is a safe and effective treatment for acne scars in Asians. It demonstrated good improvement in the scar volume as well as in the surface phenotype texture of atrophic acne scars. However, treatment parameters need to be adjusted to reduce the risk of PIH.
AUTHOR CONTRIBUTIONS
Dr Wanitphakdeedecha had full access to all of the data in the study and takes responsibility for the integrity of data and the accuracy of the data analysis; Dr Wanitphakdeedecha contributed to study concept and design and study supervision; Drs. Wanitphakdeedecha and Nitayavardhana contributed to acquisition of data; Drs. Wanitphakdeedecha, Nitayavardhana, and Eimpunth contributed to analysis and interpretation of data; Drs. Nitayavardhana and Ng drafted the manuscript; Dr Manuskiatti contributed to critical revision of the manuscript for important intellectual content; Dr Nitayavardhana contributed to statistical analysis; Dr Manuskiatti gave administrative, technical, or material support.
ACKNOWLEDGMENTS
This research project is supported by Faculty of Medicine Siriraj Hospital, Mahidol University. The authors wish to thank Ms Phassara Klamsawat, Ms Phonsuk Yamlexnoi, and Mr Panyawat Wongjaruwat for their assistance in recruiting subjects and managing the database. In addition, the authors would like to thank Venus Concept Co. Ltd. for the products used in this study.
Nitayavardhana S, Wanitphakdeedecha R, Ng JNC, Eimpunth S, Manuskiatti W. The efficacy and safety of fractional radiofrequency nanoneedle system in the treatment of atrophic acne scars in Asians. J Cosmet Dermatol. 2020;19:1636–1641. 10.1111/jocd.13484
[Correction added on February 11, 2021 after first online publication: The copyright line for this article was changed.]
REFERENCES
- 1. Gieler U, Gieler T, Kupfer JP. Acne and quality of life–impact and management. J Eur Acad Dermatol Venereol. 2015;29:12‐14. [DOI] [PubMed] [Google Scholar]
- 2. Gozali MV, Zhou B. Effective treatments of atrophic acne scars. J Clin Aesthet Dermatol. 2015;8(5):33‐40. [PMC free article] [PubMed] [Google Scholar]
- 3. Chan HH, Manstein D, Yu CS, et al. The prevalence and risk factors of post inflammatory hyperpigmentation after fractional resurfacing in Asians. Lasers Surg Med. 2007;39:381‐385. [DOI] [PubMed] [Google Scholar]
- 4. Boen M, Jacob C. A Review and update of treatment options using the acne scar classification system. Dermatol Surg. 2019;45(3):411‐422. [DOI] [PubMed] [Google Scholar]
- 5. Sriprachya‐anunt S, Marchell NL, Fitzpatrick RE, Goldman MP, Rostan EF. Facial resurfacing in patients with Fitzpatrick skin type IV. Lasers Surg Med. 2002;30(2):86‐92. [DOI] [PubMed] [Google Scholar]
- 6. Lolis MS, Goldberg DJ. Radiofrequency in cosmetic dermatology: a review. Dermatol Surg. 2012;38(11):1765‐1776. [DOI] [PubMed] [Google Scholar]
- 7. Dai R, Xie H, Hua W, Li XH, Li L. The efficacy and safety of the fractional radiofrequency technique for the treatment of atrophic acne scar in Asians: a meta‐analysis. J Cosmet Laser Ther. 2017;19(6):337‐344. [DOI] [PubMed] [Google Scholar]
- 8. Hantash BM, Ubeid AA, Chang H, Kafi R, Renton B. Bipolar fractional radiofrequency treatment induces neoelastogenesis and neocollagenesis. Lasers Surg Med. 2009;41(1):1‐9. [DOI] [PubMed] [Google Scholar]
- 9. Pongsrihadulchai N, Chalermchai T, Ophaswongse S, Pongsawat S, Udompataikul M. An efficacy and safety of nanofractional radiofrequency for the treatment of striae alba. J Cosmet Dermatol. 2017;16(1):84‐90. [DOI] [PubMed] [Google Scholar]
- 10. Simmons BJ, Griffith RD, Falto‐Aizpurua LA, Nouri K. Use of radiofrequency in cosmetic dermatology: focus on non‐ablative treatment of acne scars. Clin Cosmet Investig Dermatol. 2014;7:335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bohnert K, Dorizas A, Sadick N. Prospective, pilot evaluation of the performance of nanofractional radiofrequency for improvement of skin texture via skin resurfacing. J Cosmet Dermatol. 2018;17(1):61‐65. [DOI] [PubMed] [Google Scholar]
- 12. Goel A, Gatne V. Use of nanofractional radiofrequency for the treatment of acne scars in Indian skin. J Cosmet Dermatol. 2017;16(2):186‐192. [DOI] [PubMed] [Google Scholar]
- 13. Ray M, Gold M. A retrospective study of patient satisfaction following a trial of nano‐fractional RF treatment. J Drugs Dermatol. 2015;14(11):1268‐1271. [PubMed] [Google Scholar]
- 14. Goodman GJ, Baron JA. Post acne scarring: a qualitative global scarring grading system. Dermatol Surg. 2006;32:1458‐1466. [DOI] [PubMed] [Google Scholar]
- 15. Manuskiatti W, Triwongwaranat D, Varothai S, Eimpunth S, Wanitphakdeedecha R. Efficacy and safety of a carbon‐dioxide ablative fractional resurfacing device for treatment of atrophic acne scars in Asians. J Am Acad Dermatol. 2010;63(2):274‐283. [DOI] [PubMed] [Google Scholar]
- 16. Kwon HH, Park HY, Choi SC, et al. Combined fractional treatment of acne scars involving non‐ablative 1,550‐nm erbium‐glass laser and micro‐needling radiofrequency: a 16‐week prospective. Randomized Split‐face Study. Acta Derm Venereol. 2017;97(8):947‐951. [DOI] [PubMed] [Google Scholar]
- 17. Chandrashekar BS, Sriram R, Mysore R, Bhaskar S, Shetty A. Evaluation of microneedling fractional radiofrequency device for treatment of acne scars. J Cutan Aesthet Surg. 2014;7(2):93‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gold MH, Biron JA. Treatment of acne scars by fractional bipolar radiofrequency energy. J Cosmet Laser Ther. 2012;14(4):172‐178.22548644 [Google Scholar]
- 19. Min S, Park SY, Yoon JY, Suh DH. Comparison of fractional microneedling radiofrequency and bipolar radiofrequency on acne and acne scar and investigation of mechanism: comparative randomized controlled clinical trial. Arch Dermatol Res. 2015;307(10):897‐904. [DOI] [PubMed] [Google Scholar]
- 20. Kaminaka C, Furukawa F, Yamamoto Y. Long‐term clinical and histological effects of a bipolar fractional radiofrequency system in the treatment of facial atrophic acne scars and acne vulgaris in Japanese Patients: A Series of Eight Cases. Photomed Laser Surg. 2016;34(12):657‐660. [DOI] [PubMed] [Google Scholar]
- 21. Zeng R, Liu Y, Zhao W, et al. A split‐face comparison of a fractional microneedle radiofrequency device and fractional radiofrequency therapy for moderate‐to‐severe acne vulgaris. J Cosmet Dermatol. 2020;00:1‐6. [DOI] [PubMed] [Google Scholar]
- 22. Forbat E, Al‐Niaimi F. Fractional radiofrequency treatment in acne scars: Systematic review of current evidence. J Cosmet Laser Ther. 2016;18(8):442‐447. [DOI] [PubMed] [Google Scholar]
- 23. Yeung CK, Chan NP, Shek SY, Chan HH. Evaluation of combined fractional radiofrequency and fractional laser treatment for acne scars in Asians. Lasers Surg Med. 2012;44(8):622‐630. [DOI] [PubMed] [Google Scholar]
- 24. Vejjabhinanta V, Wanitphakdeedecha R, Limtanyakul P, Manuskiatti W. The efficacy in treatment of facial atrophic acne scars in Asians with a fractional radiofrequency microneedle system. J Eur Acad Dermatol Venereol. 2014;28(9):1219‐1225. [DOI] [PubMed] [Google Scholar]
- 25. Phothong W, Wanitphakdeedecha R, Sathaworawong A, Manuskiatti W. High versus moderate energy use of bipolar fractional radiofrequency in the treatment of acne scars: a split‐face double‐blinded randomized control trial pilot study. Lasers Med Sci. 2016;31(2):229‐234. [DOI] [PubMed] [Google Scholar]
- 26. Lu W, Wu P, Zhang Z, Chen J, Chen X, Ewelina B. Curative effects of microneedle fractional radiofrequency system on skin laxity in Asian patients: a prospective, double‐blind, randomized, controlled face‐split study. J Cosmet Laser Ther. 2017;19(2):83‐88. [DOI] [PubMed] [Google Scholar]


