Abstract
Aim
Separating infants and their parents after a Caesarean section is still the routine care worldwide. This study investigated three caregiving models on the wakefulness and physiological parameters of full‐term infants after an elective Caesarean section.
Methods
Newborn infants born in a Chilean public hospital in 2009‐12 were randomised to three groups: cot, fathers' arms or skin‐to‐skin contact with their father. They were assessed at 15‐minute intervals, from 45 to 120 minutes after the Caesarean section. Their physiological parameters were measured, and their wakefulness was assessed using the Neonatal Behavioural Assessment Scale.
Results
We studied 95 infant (53% girls) born at a mean gestational age of 38.9 ± 0.9 weeks. Heart rates were significantly higher in the skin‐to‐skin than cot or fathers' arms groups and showed greater stability over time. Wakefulness was initially higher in the skin‐to‐skin group, but there were no significant differences by the end of the observation. There were no differences between the groups in peripheral oxygen saturation. Skin‐to‐skin contact had no negative impact on the infants.
Conclusion
The skin‐to‐skin group showed some advantages over the cot and fathers' arms groups when it came to establishing stable physiological parameters and wakefulness. This approach should be supported during mother‐infant separation.
Keywords: Caesarean section, full‐term infants, physiological adaptation, skin‐to‐skin contact, wakefulness
Abbreviations
- bpm
beats per minute
- NBAS
Neonatal Behavioural Assessment Scale
Keynotes.
This study focused on the wakefulness and physiological parameters of full‐term infants, who are frequently separated from their parents after an elective Caesarean.
The 95 infants were randomised to three groups: cot, fathers' arms or skin‐to‐skin contact with their father and at 15‐minute intervals, from 45 to 120 minutes after birth.
The skin‐to‐skin group demonstrated some advantages over the other two groups when it came to establishing stable physiological parameters and wakefulness.
1. INTRODUCTION
Early mother‐infant contact during the first hours after birth is known to increase parental sensitivity to infants' signals, 1 , 2 , 3 as well as bonding and maternal satisfaction. 4 , 5 The pre‐feeding behaviour of infants who experience skin‐to‐skin contact with their mothers has also been described as one of the pathways to initiating breastfeeding. 5 One study showed that infants who had skin‐to‐skin contact with their mother cried less than those who were not held that way. 6 Such contact is also believed to enhance bonding between fathers and infants after elective Caesarean sections. 6 , 7 , 8 , 9 , 10 , 11 A systematic Cochrane review of the effects of early mother‐infant skin‐to‐skin contact confirmed that newborn infants have greater cardio‐respiratory stability than controls. 12 A randomised controlled trial showed that infants who had skin‐to‐skin contact with their mothers had a higher body and skin temperature than infants who were carefully wrapped, swaddled or dressed, but did not have skin‐to‐skin contact. 13 Another study also found that paternal substitutes were as successful as incubator care with regard to the positive effect on the infant's body temperature after Caesarean birth. 10 A study of full‐term, healthy infants found that skin‐to‐skin contact was associated with more rapid metabolic adjustment and higher levels of blood glucose than conventional cot care. 8 In that study, body temperature was maintained and stress was reduced in newborn infants who experienced skin‐to‐skin care, indicating that this practice was superior to cot care. 8 Skin‐to‐skin contact with mothers or fathers immediately after an elective Caesarean section has been reported by some researchers to promote parent‐infant communication and interaction. 7 , 11 The aim of this study was to compare the effect of three caregiving models on the wakefulness and physiological parameters of full‐term infants after a Caesarean section.
The hypothesis was that oxygen saturation, temperature, heart rate and wakefulness could be used as measures of the well‐being of newborn infants who received skin‐to‐skin contact with their fathers. This form of contact was compared with being cared for in their fathers' arms or placed in a cot.
2. METHODS AND MATERIAL
A randomised control design was used to assess the effects of three caring models on newborn full‐term infants after a Caesarean section. The study took place in Chile from 2009 to 2012 at a general public hospital that performed around 9000 deliveries per year. At the time of the study, fathers were not allowed to be present during surgery or in the post‐anaesthesia care unit, where their partners were recovering. The mothers were then transferred to the post‐surgery unit for observation, and their infants were taken to the neonatal unit.
The study comprised healthy mothers who had an uncomplicated elective Caesarean section using epidural anaesthesia. Some had surgery due to previous Caesarean sections, and some requested the procedure.
The newborn infants were included if they had a gestational age of between 37 and 42 weeks and an Apgar score of more than seven at one and five minutes. If the infants were deemed to be healthy at the first check‐up 30 minutes after birth, with a temperature of ≥36.6°C, they were included in the study and randomised to one of the three caregiving groups. The inclusion criteria for the fathers were that they had expressed their wish to take part in the study and to take care of the infant while they were separated from their mother after surgery.
2.1. Randomisation
The day before the elective Caesarean section, 130 prospective parents were selected in consecutive order and informed about the study, verbally and in writing. The parents were assured that they could withdraw from the study at any time, without any impact on the care they and their infant received. They were also told that their anonymity would be protected. The randomisation was performed using sealed, opaque envelopes that contained information about group allocation. The infants were randomised to one of three groups. In the cot group, the infants were placed in a cot on their side, dressed in a diaper, cotton pyjamas and a cotton hat, with the father sitting in a chair near the infant. In the fathers' arms group, the infants were placed in a supine position in the fathers' arms, dressed in a diaper, cotton pyjamas and cotton cap. In the father‐infant skin‐to‐skin contact group, the infants were dressed in a cotton diaper, and placed skin‐to‐skin on their fathers' chest in a prone, 30º to 45º upright position. The fathers were seated in a comfortable semi‐reclined armchair, and both the father and infant were covered with a blanket.
2.2. Procedures
All newborn infants received the same routine care before the start of the intervention. Immediately after the Caesarean birth, the umbilical cord was cut and the infant was dried. If required, oral suctioning of mucus from the infant's mouth was conducted. The Apgar score was measured from one to 10, at one and five minutes after birth. The infant was wrapped in two towels and shown to the mother, then cared for under a heater for 30 minutes and eventually transferred to the neonatal unit. The mother, in turn, was transferred to the post‐surgery unit.
All infants were checked 30 minutes after birth by a midwife in the presence of the father. Each infant was examined, measured and weighed, and their ear temperature was noted. If the infant fulfilled the inclusion criteria, they were allocated to the assigned caring model according to the randomisation process. All the infants were wearing a cotton diaper and covered with two blankets during this assessment.
The intervention began 45 minutes after birth, and the infant's physiological variables and their state of wakefulness were evaluated every 15 minutes for 75 minutes. During the intervention, the fathers were free to spontaneously interact and care for their child without limitations, except for the fathers in the cot group, who were asked not to pick up the newborn infant. The staff in the neonatal unit continuously assessed the infant's physical well‐being.
After 2 hours, the newborn infants and fathers went to the obstetric unit, to be reunited with the mothers, and the mothers and their infant were then transferred to the maternity ward for conventional care.
2.3. Data collection
The Neonatal Behavioral Assessment Scale (NBAS) was administered to measure the infants' state of wakefulness 45 minutes after delivery (Table 1). The first author (AA) or a trained research assistant conducted the naturalistic observations and performed all the measurements to ensure the reliability of the study. All the variables were then measured six times, during the first minute of every 15‐minute interval. This means that the observation period spanned 45‐120 minutes after birth.
Table 1.
The NBAS scoring scheme for infant state of wakefulness [23]
| Code 1: Sleep state | Code 2: Sleep state | Code 3: Drowsy state | Code 4: Alert state | Code 5: Alert state | Code 6: Crying state |
| Deep sleep, regular breathing, eyes closed, no activities | Light sleep | Eyes may be open, dull, heavy lidded, closed, delayed responses to stimuli, not alert | Bright look, focused, attention to stimulation, motor activities minimised, glazed look | Eyes open, motor activities, fuzzy vocalisations | Crying that is difficult to break through with stimulation with typical ‘crying' face, cupped tongue |
| Eyes closed, rapid eye movements, low activity level |
The infant's ear temperature was measured using the Braun ThermoScan thermometer (Braun GmbH, Kronberg, Germany). Heart rate and peripheral oxygen saturation were measured on the infant's index finger with a Saturator Masimo, which is a compact pulse oximetry device (Masimo Corp, California, USA). The physiological parameters were performed by the first author (AA) and a trained research assistant.
Demographic data on the health of the mothers and infants were obtained from the birth records and registered in the research protocols.
2.4. Data analysis
Descriptive statistics are used to present the participants' demographic data; continuous variables were described by means, standard deviation and quantiles. To compare differences in the state of wakefulness (NBAS) between the groups, we evaluated the trend of the responses over time analysis of covariance for repeated measurement estimated through mixed models was performed. The evolution of the physiological parameters has been described by a mean value and standard deviations for each time and measurement. The comparison between the three groups was tested by analysis of variance for repeated measurements. Statistical significance was set at 0.05. All data were processed in Stata version 14.0 (Stata Corp LLC, Texas, USA). 14
This study was approved by the Ethics Committee of the Scientific Assessment.
Metropolitan Health Service South East (D‐nr16‐05‐2008).
3. RESULTS
3.1. Participants
In total, 107 couples agreed to participate, but 12 infants did not meet the health inclusion criteria 30 minutes after birth.
This mean that 95 infants were included in the study and randomised to one of the three groups: there were 32 infants in the cot, 34 in the fathers' arms group and 29 in the skin‐to‐skin contact group.
3.2. Demographic characteristics
All the men and women were of Chilean origin and the women received elective Caesarean sections after uncomplicated pregnancies. There were no statistically significant differences between the mean ages in the three caring groups. The average age of the fathers was 32 ± 7.3 years while the mean age of the mothers was 29 ± 6.3 years. On average, the participants had two previous children. The mean gestational age was 38.9 ± 0.9 weeks for the fathers' arms group, 38.7 ± 1.7 weeks for the cot group and 38.9 ± 0.9 weeks for the skin‐to‐skin contact group. The 48 girls had a mean birth weight of 3498 ± 438.4 and the 47 boys with a mean weight of 3547 ± 382.8 grams.
3.3. Physiological parameters
The infant's physiological parameters were assessed, namely temperature, heart rate and peripheral oxygen saturation (Table 2).
Table 2.
Infant mean temperature, heart rate and oxygen saturation (SPO2) over the study period (45‐120 minutes) for the infants cared for in a cot, in the father's arm and skin‐to‐skin on the father's chest
| Variable | Cot group | Fathers arms group | Skin‐to‐skin group | P‐value | P‐value | P‐value |
|---|---|---|---|---|---|---|
| (n = 32) | (n = 34) | (n = 29) | Cot vs Fathers arms | Cot vs Skin‐to‐skin | Skin‐to‐skin vs Fathers arms | |
| Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Temperature | 98.7°F (0.85) | 98.7°F (0.78) | 98.6°F (0.65) | .999 | .217 | .211 |
| (37.1°C) (0.39) | (37.1°C) (0.73) | (37.0°C) (0.37) | ||||
| Heart rate | 142.5 bpm (7.5) | 145.9 bpm (14.2) | 150.8 bpm (16.3) | .184 | .002 * | .063 |
| Oxygen saturation | 97.10% (1.4) | 97.3% (1.4) | 97.2% (1.5) | .498 | .822 | .665 |
| Wakefulness | 3.50 (1.57) | 3.06 (1.34) | 3.71 (1.74) | 1.000 | .013 * | .086 |
Bold indicates that a statistical difference was found
P < .05.
The infants were assessed after 30 minutes under a heater and assigned to one of the three caring models. Their mean ear temperature was 36.8°C at this point. There were no significant differences in the mean ear temperature between the three groups (Table 2), and it remained stable throughout the study period, from 45 to 120 minutes (Figure 1).
Figure 1.
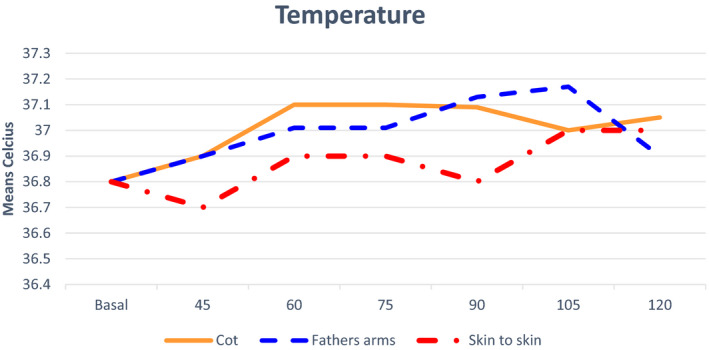
Mean temperature at 45 to 120 minutes after birth in the three groups: cot, in the father's arms and skin‐to‐skin group
Heart rate was measured in beats per minute (bpm) (Table 2). The heart rate in the skin‐to‐skin group differed significantly from the cot group, by a mean of 10.5 beats per minute (150.5 ± 16.3 bpm versus 140.0 ± 7.5 bpm (P = .002) (Figure 2). There were no significant differences in heart rate over time in the skin‐to‐skin contact group.
Figure 2.
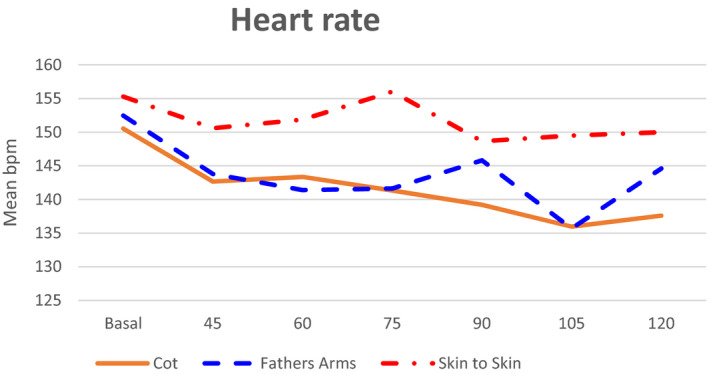
Mean heart rate, beat per minutes (bpm) at 45 to 120 minutes after birth in the three groups: cot, in the father's arms and skin‐to‐skin group
In the cot group, there was a significant decrease in heart rate over time, from a mean of 143 ± 19 bpm at 45 minutes to 138 ± 18 bpm at 120 minutes (P = .001).
The mean heart rate of the infants in the fathers' arms group was 142.4 ± 14.2 bpm. This group showed minor variations in heart rate over time, with a transient decrease to a mean of 136 ± 38.66 bpm at 105 minutes (P < .001).
The infants' mean peripheral oxygen saturation showed no statistical differences between the intervention groups (Table 2), and the pattern during the study period is displayed in Figure 3. At the end of the study period, the mean levels of peripheral oxygen saturation were nearly the same in the three groups.
Figure 3.
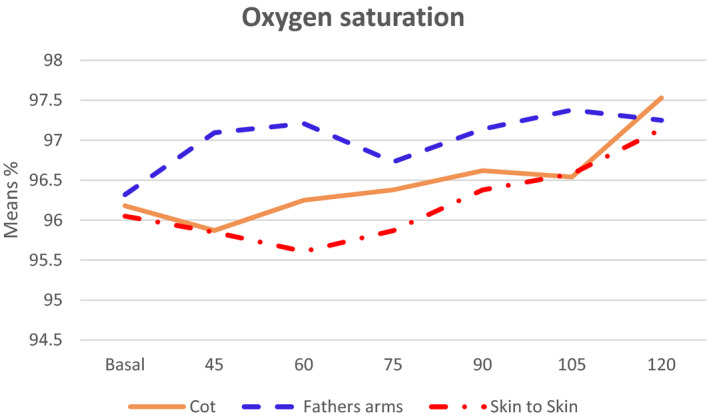
Mean peripheral oxygen saturation (%) at 45 to 120 minutes after birth in the three groups: cot, in the father's arms and skin‐to‐skin group
3.4. Wakefulness
Wakefulness was measured by the NBAS from 45 to 120 minutes after birth, with six observations, at 15‐minute intervals, for each infant. The infants' state of wakefulness is presented in Figure 4, while the mean values, standard deviations and p values for the outcome of the NBAS are listed in Table 3.
Figure 4.
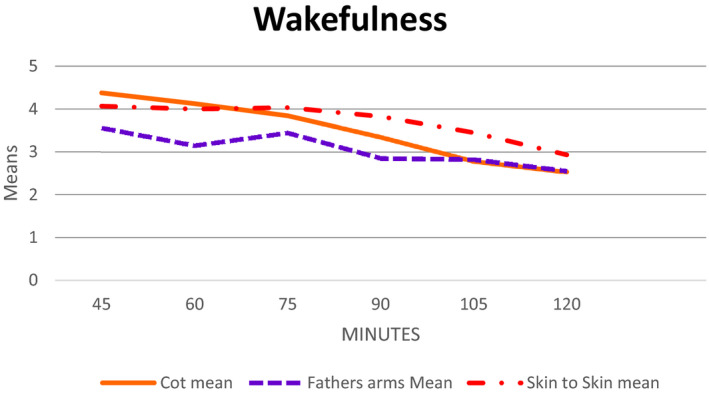
Means' wakefulness at 45 to 120 minutes after birth in the three groups: Infant in a cot join is father, infant in the father's arms, and infant skin‐to‐skin group
Table 3.
Infants' wakefulness trend in the three groups; cot, fathers' arms and skin‐to‐skin groups and comparisons between groups
| Wakefullness | Cot group | Fathers arms group | Skin‐to‐skin group | P‐value | P‐value | P‐value |
|---|---|---|---|---|---|---|
| (n = 32) | (n = 34) | (n = 29) | Cot vs Fathers arms | Cot vs Skin‐to‐skin | Skin‐to‐skin vs Fathers arms | |
| Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Time | ||||||
| 45 minutes | 4.375 (1.26) | 3.558 (1.08) | 4.068 (1.41) | .028 * | 1.000 | .329 |
| 60 minutes | 4.125 (1.34) | 3.147 (1.18) | 4.000. (1.60) | .014 * | 1.000 | .048 * |
| 75 minutes | 3.843 (1.51) | 3.441 (1.28) | 4.034 (1.67) | .824 | 1.000 | .354 |
| 90 minutes | 3.343 (1.45) | 2.852 (1.46) | 3.827 (1.85) | .637 | .712 | .051 |
| 105 minutes | 2.781 (1.36) | 2.823 (1.36) | 3.448 (1.90) | 1.000 | .287 | .339 |
| 120 minutes | 2.531 (1.66) | 2.558 (1.46) | 2.931(1.83) | 1.000 | 1.000 | 1.000 |
Bold indicates that a statistical difference was found.
P < .05
We compared the state of wakefulness in the three groups. The skin‐to‐skin group showed a higher state of wakefulness at 60 minutes than the infants in the fathers' arms group (P = .048) (Figure 4). However, there was no significant difference in the state of wakefulness between the cot group and skin‐to‐skin groups at any time points (Table 3).
The infants in the fathers' arms group demonstrated a significantly lower state of wakefulness than the infants in the cot group at both 45 minutes (P = .028) and 60 minutes (P = .014).
There were no significant differences between the groups between 105 and 120 minutes, as all the infants presented a decreased level of wakefulness at this point.
The study also looked at the pattern of wakefulness within each group as a function of time.
Infants in the skin‐to‐skin contact group maintained an alert pattern of wakefulness from 45 to 90 minutes; then, their wakefulness decreased to a drowsy state at 120 minutes.
There were significant changes in the pattern in the cot group from 45 to 105 minutes (P < .001). The infants showed an alert state between 45 and 75 minutes, followed by a drowsy state at 105 minutes and light sleep at 120 minutes.
The pattern also changed in the fathers' arms group, from 45 to 120 minutes (P = .029). At 45 to 75 minutes, the infants showed a drowsy state followed by light sleep at 120 minutes.
Comparison of infants' mean wakefulness between the groups; infant in a cot, fathers' arms and in skin‐to‐skin.
4. DISCUSSION
Our results show that the infants' physiological parameters and the level of wakefulness showed a stable pattern within the normal range in the three caregiving groups. The infants in the skin‐to‐skin contact group had a higher mean heart rate at 45 minutes after Caesarean delivery than the other two groups, and this higher alert state lasted until approximately 90 minutes. No significant differences were noted between the groups when it came to ear temperature or peripheral oxygen saturation.
The results show that newborn infants can be safely and adequately cared for by their fathers if their mothers cannot take care of them straight after birth. Another study from the same sample and hospital setting showed that fathers who took care of their newborn infants for the first hours after birth developed a better understanding of their infant's first moments of life and became more engaged with them as a result. 15 Another paper on the same cohort reported that the mothers felt that the family benefitted from the fathers caring for their newborn infant while they recovered from their Caesarean section and were separated from their baby. 16
These findings about paternal newborn care are important because many countries routinely separate both parents from their newborn infant after Caesarean sections. This is particularly true in low‐income and middle‐income countries.
Our study showed that the infants in the skin‐to‐skin group showed a specific pattern of wakefulness that was similar to the pattern observed in vaginally delivered infants 5 , 17 They showed an alert state from 45 minutes and starts to decrease at 90 minutes, followed by a drowsy state from 105 to 120 minutes. The infants' prolonged state of wakefulness in the skin‐to‐skin group might suggest a more adaptive state after a Caesarean section, which facilitates the infant's capacity for self‐regulation. 5 It also promotes the father‐infant interaction that can occur in skin‐to‐skin contact immediately after a Caesarean section. 6 , 9 This specific caring model also seems to provide beneficial cardio‐respiratory adaptation after birth. 17 , 18
All three groups in this study achieved cardio‐respiratory stability, as their temperature, heart rate and peripheral oxygen saturation reached a more stable level by the end of the study period. There was no significant difference in peripheral oxygen saturation between the three groups.
The heart rates of healthy newborn infants can vary from 120 to 160 bpm, and the average heart rates were within this range in the three groups in this study. A stable and slightly higher heart rate was observed in the skin‐to‐skin group, which in line with the values reported by Bancalari et al 19 That study showed the relationship between neonatal behavioural states and heart rate variations when newborn infant was in an active state with higher heart rates. 20 Our skin‐to‐skin group showed a higher degree of wakefulness than the other two groups.
Overall, the infants' ear temperatures were stable and within the normal range in all groups. An infants' temperature is stable when they peacefully go through the nine phases of behaviour during skin‐to‐skin contact with their mother: crying, relaxation, awakening, activity, crawling, rest, familiarisation, sucking and sleep. This leads to early optimal self‐regulation, 5 which occurred in our study when the infant was cared for by their father. It has been suggested that mothers may have the ability to modulate their infants' temperature during skin‐to‐skin contact 21 and our study fathers provided the same benefit.
We found that the mean heart rate was significantly higher (P = .002) in the skin‐to‐skin t group than in the cot group. One reason for this finding could have been the higher degree of wakefulness stimulated by sensory cues during skin‐to‐skin contact. 22
4.1. Strength and limitations
The strengths of the study included the randomised controlled trial design. The reliability of the naturalistic observations was strengthened by using Brazelton's NBAS scale, which is a validated instrument, 23 and a standardised observation protocol. In addition, the physiological parameters were standardised with the same procedure and the same personnel conducted the naturalistic observations and performed all the measurements. They strengthened the validity. A possible limitation could be that all the newborn infants were treated under a heater for 30 minutes after birth to ensure their temperature was stable immediately before the interventions. However, it was normal after 30 minutes (36.8°C) and remained normal at the end of the study period of 120 minutes. Moreover, the results of our study agreed with previous research. 24
5. CONCLUSION
Healthy newborn infants born by elective Caesarean section showed stable physiological patterns, temperature, heart rate and peripheral oxygen saturation, when they received three different caregiving models. The father‐infant skin‐to‐skin contact group demonstrated other advantages, and no negative effects were observed. This caregiving model should be supported if mothers and infants need to be separated.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
ACKNOWLEDGEMENTS
The authors are grateful to the Obstetric Service at Sótero del Río Hospital, chief midwife Veronica Gallegos, Dr Patricia Mena, head of the Neonatology Service and the midwives who made this research possible.
REFERENCES
- 1. Leavitt LA. Mothers' sensitivity to infant signals. Pediatrics. 1998;102:1247‐1249. [PubMed] [Google Scholar]
- 2. Arnott B, Meins E. Continunitity in mind‐mindedness from pregnancy to the first year of life. Infant Behav Dev. 2008;31(4):647‐654. [DOI] [PubMed] [Google Scholar]
- 3. Negayama KJT, Momose K. Embodied intersubjective engagement in mother–infant tactile communication: a cross‐cultural study of Japanese and Scottish mother–infant behaviors during infant pick‐up. Front Psychol. 2015;6:66. 10.3389/fpsyg.2015.00066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Stevens J, Schmied V, Burns E. Immediate or early skin‐to‐skin contact after a Caesarean section: a review of the literature. Maternal Child Nutri. 2014;10(4):456‐473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Widström AM, Lilja G, Aaltomaa‐Michalias P. Newborn behaviour to locate the breast when skin‐to‐skin: a possible method for enabling early self‐regulation. Acta Paediatr. 2011;100(1):79‐85. [DOI] [PubMed] [Google Scholar]
- 6. Christensson K, Cabrera T, Christensson E. Separation distress call in the human neonate in the absence of maternal body contact. Acta Paediatr. 1995;84(5):468‐473. [DOI] [PubMed] [Google Scholar]
- 7. Velandia M, Uvnäs‐Moberg K, Nissen E. Sex differences in newborn interaction with mother or father during skin‐to‐skin contact after Caesarean section. Acta Paediatr. 2012;101(4):360‐367. [DOI] [PubMed] [Google Scholar]
- 8. Christensson K, Siles C, Moreno L. Temperature, metabolic adaptation and crying in healthy full‐term newborns cared for skin‐to‐skin or in a cot. Acta Paediatr. 1992;81(6–7):488‐493. [DOI] [PubMed] [Google Scholar]
- 9. Erlandsson K, Christensson K, Dsilna A, Jonsson B. Do caregiving models after caesarean birth influence the infants' breathing adaptation and crying? A pilot study. J Children's Young People's Nursing. 2008;2(1):7‐12. [Google Scholar]
- 10. Christensson K. Fathers can effectively achieve heat conservation in healthy newborn infants. Acta Paediatr. 1996;85(11):1354‐1360. [DOI] [PubMed] [Google Scholar]
- 11. Velandia M, Matthisen AS, Uvnäs‐Moberg K, Nissen E. Onset of vocal interaction between parents and newborns in skin‐to‐skin contact immediately after elective Caesarean section. Birth. 2010;37(3):192‐201. [DOI] [PubMed] [Google Scholar]
- 12. Moore E, Bergman N, Anderson GC, Medley N. Early skin‐to‐skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2016;25(11):CD003519. 10.1002/14651858.CD003519.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bystrova K, Widström AM, Matthiesen AS. Skin‐to‐skin contact may reduce negative consequences of “the stress of being born”: a study on temperature in newborn infants, subjected to different ward routines in St. Petersburg. Acta Paediatrica. 2003;92(3):320‐326. [DOI] [PubMed] [Google Scholar]
- 14. Acock A. A gentle introduction to Stata. Stata press USA. Corvallis, OR: Oregon state University; 2008. [Google Scholar]
- 15. Ayala A, Christensson K, Velandia M, Erlandsson K. Fathers' care of the newborn infant after caesarean section in Chile: a qualitative study. Sexual Reprod Healthcare. 2016;8:75‐81. [DOI] [PubMed] [Google Scholar]
- 16. Ayala A, Christensson K, Velandia M, Erlandsson K. Mother's experiences and perceptions of a continuous caring model with fathers after caesarean section: a qualitative study. Women's Health Open J. 2015;1(3):63‐71. [Google Scholar]
- 17. Nogueras MA, Menéndez AC, Castilla FR. Piel con piel en la primera hora de vida: reflejo de las nueve etapas instintivas. (Skin to skin during the first hours of life). ENE Nursing J. 2016;10:2. ISS‐e 1988–348X. [Google Scholar]
- 18. Acolet D, Sleath K, Whitelaw A. Oxygenation, heart rate and temperature in very low birthweight infants during skin‐to‐skin contact with their mothers. Acta Paediatr. 1989;78(2):189‐193. [DOI] [PubMed] [Google Scholar]
- 19. Bancalari A, Araneda H, Echeverria P, Marinovic A, Manríques C. Arterial oxygen saturation and heart rate in term newborn in the first hour after birth. Rev Chilean Pediatric. 2019;90(4):384‐391. [DOI] [PubMed] [Google Scholar]
- 20. Van Leeuwen P, Groenemeyer D, Lange S. Relation between neonatal behavioral states and heart rate variability. Biomed Eng. 2012;57:615‐618. 10.1515/bmt-2012-4017 [DOI] [Google Scholar]
- 21. Chiu SH, Anderson GC, Burkhamme MD. Newborn temperature during skin‐to‐skin breastfeeding in couples having breastfeeding difficulties. Birt. 2005;32(2):115‐121. [DOI] [PubMed] [Google Scholar]
- 22. Feldman R, Weller A, Sirota L. Skin‐to‐Skin contact (Kangaroo care) promotes self‐regulation in premature infants: sleep‐wake cyclicity, arousal modulation, and sustained exploration. Dev Psychol. 2002;38(2):194. [DOI] [PubMed] [Google Scholar]
- 23. Brazelton TB, Nugent JK, Lester BM. In J. D. Osofsky Neonatal Behavioral Assessment Scale. Wiley series on personality processes. Handbook of infant development. Oxford, UK: John Wiley & Sons; 1987:780‐817. [Google Scholar]
- 24. Christensson K, Siles C, Cabrera T. Lower body temperatures in infants delivered by caesarean section than in vaginally delivered infant. Acta Paediatr. 1993;82(2):128‐131. [DOI] [PubMed] [Google Scholar]


