To the Editor,
The galactose‐α‐1,3‐galactose (α‐Gal) syndrome (AGS) is a novel food allergy with delayed severe allergic reactions after mammalian meat consumption, caused by IgE against the carbohydrate epitope α‐Gal present in mammalian products. We have recently characterized a cohort of AGS patients and demonstrated that atopy increased the risk of anaphylactic symptoms in the respiratory system. 1 This finding prompted us to elucidate the sensitization pattern in AGS patients in more depth, by using the multiplex ImmunoCAP Immuno Solid‐phase Allergen Chip (ISAC), and address the clinical relevance of sensitization to individual allergen molecules.
A total of 138 patients with IgE antibodies to α‐Gal (ImmunoCAP) and a doctor's diagnosis of AGS were enrolled in the study (Table S1). Almost half of the patients reported anaphylactic symptoms (47.8%). Patients' sera were tested on ISAC112. A detailed description of patient inclusion, IgE measurements and statistics can be found in Appendix [Link], [Link].
Due to the role of α‐Gal in AGS, we investigated the carbohydrate response more closely. We found that AGS patients were not more prone to develop IgE against carbohydrate residues other than α‐Gal. IgE against α‐Gal was detected in 92.8% of the patients, because of the slightly lower sensitivity of ISAC compared to ImmunoCAP. Only thirty‐one patients (23%) were sensitized against other cross‐reactive carbohydrate domains, mainly glycosylated grass pollen allergens (Phl p 4, 15.9% and Cyn d 1, 18.8%). This percentage is similar to patients with inhalant allergy (23%). 2
Figure 1A shows a heat map of the IgE reactivity to the most frequently recognized allergen families. A complete heat map and an explanatory table are available in Figure S1 and Table S2. After food allergens, grass pollen and tree pollen were the most common allergen sources (both 33%, dominated by Bet v 1 and Phl p 1), followed by the PR‐10 proteins (31%, due to cross‐reactivity with Bet v 1) and the animal dander group (27%, predominantly Fel d 1) (Table S3), which is similar to the general Swedish population. 3
Figure 1.
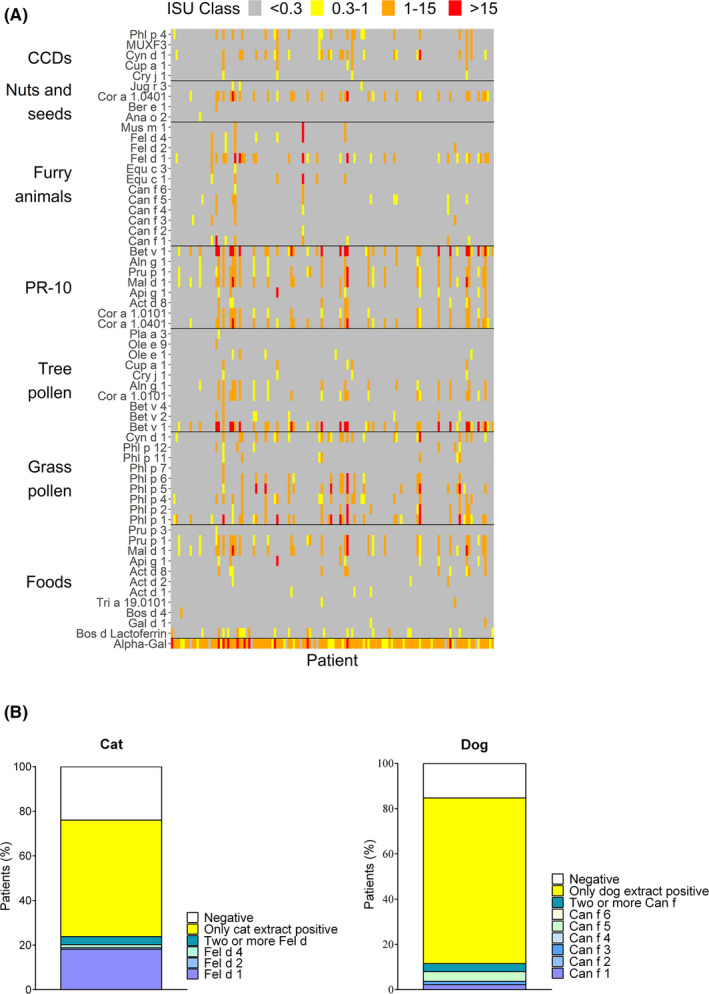
Sensitization patterns of AGS patients. Heat map representing the main allergens belonging to the most recognized allergen families (A). Only molecules with at least one subject having ISU ≥ 0.3 are shown. Frequencies of sensitization against protein extracts and individual allergens for the α‐Gal sources cat and dog (B)
The analysis on a molecular level revealed furthermore that IgE analysis to domestic animals in AGS patients needs to be based on allergen molecules to be able to identify primary sensitization. We found that the majority of the AGS patients were sensitized to cat (75%) and dog (85%) dander extracts (Figure 1B), due to the presence of α‐Gal in these allergen sources. 4 When the patients' sera were analyzed for cat and dog allergen molecules, the low frequency of genuine cat (Fel d 1) and dog (Can f 1 and 5) sensitization became apparent (Figure 1B, 21.7% and 10.1%, respectively).
Next, we investigated if sensitization to specific allergen molecules was associated with AGS symptoms. Anaphylactic patients showed a significantly higher frequency of IgE only against food allergens compared to non‐anaphylactic patients (Figure 2A). On a single allergen level, only patients with IgE against the milk protein lactoferrin had a higher risk of anaphylaxis compared to negative patients (Figure 2B, OR 4.1; 95% CI 1.5‐11.1; P = .006). The observed IgE reactivity against lactoferrin is likely due to the α‐Gal present on lactoferrin. 5 We speculate that its relation with anaphylaxis is due to higher α‐Gal‐specific IgE levels in these patients (Figure 2C), in combination with distinct characteristics of α‐Gal‐specific IgE antibodies like a higher affinity, which is linked to anaphylaxis. 6 These data provide a lead for further investigation of lactoferrin‐IgE as a potential marker of increased risk of anaphylaxis.
Figure 2.

Comparison of sensitization frequencies in patients with and without anaphylaxis. Sensitization frequencies per protein group in AGS patients suffering from anaphylaxis compared to patients without anaphylaxis (A). Frequency of anaphylaxis in lactoferrin‐negative and lactoferrin‐positive patients (B). Levels of α‐Gal‐specific IgE in lactoferrin‐negative and lactoferrin‐positive patients (C). Data are shown as median with interquartile range
In conclusion, for the first time the IgE response of AGS patients has been dissected on a broad molecular allergen level. We report new insights into AGS that will help improve the clinical management of AGS patients.
CONFLICT OF INTEREST
Dr Kiewiet, Grundström and Apostolovic declare no conflict of interest. Mr Andersson and Prof. Borres are employed by Thermo Fisher Scientific (Sweden). Dr Hamsten declares no conflict of interest. Dr Starkhammar reports fees from Mylan, ALK and Chiesi. Prof. van Hage reports personal fees from Biomay AG, Vienna, Austria, and Hycor Biomedical LLC, CA, USA, personal fees from Thermo Fisher Scientific and ALK, outside the submitted work.
Supporting information
Figure S1
Supplementary Material
ACKNOWLEDGEMENTS
This work was supported by The Swedish Research Council, Region Stockholm (ALF‐project), The Swedish Cancer and Allergy Foundation, The Swedish Asthma and Allergy Association's Research Foundation, The King Gustaf V 80th Birthday Foundation, The Swedish Heart‐Lung Foundation, The Hesselman Foundation, The Konsul Th C Bergh Foundation, Tore Nilsson Foundation for Medical Research, The Magnus Bergvall Foundation, and EU H2020 project FoodEnTwin (GA 810752). Thermo Fisher provided the reagents for ISAC.
REFERENCES
- 1. Kiewiet MBG, Apostolovic D, Starkhammar M, Grundström J, Hamsten C, van Hage M. Clinical and serological characterization of the α‐Gal syndrome—importance of atopy for symptom severity in a European Cohort. J Allergy Clin Immunol Pract. 2020;8(6):30176‐30178. [DOI] [PubMed] [Google Scholar]
- 2. Mari A. IgE to cross‐reactive carbohydrate determinants: analysis of the distribution and appraisal of the in vivo and in vitro reactivity. Int Arch Allergy Immunol. 2002;129(4):286‐295. [DOI] [PubMed] [Google Scholar]
- 3. Bjerg A, Ekerljung L, Eriksson J, et al. Increase in pollen sensitization in Swedish adults and protective effect of keeping animals in childhood. Clin Exp Allergy. 2016;46(10):1328‐1336. [DOI] [PubMed] [Google Scholar]
- 4. Commins SP, Satinover SM, Hosen J, et al. Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose‐α‐1,3‐galactose. J Allergy Clin Immunol. 2009;123(2):426‐433.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. van Leeuwen SS, Schoemaker RJW, Timmer CJAM, Kamerling JP, Dijkhuizen L. Use of Wisteria floribunda agglutinin affinity chromatography in the structural analysis of the bovine lactoferrin N‐linked glycosylation. Biochim Biophys Acta. 2012;1820(9):1444‐1455. [DOI] [PubMed] [Google Scholar]
- 6. Gowthaman U, Chen JS, Zhang B, et al. Identification of a T follicular helper cell subset that drives anaphylactic IgE. Science. 2019;365(6456). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1
Supplementary Material


