Summary
Tonsillectomy is one of the most frequently performed surgical procedures; however, pain management remains challenging. Procedure‐specific efficacy as well as specific risks of treatment options should guide selection of pain management protocols based on evidence and should optimise analgesia without harm. The aims of this systematic review were to evaluate the available literature and develop recommendations for optimal pain management after tonsillectomy. A systematic review utilising preferred reporting items for systematic reviews and meta‐analysis guidelines with procedure‐specific postoperative pain management (PROSPECT) methodology was undertaken. Randomised controlled trials published in the English language up to November 2019 assessing postoperative pain using analgesic, anaesthetic or surgical interventions were identified. Out of the 719 potentially eligible studies identified, 226 randomised controlled trials met the inclusion criteria, excluding the studies examining surgical techniques. Pre‐operative and intra‐operative interventions that improved postoperative pain were paracetamol; non‐steroidal anti‐inflammatory drugs; intravenous dexamethasone; ketamine (only assessed in children); gabapentinoids; dexmedetomidine; honey; and acupuncture. Inconsistent evidence was found for local anaesthetic infiltration; antibiotics; and magnesium sulphate. Limited evidence was found for clonidine. The analgesic regimen for tonsillectomy should include paracetamol; non‐steroidal anti‐inflammatory drugs; and intravenous dexamethasone, with opioids as rescue analgesics. Analgesic adjuncts such as intra‐operative and postoperative acupuncture as well as postoperative honey are also recommended. Ketamine (only for children); dexmedetomidine; or gabapentinoids may be considered when some of the first‐line analgesics are contra‐indicated. Further randomised controlled trials are required to define risk and combination of drugs most effective for postoperative pain relief after tonsillectomy.
Keywords: analgesia, evidence‐based medicine, pain, systematic review, tonsillectomy
Recommendations
The basic analgesic regimen should include paracetamol and non‐steroidal anti‐inflammatory drugs (NSAIDs) administered pre‐operatively or intra‐operatively and continued postoperatively.
A single dose of intravenous (i.v.) dexamethasone is recommended for its analgesic and anti‐emetic effects.
Pre‐operative gabapentinoids, intra‐operative ketamine (only in children) and dexmedetomidine are recommended in patients with contra‐indications to the basic analgesic regimen.
Analgesic adjuncts such as intra‐operative and postoperative acupuncture and postoperative honey are recommended.
Opioids should be reserved as rescue analgesics in the postoperative period.
Why was this guideline developed?
Tonsillectomy is one of the most frequently performed surgical procedures and pain management remains challenging. The aim of this procedure‐specific guideline is to provide clinicians with up‐to‐date evidence for optimal pain management in tonsillectomy, and recommendations made based on this evidence, adverse effects and considerations regarding risks of interventions. Although other guidelines for tonsillectomy pain management are available, none have used the procedure‐specific postoperative pain management (PROSPECT) methodology to critically evaluate the available literature. This includes a systematic evidence‐based approach, the inclusion of a basic analgesic regimen for efficacy evaluation, a balance between efficacy and safety and a Delphi process for the final recommendations with international surgeons and anaesthetists involved.
How does this guideline differ from other guidelines?
The French Oto‐Rhino‐Laryngology Head and Neck Surgery Society [1] and Ericsson et al. [2] published guidelines for post‐tonsillectomy pain management in adults in 2014 and children in 2015, respectively. Both made recommendations based on expert consensus within the respective national societies based on published literature. These vary from the present guidelines in the process of our literature search, the use of a Delphi study to ratify our recommendations and we include contemporary studies from the last 5 years that are not included in previous guidelines. Moreover, previous guidelines do not highlight the importance of baseline analgesia. The PROSPECT approach to developing guidelines is unique such that the available evidence is critically assessed for current clinical relevance and the use of simple, non‐opioid analgesic such as paracetamol and NSAIDs as basic analgesics are considered. This approach reports clinical effectiveness by balancing the invasiveness of the analgesic interventions and the degree of pain after surgery, as well as balancing efficacy and adverse effects.
Introduction
The management of post‐tonsillectomy pain can be challenging and often inadequate. Tonsillectomy has been identified as one of the most painful surgical procedures [1], probably because pain remains poorly managed in clinical practice [1, 2, 3]. There are many reasons for undertreating pain after tonsillectomy, including clinicians underestimating the degree of pain associated with tonsillectomy surgery due to the fact that the surgical procedure is considered to be minimally invasive [1]. Moreover, despite numerous studies comparing and combining analgesics to find the most effective postoperative regimen, there is still no consensus on the best treatment strategy. Tonsillectomy is unique for several reasons including the type of tissue trauma, the exposure of the healing wound to movement of the pharynx during ingestion, the risk of bleeding and limitations in the choice of drugs, particularly in children. Thus, the ideal regimen providing adequate analgesia with few side‐effects after tonsillectomy remains to be defined. Guidelines on pain management after tonsillectomy have previously been published [4, 5].
The PROSPECT Working Group is a collaboration of surgeons and anaesthetists working to formulate procedure‐specific recommendations for pain management after common but potentially painful operations [6]. The recommendations are based on a procedure‐specific systematic review of randomised controlled trials. The methodology considers clinical practice, efficacy and adverse effects of analgesic techniques [7].
The aim of this systematic review was to evaluate the available literature on the management of pain after tonsillectomy in both adults and children. Pain scores and analgesic requirements were the primary focus, but other recovery outcomes, including adverse effects, were also assessed when reported, and the limitations of the data were reviewed. The ultimate aim was to develop recommendations for pain management after tonsillectomy.
Methods
The methods of this review adhered to the PROSPECT methodology as previously reported [8]. Specific to this study, the Embase, MEDLINE, PubMed, OpenGrey, Web of Science and Cochrane Databases (Cochrane Central Register of Controlled Trials; Cochrane Database of Abstracts or Reviews of Effects; Cochrane Database of Systematic Reviews) were searched for randomised controlled trials on 24 November 2019 with no time limitation. The search terms related to pain management or surgical interventions for tonsillectomy are in online Supporting Information Appendix S1. Studies that reported data pooled from patients undergoing mixed surgical procedures or procedures other than tonsillectomy or adenotonsillectomy were excluded, but we included studies in which a combination of tonsillectomy and adenotonsillectomy procedures was performed. We included studies of adults or paediatric patients (< 18 years of age).
Quality assessment, data extraction and data analysis adhered to the PROSPECT methodology [8]. Pain intensity scores were used as the primary outcome measure. In this study, we defined a change of more than 10 mm on the visual analogue scale or numerical rating score as clinically relevant. The aim was to qualitatively assess the data and not to perform a meta‐analysis.
Recommendations were made according to PROSPECT methodology [8]. In brief, this involved a grading of A–D according to the overall level of evidence, as determined by the quality of studies included; consistency of evidence; and study design. The proposed recommendations were sent to the PROSPECT Working Group for review and comments and a modified Delphi approach was utilised as previously described. Once a consensus was achieved, the lead authors drafted the final document, which was ultimately approved by the Working Group.
Results
The systematic literature search identified 7851 records. After exclusion of duplicates and studies not fulfilling our predefined inclusion criteria, 226 studies were included in the qualitative analysis (Fig. 1). The results of the methodological quality assessments of are summarised in online Supporting Information Table S1. The characteristics of the included studies are shown in online Supporting Information Tables S2 and S3.
Figure 1.
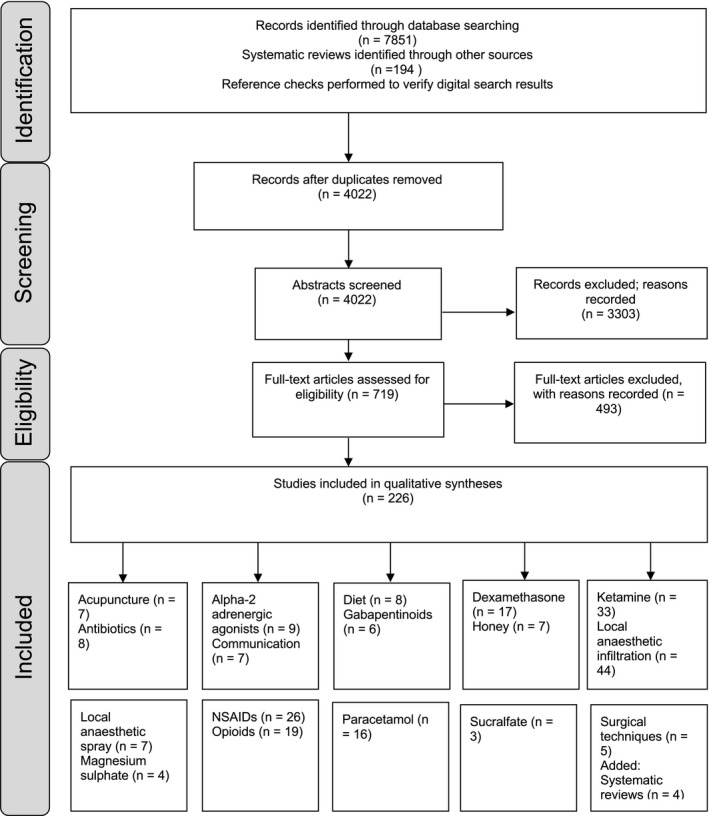
Diagram of included studies. NSAIDs, non‐steroidal anti‐inflammatory drugs.
Among the 226 studies included in our analysis, 158 included paediatric patients, 40 included adult patients and 28 involved a mixed population. The definition of adult and paediatric age groups varied considerably among studies, where some of the studies included within the paediatric group participants up to the age of 20, 18 or 16. Our results pool paediatric and adult patients as 28 of the studies included both and we were unable to elucidate the age‐groups patients in those studies. When results were different, or only studied in one population, we present specific analyses.
Paracetamol
Sixteen studies (two with a mixed population and 14 in children) involving 2058 patients were included. Paracetamol was administered intra‐operatively in 10 studies, intra‐operatively and postoperatively in four studies and postoperatively only in two studies. Two studies reported an analgesic benefit when compared with placebo [9, 10]; pain scores and morphine consumption were lower. In head‐to‐head comparisons with NSAIDs or dexamethasone, pain scores and morphine consumption were comparable [11, 12]. One study demonstrated that one dose of dexamethasone had a stronger analgesic effect than one dose of paracetamol when given intra‐operatively in children [13]. One study reported a weak benefit (reduction of opioid consumption) of the combination of NSAIDs with paracetamol [10]. Finally, the rectal route was found less efficient than i.v. or oral routes in one study [14].
Non‐steroidal anti‐inflammatory drugs
Twenty‐six studies (eight in adults; three with a mixed population; and 15 in children) including 2455 patients were considered for analysis. Pain was the primary outcome in all studies. Twenty studies supported the use of NSAIDs, showing an opioid‐sparing effect and a reduction in pain scores when compared with placebo. In most studies showing an effect, NSAIDs were administered intravenously or orally, pre‐ or intra‐operatively. Moreover, NSAIDs and cyclo‐oxygenase‐2 (COX‐2) inhibitors showed similar efficacy.
Three studies showed that the opioid‐sparing effect was associated with a reduction in postoperative nausea and vomiting [15, 16, 17]. As for complications associated with NSAIDS, there was no evidence for increased bleeding reported in the included studies. Two meta‐analyses published in 2013 confirmed that NSAIDs administration during tonsillectomy is not associated with an increased risk of bleeding [18, 19].
Local anaesthetic infiltration and topical application
Out of the 51 studies retrieved, 21 compared bupivacaine with placebo (online Supporting Information Table S3). No studies included a basic analgesic regimen. Looking at the paediatric and adult studies separately, 7/10 (70%) of adult studies reported a reduction in pain scores after local anaesthetic infiltration, while 15/31 (48%) of paediatric studies and 10/10 (100%) of the mixed population studies were supportive of it.
However, the analgesic benefit reported in some studies was minor and limited to the very early postoperative period [20, 21]. No evidence favouring one local anaesthetic agent over another was found. The technique of infiltration itself was not standardised in the literature and systemic absorption of local anaesthetic was an associated risk. Indeed, three studies have reported complications [22, 23, 24] including arrhythmias; bleeding; intravascular injection; and sedation. In detail, Unal et al. [22] reported greater sedation scores with bupivacaine and ropivacaine infiltration compared with saline infiltration. Tolska et al. [23] found that bleeding requiring haemostasis under local anaesthesia was more common in the ropivacaine group (10/54 (18%)) than in the control group (4/47 (8%)). One patient out of the 54 patients included in the ropivacaine group sustained postoperative bilateral pneumonia requiring 5 days of hospitalisation. Junaid et al. [24] reported six transient cardiac arrhythmias out of the 30 enrolled patients in the bupivacaine infiltration group and concluded that there was an increased risk of complications. Bean‐Lijewski et al. [25] described injection of 3–10 ml of bupivacaine 0.25–0.5% into each lateral pharyngeal space; the study was terminated after eight children had been enrolled because two out of four children receiving bupivacaine developed severe upper airway obstruction after tracheal extubation. This study concluded that bilateral local anaesthetic injection into the lateral pharyngeal space may induce an increased risk of severe upper airway obstruction and loss of protective reflexes.
Only one study [26] and one meta‐analysis [27] have been published since 2007 on the efficacy of lidocaine spray on postoperative pain after tonsillectomy. Jahromi et al. [26] reported that lidocaine spray reduced pain scores for only 20 min after surgery when compared with saline or ketamine spray. The meta‐analysis was inconclusive as the risk of bias was high in most of the included trials and poor reporting quality and inadequate data did not permit comprehensive and reliable conclusions to be made.
Peripheral nerve block
Glossopharyngeal nerve block demonstrated advantages over normal saline injection or no injection in four studies involving 315 patients [28, 29, 30, 31]. Two studies reported severe complications. Park et al. [29] described intravascular injection and tachycardia in 1 out of 25 patients while Debasish et al. [30] reported hypotension and bradycardia in 2 out of 32 patients (2/32).
Honey
The efficacy of postoperative honey as an analgesic adjuvant was tested in seven studies including a total of 547 patients. Only one study included adults exclusively; two studies included a mixed population; and the four other studies were performed in children. Three studies reported a reduction in pain scores and postoperative analgesic consumption when honey was administered on top of a basic analgesic regimen containing either paracetamol or NSAIDs [32, 33, 34] with no significant side‐effects. The analgesic effect was minor and the sample size was small in most studies, varying from 42 to 111 patients per study, suggesting further research in the majority of reports. Two meta‐analyses [35, 36] reported a benefit in terms of pain and a reduction in analgesic requirements, issuing low or very low‐grade recommendations. An additional positive outcome in these meta‐analyses was improved wound healing associated with the use of honey.
Opioids as rescue
Eleven out of 20 studies used tramadol administered either i.v. or via infiltration. Peritonsillar infiltration with tramadol may reduce pain and analgesic requirements when compared with placebo [37]. However, this may be a systemic effect and it cannot be recommended because of lack of data on safety of tramadol injection via this route. Intravenous tramadol had an analgesic effect postoperatively when administered once during surgery when compared with placebo [38]; however, no basic analgesic regimen was administered in this study. Other opioids have been less studied in recent years. Single studies are available for morphine infiltration [39], i.v. codeine [40], i.v. nalbuphine [41] and i.v. morphine [42]. Based on single studies for each opioid in recent years, recommendations are not possible. The risk of arterial oxygen desaturation associated with opioids in children with obstructive sleep apnoea has to be highlighted and assessed. The risk of postoperative nausea and vomiting needs to be prevented and the risk of respiratory depression needs to be evaluated in children with obstructive sleep apnoea.
Acupuncture
One meta‐analysis [43] and seven studies involving 522 patients were included [44, 45, 46, 47, 48, 49, 50]. The majority reported a benefit with a reduction in pain and analgesic requirements if acupuncture was used. Four studies compared acupuncture with sham [46, 47, 49, 50] and two with usual analgesic treatment [44, 45]. No complications have been described. Time points of acupuncture were pre, intra‐ and postoperatively.
α‐2 adrenergic agonists
Clonidine [51], and more recently, dexmedetomidine [52] have been studied peri‐operatively to reduce pain. Nine studies were included using α‐2 adrenergic agonist with 771 patients in total; the route of administration was either i.v. or by infiltrating the α‐2‐adrenergic agonist locally. A recent study documented no analgesic effect of clonidine 25 µg infiltration when a basic analgesic regimen was used [53]. There was no study assessing systemic clonidine in this setting. Clonidine is still included in some guidelines for analgesia after tonsillectomies in children based on efficacy in older studies [4]. However, these studies were mainly based on transferable results from other surgical procedures. Only two studies focused on tonsillectomy, and those did not show any additional analgesic effect of clonidine when used on top of adequate baseline medication after tonsillectomy.
From the eight studies concerning i.v. dexmedetomidine in paediatric patients, four documented an analgesic effect compared with placebo [54, 55, 56, 57] or propofol [58] but only for 30 min after surgery, while two studies did not show any benefit on pain scores compared with placebo [59, 60]. One study compared dexmedetomidine with morphine showing an inferior analgesic effect but less respiratory depression, and one compared with fentanyl [61] showing improvement in analgesia with dexmedetomidine. None of these studies assessed the benefit of adding dexmedetomidine on top of a basic analgesic regimen. Dexmedetomidine was associated with less agitation after sevoflurane‐based anaesthesia in two studies [55, 61]. In a meta‐analysis of dexmedetomidine for tonsillectomies, the drug came out favourably when compared with placebo or opioids in terms of postoperative pain, without any delay in post‐operative care unit discharge [62], although more sedation in the early recovery phase was reported.
Gabapentinoids
Four studies assessing oral gabapentin (including two with children) [63, 64, 65, 66] and two studies examining oral pregabalin in adults [67, 68] were included. All but one study [66] showed an analgesic effect of gabapentinoids when compared with placebo or when administered with paracetamol [68]. No study included a comparison with a combined basic analgesia regimen. Three studies reported side‐effects of gabapentinoids. Mathiesen et al. [68] reported more dizziness with 300 mg pregabalin. There are no clear conclusions to be drawn on dosing level or whether the pre‐operative dose should be repeated or not from these studies. However, data from meta‐analyses report that at least 600 mg gabapentin or 150 mg pregabalin is needed in the otherwise healthy adult [69, 70].
Dexamethasone
The benefit of steroids in patients having tonsillectomy was investigated in 17 studies [13, 86] including 1943 patients; 14 studies examined dexamethasone. Dexamethasone showed a significant analgesic effect after tonsillectomy when administered alone or in combination with other analgesics. Dexamethasone consistently reduced the incidence of nausea and vomiting after tonsillectomy, being effective in low doses, that is, 2–4 mg i.v. There was no consistent evidence concerning the appropriate dose, or a dose‐dependent effect for analgesia, but studies showing an analgesic effect in children use a dose of at least 0.15 mg.kg–1, whereas the adult studies used a total of 8 mg or more. There was no evidence of an increase bleeding risk with dexamethasone, or other side‐effects from the glucocorticoids, although none of the included studies have systematically addressed these effects. Known side‐effects, such as increased blood glucose levels, increased alertness and restlessness during night, are not addressed in the studies reviewed. One study [81] suggested a more relevant and sustained effect on analgesia with peritonsillar infiltration of dexamethasone instead of i.v. or oral administration. Other glucocorticoids, for example, oral prednisolone [74], seem to perform similarly, but are less studied for this purpose. Four recent meta‐analyses on the subject draw the same conclusions [87, 88, 89, 90].
Ketamine
Ketamine was investigated in 33 studies (32 with paediatric patients and one with a mixed population) including 2546 patients. Thus, recommendations on the use of ketamine for tonsillectomies were only possible for children (online Supporting Information Table S2).
Thirteen studies examined i.v. ketamine after tonsillectomy [91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103]. Ten studies compared i.v. ketamine with placebo [93, 94, 95, 103]; out of these ten studies, nine showed reduced pain intensity ratings, five of which demonstrated a reduction in morphine consumption [93, 94, 95, 98, 99, 100, 101, 102, 103] and one showed no significant effects [97]. In one study, i.v. ketamine improved the analgesic effect on top of paracetamol [99]. In all other studies comparing i.v. ketamine with placebo, baseline analgesia was not used or not mentioned. One study showed significantly better analgesia with ketamine plus i.v. dexamethasone compared with placebo or both drugs alone [96]. Another study showed better pain relief if i.v. ketamine was given pre‐operatively compared with postoperatively [98]. By comparing i.v. ketamine vs. opioids, there was significant improvement of pain scores in one study [102], reduced opioid consumption in another study [95] and no difference in two studies [92, 94]. Finally, one study compared i.v. ketamine plus midazolam with midazolam alone with only a transient effect after surgery [91]. Altogether, these studies using i.v. ketamine showed analgesic benefits of a single bolus of i.v. ketamine but almost all studies were done without baseline analgesia. In addition, patients experienced more side‐effects, predominantly sedation, with ketamine in four studies [93, 94, 97, 101].
There were 11 studies examining ketamine infiltration for tonsillectomy analgesia [93, 116]. Nine of these studies compared ketamine infiltration with placebo, and eight of these studies showed a significant benefit to ketamine infiltration [93, 98, 109, 110, 111, 112, 113, 114, 115]. One study comparing peritonsillar ketamine infiltration with i.v. ketamine showed better pain relief with infiltration [98]. Another study compared peritonsillar ketamine infiltration with tramadol infiltration and showed benefit of tramadol compared with ketamine [115]. One study compared ketamine with bupivacaine infiltration, alone or in combination. The combination of both was associated with a superior analgesic effect when compared with each drug alone [116]. Another study compared peritonsillar infiltration of ketamine with or without bupivacaine and meperidine, without any difference between each group [108]. Altogether, ketamine infiltration was consistently effective in reducing pain and analgesic requirements after tonsillectomy in children.
Topical administration of ketamine was investigated in two studies of which one showed inferior analgesia with ketamine when compared with tramadol [117] and the other showed improved analgesia compared with placebo and similar analgesia compared with i.v. morphine [118]. Intramuscular ketamine did not have analgesic efficacy [104] but subcutaneous ketamine was associated with similar analgesia to the i.v. route [100] and oral administration was less effective compared with infiltration [105, 106]. One study evaluated the effects of peritonsillar, i.v. or rectal administration of ketamine in children undergoing tonsillectomy and found no differences between the groups [107].
Other therapies
Four studies (289 patients) examining the analgesic effect of magnesium sulphate with pain as the primary outcome were included. One study [119] showed a transient effect of topical magnesium sulphate, while two studies [120, 121] did not show any difference when intra‐operative and postoperative i.v. magnesium sulphate was compared with placebo. One study [122] reported a reduction in pain scores when comparing oral postoperative magnesium sulphate with metamizol. Among the three meta‐analyses [123, 124, 125] included, two concluded that there was no benefit of i.v. administration of magnesium sulphate and two concluded that there was a small effect when administered locally.
Eight eligible studies [126, 127, 128, 129, 130, 131, 132, 133] reported inconclusive pain outcomes with the use of antibiotics. In studies reporting an analgesic effect, two tested antibiotic mouth wash. The analgesic effect lasted only one day and additional analgesic was still needed while the treatment was given for 3 to 7 days. One study reported more postoperative nausea and vomiting with the use of antibiotics [133].
Evidence from three small studies (188 patients) suggested a weak analgesic benefit when sucralfate was used as adjuvant with repeated applications over several days [134, 135, 136].
Six studies in children [137, 138, 139, 140, 141, 142] and one in adults [143] examined different methods to improve communication with patients or parents for better compliance with analgesics. Although most studies were small and of poor quality, the majority of them recommend enhanced parental education and/or telephone follow‐up to observe the need for analgesics at home and their side‐effects.
Eight studies assessed the effects of different dietary protocols on post‐tonsillectomy pain and complications. Six studies in children [144, 145, 146, 147, 148, 149], one in adults [150] and one with mixed age population [151] were included. Four studies [147, 148, 149, 151] with 204 participants did not demonstrate any benefit of restricting postoperative diet to liquids or to cold diet when pain scores, nausea or vomiting or bleeding were compared. Ice lolly use was effective in reducing pain scores for 1 hour postoperatively [144]. Minimising fasting time to 4 hours for solids and 2 hours for liquids improved postoperative outcomes in terms of analgesic requirements and postoperative nausea and vomiting in two studies [145, 146]. Only one study [150], which was of poor quality and included 49 participants, suggested effective analgesia and improved wound healing with the administration of ginger capsules postoperatively.
There were numerous studies examining surgical techniques, but these usually focused on outcomes such as bleeding, infection recurrence, hospital stay and costs. For this reason and also due to the fact that recent systematic reviews covering publications until 2016 have been published, we decided to only include studies published between 2017 and 2019. Five randomised studies [152, 153, 154, 155, 156] and four systematic reviews [157, 158, 159, 160] assessing the impact of surgical techniques on postoperative pain were included. There are two traditional methods of surgical removal of tonsils. The first is the original cold dissection approach, in which a dissector or a guillotine is used to mechanically remove the tonsils from adjacent tissue. The other method is electrocautery where electrical current is used to create burning heat and coagulation in the wound surface. In recent years, novel techniques have been introduced, including the laser evaporation technique, in which the tonsillar surface is treated with a laser beam and evaporates, and the coblation technique. Coblation involves the use of moderate heat to dissect the tonsils from the throat wall. The most recent is the vessel seal techniques, using ultrasound for the dissection. Compared with other techniques, laser tonsillotomy is less time consuming; does not require general anaesthesia; provides less bleeding and less pain but has a significant recurrence rate of tonsillitis. It is thus not considered as a method of complete tonsillectomy and not considered further for these recommendations. Coblation techniques have slightly less postoperative pain during the first day compared with cold dissection and electrocautery dissection techniques [155, 158, 159, 160], which seem to be similar in this aspect [154, 156, 160]. Vessel seal technology is new and promising, but remains understudied and results are inconclusive so far [157].
Discussion
Based on available evidence and the PROSPECT approach to providing recommendations, combinations of paracetamol and NSAIDs are recommended pre‐operatively or intra‐operatively, and continued into the postoperative period, unless there are contra‐indications (Table 1). In addition, a single intra‐operative dose of i.v. dexamethasone is also recommended (Table 1). Several interventions are not recommended for analgesia after tonsillectomy (Table 2).
Table 1.
Overall recommendations for pain management in patients undergoing tonsillectomy.
| Pre‐operative and intra‐operative |
| Paracetamol (Grade D) |
| Non‐steroidal anti‐inflammatory drugs (Grade A) |
| Dexamethasone intravenously (Grade A) |
| Pre‐operative gabapentinoids, or intra‐operative ketamine (for children), or intra‐operative dexmedetomidine may be considered, when basic analgesic regimen is contra‐indicated |
| Analgesic adjuncts: acupuncture (Grade B) |
| Postoperative |
| Paracetamol (Grade D) |
| Non‐steroidal anti‐inflammatory drugs (Grade A) |
| Opioid for rescue (Grade D) |
| Analgesic adjuncts |
| Acupuncture (Grade B) |
| Honey (Grade B) |
Table 2.
Analgesic interventions that are not recommended for pain management in patients undergoing tonsillectomy.
| Intervention | Reason for not recommending |
|---|---|
| Pre‐operative and intra‐operative | |
| Peritonsillar infiltration or topical application of local anaesthetics | Evidence of a short‐lasting effect but concerns of serious side‐effects |
| Oral or topical ketamine | Limited procedure‐specific evidence |
| Lidocaine spray | Lack of procedure‐specific evidence |
| Magnesium sulphate | Lack of procedure‐specific evidence |
| Tramadol infiltration | Lack of procedure‐specific evidence |
| Postoperative | |
| Dexamethasone | Lack of procedure‐specific evidence |
A systematic review [161] including 29 randomised controlled trials considered that single analgesics (e.g. paracetamol; NSAIDs; gabapentinoids; dextromethorphan; dexamethasone) provide only a weak to moderate benefit on post‐tonsillectomy pain on the day of surgery. Thus, the authors recommend a multimodal analgesic approach. These findings are in line with our recommendations. Of note, the concerns regarding the potential bleeding risk with the use of NSAIDs are not substantiated in recent studies. Several meta‐analyses did not report an increase in the risk of postoperative bleeding [18, 19]. Thus, most guidelines have been modified. Indeed, Swedish [4] and French [5] guidelines recommend NSAIDs as a first line treatment after tonsillectomy. Similar to NSAIDs, dexamethasone was once incriminated as increasing postoperative bleeding [162].
Intra‐operative acupuncture and postoperative honey are also recommended as analgesic adjuncts as they have been shown to provide superior pain relief when combined with paracetamol, NSAIDs or oral opioids. Importantly, these approaches have no reported side‐effects. However, intra‐operative acupuncture is rarely provided as it requires specific training.
Whenever the basic analgesic regimen (i.e. paracetamol and NSAIDs) is contra‐indicated or postoperative pain is expected to be greater than usual (e.g. patients consuming opioids pre‐operatively), we recommend considering intra‐operative i.v. ketamine or dexmedetomidine, and/or pre‐operative gabapentinoids. Despite a significant analgesic effect vs. placebo, these medications are not in the first‐line in our recommendations because of associated side‐effects. Indeed, ketamine is associated with hallucinations, agitation and sedation, and it should be administered at the beginning of the surgical procedure and only as single i.v. dose. Ketamine infiltration is not recommended because of the risks of systemic side‐effects after absorption [107, 163]. Gabapentinoids may cause sedation and dizziness at doses having an effect on pain scores or analgesic consumption [68]. Moreover, tonsillectomy is a procedure associated with risks of hypoxaemia, therefore adding gabapentinoids and opioids as rescue could increase the risk of respiratory depression [164]. A similar dilemma holds true for dexmedetomidine, which is associated with the risk of sedation, hypotension and bradycardia. Clonidine is recommended in some guidelines for analgesia after tonsillectomy in children based on efficacy in older studies and transferable results from studies other than tonsillectomy [4]. Of note, tonsillectomy is a short procedure and a single dose of one of these three medications can delay postoperative recovery.
Analgesia was reported with local anaesthesia infiltration when compared with placebo. However, this benefit was only short‐lasting and was only demonstrated in studies that were not using a basic analgesic regimen with paracetamol and a NSAID combination. Moreover, studies have reported complications associated with the technique. Indeed, tonsillar infiltration may not be as safe as other infiltration in other areas because of the neurovascular bundle in the vicinity that could explain high potential for side‐effects.
We cannot recommend a specific surgical technique that would influence pain after tonsillectomy, because most studies have evaluated surgical technique with respect to issues of bleeding as well as cost efficacy rather than focusing on differences in postoperative pain.
Some of the limitations with this review are related to the limitations with the individual studies included. There was considerable heterogeneity between studies, such as variable dosing regimens, methods of administration control groups and time‐points of pain assessments. The small sample size of most studies has the potential to overestimate effects. Also, the analgesic interventions were not always evaluated against a control group that included an optimised multimodal analgesic regimen. A significant proportion of the included studies assessed unimodal analgesic therapies rather than broader and more comprehensive analgesic techniques. Ideally, all patients should receive an optimised analgesic regimen, and the added procedure‐specific benefit of individual interventions should then be tested against this baseline [165]. Also, there was significant heterogeneity in study designs with respect to the analgesic regimen. Moreover, as it is not part of our methodology, we did not weight the recommendations nor make dosage recommendations.
Future adequately powered studies should assess the effects of analgesic interventions not only on pain, opioid consumption, opioid‐related adverse events and complications associated with the intervention, but also outcome measures such as time to ambulation, length of hospital stay and functional outcomes after discharge. Another important aspect will be to bring patient‐specific risk‐factors for postoperative pain into the studies.
In summary, this review has identified an analgesic regimen for optimal pain management after tonsillectomy (Table 1). A balance of evidence‐based analgesic efficacy and potential risks of the analgesic intervention determine these recommendations. Peri‐operative pain management for tonsillectomy surgery should include, unless contra‐indicated, paracetamol, NSAIDs, dexamethasone, honey, acupuncture and opioid as rescue. As second‐line treatment, gabapentinoids, ketamine or dexmedetomidine can be used.
Supporting information
Appendix S1. Search strategy used for this review.
Table S1. Quality assessment and level of evidence assigned to the randomised trials included in this review.
Table S2. Summary of key results from studies evaluating systemic analgesics, systemic analgesic adjuncts, regional analgesia and surgical procedures used to support the recommended interventions in patients after tonsillectomy.
Table S3. Summary of key results from studies evaluating systemic analgesics, regional analgesia, perineural analgesic adjuncts and surgical procedures used to support interventions that are not recommended for analgesic benefit in patients having tonsillectomy.
Acknowledgements
We thank M. Stone (Clinical Effectiveness Librarian, University Hospitals of North Midlands NHS Trust). PROSPECT is supported by an unrestricted grant from the European Society of Regional Anaesthesia and Pain Therapy (ESRA). In the past, PROSPECT had received unrestricted grants from Pfizer Inc. New York, NY, USA and Grunenthal, Aachen, Germany. GJ has received honoraria from Baxter and Pacira Pharmaceuticals. FB has received honoraria from Pfizer, The Medicine Company, Abbott France and Nordic Pharma France. HK has received honoraria from Pfizer and Grunenthal. The Anesthesiology Unit of the University of Western Australia, but not SS personally, has received research and travel funding and speaking and consulting honoraria from bioCSL, Eli Lilly, Indivior, iX Biopharma and Pfizer. NR has received honoraria from Baxter and Sintetica. MVdV has received honoraria from Sintetica, Grunenthal, Vifor Pharma, MSD, Nordic Pharma, Janssen Pharmaceuticals, Heron Therapeutics and Aquettant. HB has received honoraria from Orion, Abbvie and Aspen. No other competing interests declared.
Appendix 1. PROSPECT Working Group
E. Albrecht, H Beloeil, F. Bonnet, S. Freys, G. P. Joshi, H. Kehlet, P. Lavand’homme, P. Lirk, D. Lobo, E. Pogatzki‐Zahn, N. Rawal, J. Raeder, A. Sauter, S. Schug, M. van de Velde.
Contributor Information
N. Aldamluji, @AldamlujiN.
H. Beloeil, Email: helene.beloeil@chu-rennes.fr.
the PROSPECT Working Group collaborators*:
E Albrecht, H Beloeil, F Bonnet, S Freys, G. P. Joshi, H Kehlet, P. Lavand’homme, P Lirk, D Lobo, E Pogatzki‐Zahn, N Rawal, J Raeder, A Sauter, S Schug, and M van de Velde
References
- 1. Gerbershagen HJ, Aduckathil S, van Wijck AJM, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery. Anesthesiology 2013; 118: 934–44. [DOI] [PubMed] [Google Scholar]
- 2. Maier C, Nestler N, Richter H, et al. The quality of pain management in German hospitals. Deutsches Aerzteblatt Online 2010; 107: 607–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Persino PR, Saleh L, Walner DL. Pain control following tonsillectomy in children: a survey of patients. International Journal of Pediatric Otorhinolaryngology 2017; 103: 76–9. [DOI] [PubMed] [Google Scholar]
- 4. Ericsson E, Brattvvall M, Lundeberg S. Swedish guidelines for the treatment of pain in tonsil surgery in pediatric patients up to 18 years. International Journal of Pediatric Otorhinolaryngology 2015; 79: 443–50. [DOI] [PubMed] [Google Scholar]
- 5. Paganelli A, Khalfallah SA, Brunaud A, et al. Guidelines (short version) of the French Oto‐Rhino‐Laryngology ‐ Head and Neck Surgery Society (SFORL) for the management of post‐tonsillectomy pain in adults. European Annals of Otorhinolaryngology‐Head and Neck Diseases 2014; 131: 227–32. [DOI] [PubMed] [Google Scholar]
- 6. Joshi GP, Schug SA, Kehlet H. Procedure‐specific pain management and outcome strategies. Best Practice and Research Clinical Anaesthesiology 2014; 28: 191–201. [DOI] [PubMed] [Google Scholar]
- 7. Joshi GP, Kehlet H, Beloeil H, et al. Guidelines for perioperative pain management: need for re‐evaluation. British Journal of Anaesthesia 2017; 119: 720–2. [DOI] [PubMed] [Google Scholar]
- 8. Joshi GP, Van de Velde M, Kehlet H, et al. Development of evidence‐based recommendations for procedure‐specific pain management: PROSPECT methodology. Anaesthesia 2019; 74: 1298–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Atef A, Fawaz AA. Intravenous paracetamol is highly effective in pain treatment after tonsillectomy in adults. European Archives of Oto‐Rhino‐Laryngology 2008; 265: 351–5. [DOI] [PubMed] [Google Scholar]
- 10. Salonen A, Silvola J, Kokki H. Does 1 or 2 g paracetamol added to ketoprofen enhance analgesia in adult tonsillectomy patients? Acta Anaesthesiologica Scandinavica 2009; 53: 1200–6. [DOI] [PubMed] [Google Scholar]
- 11. Kocum AI, Sener M, Caliskan E, et al. Intravenous paracetamol and dipyrone for postoperative analgesia after day‐case tonsillectomy in children: a prospective, randomized, double blind, placebo controlled study. Brazilian Journal of Otorhinolaryngology 2013; 79: 89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Merry AF, Edwards K‐E, Ahmad Z, Barber C, Mahadevan M, Frampton C. Randomized comparison between the combination of acetaminophen and ibuprofen and each constituent alone for analgesia following tonsillectomy in children. Canadian Journal of Anesthesia 2013; 60: 1180–9. [DOI] [PubMed] [Google Scholar]
- 13. Faiz SHR, Rahimzadeh P, Alebouyeh MR, Sedaghat M. A randomized controlled trial on analgesic effects of intravenous acetaminophen versus dexamethasone after pediatric tonsillectomy. Iranian Red Crescent Medical Journal 2013; 15: e9267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Haddadi S, Marzban S, Karami MS, Heidarzadeh A, Parvizi A, Nabi BN. Comparing the duration of the analgesic effects of intravenous and rectal acetaminophen following tonsillectomy in children. Anesthesiology and Pain Medicine 2014; 4: e13175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moss JR, Watcha MF, Bendel LP, McCarthy DL, Witham SL, Glover CD. A multicenter, randomized, double‐blind placebo‐controlled, single dose trial of the safety and efficacy of intravenous ibuprofen for treatment of pain in pediatric patients undergoing tonsillectomy. Pediatric Anesthesia 2014; 24: 483–9. [DOI] [PubMed] [Google Scholar]
- 16. Li X, Zhou M, Xia Q, Li J. Parecoxib sodium reduces the need for opioids after tonsillectomy in children: a double‐blind placebo‐controlled randomized clinical trial. Canadian Journal of Anesthesia 2016; 63: 268–74. [DOI] [PubMed] [Google Scholar]
- 17. Hamza A, Hayat U, Khan QMK. To compare the efficacy of ketorolac and pethidine for postoperative pain relief in first 24 hours after tonsillectomy. Pakistan Journal of Medical and Health Sciences 2012; 6: 326–8. [Google Scholar]
- 18. Lewis SR, Nicholson A, Cardwell ME, Siviter G, Smith AF. Nonsteroidal anti‐inflammatory drugs and perioperative bleeding in paediatric tonsillectomy. Cochrane Database of Systematic Reviews 2013; 7: CD003591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Riggin L, Ramakrishna J, Sommer DD, Koren G. A 2013 updated systematic review & meta‐analysis of 36 randomized controlled trials; no apparent effects of non steroidal anti‐inflammatory agents on the risk of bleeding after tonsillectomy. Clinical Otolaryngology 2013; 38: 115–29. [DOI] [PubMed] [Google Scholar]
- 20. Fikret K, Nur KF, Gokhan T, Afsin OO, Atila K, Selcuk O. Comparison of peritonsillar levobupivacaine and bupivacaine infiltration for post‐tonsillectomy pain relief in children: Placebo‐controlled clinical study. International Journal of Pediatric Otorhinolaryngology 2011; 75: 322–6. [DOI] [PubMed] [Google Scholar]
- 21. Kasapoglu F, Demir UL, Kaya FN, Cetin YS, Yavascaoglu B. The effects of levobupivacaine infiltration on post‐tonsillectomy pain relief in adults: a single‐blinded, randomized, and controlled clinical study. European Archives of Oto‐Rhino‐Laryngology 2013; 270: 761–6. [DOI] [PubMed] [Google Scholar]
- 22. Unal Y, Pampal K, Korkmaz S, Arslan M, Zengin A, Kurtipek O. Comparison of bupivacaine and ropivacaine on postoperative pain after tonsillectomy in paediatric patients. International Journal of Pediatric Otorhinolaryngology 2007; 71: 83–7. [DOI] [PubMed] [Google Scholar]
- 23. Tolska HK, Takala A, Blomgren K, Hamunen K, Kontinen V. Topical ropivacaine in prevention of post‐tonsillectomy pain in adults. Anesthesia and Analgesia 2017; 124: 1459–66. [DOI] [PubMed] [Google Scholar]
- 24. Junaid M, Halim MS, Onali MAS, Qadeer S, Khan HU, Ali NS. Intraoperative use of analgesics in tonsillar fossa and postoperative evaluation with visual analogue scale scores—a prospective, randomized, placebo‐controlled, double‐blind clinical trial. International Archives of Otorhinolaryngology 2020; 24: e62–e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bean‐Lijewski J. Glossopharyngeal nerve block for pain relief after pediatric tonsillectomy: retrospective analysis and two cases of life‐threatening upper airway obstruction from an interrupted trial. Anesthesia and Analgesia 1997; 84: 1232–8. [DOI] [PubMed] [Google Scholar]
- 26. Jahromi SAH, Valami SMH, Hatamian S. Comparison between effect of lidocaine, morphine and ketamine spray on post‐tonsillectomy pain in children. Anesthesia and Pain Medicine 2012; 2: 17–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fedorowicz Z, van Zuuren EJ, Nasser M, Carter B, Al Langawi JH. Oral rinses, mouthwashes and sprays for improving recovery following tonsillectomy. Cochrane Database of Systematic Reviews 2013; CD007806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mohamed SK, Ibraheem AS, Abdelraheem MG. Preoperative intravenous dexamethasone combined with glossopharyngeal nerve block: role in pediatric postoperative analgesia following tonsillectomy. European Archives of Oto‐Rhino‐Laryngology 2009; 266: 1815–9. [DOI] [PubMed] [Google Scholar]
- 29. Park H‐P, Hwang J, Park S‐H, Jeon Y‐T, Bahk J‐H, Oh Y‐S. The effects of glossopharyngeal nerve block on postoperative pain relief after tonsillectomy: the importance of the extent of obtunded gag reflex as a clinical indicator. Anesthesia and Analgesia 2007; 105: 267–71. [DOI] [PubMed] [Google Scholar]
- 30. Debasish G, Anindita S, Aryabrata D, Arunabha S. Glossopharyngeal nerve block with long acting local anaesthetic agent (bupivacaine) and it’s effect on early post‐operative period in adult tonsillectomy: a prospective study. Indian Journal of Otolaryngology and Head and Neck Surgery 2019; 71: 390–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ahmed SA, Omara AF. The effect of glossopharyngeal nerve block on post‐tonsillectomy pain of children; randomized controlled trial. Anesthesiology and Pain Medicine 2019; 9: e90854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Boroumand P, Zamani MM, Saeedi M, Rouhbakhshfar O, Motlagh SRH, Moghaddam FA. Post tonsillectomy pain: can honey reduce the analgesic requirements? Anesthesiology and Pain Medicine 2013; 3: 198–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mohebbi S, Nia FH, Kelantari F, Nejad SE, Hamedi Y, Abd R. Efficacy of honey in reduction of post tonsillectomy pain, randomized clinical trial. International Journal of Pediatric Otorhinolaryngology 2014; 78: 1886–9. [DOI] [PubMed] [Google Scholar]
- 34. Prasad AS, Ahmed MN, Ahmed SM, et al. Post‐operative pain management of tonsillectomy patients; clinical evaluation of using oral honey in 78 patients. Journal of Evolution of Medical and Dental Sciences 2015; 4: 799–807. [Google Scholar]
- 35. Lal A, Chohan K, Chohan A, Chakravarti A. role of honey after tonsillectomy: a systematic review and meta‐analysis of randomised controlled trials. Clinical Otolaryngology 2017; 42: 651–60. [DOI] [PubMed] [Google Scholar]
- 36. Hwang SH, Song JN, Jeong YM, Lee YJ, Kang JM. The efficacy of honey for ameliorating pain after tonsillectomy: a meta‐analysis. European Archives of Oto‐Rhino‐Laryngology 2016; 273: 811–8. [DOI] [PubMed] [Google Scholar]
- 37. Akkaya T, Bedirli N, Ceylan T, et al. Comparison of intravenous and peritonsillar infiltration of tramadol for postoperative pain relief in children following adenotonsillectomy. European Journal of Anaesthesiology 2009; 26: 333–7. [DOI] [PubMed] [Google Scholar]
- 38. Ali SM, Shahrbano S, Ulhaq TS. Tramadol for pain relief in children undergoing adenotonsillectomy: a comparison with dextromethorphan. Laryngoscope 2008; 118: 1547–9. [DOI] [PubMed] [Google Scholar]
- 39. Akural EI, Alahuhta S, Ohtonen P, Lopponen H. Peritonsillar morphine infiltration to prevent early postoperative pain after tonsillectomy A randomised controlled trial. European Journal of Anaesthesiology 2016; 33: 607–9. [DOI] [PubMed] [Google Scholar]
- 40. Rawlinson E, Walker A, Skone R, Thillaivasan A, Bagshaw O. A randomised controlled trial of two analgesic techniques for paediatric tonsillectomy. Anaesthesia 2011; 66: 919–24. [DOI] [PubMed] [Google Scholar]
- 41. Akhtar N, Iqbal M. Comparison of two different doses of nalbuphine for postoperative tonsillectomy pain in children. Pakistan Journal of Medical and Health Sciences 2014; 8: 324–30. [Google Scholar]
- 42. Kelly LE, Sommer DD, Ramakrishna J, et al. Morphine or ibuprofen for post‐tonsillectomy analgesia: a randomized trial. Pediatrics 2015; 135: 307–13. [DOI] [PubMed] [Google Scholar]
- 43. Cho HK, Park IJ, Jeong YM, Lee YJ, Hwang SH. Can perioperative acupuncture reduce the pain and vomiting experienced after tonsillectomy? A meta‐analysis. Laryngoscope 2016; 126: 608–15. [DOI] [PubMed] [Google Scholar]
- 44. Dingemann J, Plewig B, Baumann I, Plinkert PK, Sertel S. Acupuncture in posttonsillectomy pain: A prospective double‐blind randomized controlled trial. German version. HNO 2017; 65: 643–50. [DOI] [PubMed] [Google Scholar]
- 45. Gilbey P, Bretler S, Avraham Y, Sharabi‐Nov A, Ibrgimov S, Luder A. Acupuncture for posttonsillectomy pain in children: a randomized, controlled study. Pediatric Anesthesia 2015; 25: 603–9. [DOI] [PubMed] [Google Scholar]
- 46. Kager H, Likar R, Jabarzadeh H, Sittl R, Breschan C, Szeles J. Electrical punctual stimulation (P‐STIM) with ear acupuncture following tonsillectomy, a randomised, controlled pilot study. Acute Pain 2009; 11: 101–6. [Google Scholar]
- 47. Tsao GJ, Messner AH, Seybold J, Sayyid ZN, Cheng AG, Golianu B. Intraoperative acupuncture for posttonsillectomy pain: A randomized, double‐blind, placebo‐controlled trial. Laryngoscope 2015; 125: 1972–8. [DOI] [PubMed] [Google Scholar]
- 48. Plunkett A, McCoart A, Howard RS, Dennison E, Bartoszek M. A randomized, single‐blind, prospective trial of auricular ‘battlefield’ acupuncture for the reduction of postoperative tonsillectomy pain in adults. Pain Management 2018; 8: 287–95. [DOI] [PubMed] [Google Scholar]
- 49. Pouy S, Etebarian Khorasgani A, Azizi‐Qadikolaee A, Yaghobi Y. Effect of acupressure on post tonsillectomy pain in adolescents: a randomized, single‐blind, placebo‐controlled trial study. International Journal of Adolescent Medicine and Health 2019. Epub 9 July. doi.org/10.1515/ijamh‐2019‐0065 [DOI] [PubMed] [Google Scholar]
- 50. Shah AN, Moore CB, Brigger MT. Auricular acupuncture for adult tonsillectomy. Laryngoscope 2020; 130: 1907–12. [DOI] [PubMed] [Google Scholar]
- 51. Kranke P, Jokinen J, Pace NL, et al. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery. Cochrane Database of Systematic Reviews 2015; 6: CD009642. [DOI] [PubMed] [Google Scholar]
- 52. Schnabel A, Reichl SU, Poepping DM, Kranke P, Pogatzki‐Zahn E, Zahn PK. Efficacy and safety of intraoperative dexmedetomidine for acute postoperative pain in children: a meta‐analysis of randomized controlled trials. Pediatric Anesthesia 2013; 23: 170–9. [DOI] [PubMed] [Google Scholar]
- 53. Moss JR, Cofer S, Hersey S, et al. Comparison of clonidine, local anesthetics, and placebo for pain reduction in pediatric tonsillectomy. Archives of Otolaryngology‐Head and Neck Surgery 2017; 137: 591–7. [DOI] [PubMed] [Google Scholar]
- 54. Abdel‐ghaffar HS, Abdel‐Haleem AK. Efficacy and safety of intraoperative dexmedetomidine in pediatric posttonsillectomy pain: peritonsillar versus intravenous administration. Egyptian Journal of Anaesthesia 2011; 27: 219–25. [Google Scholar]
- 55. Mizrak A, Karatas E, Saruhan R, et al. Does dexmedetomidine affect intraoperative blood loss and clotting tests in pediatric adenotonsillectomy patients? Journal of Surgical Research 2013; 179: 94–8. [DOI] [PubMed] [Google Scholar]
- 56. Abdel‐Ghaffar HS, Abdel‐Wahab AH, Roushdy MM. Oral trans‐mucosal dexmedetomidine for controlling of emergence agitation in children undergoing tonsillectomy: a randomized controlled trial. Brazilian Journal of Anesthesiology 2019; 69: 469–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Li H, Zhang L, Shi M, Yang S, Li S, Gao S. Impact of dexmedetomidine on pediatric agitation in the postanesthesia care unit. Journal of Perianesthesia Nursing 2018; 33: 53–7. [DOI] [PubMed] [Google Scholar]
- 58. Abdellatif A, Ali M. Prevention of sevoflurane related emergence agitation in children undergoing adenotonsillectomy: a comparison of dexmedetomidine and propofol. Saudi Journal of Anaesthesia 2013; 7: 296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Bedirli N, Akçabay M, Emik U. Tramadol vs dexmedetomidine for emergence agitation control in pediatric patients undergoing adenotonsillectomy with sevoflurane anesthesia: prospective randomized controlled clinical study. BMC Anesthesiology 2017; 17: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Sharma K, Kumar M, Gandhi R. Effect of single‐dose dexmedetomidine on intraoperative hemodynamics and postoperative recovery during pediatric adenotonsillectomy. Anesthesia: Essays and Researches 2019; 13: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Patel A, Davidson M, Tran MCJ, et al. Dexmedetomidine infusion for analgesia and prevention of emergence agitation in children with obstructive sleep apnea syndrome undergoing tonsillectomy and adenoidectomy. Anesthesia and Analgesia 2010; 111: 1004–10. [DOI] [PubMed] [Google Scholar]
- 62. Cho HK, Yoon HY, Jin HJ, Hwang SH. Efficacy of dexmedetomidine for perioperative morbidities in pediatric tonsillectomy: a metaanalysis. Laryngoscope 2018; 128: E184–E193. [DOI] [PubMed] [Google Scholar]
- 63. Amani S, Abedinzadeh MR. Effects of oral gabapentin, local bupivacaine and intravenous pethidine on post tonsillectomy pain. Iranian Journal of Otorhinolaryngology 2015; 27: 343–8. [PMC free article] [PubMed] [Google Scholar]
- 64. Amin SM, Amr YM. Comparison between preemptive gabapentin and paracetamol for pain control after adenotonsillectomy in children. Anesthesia: Essays and Researches 2011; 5: 167–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Jeon E, Park Y‐S, Park SS, Lee S‐K, Kim D‐H. The effectiveness of gabapentin on post‐tonsillectomy pain control. European Archives of Oto‐Rhino‐Laryngology 2009; 266: 1605–9. [DOI] [PubMed] [Google Scholar]
- 66. Sanders JG, Cameron C, Dawes PJD. Gabapentin in the management of pain following tonsillectomy: a randomized double‐blind placebo‐controlled trial. Otolaryngology‐Head and Neck Surgery 2017; 157: 781–90. [DOI] [PubMed] [Google Scholar]
- 67. Park SS, Kim D‐H, Nam I‐C, Lee I‐H, Hwang J‐W. The effectiveness of pregabalin for post‐tonsillectomy pain control: a randomized controlled trial. PLoS One 2015; 10: e0117161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Mathiesen O, Jorgensen DG, Hilsted KL, et al. Pregabalin and dexamethasone improves post‐operative pain treatment after tonsillectomy. Acta Anaesthesiologica Scandinavica 2011; 55: 297–305. [DOI] [PubMed] [Google Scholar]
- 69. Hwang SH, Park IJ, Cho YJ, Jeong YM, Kang JM. The efficacy of gabapentin/pregabalin in improving pain after tonsillectomy: a meta‐analysis. Laryngoscope 2016; 126: 357–66. [DOI] [PubMed] [Google Scholar]
- 70. Sanders JG, Dawes PJD. Gabapentin for perioperative analgesia in otorhinolaryngology–head and neck surgery. Otolaryngology‐Head and Neck Surgery 2016; 155: 893–903. [DOI] [PubMed] [Google Scholar]
- 71. Usman A, Bajwa Rizwan Akbar KAA. To compare the mean pain score after giving dexamethasone versus placebo following tonsillectomy in children with recurrent acute tonsillitis. Pakistan Journal of Medical and Health Sciences 2018; 12: 1327–9. [Google Scholar]
- 72. Lakhan MS, Ramlan S, Somayaji G. Efficacy of single dose preoperative intravenous dexamethasone for postoperative pain relief in tonsillectomy patients. International Journal of Otorhinolaryngology and Head and Neck Surgery 2017; 3: 323. [Google Scholar]
- 73. Montazeri K, Okhovat A, Honarmand A, Safavi MR, Ashrafy L. Pre‐incisional infiltration of tonsils with dexamethasone dose not reduce posttonsillectomy vomiting and pain in children. Saudi Journal of Anaesthesia 2009; 3: 53–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Park SK, Kim J, Kim JM, Yeon JY, Shim WS, Lee DW. Effects of oral prednisolone on recovery after tonsillectomy. Laryngoscope 2015; 125: 111–7. [DOI] [PubMed] [Google Scholar]
- 75. Thimmasettaiah NB, Chandrappa RG. A prospective study to compare the effects of pre, intra and post operative steroid (dexamethasone sodium phosphate) on post tonsillectomy morbidity. Journal of Pharmacology and Pharmacotherapeutics 2012; 3: 254–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Topal K, Aktan B, Sakat MS, Kilic K, Gozeler MS. Post‐operative pain control after tonsillectomy: dexametasone vs tramadol. Acta Oto‐Laryngologica 2017; 137: 618–22. [DOI] [PubMed] [Google Scholar]
- 77. Tuhanioglu B, Erkan SO. Tonsillectomy pain control with IV dexamethasone, infiltrated dexamethasone and infiltrated bupivacaine; a randomised, double‐blind, placebo controlled, prospective clinical trial. Journal of the Pakistan Medical Association 2018; 68: 1002–8. [PubMed] [Google Scholar]
- 78. Vaiman M, Krakovski D, Haitov Z. Oxycodone and Dexamethasone for pain management after tonsillectomy: a placebo‐controlled EMG assessed clinical trial. Medical Science Monitor 2011; 17: 125–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Attia TM. Effect of paracetamol/prednisolone versus paracetamol/ibuprofen on post‐operative recovery after adult tonsillectomy. American Journal of Otolaryngology 2018; 39: 476–80. [DOI] [PubMed] [Google Scholar]
- 80. Bhattacharya D, Mazumdar S, Chowdhury S, Basu S, Saha S. Single dose IV dexamethasone with preemptive transdermal diclofenac patch reduces opioid requirement and postoperative morbidity following tonsillectomy. Journal of Anaesthesiology, Clinical Pharmacology 2009; 25: 29–32. [Google Scholar]
- 81. Gao W, Zhang QR, Jiang L, Geng JY. Comparison of local and intravenous dexamethasone for postoperative pain and recovery after tonsillectomy. Otolaryngology‐Head and Neck Surgery 2015; 152: 530–5. [DOI] [PubMed] [Google Scholar]
- 82. Hashmi MA, Ahmed A, Aslam S, Mubeen M. Post‐tonsillectomy pain and vomiting: role of pre‐operative steroids. Journal of the College of Physicians and Surgeons Pakistan 2012; 22: 505–9. [PubMed] [Google Scholar]
- 83. Hermans V, De Pooter F, De Groote F, De Hert S, Jean Van der Linden P. Effect of dexamethasone on nausea, vomiting, and pain in paediatric tonsillectomy. British Journal of Anaesthesia 2012; 109: 427–31. [DOI] [PubMed] [Google Scholar]
- 84. Khalili G, Sajedi P, Shafa A, Hosseini B, Seyyedyousefi H. A randomized evaluation of intravenous dexamethas one versus oral acetaminophen codeine in pediatric adenotonsillectomy: emergence agitation and analgesia. Middle East Journal of Anesthesiology 2012; 21: 499–504. [PubMed] [Google Scholar]
- 85. Kim MS, Cote CJ, Cristoloveanu C, et al. There is no dose‐escalation response to dexamethasone (0.0625‐1.0 mg/kg) in pediatric tonsillectomy or adenotonsillectomy patients for preventing vomiting, reducing pain, shortening time to first liquid intake, or the incidence of voice change. Anesthesia and Analgesia 2007; 104: 1052–8. [DOI] [PubMed] [Google Scholar]
- 86. Lachance M, Lacroix Y, Audet N, Savard P, Thuot F. The use of dexamethasone to reduce pain after tonsillectomy in adults: a double‐blind prospective randomized trial. Laryngoscope 2008; 118: 232–6. [DOI] [PubMed] [Google Scholar]
- 87. Francis DO, Chinnadurai S, Sathe NA, Morad A, Jordan AK, Krishnaswami S, Fonnesbeck CMM. Tonsillectomy for obstructive sleep‐disordered breathing or recurrent throat infection in children. Agency for Healthcare Research and Quality 2017; 16: EHC042‐EF. [PubMed] [Google Scholar]
- 88. Batistaki C, Kaminiotis E, Papadimos T, Kostopanagiotou G. A narrative review of the evidence on the efficacy of dexamethasone on postoperative analgesic consumption. Clinical Journal of Pain 2017; 33: 1037–46. [DOI] [PubMed] [Google Scholar]
- 89. Bellis JR, Pirmohamed M, Nunn AJ, et al. Dexamethasone and haemorrhage risk in paediatric tonsillectomy: a systematic review and meta‐analysis. British Journal of Anaesthesia 2014; 113: 23–42. [DOI] [PubMed] [Google Scholar]
- 90. Steward DL, Grisel J, Meinzen‐Derr J. Steroids for improving recovery following tonsillectomy in children. Cochrane Database of Systematic Reviews 2011; 8: CD003997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Bameshki SA, Salari MR, Bakhshaee M, Razavi M. Effect of ketamine on post‐tonsillectomy sedation and pain relief. Iranian Journal of Otorhinolaryngology 2015; 27: 429–34. [PMC free article] [PubMed] [Google Scholar]
- 92. Taheri R, Seyedhejazi M, Ghojazadeh M, Ghabili K, Shayeghi S. Comparison of ketamine and fentanyl for postoperative pain relief in children following adenotonsillectomy. Pakistan Journal of Biological Sciences 2011; 14: 572–7. [DOI] [PubMed] [Google Scholar]
- 93. Dal D, Celebi N, Elvan EG, Celiker V, Aypar U. The efficacy of intravenous or peritonsillar infiltration of ketamine for postoperative pain relief in children following adenotonsillectomy. Pediatric Anesthesia 2007; 17: 263–9. [DOI] [PubMed] [Google Scholar]
- 94. Abdelhalim AA, Alarfaj AM. The effect of ketamine versus fentanyl on the incidence of emergence agitation after sevoflurane anesthesia in pediatric patients undergoing tonsillectomy with or without adenoidectomy. Saudi Journal of Anaesthesia 2013; 7: 392–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Abu‐Shahwan I. Ketamine does not reduce postoperative morphine consumption after tonsillectomy in children. Clinical Journal of Pain 2008; 24: 395–8. [DOI] [PubMed] [Google Scholar]
- 96. Safavi M, Honarmand A, Habibabady MR, Baraty S, Aghadavoudi O. Assessing intravenous ketamine and intravenous dexamethasone separately and in combination for early oral intake, vomiting and postoperative pain relief in children following tonsillectomy. Medicinski Arhiv 2012; 66: 111–5. [DOI] [PubMed] [Google Scholar]
- 97. Batra YK, Shamsah M, Al‐Khasti M, Rawdhan HJF, Al‐Qattan A, Belani KG. Intraoperative small‐dose ketamine does not reduce pain or analgesic consumption during perioperative opioid analgesia in children after VIP tonsillectomy. International Journal of Clinical Pharmacology and Therapeutics 2007; 45: 155–60. [DOI] [PubMed] [Google Scholar]
- 98. Khademi S, Ghaffarpasand F, Heiran HR, Yavari MJ, Motazedian S, Dehghankhalili M. Intravenous and peritonsillar infiltration of ketamine for postoperative pain after adenotonsillectomy: a randomized placebo‐controlled clinical trial. Medical Principles and Practice 2011; 20: 433–7. [DOI] [PubMed] [Google Scholar]
- 99. Asadi HK, Nikooseresht M, Noori L, Behnoud F. The effect of administration of ketamine and paracetamol versus paracetamol singly on postoperative pain, nausea and vomiting after pediatric adenotonsillectomy. Anesthesiology and Pain Medicine 2016; 6: e31210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Javid MJ, Hajijafari M, Hajipour A, Makarem J, Khazaeipour Z. Evaluation of a low dose ketamine in post tonsillectomy pain relief: a randomized trial comparing intravenous and subcutaneous ketamine in pediatrics. Anesthesiology and Pain Medicine 2012; 2: 85–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Honarmand A, Safavi M, Kashefi P, Hosseini B, Badiei S. Comparison of effect of intravenous ketamine, peritonsillar infiltration of tramadol and their combination on pediatric posttonsillectomy pain: a double‐blinded randomized placebo‐controlled clinical trial. Research in Pharmaceutical Sciences 2013; 8: 177–83. [PMC free article] [PubMed] [Google Scholar]
- 102. Elshammaa N, Chidambaran V, Housny W, Thomas J, Zhang X, Michael R. Ketamine as an adjunct to fentanyl improves postoperative analgesia and hastens discharge in children following tonsillectomy ‐ a prospective, double‐blinded, randomized study. Paediatric Anaesthesia 2017; 21: 1009–14. [DOI] [PubMed] [Google Scholar]
- 103. Eghbal MH, Taregh S, Amin A, Sahmeddini MA. Ketamine improves postoperative pain and emergence agitation following adenotonsillectomy in children. a randomized clinical trial. Middle East Journal of Anesthesiology 2013; 22: 155–60. [PubMed] [Google Scholar]
- 104. Hasnain F, Janbaz KH, Qureshi MA. Analgesic effect of ketamine and morphine after tonsillectomy in children. Pakistan Journal of Pharmaceutical Sciences 2012; 25: 599–606. [PubMed] [Google Scholar]
- 105. Norouzi A, Jafari A, Vishteh HRK, Fateh S. Comparison of the effects of oral vs. peritonsillar infiltration of ketamine in pain reduction after tonsillectomy: a randomized clinical trial. Middle East Journal of Anaesthesiology 2015; 23: 29–34. [PubMed] [Google Scholar]
- 106. Yenigun A, Et T, Aytac S, Olcay B. Comparison of different administration of ketamine and intravenous tramadol hydrochloride for postoperative pain relief and sedation after pediatric tonsillectomy. Journal of Craniofacial Surgery 2015; 26: E21–E24. [DOI] [PubMed] [Google Scholar]
- 107. Heidari SM, Mirlohi SZ, Hashemi SJ. Comparison of the preventive analgesic effect of rectal ketamine and rectal acetaminophen after pediatric tonsillectomy. International Journal of Preventive Medicine 2012; 3: S150–S155. [PMC free article] [PubMed] [Google Scholar]
- 108. El SMI, El DHA, Mostafa A, Shanab OA. Preemptive peritonsillar ketamine infiltration: postoperative analgesic efficacy versus meperidine. Middle East Journal of Anesthesiology 2011; 21: 43–51. [PubMed] [Google Scholar]
- 109. El Bahnasawy N, Abu‐Samra M. The analgesic efficacy of preincisional peritonsillar versus intravenous ketamine with bupivacaine infiltration for tonsillectomy in children: a randomized double‐blind controlled study. Ain‐Shams Journal of Anaesthesiology 2014; 7: 514. [Google Scholar]
- 110. Erhan OL, Goeksu H, Alpay C, Bestas A. Ketamine in post‐tonsillectomy pain. International Journal of Pediatric Otorhinolaryngology 2007; 71: 735–9. [DOI] [PubMed] [Google Scholar]
- 111. Farmawy MS, Rashad MM. Preemptive analgesia by peritonsillar ketamine versus ropivacaine for post‐tonsillectomy pain in children. Egyptian Journal of Anaesthesia 2014; 30: 1–5. [Google Scholar]
- 112. Honarmand A, Safavi MR, Jamshidi M. The preventative analgesic effect of preincisional peritonsillar infiltration of two low doses of ketamine for postoperative pain relief in children following adenotonsillectomy. A randomized, double‐blind, placebo‐controlled study. Paediatric Anaesthesia 2008; 18: 508–14. [DOI] [PubMed] [Google Scholar]
- 113. Pirzadeh A, Mohammadi M‐A, Allaf‐Akbari S, Entezariasl M. The effect of ketamine on posttonsillectomy pain in children: a clinical trial. Iranian Journal of Otorhinolaryngology 2012; 24: 23–8. [PMC free article] [PubMed] [Google Scholar]
- 114. Siddiqui AS, Raees US, Siddiqui SZ, Raza SA. Efficacy of pre‐incisional peritonsillar infiltration of ketamine for post‐tonsillectomy analgesia in children. Journal of the College of Physicians and Surgeons Pakistan 2013; 23: 533–7. [PubMed] [Google Scholar]
- 115. Ayatollahi V, Behdad S, Hatami M, Moshtaghiun H, Baghianimoghadam B. Comparison of peritonsillar infiltration effects of ketamine and tramadol on post tonsillectomy pain: a double‐blinded randomized placebo‐controlled clinical trial. Croatian Medical Journal 2012; 53: 155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Zokaei A, Ahmadi SJ. The comparative study of adding ketamin to pre‐incional bupivacaine infiltration on pain relief post tonsillectomy. Research Journal of Medical Sciences 2016; 10: 135–8. [Google Scholar]
- 117. Tekelioglu UY, Apuhan T, Akkaya A, et al. Comparison of topical tramadol and ketamine in pain treatment after tonsillectomy. Pediatric Anesthesia 2013; 23: 496–501. [DOI] [PubMed] [Google Scholar]
- 118. Canbay O, Celebi N, Uzun S, Sahin A, Celiker V, Aypar U. Topical ketamine and morphine for post‐tonsillectomy pain. European journal of anaesthesiology 2008; 25: 287–92. [DOI] [PubMed] [Google Scholar]
- 119. Vahabi S, Shoja T, Chaibakhsh S, Khak M, Saljoughi N. Effect of postoperative topical administration of magnesium sulfate on pain relief in paediatric adenotonsillectomy: a randomised controlled study. Hong Kong Journal of Paediatrics 2012; 17: 109–14. [Google Scholar]
- 120. Benzon HA, Shah RD, Hansen J, et al. The effect of systemic magnesium on postsurgical pain in children undergoing tonsillectomies: a double‐blinded, randomized, placebo‐controlled trial. Anesthesia and Analgesia 2015; 121: 1627–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Abdulatif M, Ahmed A, Mukhtar A, Badawy S. The effect of magnesium sulphate infusion on the incidence and severity of emergence agitation in children undergoing adenotonsillectomy using sevoflurane anaesthesia. Anaesthesia 2013; 68: 1045–52. [DOI] [PubMed] [Google Scholar]
- 122. Tugrul S, Degirmenci N, Eren SB, Dogan R, Veyseller B, Ozturan O. Analgesic effect of magnesium in post‐tonsillectomy patients: a prospective randomised clinical trial. European Archives of Oto‐Rhino‐Laryngology 2015; 272: 2483–7. [DOI] [PubMed] [Google Scholar]
- 123. Cho HK, Park IJ, Yoon HY, Hwang SH. Efficacy of adjuvant magnesium for posttonsillectomy morbidity in children: a meta‐analysis. Otolaryngology‐Head and Neck Surgery 2018; 158: 27–35. [DOI] [PubMed] [Google Scholar]
- 124. Vlok R, Melhuish TM, Chong C, Ryan T, White LD. Adjuncts to local anaesthetics in tonsillectomy: a systematic review and meta‐analysis. Journal of Anesthesia 2017; 31: 608–16. [DOI] [PubMed] [Google Scholar]
- 125. Xie M, Li X, Peng Y. Magnesium sulfate for postoperative complications in children undergoing tonsillectomies: a systematic review and meta‐analysis. Journal of Evidence‐Based Medicine 2017; 10: 16–25. [DOI] [PubMed] [Google Scholar]
- 126. Ayala M, Bruggers DG, Yarbrough JT, Scheurer MM, Hunsaker DH. The postoperative use of amoxicillin in adult tonsillectomy patients. Laryngoscope 2009; 119: S215. [Google Scholar]
- 127. Baradaranfar MH, Zand V, Dadgarnia MH, Atighechi S. Efficacy of clindamycin in reducing pain following tonsillectomy in adults: a double‐blind, randomised trial. Journal of Laryngology and Otology 2013; 127: 1106–10. [DOI] [PubMed] [Google Scholar]
- 128. Zagolski O, Kulisiewicz J. Perioperative antibiotic in adenoidectomy with partial tonsillectomy: a randomized trial. Orl‐Journal for Oto‐Rhino‐Laryngology Head and Neck Surgery 2012; 74: 86–92. [DOI] [PubMed] [Google Scholar]
- 129. Mutiso MD, Macharia IM. Single intraoperative intravenous co‐amoxiclav versus postoperative full oral course in prevention of postadenotonsillectomy morbidity: a randomised clinical trial. BMC Ear, Nose, and Throat Disorders 2011; 11: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Miura MS, Saleh C, de Andrade M, Assmann M, Hernandes LL, Neto JFL. Topical clindamycin in post‐adenotonsillectomy analgesia in children: A double‐blind, randomized clinical trial. Otolaryngology‐Head and Neck Surgery 2009; 141: 509–15. [DOI] [PubMed] [Google Scholar]
- 131. Jahanshahi J, Pazira S, Farahani F, et al. Effect of topical sucralfate vs clindamycin on posttonsillectomy pain in children aged 6 to 12 years a triple‐blind randomized clinical trial. Journal of the American Medical Association Otolaryngology‐Head and Neck Surgery 2014; 140: 698–703. [DOI] [PubMed] [Google Scholar]
- 132. Gil‐Ascencio M, Castillo‐Gómez CJ, Palacios‐Saucedo GC, Valle‐de la O A. Antibiotic prophylaxis in tonsillectomy and its relationship with postoperative morbidity. Acta Otorrinolaringológica Española 2013; 64: 273–8. [DOI] [PubMed] [Google Scholar]
- 133. Aljfout Q, Alississ A, Rashdan H, Maita A, Saraireh M. Antibiotics for post‐tonsillectomy morbidity: comparative analysis of a single institutional experience. Journal of Clinical Medicine Research 2016; 8: 385–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Miura MS, Saleh C, de Andrade M, Assmann M, Ayres M, Neto JFL. Topical sucralfate in post‐adenotonsillectomy analgesia in children: a double‐blind randomized clinical trial. Otolaryngology‐Head and Neck Surgery 2009; 141: 322–8. [DOI] [PubMed] [Google Scholar]
- 135. Sampaio ALL, Pinheiro TG, Furtado PL, Araujo MFS, Olivieira CACP. Evaluation of early postoperative morbidity in pediatric tonsillectomy with the use of sucralfate. International Journal of Pediatric Otorhinolaryngology 2007; 71: 645–51. [DOI] [PubMed] [Google Scholar]
- 136. Siupsinskiene N, Zekonien≐ J, Padervinskis E, Zekonis G, Vaitkus S. Efficacy of sucralfate for the treatment of post‐tonsillectomy symptoms. European Archives of Oto‐Rhino‐Laryngology 2015; 272: 271–8. [DOI] [PubMed] [Google Scholar]
- 137. Almasi S, Khalili A, Dehghan M, Abadi FJN, Mohammadi NA, Cheraghi F. The effect of telephone follow‐up after ambulatory surgery on pain management for children at home by parents. International Journal of Medical Research and Health Sciences 2016; 5: 263–7. [Google Scholar]
- 138. Bailey L, Sun J, Courtney M, Murphy P. Improving postoperative tonsillectomy pain management in children ‐ a double blinded randomised control trial of a patient analgesia information sheet. International Journal of Pediatric Otorhinolaryngology 2015; 79: 732–9. [DOI] [PubMed] [Google Scholar]
- 139. Paquette J, Le MS, Fiola JL, Villeneuve E, Lapointe A, Bourgault P. A randomized clinical trial of a nurse telephone follow‐up on paediatric tonsillectomy pain management and complications. Journal of Advanced Nursing 2013; 69: 2054–65. [DOI] [PubMed] [Google Scholar]
- 140. Helgadottir HL, Wilson ME. A randomized controlled trial of the effectiveness of educating parents about distraction to decrease postoperative pain in children at home after tonsillectomy. Pain Management Nursing 2014; 15: 632–40. [DOI] [PubMed] [Google Scholar]
- 141. Martin S, Smith AB, Newcomb P, Miller J. Effects of therapeutic suggestion under anesthesia on outcomes in children post tonsillectomy. Journal of Perianesthesia Nursing 2014; 29: 94–106. [DOI] [PubMed] [Google Scholar]
- 142. Vallee E, Lafrenaye S, Tetrault J‐P, Mayer S, Dorion D. Pain management after tonsillectomy: morphine is not enough. Journal of Otolaryngology‐Head and Neck Surgery 2008; 37: 279–84. [PubMed] [Google Scholar]
- 143. van Vliet LM, Godfried MB, van Deelen GW, et al. Placebo effects of nurses’ communication alongside standard medical care on pain and other outcomes: a randomized controlled trial in clinical tonsillectomy care. Psychotherapy and Psychosomatics 2020; 89: 56–8. [DOI] [PubMed] [Google Scholar]
- 144. Sylvester DC, Rafferty A, Bew S, Knight LC. The use of ice‐lollies for pain relief post‐paediatric tonsillectomy. A single‐blinded, randomised, controlled trial. Clinical Otolaryngology 2011; 36: 566–70. [DOI] [PubMed] [Google Scholar]
- 145. Klemetti S, Kinnunen I, Suominen T, et al. The effect of preoperative fasting on postoperative pain, nausea and vomiting in pediatric ambulatory tonsillectomy. International Journal of Pediatric Otorhinolaryngology 2009; 73: 263–73. [DOI] [PubMed] [Google Scholar]
- 146. Moghaddam YJ, Seyedhejazi M, Naderpour M, Yaghooblua Y, Golzari SEJ. Is fasting duration important in post adenotonsillectomy feeding time? Anesthesiology and Pain Medicine 2014; 4: e10256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Faramarzi M, Safari S, Roosta S. Comparing cold/liquid diet vs regular diet on posttonsillectomy pain and bleeding. Otolaryngology‐Head and Neck Surgery 2018; 159: 755–60. [DOI] [PubMed] [Google Scholar]
- 148. Manica D, Sekine L, Abreu LS, et al. Influence of dietary and physical activity restriction on pediatric adenotonsillectomy postoperative care in Brazil: a randomized clinical trial. Brazilian Journal of Otorhinolaryngology 2018; 84: 191–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Meybodian M, Dadgarnia M, Baradaranfar M, et al. Effect of cold diet and diet at room temperature on post‐tonsillectomy pain in children. Iranian Journal of Otorhinolaryngology 2019; 31: 81–6. [PMC free article] [PubMed] [Google Scholar]
- 150. Koçak İ, Yücepur C, Gökler O. Is ginger effective in reducing post‐tonsillectomy morbidity? A prospective randomised clinical trial. Clinical and Experimental Otorhinolaryngology 2018; 11: 65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Wijakkanalan P, Saesaew P, Wongsawatdiwat M, Piromchai P. Whether post‐tonsillectomy medication should be liquid based or can be solid? A randomised, single‐blinded, controlled trial. Journal of the Medical Association of Thailand 2015; 98 (Suppl 7): S179–S184. [PubMed] [Google Scholar]
- 152. Arbin L, Enlund M, Knutsson J. Post‐tonsillectomy pain after using bipolar diathermy scissors or the harmonic scalpel: a randomised blinded study. European Archives of Oto‐Rhino‐Laryngology 2017; 274: 2281–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Cetiner H, Cavusoglu I, Duzer S, Sakallioglu O, Susaman N, Yildirim YSS. Effect of suturation plus surgicel application on post‐tonsillectomy bleeding and pain. Journal of Craniofacial Surgery 2017; 28: e672–e675. [DOI] [PubMed] [Google Scholar]
- 154. Sanlı A, Yildiz G, Erdogan BA, Paksoy M, Altin G, Ozcelik MA. Comparison of cold technique tonsillectomy and thermal welding tonsillectomy at different age groups. Prague Medical Report 2017; 118: 26–36. [DOI] [PubMed] [Google Scholar]
- 155. Wiltshire D, Cronin M, Lintern N, et al. The debate continues: a prospective, randomised, single‐blind study comparing Coblation and bipolar tonsillectomy techniques. Journal of Laryngology and Otology 2018; 132: 240–5. [DOI] [PubMed] [Google Scholar]
- 156. Yilmazer R, Yazici ZM, Balta M, Erdim I, Erdur O, Kayhan FT. Plasma blade vs. cold dissection tonsillectomy: a prospective, randomized, double‐blind, controlled study in adults. Ear, Nose and Throat Journal 2017; 96: 250–6. [DOI] [PubMed] [Google Scholar]
- 157. Alexiou VG, Salazar‐Salvia M, Jervis PN, Falagas ME. Modern technology‐assisted vs conventional tonsillectomy a meta‐analysis of randomized controlled trials. Archives of Otolaryngology‐Head and Neck Surgery 2011; 137: 558–70. [DOI] [PubMed] [Google Scholar]
- 158. Pynnonen M, Brinkmeier JV, Thorne MC, Chong LY, Burton MJ. Coblation versus other surgical techniques for tonsillectomy. Cochrane Database of Systematic Reviews 2017; 8: CD004619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Francis DO, Fonnesbeck C, Sathe N, McPheeters M, Krishnaswami S, Chinnadurai S. Postoperative bleeding and associated utilization following tonsillectomy in children: a systematic review and meta‐analysis. Otolaryngology‐Head and Neck Surgery 2017; 156: 442–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Metcalfe C, Muzaffar J, Daultrey C, Coulson C. Coblation tonsillectomy: a systematic review and descriptive analysis. European Archives of Oto‐Rhino‐Laryngology 2017; 274: 2637–47. [DOI] [PubMed] [Google Scholar]
- 161. Tolska HK, Hamunen K, Takala A, Kontinen VK. Systematic review of analgesics and dexamethasone for post‐tonsillectomy pain in adults. British Journal of Anaesthesia 2019; 123: e397–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Czarnetzki C, Elia N, Lysakowski C, et al. Dexamethasone and risk of nausea and vomiting and postoperative bleeding after tonsillectomy in children a randomized trial. Journal of the American Medical Association 2008; 300: 2621–30. [DOI] [PubMed] [Google Scholar]
- 163. Yenigun A, Yilmaz S, Dogan R, Goktas SS, Calim M, Ozturan O. Demonstration of analgesic effect of intranasal ketamine and intranasal fentanyl for postoperative pain after pediatric tonsillectomy. International Journal of Pediatric Otorhinolaryngology 2018; 104: 182–5. [DOI] [PubMed] [Google Scholar]
- 164. Myhre M, Diep LM, Stubhaug A. Pregabalin has analgesic, ventilatory, and cognitive effects in combination with remifentanil. Anesthesiology 2016; 124: 141–9. [DOI] [PubMed] [Google Scholar]
- 165. Kehlet H, Joshi GP. Systematic Reviews and meta‐analyses of randomized controlled trials on perioperative outcomes: an urgent need for critical reappraisal. Anesthesia and Analgesia 2015; 121: 1104–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Search strategy used for this review.
Table S1. Quality assessment and level of evidence assigned to the randomised trials included in this review.
Table S2. Summary of key results from studies evaluating systemic analgesics, systemic analgesic adjuncts, regional analgesia and surgical procedures used to support the recommended interventions in patients after tonsillectomy.
Table S3. Summary of key results from studies evaluating systemic analgesics, regional analgesia, perineural analgesic adjuncts and surgical procedures used to support interventions that are not recommended for analgesic benefit in patients having tonsillectomy.


