ABSTRACT
A previous randomized controlled trial has suggested the effectiveness of a Dutch postdischarge responsive parenting program for very preterm (VPT) infants, indicating that nationwide implementation was justified. This paper describes the development and nationwide implementation of the intervention, known as the TOP program, which consisted of three phases. In the preparation phase (2006–2010), a theory of change and the structure of the TOP program were developed, and funding for phase two, based on a positive Business Case, was obtained. In the pilot implementation phase (2010–2014), intervention strategies were developed for a real‐world setting, capacity and adoption were increased, systematic evaluations were incorporated, and sustained funding was obtained. In the full‐implementation phase (2014–2019), all Dutch Healthcare Insurers reimbursed the TOP program, enabling VPT infants to participate in the program without charge. By 2018, the number of interventionists that provided the TOP program had increased from 37 to 91, and all level III hospitals and 65% of regional hospitals in the Netherlands referred VPT infants. Currently, the program reaches 70% of the Dutch target population and parental satisfaction with the TOP program is high. After a 12‐year implementation period, the TOP program forms part of routine care in the Netherlands.
Keywords: implementation, intervention reach, parental satisfaction, responsive parenting intervention, very preterm infants, infantes muy prematuros, intervención de crianza sensible, implementación, alcance de la intervención, satisfacción de los padres, nourrissons grands prématurés, intervention de sensibilité de parentage, mise en œuvre, portée de l'intervention, satisfaction parentale, Frühgeborene, responsive Elternintervention, Umsetzung, Interventionsreichweite, Elternzufriedenheit, 在胎32週未満の早産児, 応答的育児介入, 実施, 介入の普及, 親の満足度, 极早产婴儿, 响应式育儿干预, 实施, 干预范围, 父母满意度, الرضع الخدج جدا، التدخل الوالدي المستجيب، التطبيق، مدى وصول التدخل، رضا الوالدين
RESUMEN
Un previo ensayo controlado al azar ha sugerido la eficacia de un programa holandés sobre la crianza sensible para infantes muy prematuros (VPT) posterior al momento en que se les dio de alta, indicando que la implementación a lo largo de toda la nación era justificada. Este artículo describe el desarrollo y la implementación a nivel de toda la nación de la intervención, conocida como el programa ToP, el cual consistía de tres fases. En la fase de preparación (2006‐2010), se desarrollaron una teoría de cambio y la estructura del programa ToP, y se obtuvieron los fondos para la fase dos, con base en un Caso de Negocios (BC) positivo. En la fase piloto de implementación (2010‐2014), se desarrollaron estrategias de intervención para un escenario del mundo real, se aumentaron la capacidad y la adopción, se incorporaron evaluaciones sistemáticas y se obtuvieron fondos para mantener el programa. En la fase de implementación completa (2014‐2019), todas las Aseguradoras Holandesas del Sector Salud reembolsaron el costo del programa ToP, permitiéndoles a los infantes VPT participar en el programa sin costo alguno. Para 2018, el número de practicantes de la intervención que prestaban el servicio del programa ToP había aumentado de 37 a 91, y todos los hospitales del nivel III y 65% de los hospitales regionales en Holanda refirieron los infantes VPT al programa. Actualmente, el programa llega a 70% de la población holandesa para la cual está destinado y la satisfacción de los padres con el programa ToP es alta. Después de un período de implementación de 12 años, el programa ToP forma parte del cuidado de salud rutinario en Holanda.
RÉSUMÉ
Un essai contrôlé randomisé précédent a suggéré l'efficacité d'un programme hollandais de sensibilité de parentage après la sortie de l'hôpital pour les nourrissons grands prématurés (GP ici en français), indiquant qu'une mise en œuvre au niveau national était justifiée. Cet article décrit le développement et la mise en œuvre au niveau national de l'intervention, connue en tant que ToP program, qui a consisté en trois phases. Dans la phase de préparation (2006‐2010), une théorie du changement et la structure du programme ToP a été développée, et le financement pour la phase deux, basée sur une Etude de Cas positive, a été sécurisé. Dans la phase pilote d'implémentation (2010‐2014) des stratégies d'intervention ont été développées pour un contexte réel, la capacité et l'adoption ont été augmentées, les évaluations systématiques ont été incorporées, et un financement durable a été sécurisé. Dans la pleine phase de mise en œuvre (2014‐1029), tous les Assurances Santé Hollandaises ont remboursé le programme ToP, permettant aux nourrissons GP de participer au programme sans coût. En 2018 le nombre de prestataires qui offraient le programme ToP a augmenté de 37 à 91, et tous les hôpitaux de niveau III ainsi que 65% des hôpitaux régionaux aux Pays Bas ont envoyé les nourrissons GP au programme. En ce moment le programme atteint 70% de la population cible hollandaise et la satisfaction parentale avec le programme ToP est élevée. Après une période de mise en œuvre de 12 ans le programme ToP fait partie des soins de routine aux Pays Bas.
ZUSAMMENFASSUNG
Entwicklung und landesweite Umsetzung eines Interventionsprogramms für Eltern von sehr frühgeborenen Kindern nach der Entlassung: das ToP‐Programm
Eine frühere randomisierte kontrollierte Studie hat die Wirksamkeit eines niederländischen Interventionsprogramms für Eltern von sehr frühgeborenen (very preterm; VPT) Kindern nach der Entlassung nahegelegt. Dies wies darauf hin, dass eine landesweite Umsetzung gerechtfertigt wäre. Die vorliegende Studie beschreibt die aus drei Phasen bestehende Entwicklung und landesweite Umsetzung dieser, ToP‐Programm bekannten, Intervention. In der Vorbereitungsphase (2006–2010) wurden eine Veränderungstheorie und die Struktur des ToP‐Programms entwickelt und eine Finanzierung der zweiten Phase auf der Grundlage eines positiven Geschäftsszenarios (Business Case; BC) ermöglicht. In der Pilotimplementierungsphase (2010‐2014) wurden Interventionsstrategien für ein reales Umfeld entwickelt, Kapazität und Akzeptanz erhöht, systematische Evaluationen vorgenommen und eine nachhaltige Finanzierung realisiert. In der vollständigen Umsetzungsphase (2014‐2019) haben alle niederländischen Krankenversicherungen das ToP‐Programm erstattet, sodass VPT‐Säuglinge kostenlos am Programm teilnehmen konnten. Bis 2018 ist die Zahl der Anbietenden des ToP‐Programms von 37 auf 91 gestiegen und alle Krankenhäuser der Stufe III und 65% der regionalen Krankenhäuser in den Niederlanden überwiesen VPT‐Säuglinge. Derzeit erreicht das Programm 70% der niederländischen Zielgruppe und die Zufriedenheit der Eltern mit dem ToP‐Programm ist hoch. Nach einer 12‐jährigen Umsetzungsphase ist das ToP‐Programm Teil der Routineversorgung in den Niederlanden.
抄録
在胎32週未満の早産児向け退院後応答的育児介入プログラム“ToPプログラム”の沿革と全国的な実施
先行無作為化比較研究は、オランダの在胎32週未満の早産(VPT)乳児のための退院後応答的育児プログラムの有効性を示唆しており、全国的な実施の合理性が示された。本論文では、3つのフェーズからなるToPプログラムと呼ばれる介入の開発と全国的な実施について述べる。準備フェーズ(2006–2010)では、変化の理論とToPプログラムの構造が開発され、正のビジネスケース(BC)に基づいてフェーズ2の資金が調達された。パイロット導入フェーズ(2010–2014)では、実際の環境に適した介入戦略が策定され、機能と採用件数が増加し、体系的な評価が組み込まれ、持続的な資金源が得られた。完全実施フェーズ(2014–2019)では、オランダの全ての医療保険会社がToPプログラムに払い戻しを行い、VPTの乳児が無償でプログラムに参加できるようなった。2018年までに、ToPプログラムを提供する介入者の数は37人から91人に増加し、オランダの全てのレベルIIIの病院と地域病院の65%がVPT乳児を紹介した。現在、プログラムはオランダの対象人口の70%に普及し、ToPプログラムに対する親の満足度は高い。実施開始後12年が経過し、ToPプログラムはオランダでは日常的なケアの一部となっている。
摘要
此前的一项随机对照试验表明, 荷兰对极早产 (VPT) 婴儿的院后响应式育儿计划是有效的, 这表明在全国范围内实施是合理的。本文描述了干预措施的发展和在全国范围内的实施情况, 称为ToP计划, 分为三个阶段。在准备阶段 (2006–2010年) , 开发了变革理论和ToP计划的结构, 并基于积极的商业案例 (BC) 获得了第二阶段的资金支持。在试点实施阶段 (2010–2014年) , 针对现实环境制定了干预战略, 提高了业务能力和采用率, 纳入了系统评价, 并获得了持续的资金支持。在全面实施阶段 (2014–2019年) , 所有荷兰医疗保险公司都对ToP计划进行报销, 从而使VPT婴儿能够免费参与该计划。到2018年, 提供ToP计划的干预机构从37家增加到91家, 荷兰所有三级医院和65%的地区医院都将VPT婴儿纳入治疗范围。目前, 该计划覆盖了荷兰70%的目标人群, 并且父母对ToP项目的满意度很高。经过12年的实施期后, ToP计划已经成为荷兰常规护理的一部分。
ملخص
تطوير وتنفيذ برنامج رعاية والدية ا لمرحلة ما بعد خروج الأطفال المبتسرين من المستشفى: برنامج ToP
أشارت دراسة سابقة إلى فاعلية برنامج هولندي للرعاية الوالدية المستجيبة بعد خروج الرضع المبتسرين جداً (VPT) من المستشفى وأكدت على إمكانية تطبيقه على مستوى الدولة بشكل ناجح. تصف هذه الورقة تطوير وتنفيذ التدخل على مستوى الدولة، والمعروف باسم برنامج الـToP ، الذي يتكون من ثلاث مراحل. في مرحلة الإعداد (2006‐2010)، تم تطوير نظرية التغيير وهيكل برنامج الـToP ، وتم الحصول على تمويل للمرحلة الثانية، بناء على وضعه التجاري الإيجابي (BC) وفي مرحلة التنفيذ التجريبي (2010‐2014)، وضعت استراتيجيات للتدخل على أساس واقعي، وتم زيادة القدرات الاستيعابية والتبني ، واستخدام تقييمات منهجية، وبعد ذلك تم الحصول على تمويل مستدام. في مرحلة التنفيذ الكامل (2014‐2019)، قامت جميع شركات التأمين الصحي الهولندية بسداد تكاليف برنامجToP ، مما مكن الرضع من المشاركة في البرنامج دون مقابل. وبحلول عام 2018، ارتفع عدد المتدخلين الذين قدموا برنامج الـToP من 37 إلى 91، كما أن جميع مستشفيات المستوى الثالث و65% من المستشفيات الإقليمية في هولندا أصبحت تقوم بتحويل الرضع من برنامج ToP ، وفي الوقت الجالي يصل البرنامج إلى 70٪ من السكان المستهدفين الهولنديين ورضا الوالدين عن برنامجToP مرتفع. بعد فترة تنفيذ مدتها 12 عاماً، يشكل برنامج الـToP جزءاً من الرعاية الروتينية في هولندا.
1. INTRODUCTION
Preventive support for all very preterm (VPT) infants and their families after discharge home is recommended because it improves outcomes for both infants and their parents (EFCNI et al, 2018). A responsive environment, with fluent parent–infant interactions, supports infants’ resilience and healthy development (Britto, Singh, Dua, Kaur, & Yousafzai, 2018). The fact that VPT infants may profit even more than term infants from these responsive interactions (Erickson et al., 2013; Guralnick, 2012; Landry, Smith, & Swank, 2006; Milgrom et al., 2010) provides an opportunity for intervention. This is an important opportunity because VPT birth is associated with poorer developmental trajectories (Aarnoudse‐Moens, Weisglas‐Kuperus, van Goudoever, & Oosterlaan, 2009; de Kieviet, Piek, Aarnoudse‐Moens, & Oosterlaan, 2009; Twilhaar, de Kieviet, Aarnoudse‐Moens, van Elburg, & Oosterlaan, 2018). Neonatal morbidities such as bronchopulmonary dysplasia, sepsis, intraventricular hemorrhage, and necrotizing enterocolitis are known risk factors for adverse outcomes. Even without these morbidities, more than half of VPT infants have mild brain abnormalities that are related to regulatory problems in early childhood (Clark, Woodward, Horwood, & Moor, 2008; Murray et al., 2016; Spittle et al., 2011). VPT infants are less responsive and explorative, have more feeding and sleeping difficulties (Schmid, Schreier, Meyer, & Wolke, 2011), and experience more stress and behavioral disorganization. Therefore, parents of VPT infants need to be more sensitive and responsive even though they are often under psychological stress, as dealing with a VPT birth and a long hospital stay is challenging (Bilgin & Wolke, 2016). Consequently, these families are at high risk for difficulties in parent–child interactions, resulting in an additional risk factor for poorer child outcomes. This highlights the need for early preventive intervention at the stage when an infant's brain is developing faster than at any other stage in life (http://www.1001criticaldays.co.uk/).
Despite widespread agreement on the need for postdischarge support for VPT infants and their families, such support is seldom available in routine care. Organizing such an innovative healthcare service for all VPT infants and their parents is a long and complex process. The key prerequisite for implementation of an intervention is that it is effective (Milat, King, Bauman, & Redman, 2013). When this prerequisite is fulfilled, an evidence‐based intervention usually requires adaptation to allow for implementation in a real‐world setting (Wiltsey Stirman, Baumann, & Miller, 2019). Furthermore, different implementation components are required in different phases to actively implement interventions in routine care (Fixsen, Blase, Naoom, & Wallace, 2009).
In the Netherlands, research was conducted to study the feasibility and effectiveness of the Infant Behavioral Assessment and Intervention Program (IBAIP©) that aimed to support VPT infants and their parents after discharge (Hedlund, 1998). The positive outcomes of the hospital‐based neurobehavioral intervention program known as the Newborn Individualized Development Care and Assessment Program (Als et al., 1986; Als et al., 1994) and the Mother–Infant Transaction Program (Achenbach, Howell, Aoki, & Rauh, 1993) motivated the evaluation of an intervention program that could ensure the continuity and uniformity of care after discharge. The IBAIP is a preventive neurobehavioral intervention program that is primarily based on the Synactive Theory of Infant Development (Als et al., 1986), targeting infants until the corrected age (CA) of 6–8 months.
Key Findings
Responsive parenting support for very preterm (VPT) infants and their parents after discharge is now part of routine care in the Netherlands and is known as the TOP program. The cost of the program is included in basic healthcare insurance, which makes it available to the total Dutch target population at no charge.
A series of steps are required to build a solid foundation for an innovative health care service. After two pilot studies and a randomized controlled trial, the implementation of the TOP program took 12 years and consisted of three implementation phases: a preparation phase, a pilot implementation phase, and a full‐implementation phase, each consisting of different aims and components.
Pivotal to the sustainability and flexibility that is required to improve the TOP program over time is the utilization of bundled payments. These payments include the cost of interventions and overhead per infant for the management of the organization, consisting of financial management, systematic monitoring and evaluation, quality assurance, and information provision.
Statement of relevance
To impact the development of very preterm infants, effective intervention needs to be scaled up and included in routine care. In this manuscript, we describe the steps taken for nationwide implementation of an evidence‐based intervention in the Netherlands.
After two promising pilot studies (Koldewijn et al., 2005; Wolf et al., 2002), a multicenter randomized controlled trial (RCT) that evaluated the effect of the IBAIP on motor, cognitive, and neurobehavioral outcomes was performed. Better cognitive, motor, and behavioral outcomes were found at 6 months CA (for prematurity) (Koldewijn et al., 2009), and it was found that mothers were more sensitive and less intrusive toward their children (Meijssen et al., 2010). At 24 months CA, motor outcomes were improved, but cognitive and behavioral outcomes were not (Koldewijn et al., 2010). Positive developmental effects were sustained for motor development and Performance IQ, 5 years after conclusion of the intervention, especially for infants with bronchopulmonary dysplasia (Van Hus et al., 2013).
These positive effects justified integration into routine postdischarge clinical practice in order to impact VPT infants and their families. This article describes the process of development and implementation of a preventive responsive parenting program after discharge for VPT infants and their parents in the Netherlands, resulting in the TOP program (Transmural developmental support for VPT infants and their parents). Transmural care is the interface between hospital and primary care. For the integration into routine care, our aim was to enable VPT infants born in the Netherlands, and their parents, to participate in the TOP program without charge.
2. METHODS AND RESULTS
Implementing an evidence‐based intervention implies obtaining both policy and financial support and tailoring the intervention to a real‐world setting. In order to fulfil these basic conditions, the implementation of the TOP program followed the principles and strategies described by Grol and colleagues (Grol, Wensing, & Eccles, 2005; Grol, Wensing, Eccles, & Davis, 2013). The implementation process consisted of three consecutive phases: (I) a preparation phase; (II) a pilot implementation phase; and (III) a full‐implementation phase.
2.1. Phase I: Preparation phase (2006–2010)
Before implementation of the postdischarge intervention could start, an extensive preparation phase was necessary in which different components were employed: (1) designing a theory of change (TOC) and intervention protocol that matched the needs of the target group and the experiences of the professionals; (2) mobilizing financial resources to fund the pilot implementation of the intervention; (3) establishing a center of expertise for VPT infants; and (4) informing and mobilizing stakeholders to involve them as participants in the implementation of the intervention program (Table 1). The first aspects of this phase started shortly after the positive results of the RCT at 6 months. The plan was carried out parallel to the earlier described follow‐up studies of the RCT and was reinforced by positive outcomes at 24 months, 3.5 years, and 5.5 years.
TABLE 1.
Implementation components per phase
| Aim | Implementation component |
|---|---|
| Preparation phase | |
| Preparing the intervention for scaling up | ‐ Developing the structure of the intervention protocol |
| Mobilizing financial resources |
‐ Writing a Business Case comparing costs and savings of the preventive intervention, in relation to positive health care outcomes ‐ Grant application to fund pilot phase |
| Informing and mobilizing participants and stakeholders |
‐ Convince stakeholders of the need to scale up the intervention ‐ Gain the support of decision makers who can provide resources to continue funding |
| Pilot implementation phase | |
| Preparing the intervention for scaling up | ‐ Developing a Theory of Change and an intervention protocol, tailored to the context and the experiences and preferences of families and professionals |
| Increase the capacity |
‐ Developing a training protocol ‐ Developing a training manual ‐ Yearly training of therapists ‐ Selecting therapists for training for regions with low capacity |
| Increase the adoption |
‐ Developing and distributing brochures ‐ Developing a logo for the TOP program ‐ Developing a website (www.top‐eop.nl) ‐ Writing articles for scientific and non‐scientific journals ‐ Giving presentations at conferences ‐ Giving presentations for departments of Neonatology, in regions where therapists were recently trained |
| Systematic evaluation and monitoring |
‐ Developing a database for registration of all infants and their home visits ‐ Applying a web‐based application for parental questionnaires ‐ Developing a questionnaire to evaluate the experiences of the parents regarding the TOP program ‐ Generating quarterly reports of data and using this information for improvements |
| Mobilize financial resources |
‐ Writing a second Business Case comparing costs and savings of the preventive intervention, in relation to positive health care outcomes ‐ Applying for reimbursement of the TOP program by all Dutch Health Care Insurers |
| Prepare the intervention for further scaling up | ‐ Adapt the intervention protocol to increase feasibility |
| Full implementation phase | |
| Increase the capacity | ‐ Yearly training of therapists |
| Increase the adoption |
‐ Updating and distributing brochures ‐ Developing a new website (www.top‐eop.nl) ‐ Writing articles for scientific and non‐scientific journals ‐ Giving presentations at conferences ‐ Giving presentations for departments of Neonatology, in regions where therapists were recently trained ‐ Participating in the European Standards of Care for Newborn Health: postdischarge responsive parenting programs |
| Systematic evaluation and monitoring |
‐ Continue data collection ‐ Generating quarterly reports of data and using this information for improvements |
| Maintain the quality of the intervention |
‐ Developing and organizing biannual training days ‐ Setting‐up regional collective peer learning groups ‐ Training moderators of collective peer learning groups |
2.1.1. Designing a TOC and structure for the TOP program protocol
The theoretical framework for the TOP program was based on outcomes and insights obtained in the RCT and relevant scientific evidence. A TOC is a framework that links intervention strategies, via targets, to the outcomes. It is a dynamic model that can be refined over time. The TOP program is a process‐oriented intervention consisting of seven intervention strategies (Figure 1). As in the RCT, intervention strategies were chosen to target parental responsiveness, thereby establishing a developmental environment for preterm infants that was as optimal as possible (Koldewijn et al., 2009). A strength‐based approach is seen as fundamental for the delivery of the TOP program because it supports the relationship between the interventionist and the parent, whereby the interventionist always uses the child's behavior as a point of reference. This nonjudgmental approach requires a special attitude on the part of the interventionist. It is necessary to believe in the parent's and infant's potential strengths and to actually enter into a relationship with the parent based on optimism, respect, and equality. Parents are regarded as experts and their information, requests for help, and choices form the basis of the guidance. In the TOC of the TOP program, intervention strategies were added to meet increasing scientific insights that recommended a “two‐generation approach.” The aim of this approach is to bring about changes in the parent, the parent–infant dyad, and the infant, with the ultimate goal of increasing infant developmental outcomes. Such an approach combines parent and infant support to strengthen a positive interaction cycle (Shonkoff & Fisher, 2013). The targets of the TOC also include parental understanding of the infant's behavior and parental well‐being as they buffer parental responsiveness. Sensitive and responsive parents provide an environment rich in “serve and return interactions”: the infant “serves” when initiating interaction (e.g., through gaze or vocalization) and the adult “returns” the serve when responding in a developmentally supportive way (National Scientific Council on the Developing Child, 2004). These attuned interactions support the infant's self‐regulation and development, preventing stressful situations for the infant. In turn, the infant's increasingly positive behavior enhances parental feelings of confidence and joy in the interaction and, consequently, ensures more consistent responsiveness from the parent.
FIGURE 1.
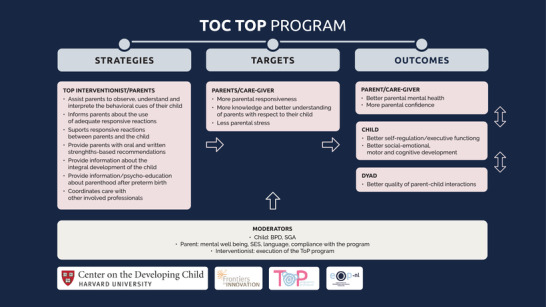
The Theory of Change (TOC) of the TOP program
Note. The last version of the dynamic TOC of the ToP program was developed in 2017, using the template of the Center of the Developing Child. The TOC is one of the three components of the IDEAS Impact Framework™ (https://developingchild.harvard.edu/innovation-application/innovation-approach/). The TOC has not undergone new adaptations since 2017
A protocol for the TOP program was developed, targeting the same infants as in the RCT: infants born <32 weeks gestational age (CA) and/or birth weight <1,500 g, and as in the RCT, to be carried out by pediatric physical therapists. In the Netherlands, pediatric physical therapists are trained to thoroughly observe infants’ sensory–motor behavior, have experience with intervention for babies and their families, are used to performing home visits, and are distributed across the country. After selection, they are trained in the holistic approach necessary to carry out the TOP program. The duration of the intervention program was extended from 6 to 12 months CA in response to feedback from the parents and interventionists, as well as the results of the RCT, which showed improved motor outcomes, but limited effects on cognitive and behavioral development. Neuroscience shows that complex functions such as executive functions and communication emerge at 6–7 months of age, and are best supported at that critical period of development (National Scientific Council on the Developing Child, 2007). Therefore, behavioral expressions were identified for infants aged 0–12 months, and intervention strategies were developed that were appropriate for that age. Consequently, the intervention protocol now included 12, instead of six to eight, 1‐hr home visits. In addition, 4 hr of designated care transfer or parental coaching were added to the protocol to support the parents and to facilitate access to additional services and intercollegiate consultations. Parents of preterm infants are at an increased risk of psychological or parenting stress. The RCT showed that even though maternal sensitivity was improved, no effects were found on maternal psychological well‐being (Meijssen, Wolf, Koldewijn, van Baar, & Kok, 2011). A comparable intervention program that included parental coaching did have positive outcomes on parental mental health (Landsem, Handegard, Tunby, Ulvund, & Ronning, 2014; Spittle et al., 2010). The TOP interventionist provides psychoeducation to parents, which involves providing information to parents to support them to understand and cope with common feelings and thoughts related to VPT birth, and to help them find supportive social resources in their environment or adequate professional support when necessary. In addition, an extra hour per home visit was included in the protocol to compose a personalized parental report with photos and text of positive interactions between parents and their infants, which was sent to the parents after each home visit. The purpose of the report is to assist parents in remembering and sharing information with family members or other care takers.
2.1.2. Mobilizing financial resources
To achieve the approval of the Dutch Health Authority (DHA) and to obtain financial support from the Dutch Healthcare Insurers for the pilot implementation, a better understanding of the costs, in relation to effects, was required. Therefore, an economic evaluation using healthcare outcome measures of infants who participated in the RCT was performed. In economic evaluations, both healthcare process measures and patient outcomes can be incorporated into cost‐effectiveness measures (Oostenbrink, Koopmanschap, & Rutten, 2002; Zorginstituut Nederland, 2016). In this implementation study, only the healthcare costs of the children were measured because the Dutch Healthcare Insurers were primarily aiming at a reduction in those costs. A comparison of data from the RCT, which included 90 infants in the intervention group and 85 infants in the control group, revealed savings due to fewer referrals at 1 year of age to paramedical professionals (10% in the intervention group vs. 22% in the control group), fewer hospital readmissions (29% vs. 40%), and fewer reports of child abuse during the first year of life (1.2% vs. 6.4%). The cost of healthcare provision was calculated in Euros. In a Business Case (BC), savings in healthcare provision were compared to the estimated costs of the TOP program. Subsequently, a grant application was prepared to cover the costs of the delivery and further development of the intervention as well as the overhead. The overall organizational management costs for each infant were calculated and included financial management systems, systematic evaluation and monitoring, quality assurance, and information provision. In the BC, the savings equaled the costs of the intervention, with better health outcomes for infants.
2.1.3. Establishing a center of expertise for VPT infants
In 2009, the Center of Expertise for Developmental Support for VPT infants (EOP‐nl) was set up and fell under the responsibility of the Amsterdam University Medical Center. The DHA required an organizational infrastructure that could continuously monitor and improve the quality of the program. Therefore, an integrated care management model was introduced (WHO, 2002). Integrated care includes a whole spectrum of care elements, such as prevention, timely signaling, referral, support, guidance, and treatment. The EOP‐nl develops and coordinates the implementation of the TOP program, provides education to healthcare professionals, guarantees quality control, and carries out evaluative research to improve the effectiveness of the TOP program. The EOP‐nl collaborates with healthcare professionals involved in caring for VPT infants and their parents and other stakeholders including Dutch Health Care Insurers.
2.1.4. Informing and mobilizing participants and stakeholders
An organizational implementation capacity assessment was conducted to share information about the intervention program and to ensure management readiness for change. University hospitals in Amsterdam and the referral hospitals in both Amsterdam and the North Holland province, involved in caring for VPT infants, were contacted. In addition, various other stakeholders were involved, such as the Dutch Parent Organization(VOC), Dutch Health Care Insurers, Dutch Pediatric Association, the Physical Therapy Organization, General Practitioners, Primary Health Care organizations, and the Dutch Health Care Authority. Partnerships were formalized through cooperation agreements between all stakeholders and the Center of Expertise for VPT infants.
2.2. Phase II: Pilot implementation of the TOP program (2010–2014)
After approval of the BC and the grant applications, the pilot implementation of the TOP program could commence. Phase II implementation components were to (1) develop intervention strategies for a real‐world practice setting; (2) increase the capacity of the intervention; (3) increase the adoption of the intervention; (4) incorporate systematic evaluations and monitoring of the implementation process of the intervention; and (5) obtain political support and mobilize financial resources for full implementation of the TOP program (Table 1).
2.2.1. Develop intervention strategies for a real‐world practice setting
The TOP program is a process‐oriented intervention. Together with the parents, the TOP interventionist identifies the topics for each home visit, which can be based on parental concerns, questions about the child's development, or day‐to‐day care giving, and can also be identified by the TOP interventionist based on their observation of the child's development or parent–child interaction. This means that during the home visits, the interventionist is flexible and adaptive and uses situations as they arise, providing a common reference point. Such a process‐oriented approach enables genuine customized care but is also complex and requires analytical and reflective competence and the necessary flexibility on the part of the interventionist. Therefore, conceptual models were developed for the TOP program to help interventionists interpret parent–infant interaction in a holistic way and choose the strategies that are most suitable for each infant and family, at a particular moment, in their situation. The key conceptual model that was developed to help interventionists stay aligned with the core principles of the TOP program is the TOP model of following and responding (Figure 2). The model distinguishes infant behavioral expressions from 0 to 12 months, indicating disbalance/stress, self‐regulatory behavior, or behavior that indicates approach and exploration, and the parental responses that match these behaviors. During joint observations in a play or caregiving situation, the TOP interventionist helps the parents to consciously monitor their infant's behavior, assisting them to give meaning to their infant's body language and to seek an appropriate response. The TOP interventionist confirms the infant's behavioral strengths and/or parents’ supportive strategies that work well in the interaction; and/or the interventionist gives strength‐based suggestions as to what parents could do to make improvements. The body language of the child also provides information about the infant's actual level of development and the small next steps in the different developmental domains, enhancing parents’ interest and realistic expectations. Using this model, the interventionist analyzes and guides the interactions from moment to moment so that the infant can participate without stress. In turn, the practical suggestions and positive results from their own responsive reactions allow parents to transfer this information to everyday interactions and increase their understanding of the needs of the child. By providing specific information and using the strength‐based approach, the interventionist aims to increase confidence and competence in the parenting role. Psychoeducation was provided to all parents and a monitoring system was set up to enable the TOP interventionists to screen for parental mental health problems and assist in finding timely support.
FIGURE 2.
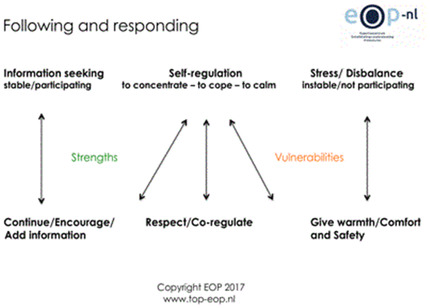
Following and responding model of the TOP program
Note. On top, the infants’ behaviors in the autonomic, motor, state, and attention/interaction system categorized to their meaning: information seeking, self‐regulation, and stress/disbalance. Below, the various parental supportive strategies, categorized to their purpose: providing warmth and safety, co‐regulation, and encouragement
FIGURE 3.
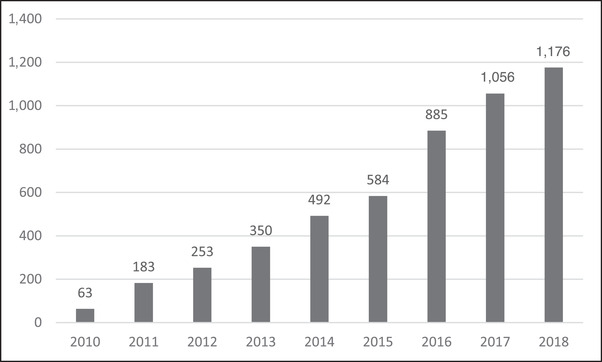
Annual inclusion of infants in the TOP program
2.2.2. Increase the capacity
Until 2012, the TOP program was carried out by pediatric physical therapists who were trained in IBAIP and received additional training and materials to fit the design and objectives of the TOP program. To increase the capacity and match the unique Dutch context, a manual and curriculum for a TOP education program were developed in 2013. The 1‐year education program consists of 14 training days, in combination with reading literature and practical assignments with intensive coaching. The manual includes, among other information, recent scientific insights about early development in all domains, the impact of preterm birth for the infant and the parents, the transition to parenthood, and the protective and risk factors that influence a responsive parent–infant relationship. The curriculum provides training in the observation and interpretation of behavioral expressions in the autonomic, motor, state, and attention/interaction system of 0–12 month infants; the observation and interpretation of the various strategies to support the infant; the use of the TOP model of following and responding for intervention practice; and the use of a strengths‐based approach in oral and written language, signaling infant or parental problems, collaborating with other health care professionals, providing psychoeducation, and using questionnaires. The Dutch Physical Therapy Association accredited the TOP education program. Candidates were pediatric physical therapists selected for their expertise with young infants and preterm babies, their motivation for joining the TOP program, and their location in order to achieve national dissemination. On an annual basis, approximately 12 candidates were trained. During the entire pilot implementation phase, a total of 37 pediatric physical therapists were trained and certified to carry out the TOP program.
2.2.3. Increase the adoption
Multiple strategies were used to enhance familiarity with and knowledge about the TOP program for both parents of VPT infants and healthcare professionals (Table 1). Presentations were given at national conferences and for departments of Neonatology, in regions where TOP interventionists had recently been trained. A brochure was developed and distributed to departments of Neonatology that referred infants to the TOP program. By providing information about the TOP program to different stakeholders, the TOP program was adopted in an increasing number of regions. In 2010, eight of the 10 level III hospitals with NICU facilities in the country and three regional hospitals referred VPT infants to the TOP program and in 2013, nine level III hospitals and 14 regional hospitals did so.
2.2.4. Systematic evaluation and monitoring
To monitor the process and outcomes of the intervention during implementation, a database was developed and records were kept for all infants. The TOP interventionists were asked to complete a digital form about the inclusion criteria for the TOP program (birth weight and gestational age), hospital discharge data, length of hospital stay, the dates of the home visits, and possible reasons for early termination of the program. Parents were asked to fill in questionnaires at the start, half‐way through the program, and at the end of the program. The questionnaires assessed parental anxiety and depression (the Hospital Anxiety and Depression Scale) (Zigmond & Snaith, 1983), infant development (Ages and Stages—III) (Squires, Twombly, Bricker, & Potter, 2009), and infant socioemotional development (Ages and Stages—Socioemotional) (Squires, Bricker, & Twombly, 2015). In addition, a questionnaire was specifically developed to evaluate the satisfaction of the parents with the TOP program. In 2011, the questionnaires, administered on paper, were included in the monitoring system of the TOP program. Regular data monitoring provided insight into the reach and receipt of the TOP program and the target population, creating opportunities to adapt the implementation components to further support implementation of the program.
The combined increase in capacity and adoption resulted in an increase in the reach of the TOP program. On an annual basis in the Netherlands, 1,675–1,800 VPT infants are eligible for the TOP program (Perined, 2015; Perined, 2019). In 2010, 63 VPT infants and their families were enrolled in the TOP program and this increased to 350 VPT infants in 2013 (Figure 2). The perinatal characteristics of infants are described in Table 2. In the pilot implementation phase, 439 families completed the TOP program before December 2013, and 254 mothers (57.8%) of 303 VPT infants filled out the questionnaire to evaluate their satisfaction with it. Overall, mothers rated the quality of the intervention at 9.0 (SD 1.0) on a scale from 1 to 10 (Table 3). The mothers were very positive about most aspects of the TOP program and the TOP interventionist, such as their expertise, attention to their personal background, and their support for increasing confidence in their interactions with their infants. Mothers were less positive about information provision prior to the TOP program. Based on the outcomes of the questionnaire, certain barriers to implementation have been addressed, such as improving the information before the start of the TOP program and developing formats for the presentation of the information, which new TOP interventionists can show in their working area, and developing a webpage.
TABLE 2.
Description of infants enrolled in the TOP program
| Pilot implementation phase | Full implementation phase | |
|---|---|---|
| Time period | 2010–2013 | 2014–2018 |
| N | 849 | 4,193 |
| Gender, male N (%) | 448 (53.3) | 2,243 (53.5) |
| Gestational age, week/day, M (SD) | 29 3/7 (2 3/7) | 29 2/7 (2 2/7) |
| Birth weight, g M (SD) | 1,247.1 (368.3) | 1,250.4 (363.0) |
| Multiples, N (%) | 242 (28.8) | 1,001 (24.6) |
| Days in hospital, M (SD) | 65.1 (31.5) | 68.1 (33.9) |
| Admitted to tertiary center at birth, N (%) | 718 (85.4) | 3,589 (89.5) |
TABLE 3.
Maternal satisfaction with the TOP program
| Maternal satisfaction | Pilot implementation phase N = 254 mothers of 303 infants | Full implementation phase N = 799 mother of 942 infants |
|---|---|---|
| N (%) | N (%) | |
| Global rating a of the care received from the TOP program ≥ 8, N (%) | 238 (93.7) | 775 (96.7) |
| Global rating a of the care received from the TOP program, Mean (SD) | 9.0 (1.0) | 9.3 (0.9) |
| Would recommend therapist, N (%) | 244 (96.0) | 794 (99.4) |
| Good expertise of TOP interventionist, N (%) | 246 (96.9) | 785 (98.2) |
| Sufficiently informed before the program, N (%) | 191 (75.2) | 698 (87.4) |
| Good amount of home visits, N (%) | 240 (94.9) | 719 (90.0) |
Global rating assessed on a Likert scale from 0 to 10.
2.2.5. Mobilizing financial resources for intervention
For full implementation, the TOP program needed to be included in the basic package of Dutch Health Care Insurers, making the program available for all infants without charge. To obtain approval of the DHA and financial support from the Health Care Insurers, we needed to show that the TOP program was feasible, acceptable, and cost‐effective in a real‐world setting. Therefore, a second BC, based on process and outcome measures of the pilot implementation phase (2010–2013) of the TOP program, was written. The aim of our second economic evaluation was to show the efficiency of the implementation of the TOP program in terms of better healthcare outcomes for the infants. Data collected from 115 infants, who were supported by the TOP program during the pilot implementation phase of the TOP program, were compared to historic data from 129 infants who had received routine care, which included standard neonatal follow‐ups and referrals when necessary but did not include a postdischarge intervention program. These 129 infants were 78 infants in the control group of the RCT as well as retrospective data of 51 VPT infants who were admitted to a regional hospital in Amsterdam in 2008. Healthcare utilization was reduced for infants who were supported by the TOP program. Infants in the TOP program received less paramedical support after the intervention had ended (11% in the TOP program vs. 22% in the routine care group), had fewer hospital readmissions (17% vs. 40%), fewer visits to the Emergency Department (20.4% vs. 29.4%), and less reports of child abuse during the first year of life (0.8% vs. 6.4%). Overall, the TOP program showed considerable savings in respect of child health care, combined with better well‐being of the infants at 12 months. The second BC was submitted to the DHA with a request to approve sustainable funding by the Health Care Insurers for the TOP program. Different funding pathways were explored. Feasible funding was accomplished in a bundled payment in terms of which the cost of the TOP program's intervention visits and overhead was included in a package price. After consultation with the DHA and the Dutch Healthcare Insurers, this bundled payment was approved, provided that care performances were described in detail. Therefore, from 2014 onward, the TOP program was included in the basic health insurance package and was available for the total Dutch target population. Overheads per infant were calculated for the management of the organization, including financial management, systematic evaluation and monitoring, quality assurance, and information provision. The rate for the overhead module decreases gradually when the number of children in the program increases. The intervention module included 33.5 hr per family for a year (12 home visits with written reports after each visit, travel costs, and hours for parental coaching). The rate for the intervention module was indexed annually.
2.3. Phase III: Full implementation phase (2014–2019)
In the final phase, the overall aim was to sustain and continuously refine the content, structure, and process of the TOP program by (1) increasing the capacity and maintaining the quality of the intervention; (2) increasing the adoption of the TOP program; and (3) continuing systematic evaluation and monitoring. Here, we present data that were collected between January 2014 and December 2018.
2.3.1. Increase capacity while maintaining the quality of the intervention
As a result of annual training, the number of therapists that provided the intervention increased from 37 in 2013 to 91 in 2018, by then covering most regions in the Netherlands. Apart from the need to make the TOP program available to the target population by training interventionists, it is important to work on maintaining and improving the quality of the TOP program. Therefore, mandatory biannual courses were organized to further support all certified TOP interventionists. Course topics were selected based on the needs of the TOP interventionists. In addition, participation in two regional collective peer learning sessions per year was mandatory for all TOP interventionists. To ascertain the quality of these sessions, moderators received training and had regular refresher courses. Individual coaching was offered by TOP educators when monitoring revealed that additional training was necessary. Furthermore, TOP‐certified therapists were required to support at least five VPT infants per year.
All TOP interventionists met the training criteria and participated in regional collective peer learning sessions. In 2018, the TOP interventionists supported a mean (SD) of 13 (7) VPT infants per year. Only one of the 91 TOP interventionists did not support five or more infants.
2.3.2. Increase the adoption
Information provision about the TOP program for different stakeholders continued. A new website was developed (www.top‐eop.nl), which included a map of the Netherlands locating all TOP interventionists and allowing both parents and professionals to find a TOP interventionist in their region. On an international level, the EOP‐nl team participated in the writing of the European Standards of Care for Newborn Health on the topic of postdischarge responsive parenting programs (EFCNI et al., 2018). This project was organized by the European Foundation for the Care of Newborn Infants (EFCNI), the European Parents Organization, in cooperation with parents, healthcare professionals, and relevant third parties (EFCNI, 2018). From October 2017 to July 2018, a Swedish multiprofessional team was trained in the core principles of the TOP program to carry out an RCT on the effect of an early intervention program for extreme preterm born infants in the Stockholm area (Baraldi et al., 2020). In 2018, all Dutch level III hospitals and 45 of 69 (65%) regional hospitals referred VPT infants.
2.3.3. Systematic evaluation and monitoring
In 2018, 1,177 VPT infants were supported in the TOP program (Figure 2) comprising 70.1% of the Dutch target population (Perined, 2019). This number is expected to increase in step with further improvements in the adoption and capacity of trained TOP interventionists throughout the Netherlands. The TOP interventionists supported an average of 13 VPT infants per year. We estimate that with 120 TOP interventionists, we could reach most families. Not all families will feel the need for postdischarge intervention; however, we have no insight into the number of families that refuse intervention. The perinatal characteristics of infants are described in Table 2.
In May 2014, a web‐based system (www.hetklikt.nu) was set up to enable parents to complete the questionnaires online instead of on paper. After training, the TOP interventionists received access to the web‐based system and gradually replaced the paper‐based system. Thereafter, training to use the web‐based system was included in the TOP education program and from 2015 onward, all TOP interventionists used the web‐based system. In August 2016, a version of the questionnaire that had been revised to evaluate satisfaction with the TOP program was incorporated into the web‐based system, which was more in line with the strategies of the TOP program.
The rate of attrition was low. Data from the web‐based system show that of all the infants enrolled in the program between 2014 and 2017, a total of 2,416 (81.5%) infants received all 12 home visits (Table 4). Only 171 infants (5.8%) received fewer than eight home visits, which was the maximum amount in the intervention in the former RCT on which effectiveness was established. Maternal satisfaction with the TOP program remained high. Between August 2016 and December 2018, 2,233 infants completed the TOP program. At the end of the TOP program, 878 mothers of 1,009 infants (45%) filled out the web‐based questionnaire, and 799 mothers of 942 infants gave permission for their data to be used for scientific research. The mothers were consistently very positive about most aspects of the TOP program and the TOP interventionist: they felt at ease with the TOP interventionist, felt supported in their parenthood, and appreciated the expertise about prematurity, and the support they received for increasing their confidence in their interactions with their infants. Overall, mothers rated the quality of the intervention to be 9.3 (SD 0.9) on a Likert scale from 1 to 10 (Table 3). In the pilot implementation, many parents reported not being sufficiently informed before the program started. Therefore, adaptations were made in the information brochure to provide parents with a better insight into the TOP program. These brochures were distributed nationally in Dutch and English. Parental satisfaction with information provision prior to the TOP program increased from 75.2% in the pilot implementation to 87.5%.
TABLE 4.
Home visits for participants in the TOP program enrolled between 2014 and 2017 and who completed the TOP program before the end of 2018
| Infants | |
|---|---|
| Infants enrolled in the TOP program, N | 2,966 |
| Home visits per infant, M (SD) | 11.3 (1.9) |
| Infants who received all 12 home visits, N (%) | 2,416 (81.5) |
| Infants who received less than 12 home visits, N (%) | 550 (18.5) |
| Infants who received less than eight home visits, N (%) | 171 (5.8) |
|
Known reasons for early termination, N (%) ‐ The infant died, N (%) ‐ Parents perceived further support from the TOP program to be unnecessary, N (%) ‐ Circumstances in the family, N (%) ‐ Family moved (temporarily) to an area without a TOP therapist, N (%) ‐ Difficulty making appointments with the family, N (%) ‐ Not satisfied with the TOP program, N (%) ‐ Other, N (%) |
172 (31.3) 6 (3.5) 75 (43.6) 31 (18.0) 29 (16.9) 15 (8.7) 8 (4.7) 6 (3.5) |
Based on outcomes of the systematic evaluation and on parental and professional feedback, the implementation components and the intervention protocol of the TOP program were further tailored to the context. For instance, in the Neonatal Departments of hospitals in regions with a lower reach, presentations about the TOP program were given, and candidates for the TOP education program for that region were specifically selected. A letter with information for parents on the web‐based system for questionnaires was updated, in Dutch and English, to make it easier for parents to register and use the system. The web‐based system itself was also adapted so that if parents gave their approval, the TOP interventionist had access to the individual answers on the questionnaire evaluating parental satisfaction. This feedback could be used by the interventionists individually to reflect on their own professional performance.
3. DISCUSSION
The TOP program is a preventive responsive parenting program for VPT infants and their parents, after discharge from hospital, which aims to enhance the developmental opportunities for these infants at a critical time of their life. After a 12‐year journey, including three different implementation phases, the program is now implemented on a nationwide scale in the Netherlands. This enables VPT infants and their parents to profit from the TOP program without charge. Currently, the reach of the TOP program is 70% of the Dutch target population and parental satisfaction is consistently high.
To our knowledge, this is one of the few nationally coordinated, postdischarge care services for VPT infants and their families in Europe. Other preventive early intervention programs for VPT infants were found to be effective (Spittle, Orton, Anderson, Boyd, & Doyle, 2015) but have not been transferred into clinical practice. Successfully moving science to a real‐world setting is complex and may take an average of 17 years (Balas & Boren, 2000; Kanter & Courneya, 2019). For the TOP program, 12 years were necessary to carry out the different implementation phases, including an extensive preparation phase. Implementation of the TOP program was facilitated by the high population density in the Netherlands and the large number of pediatric physical therapists specializing in infant development. The advantage is that they worked in existing primary healthcare systems and are well distributed across the country (Britto et al., 2018). Moreover, they were highly motivated to perform the TOP program and follow extensive training. The annual training of interventionists went hand in hand with informing other healthcare professionals and stakeholders in their working areas, which also increased the adoption over time causing increased reach to families in the program. We expect that the current reach of 70% of the Dutch target population is not the endpoint of the implementation of the TOP program based on the continuing work on adoption and training. However, we realize that some families live in areas too remote to be reached by a TOP interventionist and that some families do not feel the need to be supported by postdischarge intervention. Clearly, the TOP program did fulfil the need of the parents, healthcare professionals, and stakeholders to provide suitable support for VPT infants and their parents at home. At the same time, reports from national and international policy makers caught the attention of stakeholders in early childhood development and increased the importance of preventive intervention for VPT families (http://www.1001criticaldays.co.uk/).
The outcomes of the RCT on a child's development until age 5 built a foundation of legitimacy for implementation. However, the political will and the positive results of the BC were fundamental to establish structural financial support for the implementation of the TOP program, showing that the savings of the TOP program outweighed the costs. We assume that the integrated care management model, facilitated by the Center of Expertise, contributed to improve child well‐being, resulting in healthcare cost reduction and satisfaction of the parents with the program. Structural financial support is pivotal for the Center of Expertise to guarantee the organizational infrastructure required for the sustainability and further improvement of the program.
Multiple implementation frameworks for implementation or scalability have been identified (Hanson, Self‐Brown, Rostad, & Jackson, 2016; Milat, Bauman, & Redman, 2015). Each implementation process requires selection of the strategies that are relevant and feasible to that specific context. The principles and strategies described by Grol led to the different phases of the implementation process of the TOP program in the Netherlands (Grol et al., 2005, 2013). The emphasis is on the improvement of the provision of direct patient care, where the patient is at center stage, which corresponds well with the core principles of the TOP intervention.
Systematic evaluation of the feedback from parents and professionals provided continuous guidance for the reach and receipt of the program as well as the changes that were necessary (Grol et al., 2005). Participation and positive engagement of parents during home visits is seen as central to effective intervention for young children and their families (Korfmacher et al., 2008). Parental involvement in the TOP program was represented by the low attrition rate. In the full‐implementation phase, attrition was only 18.5%, 81.5% completed all 12 of the 12 home sessions, and the families who did terminate the program earlier still had a mean of 8.3 home visits. Higher attrition rates have been described in other home visiting programs, ranging between 35% and 50%, and were related to less favorable outcomes after dropping out of the program (Roggman, Cook, Peterson, & Raikes, 2008). The reason for early termination of the TOP program was reported in only 31% of the cases. Only 4.7% of these parents stopped because they were not satisfied with the TOP program, equating to approximately 0.9% of all participants. The engagement of families in the TOP program may have been promoted by flexible delivery options and the focus on the strengths of both infants and parents. These strategies are comparable to the actions that were suggested to lower attrition rates in another home visiting program called the Early Head Start Program (Roggman et al., 2008).
Assuring fidelity along with the flexibility to adapt the intervention over time is a challenge. Pivotal to implementation is having interventionists use intervention strategies effectively. In process‐oriented interventions such as the TOP program, there is room for the parents’ and interventionists’ own initiative. When scaled up, it may impede the degree to which the intervention is delivered as intended. Therefore, interventionists were carefully selected and trained. To help interventionists stay close to the core principles of the TOP program, the intervention program is clearly described, so that it can be taught and learned (Fixsen, Blase, Metz, & van Dyke, 2013). The TOC of the TOP program presents the “active ingredients” of the intervention and the mechanism by which they work, allowing modifications to the intervention that may enhance the benefits or increase sustainability. In addition, much effort was given to the design and training of conceptual models to support intervention practice, such as the model of following and responding. In addition, the Center of Expertise offers biannual courses and collective peer learning sessions, and if needed, ongoing coaching and consultation to advise, encourage, and engage interventionists in the effective use of the program. A limitation of our implementation process is that we did not evaluate the fidelity of the TOP program.
Evaluation of implementation fidelity is important, as it may affect the intervention outcomes. Currently, we are in the process of developing a reliable fidelity tool to assess the adherence and competence of interventionists with the execution of the TOP program. With this tool, we expect to be able to monitor and identify the modifications necessary to enhance the effectiveness of the TOP program for a specific population and to improve the impact for all families.
CONFLICT OF INTEREST
The authors developed and implemented the ToP program but did not personally receive income from the intervention. However, the University Medical Center receives income in the form of research grants.
AUTHOR CONTRIBUTIONS
Martine Jeukens‐Visser was primarily responsible for data collection, data analysis, and writing of the manuscript. Karen Koldewijn was primarily responsible for the development of the TOP program, participated in the development and execution of the implementation protocol, and contributed to the writing of the manuscript. Aleid van Wassenaer‐Leemhuis participated in the development and execution of the implementation protocol and contributed to the writing of the manuscript. Monique Flierman participated in the development of the TOP program, participated in the execution of the implementation protocol, and contributed to the writing of the manuscript. Frans Nollet supervised the design and execution of the implementation protocol as head of the Department of Rehabilitation of the Amsterdam UMC, Academic Medical Center and contributed with critical revision of the manuscript. Marie Jeanne Wolf was primarily responsible for the development and execution of the implementation protocol, participated in the development of the TOP program, and contributed to the writing of the manuscript.
ACKNOWLEDGMENTS
The preparation phase was funded by Agis Healt Insurer, the pilot‐implementation was financially supported by the Innovation Fund Health Care Insurances (Innovatiefonds zorgverzekeraars, project numbers: 1595 and 2469), and the interventions during the pilot‐implementation were reimbursed by all Dutch Health Care Insurers. The Amsterdam UMC, location AMC gave legal, logistical, technical, and staff support during the entire implementation process.
Jeukens‐Visser M, Koldewijn K, van Wassenaer‐Leemhuis AG, Flierman M, Nollet F, Wolf M‐J. Development and nationwide implementation of a postdischarge responsive parenting intervention program for very preterm born children: The TOP program. Infant Ment Health J. 2021;42:423–437. 10.1002/imhj.21902
REFERENCES
- Aarnoudse‐Moens, C. S. , Weisglas‐Kuperus, N. , van Goudoever, J. B. , & Oosterlaan, J. (2009). Meta‐analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics, 124(2), 717–728. 10.1542/peds.2008-2816 [DOI] [PubMed] [Google Scholar]
- Achenbach, T. M. , Howell, C. T. , Aoki, M. F. , & Rauh, V. A. (1993). Nine‐year outcome of the Vermont intervention program for low birth weight infants. Pediatrics, 91(1), 45–55. [PubMed] [Google Scholar]
- Als, H. , Lawhon, G. , Brown, E. , Gibes, R. , Duffy, F. H. , McAnulty, G. , & Blickman, J. G. (1986). Individualized behavioral and environmental care for the very low birth weight preterm infant at high risk for bronchopulmonary dysplasia: Neonatal intensive care unit and developmental outcome. Pediatrics, 78(6), 1123–1132. [PubMed] [Google Scholar]
- Als, H. , Lawhon, G. , Duffy, F. H. , McAnulty, G. B. , Gibes‐Grossman, R. , & Blickman, J. G. (1994). Individualized developmental care for the very low‐birth‐weight preterm infant. Medical and neurofunctional effects. JAMA, 272(11), 853–858. [PubMed] [Google Scholar]
- Balas, E. A. , & Boren, S. A. (2000). Managing clinical knowledge for health care improvement. In Bemmel J. & McCray A. T. (Eds.), Yearbook of medical informatics (pp. 65–69). Stuttgart, Germany: Schattauer Publishing Company. [PubMed] [Google Scholar]
- Baraldi, E. , Allodi, M. W. , Lowing, K. , Smedler, A. C. , Westrup, B. , & Aden, U. (2020). Stockholm preterm interaction‐based intervention (SPIBI) ‐ study protocol for an RCT of a 12‐month parallel‐group post‐discharge program for extremely preterm infants and their parents. BMC Pediatrics, 20(1), 49. 10.1186/s12887-020-1934-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilgin, A. , & Wolke, D. (2016). Regulatory problems in very preterm and full‐term infants over the first 18 months. Journal of Developmental and Behavioral Pediatrics, 37(4), 298–305. 10.1097/DBP.0000000000000297 [DOI] [PubMed] [Google Scholar]
- Britto, P. R. , Singh, M. , Dua, T. , Kaur, R. , & Yousafzai, A. K. (2018). What implementation evidence matters: Scaling‐up nurturing interventions that promote early childhood development. Annals of the New York Academy of Sciences, 1419(1), 5–16. 10.1111/nyas.13720 [DOI] [PubMed] [Google Scholar]
- Clark, C. A. , Woodward, L. J. , Horwood, L. J. , & Moor, S. (2008). Development of emotional and behavioral regulation in children born extremely preterm and very preterm: Biological and social influences. Child Development, 79(5), 1444–1462. 10.1111/j.1467-8624.2008.01198.x [DOI] [PubMed] [Google Scholar]
- de Kieviet, J. F. , Piek, J. P. , Aarnoudse‐Moens, C. S. , & Oosterlaan, J. (2009). Motor development in very preterm and very low‐birth‐weight children from birth to adolescence: A meta‐analysis. JAMA, 302(20), 2235–2242. 10.1001/jama.2009.1708 [DOI] [PubMed] [Google Scholar]
- EFCNI . (2018). European Standards of Care for Newborn Health project report . Retrieved from https://newborn-health-standards.org/call-to-action/
- EFCNI , Koldewijn, K. , Wolf, M. J. , Pierrat, V. , van Wassenaer‐Leemhuis, A. , & Wolke, D. (2018). European Standards of Care for Newborn Health: Post‐discharge responsive parenting programmes .
- Erickson, S. J. , Duvall, S. W. , Fuller, J. , Schrader, R. , MacLean, P. , & Lowe, J. R. (2013). Differential associations between maternal scaffolding and toddler emotion regulation in toddlers born preterm and full term. Early Human Development, 89(9), 699–704. 10.1016/j.earlhumdev.2013.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fixsen, D. L. , Blase, K. A. , Naoom, S. F. , & Wallace, F. (2009). Core implementation components. Research on Social Work Practice, 19(5), 531–540. [Google Scholar]
- Fixsen, D. , Blase, K. , Metz, A. , & van Dyke, M. (2013). Statewide implementation of evidence‐based programs. Council for Exceptional Children, 79(2), 215–230. [Google Scholar]
- Grol, R. , Wensing, M. , & Eccles, M. (2005). Improving patient care: The implementation of change in clinical practice. Oxford, UK: Elsevier. [Google Scholar]
- Grol, R. P. , Wensing, M. , Eccles, M. , & Davis, D. (2013). ‐Improving patient care: The implementation of change in health care (2nd ed.). Hoboken, NJ: Wiley & Sons. [Google Scholar]
- Guralnick, M. J. (2012). Preventive interventions for preterm children: Effectiveness and developmental mechanisms. Journal of Developmental and Behavioral Pediatrics, 33(4), 352–364. 10.1097/DBP.0b013e31824eaa3c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson, R. F. , Self‐Brown, S. , Rostad, W. L. , & Jackson, M. C. (2016). The what, when, and why of implementation frameworks for evidence‐based practices in child welfare and child mental health service systems. Child Abuse & Neglect, 53, 51–63. 10.1016/j.chiabu.2015.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedlund, R. (1998). The Infant Behavioral Assessment and Intervention Program© . Retrieved from http://www.ibaip.org
- Kanter, M. H. , & Courneya, P. T. (2019). Promising methods for improving quality through the faster spread of best practices. Permanente Journal, 23, 19–39. 10.7812/TPP/19-039 [DOI] [Google Scholar]
- Koldewijn, K. , van Wassenaer, A. , Wolf, M‐J. , Meijssen, D. , Houtzager, B. , Beelen, A. , … Nollet, F. (2010). A neurobehavioral intervention and assessment program in very low birth weight infants: Outcome at 24 months. Journal of Pediatrics, 156, 359–365. [DOI] [PubMed] [Google Scholar]
- Koldewijn, K. , Wolf, M. J. , van Wassenaer, A. , Meijssen, D. , van Sonderen, L. , van Baar, A. , … Kok, J. (2009). The Infant Behavioral Assessment and Intervention Program for very low birth weight infants at 6 months corrected age. Journal of Pediatrics, 154(1), 33–38.e32. 10.1016/j.jpeds.2008.07.039 [DOI] [PubMed] [Google Scholar]
- Koldewijn, K. , Wolf, M‐J. , van Wassenaer, A. , Beelen, A. , de Groot, I. J. M. , & Hedlund, R. (2005). The Infant Behavioral Assessment and Intervention Program to support preterm infants after hospital discharge: A pilot study. Developmental Medicine & Child Neurology, 47, 105–112. [DOI] [PubMed] [Google Scholar]
- Korfmacher, J. , Green, B. , Staerkel, F. , Peterson, C. , Cook, G. , Roggman, L. , … Schiffman, R. (2008). Parent involvement in early childhood home visiting. Child & Youth Care Forum, 37(4), 171–196. 10.1007/s10566-008-9057-3 [DOI] [Google Scholar]
- Landry, S. H. , Smith, K. E. , & Swank, P. R. (2006). Responsive parenting: Establishing early foundations for social, communication, and independent problem‐solving skills. Developmental Psychology, 42(4), 627–642. 10.1037/0012-1649.42.4.627 [DOI] [PubMed] [Google Scholar]
- Landsem, I. P. , Handegard, B. H. , Tunby, J. , Ulvund, S. E. , & Ronning, J. A. (2014). Early intervention program reduces stress in parents of preterms during childhood, a randomized controlled trial. Trials, 15, 387. 10.1186/1745-6215-15-387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meijssen, D. , Wolf, M. J. , Koldewijn, K. , Houtzager, B. A. , van Wassenaer, A. , Tronick, E. , … van Baar, A. (2010). The effect of the Infant Behavioral Assessment and Intervention Program on mother‐infant interaction after very preterm birth. Journal of Child Psychology and Psychiatry, 51(11), 1287–1295. 10.1111/j.1469-7610.2010.02237.x [DOI] [PubMed] [Google Scholar]
- Meijssen, D. , Wolf, M‐J. , Koldewijn, K. , van Baar, A. , & Kok, J. (2011). Maternal psychological distress in the first two years after very preterm birth and early intervention. Early Child Development and Care, 181(1), 1–11. [Google Scholar]
- Milat, A. J. , King, L. , Bauman, A. E. , & Redman, S. (2013). The concept of scalability: Increasing the scale and potential adoption of health promotion interventions into policy and practice. Health Promotion International, 28(3), 285–298. 10.1093/heapro/dar097 [DOI] [PubMed] [Google Scholar]
- Milat, A. J. , Bauman, A. , & Redman, S. (2015). Narrative review of models and success factors for scaling up public health interventions. Implementation Science, 10, 113. 10.1186/s13012-015-0301-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milgrom, J. , Newnham, C. , Anderson, P. J. , Doyle, L. W. , Gemmill, A. W. , Lee, K. , … Inder, T. (2010). Early sensitivity training for parents of preterm infants: Impact on the developing brain. Pediatric Research, 67(3), 330–335. 10.1203/PDR.0b013e3181cb8e2f [DOI] [PubMed] [Google Scholar]
- Murray, A. L. , Thompson, D. K. , Pascoe, L. , Leemans, A. , Inder, T. E. , Doyle, L. W. , … Anderson, P. J. (2016). White matter abnormalities and impaired attention abilities in children born very preterm. Neuroimage, 124(Pt A), 75–84. 10.1016/j.neuroimage.2015.08.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Scientific Council on the Developing Child . (2004). Young children develop in an environment of relationships . Working paper no. 1. Retrieved from www.developingchild.harvard.edu
- National Scientific Council on the Developing Child . (2007). The timing and quality of early experiences combine to shape brain architecture . Working paper no. 5. Retrieved from www.developingchild.harvard.edu
- Oostenbrink, J. B. , Koopmanschap, M. A. , & Rutten, F. F. (2002). Standardisation of costs: The Dutch Manual for Costing in economic evaluations. Pharmacoeconomics, 20(7), 443–454. 10.2165/00019053-200220070-00002 [DOI] [PubMed] [Google Scholar]
- Perined . (2015). Perinatale Zorg in Nederland 2014. Utrecht, the Netherlands: Perined. [Google Scholar]
- Perined . (2019). Perintale zorg in Nederland anno 2018: Landelijke perinatale cijfers en duiding. Utrecht, the Netherlands: Perined. [Google Scholar]
- Roggman, L. A. , Cook, G. A. , Peterson, C. A. , & Raikes, H. H. (2008). Who drops out of early head start home visiting programs? Early Education and Development, 19(4), 574–599. 10.1080/10409280701681870 [DOI] [Google Scholar]
- Schmid, G. , Schreier, A. , Meyer, R. , & Wolke, D. (2011). Predictors of crying, feeding and sleeping problems: A prospective study. Child: Care, Health and Development, 37(4), 493–502. 10.1111/j.1365-2214.2010.01201.x [DOI] [PubMed] [Google Scholar]
- Shonkoff, J. P. , & Fisher, P. A. (2013). Rethinking evidence‐based practice and two‐generation programs to create the future of early childhood policy. Development and Psychopathology, 25(4 Pt 2), 1635–1653. 10.1017/S0954579413000813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spittle, A. , Orton, J. , Anderson, P. J. , Boyd, R. , & Doyle, L. W. (2015). Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database of Systematic Reviews. 10.1002/14651858.CD005495.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spittle, A. J. , Anderson, P. J. , Lee, K. J. , Ferretti, C. , Eeles, A. , Orton, J. , … Doyle, L. W. (2010). Preventive care at home for very preterm infants improves infant and caregiver outcomes at 2 years. Pediatrics, 126(1), e171–178. 10.1542/peds.2009-3137 [DOI] [PubMed] [Google Scholar]
- Spittle, A. J. , Cheong, J. , Doyle, L. W. , Roberts, G. , Lee, K. J. , Lim, J. , … Anderson, P. J. (2011). Neonatal white matter abnormality predicts childhood motor impairment in very preterm children. Developmental Medicine & Child Neurology, 53(11), 1000–1006. 10.1111/j.1469-8749.2011.04095.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squires, J. , Bricker, D. , & Twombly, E. (2015). ASQ:SE‐2 user's guide. Baltimore, MD: Brookes. [Google Scholar]
- Squires, J. , Twombly, E. , Bricker, D. , & Potter, L. (2009). ASQ‐3 user's guide. Baltimore, MD: Brookes. [Google Scholar]
- Twilhaar, E. S. , de Kieviet, J. F. , Aarnoudse‐Moens, C. S. , van Elburg, R. M. , & Oosterlaan, J. (2018). Academic performance of children born preterm: A meta‐analysis and meta‐regression. Archives of Disease in Childhood ‐ Fetal and Neonatal Edition, 103(4), F322–F330. 10.1136/archdischild-2017-312916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hus, J. W. , Jeukens‐Visser, M. , Koldewijn, K. , Geldof, C. J. , Kok, J. H. , Nollet, F. , & Van Wassenaer‐Leemhuis, A. G. (2013). Sustained developmental effects of the infant behavioral assessment and intervention program in very low birth weight infants at 5.5 years corrected age. Journal of Pediatrics, 162(6), 1112–1119. 10.1016/j.jpeds.2012.11.078 [DOI] [PubMed] [Google Scholar]
- WHO . (2002). Innovative care for chronic conditions: Building blocks for action. Geneva, Switzerland: WHO. [Google Scholar]
- Wiltsey Stirman, S. , Baumann, A. A. , & Miller, C. J. (2019). The FRAME: An expanded framework for reporting adaptations and modifications to evidence‐based interventions. Implementation Science, 14(1), 58. 10.1186/s13012-019-0898-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf, M. J. , Koldewijn, K. , Beelen, A. , Smit, B. , Hedlund, R. , & de Groot, I. J. (2002). Neurobehavioral and developmental profile of very low birthweight preterm infants in early infancy. Acta Paediatrica, 91(8), 930–938. 10.1080/080352502760148667 [DOI] [PubMed] [Google Scholar]
- Zigmond, A. S. , & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- Zorginstituut Nederland . (2016). Guideline for conducting economic evaluations in healthcare [in Dutch: Richtlijn voor het uitvoeren van economische evaluaties in de gezondheidszorg] . Update from 2006. Guideline for pharmacoeconomic research. Diemen, the Netherlands: Zorginstituut Nederland. [Google Scholar]


