Abstract
Background
Environmental exposures may alter DNA methylation patterns of T helper cells. As T helper cells are instrumental for allergy development, changes in methylation patterns may constitute a mechanism of action for allergy preventive interventions. While epigenetic effects of separate perinatal probiotic or ω-3 fatty acid supplementation have been studied previously, the combined treatment has not been assessed. We aimed to investigate epigenome-wide DNA methylation patterns from a sub-group of children in an on-going randomised double-blind placebo-controlled allergy prevention trial using pre- and postnatal combined Lactobacillus reuteri and ω-3 fatty acid treatment. To this end, > 866000 CpG sites (MethylationEPIC 850K array) in cord blood CD4+ T cells were examined in samples from all four study arms (double-treatment: n = 18, single treatments: probiotics n = 16, ω-3 n = 15, and double placebo: n = 14). Statistical and bioinformatic analyses identified treatment-associated differentially methylated CpGs and genes, which were used to identify putatively treatment-induced network modules. Pathway analyses inferred biological relevance, and comparisons were made to an independent allergy data set.
Results
Comparing the active treatments to the double placebo group, most differentially methylated CpGs and genes were hypermethylated, possibly suggesting induction of transcriptional inhibition. The double-treated group showed the largest number of differentially methylated CpGs, of which many were unique, suggesting synergy between interventions. Clusters within the double-treated network module consisted of immune-related pathways, including T cell receptor signalling, and antigen processing and presentation, with similar pathways revealed for the single-treatment modules. CpGs derived from differential methylation and network module analyses were enriched in an independent allergy data set, particularly in the double-treatment group, proposing treatment-induced DNA methylation changes as relevant for allergy development.
Conclusion
Prenatal L. reuteri and/or ω-3 fatty acid treatment results in hypermethylation and affects immune- and allergy-related pathways in neonatal T helper cells, with potentially synergistic effects between the interventions and relevance for allergic disease. Further studies need to address these findings on a transcriptional level, and whether the results associate to allergy development in the children. Understanding the role of DNA methylation in regulating effects of perinatal probiotic and ω-3 interventions may provide essential knowledge in the development of efficacious allergy preventive strategies.
Trial registration ClinicalTrials.gov, ClinicalTrials.gov-ID: NCT01542970. Registered 27th of February 2012—Retrospectively registered, https://clinicaltrials.gov/ct2/show/NCT01542970.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13148-021-01115-4.
Keywords: Allergy prevention, Combined intervention, Cord blood, CD4+ T cells, DNA methylation, Lactobacillus reuteri, MethylationEPIC 850K, ω-3 fatty acids, Prenatal, Postnatal
Introduction
Present-day increases in allergy prevalence in urbanised societies may be caused by the extensive loss of diverse microbial exposures due to changed lifestyle habits, thereby affecting development of appropriate immune responses [1, 2]. This is particularly important throughout the perinatal period, when maternal exposures during pregnancy and breastfeeding lay the foundations of, and influence, immune development of the foetus and the newborn child [3–6]. Immune maturation begins prenatally during the second trimester [7], and transplacental transfer of nutrients and metabolites, produced by the maternal commensal microbiome from ingested dietary compounds, may affect not only growth but also immune development of the foetus [6]. Postnatally, breastfeeding provides nutrients as well as microbiota, immune cells and immune mediators [4]. Hence, the maternal influence on the foetal immune system is significant, and the composition of both the maternal diet and her commensal microbiome is crucial in the process [8, 9].
By supplementing pregnant women, with a high propensity of having an allergic child, during pregnancy and lactation with ω-3 fatty acids and probiotics, it may be possible to modulate the foetal immune system towards tolerance [8, 10, 11]. In Westernised societies the dietary fatty acid intake favours ω-6 over ω-3 fatty acids [12, 13], thereby promoting production of pro-inflammatory mediators, such as prostaglandins and leukotrienes [14], and possibly sustaining allergic inflammation [11]. However, by ω-3 supplementation this ratio may be altered and promote downstream production of immunoregulatory mediators [11]. ω-3 fatty acids may dampen allergic inflammation by inhibiting effects of IL-4 and IL-13, as well as by preventing isotype switching of B cells to IgE-antibodies [8]. Indeed, prenatal ω-3 intervention attenuated IL-4 and IL-13 levels in cord blood [15], and decreased the risk of developing asthma in the offspring [16]. Previously, we have investigated the effects of pre- and postnatal ω-3 supplementation, demonstrating lower prevalence of sensitisation and IgE-associated eczema throughout the first year of life [17], and a decreased risk of developing any IgE-associated disease up to 2 years of age [18], in ω-3 compared to placebo-treated children. Several studies point at altered gut microbiomes in children developing allergies [19–24], suggesting that increasing gut microbial diversity by e.g. probiotic intervention may be helpful in allergy prevention [25]. Lactobacilli, a commonly used family of probiotic bacteria, induce both innate and adaptive immunostimulatory responses, apart from improving barrier integrity and modulating gut microbiota composition [26]. We have previously shown allergy preventive effects on IgE-associated eczema upon supplementation with Lactobacillus reuteri [27]. Interestingly, children whose mothers had allergic symptoms revealed the greatest benefits of the L. reuteri treatment [27], whereas ω-3 treatment provided most benefit to children whose mothers did not have allergic symptoms [17, 18]. This suggests that combining the treatments could benefit allergy prone children regardless of maternal allergy status, and possible synergistic effects of the immunostimulating probiotics and the immunomodulatory ω-3 fatty acids could occur. However, this has thus far not been studied.
A suitable way to evaluate the effects of supplemental interventions would be to study epigenetic modifications, since they regulate transcriptional accessibility of genomic regions in response to environmental stimuli [28]. DNA methylation of CpG sites is considered the most stable epigenetic modification, and while it often is considered to lead to transcriptional repression, this is mainly true in promoter regions, as the same patterns in e.g. intergenic regions result in transcriptional activation [29, 30]. Furthermore, epigenetic mechanisms including DNA methylation are known to regulate the differentiation of T helper cells [31], which are central in development of allergic disease [28]. Indeed, differential DNA methylation patterns associate with development of sensitisation [32, 33], asthma [34, 35] and food allergies [36, 37] in children and adolescents. Epigenetic studies of prenatal fatty acid intervention have shown effects on histone modifications [38], while others report conflicting results on DNA methylation patterning [39, 40]. A study on epigenomic modulation of combined L. rhamnosus GG/Bifidobacterium lactis in obesity [41] revealed general hypomethylation, in line with findings from our previous study investigating L. reuteri in allergy prevention [42]. In newborns whose mothers had been supplemented with L. reuteri throughout the last month of pregnancy, this loss of methylation in CD4+ cord blood cells was prominent in genes related to immune activation [42]. This could indicate that treated children received a head-start in their immune maturation, which hence may affect the development of allergic disease. However, in the context of combining probiotics and ω-3 fatty acids, neither clinical outcomes nor epigenetic effects have yet been studied.
In the on-going PROOM-3 trial (PRObiotics and OMega-3, ClinicalTrials.gov-ID: NCT01542970), the allergy preventive effects of combined L. reuteri and ω-3 fatty acids supplementation, from mid-pregnancy throughout the first year of life of the child, are studied. In this paper, we examined epigenome-wide DNA methylation patterns in cord blood CD4+ cells from a sub-group of the PROOM-3 cohort. Our hypothesis was that the earlier initiated probiotic treatment will lead to more prominent effects on DNA hypomethylation in immune-related genes compared to the previous study [42]. Likewise, we hypothesised that ω-3 fatty acid supplementation will lead to hypomethylation of immune-related sites, and possibly work synergistically with the probiotic intervention to cause the greatest differential methylation in immunological pathways. Our findings indicate that the epigenome is modulated by the prenatal treatment with probiotics and ω-3 fatty acids, which may have implications for developing and improving future allergy prevention strategies.
Results
Differential DNA methylation analyses reveal mainly hypermethylated CpGs and genes upon supplementation with L. reuteri and/or ω-3 fatty acids
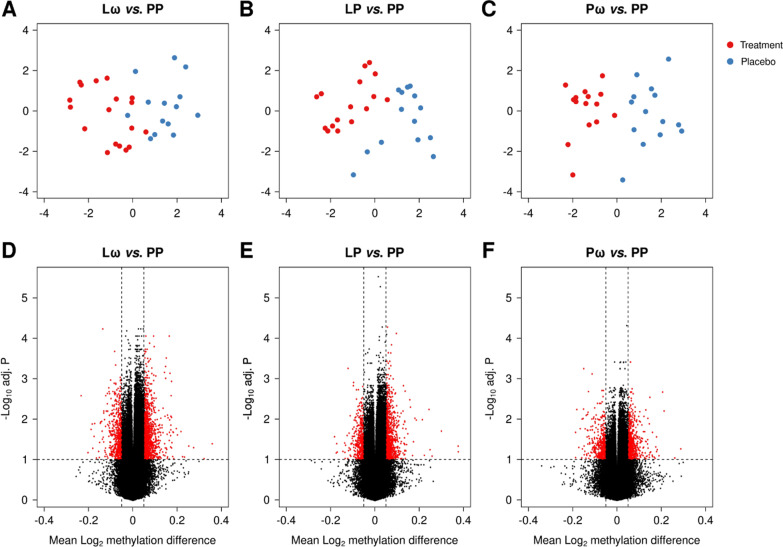
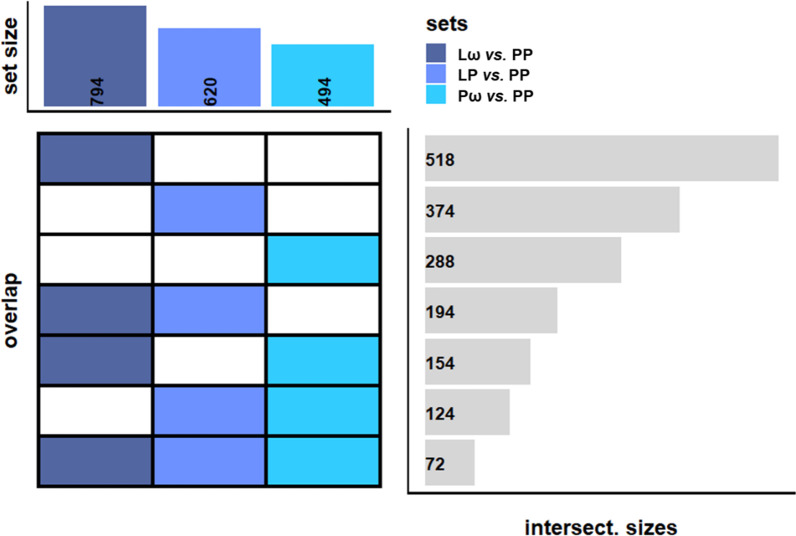
Comparisons of demographic variables revealed no differences between the treatment groups, except for a higher proportion of females in the ω-3 single active treatment (Pω) group (Table 1). This led us to exclude the sex chromosomes from further analyses, as retaining them might affect downstream results. Thereafter, we pursued multidimensional scaling (MDS) analyses to investigate inherent differences between the three active treatment groups, the double L. reuteri and ω-3-treated group (Lω), the L. reuteri single-treated group (LP) and the ω-3 single-treated group (Pω), compared to the double placebo group (PP). These analyses revealed distinct differences between the treated and untreated groups (Fig. 1A–C), indicating treatment-associated changes at the epigenome level. We then proceeded to analyse differential DNA methylation, using an FDR-adjusted p value threshold of < 0.1 along with a mean methylation difference (MMD) of > 5% to define differentially methylated CpGs (DMCs). The double-treated Lω group demonstrated the highest number of DMCs compared with the single active treatment groups (Lω: 1659, LP: 1246 and Pω: 984 CpG sites, respectively, Table 2). A majority of the DMCs were hypermethylated (58–70%, Table 2, Fig. 1D–F, Additional file 1: Table S1) in all three comparisons, suggesting that prenatal treatment with probiotics and/or ω-3 fatty acids foremostly may lead to transcriptional inhibition. To investigate the biological impact of these findings, the DMCs were mapped to their corresponding differentially methylated genes (DMGs), which thereafter were utilised for pathway enrichment analyses. The double-treated Lω group contained 794 genes compared to 620 and 494 genes in the single-treated LP and Pω groups, respectively (Fig. 2, Additional file 2: Table S2), and 72 genes were shared for all three comparisons (Fig. 2, Additional file 3: Table S3). Pathway enrichment analyses of the DMGs in the respective comparisons revealed 87 pathways for the Lω group, including immune-related pathways such as PI3K-Akt and MAPK signalling,
Table 1.
Demographic characteristics of children with available cord blood samples from the PROOM-3 study
| Intervention group | Lω | LP | Pω | PP |
|---|---|---|---|---|
| Group description and size |
L. reuteri + ω-3 PUFA n = 18 |
L. reuteri + Placebo n = 16 |
Placebo + ω-3 PUFA n = 15 |
Placebo + Placebo n = 14 |
| Female | 6/18 (33%) | 7/16 (44%) | 12/15 (80%)* | 3/14 (21%) |
| Birth week | 39.5 (39.0–41.0) | 40.0 (38.8–40.2) | 40.0 (40.0–41.0) | 40.0 (39.0–41.0) |
| Treatment duration | 19.0 (19.0–21.2) | 19.5 (19.0–20.0) | 20.0 (19.5–21.0) | 20.0 (19.0–20.8) |
| Maternal age (birth) | 31.0 (29.0–32.8) | 32.0 (30.0–33.2) | 32.0 (29.0–33.0) | 30.0 (28.2–32.5) |
| Caesarean delivery | 3/17 (18%) | 0/16 (0%) | 1/15 (7%) | 1/14 (7%) |
| Birth weight (kg) | 3.8 (3.6–3.9) | 3.5 (3.3–3.9) | 3.9 (3.7–4.1) | 3.8 (3.6–4.1) |
| Birth height (cm) | 51.0 (50.0–52.0) | 51.5 (49.8–52.2) | 51.0 (50.5–52.5) | 51.0 (50.0–52.0) |
| Maternal atopy | 14/18 (78%) | 11/16 (69%) | 7/15 (47%) | 8/14 (57%) |
| Paternal atopy | 9/18 (50%) | 9/16 (56%) | 9/15 (60%) | 11/14 (79%) |
| Siblings | 1.0 (0.0–1.0) | 1.0 (0.0–1.2) | 1.0 (0.0–1.5) | 0.0 (0.0–1.0) |
| People in home | 4.0 (3.0–4.0) | 4.0 (3.0–5.0) | 3.0 (3.0–4.0) | 3.5 (3.0–4.0) |
| Smoking in home | 0/18 (0%) | 0/16 (0%) | 0/12 (0%) | 1/14 (7%) |
| Breastfeeding (at 3 months) | 15/18 (83%) | 12/16 (75%) | 9/12 (75%) | 12/14 (86%) |
| Antibiotics (during first 3 months) | 1/15 (7%) | 1/14 (7%) | 0/10 (0%) | 0/11 (0%) |
| Pets in home (at 3 months) | 4/18 (22%) | 5/16 (31%) | 3/11 (27%) | 1/13 (8%) |
|
Naïve CD4+ CD45RA + cells (%) |
95.6 (94.6–97.4) | 96.6 (95.7–97.1) | 95.7 (95.3–97.3) | 95.9 (94.5–96.9) |
|
Memory CD4+ CD45RA- cells (%) |
4.4 (2.6–5.4) | 3.4 (2.9–4.3) | 4.3 (2.7–4.7) | 4.1 (3.1–5.5) |
Demographic variable information was retrieved from parentally reported questionnaire data at the three month follow-up. Continuous variables are expressed as medians with interquartile ranges and were analysed using the Shapiro–Wilk’s test of normality followed by Levene’s test of equal variances and the Kruskal–Wallis H test. For the categorical variables, the Pearson χ2 test was performed and the data is presented as n/N (%). *denotes significantly more females than males in the Pω group, p = 0.01. L—Lactobacillus reuteri, ω—ω-3 fatty acids, P—placebo
Fig. 1.
Graphical representations of multidimensional scaling (MDS) analyses are shown in panels A–C for the double active (Lω) and single active treatment groups (LP, Pω), respectively, in comparison to the double placebo group (PP). Red dots represent the active treatment group, blue dots the placebo group. In panels D-F, volcano plots illustrate the distribution of DMCs when comparing each of the active treatment groups to the double placebo group (PP). DMCs are defined as having an MMD of > 5% along with an FDR-corrected p value of < 0.1, and are depicted as red dots. DMC—differentially methylated CpG, MDS—multidimensional scaling, MMD—mean methylation difference, L—Lactobacillus reuteri, ω—ω-3 fatty acids, P—placebo
Table 2.
Results from the differential methylation analyses, comparing the active treatments vs. the double placebo group
| Intervention group | Lω vs. PP | LP vs. PP | Pω vs. PP |
|---|---|---|---|
| DMCs | 1 659 | 1246 | 984 |
| Hypomethylated CpGs | 576 (35%) | 380 (30%) | 415 (42%) |
| Hypermethylated CpGs | 1083 (65%) | 866 (70%) | 569 (58%) |
| DMGs | 794 | 620 | 494 |
| Hypomethylated genes | 247 (31%) | 204 (33%) | 184 (37%) |
| Hypermethylated genes | 524 (66%) | 405 (65%) | 295 (60%) |
| Mixed methylation genes | 23 (3%) | 11 (2%) | 15 (3%) |
Proportions of hypo- and hypermethylated CpGs and genes, from the differential DNA methylation analyses comparing the active treatment groups vs. the double placebo group, are presented as n (% of total). DMCs—differentially methylated CpGs, DMGs—differentially methylated genes, L—Lactobacillus reuteri, ω—ω-3 fatty acids, P—placebo
Fig. 2.
A graphic representation of overlapping DMGs between the different comparisons. The sets represent the different comparisons, and the intersectional sizes show the number of overlapping genes between the comparisons. Dark blue represents the double-treated group, light blue the L. reuteri single-treated group and coral blue the ω-3 single-treated group. DMGs—differentially methylated genes, L—Lactobacillus reuteri, ω—ω-3 fatty acids, P—placebo
Phospholipase D signalling and T cell receptor signalling (Additional file 4: Table S4). The LP group revealed 20 pathways, amongst others the Rap 1, Phospholipase D signalling and Th17 differentiation pathways (Additional file 5: Table S5), whereas the Pω group did not reveal any pathways at all.
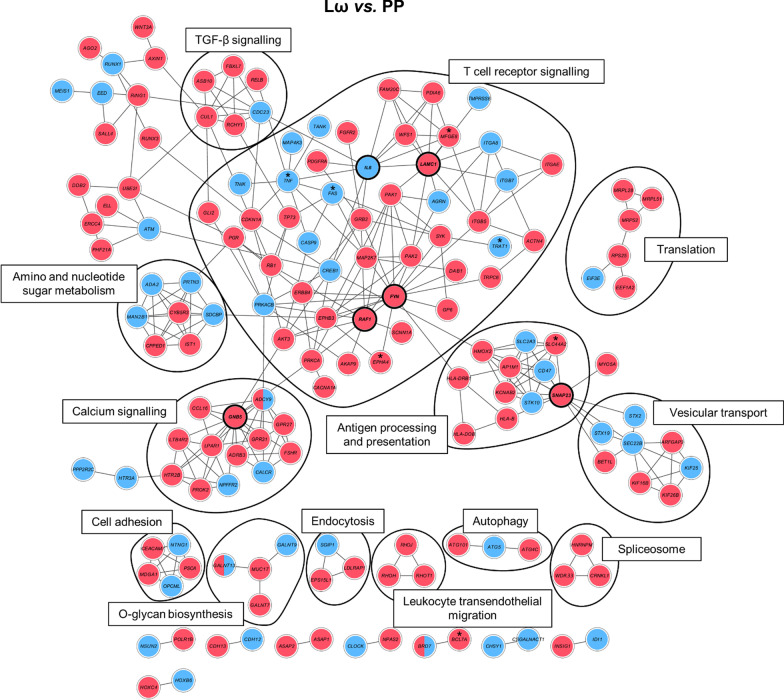
Network analyses show immune-related pathways being affected by the interventions
As a means to further elaborate on the wider biological context in which the putatively supplementation-induced DMGs act, the DMGs were mapped onto a protein–protein interaction map (STRING-db) to study these interactions in a network context. The most interconnected modules were derived from DMGs identified by four module discovery methods from the MODifieR [43] package. This approach narrowed down the number of supplementation-induced DMGs to 170, 100 and 87 genes for the Lω, LP and Pω comparisons, respectively (Additional file 3: Tables S6–S8). High-confidence interactions from the respective modules are displayed in Fig. 3 and Additional file 5: Figs. S2–S3. Of the 170 genes identified in the double-treated Lω module, six genes were considered highly connected (exhibiting 10 or more connections to other module genes), and could be considered important hubs within the network: FYN, GNB5, SNAP23, LAMC1, IL6 and RAF1 (Fig. 3). All genes but IL6 were hypermethylated. Inspecting the network module for biologically relevant clusters, pathway enrichment analyses of those clusters revealed that supplementation with both L. reuteri and ω-3 affects pathways such as T cell receptor signalling, antigen processing and presentation as well as TGF-β signalling (Fig. 3, Additional file 3: Fig. S3), clusters that were also observed in corresponding analyses of the single-treated groups (Additional file 3: Figs. S1–S2, S4–S5).
Fig. 3.
Visualisation of the consensus module created with the DMGs from the differential methylation comparison between the double-treated L.reuteri/ω-3 (Lω) and the double placebo (PP) group. Nodes represent genes and connecting lines represent protein–protein interactions (STRING combined score > 0.7) within the network. Red nodes illustrate hypermethylated genes, blue nodes indicate hypomethylated genes and both colours denote mixed methylation patterns. Black lines enclose biologically relevant clusters identified by bioinformatic pathway enrichment analyses. Nodes marked with * are also present in an independent allergy data set (described later in the paper). DMGs—differentially methylated genes, L—Lactobacillus reuteri, ω—ω-3 fatty acids, P—placebo
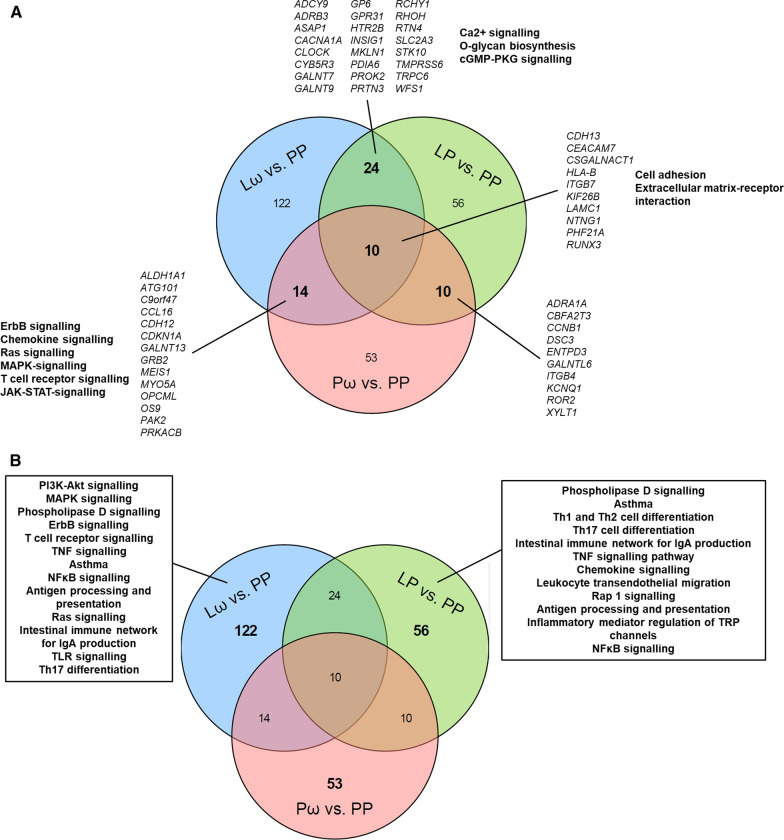
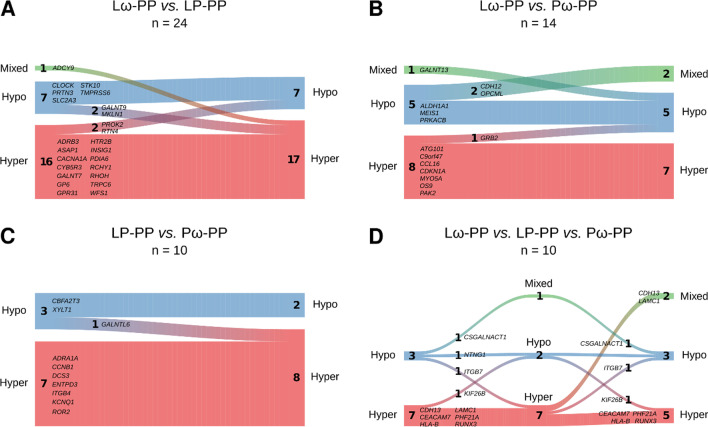
To further evaluate common and unique features of the obtained supplementation modules, comparisons were made between the three treatment groups. While 10 genes were shared between all three comparisons, 24, 14 and 10 genes overlapped when comparing the Lω group to the L. reuteri single-treated (LP) group, the Lω to the ω-3 single-treated (Pω) group and the single-treated groups (LP vs. Pω) to each other, respectively (Fig. 4A, Additional file 3: Table S9). Genes common to all treatment groups related to cellular adhesion and extracellular matrix-receptor interaction pathways, whereas the comparisons between the single-treated groups revealed no significant pathways. Compared to the Lω double-treated group, overlaps to the single-active Pω group related to T cell receptor signalling and other related signal transduction pathways, while overlaps to the LP group included Ca2+ signalling and O-glycan biosynthesis (Fig. 4A), pathways which are relevant for proper T cell function. The largest number of unique genes were revealed for the double active Lω treatment group (122 genes), which were mainly biologically related to T cell receptor signalling and related signal transduction pathways, TNF and NFκB signalling as well as asthma (Fig. 4B). The single-treated groups showed similar numbers of unique genes (LP: 56 genes, Pω: 53 genes), which related to Th1/2/17 helper cell differentiation and asthma amongst other pathways for the LP group, while yet again no relevant pathways were discovered for the Pω treatment group. Hence, combined probiotic and ω-3 supplementation seems to have synergistic effects at the network level compared to the single treatments.
Fig. 4.
Venn diagrams illustrating the degree of overlap and uniqueness for the obtained genes from the three network modules for the double active treatment (Lω vs. PP) and the single active treatment (LP vs. PP, Pω vs. PP) comparisons. In A the number of common genes from the overlap are displayed for each comparison is shown, with corresponding gene names denoted in italics, and selection of related pathways in bold. No relevant pathways were revealed for the shared genes of the LP vs. PP and Pω vs. PP comparisons. In B the number of genes that are unique for each comparison are displayed along with a selection of corresponding related pathways. No pathways of relevance were revealed for the unique genes from the Pω vs. PP comparison. L—Lactobacillus reuteri, ω—ω-3 fatty acids, P—placebo
Further evaluation of the direction of methylation in the shared genes revealed that treatment with either L. reuteri or ω-3 fatty acids led to consistent methylation patterns in most of the genes when compared to the double-treated Lω group (Fig. 5A, B, Additional file 3: Table S9). This pattern was even more distinct comparing the single active treatment groups, where only one gene revealed different methylation patterns between the groups (Fig. 5C). In the comparison between all three treatment groups, however, the patterning of approximately half the genes were similar, whereas the single active groups exhibited different and still distinct shared DNA methylation patterns with the Lω group (Fig. 5D).
Fig. 5.
River plots illustrating the methylation status for overlapping genes being shared between the double-treated Lω group and A the single-treated probiotic (LP vs. PP), and B ω-3 treated (Pω vs. PP) group. Panel C illustrates comparisons between the single treated groups (LP and Pω vs. PP) and D shows the comparison between all treatment groups. Genes are represented as flows of size proportional to number of genes within their methylation status in a particular set, and differences between sets are shown as connections between flows. The respective gene names are denoted next to each flow. Red represents hypermethylation, blue hypomethylation and green a mixed methylation pattern. The number of genes in the respective flows are denoted in the graph. L—Lactobacillus reuteri, ω—ω-3 fatty acids, P—placebo
Differentially methylated CpGs in the active treatment groups were enriched in an independent allergic disease data set
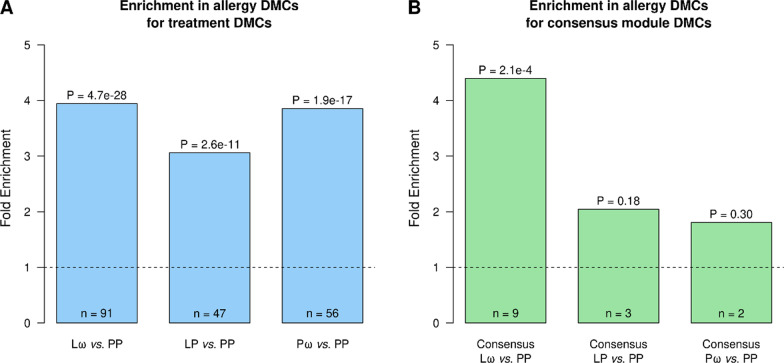
As no information is as yet available on allergy development for the children included in this study, we pursued enrichment analyses on DMCs extracted from the differential DNA methylation analyses for all three comparisons, and compared them to DMCs of a publicly available allergy data set, studying DNA methylation patterns in CD4+ T cells of adults with seasonal allergic rhinitis (8 patients vs. 8 controls). Indeed, for all three comparisons, a substantial number of DMCs were significantly enriched within the allergy data set (Lω: 91, p = 4.7e−28, LP: 47, p = 2.6e−11 and Pω: 56 CpGs, p = 1.9e−17, Fig. 6A). Investigating involved pathways of the genes from these DMCs, few or no pathways emerged (results not shown). Three CpG sites overlapped between the three groups (in the genes MYOF, C6orf123 and PTPRN2), while additionally 8 and 11 CpGs were common comparing the the double-treated Lω group to the single-treated LP and Pω groups, respectively, and 4 CpGs were overlapping between the single-treated groups (Additional file 3: Table S10).
Fig. 6.
Enrichment analyses relating DMCs from A. differential DNA methylation analyses and B. network analyses for all three comparisons, to DMCs from a study investigating DNA methylation patterns in adults with seasonal allergic rhinitis. Panel A shows treatment DMC overlaps with allergy DMCs. Panel B shows consensus module gene associated DMC overlaps with allergy DMCs. The number of overlapping DMCs is shown at the bottom of the bars (n). A one-sided Fisher’s exact test was used for the enrichment analyses. Computed p values represent the enrichment significance, while the fold enrichment illustrates how over-represented the overlap is, compared to what would be expected by chance for the given background
As some results from the network analyses indicated involvement of network genes in allergy-related pathways, we additionally pursued comparisons of our DMCs from the consensus modules for all three comparisons to the above mentioned allergy data set. Enrichment analyses revealed that there was a significant overlap between our DMCs identified by the double-treated Lω network module and allergic disease (9 genes, p = 0.00021, Fig. 6B), while no significant enrichments were revealed for the single-treated groups. Examining these nine genes within the Lω module in more detail, four were hypomethylated (TNF, FAS, TRAT1 and HIVEP3), while five were hypermethylated (SLC44A2, MFGE8, EPHA4, BCL7A and RAB11FIP1), and seven of these genes were present within the connected components of the network (all but HIVEP3 and RAB11FIP1, Fig. 3, genes marked with asterisks). Six out of seven genes were furthermore located to the central parts of the network, mainly involved in T cell receptor signalling and antigen processing and presentation. Comparing the direction of methylation to the independent allergy data set, four genes exhibited the opposite direction of patterning (HIVEP3, TRAT1, BCL7A and SLC442A), while the DNA methylation patterning of the remaining genes were identical between the groups (Additional file 3: Fig. S6).
Discussion
The role of perinatal combined allergy prevention interventions on epigenetic patterning in T helper cells has hitherto been unknown. In this paper, we set out to assess the epigenome-wide effects of combined maternal probiotic and ω-3 intervention during the latter half of pregnancy on CD4+ cells from cord blood samples in an on-going allergy prevention trial. Indeed, we show that prenatal supplementation associates with epigenomic changes of T cells from cord blood in the neonates, and the different treatments associate with different alterations in DNA methylation patterning.
The main finding of this study was that the largest treatment-induced effect on the epigenome was revealed in the Lω double active treatment group, and that regardless of treatment hypermethylation was the main outcome. The network analyses revealed the same pattern in the created intervention modules, and the genes shared between the comparisons as well as the performed network analyses revealed common biological pathways. The Lω module made up the highest number of genes while fewer, but still significant, numbers were revealed in the single-treated LP and Pω modules. This indicates that there might be some synergistic effects of the double treatment. Although the number of shared genes from the networks were limited and the methylation patterns of the genes were only partly similar, this further suggests that the combined treatment may modulate the epigenetic response differently from the single treatment groups. Probiotics may affect DNA methylation either by the production of metabolites downstream of short chain fatty acids, which are indispensable co-factors for proper functioning of enzymes such as DNA methyltransferases, or directly by modifying the actions of the same enzymes [44]. Similarly, ω-3 fatty acid intervention may alter DNA methyltransferase activity [45] and regulation of transcription factor activity [46]. However, how the combination of the two treatments act on a molecular level still needs further elaboration. Examining the genes that were unique to the respective comparisons, the Lω and LP groups featured large numbers of immune-related pathways, yet again involving signal transduction pathways important for T cell signalling, but also T helper cell differentiation and asthma. This is particularly interesting, and future studies on these children will have to settle whether induced DNA methylation differences are associated with the development of allergic disease. Altogether, our findings propose that the interventions modulate the epigenome, and more specifically so in pathways that are of general importance for proper T cell development and function.
To further understand the impact of the prenatal intervention on the epigenome, genes that were highly connected within the module network were scrutinised in detail. In the double-treated Lω group, six genes had more than 10 connections to other genes within the network. One of the genes was FYN, a non-receptor tyrosine-protein kinase involved in the downstream signal transduction pathway of the T cell receptor, regulating amongst other things T cell activation and differentiation [47]. In this study, FYN was hypermethylated, suggesting that the gene would be transcriptionally silenced by treatment and thereby also downregulating putative protein functions. Another gene of interest was the hypomethylated inflammatory cytokine gene IL6. IL-6 is heavily involved in the development and maintenance of inflammation, by inducing both innate and adaptive inflammatory immune responses [48]. In modulation of the latter, IL-6 regulates both proliferation and cytokine responses of CD4+ cells by inducing JAK/STAT, MAPK and PI3K-Akt signalling pathways, and downstream effects of this activation have been implicated in development of asthma. On an epigenomic level, hypomethylation of IL-6 has been shown in children with peanut allergy [49], and it has also been associated to worse lung function in asthmatic children [50]. Furthermore, in the first 6–12 months of life, the IL6R gene was hypomethylated in a pre-and postnatal probiotic intervention study investigating development of obesity in children [41]. As we are still collecting information about development of allergic disease such as asthma in the present PROOM-3 study, the long term implications of this finding are unknown. It is possible, however, that the intervention enables transcriptional accessibility of this gene, and hence equips the child with early inflammatory capacity. This notion is in line with the observed overlap of DMCs from the Lω consensus module with the publicly available allergy data set. Three hypomethylated genes from the T cell receptor signalling cluster were of particular interest: TNF, FAS and TRAT1. The T cell receptor-associated transmembrane adaptor protein TRAT1 is known to stabilise the T cell receptor/CD3 complex, and may thereby modulate downstream signal transduction and promote T cell function [51, 52]. TRAT1 was hypomethylated in the Lω group, whereas it was hypermethylated in the independent allergy data set, making it tempting to speculate that the combined intervention may enable proper T cell signalling propagation into the cell. While the cytokine tumor necrosis factor (TNF) may not only promote inflammatory responses and induce proliferation of both naïve and memory T cells, it may also drive apoptosis of effector T cells [53]. Similarly, the TNF-related FAS receptor may also induce apoptosis of cells by binding to FASL, leading to recruitment of caspase-8 and -10 and subsequent commencement of programmed cell death [54]. This process is of crucial importance in the establishment of peripheral tolerance, and as TNF and FAS were hypomethylated in the Lω comparison, this suggests that anti-inflammatory effects of TNF and FAS could be promoted by the supplementation of probiotics and ω-3 prenatally. However, further studies on transcriptional and protein levels of these mediators, along with functional studies in relation to allergy development should shed light on the relevance of these findings upon prenatal interventions.
During pregnancy, maternal exposures including her diet are instrumental in the shaping of foetal immunity, and her immediate influence on neonatal immune responses continues throughout breastfeeding [4, 6]. Transplacental transport enables maternal-to-foetal transmission of long-chain polyunsaturated fatty acids (such as ω-3) [55] as well as antibodies carrying microbial components originating from both commensals and pathogens [6]. Moreover, breastmilk contains long-chain polyunsaturated fatty acids [55], and probiotics may translocate from the maternal to the infant gut via the breastmilk [56]. While supplemented probiotics generally do not permanently colonise neither the mother nor the infant gut during perinatal exposure, conflicting results have been reported on long-term effects on infant gut microbiota composition [57–59]. Interestingly, ω-3 fatty acid supplementation has been reported to temporarily affect the gut microbiota abundance in adults [60]. As both probiotics and ω-3 fatty acids may modulate the DNA methylation process [44–46], this suggests that the dual supplementation in this study could provide combined epigenetic effects, both in terms of synergy of treatments as well as of the timing of pre- and postnatal intervention. In the present study, we assessed the effect of prenatal L. reuteri and/or ω-3 treatment on the epigenome of cord blood CD4+ cells, as we in a previous study observed the largest epigenetic effects of perinatal treatment with L. reuteri at the time of birth [42]. Studying how the combined supplementation will affect the epigenome later in infancy will, however, be particularly interesting as the interventions are commenced during breastfeeding and the first year of life for the ω-3 and L. reuteri treatments, respectively. As several studies have pointed at the importance of both pre- and postnatal treatment for allergy preventive effects [5, 61, 62], we would anticipate the effects to be, if not potentiated, then at least sustained throughout the treatment period.
One quite surprising finding of this study was that, in contrast to our hypothesis and results from our previous epigenome-wide study on the effects of perinatal L. reuteri treatment on cord blood CD4+ cells [42], a larger proportion of the CpG sites were hypermethylated when comparing either of the intervention groups to the double placebo group. This finding could have several explanations. First of all, unlike our previous studies investigating possible allergy preventive effects of perinatal probiotic intervention [42] or ω-3 intervention [17, 18] the combined intervention was initiated already at gestational (GW) 20 in the PROOM-3 study, compared to GW 25 for ω-3 fatty acid [17] and GW 36 for L. reuteri [63] supplementation in the previous study. Additionally, the maternal dosage of the L. reuteri strain was also higher by an order of magnitude in this study (109 colony forming units (CFU), compared to 108 CFU previously [63]), possibly allowing for potentiated effects of the probiotic intervention. Furthermore, we here utilised Illumina’s Infinium MethylationEPIC 850K array, surveying more than 866 000 sites all over the genome. Despite including more than 90% of the investigated sites from the previous Illumina 450 K platform [64], almost twice the amount of DNA methylation probes were investigated. This could possibly explain why the present findings differ from the previous study where the Illumina 450 K platform was used. Also, as only autosomal chromosomes were retained the present analyses, this may have affected the outcomes in relation to our previous study [42], where all chromosomes were included in the analyses. Altogether, these modifications to the study, experimental and statistical protocol could possibly explain the apparent reversed observations in terms of major hypermethylation upon intervention with L. reuteri and/or ω-3 fatty acids in this study, in contrast to hypomethylation upon L. reuteri intervention previously [42]. The observed general hypermethylation needs, however, to be assessed on a transcriptional and protein expression level to evaluate the possible supplementation-induced biological impact in the treated children.
Advantages of the present study include the performance of the DNA methylation analyses in purified CD4+ T cells, cells which are instrumental for development of specific long-term immune responses in general, but also for the development of allergic diseases in particular [2]. The performance of network analyses provides another benefit of this study, where the analyses have generated putative candidate genes to study further in an allergy development and prevention context. Also, despite our relatively small sample numbers, we are able to evaluate all four intervention groups in this study, enabling us to shed light on treatment-specific effects on the methylome.
Regarding limitations of the present study, the relatively small sample size limits the power of our analyses. However, we have in several ways ascertained the robustness of our data by various quality control measures, including e.g. examining maternal cell contamination, differences in estimated cell proportions, singular value decomposition and genomic inflation analyses. Another drawback is that we did not assess the contribution of different T helper cell subsets or effector/central memory cell populations to our data. Although we cannot conclusively exclude that epigenomic differences seen in our data could originate from differences in e.g. proportions of different T helper cell sub-populations, the inclusion of information on naïve and memory cell proportions from our purified CD4+ samples as a co-variate in the linear models should partly compensate for this possibility. Furthermore, we have in our statistical analyses required the fulfilling of both FDR < 0.1 and MMD ≥ 5% criteria for differential methylation, and in the module network analyses that the genes were identified by all four module-identifying methods. As we are able to reveal differences in line with previous studies by us [42] and others [34, 35], this indicates that our undertaken measures have been sufficient. As the study is still on-going, we were not able to perform any comparisons of the interventions and their respective DNA methylation patterns on outcomes of allergy development. However, we made up for this drawback by comparing our findings to an independent allergy study, where we indeed could show enrichment of our DMCs. Another limitation in our analyses include the lack of validation at the mRNA or protein expression level.
In conclusion, we demonstrate that the combined prenatal treatment with L. reuteri and/or ω-3 fatty acids results in general differential hypermethylation in neonatal CD4+ T cells, which affects both T cell-specific and immune-related pathways. This was corroborated by network analyses that condensed the findings to differentially methylated genes in linked pathways, which also showed relevance in an independent cohort of allergic disease. Future follow-ups on allergic disease and studies on transcriptional activity will confirm the long-term relevance of the presented findings, which may have an impact on future development of allergy prevention regimens.
Methods
Study participants
In this interim study, a subgroup of cord blood samples collected at the time of birth were included for 63 children from the on-going randomised double blind placebo-controlled trial PROOM-3 (ClinicalTrials.gov-ID: NCT01542970), in which the allergy preventive effects of combined pre- and postnatal Lactobacillus reuteri and ω-3 fatty acid supplementation are investigated. The study is four-armed comprising the following groups; double active treatment (Lω, L. reuteri and ω-3 fatty acids), single active treatments (placebo for either treatment, active treatment for either L. reuteri (LP) or ω-3 (Pω)) and double placebo treatment (PP). In the present study, the following numbers of samples were available per group: Lω = 18, LP = 16, Pω = 15, PP = 14. The mothers are supplemented with the probiotic intervention or the corresponding placebo supplement from GW 20 until delivery, whereas the children receive the same treatment throughout the first year of life. The active probiotic substance consists of L. reuteri (BioGaia®, Stockholm, Sweden) suspended in sun flower and palm kernel oil, which is given as droplets twice daily to the mothers (109 CFU) and once daily to the children (108 CFU). Placebo treatment for the probiotic intervention consists of the same oil mixture as above without probiotics. The ω-3 fatty acid intervention or corresponding placebo supplement are given from GW 20 throughout lactation to the mothers. Twice daily, the mothers ingest either three capsules of Pikasol® (Orkla Health, Lund, Sweden, 1 g capsules containing 640 mg ω-3 PUFA, 35% EPA, 25% DHA) or the placebo supplement olive oil. The children are followed-up at several occasions using questionnaires and by performance of clinical examinations. The primary endpoint of the study was IgE-associated disease at two years of age. To detect a 50% decrease in the cumulative incidence of any IgE-associated disease (35%) with 80% power and 5% probability, an estimate of 99 children per group was calculated. Counting with about 20% drop-off rates, this rendered for all the four arms of the study a total of 495 children, resulting in about 124 children per group. As the study still is ongoing, only parent reported questionnaire data from the 3-month follow-up were included for the purpose of this study. Parents or legal guardians provided informed consent on behalf of the children prior to inclusion in the study. Ethical permission for this study has been granted by the Regional Ethics Committee for Human Research in Linköping (Dnr 2011/45–31).
Cord blood mononuclear cell and CD4+ magnetic bead isolation
The isolation of cord blood mononuclear cells (CBMCs) from cord blood and the following magnetic bead isolation of CD4+ T cells from the CBMCs have been described in detail elsewhere [42].
Flow cytometry measurements of naïve and memory T cell proportions
In order to determine the proportion of naïve and memory cells from the isolated CD4+ cells 0.2 × 106 cells were stained for flow cytometry. Firstly, in order to determine the amount of live and dead cells in each sample Aqua LIVE/DEAD™ Fixable Dead Cell Stain (Invitrogen, Eugene, OR, USA) reconstituted reagent (according to manufacturer’s protocol) was diluted 1:500 in PBS (Medicago AB, Uppsala, Sweden) + 0.1% FCS (Sigma-Aldrich, Ayrshire, United Kingdom) and added to the samples for 15 min at RT. Thereafter, the cells were further stained with CD4 PerCP (SK3) and CD45RA FITC (L48), with a complementary isotype tube including CD4 PerCP and Mouse γ1 FITC (X40) (all antibodies: Becton–Dickinson, San José, CA, USA) for 15 min at 4 °C. After washing the cells, they were resuspended as described previously [42] and 10 000 events were collected on a FACS Canto II instrument using the FACS Diva software (version 8.0.1). The flow cytometry data were analysed using Kaluza (version 2.1, Beckman Coulter, Indianapolis, IN, USA), and the utilised gating strategy is presented in Additional file 3: Fig. S7.
DNA extraction
From the remaining CD4+ cells, DNA was extracted using Allprep RNA/DNA Mini Kit (Qiagen, Austin, TX, USA) according to the manufacturer’s instructions. DNA concentrations were measured using Qubit dsDNA BR Assay Kit (Thermo Fischer Scientific, Waltham, MA, USA) according to the manufacturer’s instructions on a Qubit 3.0 fluorometer device (Thermo Fischer Scientific, Waltham, MA, USA). DNA samples were sent to the SNP&SEQ-technology platform at SciLifeLab (Uppsala University, Uppsala, Sweden) for the performance of Illumina’s Infinium Human MethylationEPIC 850K bead chip array preceded by bisulphite conversion on site. The amount of DNA for each sample ranged from 1000–1800 ng.
Statistics
As the study is still on-going, the study has not yet been unblinded. An independent statistician has provided the code key only to collaborators that have not been involved in sample collection or laboratory experiments, as not to bias the investigators in interpretation of the data.
Descriptive analyses of demographic variables were performed. Continuous variables were tested for normality using the Shapiro–Wilk test of normality followed by Levene’s test of equal variances. Thereafter the Kruskal–Wallis H test was performed to study differences in proportions between the groups. For the categorical variables, the Pearson χ2 test was performed.
DNA methylation analyses
The scripts used to generate the below described analyses have been made available on GitLab (https://gitlab.com/davma27/proom3_project). The generated raw data from the Illumina 850K MethylationEPIC arrays were processed in GenomeStudio (version 2011.1, Illumina Inc.) by the SNP&SEQ-technology platform, to render IDAT-files manageable for downstream analyses in the R programming environment (version 3.6.3).
Pre-processing and quality control
The raw DNA methylation data were pre-processed using the ChAMP [66] package (version 2.16.1) for the R programming environment. Probes with detection p values above 0.01 and multi-hit probes were filtered out, as were non-CpG probes and probes related to SNPs and NA-probes. Furthermore, as we found significantly more females in the single active ω-3 treated (Pω) group, and as X-inactivation in females skews the beta value distribution (Additional file 3: Fig. S8), probes located on the X and Y chromosomes were omitted from the data. After the filtration step, 738 451 CpGs of the initial 865 918 investigated CpGs in the Illumina MethylationEPIC 850K array remained. Thereafter, beta values were calculated for all probes, representing the mean methylation of each CpG site, and to adjust for the inherently different designs of the Illumina DNA methylation arrays, normalisation of the beta values was conducted using the beta mixture quantile (BMIQ) method [67]. In order to identify the most significant components of variation in the data, and correct for unwanted variation if found, singular value decomposition (SVD) analyses were performed on the filtered and normalised data, using the ChAMP package. Based on results from these analyses, corrections were made in the data for the technical factors array and slide (Additional file 3: Fig. S9). The quality of the data was examined prior to and after the normalisation step (Additional file 3: Fig. S10). To ascertain possible differences in cellular content of the included samples, several methods were used to validate the findings. Maternal contamination of the cord blood samples was examined on the unfiltered data using the method proposed by Morin et al. [68]. By surveying threshold DNA methylation levels of 10 specified CpG sites, samples with values above the threshold values at five or more sites indicate contamination and should be excluded. Six samples had a beta value above the threshold value at one CpG site and one sample had beta values above the threshold values at two CpG sites (data not shown), indicating no maternal contamination and hence all 63 samples were retained in further downstream analyses. The cell type composition of the samples was evaluated on filtered and normalised samples using the Houseman method [69]. The majority of cells were CD4+ cells with median proportions in the intervention groups between 94–96% (Additional file 3: Table S11), indicating high sample purity and successful isolation of CD4+ T cells. The filtered, normalised and batch-corrected DNA methylation data are publicly available at ArrayExpress (ID: E-MTAB-10341). Multidimensional scaling (MDS) analyses were performed on the filtered, normalised and batch corrected data to study inherent differences in the data, using the R package minfi (version 1.32.0). Results of the SVD analyses using the ChAMP package showed that, apart from the sample array and slide, sex was a major source of unwanted variation in the normalised data. Therefore, sex was added as a co-variate in the batch correction step for the data used in the MDS analyses, using the ComBat function [70] from the sva package [71] (version 3.34.0), implemented in ChAMP. Following the statistical analyses, the MDS results were graphically represented by assigning the samples to their respective intervention group belonging.
Differential DNA methylation analysis
Using the limma package (version 3.42.2), differentially methylated probes were identified by fitting the DNA methylation data to a linear model. As the proportion of males and females in the samples of at least one of the groups was skewed, sex was included as a co-variate in the model, as was the proportion of memory CD4+ T cells in order to account for possible differences in T cell subtypes. Moderated t-statistics, log2 Fold Change (logFC) and p values were computed for each investigated probe. The logFC values represents the average beta methylation difference (from hereon referred to as mean methylation difference, MMD) between the respective active intervention groups in relation to the double placebo (PP) group. p values were adjusted for multiple testing using the Benjamini–Hochberg procedure for False Discovery Rate (FDR) correction. Differentially methylated CpGs (DMCs) were defined as probes having an FDR-adjusted p value of less than 0.1 along with an MMD of > 5%. Volcano plots were constructed to graphically illustrate the distribution of the DMCs using the base R environment. Identification of genes of interest was conducted by mapping the DMCs to the genome, resulting in differentially methylated genes (DMG). The DMGs were defined as genes containing at least one DMC, where hypomethylation was defined as all DMCs being hypomethylated and vice versa for the hypermethylated DMGs. Genes containing both hypo- and hypermethylated sites were considered having a mixed methylation pattern. A total of three differential methylation comparisons were made between each of the treatment groups compared to the double placebo group. The quality of these comparisons was ascertained using several approaches. First of all, the genomic inflation rate was investigated for the t-statistics of each of the three comparisons described above, as the large number of statistical comparisons made within each analysis may render a considerable number of false positive results. The genomic inflation and pertaining bias were estimated and QQ-plots plotting the differential DNA methylation data against a normal distribution were constructed using the R package BACON [72] (version 1.14.0). The estimated inflation values for each of the three comparisons was very close to one in all cases, indicating that there was no substantial genomic inflation in the comparisons (Additional file 3: Fig. S11), and hence no correction was needed. Pathway enrichment analyses were performed on the identified DMCs from the differential DNA methylation analyses, using the clusterProfiler package (version 3.14.3) and the KEGG PATHWAY database (release 94 2020/04). An adjusted p value cut-off of 0.1 was chosen to narrow down the number of pathways.
Network analyses
To further study the biological relevance of the findings from the differential methylation analyses, the DMCs identified in the different comparisons described above were annotated to their corresponding gene symbols (DMGs) with the Illumina 850K platform annotation reference. A total of 93 deprecated unique gene terms from the platform reference were corrected to the most updated nomenclature using the org.Hs.eg.db R package (version 3.10.0). Thereafter, the DMGs were used as seeds to construct the inputs for the disease module identification pipeline with MODifieR [43] R package (version 0.1.3, available at https://gitlab.com/Gustafsson-lab/MODifieR). Four different module defining algorithms from the package were implemented (Clique SuM, DIAMOnD, MCODE and Module Discoverer), and default parameters for the methods were used in each case. High confidence human protein–protein interactions (PPI) were retrieved from the STRING database (version 11.0, confidence score > 0.7). The four MODifieR methods were run for each comparison, resulting in a set of gene lists corresponding to the identified modules. Non-biased consensus modules were created for each comparison, by extracting genes found by all four module inference methods. Network visualisation was conducted in Cytoscape (version 3.7.2). Pathway enrichment analyses were performed on the module specific genes as described above to elucidate the role of the different intervention combinations on the CD4+ T cells. Furthermore, to unravel subclusters within the modules, visual inspection of the networks along with pathway enrichment analyses in the clusterProfiler R package (version 3.14.3, KEGG database) were performed. Clusters with three or more nodes were included in these analyses. Pathway enrichment analyses were also performed for unique and shared genes within the networks. To illustrate overlaps between shared and unique genes in the comparisons, Venn diagrams were constructed using the VennDiagram R package (version 1.6.20). Furthermore, to illustrate how the common genes may differ in methylation status between the comparisons, river plots were constructed using the riverplot R package (version 0.6).
Comparisons of differential methylation and network results to publicly available allergy data set
As we were interested in the relevance of our findings to allergic disease, but do not yet have any data available on this from the children of the PROOM-3 study, we compared the findings of our study with publicly available data on allergic disease. The chosen data set was downloaded from Gene Expression Omnibus (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE50222) and consisted of Illumina 450 K data from CD4+ T cells from 8 adult patients vs. 8 controls with seasonal allergic rhinitis with samples from both within and out of season (in total 32 samples) [73]. The data were pre-processed by removing probes located on the sex chromosomes, and filtering was perfomed by removing probes having more than 20% NAs and imputing remaining NAs within retained probes using the KNN method (ChAMP, version 2.12.1). Thereafter, the data were normalised using the BMIQ method and SVD analyses followed (Additional file 3: Fig. S12) as described earlier, showing that no correction was needed. Subsequent differential DNA methylation analyses were performed using the limma package (version 3.42.2), and sex as well as season of sample taking (within or outside of pollen season) were added as co-variates in the linear models. Upon this, a total of 13,102 DMCs were found for the data set, which were then compared to DMCs from our differential DNA methylation analyses and DMCs extracted from the genes identified in the respective network modules. Enrichment of any DMCs in these comparisons was performed using the enrichment function from the R package bc3net (version 1.0.4), based on a one-sided Fisher’s exact test. As the data set originated from 450 K data, the intersection of all 450 K probes and all MethylationEPIC 850K probes excluding the sex chromosomes was used as background for the analysis, and only DMCs that were present in the background were included. Corresponding pathway enrichment analyses for genes overlapping between any of the differentially methylated DMCs or consensus module originating DMCs with the allergy data set were performed as described above.
Supplementary Information
Additional file 1. Table S1. Table of extracted differentially methylated CpGs (DMCs) with corresponding mean methylation difference (MMD) from the three treatment comparisons (Lω, LP and Pω vs. PP, respectively). DMCs were defined as having a MMD of > ±5% along with an FDR-corrected p-value of <0.1. L – Lactobacillus reuteri, ω – ω-3 fatty acids, P – placebo.
Additional file 2. Table S2. Table of differentially methylated genes (DMGs) with corresponding direction of methylation from the three treatment comparisons (Lω, LP and Pω). DMGs were defined as genes with at least one DMC, and the direction of methylation depended on the direction of methylation for all DMCs in the gene. Hypomethylation is defined as > -5% mean methylation difference (MMD), hypermethylation as > +5% MMD and mixed methylation genes contained DMCs of both directions. L – Lactobacillus reuteri, ω – ω-3 fatty acids, P – placebo.
Additional file 3. Supplementary Appendix, including Figures S1-S12, Tables S3, S6-S11. Tables S1-S2 and S4-S5 are supplied separately as Additional files 1-2 and 3-4, respectively.
Additional file 4. Table S4. Table of pathways obtained from pathway enrichment analyses on DMCs from the Lω vs. PP comparison. Analyses were conducted using clusterProfiler R package and the KEGG PATHWAY database. Pathways with an adjusted p-value of 0.1 or lower were considered significantly relevant.
Additional file 5. Table S5. Table of pathways obtained from pathway enrichment analyses on DMCs from the LP vs. PP comparison. Analyses were conducted using clusterProfiler R package and the KEGG PATHWAY database. Pathways with an adjusted p-value of 0.1 or lower were considered significantly relevant.
Acknowledgements
Firstly, we would like to thank the children and mothers included in this study for their participation, and the personnel at the Allergy Center, Linköping for professionally taking care of the families throughout the study period, as well as handling samples in preparation for laboratory work. Our warmest thanks go to our skilled laboratory technicians Camilla Janefjord and Anne-Marie Fornander, for their unfailing collection of samples from the PROOM-3 study. We would also like to thank Simon Söderholm for valuable input in the initial analyses of the DNA methylation data. Lastly, we would like to acknowledge BioGaia® AB and Orkla Health for sponsoring the dietary supplements used in this study, as well as the SNP&SEQ-technology platform at SciLifeLab Uppsala University for yet another constructive collaboration.
Abbreviations
- BMIQ
Beta mixture quantile
- CBMC
Cord blood mononuclear cell
- CFU
Colony forming unit
- CpG
Cytosine–phosphate–Guanine
- DMC
Differentially methylated CpG
- DMG
Differentially methylated gene
- FDR
False discovery rate
- GW
Gestational week
- L. reuteri
Lactobacillus reuteri
- LP
Single-treated L.reuteri + placebo group
- Lω
Double-treated L.reuteri + ω-3 group
- MDS
Multidimensional scaling
- MMD
Mean methylation difference
- PBMC
Peripheral blood mononuclear cell
- PP
Double placebo group
- PROOM-3
PRObiotics and OMega-3 study
- Pω
Single-treated ω-3 + placebo group
- SVD
Singular value decomposition
- ω-3
Omega-3 fatty acids
Authors' contributions
MCJ and KD designed the study. KD and LN were responsible for the clinical evaluation of the children. JH has taken part in the sample collection and performed the experimental work presented in this paper. JE provided expertise on flow cytometry analyses, and MG on the performance of the statistical and bioinformatic analyses. DME, EO and JH performed the statistical and bioinformatic analyses. JH presented the findings. All authors interpreted and discussed the results. JH drafted the manuscript. All authors read and approved the final manuscript.
Funding
Open access funding provided by Linköping University. This study was supported by grants from the Swedish Research Council (2016-01698 and 2019-00989); the Swedish Heart and Lung Foundation (20140321 and 20170365); the Cancer and Allergy Foundation and the Medical Research Council of Southeast Sweden (FORSS-666771 and FORSS-758981).
Availability of data and materials
The datasets used and/or analysed in the presented work are available on ArrayExpress (PROOM-3 cord blood data) ID: E-MTAB-10341, as well as at: Gene Expression Omnibus (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE50222, adult seasonal allergic rhinitis data set). The utilised scripts in the analyses have been made available in the GitLab platform: https://gitlab.com/davma27/proom3_project.
Declarations
Ethics approval and consent to participate
Parents or legal guardians provided informed consent on behalf of the children prior to inclusion in the study. Ethical permission for this study has been granted by the Regional Ethics Committee for Human Research in Linköping (Dnr 2011/45-31).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mika Gustafsson and Maria C. Jenmalm shared senior authorship
References
- 1.Blaser MJ. The theory of disappearing microbiota and the epidemics of chronic diseases. Nat Rev Immunol. 2017;17:461–463. doi: 10.1038/nri.2017.77. [DOI] [PubMed] [Google Scholar]
- 2.Lambrecht BN, Hammad H. The immunology of the allergy epidemic and the hygiene hypothesis. Nat Immunol. 2017;18:1076–1083. doi: 10.1038/ni.3829. [DOI] [PubMed] [Google Scholar]
- 3.Simon KA, Hollander GA, McMichael A. Evolution of the immune system in humans from infancy to old age. Proc Biol Sci. 2015;282:20143085. doi: 10.1098/rspb.2014.3085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gollwitzer ES, Marsland BJ. Impact of early-life exposures on immune maturation and susceptibility to disease. Trends Immunol. 2015;36:684–696. doi: 10.1016/j.it.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 5.Jenmalm MC. The mother-offspring dyad: microbial transmission, immune interactions and allergy development. J Intern Med. 2017;282:484–495. doi: 10.1111/joim.12652. [DOI] [PubMed] [Google Scholar]
- 6.Macpherson AJ, de Agüero MG, Ganal-Vonarburg SC. How nutrition and the maternal microbiota shape the neonatal immune system. Nat Rev Immunol. 2017;17:508–517. doi: 10.1038/nri.2017.58. [DOI] [PubMed] [Google Scholar]
- 7.Zhang X, Zhivaki D, Lo-Man R. Unique aspects of the perinatal immune system. Nat Rev Immunol. 2017;17:495–507. doi: 10.1038/nri.2017.54. [DOI] [PubMed] [Google Scholar]
- 8.Julia V, Macia L, Dombrowicz D. The impact of diet on asthma and allergic diseases. Nat Rev Immunol. 2015;15:308–322. doi: 10.1038/nri3830. [DOI] [PubMed] [Google Scholar]
- 9.Dzidic M, Boix-Amorós A, Selma-Royo M, Mira A, Collado M. Gut microbiota and mucosal immunity in the neonate. Med Sci (Basel, Switzerland) 2018;6:56. doi: 10.3390/medsci6030056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Renz H, Skevaki C. Early life microbial exposures and allergy risks: opportunities for prevention. Nat Rev Immunol. 2020;21(3):177–191. doi: 10.1038/s41577-020-00420-y. [DOI] [PubMed] [Google Scholar]
- 11.Miles EA, Calder PC. Can early omega-3 fatty acid exposure reduce risk of childhood allergic disease? Nutrients. 2017;9:784. doi: 10.3390/nu9070784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blasbalg TL, Hibbeln JR, Ramsden CE, Majchrzak SF, Rawlings RR. Changes in consumption of omega-3 and omega-6 fatty acids in the United States during the 20th century. Am J Clin Nutr. 2011;93:950–962. doi: 10.3945/ajcn.110.006643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Warstedt K, Duchén K. Increased linoleic acid/α-linolenic acid ratio in Swedish cord blood samples collected between 1985 and 2005. Eur J Nutr. 2012;52:659–665. doi: 10.1007/s00394-012-0369-6. [DOI] [PubMed] [Google Scholar]
- 14.Miyata J, Arita M. Role of omega-3 fatty acids and their metabolites in asthma and allergic diseases. Allergol Int. 2015;64:27–34. doi: 10.1016/j.alit.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Krauss-Etschmann S, Hartl D, Rzehak P, et al. Decreased cord blood IL-4, IL-13, and CCR4 and increased TGF-β levels after fish oil supplementation of pregnant women. J Allergy Clin Immunol. 2008;121:464–470. doi: 10.1016/j.jaci.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 16.Bisgaard H, Stokholm J, Chawes BL, et al. Fish oil-derived fatty acids in pregnancy and wheeze and asthma in offspring. N Engl J Med. 2016;375:2530–2539. doi: 10.1056/NEJMoa1503734. [DOI] [PubMed] [Google Scholar]
- 17.Furuhjelm C, Warstedt K, Larsson J, et al. Fish oil supplementation in pregnancy and lactation may decrease the risk of infant allergy. Acta Paediatr. 2009;98:1461–1467. doi: 10.1111/j.1651-2227.2009.01355.x. [DOI] [PubMed] [Google Scholar]
- 18.Furuhjelm C, Warstedt K, Fagerås M, et al. Allergic disease in infants up to 2 years of age in relation to plasma omega-3 fatty acids and maternal fish oil supplementation in pregnancy and lactation. Pediatr Allergy Immunol. 2011;22:505–514. doi: 10.1111/j.1399-3038.2010.01096.x. [DOI] [PubMed] [Google Scholar]
- 19.Stokholm J, Blaser MJ, Thorsen J, et al. Maturation of the gut microbiome and risk of asthma in childhood. Nat Commun. 2018;9:141. doi: 10.1038/s41467-017-02573-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bisgaard H, Li N, Bonnelykke K, et al. Reduced diversity of the intestinal microbiota during infancy is associated with increased risk of allergic disease at school age. J Allergy Clin Immunol. 2011;128:646–652. doi: 10.1016/j.jaci.2011.04.060. [DOI] [PubMed] [Google Scholar]
- 21.Sjögren YM, Jenmalm MC, Böttcher MF, Björkstén B, Sverremark-Ekström E. Altered early infant gut microbiota in children developing allergy up to 5 years of age. Clin Exp Allergy. 2009;39:518–526. doi: 10.1111/j.1365-2222.2008.03156.x. [DOI] [PubMed] [Google Scholar]
- 22.Chiu C-Y, Chan Y-L, Tsai M-H, Wang C-J, Chiang M-H, Chiu C-C. Gut microbial dysbiosis is associated with allergen-specific IgE responses in young children with airway allergies. World Allergy Org J. 2019;12:100021. doi: 10.1016/j.waojou.2019.100021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ling Z, Li Z, Liu X, et al. Altered fecal microbiota composition associated with food allergy in infants. Appl Environ Microbiol. 2014;80:2546–2554. doi: 10.1128/AEM.00003-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abrahamsson TR, Jakobsson HE, Andersson AF, Björkstén B, Engstrand L, Jenmalm MC. Low diversity of the gut microbiota in infants with atopic eczema. J Allergy Clin Immunol. 2012;129:434. doi: 10.1016/j.jaci.2011.10.025. [DOI] [PubMed] [Google Scholar]
- 25.Cuello-Garcia CA, Brozek JL, Fiocchi A, et al. Probiotics for the prevention of allergy: A systematic review and meta-analysis of randomized controlled trials. J Allergy Clin Immunol; 136. [DOI] [PubMed]
- 26.Wells JM. Immunomodulatory mechanisms of lactobacilli. Microb Cell Fact. 2011;10(Suppl 1):S17. doi: 10.1186/1475-2859-10-S1-S17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abrahamsson TR, Sandberg Abelius M, Forsberg A, Björkstén B, Jenmalm MC. A Th1/Th2-associated chemokine imbalance during infancy in children developing eczema, wheeze and sensitization. Clin Exp Allergy. 2011;41:1729–1739. doi: 10.1111/j.1365-2222.2011.03827.x. [DOI] [PubMed] [Google Scholar]
- 28.Alhamwe B, Alhamdan F, Ruhl A, Potaczek DP, Renz H. The role of epigenetics in allergy and asthma development. Curr Opin Allergy Clin Immunol. 2020;20:48–55. doi: 10.1097/ACI.0000000000000598. [DOI] [PubMed] [Google Scholar]
- 29.Baribault C, Ehrlich KC, Ponnaluri VKCKC, Pradhan S, Lacey M, Ehrlich M. Developmentally linked human DNA hypermethylation is associated with down-modulation, repression, and upregulation of transcription. Epigenetics. 2018;13:275–289. doi: 10.1080/15592294.2018.1445900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baubec T, Schübeler D. Genomic patterns and context specific interpretation of DNA methylation. Curr Opin Genet Dev. 2014;25:85–92. doi: 10.1016/j.gde.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 31.Schmidl C, Delacher M, Huehn J, Feuerer M. Epigenetic mechanisms regulating T-cell responses. J Allergy Clin Immunol. 2018;142:728–743. doi: 10.1016/j.jaci.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 32.Zhang H, Kaushal A, Merid S, et al. DNA methylation and allergic sensitizations, a genome-scale longitudinal study during adolescence. Allergy. 2019;74:1166–1175. doi: 10.1111/all.13746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peng C, Meel ER, Cardenas A, et al. Epigenome-wide association study reveals methylation pathways associated with childhood allergic sensitization. Epigenetics. 2019;14(5):445–466. doi: 10.1080/15592294.2019.1590085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.DeVries A, Wlasiuk G, Miller SJ, et al. Epigenome-wide analysis links SMAD3 methylation at birth to asthma in children of asthmatic mothers. J Allergy Clin Immunol. 2017;140:534–542. doi: 10.1016/j.jaci.2016.10.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lund RJ, Osmala M, Malonzo M, et al. Atopic asthma after rhinovirus-induced wheezing is associated with DNA methylation change in the SMAD3 gene promoter. Allergy. 2018;73:1735–1740. doi: 10.1111/all.13473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martino D, Dang T, Sexton-Oates A, et al. Blood DNA methylation biomarkers predict clinical reactivity in food-sensitized infants. J Allergy Clin Immunol. 2015;135:1319–1328. doi: 10.1016/j.jaci.2014.12.1933. [DOI] [PubMed] [Google Scholar]
- 37.Martino D, Neeland M, Dang T, et al. Epigenetic dysregulation of naive CD4+ T-cell activation genes in childhood food allergy. Nat Commun. 2018;9:3308. doi: 10.1038/s41467-018-05608-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Harb H, Irvine J, Amarasekera M, et al. The role of PKCζ in cord blood T-cell maturation towards Th1 cytokine profile and its epigenetic regulation by fish oil. Biosci Rep. 2017;37. [DOI] [PMC free article] [PubMed]
- 39.Amarasekera M, Noakes P, Strickland D, Saffery R, Martino DJ, Prescott SL. Epigenome-wide analysis of neonatal CD4(+) T-cell DNA methylation sites potentially affected by maternal fish oil supplementation. Epigenetics. 2014;9:1570–1576. doi: 10.4161/15592294.2014.983366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Dijk SJ, Zhou J, Peters TJ, et al. Effect of prenatal DHA supplementation on the infant epigenome: results from a randomized controlled trial. Clin Epigenetics. 2016;8:114. doi: 10.1186/s13148-016-0281-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vähämiko S, Laiho A, Lund R, Isolauri E, Salminen S, Laitinen K. The impact of probiotic supplementation during pregnancy on DNA methylation of obesity-related genes in mothers and their children. Eur J Nutr. 2018:1–11. [DOI] [PubMed]
- 42.Forsberg A, Huoman J, Söderholm S, et al. Pre- and postnatal Lactobacillus reuteri treatment alters DNA methylation of infant T helper cells. Pediatric Allergy Immunol. 2020;31(5):544–553. doi: 10.1111/pai.13240. [DOI] [PubMed] [Google Scholar]
- 43.de Weerd HA, Badam TVS, Martínez-Enguita D, et al. MODifieR: an ensemble R package for inference of disease modules from transcriptomics networks. Bioinformatics (Oxford, England) 2020;36:3918–3919. doi: 10.1093/bioinformatics/btaa235. [DOI] [PubMed] [Google Scholar]
- 44.D’Aquila P, Carelli L, Rango F, Passarino G, Bellizzi D. Gut microbiota as important mediator between diet and DNA methylation and histone modifications in the host. Nutrients. 2020;12:597. doi: 10.3390/nu12030597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ceccarelli V, Ronchetti S, Marchetti M, et al. Molecular mechanisms underlying eicosapentaenoic acid inhibition of HDAC1 and DNMT expression and activity in carcinoma cells. Biochim Biophys Acta. 2020;1863:194481. doi: 10.1016/j.bbagrm.2020.194481. [DOI] [PubMed] [Google Scholar]
- 46.González-Becerra K, Ramos-Lopez O, Barrón-Cabrera E, et al. Fatty acids, epigenetic mechanisms and chronic diseases: a systematic review. Lipids Health Dis. 2019;18:178. doi: 10.1186/s12944-019-1120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Salmond RJ, Filby A, Qureshi I, Caserta S, Zamoyska R. T-cell receptor proximal signaling via the Src-family kinases, Lck and Fyn, influences T-cell activation, differentiation, and tolerance. Immunol Rev. 2009;228:9–22. doi: 10.1111/j.1600-065X.2008.00745.x. [DOI] [PubMed] [Google Scholar]
- 48.Kaur S, Bansal Y, Kumar R, Bansal G. A panoramic review of IL-6: Structure, pathophysiological roles and inhibitors. Bioorgan Med Chem. 2020;28:115327. doi: 10.1016/j.bmc.2020.115327. [DOI] [PubMed] [Google Scholar]
- 49.Zhou X, Han X, Lyu S-C, et al. Targeted DNA methylation profiling reveals epigenetic signatures in peanut allergy. JCI Insight; 2021. [DOI] [PMC free article] [PubMed]
- 50.Baccarelli A, Rusconi F, Bollati V, et al. Nasal cell DNA methylation, inflammation, lung function and wheezing in children with asthma. Epigenomics. 2012;4:91–100. doi: 10.2217/epi.11.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bruyns E, Marie-Cardine A, Kirchgessner H, et al. T cell receptor (TCR) interacting molecule (TRIM), a novel disulfide-linked dimer associated with the TCR–CD3–ζ complex, recruits intracellular signaling proteins to the plasma membrane. J Exp Med. 1998;188:561–575. doi: 10.1084/jem.188.3.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kirchgessner H, Dietrich J, Scherer J, et al. The transmembrane adaptor protein trim regulates t cell receptor (Tcr) expression and Tcr-mediated signaling via an association with the Tcr ζ chain. J Exp Med. 2001;193:1269–1284. doi: 10.1084/jem.193.11.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mehta AK, Gracias DT, Croft M. TNF activity and T cells. Cytokine. 2018;101:14–18. doi: 10.1016/j.cyto.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yamada A, Arakaki R, Saito M, Kudo Y, Ishimaru N. Dual role of fas/fasl-mediated signal in peripheral immune tolerance. Front Immunol. 2017;8:403. doi: 10.3389/fimmu.2017.00403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Demmelmair H, Koletzko B. Importance of fatty acids in the perinatal period. World Rev Nutr Diet. 2015;112:31–47. doi: 10.1159/000365427. [DOI] [PubMed] [Google Scholar]
- 56.Navarro-Tapia E, Sebastiani G, Sailer S, et al. Probiotic supplementation during the perinatal and infant period: effects on gut dysbiosis and disease. Nutrients. 2020;12:2243. doi: 10.3390/nu12082243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Davis EC, Dinsmoor AM, Wang M, Donovan SM. Microbiome composition in pediatric populations from birth to adolescence: impact of diet and prebiotic and probiotic interventions. Dig Dis Sci. 2020;65:706–722. doi: 10.1007/s10620-020-06092-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Murphy R, Morgan XC, Wang XY, et al. Eczema-protective probiotic alters infant gut microbiome functional capacity but not composition: sub-sample analysis from a RCT. Beneficial Microbes. 2019;10:5–17. doi: 10.3920/BM2017.0191. [DOI] [PubMed] [Google Scholar]
- 59.Dotterud CK, Avershina E, Sekelja M, et al. Does maternal perinatal probiotic supplementation alter the intestinal microbiota of mother and child? J Pediatr Gastroenterol Nutr. 2015;61:200–207. doi: 10.1097/MPG.0000000000000781. [DOI] [PubMed] [Google Scholar]
- 60.Watson H, Mitra S, Croden FC, et al. A randomised trial of the effect of omega-3 polyunsaturated fatty acid supplements on the human intestinal microbiota. Gut. 2017;67:1974–1983. doi: 10.1136/gutjnl-2017-314968. [DOI] [PubMed] [Google Scholar]
- 61.Forsberg A, West CE, Prescott SL, Jenmalm MC. Pre- and probiotics for allergy prevention: time to revisit recommendations? Clin Exp Allergy. 2016;46:1506–1521. doi: 10.1111/cea.12838. [DOI] [PubMed] [Google Scholar]
- 62.Jenmalm MC, Duchén K. Timing of allergy-preventive and immunomodulatory dietary interventions - are prenatal, perinatal or postnatal strategies optimal? Clin Exp Allergy. 2013;43:273–278. doi: 10.1111/cea.12003. [DOI] [PubMed] [Google Scholar]
- 63.Abrahamsson TR, Jakobsson T, Böttcher MF, et al. Probiotics in prevention of IgE-associated eczema: a double-blind, randomized, placebo-controlled trial. J Allergy Clin Immunol. 2007;119:1174–1180. doi: 10.1016/j.jaci.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 64.Solomon O, MacIsaac J, Quach H, et al. Comparison of DNA methylation measured by Illumina 450K and EPIC BeadChips in blood of newborns and 14-year-old children. Epigenetics. 2018;13(6):655–664. doi: 10.1080/15592294.2018.1497386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Martino D, Maksimovic J, Joo JH, Prescott SL, Saffery R. Genome-scale profiling reveals a subset of genes regulated by DNA methylation that program somatic T-cell phenotypes in humans. Genes immunity. 2012;13(5):388–398. doi: 10.1038/gene.2012.7. [DOI] [PubMed] [Google Scholar]
- 66.Tian Y, Morris TJ, Webster AP, et al. ChAMP: updated methylation analysis pipeline for Illumina BeadChips. Bioinformatics (Oxford, England) 2017;33:3982–3984. doi: 10.1093/bioinformatics/btx513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Teschendorff AE, Marabita F, Lechner M, et al. A beta-mixture quantile normalization method for correcting probe design bias in Illumina Infinium 450 k DNA methylation data. Bioinformatics (Oxford, England) 2013;29:189–196. doi: 10.1093/bioinformatics/bts680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Morin AM, Gatev E, McEwen LM, et al. Maternal blood contamination of collected cord blood can be identified using DNA methylation at three CpGs. Clin Epigenetics. 2017;9:75. doi: 10.1186/s13148-017-0370-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Houseman EA, Accomando WP, Koestler DC, et al. DNA methylation arrays as surrogate measures of cell mixture distribution. BMC Bioinform. 2012;13:86. doi: 10.1186/1471-2105-13-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Johnson WE, Li C, Rabinovic A. Adjusting batch effects in microarray expression data using empirical Bayes methods. Biostatistics (Oxford, England) 2007;8:118–127. doi: 10.1093/biostatistics/kxj037. [DOI] [PubMed] [Google Scholar]
- 71.Leek JT, Johnson EW, Parker HS, Jaffe AE, Storey JD. The sva package for removing batch effects and other unwanted variation in high-throughput experiments. Bioinformatics. 2012;28:882–883. doi: 10.1093/bioinformatics/bts034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.van Iterson M, van Zwet EW, Consortium B, Heijmans BT. Controlling bias and inflation in epigenome- and transcriptome-wide association studies using the empirical null distribution. Genome Biol. 2017;18:19. doi: 10.1186/s13059-016-1131-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nestor CE, Barrenas F, Wang H, et al. DNA methylation changes separate allergic patients from healthy controls and may reflect altered CD4+ T-cell population structure. PLoS Genet. 2014;10:e1004059. doi: 10.1371/journal.pgen.1004059. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Table S1. Table of extracted differentially methylated CpGs (DMCs) with corresponding mean methylation difference (MMD) from the three treatment comparisons (Lω, LP and Pω vs. PP, respectively). DMCs were defined as having a MMD of > ±5% along with an FDR-corrected p-value of <0.1. L – Lactobacillus reuteri, ω – ω-3 fatty acids, P – placebo.
Additional file 2. Table S2. Table of differentially methylated genes (DMGs) with corresponding direction of methylation from the three treatment comparisons (Lω, LP and Pω). DMGs were defined as genes with at least one DMC, and the direction of methylation depended on the direction of methylation for all DMCs in the gene. Hypomethylation is defined as > -5% mean methylation difference (MMD), hypermethylation as > +5% MMD and mixed methylation genes contained DMCs of both directions. L – Lactobacillus reuteri, ω – ω-3 fatty acids, P – placebo.
Additional file 3. Supplementary Appendix, including Figures S1-S12, Tables S3, S6-S11. Tables S1-S2 and S4-S5 are supplied separately as Additional files 1-2 and 3-4, respectively.
Additional file 4. Table S4. Table of pathways obtained from pathway enrichment analyses on DMCs from the Lω vs. PP comparison. Analyses were conducted using clusterProfiler R package and the KEGG PATHWAY database. Pathways with an adjusted p-value of 0.1 or lower were considered significantly relevant.
Additional file 5. Table S5. Table of pathways obtained from pathway enrichment analyses on DMCs from the LP vs. PP comparison. Analyses were conducted using clusterProfiler R package and the KEGG PATHWAY database. Pathways with an adjusted p-value of 0.1 or lower were considered significantly relevant.
Data Availability Statement
The datasets used and/or analysed in the presented work are available on ArrayExpress (PROOM-3 cord blood data) ID: E-MTAB-10341, as well as at: Gene Expression Omnibus (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE50222, adult seasonal allergic rhinitis data set). The utilised scripts in the analyses have been made available in the GitLab platform: https://gitlab.com/davma27/proom3_project.