Abstract
Objective
A paucity of data exists regarding surgical outcomes for patients undergoing total laryngectomy for a dysfunctional larynx. Herein, we present the largest study evaluating the method of closure on postoperative fistula rate and swallowing ability.
Method
We performed a retrospective review of patients undergoing total laryngectomy for a dysfunctional larynx after primary radiation or chemoradiation therapy for laryngeal carcinoma from 1998 to 2020. Demographic information, operative details, length of hospitalization, fistula formation, method of fistula treatment, and need for enteral feeding 6 months after surgery were analyzed.
Results
A total of 268 patients were included. Flaps were performed in 140 (52.2%) patients, including radial forearm free flaps (RFFF), pectoralis flaps, and supraclavicular flaps. Sixty‐four (23.9%) patients developed postoperative fistulas. There was no significant difference in the fistula rate between flap and primary closure methods (P = .06). However, among patients who had a flap, RFFF had a significantly lower fistula rate (P = .02). Significantly more patients who had initial closure with a pectoralis flap required an additional flap for fistula repair than those who underwent RFFF or primary closure (P < .05). Last, whereas 87 patients (32.5%) required an enteral feeding tube 6 months after surgery, significantly fewer patients who underwent RFFF were feeding tube‐dependent (P = < .0001).
Conclusion
Herein, we present the largest study of outcomes after total laryngectomy for dysfunctional larynx. Postoperative fistula rates are high, 23%; however, the majority of patients, 67%, will not require long‐term enteral support. The RFFF is an excellent option demonstrating the lowest rates of postoperative fistula and enteral feeding tube dependence.
Level of Evidence
4 Laryngoscope, 131:E1510–E1513, 2021
Keywords: Nonfunctional larynx, total laryngectomy, regional flap reconstruction, free flap reconstruction
INTRODUCTION
Organ preservation has become the norm for treatment of laryngeal cancer in the wake of the Department of Veterans Affairs and the Radiation Therapy Oncology Group trials. 1 , 2 Although the efficacy of this strategy is well established, laryngeal function is not always preserved. The sequelae of radiation and chemoradiation may be sufficiently severe to warrant total laryngectomy in cases of aspiration with recurrent pneumonia, bleeding from persistent ulceration, debilitating dyspnea, and radionecrosis. 3 , 4 Patients undergoing total laryngectomy for a dysfunctional larynx secondary to radiation with or without chemotherapy who have no evidence of recurrent or persistent malignancy constitute a relatively rare population. 4
Prior literature has established that previous radiation or chemoradiation increases the complication rate—most commonly pharyngocutaneous fistula formation—for salvage total laryngectomy. 5 , 6 , 7 , 8 Closure reinforced with nonirradiated tissue provided by a pedicled or free flap is advocated in favor of primary closure alone in order to mitigate the risk of postoperative fistula, 7 although no consensus exists as to which type of closure achieves the lowest complication rate. 6 , 9 Whereas these outcomes have been explored for patients undergoing salvage total laryngectomy, a paucity of data exists regarding similar outcomes for disease‐free patients undergoing total laryngectomy for a dysfunctional larynx secondary to radiation or chemoradiation. 3 , 4
Herein, we present the largest study on outcomes after total laryngectomy for dysfunctional larynx in disease‐free patients treated with prior radiation or chemoradiation, specifically evaluating the effect that method of closure has on mitigating the rate of postoperative fistulas and enteral feeding‐tube dependence.
MATERIALS AND METHODS
We performed a a single‐center retrospective review of laryngectomies performed between February 1998 and February 2020 by the senior author (y.d.). Approval for our study was granted by the John Peter Smith Institutional Review Board, Fort Worth, Texas. Patients undergoing total laryngectomy for a dysfunctional larynx after primary radiation therapy with or without chemotherapy for laryngeal carcinoma were included. Patients who underwent primary total laryngectomy or salvage total laryngectomy for recurrent or persistent disease were excluded. Also excluded were patients who underwent total laryngectomy for a nonfunctional larynx who had not had previous radiation therapy or chemotherapy.
Demographic information and operative details were collected by review of the medical record as well as length of hospitalization, fistula formation, method to treat fistula, and need for enteral feeding 6 months after surgery.
In our practice, a thyroid‐stimulating hormone (TSH) level is checked in each patient before surgery. If hypothyroid, then patients receive oral or intravenous hormone repletion to become euthyroid for surgery. In the operating room, we always perform primary closure if it is possible, that is, if there is sufficient remaining tissue after laryngectomy. If there is not enough tissue to allow primary closure, then a flap is chosen. If the patient is a suitable free flap candidate and has good vessels in the neck for anastomosis, then our preference is to perform a radial forearm free flap. If the patient has comorbid conditions that make the patient a poor candidate for free flap transfer (i.e.; requires intraoperative pressors, has a vessel‐deplete neck, has a clotting disorder), then a supraclavicular flap is raised for pharyngeal reconstruction. If the supraclavicular flap vessels have been compromised by previous surgery or radiation, then our last option is a pectoralis flap.
Statistical Methods
Analysis of variance was used to compare mean lengths of hospital stay. Associations between categorical variables were determined using Pearson chi‐square test. Fisher exact test was used for comparison between two groups when any subgroup had fewer than 10 patients. Statistical tests were conducted using version 23 of SPSS Statistics (IBM Corp., Armonk, N.Y.) with P < .05 as the threshold for significance.
RESULTS
Patient Characteristics
A total of 268 patients underwent total laryngectomy for a dysfunctional larynx. Men comprised the majority of patients (201, 75%). Mean ages for the male and female groups were 70.2 (54–85) and 71.4 (61–87), respectively. One hundred sixty‐three patients had stage 4 disease; 55 had stage 3; 46 had stage 2; and four had stage 1. None of the patients in this study were obese. All patients had a TSH level checked preoperatively. Patients who were found to be hypothyroid underwent oral or intravenous thyroid hormone repletion until they were euthyroid, and all patients were euthyroid at the time of surgery. Eighty‐two patients (30.6%) had undergone radiation therapy alone, whereas 186 (69.4%) patients had undergone chemoradiation. The preoperative feeding‐tube dependence rate was 100%; all patients had a nonfunctional larynx and were actively aspirating.
Type of Closure
Locoregional and free flaps were used for closure of the laryngectomy defect in 140 (52.2%) patients, including 68 radial forearm free flaps, 54 pectoralis major flaps, and 18 supraclavicular flaps. Primary closure was performed in 128 (47.8%) cases. Primary closure was performed in a higher percentage of radiation‐only patients (58 of 82, 70.7%) compared to chemoradiation patients (70 of 186, 37.6%). A higher percentage of chemoradiation patients underwent pectoralis flaps and supraclavicular flaps compared to radiation patients (26.3% vs. 6.1%; 9.1% vs. 1.2%). Radial forearm free flap closure was evenly distributed among the radiation (21.9%) and chemoradiation (26.9%) groups.
Length of Stay
The mean length of postoperative hospital stay for all patients was 12.4 days (7–41). The mean length of stay according to type of closure was 9.8 days for radial forearm free flaps, 13.5 for pectoralis flaps, 12.5 for supraclavicular flaps, and 11.1 for primary closure. Patients undergoing pectoralis flaps had significantly longer hospital stays compared to radial forearm flap (P = .0002) and primary closure patients (P = .0115). The difference in length of hospital stay among the remaining groups was not significant.
Fistula Rate
Sixty‐four (23.9%) patients developed postoperative fistulas. Of these, 50 (78.1%) patients had undergone concurrent chemoradiation, and 14 (21.9%) had undergone radiation alone. However, the rates of fistula after chemoradiation (50 of 186, 26.9%) compared to radiation alone (14 of 82, 17.1%) were not significantly different (P = .083), suggesting that the larger number of fistulas after chemoradiation therapy was simply because more of those patients were included in our study population.
Fistulas occurred in 12 of 68 (17.7%) radial forearm patients, 21 of 54 (38.9%) pectoralis patients, seven of 18 (38.9%) supraclavicular flap patients, and 24 of 128 (18.8%) primary closure patients (Fig. 1). There was no significant difference in the fistula rate between patients who had any kind of flap compared to primary closure (P = .06). Significantly fewer fistulas developed in patients after radial forearm flap reconstruction than in patients with pectoralis or supraclavicular flap reconstruction (P = .02). When specifically comparing the rate of fistula between the radial forearm and primary closure groups, no significant difference was detected (P = .85).
Fig. 1.
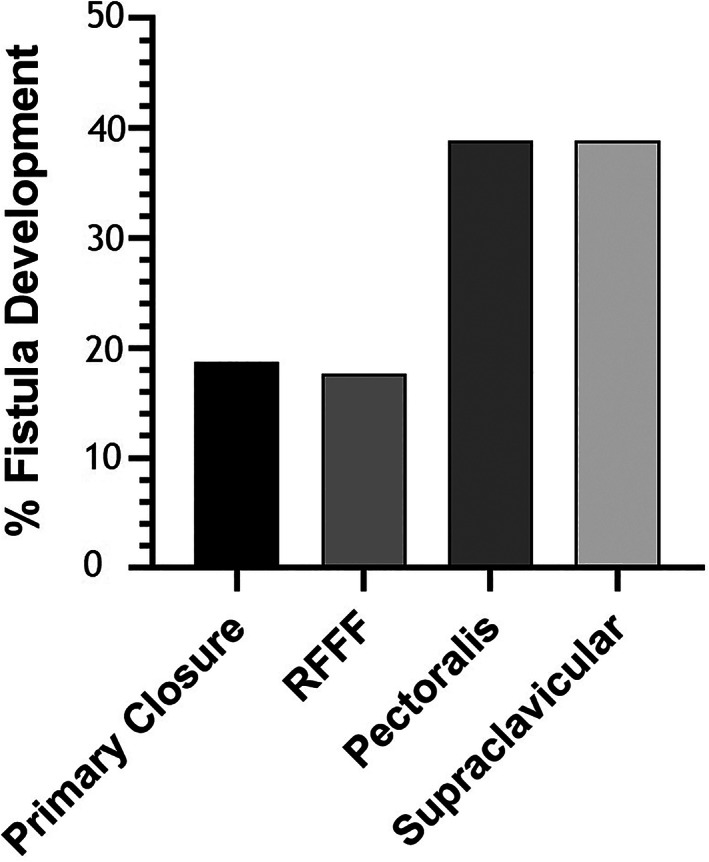
Rates of fistula development after different types of reconstruction. Significantly fewer fistulas developed in patients after RFFF reconstruction than in patients with pectoralis or supraclavicular flap reconstruction (P = .02). RFFF = radial forearm free flap.
Of the 12 patients in the radial forearm group who developed a fistula, four (33.3%) were treated conservatively with antibiotics and wound care and required no further intervention. In this group, fistulas resolved after a mean 18.2 days (range 11–28 days). Eight patients (66.7%) required additional surgery consisting of primary closure in six patients and flap augmentation in two patients with a pectoralis flap and a latissimus flap. The six patients who underwent additional primary closure required no further surgery, whereas the two patients in whom the pectoralis and latissimus flaps were performed required a third surgery without flap augmentation to address a repeat fistula in each.
Of the 21 patients in the pectoralis flap group who developed a fistula, five (23.8%) were treated conservatively without need for further surgery. In this group, fistulas resolved after a mean 21.5 days (range 14–32 days). Sixteen patients (76.2%) required additional surgery, which consisted of a second pectoralis flap in eight, radial forearm free flaps in six, and a latissimus flap in two. The six recurrent fistulas addressed with a radial forearm flap required no further intervention, whereas two addressed with a repeat pectoralis flap, and one with a latissimus flap required a third surgical intervention without further flap augmentation.
Four of the seven patients (57.1%) who developed fistulas in the supraclavicular flap group were treated conservatively without need for further intervention and experienced fistula resolution over a mean 12.5 days (range 7–21 days). Three (42.9%) patients underwent additional surgery: one with a pectoralis flap and two with a radial forearm flap. The patient who underwent the pectoralis flap required a third surgery for recurrent fistula, which did not involve flap augmentation.
Five of the 24 patients (20.8%) who developed fistulas in the primary closure group were treated conservatively, whereas 19 (79.2%) required further surgery. Of those successfully treated conservatively, fistulas resolved over an average of 14.5 days (range 11–23 days). Six fistulas were addressed with primary closure, five with a pectoralis flap, six with a radial forearm flap, one with a sternocleidomastoid flap, and one with a latissimus flap. Two of the patients who received pectoralis flap, as well as both patients repaired with the sternocleidomastoid and latissimus flaps, required a third surgery to address a recurrent fistula with primary closure.
There was no significant difference in the number of patients who required surgery for fistula repair based on initial method of closure (P = .27). More patients who had initial closure with a pectoralis flap required an additional flap for fistula repair than those who underwent initial closure with a radial forearm flap or primary closure (P < .05). There were no other differences among groups in terms of requiring additional flaps for fistula repair. No patient whose fistula was repaired using a radial forearm flap required a third surgery.
Swallowing Outcomes
Eighty‐seven of 268 patients (32.5%) required an enteral feeding tube for nutritional support 6 months after total laryngectomy. Five (7.4%) of these patients had undergone closure with a radial forearm flap, 23 (42.6%) with a pectoralis flap, seven (38.9%) with a supraclavicular flap, and 52 (40.6%) with primary closure. A significantly smaller percentage of radial forearm patients required a feeding tube 6 months postoperatively compared to those undergoing the other methods of closure (P < .0001) (Fig. 2). There were no significant differences among the other types of closure regarding this outcome.
Fig. 2.
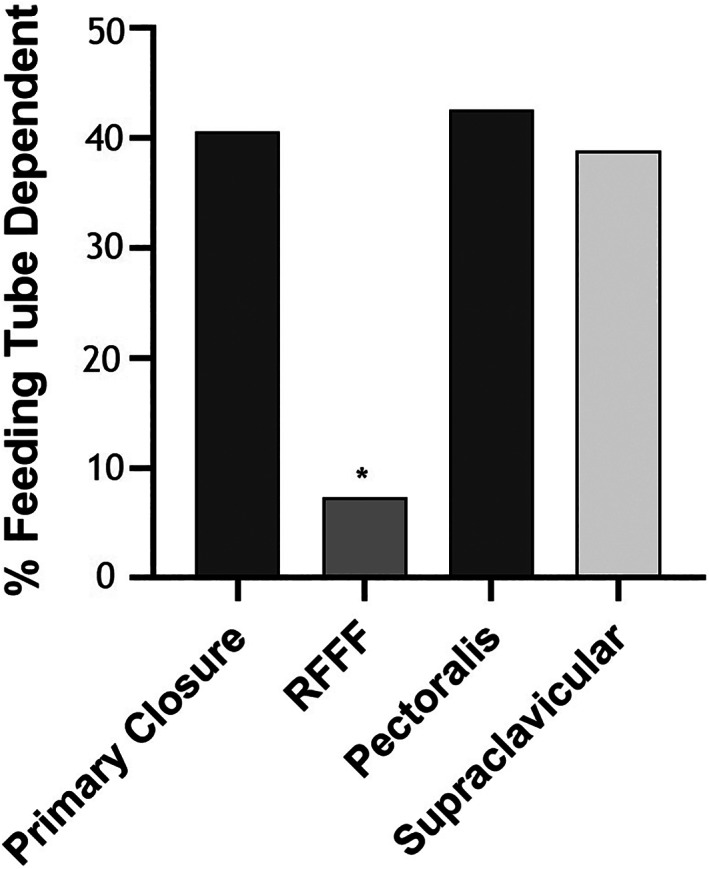
Rates of feeding‐tube dependency 6 months after surgery. Patients who underwent RFFF reconstruction had significantly lower rates of feeding tube dependency than other methods of closure (P < .001). RFFF = radial forearm free flap.
DISCUSSION
Total laryngectomy is frequently performed for recurrent or persistent disease after failure of organ‐preservation therapy. However, a relatively rare population of disease‐free patients undergo total laryngectomy for a larynx rendered nonfunctional by radiation with or without chemotherapy. This population represented 11% of patients undergoing total laryngectomy over 10 years in a recent study. 3
A consequence of the emphasis on organ preservation strategies for laryngeal malignancy is that surgeons may later be operating in a previously irradiated field with very poor tissue quality and a high risk of wound complications or fistula formation. 5 , 6 , 7 , 8 , 10 When total laryngectomy is performed in the salvage setting, closure with either a pedicled flap or a free flap is often performed with the intent of introducing healthy, well‐vascularized, nonradiated tissue to mitigate the risk of fistula formation. It is not clear from prior studies, however, whether one type of flap is superior to another in this regard. 6 , 9 In the present study, closure with a radial forearm free flap resulted in a decreased incidence of postoperative fistula formation compared to pectoralis (38.9%) or supraclavicular flaps. In contrast, a recent smaller study reported no difference in number of fistulas according to primary closure, closure with a pectoralis flap, or closure with free tissue transfer in patients undergoing total laryngectomy for dysfunctional larynx after organ preservation therapy. 3 On the other hand, a recent meta‐analysis demonstrated a reduced fistula incidence in salvage total laryngectomy patients when a flap was used rather than primary closure. 7 A greater percentage of patients undergoing primary closure in the present study had received radiation without chemotherapy. Therefore, primary closure was performed in many patients who may have been less prone to fistula formation preoperatively, which may account for the lack of a significant difference in fistulas between patients who underwent primary closure and those who underwent flap closure.
One‐third of patients in this study were dependent on an enteral feeding tube for nutrition 6 months after surgery, and significantly fewer patients who underwent radial forearm free‐flap closure were feeding tube‐dependent than those who underwent other methods of closure. These results are consistent with a recent study by Farlow et al., which found that 31% of patients undergoing total laryngectomy for the dysfunctional irradiated larynx required at least partial enteral tube feeding 1 year after surgery. 11 Farlow's study also demonstrated an association between reconstructive type and postoperative swallowing outcome, with free tissue transfer outperforming locoregional flaps. A similar publication investigating outcomes after total laryngectomy for dysfunctional larynx in disease‐free head and neck cancer survivors reported satisfactory swallowing outcomes at a median follow‐up of 28 months, with 83% of patients achieving feeding tube removal and 74% maintaining nutrition orally without enteral support. However, method of reconstruction was not significantly associated with feeding tube dependence. 4 Taken as a whole, the results suggest that most patients undergoing total laryngectomy for dysfunctional larynx after organ preservation therapy will not require a feeding tube. The thin, pliable nature of a radial forearm free flap compared to the bulk of a pectoralis flap likely accounts for improved swallowing outcomes observed in the radial forearm cohort.
Although this study sheds some light on a very specific and seldom described population, it has several limitations. First, this is a retrospective series. There are several useful data that were unable to be collected, such as the exact indication for total laryngectomy, the time between last radiation/chemotherapy and surgery, swallowing status prior to surgery, and complications apart from fistula formation. Also, the full spectrum of patient comorbidities could not be analyzed. Obesity, cardiovascular disease, hypothyroidism, and other conditions can also influence wound healing and fistula development. In our study, patients were made euthyroid before surgery, and none happened to be obese. Other conditions could not be controlled for, however. Furthermore, a comparison with a salvage total laryngectomy cohort would be valuable, and future studies could provide this data.
CONCLUSION
Herein, we describe the largest cohort of patients undergoing total laryngectomy for dysfunctional larynx after organ preservation therapy without evidence of disease. Our study confirms that the incidence of postoperative fistula is high in this population and that the majority of patients will not require long‐term enteral support after surgery. When a flap is used for reconstruction, the radial forearm free flap is an excellent option for this population because it demonstrates the lowest rate of postoperative fistula compared to locoregional flaps as well as the lowest rate of enteral feeding tube dependence among all types of closure. The radial forearm flap has furthermore demonstrated reliability for repairing postoperative fistulas. The rate of fistula formation did not differ significantly between patients reconstructed with flaps and those undergoing primary closure alone, suggesting that primary closure may be appropriate in some cases while reserving flaps as future contingency options.
Editor's Note: This Manuscript was accepted for publication on September 16, 2020.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
BIBLIOGRAPHY
- 1. Wolf GT, Fisher SG, Hong WK, et al. Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer. N Engl J Med 1991;324:1685–1690. [DOI] [PubMed] [Google Scholar]
- 2. Weber RS, Berkey BA, Forastiere A, et al. Outcome of salvage total laryngectomy following organ preservation therapy: the Radiation Therapy Oncology Group trial 91‐11. Arch Otolaryngol Head Neck Surg 2003;129:44–49. [DOI] [PubMed] [Google Scholar]
- 3. Theunissen EA, Timmermans AJ, Zuur CL, et al. Total laryngectomy for a dysfunctional larynx after (chemo)radiotherapy. Arch Otolaryngol Head Neck Surg 2012;138:548–555. [DOI] [PubMed] [Google Scholar]
- 4. Hutcheson KA, Alvarez CP, Barringer DA, Kupferman ME, Lapine PR, Lewin JS. Outcomes of elective total laryngectomy for laryngopharyngeal dysfunction in disease‐free head and neck cancer survivors. Otolaryngol Head Neck Surg 2012;146:585–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Busoni M, Deganello A, Gallo O. Pharyngocutaneous fistula following total laryngectomy: analysis of risk factors, prognosis and treatment modalities. Acta Otorhinolaryngol Italica 2015;35:400–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Patel UA, Moore BA, Wax M, et al. Impact of pharyngeal closure technique on fistula after salvage laryngectomy. JAMA Otolaryngol Head Neck Surg 2013;139:1156–1162. [DOI] [PubMed] [Google Scholar]
- 7. Sayles M, Grant DG. Preventing pharyngo‐cutaneous fistula in total laryngectomy: a systematic review and meta‐analysis. Laryngoscope 2014;124:1150–1163. [DOI] [PubMed] [Google Scholar]
- 8. Walton B, Vellucci J, Patel PB, Jennings K, McCammon S, Underbrink MP. Post‐laryngectomy stricture and pharyngocutaneous fistula: review of techniques in primary pharyngeal reconstruction in laryngectomy. Clin Otolaryngol 2018;43:109–116. [DOI] [PubMed] [Google Scholar]
- 9. Haidar YM, Kuan EC, Verma SP, Goddard JA, Armstrong WB, Tjoa T. Free flap versus pedicled flap reconstruction of laryngopharyngeal defects: a 10‐year national surgical quality improvement program analysis. Laryngoscope 2019;129:105–112. [DOI] [PubMed] [Google Scholar]
- 10. White HN, Golden B, Sweeny L, Carroll WR, Magnuson JS, Rosenthal EL. Assessment and incidence of salivary leak following laryngectomy. Laryngoscope 2012;122:1796–1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Farlow JL, Birkeland AC, Hardenbergh A, et al. Speech and swallowing outcomes after laryngectomy for the dysfunctional irradiated larynx. Eur Arch Otorhinolaryngol 2020;277:1459–1465. [DOI] [PubMed] [Google Scholar]


