Abstract
OBJECTIVE
Diabetes is associated with poor oral health, but incremental expenditures for dental care associated with diabetes in the U.S. are unknown. We aimed to quantify these incremental expenditures per person and for the nation.
RESEARCH DESIGN AND METHODS
We analyzed data from 46,633 noninstitutionalized adults aged ≥18 years old who participated in the 2016–2017 Medical Expenditure Panel Survey. We used two-part models to estimate dental expenditures per person in total, by payment source, and by dental service type, controlling for sociodemographic characteristics, health status, and geographic variables. Incremental expenditure was the difference in predicted expenditure for dental care between adults with and without diabetes. The total expenditure for the U.S. was the expenditure per person multiplied by the estimated number of people with diabetes. Expenditures were adjusted to 2017 USD.
RESULTS
The mean adjusted annual diabetes-associated incremental dental expenditure was $77 per person and $1.9 billion for the nation. Of this incremental expenditure, 51% ($40) and 39% ($30) were paid out of pocket and by private insurance, 69% ($53) of the incremental expenditure was for restorative/prosthetic/surgical services, and adults with diabetes had lower expenditure for preventive services than those without (incremental, −$7). Incremental expenditures were higher in older adults, non-Hispanic Whites, and people with higher levels of income and education.
CONCLUSIONS
Diabetes is associated with higher dental expenditures. These results fill a gap in the estimates of total medical expenditures associated with diabetes in the U.S. and highlight the importance of preventive dental care among people with diabetes.
Introduction
People with diabetes tend to have poorer oral health than those without the disease (1,2), and persistent poor glycemic management is associated with an increased risk of periodontitis, gingivitis, and alveolar bone loss (1,3–5). Periodontal disease has been recognized as the sixth most common complication of diabetes (6), and the estimated risk of periodontitis among people with diabetes is three times that of those without (4). Other oral manifestations of diabetes include dental caries (i.e., cavities), severe tooth loss, salivary dysfunction, oral mucosal diseases, candidiasis, and taste and neurosensory disorders (2,7).
Higher risk of dental disease in people with diabetes may lead to higher medical expenditures. On the other hand, differences in socioeconomic status and demographic composition between those with and without diabetes may also lead to differences in the use of dental care services. Little information is available on how dental health services and expenditures differ by diabetes status. Previous studies (8,9) have found that people with diabetes were less likely to see a dentist and receive preventive dental services. Other factors associated with less use of preventive dental services include high out-of-pocket expenditures, inadequate oral health knowledge, and poor oral health attitudes (10–12). There have been no studies to date on incremental service use and expenditures associated with overall dental care among people with versus without diabetes in the U.S. As a result, national estimated total medical expenditures associated with diabetes have not included this expenditure component (13).
The objectives of this study were to 1) quantify annual dental expenditures associated with diabetes per person among noninstitutionalized adults in the U.S., in total, by type of dental service and by payment source; 2) examine disparities among population subgroups; and 3) estimate the total incremental expenditure for dental care associated with diabetes for the nation.
Research Design and Methods
Data and Study Population
Data used in this study were obtained from the Medical Expenditure Panel Survey (MEPS). MEPS is a set of surveys for families, individuals, medical providers, and employers aimed at providing nationally representative estimates of health care use and expenditure, payment sources, and health insurance coverage in the U.S. noninstitutionalized civilian population. MEPS has been used extensively for estimating medical expenditures associated with various diseases, including diabetes, hypertension, and cardiovascular disease (14,15). MEPS collects information on dental care, including visits, expenditures, payment sources, and services types.
For our analysis, we used the full-year consolidated data file and dental visits file for the 2016 and 2017 MEPS. Our study population included all adults aged ≥18 years who participated in the survey. Diabetes was identified by the survey question, “Other than during pregnancy, have you ever been told by a doctor or other health professional that you had diabetes or sugar diabetes?”
Estimation of Dental Expenditure
Total dental expenditure included spending associated with dental services from all providers including general dentists, dental hygienists, dental technicians, dental surgeons, orthodontists, endodontists, and periodontists. Payment sources were grouped into expenditures paid from out of pocket, private insurance, and public/other sources (e.g., Medicaid). Services types were grouped into three categories: preventive care (e.g., cleaning), restorative/prosthetic/surgical services (e.g., periodontal surgery), and diagnostic/other services (e.g., X-rays, multiple dental services per dental care visit).
Because ∼65% of the study participants did not have dental services during the survey year, we used two-part models, which are commonly used for analysis of health expenditure data that contain a large proportion of zero expenditure and that are highly skewed with some large expenditures (16). In the first part, we used a logit model to estimate the probability of an individual having had dental expenditures. In the second part, among those who had dental expenditures, we used a generalized linear model with a log link and gamma distribution to estimate the amount of dental expenditure. The Box-Cox test was conducted to select the link function and a modified Park test was used to test the distribution family (16). Models controlled for age, sex, race/ethnicity, education level, marital status, family annual income level (as a percentage of the federal poverty level [FPL]), current smoking status, dental insurance coverage, other diseases (heart disease, stroke, diabetes-caused kidney damage, and eye problems), and Census region of residence. For insurance type, if a person had private dental insurance or had any dental expenses paid by private insurance, they were coded as having private dental coverage. Otherwise, if a person had public coverage or had any dental expenses paid by public insurance, they were coded as having public dental coverage (17). We combined estimates from the two parts of the model to predict dental expenditures for adults with and without diabetes. The incremental dental expenditure associated with diabetes was the difference between the predicted expenditures between the two groups.
We conducted several subgroup analyses to examine the disparity in dental expenditures among them including age (18–64 and ≥65 years), sex (male and female), race/ethnicity (Hispanic, non-Hispanic White, non-Hispanic Black, and other), income (<100%, 100–199%, 200–399%, and ≥400% of FPL) and education level (≤high school and >high school). We estimated the national expenditure for dental care associated with diabetes by multiplying per capita incremental dental expenditure by the national weighted number of adults with diabetes. The number of adults with diabetes was estimated from MEPS, which excludes institutionalized adults, women with gestational diabetes mellitus, and adults with undiagnosed diabetes.
All expenditures were adjusted to 2017 USD with use of the Personal Consumption Expenditure Health (PCE-Health) deflator (18). All analyses incorporated sampling weights and accounted for the complex survey design of MEPS. Data were analyzed with Stata (version 14). P values <0.05 were considered statistically significant.
Results
Of the 46,633 adults included in our analysis, 5,455 (11.7%) had diabetes. In comparison with adults without diabetes, a larger proportion of those with diabetes were older (aged ≥65 years, 44.0% vs. 17.9%), male (50.4% vs. 48.0%), and non-Hispanic Black (15.1% vs. 11.5%); had lower education level (≤high school, 19.0% vs. 12.7%); and had lower family annual income (≤199% of FPL, 36.5% vs. 25.9%) (Table 1). People with diabetes were more likely to have other diseases (46.3% vs. 13.8%) and were less likely to have dental insurance coverage (59.0% vs. 68.0%) than those without diabetes.
Table 1.
Characteristics of the study population by diabetes status
| Total population (n = 46,633; weighted n = 246,733,767) | With diabetes (n = 5,455; weighted n = 25,233,079)‖ | Without diabetes (n = 41,178; weighted n = 221,500,688) | P‡ | |
|---|---|---|---|---|
| Age, years | <0.0001 | |||
| ≤44 | 45.67 (0.51) | 11.32 (0.68) | 49.58 (0.54) | |
| 45–64 | 33.79 (0.39) | 44.73 (1.00) | 32.54 (0.41) | |
| ≥65 | 20.55 (0.40) | 43.95 (1.02) | 17.88 (0.41) | |
| Sex | 0.0142 | |||
| Male | 48.27 (0.27) | 50.40 (0.90) | 48.03 (0.29) | |
| Female | 51.73 (0.27) | 49.60 (0.90) | 51.97 (0.29) | |
| Race/ethnicity | <0.0001 | |||
| Hispanic | 16.04 (0.64) | 16.14 (0.96) | 16.03 (0.64) | |
| Non-Hispanic White | 63.19 (0.80) | 60.16 (1.24) | 63.53 (0.82) | |
| Non-Hispanic Black | 11.85 (0.51) | 15.14 (0.82) | 11.48 (0.50) | |
| Non-Hispanic other | 8.92 (0.43) | 8.57 (0.83) | 8.96 (0.42) | |
| Education level | <0.0001 | |||
| Some or no high school | 13.36 (0.34) | 19.00 (0.91) | 12.72 (0.34) | |
| High school graduate | 29.12 (0.44) | 33.25 (1.16) | 28.65 (0.46) | |
| At least some college | 57.52 (0.60) | 47.75 (1.36) | 58.63 (0.62) | |
| Married | 0.0017 | |||
| No | 47.84 (0.51) | 44.62 (1.09) | 48.21 (0.54) | |
| Yes | 52.16 (0.51) | 55.38 (1.09) | 51.79 (0.54) | |
| Family annual income | <0.0001 | |||
| Poor (<100% FPL) | 10.85 (0.30) | 14.33 (0.65) | 10.46 (0.30) | |
| Low (100–199% FPL) | 16.09 (0.32) | 22.12 (0.79) | 15.40 (0.34) | |
| Middle (200–399% FPL) | 28.78 (0.43) | 28.20 (0.95) | 28.85 (0.45) | |
| High (≥400% FPL) | 44.28 (0.63) | 35.35 (1.19) | 45.29 (0.65) | |
| Dental insurance | <0.0001 | |||
| Some private | 53.60 (0.59) | 39.53 (1.10) | 55.20 (0.60) | |
| Only public | 13.51 (0.41) | 19.44 (0.80) | 12.84 (0.41) | |
| Neither | 32.89 (0.48) | 41.03 (1.10) | 31.96 (0.51) | |
| Dental services use† | 41.41 (0.51) | 36.48 (0.96) | 41.97 (0.51) | <0.0001 |
| Current smoker | 0.9562 | |||
| No | 86.83 (0.34) | 86.79 (0.76) | 86.83 (0.36) | |
| Yes | 13.17 (0.34) | 13.21 (0.76) | 13.17 (0.36) | |
| Other diseases§ | <0.0001 | |||
| No | 82.89 (0.31) | 53.68 (1.03) | 86.21 (0.28) | |
| Yes | 17.11 (0.31) | 46.32 (1.03) | 13.79 (0.28) | |
| Geographic region | 0.0001 | |||
| Northeast | 17.80 (0.57) | 15.86 (0.76) | 18.03 (0.61) | |
| Midwest | 20.85 (0.66) | 21.39 (1.09) | 20.79 (0.71) | |
| South | 37.59 (0.73) | 41.97 (1.23) | 37.09 (0.76) | |
| West | 23.76 (0.57) | 20.77 (1.02) | 24.10 (0.76) |
Data are weighted % (SE).
Have a past year dental visit.
χ2 test was used to test the distribution difference of categories between individuals with and without diabetes.
Includes heart disease, stroke, diabetes-caused kidney damage, and eye problems.
Diabetes was identified by the survey question, “Other than during pregnancy, have you ever been told by a doctor or other health professional that you had diabetes or sugar diabetes?” in MEPS Priority Conditions Enumeration (PE) Section. Also, MEPS only included noninstitutionalized adults.
The mean adjusted annual incremental dental expenditure associated with diabetes was estimated at $77, mainly attributable to incremental expenditures for restorative/prosthetic/surgical services ($53), followed by diagnostic/other services ($31) (Table 2; unadjusted results in Supplementary Table 1). Adults with diabetes had slightly lower expenses for preventive services than those without (incremental, −$7). By payment source, incremental dental expenditures were paid mainly out of pocket ($40) followed by private insurance ($30), with much less paid by public dental coverage or others ($6).
Table 2.
Adjusted‡ per capita annual dental expenditures (SE) in individuals with and individuals without diabetes and incremental expenditure associated with diabetes in 2017 USD
| With diabetes | Without diabetes | Incremental expenditure§ | P | |
|---|---|---|---|---|
| Total | 393.24 (24.12) | 316.36 (9.17) | 76.88 (25.67) | 0.003 |
| Dental service type* | ||||
| Preventive | 80.68 (1.62) | 87.49 (1.32) | –6.81 (2.72) | 0.012 |
| Restorative/prosthetic/surgical | 201.52 (18.76) | 148.21 (3.71) | 53.31 (18.35) | 0.004 |
| Diagnostic/others | 110.37 (14.63) | 79.43 (3.64) | 30.94 (14.31) | 0.031 |
| Payment source | ||||
| Out of pocket | 192.44 (16.25) | 152.87 (6.87) | 39.57 (15.28) | 0.010 |
| Private insurances | 166.56 (14.15) | 136.73 (3.03) | 29.83 (13.87) | 0.032 |
| Public/others† | 32.75 (2.62) | 26.95 (1.32) | 5.80 (2.76) | 0.036 |
Dental service type: preventive, includes cleaning, prophylaxis, polishing, fluoride treatment, and sealant application; restorative/prosthetic/surgical, includes fillings, inlays, crowns, root canal, implants, bridges, dentures, oral surgery, and periodontal surgery; diagnostic, includes consultation, X-rays, radiographs, or bitewings; others, includes unidentified dental services and multiple services in one dental visit.
Payment source: public, includes Medicaid, Medicare, Veterans Administration/Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA), TRICARE, other federal sources (including Indian Health Service, military treatment facilities, and other care by the federal government), and other state and local sources (including community and neighborhood clinics, state and local health departments, and state programs other than Medicaid); others, include workers’ compensation and sources such as automobile, homeowners, and liability insurance and other miscellaneous or unknown sources.
Two-part models were used for all estimations, with adjustment for sociodemographic characteristics, health status, and geographic variables. Interaction terms such as diabetes and age-group were included in the models to control for the interaction effects. Total does not equal the sum of service types or sum of payment sources because of separate regression estimates.
Two-part models predict the dental expenditures for all adults with and without diabetes—not just for adults with dental visits. The incremental expenditure is the difference between the predicted expenditures of adults with diabetes and those of adults without diabetes.
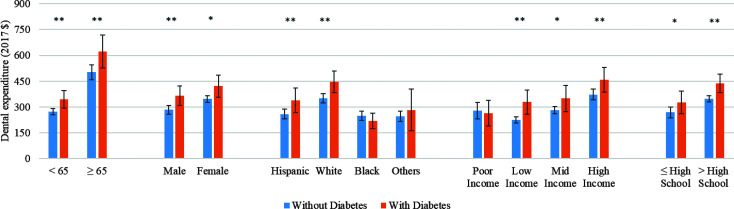
Figure 1 shows the per capita dental expenditure associated with diabetes by population subgroup. Older adults (≥65 years) had higher dental expenditures than younger adults. Among older adults, those with diabetes had $120 higher expenditure than those without diabetes compared with $72 incremental among younger adults. Although females had higher average dental expenditures than males, incremental expenditures associated with diabetes were $74 for females and $80 for males. Non-Hispanic Whites had the highest dental expenditures, followed by Hispanics. In comparison with those without diabetes, non-Hispanic Whites with diabetes had $97 incremental dental expenditures and Hispanics had $79 incremental expenditures. Dental expenditures increased with family income. In all income groups above the poverty level, however, people with diabetes had higher dental expenditures than those without ($68 to $104 incremental expenditures). Mirroring income, higher education was also associated with larger dental expenditures; incremental expenditure associated with diabetes was $90 among those with more than high school education and $57 for those with high school education or less.
Figure 1.
Estimated per capita dental expenditure (2017 USD) associated with diabetes among adults by population subgroup. Family annual income: poor income (<100% FPL), low income (100–199% FPL), middle (Mid) income (200–399% FPL), and high income (≥400% FPL). Age is presented as <65 or ≥65 years old. **Significant difference between people with and without diabetes at P = 0.05; *significant difference between people with and without diabetes at P = 0.10.
We estimated that 25.2 million noninstitutionalized U.S. adults had diabetes. At a $49 unadjusted incremental per capita dental expenditure in people with versus without diabetes (Supplementary Table 1), nationwide, people with diabetes spent $1.2 billion more on dental care if they did not have diabetes (Table 3). The majority of this ($1.1 billion) was for restorative/prosthetic/surgical dental services and was paid out of pocket ($938 million). After adjustment for sociodemographic characteristics, health status, and geographic variables, the estimated national dental expenditure associated with diabetes was $1.9 billion.
Table 3.
National dental expenditure associated with diabetes among adults in the U.S., 2017 USD (millions)
| Unadjusted excess expenditure‡ | % | Adjusted excess expenditure§ | % | |
|---|---|---|---|---|
| Total | 1,231.98 | 100 | 1,939.68 | 100 |
| Dental service type* | ||||
| Preventive | –265.67 | –21 | –171.82 | –9 |
| Restorative/prosthetic/surgical | 1,127.02 | 91 | 1,345.01 | 69 |
| Diagnostic/others | 370.38 | 30 | 780.62 | 40 |
| Payment source | ||||
| Out of pocket | 937.55 | 76 | 998.35 | 51 |
| Private insurances | –239.18 | –19 | 752.61 | 39 |
| Public/others† | 533.61 | 43 | 146.33 | 8 |
Dental service type: preventive, includes cleaning, prophylaxis, polishing, fluoride treatment, and sealant application; restorative/prosthetic/surgical, includes fillings, inlays, crowns, root canal, implants, bridges, dentures, oral surgery, and periodontal surgery; diagnostic, includes consultation, X-rays, radiographs, or bitewings; others, includes unidentified dental services and multiple services in one dental visit.
Payment source: public, includes Medicaid, Medicare, Veterans Administration/Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA), TRICARE, other federal sources (including Indian Health Service, military treatment facilities, and other care by the federal government), and other state and local sources (including community and neighborhood clinics, state and local health departments, and state programs other than Medicaid); others, include workers’ compensation and sources such as automobile, homeowners and liability insurance and other miscellaneous or unknown sources.
The unadjusted excess expenditure was calculated by multiplication of the weighted number of estimated people with diabetes (25.23 million) in our data set by the unadjusted per capita annual excess expenditure associated with diabetes (shown in Supplementary Table 1). The number of estimated people with diabetes in our analysis is close to but not exactly the same as the statistics reported in the U.S. Diabetes Surveillance System because the data sources are different.
The adjusted excess expenditure was calculated by multiplication of the weighted number of estimated people with diabetes by the adjusted per capita annual excess expenditure associated with diabetes (adjusted for sociodemographic characteristics, health status, and geographic variables [shown in Table 2]). Total does not equal the sum of service types or sum of payment sources because of separate regression estimates.
Conclusions
Although previous studies have documented that adults with diabetes are at an increased risk of developing oral diseases and thus may have a greater need and higher expenditures for dental care, the incremental expenditure of dental care associated with diabetes has not been estimated prior to our study. Our results show that in 2016–2017, adjusted per capita annual incremental dental expenditure associated with diabetes was ∼$77, mainly for restorative/prosthetic/surgical services, and largely paid out of pocket by people with diabetes and their families. Nationwide, the estimated total adjusted dental expenditure associated with diabetes was $1.9 billion. There were disparities in diabetes-associated incremental expenditures, with higher incremental expenditures among older, non-Hispanic White, wealthier, and more educated people with diabetes.
The higher total medical expenditures associated with dental care in adults with diabetes is a result of a combination of factors. Consistent with prior studies (8,9), we found that people with diabetes were less likely than those without to have a past year dental visit (36.5% vs. 42.0%). However, among those who had at least one visit, people with diabetes had more dental visits (2.43 vs. 2.16 annually) and spent more per visit ($358 vs. $303) than those without diabetes. Both more visits and higher expenditure per visit may imply that among those who access dental care, dental problems in people with diabetes are more severe.
The mix of dental services provided to adults with diabetes also suggests that they may have severe dental treatment needs. Of the three types of dental services, the highest per capita incremental expenditures ($53) were associated with restorative/prosthetic/surgical services, while expenditures on preventive services were lower. A previous study reported similar findings: people with diabetes were more likely to receive periodontal care and tooth extractions while being less likely to receive preventive dental services (9). Other studies have found that people with diabetes are more likely to receive oral surgery and procedures to replace missing teeth, e.g., implants—in line with the established link between diabetes and periodontitis and between periodontitis and tooth loss (19,20).
Increasing receipt of clinical preventive dental services could reduce the severity of dental treatment needs among adults with diabetes. Fluorides are effective in preventing caries (21), and one study suggested that periodontitis was preventable with routine receipt of preventive dental care (22). In addition, good oral hygiene (e.g., brushing with fluoride toothpaste) is effective in preventing dental caries (23). Less use of preventive dental services among people with diabetes could be due to low oral health literacy and financial barriers. Previous studies found that many people with diabetes were unaware of the oral complications of diabetes and the need for proper preventive care, had limited oral health knowledge, and had poor oral health attitudes (12,24). One study found that dental care use among people with diabetes, although higher than the 36.5% reported in our study, was still low—just over half (54%) of people with diabetes had dental visits in the last 12 months (12). National data also indicate that diabetes is associated with higher prevalence of unmet treatment needs for dental caries and periodontitis (25).
We also found that people with diabetes had greater financial barriers (i.e., lower household incomes and being less likely to have dental insurance) to receiving dental care than did people without diabetes. Moreover, diabetes-related incremental dental expenditure was mainly paid out of pocket. Dental services are mostly provided by private dentists and are financed separately from medical services (26). One previous study found that in comparison with payment sources for clinical services, a much larger proportion of dental services (41% vs. 9%) are paid out of pocket by patients (27). Higher out-of-pocket payment could also be a financial barrier to dental care for people with diabetes. One study found that compared with adults without diabetes, those with diabetes were more likely to identify cost as the main reason for avoiding dental visits (24). It is important to note that while state Medicaid programs are an important component of the medical safety net for many individuals, Medicaid dental benefits are both limited and not available in all states (11). Also, the traditional Medicare fee-for-service program does not cover routine dental services (28).
Our results highlight the importance of increasing oral health awareness among people with diabetes, to encourage them to seek preventive dental care and to engage in appropriate preventive behaviors, which could reduce dental problems and alleviate incremental dental expenditures in the long-term. For improvement of health care outcomes, the American Diabetes Association recommends having a dentist as part of the diabetes care team (29). In addition, interprofessional collaboration between dentists and primary care providers might be considered. For example, primary care providers could screen for signs of early oral disease, provide preventive dental care, and refer people with treatment needs to the dentist (30). The Smiles for Life oral health curriculum has been developed to educate primary care providers to integrate oral health into their practice (31).
Our results on disparities in dental care expenditure across subgroups were consistent with findings from previous studies. Reda et al. (32) found that individuals with less education or less economic resources had less use of dental services. Another study found that low income was associated with a higher rate of dental problems and less use of dental prostheses among people with diabetes (33). Also, lower socioeconomic status could contribute to the underuse of recommended preventive care in people with diabetes (34).
Previous studies reported that older adults were more likely to use dental care than younger adults (35). We observed higher dental expenditures among older adults, and incremental diabetes-related dental expenditures were higher among them. This could be due to higher prevalence of dental disease and the need for more expensive and complex dental procedures. Older adults are more likely to have periodontal disease (68% prevalence [36]) and to have lost all their natural teeth (∼20% [37]). For older adults with diabetes, these problems could worsen due to poor glycemic management (38). With the aging of the population in the U.S. and the increased prevalence of both diabetes and oral diseases in older adults, dental expenditures associated with diabetes among older adults could pose an increasing financial burden on both individuals and the nation as a whole.
This study was subject to several limitations. First, both per-person and aggregated estimates are likely conservative. MEPS does not include individuals residing in nursing homes or other institutions who may have higher dental treatment needs (39) and who are also more likely to be older, a risk factor for diabetes. Similarly, it did not include dental expenditures incurred by individuals with undiagnosed diabetes: ∼20% of people with diabetes (40). Second, we conducted a cross-sectional analysis and examined the association between dental expenditure and diabetes; thus, no causal relationship should be assumed. Third, we did not control for dental market conditions, such as the number of providers per capita in different geographic regions, which can influence both dental services use and expenditures. Fourth, we were not able to distinguish types of diabetes using the MEPS data. Both type 1 and type 2 diabetes are associated with an increased risk of oral diseases (2), and future studies may look at whether diabetes-associated dental expenditures differ by diabetes type.
To our knowledge, this is the first study to examine incremental dental expenditures associated with diabetes. Diabetes-associated incremental dental expenditure was estimated to be $77 per person and $1.9 billion for the nation. This incremental expenditure was largely paid out of pocket and was mainly for restorative/prosthetic/surgical services. Incremental expenditures were higher among older adults, non-Hispanic Whites, and patients with higher levels of family income and education. Our results fill this missing component in the current estimates of total medical expenditures associated with diabetes in the U.S. and highlight the importance of preventive dental care among people with diabetes.
Article Information
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. Y.C. designed the study, analyzed data, interpreted results, and drafted the manuscript. P.Z. designed the study, interpreted results, and revised the manuscript. E.T.L. and S.O.G. reviewed and revised the manuscript. D.B.R. interpreted results and revised the manuscript. Y.C. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
This article contains supplementary material online at https://doi.org/10.2337/figshare.14224274.
References
- 1. Lamster IB, Lalla E, Borgnakke WS, Taylor GW. The relationship between oral health and diabetes mellitus. J Am Dent Assoc 2008;139(Suppl.):19S–24S [DOI] [PubMed] [Google Scholar]
- 2. Ship JA. Diabetes and oral health: an overview. J Am Dent Assoc 2003;134:4S–10S [DOI] [PubMed] [Google Scholar]
- 3. Mealey BL. Periodontal disease and diabetes. A two-way street. J Am Dent Assoc 2006;137(Suppl.):26S–31S [DOI] [PubMed] [Google Scholar]
- 4. Mealey BL, Ocampo GL. Diabetes mellitus and periodontal disease. Periodontol 2000 2007;44:127–153 [DOI] [PubMed] [Google Scholar]
- 5. Taylor GW, Burt BA, Becker MP, Genco RJ, Shlossman M. Glycemic control and alveolar bone loss progression in type 2 diabetes. Ann Periodontol 1998;3:30–39 [DOI] [PubMed] [Google Scholar]
- 6. Löe H. Periodontal disease. The sixth complication of diabetes mellitus. Diabetes Care 1993;16:329–334 [PubMed] [Google Scholar]
- 7. Parker ML, Thornton-Evans G, Wei L, Griffin SO. Prevalence of and changes in tooth loss among adults aged ≥50 years with selected chronic conditions - United States, 1999-2004 and 2011-2016. MMWR Morb Mortal Wkly Rep 2020;69:641–646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tomar SL, Lester A. Dental and other health care visits among U.S. adults with diabetes. Diabetes Care 2000;23:1505–1510 [DOI] [PubMed] [Google Scholar]
- 9. Chaudhari M, Hubbard R, Reid RJ, et al. Evaluating components of dental care utilization among adults with diabetes and matched controls via hurdle models. BMC Oral Health 2012;12:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Willink A, Schoen C, Davis K. Dental care and Medicare beneficiaries: access gaps, cost burdens, and policy options. Health Aff (Millwood) 2016;35:2241–2248 [DOI] [PubMed] [Google Scholar]
- 11. American Dental Association . Breaking Down Barriers to Oral Health for all Americans: Repairing the Tattered Safety Net. American Dental Association, Washington, DC, 2011 [Google Scholar]
- 12. Poudel P, Griffiths R, Wong VW, et al. Oral health knowledge, attitudes and care practices of people with diabetes: a systematic review. BMC Public Health 2018;18:577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. American Diabetes Association . Economic costs of diabetes in the U.S. in 2017. Diabetes Care 2018;41:917–928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang G, Zhou X, Zhuo X, Zhang P. Annual total medical expenditures associated with hypertension by diabetes status in U.S. adults. Am J Prev Med 2017;53:S182–S189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang G, Pratt M, Macera CA, Zheng ZJ, Heath G. Physical activity, cardiovascular disease, and medical expenditures in U.S. adults. Ann Behav Med 2004;28:88–94 [DOI] [PubMed] [Google Scholar]
- 16. Deb P, Norton EC. Modeling health care expenditures and use. Annu Rev Public Health 2018;39:489–505 [DOI] [PubMed] [Google Scholar]
- 17. Manski RJ, Rohde F. Dental Services: Use, Expenses, Source of Payment, Coverage and Procedure Type, 1996-2015: Research Findings No. 38. Rockville, MD, Agency for Healthcare Research and Quality, 2017 [Google Scholar]
- 18. Dunn A, Grosse SD, Zuvekas SH. Adjusting health expenditures for inflation: a review of measures for health services research in the United States. Health Serv Res 2018;53:175–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Taylor GW, Borgnakke WS. Periodontal disease: associations with diabetes, glycemic control and complications. Oral Dis 2008;14:191–203 [DOI] [PubMed] [Google Scholar]
- 20. Kapp JM, Boren SA, Yun S, LeMaster J. Diabetes and tooth loss in a national sample of dentate adults reporting annual dental visits. Prev Chronic Dis 2007;4:A59. [PMC free article] [PubMed] [Google Scholar]
- 21. Griffin SO, Regnier E, Griffin PM, Huntley V. Effectiveness of fluoride in preventing caries in adults. J Dent Res 2007;86:410–415 [DOI] [PubMed] [Google Scholar]
- 22. Shay K. Infectious complications of dental and periodontal diseases in the elderly population. Clin Infect Dis 2002;34:1215–1223 [DOI] [PubMed] [Google Scholar]
- 23. World Health Organization . Oral Health, 2020. Accessed 18 August 2020. Available from https://www.who.int/news-room/fact-sheets/detail/oral-health
- 24. Moore PA, Orchard T, Guggenheimer J, Weyant RJ. Diabetes and oral health promotion: a survey of disease prevention behaviors. J Am Dent Assoc 2000;131:1333–1341 [DOI] [PubMed] [Google Scholar]
- 25. Griffin SO, Barker LK, Griffin PM, Cleveland JL, Kohn W. Oral health needs among adults in the United States with chronic diseases. J Am Dent Assoc 2009;140:1266–1274 [DOI] [PubMed] [Google Scholar]
- 26. Vujicic M. How affordable is health care in the United States and other countries? J Am Dent Assoc 2014;145:482–483 [DOI] [PubMed] [Google Scholar]
- 27. Centers for Medicare & Medicaid Services . National Health Expenditures by type of service and source of funds, CY 1960-2018. Centers for Medicare & Medicaid Services. Accessed 17 December 2019. Available from https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical
- 28. Freed M, Neuman T, Jacobson G. Drilling Down on Dental Coverage and Costs for Medicare Beneficiaries. Henry J Kaiser Family Foundation, San Francisco, California, 2019 [Google Scholar]
- 29. American Diabetes Association . Get to know your diabetes care team, 2020. Accessed 26 August 2020. Available from https://www.diabetes.org/diabetes/medication-management/your-health-care-team
- 30. Hummel J, Phillips K, Holt B, Hayes C. Oral Health: An Essential Component of Primary Care. Seattle, WA, Qualis Health, 2015 [Google Scholar]
- 31. Smiles for Life: a national oral health curriculum. Accessed 22 August 2020. Available from https://www.smilesforlifeoralhealth.org
- 32. Reda SF, Reda SM, Thomson WM, Schwendicke F. Inequality in utilization of dental services: a systematic review and meta-analysis. Am J Public Health 2018;108:e1–e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Azogui-Lévy S, Dray-Spira R. Sociodemographic factors associated with the dental health of persons with diabetes in France. Spec Care Dentist 2012;32:142–149 [DOI] [PubMed] [Google Scholar]
- 34. Brown AF, Ettner SL, Piette J, et al. Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiol Rev 2004;26:63–77 [DOI] [PubMed] [Google Scholar]
- 35. Manski RJ, Goodman HS, Reid BC, Macek MD. Dental insurance visits and expenditures among older adults. Am J Public Health 2004;94:759–764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Eke PI, Dye BA, Wei L, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol 2015;86:611–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dye B, Thornton-Evans G, Li X, Iafolla T. Dental caries and tooth loss in adults in the United States, 2011-2012. NCHS Data Brief, no. 197. Hyattsville, MD, National Center for Health Statistics, 2015 [PubMed] [Google Scholar]
- 38. Lin BP, Taylor GW, Allen DJ, Ship JA. Dental caries in older adults with diabetes mellitus. Spec Care Dentist 1999;19:8–14 [DOI] [PubMed] [Google Scholar]
- 39. Griffin SO, Griffin PM, Li CH, Bailey WD, Brunson D, Jones JA. Changes in older adults’ oral health and disparities: 1999 to 2004 and 2011 to 2016. J Am Geriatr Soc 2019;67:1152–1157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Centers for Disease Control and Prevention . National Diabetes Statistics Report, 2020. Atlanta, GA, Centers for Disease Control and Prevention, U.S. Department of Health Human Services, 2020 [Google Scholar]