Abstract
OBJECTIVE
To investigate the effects of alcohol abstinence on prevention of new-onset atrial fibrillation (AF) in patients with type 2 diabetes mellitus (T2DM).
RESEARCH DESIGN AND METHODS
A total of 1,112,682 patients newly diagnosed with T2DM between 2011 and 2014 were identified from the Korean National Health Insurance Service database. After excluding those with a history of AF, 175,100 patients were included. The primary outcome was new-onset AF.
RESULTS
During a mean follow-up of 4.0 years, AF occurred in 4,174 patients. Those with heavy alcohol consumption (alcohol intake ≥40 g/day) before T2DM diagnosis had a higher risk of AF (adjusted hazard ratio [aHR] 1.22; 95% CI 1.06–1.41) compared with patients with no alcohol consumption. After T2DM diagnosis, those with moderate to heavy alcohol consumption (alcohol intake ≥20 g/day) who abstained from alcohol had a lower risk of AF (aHR 0.81; 95% CI 0.68–0.97) compared with constant drinkers. Alcohol abstinence showed consistent trends toward lower incident AF in all subgroups and was statistically significant in men (aHR 0.80; 95% CI 0.67–0.96), those aged >65 years (aHR 0.69; 95% CI 0.52–0.91), those with CHA2DS2-VASc score <3 points (aHR 0.71; 95% CI 0.59–0.86), noninsulin users (aHR 0.77; 95% CI 0.63–0.94), and those with BMI <25 kg/m2 (aHR 0.68; 95% CI 0.53–0.88).
CONCLUSIONS
In patients with newly diagnosed T2DM, alcohol abstinence was associated with a low risk of AF development. Lifestyle modifications, such as alcohol abstinence, in patients newly diagnosed with T2DM should be recommended to reduce the risk of AF.
Introduction
With an increase in the aging population, the prevalence of atrial fibrillation (AF), which is the most common sustained arrhythmia worldwide, is increasing, and effective prevention strategies should be implemented to mitigate this public health problem (1,2). The prevalence of diabetes is also rapidly increasing, with an increase in the number of patients at high risk of cardiovascular disease (3). Diabetes, specifically type 2 diabetes mellitus (T2DM), is a strong risk factor for atherosclerotic cardiovascular disease, and it also increases the risk of AF development by 28% (4). Therefore, a combined approach to target diabetes and cardiovascular disease is important.
Unhealthy lifestyle habits, including lack of regular physical activity, obesity, weight fluctuation, and smoking, have a close association with a higher risk of incident AF (5–7). However, the association between alcohol consumption and cardiovascular disease is still controversial (8). The cardioprotective effects of alcohol consumption have been touted since the 18th century, and the majority of the literature suggests that a small amount of alcohol is beneficial but excess drinking is detrimental to the cardiovascular system (9). Moreover, a recent clinical trial on secondary prevention of AF supported that a substantial reduction in alcohol consumption could reduce the recurrence of AF (10). Although the mechanism underlying the increased susceptibility to AF because of alcohol consumption is not clearly understood, there are several pathophysiological mechanisms for AF development resulting from alcohol, including alternations in calcium handling (11), hypertension (12), obesity, and sleep apnea (13).
On the basis of these considerations, we hypothesized that alcohol abstinence in a T2DM population at high risk of developing AF would reduce the risk of incident AF development. To test this hypothesis, we aimed to investigate whether changes in alcohol consumption behavior in moderate to heavy alcohol consumption (≥20 g/day) would influence new-onset AF in patients newly diagnosed with T2DM.
Research Design and Methods
Data Sources and Study Population
In this study, we used the Korean National Health Insurance Service–Health Screening Cohort (NHIS-HEALS) database, which is the national health claims database linked with the National Health Screening Program database (14). The National Health Screening Program includes physical examinations, regular blood tests, and self-administered questionnaires on lifestyle behavior, including alcohol consumption behavior, smoking status, and amount of moderate- to vigorous-intensity physical activity. The Korean government established the NHIS-HEALS database in 2015 to provide integrated health claims data appropriate and useful for a wide range of health research efforts. In the NHIS database, diagnoses are recorded based on the ICD-10 Clinical Modification (ICD-10-CM) codes.
We identified 1,112,682 patients newly diagnosed with T2DM between 2011 and 2014 from the NHIS database. T2DM was defined on the basis of diagnostic codes of T2DM (E11–E14), either one recorded during hospitalization or at least two recorded in outpatient clinics and/or the prescription of insulin and/or at least one oral hypoglycemic agent (14). Oral hypoglycemic agents included metformin, sulfonylurea, meglitinides, thiazolidinedione, dipeptidyl peptidase 4 inhibitor, and α-glucosidase inhibitor.
This study was approved by the institutional review board of Seoul National University Hospital (E-1912-085-1089). This study was conducted in accordance with the Declaration of Helsinki. The NHIS-HEALS database has been made publicly available to facilitate wider use of the health screening database with anonymous and deidentified information; therefore, the requirement for informed consent was waived.
Alcohol Consumption Behavior
Alcohol consumption behavior was defined based on data on the frequency of alcohol intake per week and the amount of alcohol consumed per drinking episode obtained from a health screening self-administered questionnaire in the NHIS-HEALS database.
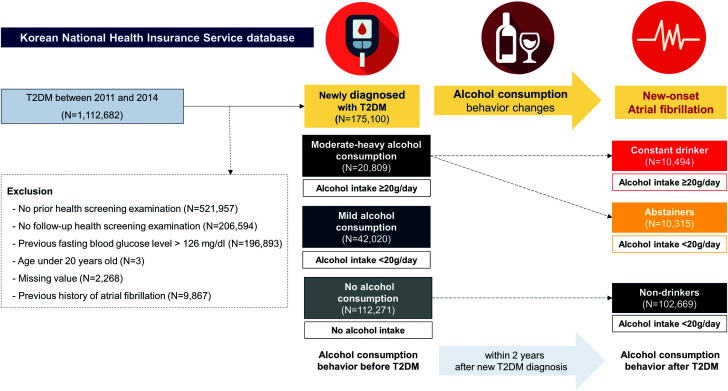
After excluding individuals with a history of AF, we reviewed information on alcohol consumption behavior of 175,100 patients within 2 years before the first diagnosis of T2DM (Fig. 1). Alcohol consumption behavior was divided into three groups according to the average amount of alcohol intake per day as follows: 1) no alcohol consumption (0 g/day), 2) mild alcohol consumption (<20 g/day), and 3) moderate to heavy consumption (≥20 g/day).
Figure 1.
Flow of study population. Patients were divided into three groups based on the average amount of alcohol consumed before the first diagnosis of T2DM (alcohol consumption behavior): 1) no alcohol consumption (0 g/day), 2) mild alcohol consumption (<20 g/day), and 3) moderate to heavy consumption (≥20 g/day). Alcohol consumption behavior change among those who drank a moderate to heavy amount (≥20 g/day) was defined as the average amount of alcohol consumed within 2 years after new diagnosis of T2DM: 1) constant drinkers (≥20 g/day) and 2) abstainers (<20 g/day); those who did not drink alcohol either before or after T2DM diagnosis were defined as 3) nondrinkers.
Alcohol Consumption Behavior Change in Patients With Moderate to Heavy Alcohol Consumption
To evaluate the impact of alcohol abstinence on the risk of AF, we classified patients with moderate to heavy alcohol consumption before T2DM diagnosis (n = 20,809) into two groups according to average alcohol consumption within 2 years after the first diagnosis of T2DM: 1) abstainers who became non- to mild drinkers (<20 g/day) and 2) constant drinkers who continued to drink alcohol moderately or heavily (≥20 g/day) (Fig. 1). Among patients reporting no alcohol consumption (n = 112,271), those who did not drink after being newly diagnosed with T2DM were defined as nondrinkers.
Primary Outcome: New-Onset AF
The primary outcome was new-onset AF, which was defined as a new diagnosis with ICD-10-CM codes I480–I484 and I489 by either one record during hospitalization or at least two records in the outpatient clinic. Because of apparent differences in a pathophysiological mechanism in valvular and nonvalvular AF, we excluded patients diagnosed as having mitral stenosis (I050, I052, and I059) and those who had mechanical heart valves (Z952–Z954) from the analysis to identify new-onset AF with a mechanism other than those by valvular heart disease. This definition has been validated in previous studies (15). The study population was followed up until the occurrence of AF, death, or 31 December 2017, whichever came first. Death or emigration before the primary event was treated as a censoring event.
Definition of Covariates
Demographic findings and socioeconomic variables were based on the NHIS-HEALS database. ICD-10-CM codes, prescription, and use of health care services (claims data) were used to define the comorbidities of the study population (Supplementary Table 1).
BMI was defined as weight in kilograms divided by the square of height in meters (kg/m2). Smoking status (non-, former, or current smoker) and amount of moderate- to vigorous-intensity physical activity were obtained using a health screening self-administered questionnaire. Regular physical activity was defined as moderate physical activity for >30 min, at least five times per week, or strenuous physical activity for >20 min, at least three times per week. Low-income status indicated the lowest quadrant (25%) of income level. The CHA2DS2-VASc score comprises congestive heart failure, hypertension, age (>65 years = 1 point; >75 years = 2 points), diabetes, previous stroke/transient ischemic attack (2 points), vascular disease (peripheral arterial disease, previous myocardial infarction, and aortic atheroma), and sex category (female sex).
Statistical Analyses
Baseline characteristics are presented as numbers and percentages for categorical variables and means ± SDs for continuous variables. For baseline comparisons, the Student t or Mann-Whitney U test was used for continuous variables, and the χ2 or Fisher exact test was used for categorical variables.
The event rate of the primary outcome is presented as 1,000 person-years, determined by dividing the number of events by the total person-year period. Hazard ratios (HRs) and 95% CIs for AF development were analyzed using the Cox proportional hazards model. For multivariate analysis, model 1 was adjusted for age and sex, and model 2 was adjusted for age, sex, BMI, smoking status, regular physical activity, low-income status, CHA2DS2-VASc score, hypertension, dyslipidemia, stroke/transient ischemic attack, congestive heart failure, peripheral artery disease, thromboembolism, use of insulin, and number of oral hypoglycemic agents. Subgroup analysis was performed according to the following: sex, age (<65 or ≥65 years), CHA2DS2-VASc score (<3 or ≥3 points), use of insulin, smoking status (non-, former, or current smoker), and BMI (<25 and ≥25 kg/m2).
Statistical significance was defined as a two-sided P value of <0.05. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Inc.) and R version 3.2.4 (R Core Team) software.
Results
Baseline Characteristics of Patients Newly Diagnosed With T2DM
Overall, 175,100 patients (mean age 61.1 years; male 50.4%) were newly diagnosed with T2DM between 2011 and 2014. Before they were diagnosed with T2DM, there were a total of 112,271 (64.1%), 42,020 (24.0%), and 20,809 (11.9%) nondrinkers, mild drinkers, and moderate to heavy drinkers, respectively. Baseline characteristics according to alcohol consumption before diagnosis of T2DM are summarized in Supplementary Table 2.
Risk of AF According to Alcohol Consumption Behavior Before T2DM Diagnosis
During a mean follow-up period of 4.0 years, new-onset AF was observed in 4,174 patients with T2DM. The risk of AF was different depending on the amount and frequency of alcohol consumption before T2DM diagnosis (Supplementary Table 3). Compared with no alcohol consumption, heavy alcohol consumption (average amount of alcohol consumed ≥40 g/day) was associated with a high risk of AF development (adjusted HR [aHR] 1.22; 95% CI 1.06–1.41). Drinking more than or equal to three times a week was significantly associated with AF development (aHR 1.13; 95% CI 1.03–1.25). Mild or moderate alcohol consumption (<40 g/day) and drinking fewer than three times a week was not statistically significantly associated with AF development compared with no alcohol consumption.
Baseline Characteristics According to Alcohol Consumption Behavior Change
According to alcohol consumption behavior change within 2 years after new diagnosis of T2DM, abstainers and constant drinkers were younger (mean age 57.2 ± 11.1 and 55.3 ± 10.3 years, respectively) and more commonly male (91.5% and 97.3%, respectively) compared with nondrinkers (mean age 63.9 ± 10.4 years; male 29.3%). Nondrinkers had more underlying comorbidities, such as congestive heart failure, dyslipidemia, stroke/transient ischemic attack, and peripheral arterial disease compared with abstainers and constant drinkers (Table 1).
Table 1.
Baseline characteristics according to alcohol consumption behavior change after the first diagnosis of T2DM
| Variable | Nondrinkers (n = 102,669) | Abstainers (n = 10,315) | Constant drinkers (n = 10,494) |
|---|---|---|---|
| Age, years | 63.9 ± 10.4 | 57.2 ± 11.1 | 55.3 ± 10.3 |
| <65 | 52,255 (50.9) | 7,705 (74.7) | 8,584 (81.8) |
| 65–75 | 35,783 (34.9) | 2,071 (20.1) | 1,592 (15.2) |
| ≥75 | 14,631 (14.3) | 539 (5.2) | 318 (3.0) |
| Male sex | 30,073 (29.3) | 9,439 (91.5) | 10,211 (97.3) |
| BMI, kg/m2 | 25.1 ± 3.5 | 25.3 ± 3.5 | 25.7 ± 3.4 |
| BP measurement, mmHg | |||
| Systolic | 126.7 ± 14.9 | 126.8 ± 14.1 | 129.0 ± 14.0 |
| Diastolic | 76.9 ± 9.5 | 78.6 ± 9.5 | 80.4 ± 9.6 |
| Comorbidities | |||
| Congestive heart failure | 4,582 (4.5) | 295 (2.9) | 174 (1.7) |
| Hypertension | 22,240 (21.7) | 2,233 (21.7) | 2,798 (26.7) |
| Dyslipidemia | 62,350 (60.7) | 5,600 (54.3) | 5,725 (54.6) |
| Stroke/transient ischemic attack | 4,654 (4.5) | 448 (4.4) | 236 (2.3) |
| Thromboembolism | 902 (0.9) | 79 (0.8) | 1,095 (0.8) |
| Peripheral artery disease | 21,648 (21.1) | 1,651 (16.0) | 1,533 (14.6) |
| Myocardial infarction | 1,943 (1.9) | 194 (1.9) | 113 (1.1) |
| Total cholesterol, mg/dL | 185.9 ± 40.4 | 184.4 ± 40.8 | 188.5 ± 40.7 |
| Serum glucose, mg/dL | 111.9 ± 26.0 | 117.0 ± 31.0 | 121.9 ± 32.8 |
| AST, units/L | 28.1 ± 23.4 | 33.1 ± 36.4 | 37.8 ± 47.4 |
| ALT, units/L | 28.4 ± 28.6 | 34.4 ± 33.1 | 37.7 ± 50.7 |
| Smoking status | |||
| Never | 82,964 (80.8) | 3,115 (30.2) | 1,799 (17.1) |
| Former | 11,644 (11.3) | 3,586 (34.8) | 3,798 (36.2) |
| Current | 8,061 (7.9) | 3,614 (35.0) | 4,897 (46.7) |
| Low income | 22,494 (21.9) | 1,993 (19.3) | 1,792 (17.1) |
| Regular physical activity | 21,019 (20.5) | 2,513 (24.4) | 2,379 (22.7) |
| Insulin user | 14,241 (13.9) | 1,974 (19.1) | 1,148 (10.9) |
| Oral hypoglycemic agent | |||
| Single | 66,334 (64.6) | 6,266 (60.8) | 6,713 (64.0) |
| Dual combination | 26,864 (26.2) | 2,858 (27.7) | 2,891 (27.6) |
| Triple combination | 9,471 (9.2) | 1,191 (11.6) | 890 (8.5) |
| CHA2DS2-VASc points | 2.93 ± 1.28 | 1.91 ± 1.04 | 1.73 ± 0.91 |
| ≥3 | 58,965 (57.4) | 2,425 (23.5) | 1,747 (16.7) |
| CHA2DS2-VASc score* | |||
| 1 | 10,714 (10.4) | 4,546 (44.1) | 5,268 (50.2) |
| 2 | 32,990 (32.1) | 3,344 (32.4) | 3,479 (33.2) |
| 3 | 28,805 (28.1) | 1,622 (15.7) | 1,256 (12.0) |
| 4 | 18,211 (17.7) | 552 (5.35) | 368 (3.51) |
| 5 | 8,259 (8.04) | 175 (1.7) | 88 (0.84) |
| 6 | 2,753 (2.68) | 60 (0.58) | 31 (0.3) |
| 7 | 732 (0.71) | 14 (0.14) | 4 (0.04) |
| 8 | 193 (0.19) | 2 (0.02) | 0 (0) |
| 9 | 12 (0.01) | 0 (0) | 0 (0) |
Data are presented as n (%) or mean ± SD. All variables were significantly different among the groups (all P < 0.001).
CHA2DS2-VASc score includes congestive heart failure, hypertension, age (>65 = 1 point; >75 = 2 points), diabetes, previous stroke/transient ischemic attack/thromboembolism (2 points), vascular disease (peripheral arterial disease, previous myocardial infarction, and aortic atheroma), and sex category (female sex).
Risk of AF According to Alcohol Consumption Behavior Change After T2DM Diagnosis
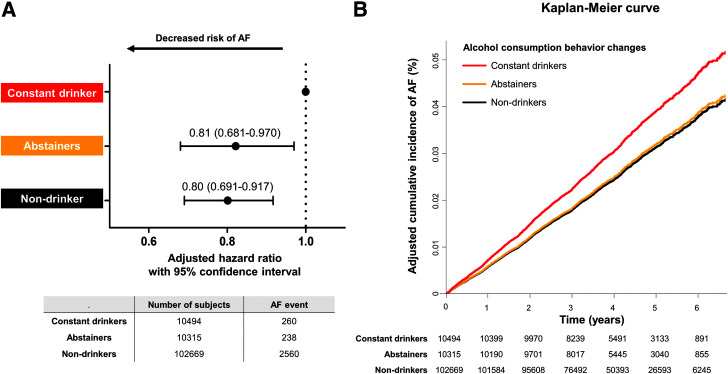
Compared with constant drinkers (average amount of alcohol consumed ≥20 g/day), abstainers (average amount of alcohol consumed <20 g/day) who previously engaged in moderate to heavy drinking after T2DM diagnosis (aHR 0.81; 95% CI 0.68–0.97) and nondrinkers (aHR 0.80; 95% CI 0.69–0.92) showed a significantly lower risk of new-onset AF (Fig. 2 and Supplementary Table 4). The risk of new-onset AF in the abstainer group was comparable to that in the nondrinker group (P = 0.762).
Figure 2.
The risk of AF according to alcohol consumption behavior change after diagnosis of T2DM. A: Forest plot of aHRs (adjusted for age, sex, BMI, smoking status, regular physical activity, low income, CHA2DS2-VASc score, hypertension, dyslipidemia, chronic heart failure, peripheral arterial disease, stroke/transient ischemic attack, thromboembolism, use of insulin, and number of oral hypoglycemic agents) with 95% CIs of the risk of AF in abstainers and nondrinkers compared with constant drinkers. B: Kaplan-Meier curve estimates of the cumulative incidence of AF according to alcohol consumption behavior change.
Subgroup Analysis
In the subgroup analysis, alcohol abstinence showed consistent trends toward lower incident AF compared with constant drinking across all subgroups (Table 2). Despite the small number in each subgroup, there were statistically significant differences for men (aHR 0.80; 95% CI 0.67–0.96), those aged <65 years (aHR 0.69; 95% CI 0.52–0.91) and ≥65 years (aHR 0.79; 95% CI 0.64–0.97), those with CHA2DS2-VAS score <3 points (aHR 0.71; 95% CI 0.59–0.86), noninsulin users (aHR 0.77; 95% CI 0.63–0.94), and those with low BMI (<25 kg/m2) (aHR 0.68; 95% CI 0.53–0.88). Subgroup analysis according to changes in smoking habits and BMI also had no statistically significant interaction (Supplementary Table 5).
Table 2.
Subgroup analysis
| Variable | n of patients | Follow-up duration, person-years | Unadjusted | Adjusted | |||||
|---|---|---|---|---|---|---|---|---|---|
| Total | AF | HR (95% CI) | P* | Model 1† | Model 2‡ | ||||
| HR (95% CI) | P* | HR (95% CI) | P* | ||||||
| Sex group | 0.728 | 0.261 | 0.350 | ||||||
| Male | |||||||||
| Constant drinkers | 10,211 | 255 | 41,499 | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Abstainers | 9,439 | 222 | 38,361 | 0.94 (0.79–1.13) | 0.83 (0.69–0.99) | 0.80 (0.67–0.96) | |||
| Nondrinkers | 30,073 | 930 | 118,248 | 1.28 (1.12–1.47) | 0.83 (0.71–0.95) | 0.80 (0.69–0.92) | |||
| Female | |||||||||
| Constant drinkers | 283 | 5 | 1,091 | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Abstainers | 876 | 16 | 3,499 | 1.00 (0.37–2.72) | 0.90 (0.33–2.46) | 0.86 (0.31–2.34) | |||
| Nondrinkers | 72,596 | 1,630 | 289,418 | 1.23 (0.51–2.95) | 0.69 (0.29–1.68) | 0.66 (0.27–1.61) | |||
| Age group, years | 0.429 | 0.329 | 0.267 | ||||||
| <65 | |||||||||
| Constant drinkers | 8,584 | 156 | 35,200 | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Abstainers | 7,705 | 135 | 31,745 | 0.96 (0.76–1.21) | 0.97 (0.77–1.22) | 0.92 (0.73–1.16) | |||
| Nondrinkers | 52,255 | 684 | 212,466 | 0.73 (0.61–0.86) | 0.80 (0.66–0.98) | 0.75 (0.61–0.92) | |||
| ≥65 | |||||||||
| Constant drinkers | 1,910 | 104 | 7,390 | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Abstainers | 2,610 | 103 | 10,115 | 0.72 (0.55–0.95) | 0.71 (0.54–0.93) | 0.69 (0.52–0.91) | |||
| Nondrinkers | 50,414 | 1,876 | 195,200 | 0.68 (0.56–0.83) | 0.82 (0.66–1.00) | 0.79 (0.64–0.97) | |||
| CHA2DS-VASc points | 0.552 | 0.142 | 0.144 | ||||||
| < 3 | |||||||||
| Constant drinkers | 8,747 | 180 | 35,709 | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Abstainers | 7,890 | 137 | 32,390 | 0.84 (0.67–1.05) | 0.81 (0.65–1.01) | 0.78 (0.63–0.98) | |||
| Nondrinkers | 43,704 | 600 | 176,686 | 0.68 (0.57–0.80) | 0.74 (0.61–0.88) | 0.71 (0.59–0.86) | |||
| ≥3 | |||||||||
| Constant drinkers | 1,747 | 80 | 6,881 | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Abstainers | 2,425 | 101 | 9,471 | 0.92 (0.68–1.20) | 0.91 (0.68–1.22) | 0.87 (0.65–1.17) | |||
| Nondrinkers | 58,965 | 1,960 | 230,980 | 0.73 (0.58–0.91) | 0.95 (0.75–1.20) | 0.90 (0.71–1.14) | |||
| Insulin use | 0.547 | 0.605 | 0.639 | ||||||
| Nonuser | |||||||||
| Constant drinkers | 9,346 | 228 | 38,077 | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Abstainers | 8,341 | 175 | 34,184 | 0.85 (0.70–1.04) | 0.77 (0.63–0.94) | 0.77 (0.63–0.94) | |||
| Nondrinkers | 88,428 | 2,085 | 353,409 | 0.99 (0.86–1.13) | 0.78 (0.67–0.91) | 0.77 (0.66–0.89) | |||
| User | |||||||||
| Constant drinkers | 1,148 | 32 | 4,513 | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Abstainers | 1,974 | 63 | 7,676 | 1.16 (0.76–1.77) | 1.05 (0.69–1.62) | 1.03 (0.67–1.58) | |||
| Nondrinkers | 14,241 | 475 | 54,257 | 1.23 (0.86–1.76) | 0.98 (0.67–1.43) | 0.95 (0.65–1.39) | |||
| Smoking status | <0.001 | 0.213 | 0.222 | ||||||
| Nonsmoker | |||||||||
| Constant drinkers | 1,799 | 60 | 7,336 | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Abstainers | 3,115 | 80 | 12,598 | 0.78 (0.56–1.08) | 0.77 (0.55–1.07) | 0.73 (0.52–1.02) | |||
| Nondrinkers | 82,964 | 1,975 | 330,168 | 0.73 (0.57–0.95) | 0.70 (0.53–0.92) | 0.66 (0.51–0.87) | |||
| Former | |||||||||
| Constant drinkers | 3,798 | 90 | 15,375 | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Abstainers | 3,586 | 91 | 14,559 | 1.07 (0.80–1.43) | 0.95 (0.71–1.27) | 0.92 (0.68–1.23) | |||
| Nondrinkers | 11,644 | 396 | 45,237 | 1.50 (1.19–1.88) | 1.02 (0.80–1.29) | 0.99 (0.78–1.26) | |||
| Current | |||||||||
| Constant drinkers | 4,897 | 110 | 19,880 | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Abstainers | 3,614 | 67 | 14,703 | 0.82 (0.61–1.12) | 0.76 (0.56–1.03) | 0.75 (0.56–1.02) | |||
| Nondrinkers | 8,061 | 189 | 32,261 | 1.06 (0.84–1.34) | 0.73 (0.57–0.94) | 0.73 (0.57– 0.95) | |||
| BMI, kg/m2 | 0.191 | 0.104 | 0.073 | ||||||
| <25 | |||||||||
| Constant drinkers | 4,612 | 129 | 18,601 | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Abstainers | 5,017 | 110 | 20,217 | 0.79 (0.61–1.01) | 0.71 (0.55–0.91) | 0.68 (0.53–0.88) | |||
| Nondrinkers | 53,635 | 1,370 | 212,530 | 0.93 (0.78–1.12) | 0.81 (0.67–0.99) | 0.79 (0.65–0.96) | |||
| ≥25 | |||||||||
| Constant drinkers | 5,882 | 131 | 23,989 | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Abstainers | 5,298 | 128 | 21,643 | 1.08 (0.85–1.38) | 0.99 (0.77–1.26) | 0.96 (0.75–1.23) | |||
| Nondrinkers | 49,034 | 1,190 | 195,136 | 1.12 (0.93–1.34) | 0.83 (0.68–1.02) | 0.80 (0.65–0.99) | |||
P for interaction.
Model 1: adjusted for age and sex.
Model 2: adjusted for age, sex, BMI, smoking status, regular physical activity, low income, CHA2DS2-VASc score, hypertension, dyslipidemia, chronic heart failure, peripheral arterial disease, stroke/transient ischemic attack, thromboembolism, use of insulin, and number of oral hypoglycemic agents.
Conclusions
To our knowledge, this is the first study showing the beneficial effects of alcohol abstinence in preventing cardiovascular disease, specifically new-onset AF, in patients with T2DM. Our principal findings are as follows: 1) heavy and frequent drinking patterns were both associated with a high risk of incident AF; 2) alcohol abstainers who previously engaged in moderate to heavy drinking after T2DM diagnosis had a lower risk of AF development compared with those who still engaged in constant moderate to heavy drinking; 3) those abstaining from alcohol had a low risk of incident AF, similar to that of nondrinkers, despite a history of moderate to heavy alcohol consumption before T2DM diagnosis; and 4) subgroup analyses showed consistent trends in all relevant patient subgroups.
AF is common in patients with diabetes, and both conditions will be more prevalent in the future because of the aging population. Experimental and clinical evidence suggests that diabetes and AF are strongly pathologically interconnected (16,17). Mutual mechanisms that can explain an increased risk of AF with diabetes include structural remodeling of the left atrium in the form of atrial dilation and fibrosis (18), and electromechanical (19) and autonomic remodeling (20). Considering that diabetes has been associated with worse AF symptoms, lower quality of life, and increased risk of death and hospitalization, our main finding, that is, alcohol abstinence in patients with T2DM could lower the risk of developing AF, is an important consideration in the holistic approach to AF care (21,22).
Alcohol consumption is highly prevalent in the U.S. and has increased over the past few decades, reaching 2.35 gallons of ethanol per capita in 2018 (23). In Korea, the prevalence of high-risk alcohol consumption is 15.1%, with the highest prevalence of 28.3% found in middle-aged men (45–64 years) (24). Considering that the liver significantly metabolizes alcohol, this may have an impact on controlling blood glucose levels among patients with diabetes (25). Furthermore, alcohol is high in carbohydrates and calories, which increase blood glucose levels and stimulate patients’ appetite, leading to increased glucose levels as a result of overeating.
The lowering of AF risk through alcohol abstinence could be explained by several mechanisms. First, alcohol could affect the autonomic nervous system, including sympathetic effects and vagal stimulation, which are considered important triggers for AF (26). Second, alcohol is well known to cause direct cardiac toxicity, triggering AF by rendering the myocardium in the atria more susceptible to AF, and binge and frequent drinking could lead to cardiac inflammation (27). Previous observational studies have linked regular alcohol consumption (as compared with no alcohol consumption) with dose-related increases in left atrial size (28), impairments in atrial mechanical and reservoir function (29), and adverse electrical remodeling (30). Alcohol is also associated with systolic hypertension, which increases the risk of AF by the activation of the renin-angiotensin system, increased vascular reactivity, and inhibition of endothelial nitric oxide production (12).
The effect of mild alcohol consumption (usually defined as <10–20 g/day) is associated with lower incidence, in a U-shaped pattern, of cardiovascular disease (31,32). As one of the major cardiovascular diseases, AF showed tendencies with regard to alcohol consumption similar to those of other cardiovascular diseases. Among middle-aged patients with diabetes, mild alcohol consumption did not seem to be associated with an increased risk of AF, but excessive alcohol consumption was associated with an increased risk of AF (33). Consistently, our findings showed that frequent drinking and heavy alcohol consumption led to a significantly higher risk of AF development, whereas less frequent or mild alcohol consumption did not lead to a higher risk of AF development. However, the association between mild alcohol consumption and dose-dependent risk of AF has been reported in several large meta-analyses (34–36). In the most recent meta-analysis of seven prospective studies with 79,019 men and women, Larsson et al. (36) reported that all studies demonstrated a linear dose-dependent pattern of association between the risk of AF and alcohol consumption, even a mild amount, with an overall 8% increase in the risk of AF per 1 drink/day increment in alcohol consumption. Additional studies are needed to determine the association between mild alcohol consumption and the risk of AF in patients with cardiovascular diseases, leading to a higher risk of AF.
Our findings suggest that regular alcohol consumption is a potentially modifiable risk factor for AF in patients with T2DM. For patients with diabetes, lifestyle modification is an important and effective nonpharmaceutical strategy to prevent cardiovascular disease, as much as controlling serum glucose levels with medication. Alcohol abstinence should be considered part of the overall management strategy for preventing AF development in patients with T2DM (37). Indeed, lifestyle modification (addressing excessive alcohol consumption) is part of the Atrial fibrillation Better Care (ABC) pathway for holistic AF care, which is advocated in the new 2020 European Society of Cardiology guidelines (38). The ABC pathway has been shown to improve adverse clinical outcomes in AF populations (39).
There are limitations to the current study. First, this was an observational study, which did not allow ascertainment of causality. However, we tried to show the time-sequential changes to demonstrate the cause-effect associations of alcohol consumption behavior change with data from the serial health examination program database. Second, this study was conducted in the Korean population; it is unclear whether the results could be extrapolated to the non-Asian population. Considering that ADH1B*2 variant alleles are predominant among East Asians, the effect of abstinence on the risk of AF would be more prominent (40). Therefore, it may be necessary to conduct a large-scale multiethnic study, including various high-risk populations, to generalize the effects of alcohol abstinence in preventing AF development. Finally, this study, based on the NHIS database, did not provide detailed information on the characteristics of patients with T2DM, such as serial HbA1c levels, genetic mutations, and combined diabetes-related complications.
In summary, in patients with newly diagnosed T2DM, alcohol abstinence in those with moderate to heavy alcohol consumption before diagnosis was associated with a low risk of AF development. Lifestyle modification, such as alcohol abstinence, in patients newly diagnosed with T2DM should be recommended to reduce the risk of AF.
Article Information
Funding. This work was supported by a Korea Medical Device Development Fund grant funded by the Korean government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health and Welfare, and the Ministry of Food and Drug Safety) (project 202013B14) and by the Korea National Research Foundation funded by the Ministry of Education, Science and Technology (grant 2020R1F1A106740).
Duality of Interest. E.-K.C. reports research grants from Bayer, Bristol-Myers Squibb/Pfizer, Biosense Webster, Chong Kun Dang, Daiichi-Sankyo, Samjinpharm, Sanofi, Seers Technology, Skylabs, and Yuhan. G.Y.H.L. reports consultancy for Bayer/Janssen, Bristol-Myers Squibb/Pfizer, Medtronic, Boehringer Ingelheim, Novartis, Verseon, and Daiichi-Sankyo and speakers bureau for Bayer, Bristol-Myers Squibb/Pfizer, Medtronic, Boehringer Ingelheim, and Daiichi-Sankyo. No fees were directly received personally. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. Y.-j.C., K.-D.H., E.-K.C., and S.-R.L. were responsible for conceptualization and methodology. Y.-j.C., K.-D.H., and J.-H.J. curated data. Y.-j.C. visualized and wrote the original draft. K.-D.H. and J.-H.J. performed the formal analysis. E.-K.C. was responsible for funding acquisition, project administration, and supervision. E.-K.C., S.O., and G.Y.H.L. were responsible for reviewing and editing the manuscript. E.-K.C. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Y.-j.C. and K.-D.H. contributed equally to this study.
This article contains supplementary material online at https://doi.org/10.2337/figshare.13956677.
References
- 1. Lee SR, Choi EK, Han KD, Cha MJ, Oh S. Trends in the incidence and prevalence of atrial fibrillation and estimated thromboembolic risk using the CHA2DS2-VASc score in the entire Korean population. Int J Cardiol 2017;236:226–231 [DOI] [PubMed] [Google Scholar]
- 2. Kim MH, Johnston SS, Chu BC, Dalal MR, Schulman KL. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes 2011;4:313–320 [DOI] [PubMed] [Google Scholar]
- 3. Balakumar P, Maung-U K, Jagadeesh G. Prevalence and prevention of cardiovascular disease and diabetes mellitus. Pharmacol Res 2016;113:600–609 [DOI] [PubMed] [Google Scholar]
- 4. Aune D, Feng T, Schlesinger S, Janszky I, Norat T, Riboli E. Diabetes mellitus, blood glucose and the risk of atrial fibrillation: a systematic review and meta-analysis of cohort studies. J Diabetes Complications 2018;32:501–511 [DOI] [PubMed] [Google Scholar]
- 5. Huxley RR, Misialek JR, Agarwal SK, et al. Physical activity, obesity, weight change, and risk of atrial fibrillation: the Atherosclerosis Risk in Communities study. Circ Arrhythm Electrophysiol 2014;7:620–625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Heeringa J, Kors JA, Hofman A, van Rooij FJ, Witteman JC. Cigarette smoking and risk of atrial fibrillation: the Rotterdam study. Am Heart J 2008;156:1163–1169 [DOI] [PubMed] [Google Scholar]
- 7. Chamberlain AM, Agarwal SK, Folsom AR, et al. Smoking and incidence of atrial fibrillation: results from the Atherosclerosis Risk in Communities (ARIC) study. Heart Rhythm 2011;8:1160–1166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Klatsky AL. Alcohol and cardiovascular diseases: where do we stand today? J Intern Med 2015;278:238–250 [DOI] [PubMed] [Google Scholar]
- 9. Whitfield JB, Heath AC, Madden PAF, Pergadia ML, Montgomery GW, Martin NG. Metabolic and biochemical effects of low-to-moderate alcohol consumption. Alcohol Clin Exp Res 2013;37:575–586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Voskoboinik A, Kalman JM, De Silva A, et al. Alcohol abstinence in drinkers with atrial fibrillation. N Engl J Med 2020;382:20–28 [DOI] [PubMed] [Google Scholar]
- 11. Guppy LJ, Crabbe JC, Littleton JM. Time course and genetic variation in the regulation of calcium channel antagonist binding sites in rodent tissues during the induction of ethanol physical dependence and withdrawal. Alcohol Alcohol 1995;30:607–615 [PubMed] [Google Scholar]
- 12. Husain K, Ansari RA, Ferder L. Alcohol-induced hypertension: mechanism and prevention. World J Cardiol 2014;6:245–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sidhu K, Tang A. Modifiable risk factors in atrial fibrillation: the role of alcohol, obesity, and sleep apnea. Can J Cardiol 2017;33:947–949 [DOI] [PubMed] [Google Scholar]
- 14. Choi EK. Cardiovascular research using the Korean National Health Information Database. Korean Circ J 2020;50:754–772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lee SS, Ae Kong K, Kim D, et al. Clinical implication of an impaired fasting glucose and prehypertension related to new onset atrial fibrillation in a healthy Asian population without underlying disease: a nationwide cohort study in Korea. Eur Heart J 2017;38:2599–2607 [DOI] [PubMed] [Google Scholar]
- 16. Tadic M, Cuspidi C. Type 2 diabetes mellitus and atrial fibrillation: from mechanisms to clinical practice. Arch Cardiovasc Dis 2015;108:269–276 [DOI] [PubMed] [Google Scholar]
- 17. De Sensi F, De Potter T, Cresti A, Severi S, Breithardt G. Atrial fibrillation in patients with diabetes: molecular mechanisms and therapeutic perspectives. Cardiovasc Diagn Ther 2015;5:364–373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kato T, Yamashita T, Sekiguchi A, et al. What are arrhythmogenic substrates in diabetic rat atria? J Cardiovasc Electrophysiol 2006;17:890–894 [DOI] [PubMed] [Google Scholar]
- 19. Tadic M, Ilic S, Cuspidi C, et al. Left and right atrial phasic function and deformation in untreated patients with prediabetes and type 2 diabetes mellitus. Int J Cardiovasc Imaging 2015;31:65–76 [DOI] [PubMed] [Google Scholar]
- 20. Otake H, Suzuki H, Honda T, Maruyama Y. Influences of autonomic nervous system on atrial arrhythmogenic substrates and the incidence of atrial fibrillation in diabetic heart. Int Heart J 2009;50:627–641 [DOI] [PubMed] [Google Scholar]
- 21. Echouffo-Tcheugui JB, Shrader P, Thomas L, et al. Care patterns and outcomes in atrial fibrillation patients with and without diabetes: ORBIT-AF registry. J Am Coll Cardiol 2017;70:1325–1335 [DOI] [PubMed] [Google Scholar]
- 22. Lip GYH. The ABC pathway: an integrated approach to improve AF management. Nat Rev Cardiol 2017;14:627–628 [DOI] [PubMed] [Google Scholar]
- 23. Slater ME, Alpert HR. Apparent per capita alcohol consumption: national, state, and regional trends, 1977–2016 (surveillance report no. 115). Accessed December 2020. Available from https://pubs.niaaa.nih.gov/publications/surveillance115/CONS18.htm
- 24. Hong JW, Noh JH, Kim DJ. The prevalence of and factors associated with high-risk alcohol consumption in Korean adults: the 2009-2011 Korea National Health and Nutrition Examination Survey. PLoS One 2017;12:e0175299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Steiner JL, Crowell KT, Lang CH. Impact of alcohol on glycemic control and insulin action. Biomolecules 2015;5:2223–2246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. van de Borne P, Mark AL, Montano N, Mion D, Somers VK. Effects of alcohol on sympathetic activity, hemodynamics, and chemoreflex sensitivity. Hypertension 1997;29:1278–1283 [DOI] [PubMed] [Google Scholar]
- 27. Zagrosek A, Messroghli D, Schulz O, Dietz R, Schulz-Menger J. Effect of binge drinking on the heart as assessed by cardiac magnetic resonance imaging. JAMA 2010;304:1328–1330 [DOI] [PubMed] [Google Scholar]
- 28. McManus DD, Yin X, Gladstone R, et al. Alcohol consumption, left atrial diameter, and atrial fibrillation. J Am Heart Assoc 2016;5:e004060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Voskoboinik A, Costello BT, Kalman E, et al. Regular alcohol consumption is associated with impaired atrial mechanical function in the atrial fibrillation population: a cross-sectional MRI-based study. JACC Clin Electrophysiol 2018;4:1451–1459 [DOI] [PubMed] [Google Scholar]
- 30. Voskoboinik A, Wong G, Lee G, et al. Moderate alcohol consumption is associated with atrial electrical and structural changes: insights from high-density left atrial electroanatomic mapping. Heart Rhythm 2019;16:251–259 [DOI] [PubMed] [Google Scholar]
- 31. Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 2011;342:d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mostofsky E, Chahal HS, Mukamal KJ, Rimm EB, Mittleman MA. Alcohol and immediate risk of cardiovascular events: a systematic review and dose-response meta-analysis. Circulation 2016;133:979–987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Liang Y, Mente A, Yusuf S, et al.; ONTARGET and TRANSCEND Investigators . Alcohol consumption and the risk of incident atrial fibrillation among people with cardiovascular disease. CMAJ 2012;184:E857–E866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kodama S, Saito K, Tanaka S, et al. Alcohol consumption and risk of atrial fibrillation: a meta-analysis. J Am Coll Cardiol 2011;57:427–436 [DOI] [PubMed] [Google Scholar]
- 35. Samokhvalov AV, Irving HM, Rehm J. Alcohol consumption as a risk factor for atrial fibrillation: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil 2010;17:706–712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Larsson SC, Drca N, Wolk A. Alcohol consumption and risk of atrial fibrillation: a prospective study and dose-response meta-analysis. J Am Coll Cardiol 2014;64:281–289 [DOI] [PubMed] [Google Scholar]
- 37. Gorenek B, Pelliccia A, Benjamin EJ, et al. European Heart Rhythm Association (EHRA)/European Association of Cardiovascular Prevention and Rehabilitation (EACPR) position paper on how to prevent atrial fibrillation endorsed by the Heart Rhythm Society (HRS) and Asia Pacific Heart Rhythm Society (APHRS). Europace 2017;19:190–225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hindricks G, Potpara T, Dagres N, et al.; ESC Scientific Document Group . 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS) [published corrections appear in Eur Heart J 2021;42:507 and Eur Heart J 2021;42:546-547]. Eur Heart J 2021;42:373–498 [DOI] [PubMed] [Google Scholar]
- 39. Guo Y, Lane DA, Wang L, et al.; mAF-App II Trial Investigators . Mobile health technology to improve care for patients with atrial fibrillation. J Am Coll Cardiol 2020;75:1523–1534 [DOI] [PubMed] [Google Scholar]
- 40. Eng MY, Luczak SE, Wall TL. ALDH2, ADH1B, and ADH1C genotypes in Asians: a literature review. Alcohol Res Health 2007;30:22–27 [PMC free article] [PubMed] [Google Scholar]