The impact of the coronavirus disease 2019 (COVID-19) pandemic on amputation incidence in whole populations with diabetes is unknown. Previous reports are restricted to small cohorts from single specialist centers showing varying outcomes, including greater ulcer severity on presentation (1) and increased amputations (2). We aimed to carry out a population-based assessment of lower-limb major amputation, minor amputation, and revascularization procedure numbers and incidences during the first wave of the COVID-19 pandemic in England, covering the period March to June 2020, compared with equivalent time periods in 2017–2019. We also examined data 4 months following the first wave to assess if delayed presentations resulted in a rebound leading to higher than usual amputation incidence.
The Secondary Uses Service data set contains data on inpatient care for all admissions to hospitals in England and was used to identify all major and minor lower-limb amputation and revascularization procedures in people with diabetes in England between 1 January 2017 and 31 October 2020, using all discharges from the hospital up to 31 December 2020. If more than one procedure was performed, all were counted for their respective analyses. For each year, the total number of people with diabetes aged 18 years and over was obtained from the National Diabetes Audit. Age, sex, ethnicity, and deprivation were identified as potential confounding factors. Due to geographical variations in population exposure to severe acute respiratory syndrome coronavirus 2 across England, region was also included as a covariate. To estimate incidence rate ratios (IRRs) for the 2020 versus 2017–2019 periods, we fitted negative binomial regression models for each outcome. We have recently outlined the legal bases for the data collections and linkages (3).
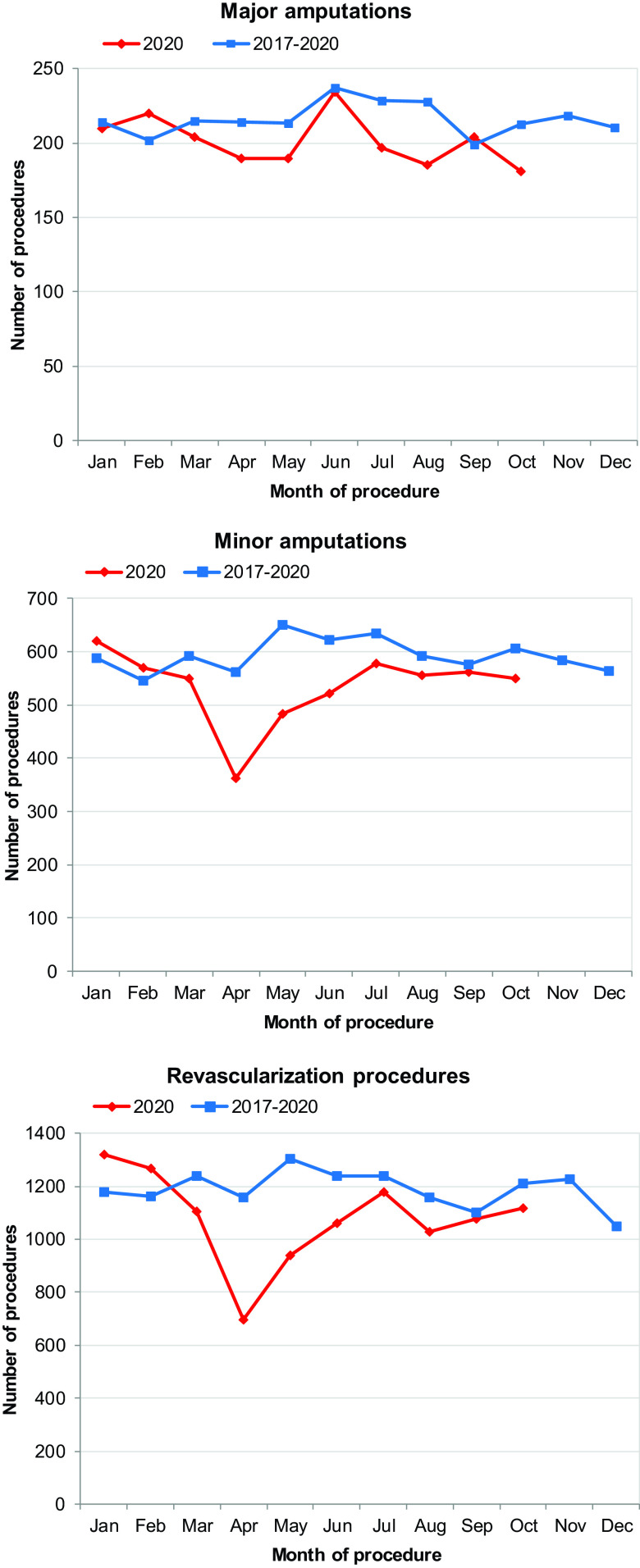
The numbers of procedures performed in 2020 compared with the mean numbers of procedures for equivalent time periods over the past 3 years are shown in Fig. 1. During March to June 2020, 818 major amputations, 1,918 minor amputations, and 3,801 revascularization procedures were performed on people with diabetes in England. Compared with means from the equivalent time periods in 2017–2019, major amputations were 7% (95% CI −0.7 to 14) lower, minor amputations were 21% (17–25) lower, and revascularization procedures were 23% (20–26) lower. There was no subsequent rebound in numbers of procedures from July to October 2020 (Fig. 1).
Figure 1.
Number of lower-limb major and minor amputation and revascularization procedures in people with diabetes between January 2017 and October 2020 in England by month of procedure.
Incidence rates per 10,000 people with diabetes between March and June 2020 were 2.4 (95% CI 2.2–2.6) for major amputations, 5.6 (5.4–5.9) for minor amputations, and 11.2 (10.8–11.5) for revascularization procedures, all significantly lower than the equivalent time periods over the last 3 years, corresponding to IRRs of 0.84 (95% CI 0.78–0.91), 0.72 (0.68–0.75), and 0.70 (0.67–0.72), respectively.
For all procedures during March–June 2020, there were higher proportions of men, those of white ethnicity, and those from the most deprived quintile, similar to previous years. Over the past 3 years, rates for all procedures increased with age, but in 2020, there were declines in rates for major amputations from age 65 years, revascularization procedures from 45 years, and minor amputations for all ages.
Regression analysis showed that, compared with equivalent time periods over the last 3 years, rates of major amputations, minor amputations, and revascularization procedures during March–June 2020 remained significantly lower after adjustment for age, sex, ethnicity, deprivation, and region, with adjusted IRRs of 0.86 (95% CI 0.78–0.93), 0.73 (0.68–0.78), and 0.75 (0.70–0.80), respectively.
This whole-population study in England suggests significant reductions in rates of lower-limb major and minor amputation and revascularization procedures and significant reductions in numbers of minor amputations and revascularization procedures in those with diabetes during the first wave of the COVID-19 pandemic compared with those over the same periods in the previous 3 years. The reduction in major amputation incidence was predominantly confined to those over age 65 years, so the competing end point of COVID-19–related mortality may have contributed (3). Lower minor amputation incidence may have resulted from lower ulcer incidence due to reduced ambulation in the context of home confinement, although no reliable data on ulcer incidence for the whole of England are available. The ecological nature of our study did not allow the assessment of associations between study outcomes and patient characteristics at an individual level (e.g., changes in health care–seeking behavior during lockdown) or analysis of the risk of amputation and revascularization procedures while accounting for the proximal risk of dying from COVID-19. We have only included data on procedures undertaken until the end of October 2020, so it is currently unclear whether rates will return to usual levels or whether delayed presentations, through fear of contagion or difficult access to health care during the pandemic (4,5), will result in a subsequent rebound.
Article Information
Duality of Interest. J.V. is the National Clinical Director for Diabetes and Obesity at NHS England & Improvement. P.K. is a National Specialty Advisor for diabetes and obesity at NHS England & Improvement. B.Y. is Clinical Lead of the National Diabetes Audit for England and Wales and a Trustee of Diabetes UK. K.K. has acted as a consultant and speaker for Novartis, Novo Nordisk, Sanofi, Lilly, and Merck Sharp & Dohme; has received grants in support of investigator and investigator-initiated trials from Novartis, Novo Nordisk, Sanofi, Lilly, Merck Sharp & Dohme, Pfizer, and Boehringer Ingelheim; has served on advisory boards for Novo Nordisk, Sanofi, Lilly, and Merck Sharp & Dohme. K.D. has acted as a consultant to Lexicon Pharmaceuticals and Sanofi Diabetes and has had personal fees from Novo Nordisk and Frazier Healthcare. F.G. has received honoraria for educational events from Novo Nordisk, AstraZeneca, Urgo, Lilly, Sanofi, and MiMedX; sponsorship for meeting attendance from Sanofi, Novo Nordisk, and AstraZeneca; and research funding from Reapplix Aps and NuVision. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. J.V. conceived the study. E.B., E.P.V., and S.V. managed the data and did the statistical analysis. All authors collaborated in interpretation of the results and drafting the report. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. J.V. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article is part of a special article collection available at https://care.diabetesjournals.org/collection/diabetes-and-COVID19.
References
- 1. Liu C, You J, Zhu W, et al. The COVID-19 outbreak negatively affects the delivery of care for patients with diabetic foot ulcers. Diabetes Care 2020. 43:e125–e126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Caruso P, Longo M, Signoriello S, et al. Diabetic foot problems during the COVID-19 pandemic in a tertiary care center: the emergency among the emergencies. Diabetes Care 2020;43:e123–e124 [DOI] [PubMed] [Google Scholar]
- 3. Barron E, Bakhai C, Kar P, et al. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. Lancet Diabetes Endocrinol 2020;8:813–822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tam CF, Cheung KS, Lam S, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes 2020;13:e006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ball S, Banerjee A, Berry C, et al. The 4C Initiative (clinical care for cardiovascular disease in the COVID-19 pandemic)–monitoring the indirect impact of the coronavirus pandemic on services for cardiovascular diseases in the UK. medRxiv. 11 July 2020 [preprint]. DOI: 10.1101/2020.07.10.20151118 [Google Scholar]