Abstract
OBJECTIVE
Cotadutide, a dual GLP-1 and glucagon receptor agonist, is under development for nonalcoholic steatohepatitis (NASH) and chronic kidney disease with type 2 diabetes. The effects of cotadutide on hepatic and metabolic parameters were evaluated in participants with overweight/obesity and type 2 diabetes.
RESEARCH DESIGN AND METHODS
In this phase 2b study, 834 adults with BMI ≥25 kg/m2 and type 2 diabetes inadequately controlled with metformin (glycated hemoglobin A1c [HbA1c] of 7.0%–10.5% [53–91 mmol/mol]) were randomized to double-blind cotadutide 100 μg (n = 100), 200 μg (n = 256), or 300 μg (n = 256); placebo (n = 110); or open-label liraglutide 1.8 mg (n = 110)—all administered subcutaneously. Coprimary end points were changes in HbA1c and body weight at week 14. The originally randomized interventions were continued to week 54. Liver damage biomarkers and liver fibrosis algorithms were assessed.
RESULTS
Cotadutide significantly decreased HbA1c and body weight at weeks 14 and 54 versus placebo (all P < 0.001). Improvements in lipid profile, AST and ALT levels, propeptide of type III collagen level, fibrosis-4 index, and nonalcoholic fatty liver disease fibrosis score were observed with cotadutide 300 μg versus placebo, but not with liraglutide. Weight loss with cotadutide 200 μg was similar to that with liraglutide 1.8 mg and greater with cotadutide 300 μg versus liraglutide 1.8 mg. The most common adverse events with cotadutide (nausea, 35%; vomiting, 17%) decreased over time.
CONCLUSIONS
Cotadutide treatment for 54 weeks improved glycemic control and weight loss in participants with overweight/obesity and type 2 diabetes. Ad hoc analyses demonstrated improvements in hepatic parameters and support further evaluation of cotadutide in NASH.
Introduction
Approximately 70% of people with type 2 diabetes, and 93% of people with severe obesity who are candidates for weight reduction procedures or surgeries, have nonalcoholic fatty liver disease (NAFLD) (1–3). In patients with NAFLD, ectopic fat accumulation in the liver contributes to increased insulin resistance and lipotoxicity (4–6). The pathology of NAFLD can progress further to nonalcoholic steatohepatitis (NASH), advanced fibrosis, and end-stage cirrhosis (7). Moreover, in people with type 2 diabetes, NAFLD and NASH may contribute to the progression of cardiovascular disease, kidney disease, and other complications (8–12). Hence, a significant unmet need exists among patients with type 2 diabetes and NASH for treatments that simultaneously improve liver health, reduce cardiovascular and renal disease, provide glycemic control, and promote weight loss.
Treatment with glucagon-like peptide 1 (GLP-1) receptor agonists has been shown to improve glycemic control (13), delay gastric emptying, and induce weight loss in people with type 2 diabetes (14,15). The GLP-1 receptor monoagonist liraglutide is indicated for the treatment of obesity in many parts of the world (16). In phase 2 and phase 3 clinical trials, liraglutide reduced body weight by 6–8% (17,18). Additionally, the GLP-1 receptor agonist semaglutide was more effective at inducing weight loss in a head-to-head phase 2 trial with liraglutide, as mean body weight was reduced 6.0–13.8% compared with 7.8% with liraglutide (18).
Treatment with GLP-1 receptor monoagonists may also improve liver biomarkers (19). Liraglutide, semaglutide, and exenatide treatment all improved liver biomarkers (19–22), and liraglutide decreased histological inflammation in patients with biopsy-proven NASH (23). Some studies, however, did not demonstrate any marked improvement in liver biomarkers after liraglutide treatment, or the improvements were not sustained (19–21,23). Two years of treatment with semaglutide significantly reduced ALT and hs-CRP levels in patients with obesity and/or type 2 diabetes, although significance was lost after adjustment for changes in body weight (24).
Cotadutide (MEDI0382), a dual GLP-1 and glucagon receptor agonist, is under development for type 2 diabetes and NASH. The ratio of GLP-1 and glucagon activity was optimized to achieve a maximally beneficial overall effect from the agonism of each receptor. In animal models, the beneficial effects of glucagon include reduced liver lipogenesis, inflammation, and fibrosis, together with improved liver mitochondrial function (25,26). The robust improvements in NASH and fibrosis scores in preclinical NASH mouse models after cotadutide treatment were significantly greater than after treatment with the GLP-1 monoagonist liraglutide (26). In humans, the glucagon receptor is highly expressed in liver and kidney tissue, suggesting that glucagon plays a role in hepatic and renal physiology (27).
In early phase 2a trials, cotadutide treatment resulted in robust and consistent glycemic control, increased postprandial insulin levels, and weight loss in participants with overweight or obesity and who have type 2 diabetes (28,29). An exploratory phase 2a analysis using MRI demonstrated that cotadutide was associated with significant reductions in hepatic fat compared with placebo in participants with overweight or obesity and who have type 2 diabetes (30).
We report results from a 54-week phase 2b study evaluating the clinical utility of cotadutide in participants with overweight or obesity and type 2 diabetes. Safety and effects of cotadutide on metabolic and hepatic parameters were assessed.
Research Design and Methods
Study Design and Procedures
This was a randomized, parallel-group, double-blind, placebo-controlled, phase 2b study of cotadutide with an open-label, active comparator, liraglutide (ClinicalTrials.gov identifier NCT03235050). The study was designed by AstraZeneca and conducted at 120 sites in eight countries: Bulgaria, Canada, Czech Republic, Germany, Mexico, Russia, Slovakia, and the U.S. The relevant independent ethics committees or institutional review boards approved the protocol prior to initiation of the study, which was conducted in accordance with the ethics principles outlined by the Declaration of Helsinki, the International Council for Harmonisation Guidance for Good Clinical Practice, and local laws, regulations, and organizations. All participants provided written informed consent prior to participating in the study.
Eligible participants were aged ≥18 years, had a BMI ≥25 kg/m2, were diagnosed with type 2 diabetes and inadequate blood glucose control (glycated hemoglobin A1c [HbA1c] level 7.0–10.5% [53–91 mmol/mol], inclusive), and had AST and ALT levels <3 times the upper limit of normal. Participants were excluded if they had received a GLP-1 receptor monoagonist within the previous 30 days or five half-lives of the drug (whichever was longer), received daily subcutaneous insulin for >2 weeks within 90 days prior to screening, or were currently participating in another interventional study. Participants with alcohol dependence were also excluded from this study.
Participants were randomly assigned (overall ratio 4:9:9:4:4) to receive once-daily subcutaneous injections of cotadutide at 100 µg, 200 µg, or 300 µg; liraglutide 1.8 mg; or placebo (Fig. 1A). Administration of cotadutide or placebo with single-use prefilled syringes was double-blind; liraglutide administration, with commercially available multiuse 3-mL pen injectors, was open-label. Liraglutide was initiated at a dose of 0.6 mg and uptitrated by an additional 0.6 mg weekly until a daily dose of 1.8 mg was reached. Cotadutide dosing was initiated at 100 μg once daily in each cohort and increased weekly by 100 μg where required. Assignment to treatment groups was determined by a computer-generated randomized sequence with use of interactive web response systems and interactive voice-response systems. Randomization was stratified with respect to screening HbA1c level (≤8% or >8% [64 mmol/mol]). Study drugs were administered independently of meals with no restrictions on time of day for dosing. The study had a run-in period of 2 weeks (on a background of stable metformin treatment that was maintained for the study duration), a 14-week treatment period (primary analysis), a minimum 40-week extension of the treatment period, and a 4-week follow-up period (Fig. 1A).
Figure 1.
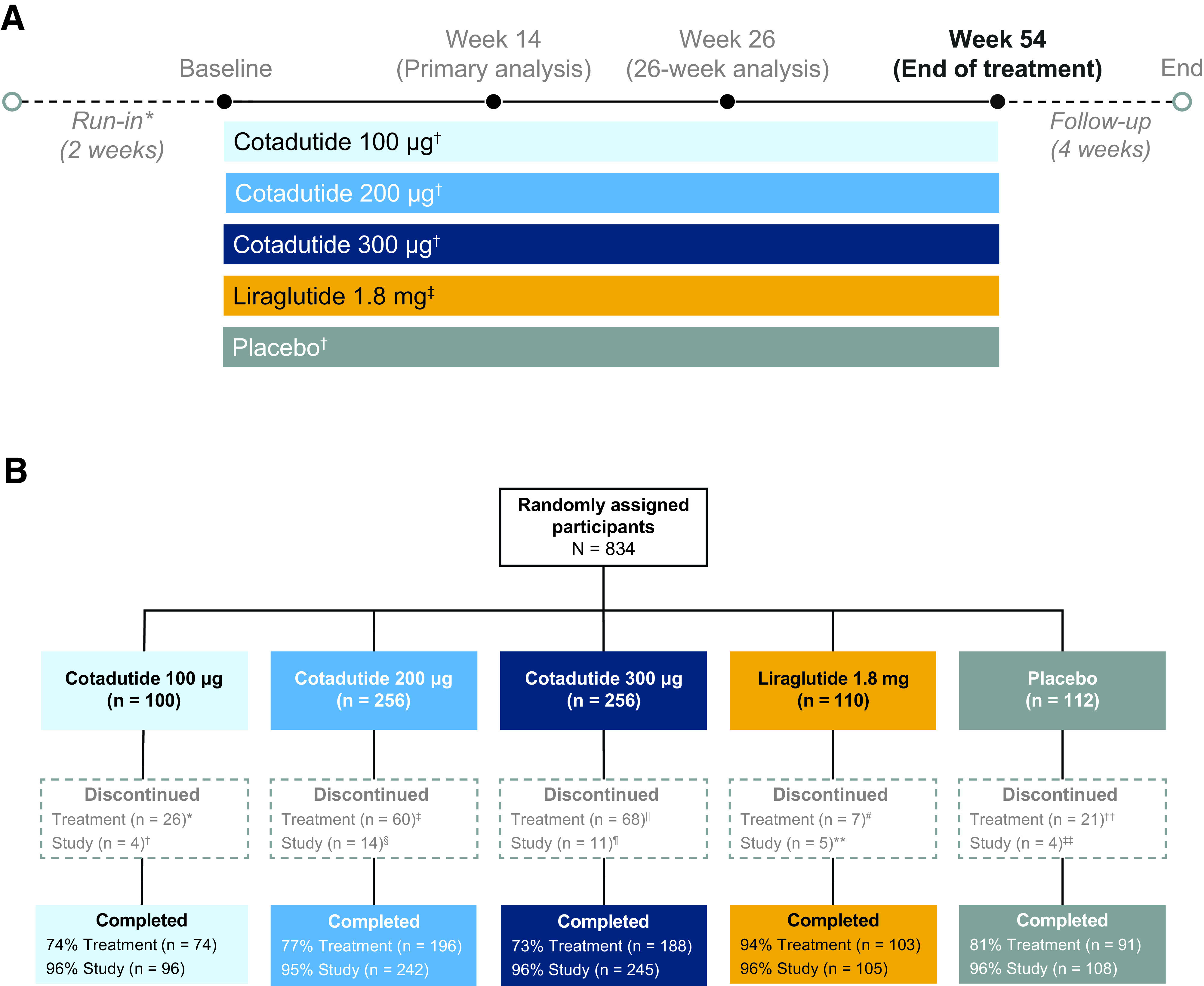
Study design and participant disposition. A: Cotadutide (double blind) and liraglutide (open-label) were given as once-daily subcutaneous injections. *Run-in was performed on a background of stable metformin treatment, which was maintained for the duration of the study. †Double-blinded, once-daily, subcutaneous injections. ‡Open-label, once-daily, subcutaneous injections. B: Participant disposition. *Due to adverse event (n = 13), lack of therapeutic response (n = 1), protocol violation (n = 1), subject decision (n = 7), other (n = 3), lost to follow-up (n = 1). †Due to adverse event (n = 1), lost to follow-up (n = 1), subject decision (n = 2). ‡Due to adverse event (n = 39), condition under investigation worsened (n = 1), lack of therapeutic response (n = 3), subject decision (n = 16), other (n = 1). §Due to adverse event (n = 4), death (n = 2), lost to follow-up (n = 2), subject decision (n = 5), other (n = 1). ǁDue to adverse event (n = 55), subject decision (n = 13). ¶Due to adverse event (n = 1), death (n = 1), subject decision (n = 7), other (n = 2). #Due to adverse event (n = 2), subject decision (n = 4), lost to follow-up (n = 1). **Due to subject decision (n = 2), lost to follow-up (n = 2) other (n = 1). ††Due to adverse event (n = 5), condition under investigation worsened (n = 1), lack of therapeutic response (n = 4), subject decision (n = 10), development of study-specific discontinuation criteria (n = 1). ‡‡Due to subject decision (n = 3), lost to follow-up (n = 1).
Study End Points
The coprimary end points included change from baseline to week 14 in HbA1c levels and percent change in body weight with cotadutide versus placebo. Secondary efficacy end points included change in HbA1c levels, proportion of participants achieving target HbA1c levels <7.0% (53 mmol/mol), absolute change in body weight, percent change in body weight, proportion of participants achieving weight loss ≥5% and ≥10%, and proportion of participants rescued or discontinued for lack of glycemic control. These secondary end points were assessed at 26 and 54 weeks.
Exploratory end points included waist circumference, fasting plasma glucose levels, glucose and insulin HOMA scores, and the proportion of participants achieving target HbA1c levels <6.5% (48 mmol/mol). Parameters for hepatocyte damage and algorithms reflecting liver fat and liver fibrosis were assessed ad hoc and included change from baseline to week 54 in ALT and AST levels, γ-glutamyl transpeptidase (GGT) level, fibrosis-4 (FIB-4) index, and NAFLD fibrosis score (NFS). Changes in ALT and AST levels by baseline quartile were assessed ad hoc. Propeptide of type III collagen (PRO-C3) levels were also assessed ad hoc in the cotadutide 300 µg, liraglutide 1.8 mg, and placebo groups only. Fasting-state lipid parameters were assessed and included changes in levels of LDL cholesterol, HDL cholesterol, non-HDL cholesterol, and triglycerides. Safety assessments included the incidence of treatment-emergent adverse events (TEAEs) as defined by the Medical Dictionary for Regulatory Activities (MedDRA) (version 22.0) and change in pulse rate. The development of anti-drug antibodies was assessed as a secondary end point. Diastolic and systolic blood pressure measurements were assessed as exploratory end points and rate-pressure product was assessed ad hoc.
Based on the time line of the effects of cotadutide reported in an earlier study (29), it was considered that a study duration of 12 weeks would be adequate for discriminating the dose-dependent efficacy of the drug with regard to glycemic control and weight loss. The time point for the coprimary analysis was 14 weeks to allow sufficient time for dose uptitration. The study had an additional extension period (to 54 weeks) for assessment of the durability of the initial efficacy and long-term efficacy and safety results.
The coprimary end points of change in HbA1c and percent change in body weight were selected for exploration of the impact of a dual GLP-1 and glucagon receptor agonist on each of these end points, as well as for assessment of efficacy.
Statistical Analyses
A sample size of 750 participants was planned (cotadutide 100 µg, n = 100; cotadutide 200 µg, n = 225; cotadutide 300 µg, n = 225; liraglutide 1.8 mg, n = 100; placebo, n = 100). With this sample size, we factored in an anticipated dropout rate of ∼10% by 14 weeks. The sample size provided a >95% power to detect a 0.9% change from baseline in HbA1c levels with cotadutide versus placebo, a two-sided significance level of 5%. This sample size also provided >95% power to detect a difference of 4% in weight loss from baseline to week 14 with cotadutide versus liraglutide or placebo. Statistical comparisons were performed at the 0.05 significance level (two sided).
Secondary efficacy analyses were based on the per-protocol population, which included only participants who did not discontinue the study drug during the relevant treatment period and excluded those with important protocol violations. Primary and secondary efficacy end points were initially planned to be assessed using the intent-to-treat (ITT) population. The ITT population was defined as those participants who received any study drug and were analyzed according to the randomly assigned treatment group. Analyses performed on the per-protocol population are presented to address the confounding effect of treatment adherence owing to the high proportion of treatment discontinuations. The as-treated population was defined as those participants who received any study drug and were analyzed according to the treatment received. All safety analyses were performed in the as-treated population. Additional ad hoc analyses were performed in the per-protocol population. For the ad hoc analyses, all P values were nominal.
Primary efficacy end points were analyzed using ANCOVA with last-observation-carried-forward imputation for missing data and adjusted for treatment and measurement at baseline. For the end point of weight loss, the strata at screening for HbA1c level (≤8% or >8% [64 mmol/mol]) were added as covariates. Secondary efficacy end points of changes in body weight and HbA1c levels at 54 weeks were analyzed by ANCOVA model with last-observation-carried-forward imputation, including fixed effects and covariates of treatment, baseline measurement, and strata of screening for HbA1c (≤8% or >8%; except for HbA1c-related analyses). Secondary proportion-related end points were analyzed by a logistic regression model with similar fixed effects and covariates (ITT population). Descriptive statistics were used for safety analyses. Statistical analyses were performed with SAS software, version 9.4 (SAS Institute, Cary, NC).
For further exploration of the relationship between the change in weight and the change in ALT, a post hoc analysis was performed using percentage weight loss as a predictor of percentage ALT reduction to fit a least squares (LS) regression line for each treatment arm.
Data and Resource Availability
The data sets generated during or analyzed during the current study are not publicly available but could be obtained from the corresponding author on reasonable request.
Results
Between 2 August 2017 and 14 June 2019, 834 participants were randomly assigned to cotadutide, liraglutide, or placebo, and 78.2% (652 of 834) completed treatment up to 54 weeks. The proportion of participants who completed treatment with liraglutide (93.6% [103 of 110]) was higher in comparison with cotadutide (74.8% [458 of 612]) or placebo (81.3% [91 of 112]) (Fig. 1B). Participant demographics and baseline characteristics were generally well balanced across all treatment groups (Supplementary Table 1). Statin use at baseline was similar across all treatment groups, ranging from 39% to 48% (Supplementary Table 1).
The coprimary end points were met. Significant decreases from baseline to week 14 in LS means (95% CI) for HbA1c levels were observed with cotadutide 100 µg (–1.11 [–1.30, –0.93]), 200 µg (–1.32 [–1.44, –1.21]), and 300 µg (–1.26 [–1.38, –1.14]) and liraglutide 1.8 mg (–1.30 [–1.45, –1.14]) versus placebo (–0.23 [–0.40, –0.07]; all P < 0.001). No differences in HbA1c levels were observed between the cotadutide dose groups and the liraglutide group from baseline to 14 weeks. Significant decreases from baseline to week 14 in percent change in body weight were observed with cotadutide 100 µg (LS mean [95% CI] –2.98 [–3.87, –2.09]), 200 µg (–3.67 [–4.22, –3.13]), and 300 µg (–5.01 [–5.57, –4.45]) and liraglutide 1.8 mg (–3.44 [–4.20, –2.68]) versus placebo (–0.74 [–1.56, 0.07]; all P < 0.001). A significant difference in body weight from baseline to week 14 was observed with cotadutide 300 µg versus liraglutide (P = 0.001).
At 54 weeks, significant decreases in HbA1c levels were observed with all tested doses of cotadutide versus placebo (all P < 0.001) (Fig. 2A). No differences in HbA1c levels were observed between the cotadutide dose groups and the liraglutide group (Fig. 2A). Significant decreases in percent body weight were observed with all three tested doses of cotadutide versus placebo (all P < 0.001) (Fig. 2B). A significant decrease was also observed in percentage change in body weight at week 54 with cotadutide 300 µg versus liraglutide (P = 0.009) but not with lower doses of cotadutide (Fig. 2B).
Figure 2.
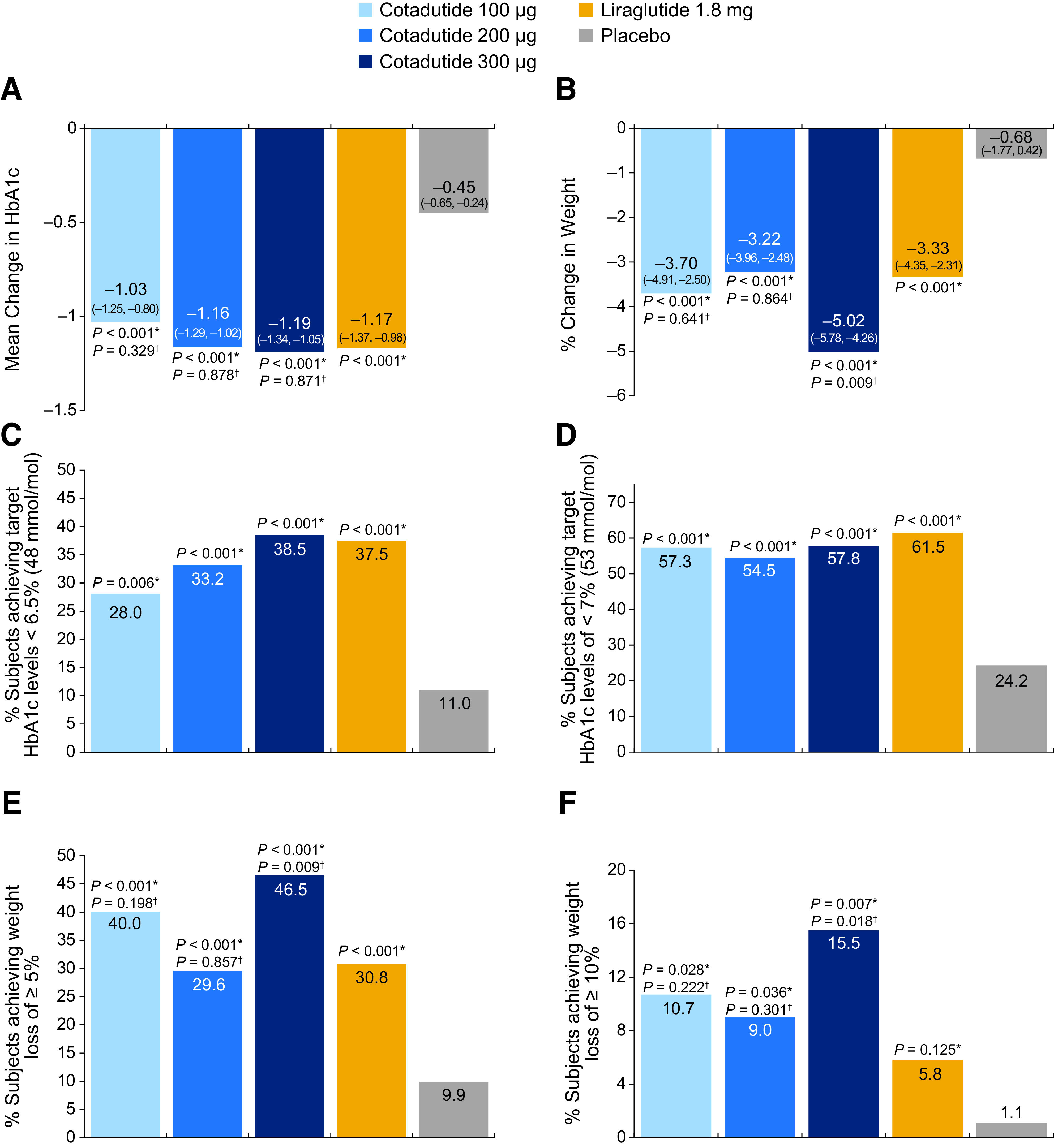
Changes in glycemic and body weight outcomes from baseline to week 54. A: Change in HbA1c levels. Data are LS means (95% CI). B: Percentage change in body weight. Data are LS means (95% CI). C: Percentage of participants achieving HbA1c levels of <6.5% (48 mmol/mol). D: Percentage of participants achieving HbA1c levels of <7% (53 mmol/mol). E: Percentage of participants achieving weight loss of ≥5%. F: Percentage of participants achieving weight loss of ≥10%. *Vs. placebo. †Vs. liraglutide. All data include the per-protocol population.
Target HbA1c levels of <6.5% (48 mmol/mol) were achieved by significantly more participants treated with cotadutide 100 µg (28% [21 of 75]; P = 0.006), 200 µg (33% [67 of 202]; P < 0.001), and 300 µg (39% [72 of 187]; P < 0.001) versus placebo (11% [10 of 91]) (Fig. 2C). Similarly, more participants achieved target HbA1c levels of <7.0% (53 mmol/mol) at 54 weeks with cotadutide 100 µg (57% [43 of 75]), 200 µg (55% [110 of 202]), and 300 µg (58% [108 of 187]) versus placebo (24% [22 of 91]; all P < 0.001) (Fig. 2D). However, the proportion of participants achieving HbA1c <7.0% (53 mmol/mol) or <6.5% (48 mmol/mol) with cotadutide was similar to that with liraglutide 1.8 mg.
After 54 weeks of treatment, significantly more participants achieved target weight loss of ≥5% with cotadutide 100 µg (40% [30 of 75]), 200 µg (30% [59 of 199]), and 300 µg (47% [87 of 187]) and liraglutide 1.8 mg (31% [32 of 104]) versus placebo (10% [9 of 91]; all P < 0.001). Target weight loss of ≥5% was achieved by significantly more participants treated with cotadutide 300 µg versus liraglutide (P = 0.009) (Fig. 2E). Furthermore, significantly greater proportions of participants achieved a target weight loss of ≥10% with cotadutide 200 µg and 300 µg versus placebo and with cotadutide 300 µg versus liraglutide 1.8 mg (Fig. 2F). Additional measures are summarized in Supplementary Table 2.
After 54 weeks of treatment, larger reductions in AST levels were observed with cotadutide 200 µg and 300 µg versus placebo (P = 0.009 and P = 0.001, respectively) (Fig. 3A). Also, greater reductions in ALT levels were observed with cotadutide 200 µg and 300 µg versus placebo (P = 0.009 and P = 0.003, respectively) and with cotadutide 300 µg versus liraglutide (P = 0.023) (Fig. 3B). In participants with baseline AST levels in the fourth quartile, greater reductions in AST levels were observed with cotadutide 200 µg and 300 µg versus placebo (both P < 0.001) (Supplementary Table 3). In participants with ALT levels in the fourth quartile at baseline, greater reductions in ALT levels were observed with cotadutide 200 µg (P = 0.002) and 300 µg (P < 0.001) versus placebo (Supplementary Table 4). Greater reductions in GGT levels were observed with cotadutide 100 µg (LS mean [95% CI] for percent change from baseline –10.54 [–26.75, 5.68]; P = 0.04) and 300 µg (–12.17 [–22.45, –1.90]; P = 0.007) and liraglutide 1.8 mg (–10.54 [–24.41, 3.33]; P = 0.026) versus placebo (12.46 [–2.28, 27.21]). Based on the post hoc regression analysis of the effect of weight loss on changes in ALT, a numerically greater reduction in ALT levels was observed with cotadutide 200 µg and 300 µg versus liraglutide (Supplementary Fig. 1).
Figure 3.
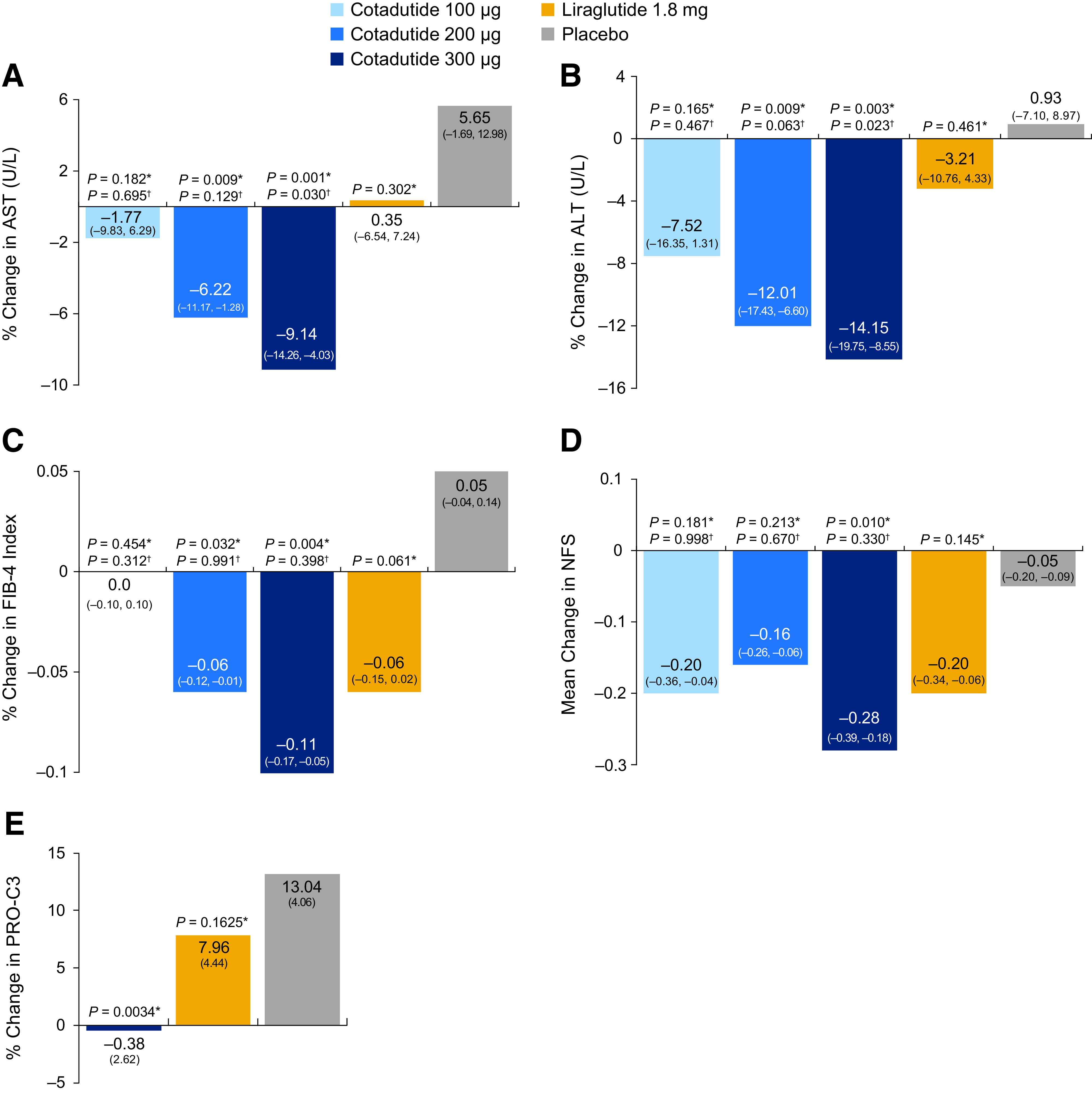
Percent change in hepatic parameters from baseline to week 54. A: Percent change in AST levels. B: Percent change in ALT levels. C: Percent change in FIB-4 index. D: Percent change in NFS. E: Percent change in PRO-C3. *Vs. placebo. †Vs. liraglutide. Data are presented as LS means (95% CI) (A—D) and mean (SD) (E). All data are per-protocol population. Baseline PRO-C3 values were 10.8 ng/mL (placebo), 11.9 ng/mL (liraglutide 1.8 mg), and 10.8 ng/mL (cotadutide 300 µg).
Mean baseline fatty liver index values for all treatment groups ranged from 85.0 to 87.5 (Supplementary Table 1). These levels are substantially above a previously established cutoff of 60 that was found to be indicative of a high prevalence of NAFLD in this patient population (31). Greater decreases in percent change in fatty liver index were observed with cotadutide 100 µg (LS mean [95% CI] change from baseline –8.08 [–10.62, –5.54]; P < 0.001), 200 µg (–6.73 [–8.29, –5.17]; P < 0.001), and 300 µg (–8.18 [–9.79, –6.57]; P < 0.001) and liraglutide 1.8 mg (–6.22 [–8.38, –4.06] P = 0.005) versus placebo (–1.62 [–3.94, 0.71]). Decreases in FIB-4 with cotadutide 200 µg and 300 µg versus placebo (P = 0.032 and P = 0.004, respectively) were observed (Fig. 3C). A reduction in NFS was observed with cotadutide 300 µg versus placebo (P = 0.010) (Fig. 3D). Cotadutide 300 µg reduced PRO-C3 levels at 54 weeks versus placebo (percent change from baseline [SD] –0.38% [2.62]; P = 0.0034), while liraglutide 1.8 mg did not have an effect on PRO-C3 levels (7.96% [4.44]; P = 0.1625) (Fig. 3E). While changes in total cholesterol, LDL cholesterol, or HDL cholesterol did not reach significance, cotadutide 200 µg and 300 µg also reduced triglyceride levels versus placebo (P = 0.042 and P = 0.014, respectively) (Fig. 4).
Figure 4.
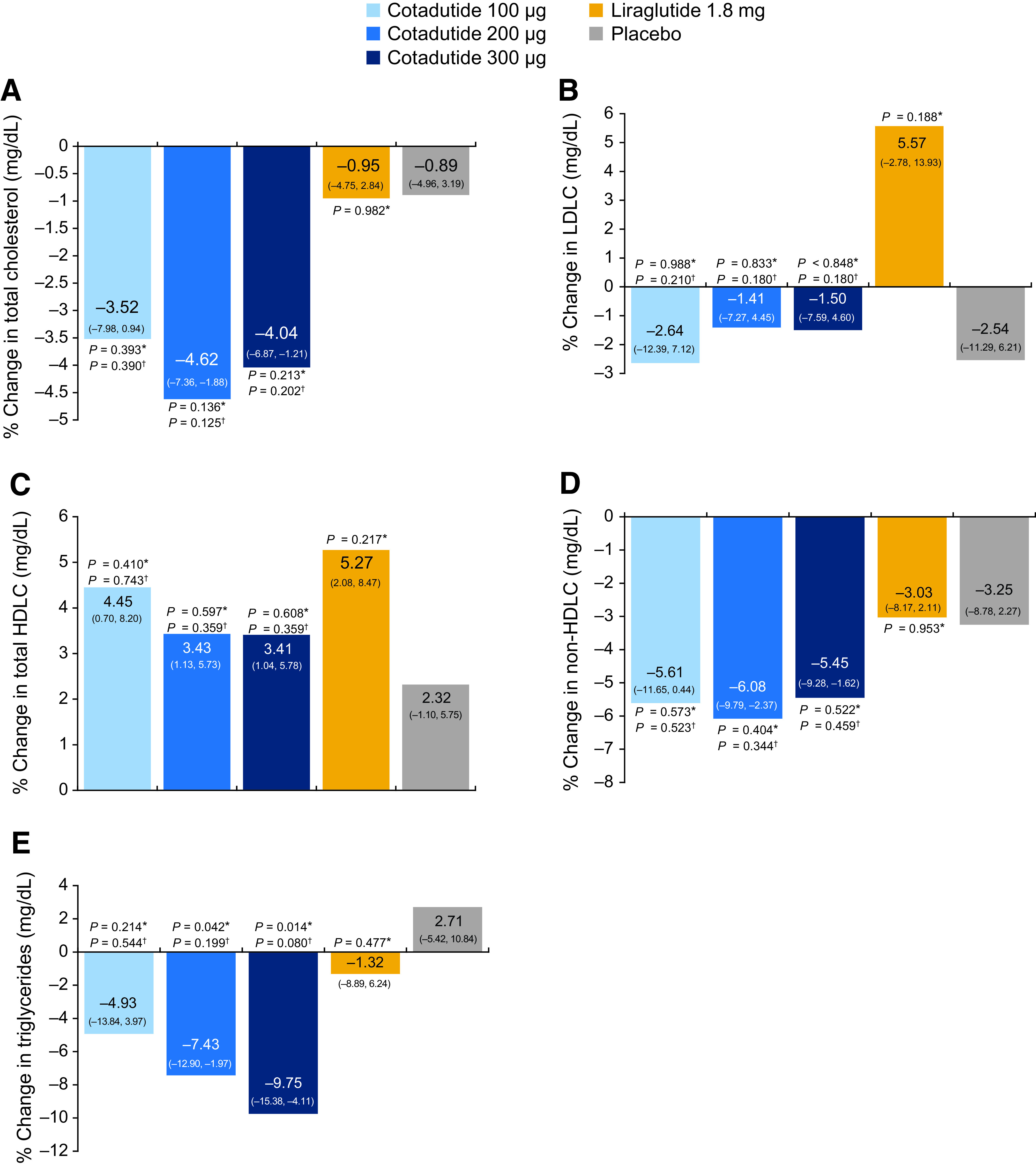
Percent change in secondary end points from baseline to week 54. A: Levels of total cholesterol. B: Levels of LDL cholesterol (LDLC). C: Levels of HDL cholesterol (HDLC). D: Levels of non-HDL cholesterol. E: Levels of triglycerides. *Vs. placebo. †Vs. liraglutide. Data are per-protocol population and are presented as LS means (95% CI).
Cotadutide was associated with a higher incidence of TEAEs across all doses compared with liraglutide or placebo (Supplementary Table 5). Gastrointestinal disorders, including diarrhea, nausea, and vomiting, were the most commonly reported TEAEs with cotadutide treatment at any tested dose (Supplementary Table 5 and Supplementary Table 6). For all doses of cotadutide, a marked decrease in the event rate (per person/day) of these gastrointestinal events was observed over time (Supplementary Fig. 2). Three deaths occurred in the study: two in the cotadutide 200 μg treatment group (myocardial infarction and hemorrhagic stroke) and one in the cotadutide 300 μg treatment group (pulmonary edema). None of the deaths were deemed related to treatment (Supplementary Table 5). A reduction in systolic blood pressure was observed with cotadutide 300 µg (Supplementary Table 7). Increases in pulse rates were observed with all tested doses of cotadutide versus placebo (all P = 0.001 to P = 0.006) (Supplementary Table 7). However, there were no notable changes in rate pressure product with cotadutide treatment.
Anti-drug antibody (ADA) levels were assessed for all cotadutide-treated subjects in the study using a high-sensitivity assay. The ADA incidence was 60.8% (range 56.7–62.0) in cotadutide-treated participants (Supplementary Table 5). ADA levels were not determined for the liraglutide-treated group. Participants who developed higher ADA titers (titer >80) also had higher trough cotadutide concentrations, but the change in HbA1c and body weight from baseline in those who were ADA positive was not different from that for ADA-negative subjects or ADA-positive subjects with lower titers (titer <80). Among cotadutide-treated subjects, a positive ADA status (i.e., above the median) was associated with an increased risk for injection site reactions, but there was no relationship reported with reaction severity.
Conclusions
In this 54-week randomized phase 2b study, treatment with cotadutide yielded significant reductions compared with placebo in HbA1c levels and body weight in participants with overweight or obesity and who have type 2 diabetes with prevalent NAFLD. Target HbA1c levels of <7.0% (53 mmol/mol) at 54 weeks were achieved by more participants treated with cotadutide at any tested dose and liraglutide compared with placebo. Significant reductions in body weight at 54 weeks were observed with all three tested doses of cotadutide versus placebo and with cotadutide 300 µg versus liraglutide. Serum transaminases and GGT improved with the higher doses of cotadutide compared with placebo. At 54 weeks, cotadutide 200 µg treatment resulted in weight loss similar to that observed with liraglutide treatment, and cotadutide 300 µg treatment yielded additional weight loss and reductions in ALT. Improvements in triglyceride levels were also noted with cotadutide 300 µg versus placebo, but not with liraglutide (Fig. 4). These results suggest a potential effect of cotadutide on transaminase levels that was independent of weight loss, along with effects on plasma lipid levels that may be dependent on the glucagon-activity component of cotadutide.
The efficacy of cotadutide in providing glycemic control in participants with overweight or obesity and type 2 diabetes has been demonstrated in earlier studies (28,29). In the current study, cotadutide 300 µg demonstrated similar glycemic control in comparison with liraglutide 1.8 mg. The degree of HbA1c reduction observed with liraglutide is also in line with a previous phase 3 study of liraglutide in participants with overweight or obesity and type 2 diabetes (17).
In previous studies of participants with obesity and NASH, weight loss achieved through lifestyle modifications decreased intrahepatic fat and ALT levels while improving hepatic fibrosis (32,33). With the clear association between weight loss and liver health, a clinically meaningful body weight reduction is expected to be effective therapy for NAFLD or NASH. In the current study, the weight loss observed with cotadutide 300 µg was greater than that with liraglutide 1.8 mg (–4.34% vs. –2.65%, placebo-adjusted change from baseline; P = 0.009). The degree of weight loss observed with liraglutide is similar to that in a previous phase 3 study of participants with overweight or obesity and type 2 diabetes (17).
Preclinical studies in diet-induced NASH mouse models showed significant reductions in NAFLD activity score and fibrosis with cotadutide treatment (26). The hepatic effects were more pronounced in the cotadutide-treated versus the liraglutide-treated mice, even though doses were adjusted to result in similar weight loss. These results were attributed to increased glucagon receptor signaling (26) and warranted additional investigation into the potential effect of cotadutide on liver health. Consequently, the effect of cotadutide on improvements in hepatic parameters was assessed, although participants were not screened for preexisting NAFLD or NASH, and all analyses related to liver function were conducted ad hoc. Decreases in ALT, AST, and GGT levels, as well as improvements in NFS and FIB-4 index, were observed in comparison with placebo. We also observed a reduction in PRO-C3 levels with cotadutide 300 µg compared with placebo. The PRO-C3 neo-epitope is a putative direct marker of fibrogenesis and its use as a biomarker in those with type 2 diabetes can aid the identification of patients with moderately advanced and advanced fibrosis (34,35). Treatment with the GLP-1 monoagonist liraglutide had no notable effect on ALT or AST levels, PRO-C3 levels, NFS, or FIB-4 index in comparison with placebo in this study. Therefore, the observed hepatic benefits of cotadutide treatment may be attributable to the glucagon component. Overall, the results of this study support further development of cotadutide as a potential therapeutic agent for NASH.
Because the majority of deaths linked with NAFLD are attributable to cardiovascular disease, and given the close association between type 2 diabetes and NAFLD, therapeutic agents that improve both liver health and cardiometabolic risk are clinically valuable (36,37). In the current study, treatment with cotadutide resulted in decreased levels of triglycerides. As liraglutide had no appreciable effect on any lipid parameters compared with placebo, these changes also may be attributed to the glucagon activity of cotadutide (38,39). Meta-analyses demonstrate modest reductions in levels of fasting triglycerides and LDL cholesterol by GLP-1 receptor monoagonists (40). GLP-1 regulates intestinal lipoprotein metabolism (41), while glucagon regulates hepatic lipoprotein metabolism (42). Therefore, combined glucagon and GLP-1 action could reduce both hepatic and intestinal production of triglyceride-rich lipoproteins and, thus, improve triglyceride levels in the fasting and postprandial states.
In a previous phase 2a study, cotadutide reduced subcutaneous and visceral adipose tissue (28). Increased adipose tissue has been associated with increased cardiometabolic risk (43,44). Glucagon plays a role in the regulation of hepatic lipid metabolism by reducing hepatic lipid accumulation and secretion (38), as well as increasing LDL receptor expression (39). In contrast, farnesoid X receptor agonists currently being tested in clinical trials for NAFLD are associated with increased levels of LDL cholesterol and total cholesterol and do not significantly impact body weight (45,46). The current results suggest that the glucagon receptor agonist component of cotadutide may be primarily responsible for the observed improvement in lipid profiles, suggesting a potential to reduce cardiovascular risk, in addition to metabolic benefits, for people with overweight or obesity and type 2 diabetes.
In this study, cotadutide was associated with an increased incidence of gastrointestinal disorders, such as nausea and vomiting, versus placebo and liraglutide. This effect is similar to those observed with GLP-1 receptor monoagonists (17,47). The increased incidence of gastrointestinal adverse events may be attributed to a dose-dependent delay in gastric emptying time that was previously observed with cotadutide treatment (48). Furthermore, a reduction in the event rate of nausea and vomiting over time was observed at all tested doses of cotadutide, similar to other GLP-1 receptor monoagonists (17,47). In the current study, starting at a lower dose followed by escalation may have improved tolerability and reduced the incidence of nausea and vomiting. Improved tolerability with a lower starting dose and stepwise titration would allow the exploration of doses >300 µg, which may further improve the glucagon-specific efficacy outcomes, such as reduction in plasma lipids and liver health biomarkers.
A high ADA incidence was observed in this study, during which subjects received chronic treatment for ∼1 year. However, only 16% of subjects developed ADAs above a titer of 80, at which level the impact on pharmacokinetics was approximately twofold above the population average. The overall exposure for participants with maximal ADA titers ≤40 was comparable with the exposure of ADA-negative subjects.
A limitation with respect to study design was that the liraglutide was delivered open-label, while cotadutide treatment was blinded. This may have led to underreporting of gastrointestinal adverse events for liraglutide versus available data from previous blinded trials of liraglutide and may have contributed to better compliance with liraglutide. Another limitation is that the participant population was predominantly white. Further research in a more ethnically diverse population is warranted.
In conclusion, treatment with cotadutide for 54 weeks resulted in improvements across metabolic and hepatic parameters in participants with overweight or obesity and type 2 diabetes with prevalent NAFLD. Effects on hepatic parameters were more pronounced with cotadutide than with the GLP-1 receptor monoagonist liraglutide and occurred in addition to what was expected from weight loss alone. Currently, a phase 2 proof-of-concept study of cotadutide is underway among participants with obesity and biopsy-confirmed NAFLD/NASH and liver fibrosis (ClinicalTrials.gov identifier NCT04019561), which is also exploring a higher cotadutide dose with an improved titration schedule.
Article Information
Acknowledgments. The authors thank Jennifer Schumi (AstraZeneca) for statistical analysis support and Rosalin Arends (AstraZeneca) for contributions to pharmacokinetic and immunogenicity data.
Funding and Duality of Interest. All aspects of the study and manuscript preparation were sponsored by AstraZeneca. The sponsor had a role in the study design; in the collection, analysis, and interpretation of data; in the development of the manuscript; and in the decision to submit the manuscript for publication. Medical writing support was provided by April Suriano, PhD, of Oxford PharmaGenesis Inc., Newtown, PA, and was funded by AstraZeneca. R.N., J.O., L.J., B.H., and P.A. are shareholders and employees of AstraZeneca. T.W. was a shareholder and employee of AstraZeneca during the development of the manuscript. K.M.G. received grant support from AstraZeneca for the conduct of this study and provided oversight for the study in the role of International Coordinating Investigator, for which AstraZeneca made payment to his employer, Pennington Biomedical Research Center. K.M.G. reports research grant support unrelated to the current study from BioKier and National Institutes of Health. M.S. reports personal fees from AstraZeneca for contributing to the conduct of the study. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. R.N., T.W., K.M.G., L.J., B.H., P.A., and M.S. devised the study concept and design. R.N., T.W., K.M.G., J.O., M.S., L.J., B.H., and P.A. acquired the data. R.N., T.W., K.M.G., J.O., L.J., B.H., and P.A. performed analysis and interpretation of the data. T.W. conducted statistical analysis. R.N., K.M.G., and P.A. performed study supervision. R.N. and T.W. wrote the manuscript. R.N., T.W., K.M.G., J.O., M.S., L.J., B.H., and P.A. performed critical revisions of the manuscript. R.N., T.W., and P.A. had access to the data and vouch for the integrity of the data analyses. All authors reviewed and approved the final draft for submission. R.N. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the 70th Annual Meeting of the American Association for the Study of Liver Diseases, Boston, MA, 8–12 November 2019, and at the European Association for the Study of the Liver Digital International Liver Congress, 27–29 August 2020.
Footnotes
Clinical trial reg. no. NCT03235050, clinicaltrials.gov
This article contains supplementary material online at https://doi.org/10.2337/figshare.14272955.
T.W. is currently affiliated with Bristol Myers Squibb, Lawrence Township, NJ.
B.H. is currently affiliated with BOL Pharma, Revadim, Israel.
References
- 1. Targher G, Bertolini L, Padovani R, et al. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care 2007;30:1212–1218 [DOI] [PubMed] [Google Scholar]
- 2. Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology 2012;55:2005–2023 [DOI] [PubMed] [Google Scholar]
- 3. Ong JP, Elariny H, Collantes R, et al. Predictors of nonalcoholic steatohepatitis and advanced fibrosis in morbidly obese patients. Obes Surg 2005;15:310–315 [DOI] [PubMed] [Google Scholar]
- 4. van Herpen NA, Schrauwen-Hinderling VB. Lipid accumulation in non-adipose tissue and lipotoxicity. Physiol Behav 2008;94:231–241 [DOI] [PubMed] [Google Scholar]
- 5. Gastaldelli A. Insulin resistance and reduced metabolic flexibility: cause or consequence of NAFLD? Clin Sci (Lond) 2017;131:2701–2704 [DOI] [PubMed] [Google Scholar]
- 6. Lotta LA, Gulati P, Day FR, et al.; EPIC-InterAct Consortium; Cambridge FPLD1 Consortium . Integrative genomic analysis implicates limited peripheral adipose storage capacity in the pathogenesis of human insulin resistance. Nat Genet 2017;49:17–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology 1999;116:1413–1419 [DOI] [PubMed] [Google Scholar]
- 8. Targher G, Byrne CD. Clinical review: nonalcoholic fatty liver disease: a novel cardiometabolic risk factor for type 2 diabetes and its complications. J Clin Endocrinol Metab 2013;98:483–495 [DOI] [PubMed] [Google Scholar]
- 9. Dai W, Ye L, Liu A, et al. Prevalence of nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus: A meta-analysis. Medicine (Baltimore) 2017;96:e8179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kiapidou S, Liava C, Kalogirou M, Akriviadis E, Sinakos E. Chronic kidney disease in patients with non-alcoholic fatty liver disease: what the hepatologist should know? Ann Hepatol 2020;19:134–144 [DOI] [PubMed] [Google Scholar]
- 11. Asrih M, Jornayvaz FR. Metabolic syndrome and nonalcoholic fatty liver disease: is insulin resistance the link? Mol Cell Endocrinol 2015;418:55–65 [DOI] [PubMed] [Google Scholar]
- 12. Gastaldelli A, Cusi K. From NASH to diabetes and from diabetes to NASH: mechanisms and treatment options. JHEP Rep 2019;1:312–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Piya MK, Tahrani AA, Barnett AH. Emerging treatment options for type 2 diabetes. Br J Clin Pharmacol 2010;70:631–644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Meier JJ. GLP-1 receptor agonists for individualized treatment of type 2 diabetes mellitus. Nat Rev Endocrinol 2012;8:728–742 [DOI] [PubMed] [Google Scholar]
- 15. Potts JE, Gray LJ, Brady EM, Khunti K, Davies MJ, Bodicoat DH. The effect of glucagon-like peptide 1 receptor agonists on weight loss in type 2 diabetes: a systematic review and mixed treatment comparison meta-analysis. PLoS One 2015;10:e0126769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Saxenda (liraglutide) injection [package insert]. Plainsboro, NJ, Novo Nordisk, 2020 [Google Scholar]
- 17. Davies MJ, Bergenstal R, Bode B, et al.; NN8022-1922 Study Group . Efficacy of liraglutide for weight loss among patients with type 2 diabetes: the SCALE Diabetes randomized clinical trial. JAMA 2015;314:687–699 [DOI] [PubMed] [Google Scholar]
- 18. O’Neil PM, Birkenfeld AL, McGowan B, et al. Efficacy and safety of semaglutide compared with liraglutide and placebo for weight loss in patients with obesity: a randomised, double-blind, placebo and active controlled, dose-ranging, phase 2 trial. Lancet 2018;392:637–649 [DOI] [PubMed] [Google Scholar]
- 19. Sofogianni A, Filippidis A, Chrysavgis L, Tziomalos K, Cholongitas E. Glucagon-like peptide-1 receptor agonists in non-alcoholic fatty liver disease: an update. World J Hepatol 2020;12:493–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Khoo J, Hsiang JC, Taneja R, et al. Randomized trial comparing effects of weight loss by liraglutide with lifestyle modification in non-alcoholic fatty liver disease. Liver Int 2019;39:941–949 [DOI] [PubMed] [Google Scholar]
- 21. Smits MM, Tonneijck L, Muskiet MH, et al. Twelve week liraglutide or sitagliptin does not affect hepatic fat in type 2 diabetes: a randomised placebo-controlled trial. Diabetologia 2016;59:2588–2593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shao N, Kuang HY, Hao M, Gao XY, Lin WJ, Zou W. Benefits of exenatide on obesity and non-alcoholic fatty liver disease with elevated liver enzymes in patients with type 2 diabetes. Diabetes Metab Res Rev 2014;30:521–529 [DOI] [PubMed] [Google Scholar]
- 23. Armstrong MJ, Gaunt P, Aithal GP, et al.; LEAN trial team . Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet 2016;387:679–690 [DOI] [PubMed] [Google Scholar]
- 24. Newsome P, Francque S, Harrison S, et al. Effect of semaglutide on liver enzymes and markers of inflammation in subjects with type 2 diabetes and/or obesity. Aliment Pharmacol Ther 2019;50:193–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Perry RJ, Zhang D, Guerra MT, et al. Glucagon stimulates gluconeogenesis by INSP3R1-mediated hepatic lipolysis. Nature 2020;579:279–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Boland ML, Laker RC, Mather K, et al. Resolution of NASH and hepatic fibrosis by the GLP-1R/GcgR dual-agonist Cotadutide via modulating mitochondrial function and lipogenesis. Nat Metab 2020;2:413–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Habegger KM, Heppner KM, Geary N, Bartness TJ, DiMarchi R, Tschöp MH. The metabolic actions of glucagon revisited. Nat Rev Endocrinol 2010;6:689–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ambery P, Parker VE, Stumvoll M, et al. MEDI0382, a GLP-1 and glucagon receptor dual agonist, in obese or overweight patients with type 2 diabetes: a randomised, controlled, double-blind, ascending dose and phase 2a study. Lancet 2018;391:2607–2618 [DOI] [PubMed] [Google Scholar]
- 29. Parker VER, Robertson D, Wang T, et al. Efficacy, safety, and mechanistic insights of cotadutide, a dual receptor glucagon-like peptide-1 and glucagon agonist. J Clin Endocrinol Metab 2020;105:dgz047. [DOI] [PubMed] [Google Scholar]
- 30. Jain M, Tsai L-F, Robertson D, et al. MEDI0382, a GLP/glucagon receptor dual agonist, significantly reduces hepatic fat content in subjects with type 2 diabetes mellitus (Abstract). Diabetes 2018;67(Suppl. 1):78-OR29079704 [Google Scholar]
- 31. Chen LD, Huang JF, Chen QS, et al. Validation of fatty liver index and hepatic steatosis index for screening of non-alcoholic fatty liver disease in adults with obstructive sleep apnea hypopnea syndrome. Chin Med J (Engl) 2019;132:2670–2676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Promrat K, Kleiner DE, Niemeier HM, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology 2010;51:121–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hannah WN Jr, Harrison SA. Effect of weight loss, diet, exercise, and bariatric surgery on nonalcoholic fatty liver disease. Clin Liver Dis 2016;20:339–350 [DOI] [PubMed] [Google Scholar]
- 34. Bril F, Leeming DJ, Karsdal MA, et al. Use of plasma fragments of propeptides of type III, V, and VI procollagen for the detection of liver fibrosis in type 2 diabetes. Diabetes Care 2019;42:1348–1351 [DOI] [PubMed] [Google Scholar]
- 35. Daniels SJ, Leeming DJ, Eslam M, et al. ADAPT: an algorithm incorporating PRO-C3 accurately identifies patients with NAFLD and advanced fibrosis. Hepatology 2019;69:1075–1086 [DOI] [PubMed] [Google Scholar]
- 36. Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol 2015;62(Suppl.):S47–S64 [DOI] [PubMed] [Google Scholar]
- 37. Lonardo A, Ballestri S, Targher G, Loria P. Diagnosis and management of cardiovascular risk in nonalcoholic fatty liver disease. Expert Rev Gastroenterol Hepatol 2015;9:629–650 [DOI] [PubMed] [Google Scholar]
- 38. Galsgaard KD, Pedersen J, Knop FK, Holst JJ, Wewer Albrechtsen NJ. Glucagon receptor signaling and lipid metabolism. Front Physiol 2019;10:413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rudling M, Angelin B. Stimulation of rat hepatic low density lipoprotein receptors by glucagon. Evidence of a novel regulatory mechanism in vivo. J Clin Invest 1993;91:2796–2805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Xiao C, Dash S, Morgantini C, Adeli K, Lewis GF. Gut peptides are novel regulators of intestinal lipoprotein secretion: experimental and pharmacological manipulation of lipoprotein metabolism. Diabetes 2015;64:2310–2318 [DOI] [PubMed] [Google Scholar]
- 41. Xiao C, Bandsma RH, Dash S, Szeto L, Lewis GF. Exenatide, a glucagon-like peptide-1 receptor agonist, acutely inhibits intestinal lipoprotein production in healthy humans. Arterioscler Thromb Vasc Biol 2012;32:1513–1519 [DOI] [PubMed] [Google Scholar]
- 42. Xiao C, Pavlic M, Szeto L, Patterson BW, Lewis GF. Effects of acute hyperglucagonemia on hepatic and intestinal lipoprotein production and clearance in healthy humans. Diabetes 2011;60:383–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol 2018;17:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Fox CS, Massaro JM, Hoffmann U, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 2007;116:39–48 [DOI] [PubMed] [Google Scholar]
- 45. Siddiqui MS, Van Natta ML, Connelly MA, et al.; NASH CRN . Impact of obeticholic acid on the lipoprotein profile in patients with non-alcoholic steatohepatitis. J Hepatol 2020;72:25–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Neuschwander-Tetri BA, Loomba R, Sanyal AJ, et al.; NASH Clinical Research Network . Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo-controlled trial. Lancet 2015;385:956–965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Nauck MA, Petrie JR, Sesti G, et al.; Study 1821 Investigators . A phase 2, randomized, dose-finding study of the novel once-weekly human GLP-1 analog, semaglutide, compared with placebo and open-label liraglutide in patients with type 2 diabetes. Diabetes Care 2016;39:231–241 [DOI] [PubMed] [Google Scholar]
- 48. Robertson D, Parker VE, Ambery P, et al. MEDI0382, an oxyntomodulin-like peptide with targeted GLP-1/glucagon receptor activity, promotes a dose-dependent increase in gastric emptying time (Abstract). Diabetes 2019;68(Suppl. 1):988-P30833470 [Google Scholar]


