Supplemental Digital Content is available in the text.
Keywords: anxiety, cardiac rehabilitation, depression, metacognitive therapy
Background:
Depression and anxiety in cardiovascular disease are significant, contributing to poor prognosis. Unfortunately, current psychological treatments offer mixed, usually small improvements in these symptoms. The present trial tested for the first time the effects of group metacognitive therapy (MCT; 6 sessions) on anxiety and depressive symptoms when delivered alongside cardiac rehabilitation (CR).
Methods:
A total of 332 CR patients recruited from 5 National Health Service Trusts across the North-West of England were randomly allocated to MCT+CR (n=163, 49.1%) or usual CR alone (n=169, 50.9%). Randomization was 1:1 via minimization balancing arms on sex and Hospital Anxiety and Depression Scale scores within hospital site. The primary outcome was Hospital Anxiety and Depression Scale total after treatment (4-month follow-up). Secondary outcomes were individual Hospital Anxiety and Depression Scales, traumatic stress symptoms, and psychological mechanisms including metacognitive beliefs and repetitive negative thinking. Analysis was intention to treat.
Results:
The adjusted group difference on the primary outcome, Hospital Anxiety and Depression Scale total score at 4 months, significantly favored the MCT+CR arm (–3.24 [95% CI, –4.67 to –1.81], P<0.001; standardized effect size, 0.52 [95% CI, 0.291 to 0.750]). The significant difference was maintained at 12 months (–2.19 [95% CI, –3.72 to –0.66], P=0.005; standardized effect size, 0.33 [95% CI, 0.101 to 0.568]). The intervention improved outcomes significantly for both depression and anxiety symptoms when assessed separately compared with usual care. Sensitivity analysis using multiple imputation of missing values supported these findings. Most secondary outcomes favored MCT+CR, with medium to high effect sizes for psychological mechanisms of metacognitive beliefs and repetitive negative thinking. No adverse treatment-related events were reported.
Conclusions:
Group MCT+CR significantly improved depression and anxiety compared with usual care and led to greater reductions in unhelpful metacognitions and repetitive negative thinking. Most gains remained significant at 12 months. Study strengths include a large sample, a theory-based intervention, use of longer-term follow-up, broad inclusion criteria, and involvement of a trials unit. Limitations include no control for additional contact as part of MCT to estimate nonspecific effects, and the trial was not intended to assess cardiac outcomes. Nonetheless, results demonstrated that addition of the MCT intervention had broad and significant beneficial effects on mental health symptoms.
Registration:
URL: https://www.clinicaltrials.gov; Unique identifier: ISRCTN74643496.
Clinical Perspective.
What Is New?
A psychological treatment called metacognitive therapy was evaluated for the first time in the treatment of anxiety and depression in patients with cardiovascular disease.
The treatment improved anxiety and depression symptoms when added to usual cardiac rehabilitation. Compared with usual care, there were also greater improvements in trauma symptoms, beliefs about thinking, and unhelpful thinking styles.
The effect sizes were medium to large, compare favorably with the best reported outcomes for depression, and are better for anxiety than those obtained in earlier cardiovascular disease studies.
What Are the Clinical Implications?
Anxiety and depression can be effectively managed using group metacognitive therapy in patients with cardiovascular disease.
The addition of group metacognitive therapy to cardiac rehabilitation is well-tolerated and does not impact negatively on clinic attendance.
Metacognitive therapy is deliverable by non–mental health specialists and could improve psychological outcomes for patients with cardiovascular disease.
Cardiovascular disease (CVD) is the most common noncommunicable disease1 and makes the largest contribution to morbidity and mortality worldwide. The psychological impacts of CVD are substantial, with anxiety and depression affecting up to one-third of people with CVD and linked to increased future cardiac events, poorer quality of life, greater health care costs, and poorer long-term psychological adjustment.2,3 The effective management of anxiety and depression is therefore important. Several trials have evaluated the effect of antidepressant drugs and psychotherapy on depression in CVD, including the CREATE (Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy Trial)4 and ENRICHD (Enhancing Recovery in Coronary Heart Disease)5 trials, but the effect for psychological therapy on depression symptoms was nonsignificant or small.
The Cochrane review6 and meta-analysis published in 2017 included 35 randomized, controlled trials of 10 703 people with CVD treated for anxiety and depression using a variety of psychological interventions compared with usual care. The majority of studies (23 out of 35) evaluated multifaceted interventions including multiple therapy components. There was evidence of reductions in anxiety (pooled standardized mean difference [SMD], –0.24 [95% CI, –0.09 to –0.38]) and depression (pooled SMD, –0.27 [95% CI, –-0.15 to –0.39]), but low evidence quality means there is considerable uncertainty about the effects observed.
Metacognitive therapy (MCT7) is a theory-based, structured treatment approach that may be particularly suited to addressing the psychological needs of patients with CVD. Unlike other therapies, MCT does not require an in-depth analysis and challenging of the content of patients’ worries, which in the CVD context are often realistic.8 MCT focuses on enabling patients to regulate repetitive negative thinking cycles such as worry and rumination and other unhelpful behaviors that research shows maintain anxiety and depression. Results from randomized, controlled trials in mental health settings demonstrate that MCT is a highly effective treatment for anxiety9 and depression10 and may be more effective than cognitive behavior therapy.11 An important question is whether such effects might translate to mental health symptoms in patients with CVD. Cardiac rehabilitation (CR) services may be particularly interested in implementing MCT rather than other approaches because it is brief, is highly structured, and can be delivered in groups irrespective of the nature of psychological problems. Delivering such an intervention within CR services has the added value of availability of specialist cardiac knowledge while avoiding delay and potential stigma associated with a secondary mental health referral.
In this article, we report the results of the PATHWAY trial, the first large-scale trial of group-MCT in patients with CVD patients. We aimed to evaluate if the addition of MCT to usual clinical management (CR) improved depression and anxiety outcomes. CR in the United Kingdom is offered routinely in a group setting to patients after a cardiac event, reduces mortality and hospital readmissions, and improves quality of life.12 However, the impact on anxiety and depression is small. CR consists of exercise sessions, education and stress management techniques directed at improving CVD risk profiles, physical fitness, and psychological functioning.13 The psychological components are not standardized and vary by CR program but may include counseling, relaxation, meditation, and cognitive challenging of negative thoughts.
We implemented a pragmatic trial with the primary hypothesis that the addition of group-MCT to usual CR is more effective than CR alone in alleviating symptoms of anxiety and depression in patients with CVD between baseline and 4-month follow-up. For maximal reach, we did not restrict the study to patients with CVD with diagnoseable depression or anxiety disorders. Instead, we set a minimal inclusion criterion as presence of mild symptoms of anxiety, depression, or both, which could include individuals with current or previous psychological disorders.
Methods
Study Design
PATHWAY is a multicenter, 2-arm, single-blind randomized, controlled trial with 4- and 12-month follow-up comparing group-MCT plus usual CR (MCT+CR) with usual CR alone. Patients were recruited from CR services at 5 National Health Service (NHS) Trust hospitals (University Hospital of South Manchester NHS Foundation Trust, Central Manchester University Hospitals NHS Foundation Trust, East Cheshire NHS Trust, Stockport NHS Foundation Trust, and Pennine Acute Hospitals NHS Trust) across the North-West of England. Ethical approval was obtained from the Preston Research Ethics Committee (REC Reference 14/NW/0163), along with site-specific approval. Further details are presented in the published study protocol.14 The trial is registered with the ISCRTN registry, No. ISRCTN74643496. The data that support the findings of this study are available from the corresponding author on reasonable request.
Participants
All eligible patients were referred to CR services and met the Department of Health or British Association for Cardiac Prevention and Rehabilitation CR eligibility criteria. A summary of reasons for referral to CR by group is presented in Table 1. Patients were required to have a score of 8 or greater on either the depression or anxiety subscale of the Hospital Anxiety and Depression Scale (HADS),15 be age 18 years or older, and have a competent level of English language comprehension (read, understand, and complete questionnaires in English). For more details on the inclusion/exclusion criteria, see the study protocol.14
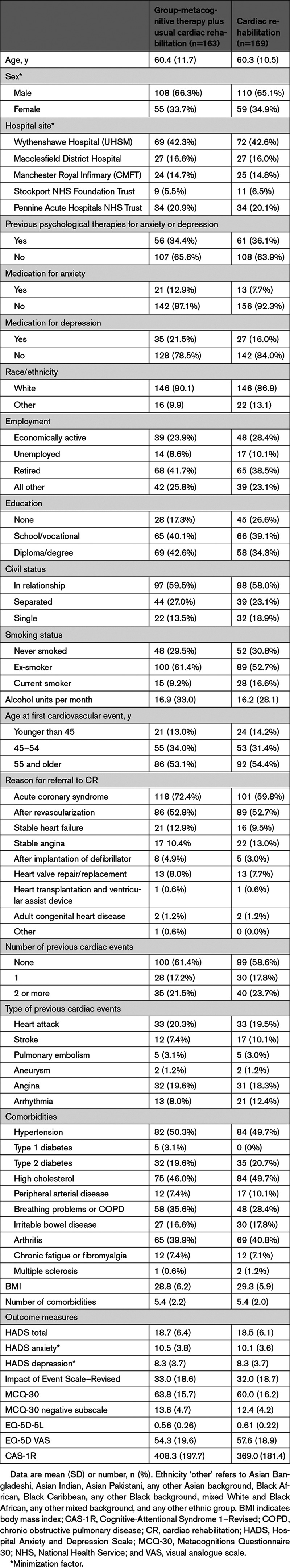
Table 1.
Baseline Demographic and Clinical Characteristics
All patients referred to the CR program are sent a National Audit of Cardiac Rehabilitation assessment pack,16 which includes a HADS questionnaire,15 to be returned to the CR team at CR assessment. Patients who scored 8 or above on the anxiety or depression subscale of the HADS were screened for eligibility by the CR staff. A score of 8 or greater is considered to be the cutoff for mild clinical symptoms and yields the optimal sensitivity and specificity for identifying clinical caseness.17 Eligible patients were provided with study information and contacted by a research assistant (RA) to obtain written consent and administer baseline questionnaires before starting CR.
Randomization and Masking
Patients were randomized by computer via a telephone link to the Manchester Academic Health Science Center Clinical Trials Co-Ordination Unit. Patients were allocated to trial arms in a 1:1 ratio using a minimization algorithm18 to maximize balance between the 2 arms within each hospital site on sex and HADS scores (in 3 subgroups: anxiety score ≥8; depression ≥8; anxiety and depression ≥8). The chief investigator, RAs, and trial statisticians were masked to treatment allocation throughout data collection and analysis. Instances of accidental unmasking were recorded to assess their frequency and severity, which was routinely reviewed by the Trial Steering Committee.
Interventions
Participation in study arms did not preclude the addition of treatments for more severe anxiety and depression that might be required and offered by mental health specialists as part of the usual CR treatment pathway.
Usual CR
CR programs are group-based programs including group exercise sessions and educational seminars. They vary somewhat in content across services, but all offered core components19 as part of outpatient provision using group-based delivery by a multidisciplinary team in hospital or community settings. CR was run weekly over a period of 8 to 10 weeks. Educational seminars covered topics including lifestyle and medical risk factor management. In addition, sites provided elements of psychosocial interventions including talks on stress management and relaxation. All sites delivered sessions on relaxation, which included breathing techniques and progressive muscle relaxation. Seminars on stress management varied. Whereas 2 sites delivered psychoeducation on stress, 3 sites incorporated cognitive therapy methods (ie, challenging negative thoughts, worry decision tree, behavioral activation). In addition, 1 site offered a 4-week stress management course as part of CR, which included cognitive therapy procedures such as generating and sharing a case formulation based on Greenberger and Padesky treatment manual.20
Group-MCT Plus Usual CR
We chose CR staff to administer group-MCT because CR is the main point of repeated contact for patients with CVD, and our service-user interviews suggested that patients valued their relationship with staff. The intervention group received group-MCT in addition to usual CR (MCT+CR), which consisted of 6 sessions of group-MCT of 60 to 90 minutes, with 1 session scheduled per week.
MCT+CR was delivered by 2o CR professionals at each site (ie, physiotherapist, CR nurse, occupational therapists) or research nurses. Therapists received 2 days of training in group-MCT followed by supervised practice in delivering the intervention to a pilot group, and an additional 1-day workshop to address difficulties experienced in delivering the intervention. Therapists received supervision throughout the trial. Therapist adherence to the trial protocol was assessed using a checklist, which recorded the components of the protocol implemented in each session, if any components had been missed, and if so, why. Session adherence scores were computed by counting the total number of elements completed in the session.
Group-MCT consisted of helping participants identify triggering thoughts leading to the processes of worry, rumination, and other unhelpful coping behaviors. They were guided in the practice of specific techniques to help them discover flexibility and control over such patterns of extended negative thinking. One such technique is the Spatial Attention Control Exercise (SpACE), consisting of directing attention as a means of enhancing awareness of thoughts and the capacity for independent flexible mental control—for example, focusing on sounds that might occur on the right and left while being aware of the independence of attention control from the occurrence of any internal (thoughts and sensations) and external events. The therapist uses the exercise to shape and strengthen more adaptive metacognitions and weaken beliefs about the uncontrollability of thinking. At the end of treatment, each patient received their own “helpful behaviors” prescription summarizing what they had learned. Homework practice of techniques was a feature throughout, and implementation of treatment followed the session-by-session manual.
Data Collection
Patients completed assessments at 3 time points: baseline (pre-CR), 4 months after randomization (4-month follow-up), and 12 months after randomization (12-month follow-up). Baseline assessments were completed face-to-face with an RA, and a range of options were offered for completing follow-up assessments: by mail, face-to-face, or via telephone. Patients received £5 cash for completing the baseline assessment and a £10 shopping voucher for each follow-up assessment returned. All outcome measures were collected at each time point. Adverse and serious adverse events were further reviewed on a quarterly basis at the program’s executive committee meetings.
Outcomes
The primary outcome was the HADS15 total score at 4-month follow-up (after treatment). The HADS measures symptoms of anxiety (7 items) and depression (7 items). Items are rated using a 4-point (0–3) scale, with greater scores indicating elevated distress. Scores for each subscale range from 0 to 21 and can be categorized as normal (0–7), mild (8–10), moderate (11–14), or severe (15–21). Secondary outcomes were the HADS at 12 months, and other measures at 4 and 12 months as follows: posttraumatic stress symptoms were measured using the Impact of Event Scale–Revised (IES-R).21 Change in metacognitive beliefs (an underlying psychological causal variable) was measured with the total score on the Metacognitions Questionnaire 30 (MCQ-30)22 and the “negative beliefs about thoughts concerning uncontrollability and danger” MCQ-30 subscale,22 preselected as representing the primary mechanism targeted in MCT.7 Quality of life was assessed with the EQ-5D-5L (EuroQol 5 dimensions 5 levels; both the utility score and visual analogue scale [VAS] score),23 derived using the recommended methods of the National Institute for Health and Care Excellence.24,25 The Cognitive-Attentional Syndrome 1–Revised (CAS-1R26) was used to measure repetitive negative thinking and unhelpful coping behaviors, considered as mechanism variables. Adverse events were continuously monitored by the health professionals delivering Group-MCT and were reported and assessed as related or unrelated to the study. Adverse and serious adverse events were further reviewed on a quarterly basis at the program’s executive committee meetings. We assessed therapist adherence to the MCT intervention using a session-by-session checklist completed by the cotherapist. The checklist assessed whether or not each of the compulsory elements for the particular session had been completed.
Statistical Analysis
The trial was designed to detect a SMD between trial arms of 0.4 in HADS total score at 4-month follow-up with 90% power, where 0.4 is in the middle of the range of effect sizes reported for other forms of psychological interventions for depression.27 The first 52 patients constituted an internal pilot study for the purpose of ascertaining feasibility of recruitment, ascertaining retention, and computing a definitive sample size for the main trial.14,28 The pilot sample SD in HADS scores at baseline was 5.7, and based on this, the retention rate, and other statistical parameters from the pilot, a total recruited sample of 332 patients was required to detect an effect of 0.4, equivalent to a 2.2-point difference in HADS total score (for full details, see Wells et al28).
Analysis was conducted in accordance with a prespecified analysis plan detailing the analytic models, primary and secondary outcomes, choice of covariates, sensitivity analyses, and all other key aspects of the analysis. The plan was finalized and approved by the trial steering committee before data analysis or unmasking. The primary analyses used intention-to-treat principles. For continuous outcomes, a linear mixed effects regression model was applied incorporating all 3 time points (baseline, 4 months, and 12 months). Prespecified covariates in the model were randomization factors (hospital site, sex, baseline total HADS score), age, and medication for depression or anxiety (never taken/currently taking/taken in the past). All other potential covariates (Table 1) were below predefined imbalance criteria for sensitivity testing (standardized mean difference >0.25 or category difference >10% between arms). We applied hierarchical regression models with random effects at the levels of the patient and the CR (or MCT+CR) course attended. The covariance matrix for the model was chosen as either unstructured or first-order autoregressive depending on whichever gave the lowest Bayesian Information Criteria score.29
The effects of the intervention at 4-month and 12-month follow-up were examined using the treatment group by time point interaction terms from the mixed effects model analysis, where time point was a categorical variable to provide independent tests of effect at 4 and 12 months. No adjustments for multiple testing were applied, and an α-value of 5% was used throughout. We ran sensitivity analysis using multiple imputation (MI) to assess robustness of results against missing values. There were few missing values at baseline (1 missing outcome value and a maximum of 3 missing values on any covariate); therefore, these were imputed by simple regression imputation using all available variables at baseline but excluding treatment arm. MI was then used to impute missing outcome values at 4 months and 12 months, using the full set of variables and including the interaction term between treatment arm and time point (for consistency with the analysis model). We used the chained-equations MI procedure and 20 MI datasets.30
All outcome measures demonstrated skewness and kurtosis below the threshold of 1.0 specified in our analysis plan, so sensitivity against nonnormality was not assessed. The trial eligibility criteria allowed inclusion of participants without clinically relevant anxiety provided they had at least mild depression, and vice versa; 23% and 40% of participants, respectively, fell into these categories at baseline, closely balanced across arms. To determine how this may have impacted analysis results for HADS anxiety and depression as separate outcomes, we conducted sensitivity analyses excluding these individuals. Analyses were conducted using Stata version 14.
Role of the Funding Source
The funder of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author (A.W.) had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
A total of 3808 patients were referred to CR between July 13, 2015, and January 12, 2018, of whom 992 had an elevated HADS score and were screened for eligibility (Figure 1). A total of 193 patients did not meet full eligibility criteria (eg, not proficient in English), resulting in 799 eligible patients. Of these, 360 declined to take part, 67 were uncontactable, 17 no longer met the inclusion criteria (eg, began taking antidepressants, had presence of suicidality, experienced symptoms of psychosis), and 23 started CR before being approached. Consequently, 332 patients consented to the trial, of whom 163 (49.1%) were randomly allocated to MCT+CR and 169 (50.9%) to CR. There were 52 incidents of unmasking, all involving an RA accidently discovering a patient’s allocation. For these cases, subsequent collection of follow-up data from the patient was undertaken by a different RA still masked to allocation. There were no cases of the trial statisticians or chief investigator becoming unmasked.
Figure 1.
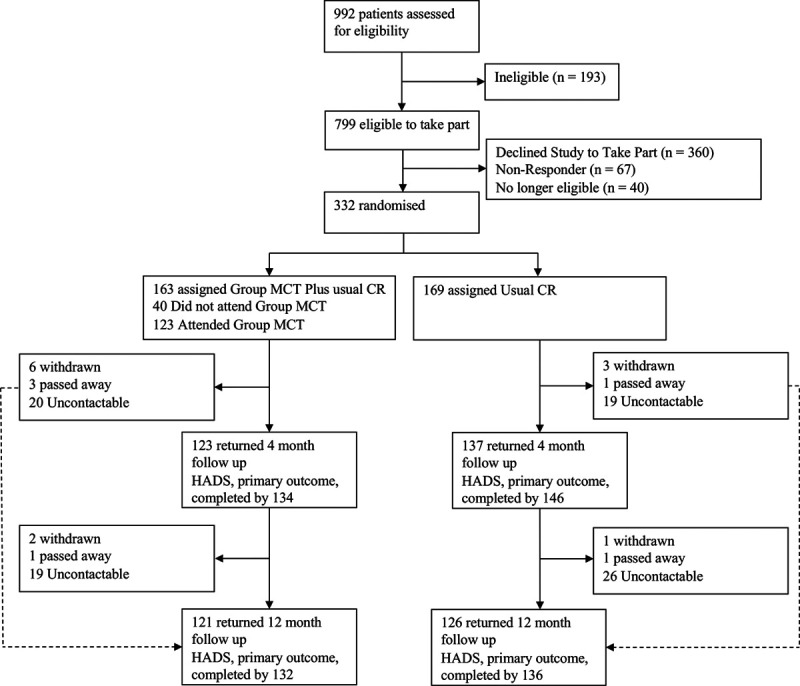
Trial profile. CR indicates cardiac rehabilitation; HADS, Hospital Anxiety and Depression Scale; and MCT, metacognitive therapy.
Table 1 provides demographic and clinical data for the sample at baseline. The groups were well balanced on all measured variables. Of patients in the MCT+CR arm, 34% were female, compared with 35% of patients in the CR arm. In both arms, the mean age was 60 years, and exposure to previous psychological therapy was 34% and 36%, respectively. HADS total scores were similar (18.5 versus 18.7), as were IES-R (32.0 versus 33.0) and EQ-5D-5L utility scores (10.6 versus 11.4). Differences were only a little larger with regard to EQ-5D VAS (57.6 versus 54.3), MCQ-30 (60.0 versus 63.8), and CAS-1R (369.0 versus 408.3) scores.
The mean intervals between baseline and 4-month assessments were similar for both arms (CR, 133.6 days; MCT+CR, 134.7 days), as were the baseline to 12-month intervals (369.2 versus 370.0 days).
Figure 2 presents mean HADS total scores and 95% CIs for each trial arm at each pretreatment and posttreatment assessment point. The pattern of results shows a small gradual linear improvement in scores for the CR group, which contrasts with a greater and more rapid improvement in MCT+CR. Results of the main analysis of primary and secondary end points are summarized in Table 2. The adjusted group difference on the primary outcome (HADS total score at 4 months) significantly favored the MCT+CR arm (–3.24 [95% CI, –4.67 to –1.81]; P<0.001; SMD=0.52), as did the difference at the 12-month secondary outcome point (–2.19 [95% CI, –3.72 to –0.66]; P=0.005; SMD=0.33).
Figure 2.
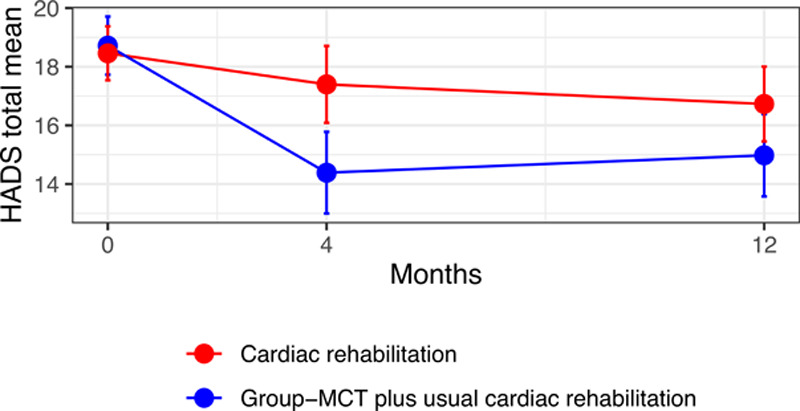
Unadjusted mean total Hospital Anxiety and Depression Scale (HADS) scores at baseline, 4-month follow-up, and 12-month follow-up. Bars are 95% CIs. MCT indicates metacognitive therapy.
Table 2.
Summary of Analyses of Primary and Secondary Outcomes
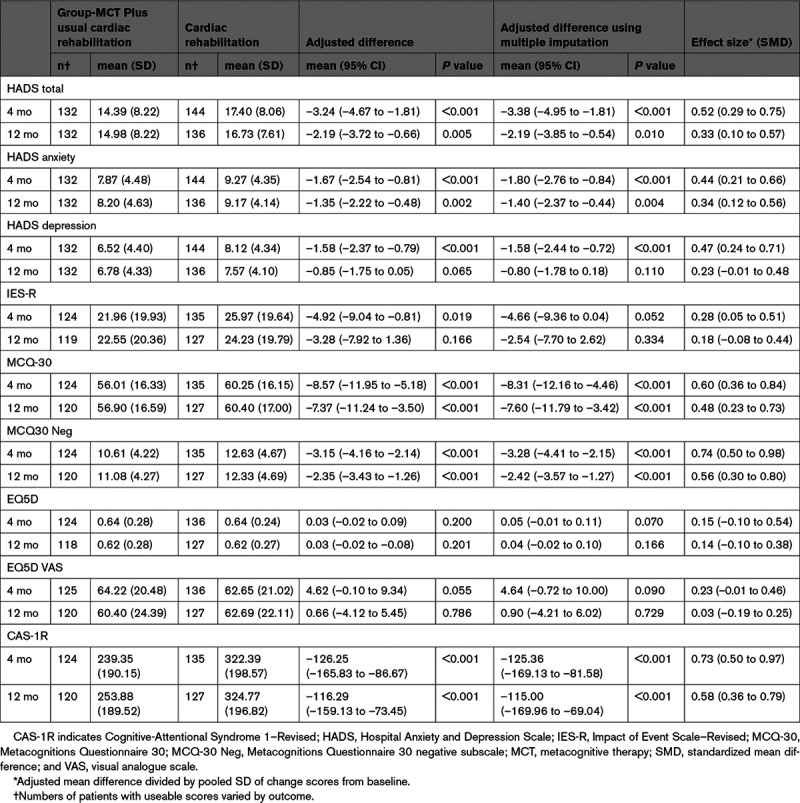
Patients in the MCT+CR arm achieved significantly lower mean HADS anxiety subscale score at both 4 months (–1.67 [95% CI, –2.54 to –0.81]; P<0.001; SMD=0.44) and 12 months (–1.35 [95% CI, –2.22 to –0.48]; P=0.002; SMD=0.34), plus a lower HADS depression subscale mean score at 4 months (–1.58 [95% CI, – 2.37 to –0.79]; P<0.001; SMD=0.47) but not at 12 months (–0.85 [95% CI, –1.75 to 0.05]; P=0.065; SMD=0.23). Results were similar when individuals without clinical levels of baseline anxiety or depression scores were excluded: for anxiety, an adjusted group difference of –1.70 ([95% CI, –2.75 to –0.65]; P=0.001; SMD=0.43) at 4 months and –1.38 ([95% CI, –2.50 to –0.25]; P=0.016; SMD=0.33) at 12 months; for depression, –1.63 ([95% CI, –2.67 to –0.58]; P=0.002; SMD=0.46) and –0.65 ([95% CI, –1.82 to 0.53]; P=0.281; SMD=0.17), respectively. Most other secondary outcomes also favored the MCT intervention: the IES-R at 4 months (–4.92 [95% CI, –9.04 to –0.81]; P=0.019) but not 12 months (–3.28 [95% CI, –7.92 to 1.36]; P=0.166); MCQ-30 total scores at both 4 and 12 months (–8.57 [95% CI, –11.95 to –5.18]; P<0.001; and –7.37 [95% CI, –11.24 to –3.50]; P<0.001, respectively); MCQ-30 negative beliefs subscale scores at both time points (–3.15 [95% CI, –4.16 to –2.14]; P<0.001; and –2.35 [95% CI, –3.43 to –1.26]; P<0.001) and the CAS-1R also at both 4 months (–126.25 [95% CI, –165.83 to –86.67]; P<0.001) and 12 months (–116.29 [95% CI, –159.13 to –73.45]; P<0.001). For the EQ5D utility scores, there was no statistically significant difference at 4 months (0.03 [95% CI, –0.02 to 0.09]; P=0.200) or at 12 months (0.03 [95% CI, –0.02 to 0.10]; P=0.201); similarly, the difference on the EQ5D-VAS was not significant at either time point (4 months: 4.62 [95% CI, –0.10 to 9.34]; P=0.055; 12 months: 0.66 [95% CI, –4.12 to 5.45]; P=0.786). Sensitivity analysis using MI changed the statistical significance of the results for only 1 secondary outcome, the IES-R at 4 months, which ceased to be statistically significant (P>0.05).
Patients in both trial arms attended routine CR sessions at their site as members of larger groups (of up to 15) including patients with CVD not part of the trial. Patients in the MCT+CR arm also attended the trial-specific group-MCT sessions. Across the trial, a total of 77 group-MCT courses were conducted, ranging from 3 at the Stockport NHS Foundation Trust to 30 at Wythenshawe Hospital, with numbers of trial participants varying from a minimum of 1 to a maximum of 7 with a mean of 3.5. Attendance at CR exercise sessions was high in both groups, with a mean of 6.0 out of 10 sessions attended by CR arm patients and 6.3 by MCT+CR patients, a nonsignificant difference (0.34 [95% CI, –0.41 to 1.08]; P=0.374). Mean attendance at CR educational sessions was lower (CR 3.6, MCT+CR 4.0) and also did not differ between groups (0.4 [95% CI, –0.43 to 1.23]; P=0.343). Attendance at group-MCT was high, with 61% attending 4 or more sessions, and 14% attending 1 to 3 sessions. As both conditions involved treatment (and case management) as usual, this meant that additional treatment could be sought. Across the follow-up period, 14 patients under CR and 6 under CR+MCT received new psychological therapy outside of CR or MCT; the difference was not statistically significant (odds ratio, 0.3230 [95% CI, 0.1307–0.801.29]; P=0.106); however, the numbers involved were small.
Strength and Clinical Significance of Treatment Effects
To aid in the interpretation of findings, we computed effect sizes in the form of SMDs between groups at 4- and 12-month follow-ups. SMDs were computed as the adjusted mean difference between groups from the mixed effects model, divided by the pooled SD of change scores from baseline for consistency with Cochrane6,31 to enable cross-study comparisons. The effect sizes for primary and secondary outcomes are presented in Table 2.
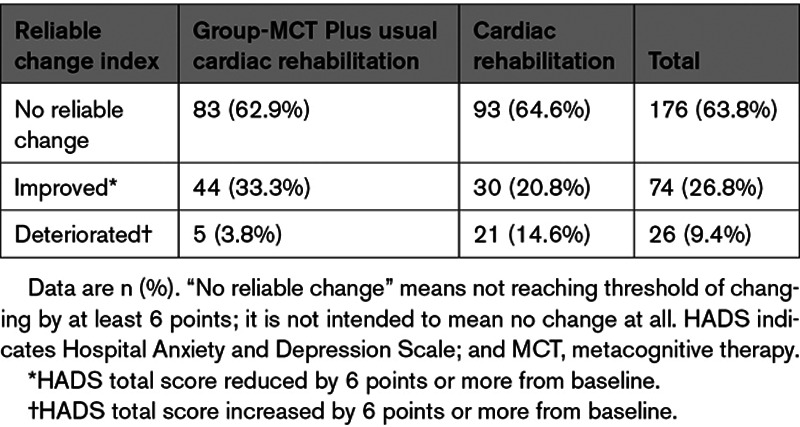
In addition, we computed the reliable change index32 for the HADS total score at the primary 4-month follow-up. The reliable change index represents the difference between 2 measurements made on a single individual that would be statistically significant at P<0.05. A Cronbach alpha of 0.91 derived from the control sample at 4 months was used as the estimate of reliability for a usual CR population, because baseline HADS scores had restricted variance as a result of being a study eligibility criterion. From this, a reduction of 6 points in an individual’s score was defined as statistically reliable improvement, whereas an increase of 6 points was defined as reliable worsening of symptoms. The proportions of patients falling into each category by trial arm are presented in Table 3. The percentage of patients reliably improved was 21% in CR compared with 33% in MCT+CR; the percentages exhibiting psychological deterioration were 15% in CR compared with 4% in MCT+CR.
Table 3.
Reliable Change in HADS Total Score in Individual Patients by 4 Months by Treatment Group, Using Complete Cases
Protocol Adherence
Across sites, mean adherence to protocol was high at 98.8% (SD = 2.43) but varied across sessions and between sites with a range of 50% to 100%. The most common deviations were not reviewing homework (9 deviations) and not practicing SpACE in session (4 deviations).
Adverse Events Reporting
Safety and adverse events (increased suicidality, death, self-injury) associated with the treatments were monitored throughout the trial. No adverse events were reported.
Discussion
This trial demonstrated that 6 sessions of group-MCT significantly reduced overall depression and anxiety when added to CR, compared with CR alone. Improvement in the primary outcome, HADS total at 4 months (after treatment), was maintained at 12 months of follow-up. The addition of MCT to CR also showed superiority compared with CR alone on the majority of secondary outcomes, at both 4 months and 12 months.
We used the SMD to interpret the size of the effects and for comparison with other study findings. The SMDs of 0.44 for HADS anxiety and 0.47 for HADS depression at 4 months in the present study compare favorably with the aggregated SMDs reported for anxiety (0.24) and depression (0.27) across other studies.6 The depression effect sizes are similar to the MOSAIC33 trial of collaborative care (g=0.45) and the CODIACS34 trial of patient preference with a range of treatments offered (g=0.59); however, in the current study, we found significant improvements in anxiety outcomes that these other studies did not.
With respect to overall psychological distress (HADS-total), 21% of patients individually improved in CR on the basis of the 6-point reliable change index, which increased to 33% with the addition of group-MCT. In addition, an unexpected finding was that MCT+CR demonstrated lower rates of statistically reliable deterioration compared with CR at 4 months. However, the reliable change index sets a high bar with its criteria of statistically significant change within an individual, and possibly underestimates the numbers experiencing a clinically meaningful change. Nonetheless, these effects suggest 2 areas of benefit. First, the provision of MCT lowered both anxiety and depression symptom severity. Second, the provision of MCT might also reduce the risk of psychological deterioration. The results at 12 months on HADS total continued to show a superiority of the MCT group compared with treatment as usual. Although the SMD was smaller compared with the 4-month assessment, the result suggests that a significant psychological advantage achieved in the MCT condition persisted over the longer term. The addition of MCT to CR impacted most of the secondary outcomes. Significant differences favoring MCT+CR were found at 4 months in both HADS anxiety and depression when measured separately, suggesting that the overall effect reflects changes in both subsets of symptoms, although only anxiety maintained a statistically significant group difference at 12 months. These results were unchanged when we excluded individuals without clinically relevant scores at baseline. This suggests that MCT had a similar degree of effect on those with or without clinical levels at baseline. Similarly, the outcomes for posttraumatic stress disorder symptoms (IES-R) favored MCT at 4 months, but the difference was lost at 12 months. The loss of significant differences at 12 months in depression and posttraumatic stress disorder symptoms likely reflects the natural time-course by which these symptoms are known to improve over a 6- to 12-month period (Diagnostic and Statistical Manual of Mental Diorders, 5th edition).35 Regardless, the results suggest broader advantageous effects in the MCT+CR group in more rapid improvements of trauma-related symptoms and depressed mood. We found no evidence for an impact on EQ5D utility or VAS scores. These outcomes will be explored in more depth as part of a health economics analysis that will be the focus of a separate publication.
We included measures of psychological mechanism variables linked to the underlying model of MCT. These included metacognitive beliefs (MCQ-30), the MCQ-30 subscale of negative beliefs about thoughts on uncontrollability and danger, and repetitive negative thinking and unhelpful coping strategies assessed with CAS-1R. In each case, the addition of MCT to CR led to medium to large improvements in outcomes over CR at posttreatment and at 12-month follow-up. Thus, the additional treatment appears to have reduced to a greater extent maladaptive metacognitive beliefs and repetitive and unhelpful coping styles, which are hypothesized mechanisms of psychological disorder.36
The present study sample is large and representative of patients in CR. For example, Sever et al37 reported that 66.4% of CR patients with a HADS ≥8 were male, and the mean age was 60.77 (SD = 10.53). Such sex and HADS data are comparable with our study. They also reported that patients with elevated distress had on average 4.90 (SD = 2.19) comorbid physical illnesses, which is similar to the current study, in which patients had on average 5.4.
There are limitations of the present study that should be considered when interpreting the findings. Of eligible patients, 53% declined participation or were unable to be contacted. Although this is a high proportion, it is in line with previous studies evaluating psychological intervention in CVD, which report 41% to 68% of eligible patients declining or unable to take part.5,34,38 Further research on reasons for declining may help to identify important factors in implementation.
Treatment was delivered by CR staff rather than specialists in psychological therapies, which may mean that group-MCT was not delivered optimally. We attempted to mitigate this by offering training and supervision in delivery of the treatment and providing a detailed treatment manual for staff to follow. However, it is notable that the effects are smaller than those found in the treatment of patients with primary mental health disorders using MCT.9–11 The smaller effect might be accounted for by the briefer nature of the treatment used here and the inexperience of cardiac staff delivering a psychological intervention. In addition, disease factors such as physical disability and poorer physical health might also impact the effects observed.
The provision of group-MCT necessitated greater patient contact hours, and we do not know how much this contributed to the effects. However, our aim was not to address questions on active ingredients of treatment but a more pressing need about whether or not depression and anxiety outcomes could be improved. Last, we did not intend to assess the impact on cardiac and physical health outcomes, which would have required a larger sample size, but this is an important question for future studies. Because psychological distress can influence secondary prevention behaviors, assessment of behavior change should be an important outcome for future research in this area.
In conclusion, group-MCT in routine CR appears to be safe and effective in reducing anxiety and depression and improving psychological outcomes beyond those achieved in usual care. The benefits appeared to be stable over a 12-month follow-up period. The effect sizes are comparable with the best existing study outcomes for depression, while exceeding other studies in reducing anxiety. An implication is that the intervention might be incorporated in routine CR as a first-line approach for patients with anxiety and depression, with more complex specialist-delivered mental health interventions offered subsequently to nonresponders or those requiring additional help. The present study did not aim to test cardiac event outcomes, and therefore we have tempered our consideration of implications of the study in this respect. However, our results suggest that in patients showing distress symptoms, combining MCT with CR reliably improved anxiety and depression for 1 in 3, while cutting rates of deterioration in others. The psychological benefits and reduced risks could be substantial if MCT was offered to the 90 000 patients in the United Kingdom commencing CR annually.16 In conclusion, group-MCT has the potential to significantly improve psychological outcomes in patients with CVD and offer added value over standard CR.
Acknowledgments
The authors thank the PATHWAY research assistants, Rebecca McPhillips, Helen Morley, Hannah Gaffney, and Rebecca Anderson, and PATHWAY administrator Wendy Clarke, who contributed to patient recruitment and study organization. The authors thank Dr Kirsten McNicoll for assisting A.W. and D.R. in grant preparation and members of the trial steering committee, Prof Kate Jolly, Prof Gill Lancaster, Prof Gerry Humphris, and Chris Houston. A.W. is the chief investigator, developed the initial trial protocol and design, developed the trial intervention and the metacognitive therapy treatment manual, trained the therapists and supervisors, and contributed to the first and subsequent drafts of the article. D.R. contributed to the trial design with particular emphasis on the design of the quantitative evaluation. D.R. conducted the analysis of the study and contributed to the first and subsequent drafts of the article. C.H. contributed to the analysis of the study and the first and subsequent drafts of the article. P.F. contributed to development of trial design and to article revisions. L.D. developed the health economics components of the trial and contributed to revisions of the article. A.H. contributed to development of the trial recruitment strategy and inclusion/exclusion criteria, and article revisions. P.D. contributed to development of the trial recruitment strategy, provided advice on recruitment of study sites, provided the team with data from the National Audit of Cardiac Rehabilitation database, and contributed to drafts of the article. L.C. contributed to the trial protocol, patient recruitment, trial management, and the first and subsequent drafts of the article. All authors edited the article and read and approved the final article.
Sources of Funding
This article presents independent research funded by the National Institute for Health Research under its Program Grants for Applied Research Program (grant No. RP-PG-1211-20011). The views expressed are those of the author(s) and not necessarily those of the National Institute for Health Research or the Department of Health.
Disclosures
Dr Wells is the director of the MCT-Institute and developer of MCT. A.W. has written books on cognitive behavior therapy and MCT. The other authors report no conflicts.
Nonstandard Abbreviations and Acronyms
- CAS-1R
- Cognitive-Attentional Syndrome 1–Revised
- CR
- cardiac rehabilitation
- CVD
- cardiovascular disease
- HADS
- Hospital Anxiety and Depression Scale
- IES-R
- Impact of Event Scale–Revised
- MCT
- metacognitive therapy
- MCQ-30
- Metacognitions Questionnaire 30
- MI
- multiple imputation
- RA
- research assistant
- SMD
- standardized mean difference
- SpACE
- Spatial Attention Control Exercise
- VAS
- visual analogue scale
Continuing medical education (CME) credit is available for this article. Go to http://cme.ahajournals.org to take the quiz.
The podcast and transcript are available as a Data Supplement at https://www.ahajournals.org/doi/suppl/10.1161/CIRCULATIONAHA.120.052428.
For Sources of Funding and Disclosures, see page 32.
Contributor Information
David Reeves, Email: david.reeves@manchester.ac.uk.
Lora Capobianco, Email: lora.capobianco@manchester.ac.uk.
Calvin Heal, Email: calvin.heal@manchester.ac.uk.
Linda Davies, Email: linda.davies@manchester.ac.uk.
Anthony Heagerty, Email: tony.heagerty@manchester.ac.uk.
Patrick Doherty, Email: patrick.doherty@york.ac.uk.
Peter Fisher, Email: peter.fisher@liverpool.ac.uk.
References
- 1.World Health Organization (WHO). WHO Global NCD Action Plan 2013–2020. 2013. WHO; Accessed June 10, 2020. https://www.who.int/nmh/events/ncd_action_plan/en/. [Google Scholar]
- 2.Meijer A, Conradi HJ, Bos EH, Thombs BD, van Melle JP, de Jonge P. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis of 25 years of research. Gen Hosp Psychiatry. 2011;33:203–216. doi: 10.1016/j.genhosppsych.2011.02.007 [DOI] [PubMed] [Google Scholar]
- 3.Palacios J, Khondoker M, Mann A, Tylee A, Hotopf M. Depression and anxiety symptom trajectories in coronary heart disease: a ssociations with measures of disability and impact on 3-year health care costs. J Psychosom Res. 2018;105:1–8. doi: 10.1016/j.jpsychores.2017.10.015 [DOI] [PubMed] [Google Scholar]
- 4.Lespérance F, Frasure-Smith N, Koszycki D, Laliberté MA, van Zyl LT, Baker B, Swenson JR, Ghatavi K, Abramson BL, Dorian P, et al. ; CREATE Investigators. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA. 2007;297:367–379. doi: 10.1001/jama.297.4.367 [DOI] [PubMed] [Google Scholar]
- 5.Carney RM, Blumenthal JA, Freedland KE, Youngblood M, Veith RC, Burg MM, Cornell C, Saab PG, Kaufmann PG, Czajkowski SM, et al. Depression and late mortality after myocardial infarction in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) study. Psychosom Med. 2004;66:466–474. doi: 10.1097/01.psy.0000133362.75075.a6 [DOI] [PubMed] [Google Scholar]
- 6.Richards SH, Anderson L, Jenkinson CE, Whalley B, Rees K, Davies P, Bennett P, Liu Z, West R, Thompson DR, et al. Psychological interventions for coronary heart disease. Cochrane Database Syst Rev. 2017;4:CD002902. doi: 10.1002/14651858.CD002902.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wells A. Metacognitive Therapy for Anxiety and Depression. 2009. Guilford Press [Google Scholar]
- 8.McPhillips R, Salmon P, Wells A, Fisher P. Qualitative analysis of emotional distress in cardiac patients from the perspectives of cognitive behavioral and metacognitivetheories: why might cognitive behavioral therapy have limited benefit, and might metacognitive therapy be more effective? Front Psychol. 2018;9:2288. doi: 10.3389/fpsyg.2018.02288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nordahl HM, Borkovec TD, Hagen R, Kennair LEO, Hjemdal O, Solem S, Hansen B, Haseth S, Wells A. Metacognitive therapy versus cognitive-behavioural therapy in adults with generalised anxiety disorder. BJPsych Open. 2018;4:393–400. doi: 10.1192/bjo.2018.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Callesen P., Reeves D., Heal C, Wells A. Metacognitive therapy versus cognitive behaviour therapy in a dults with major depression: a parallel single-blind randomised trial. Sci Rep. 2020;10:7878. doi: 10.1038/s41598-020-64577-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Normann N, Morina N. The efficacy of metacognitive therapy: a systematic review and meta-analysis. Front Psychol. 2018;9:2211. doi: 10.3389/fpsyg.2018.02211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson L, Oldridge N, Thompson DR, Oldridge N., Zwisler AD., Rees K., Martin N., Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2016;67:1–12. doi: 10.1002/14651858.CD001800.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cowie A, Buckley J, Doherty P, Furze G, Hayward J, Hinton S, Jones J, Speck L, Dalal H, Mills J; British Association for Cardiovascular Prevention and Rehabilitation (BACPR). Standards and core components for cardiovascular disease prevention and rehabilitation. Heart. 2019;105:510–515. doi: 10.1136/heartjnl-2018-314206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wells A, McNicol K, Reeves D, Salmon P, Davies L, Heagerty A, Doherty P, McPhillips R, Anderson R, Faija C, et al. Improving the effectiveness of psychological interventions for depression and anxiety in the cardiac rehabilitation pathway using group-based metacognitive therapy (PATHWAY Group MCT): study protocol for a randomised controlled trial. Trials. 2018;19:215. doi:10.1186/s13063-018-2593-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 16.National Audit of Cardiac Rehabilitation (NACR). Annual report. 2019. British Heart Foundation, University of York; https://www.bhf.org.uk/informationsupport/publications/statistics/national-audit-of-cardiac-rehabilitation-quality-and-outcomes-report-2019 [Google Scholar]
- 17.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3 [DOI] [PubMed] [Google Scholar]
- 18.Scott NW, McPherson GC, Ramsay CR, Campbell MK. The method of minimization for allocation to clinical trials. A review. Control Clin Trials. 2002;23:662–674. doi: 10.1016/s0197-2456(02)00242-8 [DOI] [PubMed] [Google Scholar]
- 19.British Association of Cardiovascular Prevention and Rehabilitation (BACPR). The BACPR standards and core components for cardiovascular disease prevention and rehabilitation. 2017. 3rd e. d. http://www.bacpr.com/resources/AC6_BACPRStandards&CoreComponents2017.pdf [Google Scholar]
- 20.Greenberger D, Padesky C. Mind Over Mood: A Cognitive Therapy Treatment Manual for Clients. 1995. Guilford Press [Google Scholar]
- 21.Weiss DS, Marmar CR. Wilson JP, Leane TM, eds. The Impact of Event Scale—Revised. In: Assessing Psychological Trauma and PTSD. 1997. Guildford Press; 399–411. [Google Scholar]
- 22.Wells A, Cartwright-Hatton S. A short form of the metacognitions questionnaire: properties of the MCQ-30. Behav Res Ther. 2004;42:385–396. doi: 10.1016/S0005-7967(03)00147-5 [DOI] [PubMed] [Google Scholar]
- 23.Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Bonsel G, Badia X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20:1727–1736. doi: 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, Lloyd A, Scalone L, Kind P, Pickard AS. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15:708–715. doi: 10.1016/j.jval.2012.02.008 [DOI] [PubMed] [Google Scholar]
- 25.National Institute for Health and Care Excellence. Position statement on use of the EQ-5D-5L valuation set. Updated October 2019 https://www.nice.org.uk/Media/Default/About/what-we-do/NICE-guidance/NICE-technology-appraisal-guidance/eq5d5l_nice_position_statement.pdf. Accessed June 5, 2020.
- 26.Wells A. Cognitive Attentional Syndrome Scale 1 Revised (CAS-1R). 2015. University of Manchester [Google Scholar]
- 27.Baumeister H, Hutter N, Bengel J. Psychological and pharmacological interventions for depression in patients with coronary artery disease. Cochrane Database Syst Rev. 2011;9:CD008012. do:10.1002/14651858.CD008012.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wells A, Reeves D, Heal C, Fisher P, Davies L, Heagerty A, Doherty P, Capobianco L. Establishing the feasibility of group metacognitive therapy for anxiety and depression in cardiac rehabilitation: a single bind randomized pilot study. Front Psychiatry. 2020;11:582. doi:10.3389/fpsyt.2020.00582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Littell RC, Pendergast J, Natarajan R. Modelling covariance structure in the analysis of repeated measures data. Stat Med. 2000;19:1793–1819. doi: 10.1002/1097-0258(20000715)19:13<1793::aid-sim482>3.0.co;2-q [DOI] [PubMed] [Google Scholar]
- 30.Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20:40–49. doi: 10.1002/mpr.329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Higgins JPT, Li T, Deeks JJ.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, eds. Chapter 6: choosing effect measures and computing estimates of effect. In: Cochrane Handbook for Systematic Reviews of Interventions Version 6.0. Updated July 2019. 2019. Cochrane; https://www.training.cochrane.org/handbook [Google Scholar]
- 32.Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12 [DOI] [PubMed] [Google Scholar]
- 33.Huffman JC, Mastromauro CA, Beach SR, Celano CM, DuBois CM, Healy BC, Suarez L, Rollman BL, Januzzi JL. Collaborative care for depression and anxiety disorders in patients with recent cardiac events: the Management of Sadness and Anxiety in Cardiology (MOSAIC) randomized clinical trial. JAMA Intern Med. 2014;174:927–935. doi: 10.1001/jamainternmed.2014.739 [DOI] [PubMed] [Google Scholar]
- 34.Davidson KW, Bigger JT, Burg MM, Carney RM, Chaplin WF, Czajkowski S, Dornelas E, Duer-Hefele J, Frasure-Smith N, Freedland KE, et al. Centralized, stepped, patient preference-based treatment for patients with post-acute coronary syndrome depression: CODIACS vanguard randomized controlled trial. JAMA Intern Med. 2013;173:997–1004. doi: 10.1001/jamainternmed.2013.915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 2013. Fifth Ed. Arlington, VA: American Psychiatric Association [Google Scholar]
- 36.Wells A. Breaking the cybernetic code: understanding and treating the human metacognitive control system to enhance mental health. Front Psychol. 2019;10:2621. doi: 10.3389/fpsyg.2019.02621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sever S, Harrison AS, Golder S, Doherty P. Determinants of depression in patients with comorbid depression following cardiac rehabilitation. Open Heart. 2019;6:e000973. doi: 10.1136/openhrt-2018-000973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blumenthal JA, Sherwood A, Smith PJ, Watkins L, Mabe S, Kraus WE, Ingle K, Miller P, Hinderliter A. Enhancing cardiac rehabilitation with stress management training: a randomized, clinical efficacy trial. Circulation. 2016;133:1341–1350. doi: 10.1161/CIRCULATIONAHA.115.018926 [DOI] [PMC free article] [PubMed] [Google Scholar]


