Abstract
Background
People with spatial neglect after stroke or other brain injury have difficulty attending to one side of space. Various rehabilitation interventions have been used, but evidence of their benefit is unclear.
Objectives
The main objective was to determine the effects of non‐pharmacological interventions for people with spatial neglect after stroke and other adult‐acquired non‐progressive brain injury.
Search methods
We searched the Cochrane Stroke Group Trials Register (last searched October 2020), the Cochrane Central Register of Controlled Trials (CENTRAL; last searched October 2020), MEDLINE (1966 to October 2020), Embase (1980 to October 2020), the Cumulative Index to Nursing and Allied Health Literature (CINAHL; 1983 to October 2020), and PsycINFO (1974 to October 2020). We also searched ongoing trials registers and screened reference lists.
Selection criteria
We included randomised controlled trials (RCTs) of any non‐pharmacological intervention specifically aimed at spatial neglect. We excluded studies of general rehabilitation and studies with mixed participant groups, unless separate neglect data were available.
Data collection and analysis
We used standard Cochrane methods. Review authors categorised the interventions into eight broad types deemed to be applicable to clinical practice through iterative discussion: visual interventions, prism adaptation, body awareness interventions, mental function interventions, movement interventions, non‐invasive brain stimulation, electrical stimulation, and acupuncture. We assessed the quality of evidence for each outcome using the GRADE approach.
Main results
We included 65 RCTs with 1951 participants, all of which included people with spatial neglect following stroke. Most studies measured outcomes using standardised neglect assessments. Fifty‐one studies measured effects on ADL immediately after completion of the intervention period; only 16 reported persisting effects on ADL (our primary outcome). One study (30 participants) reported discharge destination, and one (24 participants) reported depression. No studies reported falls, balance, or quality of life. Only two studies were judged to be entirely at low risk of bias, and all were small, with fewer than 50 participants per group. We found no definitive (phase 3) clinical trials. None of the studies reported any patient or public involvement.
Visual interventions versus any control: evidence is very uncertain about the effects of visual interventions for spatial neglect based on measures of persisting functional ability in ADL (2 studies, 55 participants) (standardised mean difference (SMD) ‐0.04, 95% confidence interval (CI) ‐0.57 to 0.49); measures of immediate functional ability in ADL; persisting standardised neglect assessments; and immediate neglect assessments.
Prism adaptation versus any control: evidence is very uncertain about the effects of prism adaptation for spatial neglect based on measures of persisting functional ability in ADL (2 studies, 39 participants) (SMD ‐0.29, 95% CI ‐0.93 to 0.35); measures of immediate functional ability in ADL; persisting standardised neglect assessments; and immediate neglect assessments.
Body awareness interventions versus any control: evidence is very uncertain about the effects of body awareness interventions for spatial neglect based on measures of persisting functional ability in ADL (5 studies, 125 participants) (SMD 0.61, 95% CI 0.24 to 0.97); measures of immediate functional ability in ADL; persisting standardised neglect assessments; immediate neglect assessments; and adverse events.
Mental function interventions versus any control: we found no trials of mental function interventions for spatial neglect reporting on measures of persisting functional ability in ADL. Evidence is very uncertain about the effects of mental function interventions on spatial neglect based on measures of immediate functional ability in ADL and immediate neglect assessments.
Movement interventions versus any control: we found no trials of movement interventions for spatial neglect reporting on measures of persisting functional ability in ADL. Evidence is very uncertain about the effects of body awareness interventions on spatial neglect based on measures of immediate functional ability in ADL and immediate neglect assessments.
Non‐invasive brain stimulation (NIBS) versus any control: evidence is very uncertain about the effects of NIBS on spatial neglect based on measures of persisting functional ability in ADL (3 studies, 92 participants) (SMD 0.35, 95% CI ‐0.08 to 0.77); measures of immediate functional ability in ADL; persisting standardised neglect assessments; immediate neglect assessments; and adverse events.
Electrical stimulation versus any control: we found no trials of electrical stimulation for spatial neglect reporting on measures of persisting functional ability in ADL. Evidence is very uncertain about the effects of electrical stimulation on spatial neglect based on immediate neglect assessments.
Acupuncture versus any control: we found no trials of acupuncture for spatial neglect reporting on measures of persisting functional ability in ADL. Evidence is very uncertain about the effects of acupuncture on spatial neglect based on measures of immediate functional ability in ADL and immediate neglect assessments.
Authors' conclusions
The effectiveness of non‐pharmacological interventions for spatial neglect in improving functional ability in ADL and increasing independence remains unproven. Many strategies have been proposed to aid rehabilitation of spatial neglect, but none has yet been sufficiently researched through high‐quality fully powered randomised trials to establish potential or adverse effects. As a consequence, no rehabilitation approach can be supported or refuted based on current evidence from RCTs. As recommended by a number of national clinical guidelines, clinicians should continue to provide rehabilitation for neglect that enables people to meet their rehabilitation goals. Clinicians and stroke survivors should have the opportunity, and are strongly encouraged, to participate in research. Future studies need to have appropriate high‐quality methodological design, delivery, and reporting to enable appraisal and interpretation of results. Future studies also must evaluate outcomes of importance to patients, such as persisting functional ability in ADL. One way to improve the quality of research is to involve people with experience with the condition in designing and running trials.
Plain language summary
Non‐drug treatments for spatial neglect/inattention following stroke or adult brain injury
What is the review about? Spatial neglect, or inattention, is a condition that affects many brain injury survivors, particularly stroke survivors. It reduces a person's awareness of one side of the body or of the surrounding environment. This can affect a person's ability to carry out many everyday tasks such as eating, reading, and getting dressed, which can reduce independence.
What did we want to know? We wanted to find out if non‐drug treatments: • improve patients' ability to complete daily living activities; and • reduce spatial neglect.
What did we do? We reviewed evidence from randomised trials ‐ studies that compared one treatment to another by randomly assigning people with stroke or brain injury to one or the other treatment.
Evidence from 1966 to October 2020 was reviewed.
What evidence did we find? We found 65 studies involving 1951 participants.
All studies included participants with spatial neglect as a result of stroke. It is surprising that only one study included three participants with spatial neglect caused by another type of brain injury.
All studies included participants with right‐sided damage to the brain; seven studies also included participants with left‐sided damage.
Studies were considered small, with 4 to 69 participants (average 30). Eight studies included 50 or more participants; four studies involved 10 or fewer.
None of the studies reported any patient or public involvement in how the studies were designed, conducted, or reported.
We categorised the studies into eight different types of treatments.
• Visual treatment: 17 studies involving 398 participants explored visual treatments. All treatments encouraged eye movement or scanning by a range of methods including paper‐based tasks, computer activities, and daily living activities.
• Prism adaptation training: 8 studies involving 257 participants explored prism adaptation training. This involved participants wearing glasses with prism lenses during a pointing activity.
• Body awareness treatments: 12 studies involving 447 participants explored body awareness treatments. These studies involved various physical, visual, or verbal prompting or cueing aimed at increasing awareness of the affected side.
• Mental function treatments: 7 studies involving 170 participants explored treatments that focused on mental processing/thinking (e.g. mental imagery, virtual reality).
• Movement treatments: 6 studies involving 220 participants explored treatments that used movement of the arm or the whole body. These included the use of robotics, visual and motor feedback, and restricting movement on the side of the body that was not affected.
• Non‐invasive brain stimulation: 17 studies involving 467 participants explored non‐invasive brain stimulation. These involved different methods of applying electrical or magnetic stimulation to the skull to change brain activity.
• Electrical stimulation: 8 studies involving 270 participants explored electrical stimulation to other parts of the body. These involved sending mild electrical impulses to a particular part of the body (e.g. the arm). Four different types of electrical stimulation were used.
• Acupuncture: 2 studies involving 104 participants explored the use of acupuncture. These involved inserting thin needles into specific points in the body.
What was the quality of the evidence? We rated the evidence on use of these treatments and found it to be of very low quality due to:
• the small size of studies; • differences between studies within each of the eight treatment categories, including participant characteristics, types of treatments, and assessments used to measure changes; and • concerns about how participants were randomised, and whether people carrying out the assessments were "blinded" (i.e. knew which treatment each patient received).
What were the main results?
Most studies used standard tests of spatial neglect. Many also measured effects on daily living activities soon after treatment, but very few reports described longer‐term effects.
Other meaningful treatment outcomes were rarely reported.
Overall we found only very low‐quality evidence about whether these treatments had benefits or harms for people with spatial neglect.
What does this mean?
Despite 65 (small) trials, the benefits or risks of non‐drug treatments for reducing neglect and increasing independence remain unknown. It would be a mistake to interpret this review as concluding that the proposed treatments are ineffective. Rather, we conclude that evidence for or against any treatment used within randomised trials conducted worldwide is insufficient. Future trials must be of much higher quality to answer important clinical questions. One way to improve research quality is to involve patients in designing and running the trial. Clinicians should continue to follow national clinical guidelines and are strongly encouraged to participate in trials. People with spatial neglect should continue to receive general stroke or neurological rehabilitation that enables them to meet their rehabilitation goals, including any available intervention for neglect. People with spatial neglect should also have the opportunity to take part in high‐quality research.
Summary of findings
Background
Description of the condition
Brain injury, including stroke, can affect cognitive as well as physical and sensory abilities (Wade 1985). Cognitive deficits include a disorder of spatial awareness or attention known as spatial neglect or inattention. The most widely quoted definition of neglect is a description of the resulting behavioural disabilities: "fails to report, respond, or orient to novel or meaningful stimuli presented to the side opposite a brain lesion" (Heilman 2003). Neglect is not due to a sensory or motor impairment, although these often co‐occur. Neglect is a disorder that can reduce a person's ability to look, listen, or make movements towards one‐half of their environment. This disorder can also affect an individual's ability to carry out everyday tasks, such as eating, reading, and getting dressed (Nijboer 2013).
Many patients are unaware that they have the disorder (anosognosia), which makes treatment more complex. Brain injury may differentially affect the ability to direct attention in visual, auditory, and tactile modalities. Several different subtypes of neglect have been identified, and little consensus has been reached on how these are identified or categorised (Checketts 2020). As a result, many different terms are used in research and in clinical practice (e.g. visual neglect, hemi‐neglect, egocentric neglect, personal neglect, inattention) (Rode 2017). Although neglect of left space is more common than neglect of right space, either can occur and both are disabling.
A majority of cases of adult‐acquired spatial neglect occur following stroke. It is not surprising, given the clinical heterogeneity of the neglect syndrome, that the reported incidence of neglect in stroke patients varies hugely. An analysis of recent national audit data from 88,000 UK stroke survivors found that at least 30% screened positive in the acute phase and had a much longer stay in hospital (Hammerbeck 2019). In the light of functional implications of neglect, rehabilitation is an important aim.
For the purposes of this review update, we have chosen to use the term 'neglect' for consistency with previous versions of this review, and to distinguish this review from reviews of attentional deficits after stroke (Loetscher 2019). Based on consultation with stroke survivors who were involved in this update, we have also included the preferred term 'inattention' in the review title and in the Background section of the Plain Language Summary.
Description of the intervention
Many different interventions are used in the rehabilitation of spatial neglect, all of which aim to reduce the adverse effects that cognitive impairments may have on a person’s ability to perform everyday activities, as well as on an individual's social participation and quality of life. Traditionally, non‐pharmacological rehabilitation is the main treatment method, although pharmacological treatments also exist and have been reviewed elsewhere (Luvizutto 2015). In the current update and expansion of this review of non‐pharmacological interventions, we have categorised them into eight types, as described below. We have noted differences in delivery mode (e.g. therapist‐delivered, self‐directed), professionals involved (e.g. occupational therapists, psychologists), settings (e.g. inpatient, community based), and dose (e.g. length and frequency of intervention sessions).
How the intervention might work
Interventions for spatial neglect might aim to train individuals to voluntarily compensate for their neglect and require awareness of the disorder; or they might aim to modify underlying factors (i.e. to alter impaired representation of space without requiring awareness of the disorder). For the purposes of this review, we (VL, CH, AB) identified interventions used in each included study; we then developed eight broad groupings through discussion to categorise the non‐pharmacological neglect interventions as follows.
Visual interventions: examples include visual scanning training aimed at active and purposeful exploration of the visual field; training of saccadic or pursuit eye movement using static or moving stimuli; or half‐visual field eye‐patching, which induces visual exploration of neglected space.
Prism adaptation training: patients point at a visual target wearing ipsilesional prisms. Patients initially mis‐reach, then compensate for this error by recalibrating their pointing movements to point accurately (adaptation). This adaptation persists after removal of the prisms (Rossetti 1998).
Body awareness interventions: examples include verbal cueing, devices delivering sensory cues, biofeedback, and focused movement ‐ all aimed to cue awareness of the neglected side of the body or space.
Mental function interventions: these include treatments that focus on mental processing/thinking aimed at improving motor and visual representation without physical activity (e.g. mental imagery, virtual reality).
Movement‐based interventions: examples include upper limb training or balance training, in which specific training of the affected limb or the whole body has an indirect effect on reducing neglect.
Non‐invasive brain stimulation (NIBS): manipulating excitability of the motor cortex has been found to cause changes to sensory and motor functions post stroke, including neglect symptoms (Müri 2013). Methods include repetitive transcranial magnetic stimulation (rTMS), including inhibitory or excitatory theta burst stimulation (TBS); and transcranial direct current stimulation (tDCS).
Electrical stimulation: examples include passive transcutaneous electrical stimulation to the hand and galvanic vestibular stimulation (GVS), which manipulates stimulation of the vestibular and proprioceptive system. Stimulation used is often below the threshold of perception so differs among patients cued to attend to the stimulated side.
Acupuncture: a form of complementary stroke treatment that may improve motor function by continually stimulating the nervous system during treatment (Hou 2020).
Why it is important to do this review
The two main reasons for this review are, first, that neglect is a major problem for people with adult‐acquired brain injury, particularly stroke, and second, there is clinical uncertainty about the effectiveness of rehabilitation for this cognitive impairment. Spatial neglect affects long‐term outcomes. It can impede active participation in rehabilitation programmes, decrease independence in activities of daily living (ADL) and quality of life, and increase caregiver burden (Bosma 2020; Hammerbeck 2019; Jehkonen 2006). This updated review aimed to systematically consider evidence from randomised controlled trials (RCTs) on the effectiveness of any non‐pharmacological intervention for people with spatial neglect. Previous versions of this review included only cognitive rehabilitation interventions and stroke populations. We have chosen to expand the inclusion criteria (participants and interventions) to increase relevance for clinical practice and to guide future researchers by examining the quality and certainty of existing evidence.
Stroke survivor involvement in this review
We consulted three stroke survivors with experience of spatial neglect in the analysis and dissemination stages of this review update to improve the relevance of our findings to patients. One co‐author (CM or KWN) met with the group regularly to inform group members of progress, and we gathered feedback on results and conclusions. The group provided input to the plain language summary to improve accessibility and relevance to stroke survivors. Our patient involvement was limited to stroke survivors and could have been changed by also including carers.
Objectives
The main objective was to determine the effects of non‐pharmacological interventions for people with spatial neglect after stroke and other adult‐acquired non‐progressive brain injury.
Specific objectives
To assess the effects of non‐pharmacological interventions on:
functional ability in ADL and spatial neglect at an impairment level, (measured at two timepoints: immediately post intervention and persisting at least one month post intervention);
proportion of patients not discharged to their usual residence;
falls; balance; depression/anxiety; quality of life persisting at least one month post intervention; and
adverse events.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials only. As our primary outcome entails persisting effects of treatment (defined as the effect at least one month after completion of the intervention), we excluded trials that could not by design consider this. For example, we excluded early‐phase trials that delivered an intervention not intended to have lasting effects as well as trials that crossed participants over to an alternative intervention before persisting effects could be measured. Cross‐over trials are not appropriate for rehabilitation for cognitive impairment, as the effects of one approach may contaminate the next. We did not exclude trials that simply failed to record or report persisting effects.
All previously included trials that have been excluded in this update are listed in the Characteristics of excluded studies table.
Types of participants
We included participants with spatial neglect following any adult‐acquired non‐progressive brain injury. We expected the majority of such individuals to be stroke patients. Stroke was confirmed by neurological examination or by brain scanning, or both, and spatial neglect by neuropsychological assessment. We excluded studies of people with general perceptual problems unless a subgroup with neglect could be identified. A separate review has been published on cognitive rehabilitation for people with perceptual problems (Bowen 2011).
Types of interventions
To be included in the review, a clinical trial had to report a comparison between an active treatment group that received an intervention specifically targeting neglect versus a control group that received either an alternative form of treatment or none. Rehabilitation was broadly defined to include an activity designed to directly reduce the severity of neglect impairment or of the resulting disability. The intervention had to directly target neglect rather than examine whether people with neglect happened to benefit from general rehabilitation services. We excluded pharmacological (drug) treatments and invasive procedures.
Types of outcome measures
We were interested in outcomes at two time points: (1) persisting at least one month beyond completion of the intervention (i.e. follow‐up outcome), and (2) immediately after completion of an intervention. When more than one follow‐up time point was eligible for inclusion, we selected the latest within six months of completion of the intervention. We did not extract data on precise time points.
Primary outcomes
Functional ability in activities of daily living (ADL)
For the primary outcome, we were interested only in the effect of any treatment, measured at the functional level, persisting for at least one month beyond completion of the intervention. We included the following scales: Catherine Bergego Scale (Azouvi 1996), Everyday Neglect Questionnaire (Towle 1991), Nottingham Extended Activities of Daily Living Scale (Nouri 1987), Lawton Instrumental Activities of Daily Living (Graf 2008), Frenchay Activities Index (Holbrook 1983), Rivermead ADL (Lincoln 1990), Edmans EADL (Edmans 1997), Modified Rankin Scale (Wilson 2005), Barthel ADL Index (Collin 1988), Functional Independence Measure (Keith 1987), Katz Index of Activities of Daily Living (Katz 1963), and Rehabilitation Activities Profile (Van Bennekom 1995). When more than one of these scales was reported, we used the scale listed first above. We excluded non‐standardised functional measures designed for a specific study (e.g. avoiding obstacles, observing an ADL task).
Secondary outcomes
We included the following secondary outcomes.
Ratings on measures of functional ability in ADL (as specified above) recorded immediately after completion of the intervention.
Performance on a standardised neglect assessment. We separately analysed persisting and immediate effects as defined above. When more than one eligible outcome was presented, we chose the first of target cancellation (single letter, double letter, line, shape) or line bisection. In addition to a conventional subtest score (such as letter cancellation), we used the behavioural summary score from the Behavioural Inattention Test (BIT) when available (Wilson 1987).
Discharge destination: whether persons were discharged to live in their own home or to a care facility was included when available, with death before discharge treated as not discharged to their own home.
Balance measured as a persisting effect: Berg Balance Scale (Berg 1992), Functional Reach (Duncan 1990), Get Up and Go Test (Podsiadlo 1991), Standing Balance Test, Step Test (Hill 1996), or other standardised balance measures. We did not include measures of weight distribution or postural sway during standing, as the relationship between ability to maintain balance and these outcomes has not been established.
Falls measured as a persisting effect: number of reported falls, Falls Efficacy Scale (Yardley 2005).
Depression/anxiety measured as a persisting effect (e.g. Hospital Anxiety and Depression Scale (Zigmond 1983), Beck Depressive Inventory (Beck 1961), General Health Questionnaire (Goldberg 1970), Geriatric Depression Scale (Yesavage 1983)).
Quality of life and social isolation as a persisting effect: EuroQoL Group Quality of Life Questionnaire based on 5 dimensions (EQ‐5D), Health‐Related Quality of Life Scale (Flanagan 1978), Quality of Well‐Being Scale (Bush 2006), and Short Form Health Survey (SF‐36) (Ware 1992).
Adverse events (excluding falls) such as death or accident before final scheduled follow‐up.
Search methods for identification of studies
See the 'Specialised Register' section at the Cochrane Stroke Group website. We searched for relevant trials in all languages and arranged translation of trial reports published in languages other than English.
Electronic searches
We developed search strategies with the help of the Cochrane Stroke Group Trials Information Specialist. We searched the Cochrane Stroke Group Trials Register (October 2020) and the following electronic databases.
Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 10), in the Cochrane Library (searched 20 October 2020) (Appendix 1).
MEDLINE Ovid (1946 to 20 October 2020) (Appendix 2).
Embase Ovid (1974 to 20 October 2020) (Appendix 3).
Cumulative Index to Nursing and Allied Health Literature (CINAHL; EBSCO; 1982 to 20 October 2020) (Appendix 4).
PsycINFO Ovid (from 1806 to 20 October 2020) (Appendix 5).
Searching other resources
In an effort to identify further published, unpublished, and ongoing trials, we searched the following registers of ongoing trials.
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov; 20 October 2020) (Appendix 6).
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; 20 October 2020) (Appendix 7).
We searched the ORCID and ResearchGate pages of principal investigators identified from trial registries for relevant publications. We screened reference lists of all relevant articles and contacted experts in the field. We also checked Cochrane Reviews of NIBS for relevant studies through liaison with those review authors (Elsner 2020).
See Appendix 8 for search methods used in previous versions of this review.
Data collection and analysis
The Cochrane Stroke Group Information Specialist ran all electronic searches. One review author (VL or CJH) downloaded references into bibliographic software and removed duplicates. One review author (VL or CJH) excluded any titles that were obviously not related to stroke or other adult‐acquired non‐progressive brain injury and neglect. We obtained the abstracts for remaining references, and two review authors (of VL, CM, CJH, CH, and AB) independently considered each of these abstracts, excluded any studies that clearly were not RCTs, and excluded any studies for which the intervention was not specifically aimed at improving spatial neglect. Review authors resolved any disagreements through discussion, involving a third review author when necessary. We obtained the full papers for any studies included at this stage.
Selection of studies
Two review authors (of VL, CM, CH, CJH, AP, or AB) independently selected studies to be included in this review using the four inclusion criteria (types of trials, participants, interventions, and outcome measures). Each review author classified studies as 'include' or 'exclude'. We resolved disagreements by discussion involving a third review author.
Data extraction and management
We used a pre‐designed data extraction form to extract data from the included studies. Four review authors (VL, CM, AV, CJH) independently extracted data from the included trials. We extracted the following: eligibility criteria and baseline characteristics of participants, risk of bias criteria, numbers randomised and analysed, reported results, and publication details. We contacted study authors for further information or for clarification related to randomisation and primary outcomes only. We extracted descriptions of interventions using the Template for Intervention Description and Replication (TIDieR) checklist (Hoffman 2014).
We identified the intervention used in each study; then three review authors (VL, CH, and AB) developed broad groupings through discussion: prism adaptation training, non‐invasive brain stimulation, body awareness interventions, visual interventions, movement interventions, electrical stimulation, mental function interventions, and acupuncture. These groupings were developed using an iterative process to cover all intervention types identified.
Assessment of risk of bias in included studies
Two review authors (AV, CJH) independently documented risk of bias for all studies, classifying each as being at 'high risk', 'low risk', or 'unclear risk' for the following potential biases, using the Cochrane Collaboration Risk of Bias tool 1 for assessing risk of bias (Cochrane Handbook Chapter 8). Any differences were resolved through discussion, involving a third reviewer (VL) when necessary.
Allocation (selection bias). Studies with adequate allocation included those that reported a method of randomisation using a central system at a site remote from the study, computerised allocation in which records were in a locked readable file that could be assessed only after participant details were entered, or drawing of sequentially numbered, sealed opaque envelopes that allowed retrospective verification of the order. Studies with inadequate allocation included those using open lists or tombola systems.
Blinding (performance and detection bias). We thought it unlikely that any intervention could be blind to those delivering it. Adequate masking of participants included studies using a sham or placebo procedure and verifying its success. Adequate masking of outcome assessment included studies that stated that a masked (blinded) outcome assessor was used and verified.
Incomplete outcome data (attrition bias). Studies at low risk for this domain had no missing outcome data; missing outcome data that were unlikely to be related to true outcomes; few missing outcome data that were balanced across intervention groups; or missing data that had been imputed by appropriate methods.
Selective reporting (reporting bias). Studies were considered at low risk of bias if all recorded outcomes were reported in adequate detail to allow analysis.
Other potential sources of bias. Studies were considered at low risk if there was no evidence of other sources of bias, such as design flaws or unplanned interim analyses. We planned to study publication bias through funnel plot asymmetry if at least 10 studies were included in subgroup analyses.
Measures of treatment effect
We anticipated that multiple scales would be used by studies measuring the same underlying constructs. We therefore used the standardised mean difference (SMD) approach and interpreted results as SMD throughout. Our analyses used the fixed‐effect approach for all outcomes to provide a simple summary of available evidence.
We treated ADL data, such as the Barthel Index (BI), as continuous measures; we extracted, requested (from study authors), or calculated mean and standard deviation (SD) data. We are aware that there is a difference of opinion regarding how to deal with ordinal level ADL scales. We have treated them as interval level measures, as in practice this makes relatively little difference. This is supported by a study of parametric versus non‐parametric methods in stroke trials, which recommended that means and SDs should be reported (Song 2005). We used intention‐to‐treat analyses when possible.
For all such analyses, we entered data so that a higher score represented a favourable outcome, and the right side of the graph favoured the experimental group. Some of the neglect assessment studies reported outcomes for which a low score was better; for example, for 'number of errors' in cancellation tests and 'line bisection'. In this case, we multiplied these outcomes by ‐1 to pool them with other neglect assessments for which the direction of effect was opposite.
We used odds ratios (ORs) categorical outcomes. For 'discharge destination', we considered the odds of being discharged to their own homes. We treated deaths before discharge as 'not discharged to their own home'. We also calculated ORs for the outcome 'falls', comparing the number of participants experiencing at least one fall.
Unit of analysis issues
As described above, we excluded cross‐over trials from consideration as they were unable to assess our primary outcome of persisting differences in this context. When studies had repeated assessments of the same participant, we selected the measure immediately following intervention or, for persisting effect, the latest assessment between one and six months following scheduled completion of the intervention.
Dealing with missing data
If an included study did not record a particular outcome, we could not include that study in the analysis of that outcome.
If an included study had missing data (e.g. reported means but not standard deviations for follow‐up data), we first tried to calculate this from other statistics (e.g. P value), or we requested the information from study authors. As a last resort, we imputed a value typically equal to the largest SD observed in other studies contributing this outcome.
Assessment of heterogeneity
We visually assessed heterogeneity by looking at the extent of overlap of the CIs on forest plots. We considered an I² statistic over 50% as evidence of substantial heterogeneity. In this case, we explored individual trial characteristics to generate hypotheses regarding potential sources of heterogeneity.
Assessment of reporting biases
We attempted to minimise publication bias by using a comprehensive search strategy that included searching for unpublished studies and searching trials registers. When 10 or more trials contributed to a meta‐analysis, we examined the funnel plot for any evidence of asymmetry.
Data synthesis
One review author (VL) entered the data into RevMan 5.4.1 (RevMan 2020), and another review author (AV) checked entries; we resolved any inconsistencies through discussion, with reference to the original report.
Subgroup analysis and investigation of heterogeneity
We re‐structured the earlier review of cognitive rehabilitation approaches to separate comparisons for the eight categories of intervention.
Visual interventions.
Prism adaptation training.
Body awareness interventions.
Mental function interventions.
Movement interventions.
Non‐invasive brain stimulation.
Electrical stimulation.
Acupuncture.
Within each of these comparisons, we stratified analyses when appropriate by nature of intervention, nature of control group, and a categorisation summarising overall risk of bias to explore likely sources of heterogeneity in the results. No subgroup analyses were planned.
Sensitivity analysis
We planned to carry out sensitivity analyses to explore the effect of any imputation undertaken.
We then considered how results would have been changed if we had restricted eligibility to studies for which the size suggested a definitive phase 3 clinical trial, operationalised as allocating more than 50 participants to each intervention arm.
Finally, we considered how results would have been changed if we had restricted eligibility to those clearly at low risk of allocation bias and without clear evidence of high risk of bias in any other domain aside from blinding, which we believe would be impractical in this context.
Summary of findings and assessment of the certainty of the evidence
We presented results of the main analyses for each comparison in 'Summary of findings' tables.
We summarised data for our primary outcome of interest (persisting effects on functional ability in activities of daily living), the three secondary outcomes for which we identified the greatest volume of evidence (immediate effects on functional ability, persisting effects on neglect outcomes, immediate effects on neglect outcome), and any data related to adverse events.
For each of the outcomes, we assessed quality of the evidence using the GRADE approach (Guyatt 2011). One review author (VL) assessed quality of evidence, reported identified concerns, and applied downgrades. Other review authors (AB, AP, AV) checked agreement with these judgements and resolved any disagreements through discussion.
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification; and Characteristics of ongoing studies.
Results of the search
Results of the search are shown in Figure 1. We identified 25,695 records through the database searches. One review author (VL or CJH) eliminated 15,269 irrelevant titles. Two (of VL, CM, CJH, CH, AB) review authors screened the remaining abstracts against our inclusion criteria and reviewed the full text of 256 studies. We identified 65 studies for inclusion. We also identified 19 ongoing studies (see Characteristics of ongoing studies) and 13 studies awaiting assessment (see Studies awaiting classification).
1.
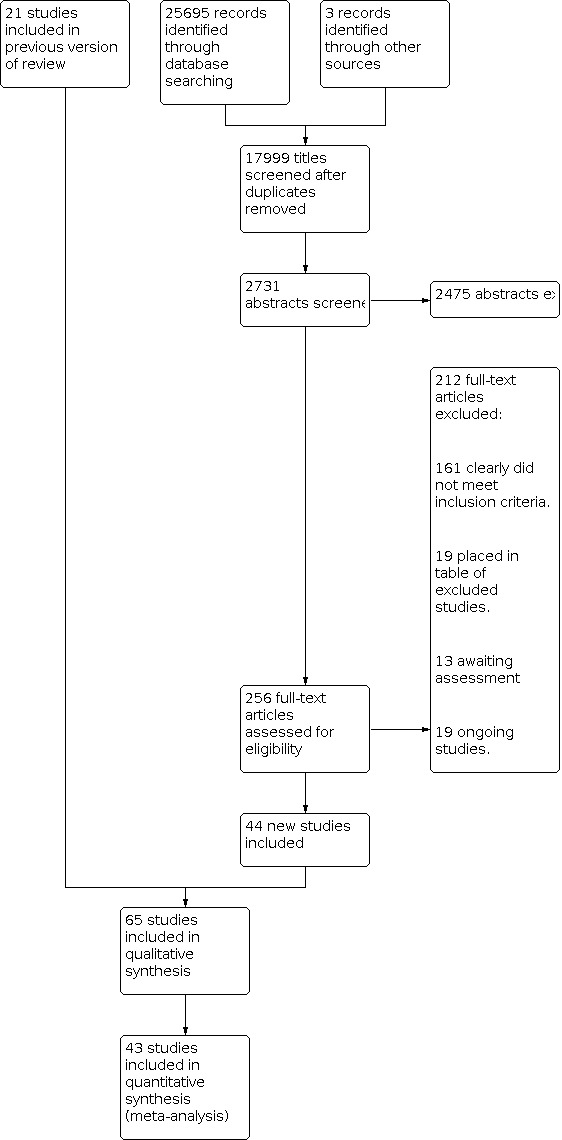
Study flow diagram.
Included studies
We included in this updated review 65 RCTs involving 1951 participants. Forty‐four of these were newly identified studies (Aparicio‐Lopez 2016; Bang 2015; Cazzoli 2012; Cha 2016; Choi 2016; Choi 2019; Dolkun 2019; Fong 2013; Fu 2017; Goedert 2020; Iwanski 2020; Karner 2019; Katz 2005; Kerkhoff 2014; Kim 2011; Kim 2013; Kim 2015; Kim 2018; Koch 2012; Kutlay 2018; Learmonth 2020; Li 2017; Machner 2012; Mancuso 2012; Nyfeller 2019; Pandian 2014; Park 2015; Park 2015b; Raghavan 2017; Rode 2015; Rossit 2019; Seniow 2016; Sesh 2018; Song 2009; Ten‐Brink 2017; Van Wyk 2014; Varalta 2019; Vatanparasti 2019; Volkening 2016; Wilkinson 2014; Wu 2013; Yang 2015; Yang 2017; Yi 2016). The previous version of this review included 23 RCTs (Cherney 2002; Cottam 1987; Edmans 2000; Fanthome 1995; Ferreira 2011; Fong 2007; Kalra 1997; Kerkhoff 2012; Luukkainen‐Markkula 2009; Mizuno 2011; Nys 2008; Polanowska 2009; Robertson 1990; Robertson 2002; Rusconi 2002; Schroder 2008; Tsang 2009; Turton 2010; Welfringer 2011; Wiart 1997; Zeloni 2002). We have excluded two of these studies from this update (Rossi 1990Weinberg 1977); see Excluded studies for reasoning.
Full descriptions of the included studies are presented in the Characteristics of included studies table. The table presents 72 entries due to the fact that three studies have multiple entries to enable comparisons when meta‐analysis is conducted (Nyfeller 2019; Yang 2015; Yi 2016).
Populations studied
All studies included people with spatial neglect after stroke. Whilst we expanded inclusion criteria for any type of brain injury, only one study also included a small number of non‐stroke patients (Robertson 1990). It is unclear whether brain damage in Schroder 2008 was the result of stroke or of other brain injury.
Fifty‐one of the 65 included studies included only participants with right hemisphere stroke. Seven included those with either left or right hemisphere lesions, although in each study, there were more people with right hemisphere lesions (Edmans 2000; Kalra 1997; Kutlay 2018; Pandian 2014; Robertson 1990; Ten‐Brink 2017; Van Wyk 2014). The remaining seven studies are unclear on the side of the lesion (Bang 2015; Cha 2016; Choi 2019; Park 2015; Varalta 2019; Vatanparasti 2019; Yang 2015). We did not extract data on stroke severity.
Sample size
All studies had small or extremely small sample sizes, with mean size of 30 participants and range from 4 to 69. Four studies had 10 or fewer participants (Cherney 2002; Ferreira 2011; Kerkhoff 2012; Zeloni 2002); only eight studies had 50 or more participants (Dolkun 2019; Kalra 1997; Fong 2007; Kutlay 2018; Nyfeller 2019; Ten‐Brink 2017; Wilkinson 2014; Yang 2017). No studies met our criterion of a large phase 3 trial (operationalised as allocating more than 50 participants to each intervention arm). Thirteen studies explicitly stated they were intended as pilot or feasibility studies (Cherney 2002; Fanthome 1995; Ferreira 2011; Fong 2013; Fu 2017; Kalra 1997; Learmonth 2020; Nys 2008; Rossit 2019; Turton 2010; Varalta 2019; Vatanparasti 2019; Welfringer 2011).
Interventions studied
A range of interventions were investigated (for full details, see Characteristics of included studies and TIDieR (TIDIER)). Fourteen studies explored two different types of interventions (Aparicio‐Lopez 2016; Bang 2015; Choi 2019; Ferreira 2011; Fong 2007; Katz 2005; Kim 2018; Learmonth 2020; Luukkainen‐Markkula 2009; Park 2015b; Rusconi 2002; Schroder 2008; Wu 2013; Yang 2017) (see Table 9).
1. Included studies interventions and comparisons.
| Study name | Active intervention 1 (subtype) | Active intervention 2 (if applicable) | Active intervention 3 (if applicable) | Control intervention |
| Aparicio‐Lopez 2016 | Visual (eye‐patching) + Mental function (cognitive rehabilitation) | Mental function (cognitive rehabilitation) | ||
| Bang 2015 | NIBS (tDCS) + Body awareness (mirror therapy) | Body awareness (mirror therapy) | ||
| Cazzoli 2012 | NIBS (TBS) | Sham | ||
| Cha 2016 | NIBS (rTMS) | Sham | ||
| Cherney 2003 | Visual (scanning) | Attention control | ||
| Choi 2016 | Movement (upper limb training) | Usual care | ||
| Choi 2019 | Prism adaptation | Electrical stimulation (FES) | Prism adaptation + Electrical stimulation (FES) | |
| Cottam 1987 | Visual (scanning) | No treatment | ||
| Dolkun 2019 | Acupuncture | Usual care | ||
| Edmans 2000 | Body awareness (perceptual training) | Attention control | ||
| Fanthome 1995 | Visual (eye movement feedback) | No treatment | ||
| Ferreira 2011 | Visual (scanning) | Mental function (mental practice) | ||
| Fong 2007 | Body awareness (trunk rotation) | Body awareness (trunk rotation) + Visual (eye‐patching) | Usual care | |
| Fong 2013 | Body awareness (sensory cueing) | Sham | ||
| Fu 2017 | NIBS (cTBS 80%) | NIBS (cTBS 40%) | ||
| Goedert 2020 | Prism adaptation | Usual care | ||
| Iwanski 2020 | NIBS (rTMS) + Visual (scanning) | Sham + Visual (scanning) | ||
| Kalra 1997 | Body awareness (sensory cueing) | Usual care | ||
| Karner 2019 | Body awareness (sensory cueing) | Attention control | ||
| Katz 2005 | Mental function (VR training) | Visual (scanning) | ||
| Kerkhoff 2012 | Visual (OKS) | Visual (scanning) | ||
| Kerkhoff 2014 | Visual (smooth pursuit training) | Visual (scanning) | ||
| Kim 2011 | Mental function (VR training) | Usual care | ||
| Kim 2013 | NIBS (high‐frequency rTMS) | NIBS (low‐frequency rTMS) | Sham | |
| Kim 2015 | NIBS (1 rTMS) + Visual (scanning) | NIBS (10 rTMS) + Visual (scanning) | ||
| Kim 2018 | NIBS (rTMS) | Movement (upper limb training) | NIBS (rTMS) + Movement (upper limb training) | |
| Koch 2012 | NIBS (cTBS) | Sham | ||
| Kutlay 2018 | Movement (balance training) | Usual care | ||
| Learmonth 2020 | NIBS (tDCS) | Movement (visuomotor feedback) | NIBS (tDCS) + Movement (visuomotor feedback) | Attention control |
| Li 2017 | Acupuncture | Usual care | ||
| Luukkainen‐Markkula 2009 | Body awareness (limb activation) | Visual (scanning) | ||
| Machner 2014 | Visual (OKS) + Visual (eye‐patching) | Usual care | ||
| Mancuso 2012 | Prism adaptation | Sham | ||
| Mizuno 2011 | Prism adaptation | Sham | ||
| Nyffeler 2019* | NIBS (8 cTBS) + Visual (smooth pursuit training) | NIBS (16 cTBS) + Visual (smooth pursuit training) | Sham + Visual (smooth pursuit training) | |
| Nys 2008 | Prism adaptation | Sham | ||
| Pandian 2014 | Body awareness (mirror therapy) | Sham | ||
| Park 2015 | Mental function (mental practice) | Usual care | ||
| Park 2015b | Mental function (mental practice) | Electrical stimulation | ||
| Polanowska 2009 | Electrical stimulation (TENS) + Visual (scanning) | Sham + Visual (scanning) | ||
| Raghavan 2017 | NIBS (rTMS) | Sham | ||
| Robertson 1990 | Visual (scanning) | Attention control | ||
| Robertson 2002 | Body awareness (limb activation) + Visual (scanning) | Sham + Visual (scanning) | ||
| Rode 2015 | Prism adaptation | Sham | ||
| Rossit 2019 | Movement (visuomotor feedback) | Attention control | ||
| Rusconi 2002 | Electrical stimulation (TENS) + Mental function (cognitive training) | Mental function (cognitive training) | ||
| Schroder 2008 | Electrical stimulation (TENS) + Visual (scanning) | Visual (OKS) + Visual (scanning) | Visual (scanning) | |
| Seniow 2016 | Electrical stimulation (TENS) + Visual (scanning) | Sham + Visual (scanning) | ||
| Sesh 2018 | Body awareness (sensory stimulation) | Usual care | ||
| Song 2009 | NIBS (rTMS) | Usual care | ||
| Ten‐Brink 2017 | Prism adaptation | Sham | ||
| Tsang 2009 | Visual (eye‐patching) | Usual care | ||
| Turton 2010 | Prism adaptation | Sham | ||
| Van Wyk 2014 | Visual (scanning) | Attention control | ||
| Varalta 2019 | Body awareness (neck taping) | Sham | ||
| Vatanparasti 2019 | NIBS (cTBS) + Prism adaptation | Sham NIBS + Prism adaptation | ||
| Volkening 2016 | Electrical stimulation (GVS) + Visual (scanning) | Sham + Visual (scanning) | ||
| Welfringer 2011 | Mental function (mental practice) | Usual care | ||
| Wiart 1997 | Body awareness (trunk rotation) | Usual care | ||
| Wilkinson 2014 | Electrical stimulation (1 GVS) | Electrical stimulation (5 GVS) | Electrical stimulation (5 GVS) | |
| Wu 2013 | Movement (CIMT) | Movement (CIMT) + Visual (eye‐patching) | Usual care | |
| Yang 2015* | NIBS (1 Hz TBS) | NIBS (10 Hz TBS) | NIBS (cTBS) | Sham |
| Yang 2017 | NIBS (rTMS) | NIBS (rTMS) + Body awareness (sensory cueing) | Usual care | |
| Yi 2016* | NIBS (anodal tDCS) | NIBS (cathodal tDCS) | Sham | |
| Zeloni 2002 | Visual (eye‐patching) | Usual care |
* Denotes studies with multiple entries in Characteristics of included studies table.
CIMT: constraint‐induced movement therapy. cTBS: continuous theta burst stimulation. GVS: galvanic vestibular stimulation. OKS: optokinetic stimulation. rTMS: repetitive transcranial magnetic stimulation. TBS: theta burst stimulation. tDCS: transcranial direct current stimulation. TENS: transcutaneous electrical nerve stimulation.
Visual interventions
We identified 17 studies involving 398 participants that explored visual interventions. Two of these compared two different types of visual interventions (Kerkhoff 2012; Kerkhoff 2014), and participants in the intervention arm of Machner 2012 received two different visual interventions during the intervention period. All studies in this category had an underlying rationale to encourage eye scanning or eye movement using a variety of mechanisms. Interventions included visual scanning training (Cherney 2002; Cottam 1987; Ferreira 2011; Katz 2005; Kerkhoff 2012; Kerkhoff 2014; Luukkainen‐Markkula 2009; Robertson 1990; Van Wyk 2014), half‐field eye patching (Aparicio‐Lopez 2016; Fong 2007; Machner 2012; Tsang 2009; Wu 2013; Zeloni 2002), optokinetic stimulation (Kerkhoff 2012; Machner 2012; Schroder 2008), eye movement feedback training (Fanthome 1995), and smooth pursuit eye movement training (Kerkhoff 2014). Studies used a range of methods, such as paper‐based tasks (e.g. Cherney 2002), computer‐based tasks (e.g. Kerkhoff 2014), and functional tasks (e.g. Van Wyk 2014).
Patients in every arm of seven studies received visual scanning training as an additional intervention (Iwanski 2020; Kim 2015; Polanowska 2009; Robertson 2002; Schroder 2008; Seniow 2016; Volkening 2016), and in one study, all patients received smooth pursuit eye movement training (Nyfeller 2019); therefore these studies were not considered under this comparison.
Prism adaptation training
Eight studies involving 257 participants explored prism adaptation training (Choi 2019; Goedert 2020; Mancuso 2012; Mizuno 2011; Nys 2008; Rode 2015; Ten‐Brink 2017; Turton 2010). Patients in both arms of Vatanparasti 2019 received prism adaptation training; therefore this study was not considered under this comparison.
Body awareness interventions
We identified 12 studies involving 447 participants that aimed to cue awareness of the affected side of the body. Studies in this category focused on proprioception and awareness of the body in space or in relation to midline. Interventions included sensory cueing (Fong 2013; Kalra 1997; Karner 2019; Yang 2017), limb activation (Luukkainen‐Markkula 2009; Robertson 2002), trunk rotation (Fong 2007; Wiart 1997), cueing and feedback (Edmans 2000), mirror therapy (Pandian 2014), neck taping (Varalta 2019), and a combination of visual, auditory, and sensory stimuli (Sesh 2018). Patients in both arms of Bang 2015 received mirror therapy; therefore this study was not considered under this comparison.
Mental function interventions
We identified seven studies involving 170 participants exploring interventions targeting mental functions, including mental imagery practice (Ferreira 2011; Park 2015; Park 2015b; Welfringer 2011), virtual reality training (Katz 2005; Kim 2011), and general cognitive rehabilitation without a specific visual search focus (Rusconi 2002). All participants in Aparicio‐Lopez 2016 received general cognitive rehabilitation; therefore this study was not considered under this comparison.
Movement interventions
Six studies involving 220 participants explored interventions that used movement of the upper limb or of the whole body to treat neglect. These studies used methods different from those focused on body awareness and included a robotic upper limb treatment (Choi 2016; Kim 2018), a robotic kinaesthetic ability training programme (Kutlay 2018), constraint‐induced movement therapy (Wu 2013), and visuomotor feedback training (Learmonth 2020; Rossit 2019).
Non‐invasive brain stimulation (NIBS)
Seventeen studies involving 467 participants explored NIBS. Six of these explored a variety of doses of NIBS (Fu 2017; Kim 2013; Kim 2015; Nyfeller 2019; Yang 2015; Yi 2016), whereas the other 11 did not explore different doses within each study. We identified studies using different stimulation protocols: repetitive transcranial magnetic stimulation (rTMS) (Cha 2016; Iwanski 2020; Kim 2013; Kim 2015; Kim 2018; Raghavan 2017; Song 2009; Yang 2015; Yang 2017), including inhibitory continuous theta burst stimulation (TBS) (Cazzoli 2012; Fu 2017; Koch 2012; Nyfeller 2019; Vatanparasti 2019), and transcranial direct current stimulation tDCS (Bang 2015; Learmonth 2020; Yi 2016).
Electrical stimulation
Eight studies involving 270 participants explored electrical stimulation. One of these explored different doses of the same type of intervention (Wilkinson 2014). Studies used transcutaneous electrical nerve stimulation (TENS) (Polanowska 2009; Schroder 2008; Seniow 2016), galvanic vestibular stimulation (GVS) (Volkening 2016; Wilkinson 2014), functional electrical stimulation (FES) (Choi 2019; Rusconi 2002), or electromyogram‐triggered electrical stimulation (Park 2015b).
Acupuncture
Two studies involving 104 participants explored acupuncture on specific points as treatment for neglect (Dolkun 2019; Li 2017).
Dose of interventions
The nature of the intervention was usually well described, as were the number, frequency, and duration of therapy sessions. The number of sessions varied from one in Choi 2019 to 40 in Rusconi 2002 over a duration of 1 day to 12 weeks. Sessions ranged from 10 times a day to once a week and lasted from 5 minutes to constant application of a wearable device for the entire intervention period. See TIDIER for details.
Comparisons
Table 9 summarises the interventions delivered in each study alongside the control intervention.
Outcomes
Table 10 summarises relevant outcome measures used in the included studies and highlights which studies yielded data suitable for inclusion in our meta‐analysis.
2. Included studies outcome measures used.
| Study name | Primary outcome measure reported | Secondary outcome measure reported | Data used in: | |||
| Target cancellation | Line bisection | BIT‐B | Other | |||
| Aparicio‐Lopez 2016 | CBS | x | x | Analysis 1.4 | ||
| Bang 2015 | BI | x | Analysis 6.4 | |||
| Cazzoli 2012 | CBS | x | x | No usable data | ||
| Cha 2016 | x | Analysis 6.4 | ||||
| Cherney 2003 | x | Analysis 1.4 | ||||
| Choi 2016 | CBS | x | x | Analysis 5.2; Analysis 5.4 | ||
| Choi 2019 | CBS | x | Analysis 2.2; Analysis 2.4; Analysis 7.4 | |||
| Cottam 1987 | x | Analysis 1.3 | ||||
| Dolkun 2019 | BI | x | x | Analysis 8.2; Analysis 8.4 | ||
| Edmans 2000 | BI | x | Analysis 3.2; Analysis 3.4; | |||
| Fanthome 1995 | x | Analysis 1.3; Analysis 1.4 | ||||
| Ferreira 2011 | FIM | x | Table 11; Table 12 | |||
| Fong 2007 | FIM | x | Analysis 1.1; Analysis 1.2; Analysis 1.3; Analysis 1.4; Analysis 3.1; Analysis 3.2; Analysis 3.3; Analysis 3.4 | |||
| Fong 2013 | FIM | x | Analysis 3.2; Analysis 3.4 | |||
| Fu 2017 | x | x | No usable data | |||
| Goedert 2020 | CBS | x | Analysis 2.1; Analysis 2.2 | |||
| Iwanski 2020 | FIM | x | Analysis 6.1; Analysis 6.2; Analysis 6.3; Analysis 6.4 | |||
| Kalra 1997 | BI | x | Analysis 3.4; Analysis 3.6 | |||
| Karner 2019 | SINGER | x | x | Analysis 3.4 | ||
| Katz 2005 | ADL test | x | Table 11 | |||
| Kerkhoff 2012 | x | x | Table 11 | |||
| Kerkhoff 2014 | ADL test | x | Table 11 | |||
| Kim 2011 | CBS | x | x | Analysis 4.2; Analysis 4.4 | ||
| Kim 2013 | CBS | x | x | Table 12 | ||
| Kim 2015 | x | x | Table 11 | |||
| Kim 2018 | CBS | x | x | Analysis 5.2; Analysis 5.4; Analysis 6.2; Analysis 6.4 | ||
| Koch 2012 | x | x | x | Analysis 6.4 | ||
| Kutlay 2018 | FIM | x | x | x | Table 12 | |
| Learmonth 2020 | SIS | x | x | Table 11; Table 12 | ||
| Li 2017 | BI | x | x | Analysis 8.2; Analysis 8.4 | ||
| Luukkainen‐Markkula 2009 | CBS | x | Table 11 | |||
| Machner 2014 | CBS | x | x | Analysis 1.1; Analysis 1.2; Analysis 1.3; Analysis 1.4 | ||
| Mancuso 2012 | x | x | Analysis 2.4 | |||
| Mizuno 2011 | CBS, FIM | x | Analysis 2.2; Analysis 2.4 | |||
| Nyffeler 2019 | CBS, FIM | x | Analysis 6.1; Analysis 6.2; no usable secondary outcome data | |||
| Nys 2008 | x | x | Analysis 2.3; Analysis 2.4 | |||
| Pandian 2014 | FIM, mRS | x | x | Table 12 | ||
| Park 2015 | x | x | Analysis 4.4 | |||
| Park 2015b | CBS | x | x | Table 11 | ||
| Polanowska 2009 | x | x | Analysis 7.4 | |||
| Raghavan 2017 | x | x | No usable data | |||
| Robertson 1990 | Frenchay Activities Index | x | Analysis 1.3; Analysis 1.4 | |||
| Robertson 2002 | BI | x | x | Analysis 3.1; Analysis 3.2; Analysis 3.3; Analysis 3.4 | ||
| Rode 2015 | FIM | x | No usable data | |||
| Rossit 2019 | SIS | x | No usable data | |||
| Rusconi 2002 | BI | x | x | No usable data | ||
| Schroder 2008 | x | No usable data | ||||
| Seniow 2016 | x | No usable data | ||||
| Sesh 2018 | mRS | x | x | Analysis 3.1; Analysis 3.2; Analysis 3.3; Analysis 3.4 | ||
| Song 2009 | x | x | Analysis 6.4 | |||
| Ten‐Brink 2017 | CBS | x | Analysis 2.2; Analysis 2.4 | |||
| Tsang 2009 | FIM | x | x | Table 12 | ||
| Turton 2010 | CBS | x | Analysis 2.1; Analysis 2.2 | |||
| Van Wyk 2014 | BI | x | No usable data | |||
| Varalta 2019 | x | Analysis 3.4 | ||||
| Vatanparasti 2019 | mRS | x | x | Analysis 6.4 | ||
| Volkening 2016 | x | No usable data | ||||
| Welfringer 2011 | x | Analysis 4.4 | ||||
| Wiart 1997 | FIM | x | x | Analysis 3.1; Analysis 3.2; Analysis 3.3; Analysis 3.4 | ||
| Wilkinson 2014 | BI | x | Table 11 | |||
| Wu 2013 | CBS | Analysis 1.2; | ||||
| Yang 2015 | x | x | Analysis 6.3; Analysis 6.4 | |||
| Yang 2017 | CBS | x | Analysis 3.1; Analysis 3.2; Analysis 3.3; Analysis 3.4; Analysis 6.1; Analysis 6.2; Analysis 6.3; Analysis 6.4 | |||
| Yi 2016 | CBS | x | x | Analysis 6.2; Analysis 6.4 | ||
| Zeloni 2002 | x | x | Analysis 1.4 | |||
ADL: activities of daily living. BI: Barthel Index. CBS: Catherine Bergego Scale. FIM: Functional Independence Measure. mRS: modified Rankin Scale. SINGER: Scores of Independence Index for Neurological and Geriatric Rehabilitation. SIS: Stroke Impact Scale.
Measures of functional ability
Fifty‐two of the 65 included studies measured functional ability using an 'activities of daily living' scale. Eighteen used the Catherine Bergego Scale (CBS) (Aparicio‐Lopez 2016; Cazzoli 2012; Choi 2016; Choi 2019; Goedert 2020; Kim 2011; Kim 2013; Kim 2018; Luukkainen‐Markkula 2009; Machner 2012; Mizuno 2011; Nyfeller 2019; Park 2015b; Ten‐Brink 2017; Turton 2010; Wu 2013; Yang 2017; Yi 2016); 11 the Functional Independence Measure (FIM) (Ferreira 2011; Fong 2007; Fong 2013; Iwanski 2020; Kutlay 2018; Mizuno 2011; Nyfeller 2019; Pandian 2014; Rode 2015; Tsang 2009; Wiart 1997); 11 the Barthel Index (BI) (Bang 2015; Dolkun 2019; Edmans 2000; Kalra 1997; Li 2017; Nys 2008; Polanowska 2009; Robertson 2002; Rusconi 2002; Van Wyk 2014; Wilkinson 2014); 3 the modified Rankin Scale (Pandian 2014; Sesh 2018; Vatanparasti 2019); and 1 the Frenchay Activities Index (Robertson 1990). The remaining 6 studies reported measures not listed in our protocol: Stroke Impact Scale (Learmonth 2020; Rossit 2019); Unawareness and Behavioural Neglect Index (Kerkhoff 2014); scores on Independence Index for Neurological and Geriatric Rehabilitation (SINGER) (Karner 2019); stroke‐specific quality of life scale (Raghavan 2017); and unspecified measures of ADL (Katz 2005).
Only 16 studies reported ADL outcomes at least one month post intervention (persisting effects) ‐ our primary outcome of interest (Ferreira 2011; Fong 2007; Goedert 2020; Iwanski 2020; Learmonth 2020; Machner 2012; Pandian 2014; Raghavan 2017; Robertson 2002; Rode 2015; Rossit 2019; Sesh 2018; Turton 2010; Wiart 1997; Wilkinson 2014; Yang 2017).
Kalra 1997, Mizuno 2011, and Tsang 2009 recorded ADL outcomes at the time of hospital discharge, rather than at a set time following completion of the intervention; we omitted these data from meta‐analysis, as the time of discharge itself would depend on the participant's recovery.
Standardised neglect assessments
All but 2 of the 65 included studies reported a standardised assessment of spatial neglect (Kerkhoff 2014; Wu 2013). Forty‐six studies used target cancellation, 35 used line bisection, and 32 used both measures. Ten studies reported neglect assessments that were not our chosen secondary outcomes. Twenty‐three studies reported neglect outcomes at least one month post intervention. One study provided data for persisting effect at follow‐up but not immediately after treatment (Cottam 1987). Two studies recorded neglect outcomes at the time of hospital discharge (Mizuno 2011; Tsang 2009); we omitted these from meta‐analysis as described above.
Other secondary outcomes
One study reported discharge destination (Kalra 1997). Two studies measured depression using the Beck Depression Inventory (Learmonth 2020; Luukkainen‐Markkula 2009), but only Learmonth 2020 provided data post intervention. Five studies recorded adverse events (Choi 2016; Edmans 2000; Ferreira 2011; Kalra 1997; Learmonth 2020). No other relevant outcome data (i.e. falls, balance, quality of life) were reported.
Excluded studies
We excluded 212 papers after assessment of the full paper in this update (see Figure 1). Of these, 161 clearly did not meet the inclusion criteria. Nineteen of the 212 papers required more in‐depth appraisal prior to exclusion; we have provided our reasons for exclusion of these studies, as well as those excluded from previous versions of this review, in the Characteristics of excluded studies table. We excluded most of these because the study was not randomised, or because the intervention was not specifically targeted at neglect.
We excluded two studies that were included in previous versions of this review. We excluded Rossi 1990 because less than 50% of participants had neglect. We excluded Weinberg 1977 because we believe participants did not necessarily have neglect but we were unable to obtain clarification due to the age of the study.
Risk of bias in included studies
Information on risk of bias is provided in the Characteristics of included studies table and is summarised in Figure 2 and Figure 3. Risk of bias for Nyfeller 2019Yang 2015 and Yi 2016 is also presented under Nyfeller 2019 16c TBSYang 2015 10Hz and Yi 2016 anodal to enable presentation of risk of bias in forest plots. We judged only two studies to be entirely at low risk of bias (Rode 2015; Wilkinson 2014).
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.

Allocation
We assessed 24 of the included RCTs as having low risk of bias with adequate allocation and concealment (Aparicio‐Lopez 2016; Dolkun 2019; Edmans 2000; Ferreira 2011; Fong 2013; Kalra 1997; Kutlay 2018; Learmonth 2020; Li 2017; Machner 2012; Mizuno 2011; Nyfeller 2019; Pandian 2014; Park 2015b; Polanowska 2009; Robertson 1990; Robertson 2002; Rode 2015; Tsang 2009; Turton 2010; Volkening 2016; Welfringer 2011; Wilkinson 2014; Wu 2013). Twenty‐three studies provided insufficient details for determining adequacy of the allocation process or its concealment without clearly being at high risk in either regard (Bang 2015; Cazzoli 2012; Cherney 2002; Choi 2016; Fu 2017; Goedert 2020; Iwanski 2020; Karner 2019; Kim 2011; Kim 2013; Kim 2015; Koch 2012; Nys 2008; Park 2015; Raghavan 2017; Schroder 2008; Seniow 2016; Song 2009; Ten‐Brink 2017; Vatanparasti 2019; Yang 2015; Yang 2017; Yi 2016). The remaining 18 studies reported methods of allocation or concealment that we assessed to be at high risk of bias.
Blinding
We assessed five of the included RCTs to have adequate blinding of outcome assessors (Fong 2007; Rode 2015; Tsang 2009; Varalta 2019; Wilkinson 2014). This information was unclear for 33 studies (Cazzoli 2012; Cha 2016; Fanthome 1995; Fu 2017; Iwanski 2020; Kalra 1997; Karner 2019; Kerkhoff 2014; Kim 2013; Koch 2012; Kutlay 2018; Learmonth 2020; Li 2017; Mizuno 2011; Nyfeller 2019; Nys 2008; Pandian 2014; Park 2015; Polanowska 2009; Robertson 1990; Robertson 2002; Rossit 2019; Seniow 2016; Song 2009; Turton 2010; Van Wyk 2014; Volkening 2016; Welfringer 2011; Wiart 1997; Wu 2013; Yang 2015; Yang 2017; Yi 2016), and we judged the remaining 27 studies to be at high risk of bias due to not having a blinded outcome assessor or because blinding was not possible.
Incomplete outcome data
We assessed 39 of the included RCTs as having low risk of bias arising from incomplete outcome data (Aparicio‐Lopez 2016; Bang 2015; Cazzoli 2012; Cha 2016; Cherney 2002; Choi 2019; Cottam 1987; Dolkun 2019; Edmans 2000; Ferreira 2011; Iwanski 2020; Kalra 1997; Karner 2019; Kerkhoff 2012; Kerkhoff 2014; Kim 2015; Koch 2012; Li 2017; Nys 2008; Pandian 2014; Park 2015; Park 2015b; Polanowska 2009; Raghavan 2017; Robertson 2002; Rode 2015; Rossit 2019; Song 2009; Turton 2010; Van Wyk 2014; Varalta 2019; Welfringer 2011; Wiart 1997; Wilkinson 2014; Wu 2013; Yang 2015; Yang 2017; Yi 2016; Zeloni 2002). Eighteen were assessed to be at high risk of bias due to incomplete outcome data (Choi 2016; Fong 2007; Fong 2013; Fu 2017; Goedert 2020; Kim 2011; Kim 2013; Kim 2018; Kutlay 2018; Learmonth 2020; Mancuso 2012; Mizuno 2011; Robertson 1990; Rusconi 2002; Sesh 2018; Ten‐Brink 2017; Tsang 2009; Volkening 2016), for example, due to omission of baseline data for dropouts in Choi 2016 and loss of 45% of the control group prior to follow‐up in Fong 2013. Insufficient information was available for assessment of the remaining eight studies
Selective reporting
We assessed 50 of the included RCTs to be free of reporting bias. Six had some selective reporting (Aparicio‐Lopez 2016; Cottam 1987; Ferreira 2011; Fu 2017; Kalra 1997; Mizuno 2011), for example, they reported subscales to differing levels of detail. For nine studies, this information was unclear (Fong 2007; Katz 2005; Luukkainen‐Markkula 2009; Pandian 2014; Polanowska 2009; Schroder 2008; Tsang 2009; Vatanparasti 2019; Volkening 2016).
Other potential sources of bias
We assessed 49 studies to be free from other potential sources of bias. For 12 studies, we identified some other source of potential bias mainly due to unadjusted baseline differences between groups (Fu 2017; Iwanski 2020; Kalra 1997; Katz 2005; Kim 2011; Luukkainen‐Markkula 2009; Pandian 2014; Polanowska 2009; Sesh 2018; Song 2009; Volkening 2016; Wiart 1997); for four studies, other potential sources of bias were unclear (Goedert 2020; Kim 2013; Machner 2012; Zeloni 2002).
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8
Summary of findings 1. Visual interventions compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury.
| Visual interventions compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury | ||||
| Patient or population: spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury Setting: inpatient or community rehabilitation Intervention: visual interventions Comparison: any control | ||||
| Outcomes | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Primary outcome | ||||
| Activities of daily living: effects persisting at least 1 month post intervention | SMD ‐0.04 lower (‐0.57 lower to 0.49 higher) | 55 (2 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c | No evidence of benefit or detriment from intervention |
| Secondary outcomes | ||||
| Activities of daily living: immediate effects | SMD ‐0.15 lower (‐0.6 lower to 0.3 higher) | 75 (3 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c,d | No evidence of benefit or detriment from intervention |
| Neglect outcomes: effects persisting at least 1 month post intervention | SMD 0.14 higher (‐0.26 lower to 0.55 higher) | 98 (5 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c,d | No evidence of benefit or detriment from intervention |
| Neglect outcomes: immediate effects | SMD 0.08 higher (‐0.26 lower to 0.42 higher) | 142 (7 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c,d | No evidence of benefit or detriment from intervention |
| Adverse events | ‐ | No studies | ‐ | |
| CI: confidence interval; RCT: randomised controlled trial; SMD: standardised mean difference. | ||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aOverall, studies contributing to this analysis had limitations regarding risk of bias sufficient to lower certainty regarding the estimate of effect and were downgraded once.
bDowngraded twice for serious imprecision (very small numbers of participants).
cDowngraded once for indirectness. Studies included only participants with recent‐onset stroke.
dDowngraded once for indirectness. Studies used different interventions or measured outcomes using different scales.
Summary of findings 2. Prism adaptation training compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury.
| Prism adaptation training compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury | ||||
| Patient or population: spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury Setting: inpatient or community rehabilitation Intervention: prism adaptation training Comparison: any control | ||||
| Outcomes | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Primary outcome | ||||
| Activities of daily living: effects persisting at least 1 month post intervention | SMD ‐0.29 lower (‐0.93 lower to 0.35 higher) | 39 (2 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c | No evidence of benefit or detriment from intervention |
| Secondary outcomes | ||||
| Activities of daily living: immediate effects | SMD 0.20 higher (‐0.12 lower to 0.51 higher) | 158 (5 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c | No evidence of benefit or detriment from intervention |
| Neglect outcomes: effects persisting at least 1 month post intervention | SMD 0.05 higher (‐0.96 lower to 1.06 higher) | 16 (1 RCT) |
⊕⊝⊝⊝ Very lowa,b,c | No evidence of benefit or detriment from intervention |
| Neglect outcomes: immediate effects | SMD 0.28 higher (‐0.05 lower to 0.60 higher) | 154 (5 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c,d | No evidence of benefit or detriment from intervention |
| Adverse events | ‐ | No studies | ‐ | |
| CI: confidence interval; RCT: randomised controlled trial; SMD: standardised mean difference. | ||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aOverall, studies contributing to this analysis had limitations regarding risk of bias sufficient to lower certainty regarding the estimate of effect and were downgraded once.
bDowngraded twice for serious imprecision (very small numbers of participants).
cDowngraded once for indirectness. Studies included only participants with recent‐onset stroke.
dDowngraded once for indirectness. Studies used different interventions or measured outcomes using different scales.
Summary of findings 3. Body awareness interventions compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury.
| Body awareness interventions compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury | ||||
| Patient or population: spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury Setting: inpatient or community rehabilitation Intervention: body awareness interventions Comparison: any control | ||||
| Outcomes | Relative effect (95% CI) |
No. of participants (studies) |
Certainty of the evidence (GRADE) | Comments |
| Primary outcome | ||||
| Activities of daily living: effects persisting at least 1 month post intervention | SMD 0.61 higher (0.24 higher to 0.97 higher) | 125 (5 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c,d | Evidence suggests possible benefit from intervention |
| Secondary outcomes | ||||
| Activities of daily living: immediate effects | SMD 0.26 higher (‐0.01 lower to 0.53 higher) | 221 (7 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c,d | No evidence of benefit or detriment from intervention |
| Neglect outcomes: effects persisting at least 1 month post intervention | SMD 0.36 higher (0.00 lower to 0.72 higher) | 125 (5 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c,d | Evidence suggests possible benefit from intervention |
| Neglect outcomes: immediate effects | SMD 0.16 higher (‐0.07 lower to 0.39 higher) | 311 (10 RCTs) |
⊕⊝⊝⊝ Very lowa,c,d | No evidence of benefit or detriment from intervention |
| Adverse events | OR 0.36 higher (0.05 to 2.6) | 130 (2 RCTs) |
⊕⊝⊝⊝ Very lowa,b,d | No evidence of benefit or detriment from intervention |
| CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial; SMD: standardised mean difference. | ||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aOverall, studies contributing to this analysis had limitations regarding risk of bias sufficient to lower certainty regarding the estimate of effect and were downgraded once.
bDowngraded twice for serious imprecision (very small numbers of participants).
cDowngraded once for indirectness. Studies used different interventions or measured outcomes using different scales.
dDowngraded once for indirectness. Studies included only participants with recent‐onset stroke.
Summary of findings 4. Mental function interventions compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury.
| Mental function interventions compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury | ||||
| Patient or population: spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury Setting: inpatient or community rehabilitation Intervention: mental function interventions Comparison: any control | ||||
| Outcomes | Relative effect (95% CI) |
No. of participants (studies) |
Certainty of the evidence (GRADE) | Comments |
| Primary outcome | ||||
| Activities of daily living: effects persisting at least 1 month post intervention | ‐ | No studies | ‐ | |
| Secondary outcomes | ||||
| Activities of daily living: immediate effects | SMD 0.32 higher (‐0.49 lower to 1.12 higher) | 24 (1 RCT) |
⊕⊝⊝⊝ Very lowa,b,c | No evidence of benefit or detriment from intervention |
| Neglect outcomes: effects persisting at least 1 month post intervention | ‐ | No studies | ‐ | |
| Neglect outcomes: immediate effects | SMD 0.10 higher (‐0.32 lower to 0.53 higher) | 60 (3 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c | No evidence of benefit or detriment from intervention |
| Adverse events | ‐ | No studies | ‐ | |
| CI: confidence interval; RCT: randomised controlled trial; SMD: standardised mean difference. | ||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aOverall, studies contributing to this analysis had limitations regarding risk of bias sufficient to lower certainty regarding the estimate of effect and were downgraded once.
bDowngraded twice for serious imprecision (very small numbers of participants).
cDowngraded once for indirectness. Studies included only participants with recent‐onset stroke.
Summary of findings 5. Movement interventions compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury.
| Movement interventions compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury | ||||
| Patient or population: spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury Setting: inpatient or community rehabilitation Intervention: movement interventions Comparison: any control | ||||
| Outcomes | Relative effect (95% CI) |
No. of participants (studies) |
Certainty of the evidence (GRADE) | Comments |
| Primary outcome | ||||
| Activities of daily living: effects persisting at least 1 month post intervention | ‐ | No studies | ‐ | |
| Secondary outcomes | ||||
| Activities of daily living: immediate effects | SMD 0.57 higher (0.09 higher to 1.04 higher) | 75 (3 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c | Evidence suggests possible benefit from intervention |
| Neglect outcomes: effects persisting at least 1 month post intervention | ‐ | No studies | ‐ | |
| Neglect outcomes: immediate effects | SMD 0.57 higher (0.04 higher to 1.10 higher) | 58 (2 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c | Evidence suggests possible benefit from intervention |
| Adverse events | ‐ | No studies | ‐ | |
| CI: confidence interval; RCT: randomised controlled trial; SMD: standardised mean difference. | ||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aOverall, studies contributing to this analysis had limitations regarding risk of bias sufficient to lower certainty regarding the estimate of effect and were downgraded once.
bDowngraded twice for serious imprecision (very small numbers of participants).
cDowngraded once for indirectness. Studies included only participants with recent‐onset stroke.
Summary of findings 6. NIBS compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury.
| NIBS compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury | ||||
| Patient or population: spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury Setting: inpatient or community rehabilitation Intervention: NIBS Comparison: any control | ||||
| Outcomes | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Primary outcome | ||||
| Activities of daily living: effects persisting at least 1 month post intervention | SMD 0.35 higher (‐0.08 lower to 0.77 higher) | 92 (3 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c | No evidence of benefit or detriment from intervention |
| Secondary outcomes | ||||
| Activities of daily living: immediate effects | SMD 0.61 higher (0.27 higher to 0.94 higher) | 160 (6 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c,d | Evidence suggests possible benefit from intervention |
| Neglect outcomes: effects persisting at least 1 month post intervention | SMD 0.77 (0.29 higher to 1.24 higher) | 102 (3 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c,d | Evidence suggests possible benefit from intervention |
| Neglect outcomes: immediate effects | SMD 0.75 higher (0.47 higher to 1.04 higher) | 244 (10 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c,d | Evidence suggests possible benefit from intervention |
| Adverse events | ‐ | 24 (1 RCT) | ‐ | All adverse events reported deemed to be unrelated to intervention |
| CI: Confidence interval | ||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aOverall, studies contributing to this analysis had limitations regarding risk of bias sufficient to lower certainty regarding the estimate of effect and were downgraded once.
bDowngraded twice for serious imprecision (very small numbers of participants).
cDowngraded once for indirectness. Studies included only participants with recent‐onset stroke.
dDowngraded once for indirectness. Studies used different interventions or measured outcomes using different scales.
Summary of findings 7. Electrical stimulation compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury.
| Electrical stimulation compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury | ||||
| Patient or population: spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury Setting: inpatient or community rehabilitation Intervention: electrical stimulation Comparison: any control | ||||
| Outcomes | Relative effect (95% CI) |
No. of participants (studies) |
Certainty of the evidence (GRADE) | Comments |
| Primary outcome | ||||
| Activities of daily living: effects persisting at least 1 month post intervention | ‐ | No studies | ‐ | |
| Secondary outcomes | ||||
| Activities of daily living: immediate effects | ‐ | No studies | ‐ | |
| Neglect outcomes: effects persisting at least 1 month post intervention | ‐ | No studies | ‐ | |
| Neglect outcomes: immediate effects | SMD 0.99 higher (0.44 higher to 1.53 higher) | 60 (2 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c | Evidence suggests possible benefit from intervention |
| Adverse events | ‐ | No studies | ‐ | |
| CI: confidence interval; RCT: randomised controlled trial; SMD: standardised mean difference. | ||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aOverall, studies contributing to this analysis had limitations regarding risk of bias sufficient to lower certainty regarding the estimate of effect and were downgraded once.
bDowngraded twice for serious imprecision (very small numbers of participants).
cDowngraded once for indirectness. Studies included only participants with recent‐onset stroke.
Summary of findings 8. Acupuncture compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury.
| Acupuncture compared to any control for spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury | ||||
| Patient or population: spatial neglect or inattention following stroke and other adult‐acquired non‐progressive brain injury Setting: inpatient or community rehabilitation Intervention: acupuncture Comparison: any control | ||||
| Outcomes | Relative effect (95% CI) |
No. of participants (studies) |
Certainty of the evidence (GRADE) | Comments |
| Primary outcome | ||||
| Activities of daily living: effects persisting at least 1 month post intervention | ‐ | No studies | ‐ | |
| Secondary outcomes | ||||
| Activities of daily living: immediate effects | SMD 0.65 higher (0.26 higher to 1.05 higher) | 104 (2 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c | Evidence suggests possible benefit from intervention |
| Neglect outcomes: effects persisting at least 1 month post intervention | ‐ | No studies | ‐ | |
| Neglect outcomes: immediate effects | SMD 0.57 higher (0.18 higher to 0.97 higher) | 104 (2 RCTs) |
⊕⊝⊝⊝ Very lowa,b,c,d | Evidence suggests possible benefit from intervention |
| Adverse events | ‐ | No studies | ‐ | |
| CI: confidence interval; RCT: randomised controlled trial; SMD: standardised mean difference. | ||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aOverall, studies contributing to this analysis had limitations regarding risk of bias sufficient to lower certainty regarding the estimate of effect and were downgraded once.
bDowngraded twice for serious imprecision (very small numbers of participants).
cDowngraded once for indirectness. Studies included only participants with recent‐onset stroke.
dDowngraded once for indirectness. Studies used different interventions or measured outcomes using different scales.
Studies included in meta‐analysis within this review
From the 65 studies included in this review, 43 were included in meta‐analysis.
Studies not included in meta‐analysis within this review
Twenty‐two studies were not included in meta‐analysis. Nine studies compared multiple different active treatments with no control (Ferreira 2011; Katz 2005; Kerkhoff 2012; Kerkhoff 2014; Kim 2015; Luukkainen‐Markkula 2009; Park 2015b; Schroder 2008; Wilkinson 2014). We included data from head‐to‐head comparisons in multi‐arm studies in Table 11. Seven studies included no usable data in the published paper, and we were unable to obtain further data (Cazzoli 2012; Fu 2017; Rode 2015; Rusconi 2002; Seniow 2016; Van Wyk 2014; Volkening 2016). Six studies reported change from baseline data for only for outcomes, and we did not obtain raw scores (Ferreira 2011; Kim 2013; Koch 2012; Learmonth 2020; Pandian 2014; Tsang 2009). These studies are presented in Table 12 and are not included in meta‐analysis.
3. Results of studies comparing multiple interventions.
| Study identifier | Intervention | Outcome | Mean (SD) | Number of participants | Reported result |
| Aparicio‐Lopez 2016 | Visual (eye‐patching) + Mental function (cognitive rehabilitation) | Immediate ADL (CBS) | 10.33 (6.6) | 13 | “No significant difference” |
| Mental function (cognitive rehabilitation) | 8.83 (6.7) | 15 | |||
| Visual (eye‐patching) + Mental function (cognitive rehabilitation) | Immediate neglect (line bisection) | 2.85 (3.55) | 13 | “No significant difference” | |
| Mental function (cognitive rehabilitation) | 0.93 (1.38) | 15 | |||
| Bang 2015 | NIBS (tDCS) + Body awareness (mirror therapy) | Immediate ADL (BI) | 78.3 (3.9) | 6 | Mann‐Whitney U, P = 0.004 in favour of NIBS + body awareness |
| Body awareness (mirror therapy) | 69.2 (2.4) | 6 | |||
| NIBS (tDCS) + Body awareness (mirror therapy) | Immediate neglect (line bisection) | 5.37 (0.4) | 6 | Mann‐Whitney U, P = 0.031 in favour of NIBS + body awareness | |
| Body awareness (mirror therapy) | 5.9 (0.3) | 6 | |||
| Choi 2019 | Prism adaptation | Immediate ADL (CBS) | 12.7 (3.88) | 10 | ANOVA, P < 0.001 in favour of prism adaptation + FES |
| Electrical stimulation (FES) | 14.8 (3.04) | 10 | |||
| Prism adaptation + Electrical stimulation (FES) | 10.8 (2.78) | 10 | |||
| Prism adaptation | Immediate neglect (target cancellation) | 8 (2.3) | 10 | ANOVA, P < 0.001 in favour of prism adaptation + FES | |
| Electrical stimulation (FES) | 9.1 (1.19) | 10 | |||
| Prism adaptation + Electrical stimulation (FES) | 5.0 (2.21) | 10 | |||
| Ferreira 2011 | Mental function (mental practice) | Persisting ADL (FIM) | 92.1 (24.4) | 5 | “No significant difference” |
| Visual (scanning training) | 90.1 (26.5) | 5 | |||
| Fong 2007 | Body awareness (trunk rotation) | Persisting ADL (FIM) | 52.9 (19.5) | 14 | “No significant difference” |
| Body awareness (trunk rotation) + Visual (eye‐patching) | 51.5 (21.7) | 20 | |||
| Usual care | 40.7 (20.9) | 12 | |||
| Body awareness (trunk rotation) | Immediate ADL (FIM) | 50.2 (19.4) | 19 | “No significant difference” | |
| Body awareness (trunk rotation) + Visual (eye‐patching) | 44.3 (18.7) | 20 | |||
| Usual care | 37.1 (16.4) | 15 | |||
| Body awareness (trunk rotation) | Persisting neglect (BIT‐B) | 54.9 (28.8) | 14 | “No significant difference” | |
| Body awareness (trunk rotation) + Visual (eye‐patching) | 53.8 (31.1) | 20 | |||
| Usual care | 46.8 (31.7) | 12 | |||
| Body awareness (trunk rotation) | Immediate neglect (BIT‐B) | 44.2 (20.8) | 14 | “No significant difference” | |
| Body awareness (trunk rotation) + Visual (eye‐patching) | 44.6 (27.3) | 20 | |||
| Usual care | 4.4 (26) | 12 | |||
| Fu 2017 | NIBS (cTBS 80%) | Immediate neglect (target cancellation) | No useable data | ||
| NIBS (cTBS 40%) | |||||
| Katz 2005 | Mental function (VR training) | Immediate ADL (FIM) | 73.7 (14) | 11 | “No significant difference” |
| Visual (scanning training) | 73.6 (22.8) | 8 | |||
| Mental function (VR training) | Immediate neglect (target cancellation) | 14.8 (12.9) | 11 | No statistical comparison reported | |
| Visual (scanning training) | 14.6 (10.40) | 8 | |||
| Kerkhoff 2012 | Visual (OKS) | Immediate neglect (target cancellation) | 3.3 (4.2) | 3 | Mann‐Whitney U; P < 0.001 In favour of OKS |
| Visual (scanning training) | 9.3 (1.2) | 3 | |||
| Kerkhoff 2014 | Visual (smooth pursuit training) | Immediate ADL (BI) | 28 (5) | 12 | Mann‐Whitney U = P > 0.55 |
| Visual (scanning training) | 26 (8) | 12 | |||
|
Kim 2013 (Mean change from baseline data available only) |
NIBS (low‐frequency rTMS) | Immediate ADL (CBS) | ‐5.4 (3.3) | 9 | “No significant difference” |
| NIBS (high‐frequency rTMS) | ‐8.6 (3.1) | 9 | |||
| Sham | ‐2.6 (1.7) | 9 | |||
| NIBS (low‐frequency rTMS) | Immediate neglect (target cancellation) | 16.4 (5.4) | 9 | “No significant difference” | |
| NIBS (high‐frequency rTMS) | 10.4 (3.6) | 9 | |||
| Sham | 3.6 (4.7) | 9 | |||
| Kim 2015 | NIBS (rTMS 1 session) | Immediate neglect (target cancellation) | 16.63 (3.24) | 19 | ANOVA, P < 0.01, in favour of 10 sessions |
| NIBS (rTMS 10 sessions) | 17 (2.85) | 15 | |||
| Kim 2018 | NIBS (rTMS) | Immediate ADL (CBS) | 15.2 (3.7) | 10 | Kruskal‐Wallis P = 0.152 |
| Movement (upper limb robot) | 17.5 (4.1) | 10 | |||
| NIBS (rTMS) | Immediate neglect (target cancellation) | 15.2 (4.9) | 10 | Kruskal‐Wallis P = 0.125 | |
| Movement (upper limb robot) | 14.5 (3.5) | 10 | |||
|
Learmonth 2020 (mean change from baseline data only available) |
NIBS (tDCS) | Persisting neglect (line bisection) | 0.20 (49) | 5 | No statistical comparison reported |
| Movement (visuomotor feedback training) | 3.39 (4.78) | 2 | |||
| NIBS (tDCS) + Movement (visuomotor feedback training) | ‐0.20 (0.31) | 3 | |||
| Attention control | 0.01 (0.44) | 4 | |||
| NIBS (tDCS) | Immediate neglect (line bisection) | 0.68 (2.70) | 6 | No statistical comparison reported | |
| Movement (visuomotor feedback training) | 0.64 (1.01) | 5 | |||
| NIBS (tDCS) + Movement (visuomotor feedback training) | 0.12 (0.89) | 5 | |||
| Attention control | ‐0.31 (0.56) | 5 | |||
| Luukkainen‐Markkula 2009 | Body awareness (arm activation) | Persisting ADL (CBS) | 3.4 (2.4) | 6 | No statistical comparison reported |
| Visual (scanning training) | 6.9 (3.8) | 6 | |||
| Body awareness (arm activation) | Immediate ADL (CBS) | 5.9 (3.1) | 6 | No statistical comparison reported | |
| Visual (scanning training) | 8.9 (5.1) | 6 | |||
| Nyfeller 2019 | NIBS (8 cTBS) | Persisting ADL (CBS) | 5.38 (4.41) | 8 | ANOVA, P = 0.94 |
| NIBS (16 cTBS) | 5.9 (6.28) | 10 | |||
| Sham | 12.2 (7.03) | 9 | |||
| NIBS (8 cTBS) | Immediate ADL (CBS) | 7 (6.16) | 10 | ANOVA, P < 0.02 in favour of 16 cTBS | |
| NIBS (16 cTBS) | 6.8 (7.1) | 10 | |||
| Sham | 12.5 (6.52) | 10 | |||
| Park 2015b | Mental function (mental practice) + electromyogram‐ triggered electrical stimulation |
Immediate ADL (CBS) | 10.1 (4.6) | 16 | “No significant difference” |
| Mental function (mental practice) + cyclical electrical stimulation | 11.2 (4.1) | 17 | |||
| Mental function (mental practice) + electromyogram‐ triggered electrical stimulation |
Immediate neglect (target cancellation) | 13.0 (5.5) | 16 | “No significant difference” | |
| Mental function (mental practice) + cyclical electrical stimulation | 11.0 (4.6) | 17 | |||
| Rusconi 2002 | Mental function (cognitive training type 1) | Immediate ADL (BI) | No usable data | ||
| Mental function (cognitive training type 2) | |||||
| Electrical stimulation (TENS) + mental function (cognitive training type 1) | |||||
| Electrical stimulation (TENS) + mental function (cognitive training type 2) | |||||
| Mental function (cognitive training type 1) | Immediate neglect (target cancellation) | No usable data | |||
| Mental function (cognitive training type 2) | |||||
| Electrical stimulation (TENS) + mental function (cognitive training type 1) | |||||
| Electrical stimulation (TENS) + mental function (cognitive training type 2) | |||||
| Schroder 2008 | Electrical stimulation (TENS) | Immediate neglect (bespoke score) | No usable data | ||
| Visual (OKS) | |||||
| Wilkinson 2014 | Electrical stimulation (GVS) 1 session | Persisting ADL (BI) | 64.3 (24.5) | 14 | “No significant difference” |
| Electrical stimulation (GVS) 5 sessions | 56.9 (25.6) | 16 | |||
| Electrical stimulation (GVS) 10 sessions | 66.4 (26.5) | 14 | |||
| Electrical stimulation (GVS) 1 session | Immediate ADL (BI) | 49.6 (24.1) | 13 | “No significant difference” | |
| Electrical stimulation (GVS) 5 sessions | 60.8 (29.1) | 18 | |||
| Electrical stimulation (GVS) 10 sessions | 32.6 (31) | 15 | |||
| Wu 2013 | Movement (CIMT) + visual (eye patching) | Immediate ADL (CBS) | 10.4 (3.2) | 7 | ANOVA, P < 0.01 |
| Movement (CIMT) | 9.9 (4.4) | 8 | |||
| Usual care | 16.3 (4.5) | 9 | |||
| Yang 2015 | NIBS (1 Hz TBS) | Persisting neglect (target cancellation) | 18.46 (4.91) | 9 | ANOVA, P < 0.05 |
| NIBS (10 Hz TBS) | 24.44 (4.54) | 10 | |||
| NIBS (cTBS) | 14.79 (4.59) | 9 | |||
| Sham | 15.54 (5.74) | 10 | |||
| NIBS (1 Hz TBS) | Immediate neglect (target cancellation) | 27.4 (5.76) | 9 | ANOVA, P < 0.05 | |
| NIBS (10 Hz TBS) | 29.01 (5.57) | 10 | |||
| NIBS (cTBS) | 16.54 (5.15) | 9 | |||
| Sham | 49.28 (5.41) | 10 | |||
| Yang 2015 | NIBS (rTMS) | Persisting ADL (CBS) | 13.9 (5.2) | 18 | “No significant difference” |
| NIBS (rTMS) + Body awarenss (sensory cueing) | 1.2 (6.4) | 19 | |||
| NIBS (rTMS) | Immediate ADL (CBS) | 16.4 (5.8) | 20 | “No significant difference” | |
| NIBS (rTMS) + Body awarenss (sensory cueing) | 14.1 (7) | 20 | |||
| NIBS (rTMS) | Persisting neglect (target cancellation) | 93.5 (24.1) | 18 | “No significant difference” | |
| NIBS (rTMS) + Body awarenss (sensory cueing) | 101.6 (24.7) | 19 | |||
| NIBS (rTMS) | Immediate neglect (target cancellation) | 83.5 (26.8) | 20 | “No significant difference” | |
| NIBS (rTMS) + Body awarenss (sensory cueing) | 93.4 (30.4) | 20 | |||
| Yi 2016 | NIBS (anodal tDCS) | Immediate ADL (CBS) | 8.4 (9) | 10 | “No significant difference” |
| NIBS (cathodal tDCS) | 10 (6.2) | 10 | |||
| Sham | 12.3 (10.8) | 10 | |||
| NIBS (anodal tDCS) | Immediate neglect (target cancellation) | 13.3 (8.2) | 10 | “No significant difference” | |
| NIBS (cathodal tDCS) | 13.2 (8.5) | 10 | |||
| Sham | 8.5 (4.9) | 10 | |||
ADL: activities of daily living. CBS: Catherine Bergego Scale. CIMT: constraint‐induced movement therapy. cTBS: continuous theta burst stimulation. FES: functional electrical stimulation. GVS: galvanic vestibular stimulation. NIBS: non‐invasive brain stimulation. OKS: optokinetic stimulation. rTMS: repetitive transcranial magnetic stimulation. TBS: theta burst stimulation. tDCS: transcranial direct current stimulation. TENS: transcutaneous electrical nerve stimulation. VR: virtual reality.
4. Results of studies with change from baseline data.
| Study identifier | Intervention | Outcome | Mean change from baseline (SD) | Number of participants | Reported result |
| Ferreira 2011 | Mental practice | Immediate ADL (FIM) | 7.4 (7.3) | 5 | “No significant difference” |
| Scanning training | 10.3 (6.7) | 5 | |||
| Kim 2013 | Low‐frequency rTMS | Immediate ADL (CBS) | ‐5.4 (3.3) | 9 | “No significant difference” |
| High‐frequency rTMS | ‐8.6 (3.1) | 9 | |||
| Sham | ‐2.6 (1.7) | 9 | |||
| Low‐frequency rTMS | Immediate neglect (target cancellation) | 16.4 (5.4) | 9 | “No significant difference” | |
| High‐frequency rTMS | 10.4 (3.6) | 9 | |||
| Sham | 3.6 (4.7) | 9 | |||
| Kutlay 2018 | Kinaesthetic ability training | Immediate ADL (FIM) | Median change: 82 (IQR 75.5 to 99) | 25 | “No significant difference” |
| Usual care | Median change: 79 (IQR 68.3 to 86.8) | 28 | |||
| Kinaesthetic ability training | Immediate neglect (BIT behavioural) | Median change: 67 (IQR 57.5 to 12) | 25 | “No significant difference” | |
| Usual care | Median change: 56.5 (IQR 25.75 to 66.5) | 28 | |||
| Learmonth 2020 | tDCS | Persisting neglect (line bisection) | 0.20 (49) | 5 | No statistical comparison reported |
| Behavioural training | 3.39 (4.78) | 2 | |||
| tDCS + Behavioural training | ‐0.20 (0.31) | 3 | |||
| Control behavioural training | 0.01 (0.44) | 4 | |||
| tDCS | Immediate neglect (line bisection) | 0.68 (2.70) | 6 | No statistical comparison reported | |
| Behavioural training | 0.64 (1.01) | 5 | |||
| tDCS + Behavioural training | 0.12 (0.89) | 5 | |||
| Control behavioural training | ‐0.31 (0.56) | 5 | |||
| tDCS | Persisting depression (Beck Depression Inventory) | 8.25 (9.22) | 4 | No statistical comparison reported | |
| Behavioural training | 2.00 (1.41) | 2 | |||
| tDCS + Behavioural training | 19.50 (19.09) | 2 | |||
| Control behavioural training | 17.33 (14.57) | 3 | |||
| Pandian 2014 | Body awareness (mirror therapy) | Persisting neglect (target cancellation) | 35 (1.5) | 26 | ANCOVA, P < 0.0001 in favour of intervention |
| Sham | 12 (1.5) | 20 | |||
| Body awareness (mirror therapy) | Immediate neglect (target cancellation) | 20 (1) | 26 | ANCOVA, P < 0.0001 in favour of intervention | |
| Sham | 6 (1.25) | 20 | |||
| Tsang 2009 | Visual (eye‐patching) | Immediate ADL (FIM) | 16 (14.24) | 17 | “No significant difference” |
| Usual care | 12.41 (14.21) | 17 | |||
| Visual (eye‐patching) | Immediate neglect (target cancellation) | 8.65 (13.15) | 17 | t‐test, P = 0.037 in favour of intervention | |
| Usual care | 1.88 (5.02) | 17 |
ADL: activities of daily living. BIT: Behavioural Inattention Test. FIM: Functional Independence Measure. CBS: Catherine Bergego Scale. tDCS: transcranial direct current stimulation. BIT: Behavioural Inattention Test. IQR: interquartile range. rTMS: repetitive transcranial magnetic stimulation.
Visual interventions versus any control
Ratings on measures of functional ability in ADL: persisting effects
Two studies (55 participants) provided usable data for a measure of ADL persisting for at least one month after completion of rehabilitation, one with the Catherine Bergego Scale (CBS) (Machner 2012), the other with the Functional Independence Measure (FIM) (Fong 2007).
Results were consistent (I² = 0%), with no evidence of benefit or detriment from intervention (standardised mean difference (SMD) ‐0.04, 95% confidence interval (CI) ‐0.57 to 0.49; very low‐certainty evidence; Analysis 1.1).
1.1. Analysis.

Comparison 1: Visual interventions versus any control, Outcome 1: Activities of daily living: persisting effects
Ratings on measures of functional ability in ADL: immediate effects
Three studies (75 participants) provided usable data for a measure of ADL immediately after completion of rehabilitation, two with the CBS (Machner 2012; Wu 2013), one with the FIM (Fong 2007).
Results were consistent (I² = 0%), with no evidence of benefit or detriment from intervention (SMD ‐0.15, 95% CI ‐0.60 to 0.30; very low‐certainty evidence; Analysis 1.2).
1.2. Analysis.

Comparison 1: Visual interventions versus any control, Outcome 2: Activities of daily living: immediate effects
Performance on standardised neglect assessment: persisting effects
Five studies (98 participants) provided usable data for a measure of neglect persisting for at least one month after completion of rehabilitation, two with target cancellation (Cottam 1987; Machner 2012), three with the Behavioural Inattention Test (BIT) behavioural subtest (Fanthome 1995; Fong 2007; Robertson 1990).
Results were consistent (I² = 0%), with no evidence of benefit or detriment from intervention (SMD 0.07, 95% CI ‐0.33 to 0.48; very low‐certainty evidence; Analysis 1.3).
1.3. Analysis.

Comparison 1: Visual interventions versus any control, Outcome 3: Neglect outcomes: persisting effects
Performance on standardised neglect assessment: immediate effects
Seven studies (142 participants) provided usable data for a measure of neglect immediately after completion of rehabilitation, three with target cancellation (Fanthome 1995; Machner 2012; Zeloni 2002), one with line bisection (Aparicio‐Lopez 2016), and three with the BIT behavioural subtest (Cherney 2002; Fong 2007; Robertson 1990).
Results were consistent (I² = 0%), with no evidence of benefit or detriment from intervention (SMD 0.08, 95% CI ‐0.26 to 0.42; very low‐certainty evidence; Analysis 1.4).
1.4. Analysis.

Comparison 1: Visual interventions versus any control, Outcome 4: Neglect outcomes: immediate effects
No studies of this intervention recorded other outcomes specified for this review.
Prism adaptation training versus any control
Ratings on measures of functional ability in ADL: persisting effects
Two studies (39 participants) provided usable data for a measure of ADL persisting for at least one month after completion of rehabilitation, both using the CBS (Goedert 2020; Turton 2010).
Results were consistent (I² = 0%), with no evidence of benefit or detriment from intervention (SMD ‐0.29, 95% CI ‐0.93 to 0.35; very low‐certainty evidence; Analysis 2.1).
2.1. Analysis.

Comparison 2: Prism adaptation versus any control, Outcome 1: Activities of daily living: persisting effects
Ratings on measures of functional ability in ADL: immediate effects
Five studies (158 participants) provided usable data for a measure of ADL immediately after completion of rehabilitation, all with the CBS (Choi 2019; Goedert 2020; Mizuno 2011; Ten‐Brink 2017; Turton 2010).
Results were consistent (I² = 0%), with no evidence of benefit or detriment from intervention (SMD 0.20, 95% CI ‐0.12 to 0.51; very low‐certainty evidence; Analysis 2.2).
2.2. Analysis.

Comparison 2: Prism adaptation versus any control, Outcome 2: Activities of daily living: immediate effects
Performance on standardised neglect assessment: persisting effects
One study (16 participants) provided usable data for a measure of neglect persisting for at least one month after completion of rehabilitation, with target cancellation (Nys 2008).
There was no evidence of benefit or detriment from intervention (SMD 0.05, 95% CI ‐0.96 to 1.06; very low‐certainty evidence; Analysis 2.3).
2.3. Analysis.

Comparison 2: Prism adaptation versus any control, Outcome 3: Neglect outcomes: persisting effects
Performance on standardised neglect assessment: immediate effects
Five studies (154 participants) provided usable data for a measure of neglect immediately after completion of rehabilitation, four with target cancellation (Choi 2019; Mancuso 2012; Nys 2008; Ten‐Brink 2017), one with the BIT behavioural subtest (Mizuno 2011).
Results were not consistent (I² = 66%), with no evidence of benefit or detriment from intervention (SMD 0.28, 95% CI ‐0.05 to 0.60; very low‐certainty evidence; Analysis 2.4).
2.4. Analysis.

Comparison 2: Prism adaptation versus any control, Outcome 4: Neglect outcomes: immediate effects
No studies of this intervention recorded other outcomes specified for this review.
Body awareness interventions versus any control
Ratings on measures of functional ability in ADL: persisting effects
Five studies (125 participants) provided usable data for a measure of ADL persisting for at least one month after completion of rehabilitation, two with the CBS (Robertson 2002; Yang 2017), two with the FIM (Fong 2007; Wiart 1997), and one with the modified Rankin Scale (mRS) (Sesh 2018).
Results were consistent (I² = 11%) and suggested possible benefit from intervention (SMD 0.61, 95% CI 0.24 to 0.97; very low‐certainty evidence; ,Analysis 3.1). The only studies reporting possible benefit were at high or unclear risk of bias for allocation of participants.
3.1. Analysis.

Comparison 3: Body awareness interventions versus any control, Outcome 1: Activities of daily living: persisting effects
Ratings on measures of functional ability in ADL: immediate effects
Seven studies (221 participants) provided usable data for a measure of ADL immediately after completion of rehabilitation, two with the CBS (Robertson 2002; Yang 2017), one with the Barthel Index (BI) (Edmans 2000), one with the FIM (Fong 2007; Fong 2013; Wiart 1997), and one with the mRS (Sesh 2018).
Results were not consistent (I² = 51%), with no evidence of benefit or detriment from intervention (SMD 0.26, 95% CI ‐0.01 to 0.53; very low‐certainty evidence; Analysis 3.2).
3.2. Analysis.

Comparison 3: Body awareness interventions versus any control, Outcome 2: Activities of daily living: immediate effects
Performance on standardised neglect assessment: persisting effects
Five studies (125 participants) provided usable data for a measure of neglect persisting for at least one month after completion of rehabilitation, two with target cancellation (Sesh 2018; Yang 2017), one with line bisection (Wiart 1997), and two with the BIT behavioural subtest (Fong 2007; Robertson 2002).
Results were a little consistent (I² = 41%) and suggested possible benefit from intervention (SMD 0.36, 95% CI 0.00 to 0.72; very low‐certainty evidence; Analysis 3.3). The only studies reporting possible benefit were at high or unclear risk of bias for allocation of participants or outcome assessor blinding.
3.3. Analysis.

Comparison 3: Body awareness interventions versus any control, Outcome 3: Neglect outcomes: persisting effects
Pandian 2014 (46 participants) reported change from baseline data only (see Table 12) and provided results consistent with the above.
Performance on standardised neglect assessment: immediate effects
Ten studies (311 participants) provided usable data for a measure of neglect immediately after completion of rehabilitation, seven with target cancellation (Edmans 2000; Fong 2013; Kalra 1997; Karner 2019; Sesh 2018; Varalta 2019; Yang 2017), one with line bisection (Wiart 1997), and two with the BIT behavioural subtest (Fong 2007; Robertson 2002).
Results were a little consistent (I² = 47%), with no evidence of benefit or detriment from intervention (SMD 0.16, 95% CI ‐0.07 to 0.39; very low‐certainty evidence; Analysis 3.4).
3.4. Analysis.

Comparison 3: Body awareness interventions versus any control, Outcome 4: Neglect outcomes: immediate effects
Pandian 2014 (46 participants) reported change from baseline data only (see Table 12) and provided results not consistent with the above.
Discharge destination
One study (50 participants) investigated discharge destination as an outcome (Kalra 1997). There was no evidence of benefit or detriment from intervention (odds ratio (OR) 1.4, 95% CI 0.45 to 4.4; very low‐certainty evidence; Analysis 3.5).
3.5. Analysis.

Comparison 3: Body awareness interventions versus any control, Outcome 5: Discharge destination (home)
Adverse events
Two studies (130 participants) recorded adverse events. Edmans 2000 reported one death in the control group; Kalra 1997 reported one death in the intervention group and two in the control group. Results were consistent (I² = 0%), with no evidence of benefit or detriment from intervention (OR 0.36, 95% CI 0.05 to 2.6; very low‐certainty evidence; Analysis 3.6).
3.6. Analysis.

Comparison 3: Body awareness interventions versus any control, Outcome 6: Adverse events
No studies of this intervention recorded other outcomes specified for this review.
Mental function interventions versus any control
Ratings on measures of functional ability in ADL: persisting effects
No studies of this intervention recorded this outcome.
Ratings on measures of functional ability in ADL: immediate effects
One study (24 participants) provided usable data for a measure of ADL immediately after completion of rehabilitation, using the CBS (Kim 2011).
There was no evidence of benefit or detriment from intervention (SMD 0.32, 95% CI ‐0.49 to 1.12; very low‐certainty evidence; Analysis 4.2).
4.2. Analysis.

Comparison 4: Mental function interventions versus any control, Outcome 2: Activities of daily living: immediate effects
Performance on standardised neglect assessment: persisting effects
No studies of this intervention recorded this outcome.
Performance on standardised neglect assessment: immediate effects
Three studies (60 participants) provided usable data for a measure of neglect immediately after completion of rehabilitation, all with target cancellation (Kim 2011; Park 2015; Welfringer 2011).
Results were consistent (I² = 0%), with no evidence of benefit or detriment from intervention (SMD 0.10, 95% CI ‐0.32 to 0.53; very low‐certainty evidence; Analysis 4.4).
4.4. Analysis.

Comparison 4: Mental function interventions versus any control, Outcome 4: Neglect outcomes: immediate effects
No studies of this intervention recorded other outcomes specified for this review.
Movement interventions versus any control
Ratings on measures of functional ability in ADL: persisting effects
No studies of this intervention recorded this outcome.
Ratings on measures of functional ability in ADL: immediate effects
Three studies (75 participants) provided usable data for a measure of ADL immediately after completion of rehabilitation, all with the CBS (Choi 2016; Kim 2018; Wu 2013).
Results were a little consistent (I² = 46%) and suggested possible benefit from intervention (SMD 0.57, 95% CI 0.09 to 1.04; very low‐certainty evidence; Analysis 5.2). The only studies reporting possible benefit were at high risk of bias for allocation of participants or outcome assessor blinding.
5.2. Analysis.

Comparison 5: Movement intervention versus any control, Outcome 2: Activities of daily living: immediate effects
Kutlay 2018 (52 participants) provided change from baseline data only (see Table 12) and reported results consistent with the above.
Performance on standardised neglect assessment: persisting effects
No studies of this intervention recorded this outcome.
Performance on standardised neglect assessment: immediate effects
Two studies (58 participants) provided usable data for a measure of neglect persisting for at least one month after completion of rehabilitation, both with target cancellation (Choi 2016; Kim 2018).
Results were consistent (I² = 0%) and suggested possible benefit from intervention (SMD 0.57, 95% CI 0.04 to 1.10; very low‐certainty evidence; Analysis 5.4). The only studies reporting possible benefit were at high risk of bias for allocation of participants and outcome assessor blinding.
5.4. Analysis.

Comparison 5: Movement intervention versus any control, Outcome 4: Neglect outcomes: immediate effects
Kutlay 2018 (52 participants) provided change from baseline data only (see Table 12) and reported results consistent with the above..
Adverse events
One study recorded adverse events (Choi 2016); none were reported.
No studies of this intervention recorded other outcomes specified for this review.
Non‐invasive brain stimulation versus any control
Ratings on measures of functional ability in ADL: persisting effects
Three studies (92 participants) provided usable data for a measure of ADL persisting for at least one month after completion of rehabilitation, two with the CBS (Nyfeller 2019; Yang 2017), one with the FIM (Iwanski 2020).
Results were a little inconsistent (I² = 21%), with no evidence of benefit or detriment from intervention (SMD 0.35, 95% CI ‐0.08 to 0.77; very low‐certainty evidence; Analysis 6.1).
6.1. Analysis.

Comparison 6: NIBS versus any control, Outcome 1: Activities of daily living: persisting effects
Ratings on measures of functional ability in ADL: immediate effects
Six studies (160 participants) provided usable data for a measure of ADL immediately after completion of rehabilitation, four with the CBS (Kim 2018; Nyfeller 2019; Yang 2017; Yi 2016), one with the FIM (Iwanski 2020), and one with the BI (Bang 2015).
Results were a little inconsistent (I² = 28%) and suggested possible benefit from intervention (SMD 0.61, 95% CI 0.27 to 0.94; very low‐certainty evidence; Analysis 6.2). In particular, the estimate of effect size from Bang 2015 appears implausible for a clinical outcome and may be a reporting error.
6.2. Analysis.

Comparison 6: NIBS versus any control, Outcome 2: Activities of daily living: immediate effects
Kim 2013 (27 participants) provided change from baseline data only (see Table 12) but found no evidence of benefit of non‐invasive brain stimulation (NIBS).
Performance on standardised neglect assessment: persisting effects
Three studies (102 participants) provided usable data for a measure of neglect persisting for at least one month after completion of rehabilitation, two with target cancellation (Yang 2015; Yang 2017), one with the BIT behavioural subtest (Iwanski 2020).
Results were not consistent (I² = 89%) and suggested possible benefit from intervention (SMD 0.77, 95% CI 0.29 to 1.24; very low‐certainty evidence; Analysis 6.3). In particular, estimated effect sizes from Yang 2015 appear implausible for a clinical outcome and may reflect a reporting error.
6.3. Analysis.

Comparison 6: NIBS versus any control, Outcome 3: Neglect outcomes: persisting effects
Performance on standardised neglect assessment: immediate effects
Ten studies (244 participants) provided usable data for a measure of neglect immediately after completion of rehabilitation, seven with target cancellation (Kim 2018; Koch 2012; Song 2009; Vatanparasti 2019; Yang 2015; Yang 2017; Yi 2016), two with line bisection (Bang 2015; Cha 2016), and one with the BIT behavioural subtest (Iwanski 2020).
Results were not consistent (I² = 79%) and suggested possible benefit from intervention (SMD 0.75, 95% CI 0.47 to 1.04; very low‐certainty evidence;.Analysis 6.4). In particular, estimated effect sizes from Yang 2015 and Cha 2016 appear implausible for a clinical outcome and may reflect a reporting error.
6.4. Analysis.

Comparison 6: NIBS versus any control, Outcome 4: Neglect outcomes: immediate effects
Kim 2013 (27 participants) provided change from baseline data only (see Table 12) but found no evidence of benefit of NIBS.
Adverse events
One study recorded serious adverse events. Learmonth 2020 reported four deaths, one per group, all of which were deemed to be unrelated to the intervention.
No studies of this intervention recorded other outcomes specified for this review.
Electrical stimulation versus any control
Ratings on measures of functional ability in ADL: persisting effects
No studies of this intervention recorded this outcome.
Ratings on measures of functional ability in ADL: immediate effects
No studies of this intervention recorded this outcome.
Performance on standardised neglect assessment: persisting effects
No studies of this intervention recorded this outcome.
Performance on standardised neglect assessment: immediate effects
Two studies (60 participants) provided usable data for a measure of neglect immediately after completion of rehabilitation, both with target cancellation (Choi 2019; Polanowska 2009).
Results were consistent (I² = 0%) and suggested possible benefit from intervention (SMD 0.99, 95% CI 0.44 to 1.53; very low‐certainty evidence; Analysis 7.4). One study reporting possible benefit was at high risk of bias for allocation of participants and outcome assessor blinding.
7.4. Analysis.

Comparison 7: Electrical stimulation versus any control, Outcome 4: Neglect outcomes: immediate effects
No studies of this intervention recorded other outcomes specified for this review.
Acupuncture versus any control
Ratings on measures of functional ability in ADL: persisting effects
No studies of this intervention recorded this outcome.
Ratings on measures of functional ability in ADL: immediate effects
Two studies (104 participants) provided usable data for a measure of ADL immediately after completion of rehabilitation, both with the BI (Dolkun 2019; Li 2017).
Results were consistent (I² = 0%) and suggested possible benefit from intervention (SMD 0.65, 95% CI 0.26 to 1.05; very low‐certainty evidence; Analysis 8.2). These studies were at high risk of bias for blinding.
8.2. Analysis.

Comparison 8: Acupuncture versus any control, Outcome 2: Activities of daily living: immediate effects
Performance on standardised neglect assessment: persisting effects
No studies of this intervention recorded this outcome.
Performance on standardised neglect assessment: immediate effects
Two studies (104 participants) provided usable data for a measure of neglect immediately after completion of rehabilitation, one with target cancellation (Dolkun 2019), one with line bisection (Li 2017).
Results were consistent (I² = 0%) and suggested possible benefit from intervention (SMD 0.57, 95% CI 0.18 to 0.97; very low‐certainty evidence; Analysis 8.4). These studies were at high risk of bias for blinding.
8.4. Analysis.

Comparison 8: Acupuncture versus any control, Outcome 4: Neglect outcomes: immediate effects
Sensitivity analyses
No study met our first criterion for conducting sensitivity analyses of sample size suggestive of a definitive clinical trial (more than 50 participants per intervention arm). Nine studies met our second criterion ‐ low risk of allocation bias without clear evidence of high risk of bias in any other domain aside from blinding (Dolkun 2019; Edmans 2000; Nyfeller 2019; Rode 2015; Turton 2010; Welfringer 2011; Wilkinson 2014; Wu 2013; Yi 2016). Neither Rode 2015 nor Wilkinson 2014 contributed data to our meta‐analyses, leaving seven 'lower‐risk' studies for consideration. Restricting analyses to these seven studies did not alter our overall conclusions, as each reached the same broad conclusion or estimated similar effect sizes as the meta‐analyses to which they contributed data.
Discussion
In this updated version of the review, we included 44 new randomised controlled trials (RCTs), bringing the total to 65 trials (1951 participants).
Summary of main results
Visual interventions versus any control
We found very low‐certainty evidence suggesting there may be no benefit or detriment of visual interventions based on measures of persisting functional ability in activities of daily living (ADL) (2 studies, 55 participants); immediate functional ability in ADL (3 studies, 75 participants); persisting standardised neglect assessments (5 studies, 98 participants); and immediate neglect assessments (7 studies, 142 participants).
Prism adaptation training versus any control
We found very low‐certainty evidence suggesting there may be no benefit or detriment of prism adaptation training based on measures of persisting functional ability in ADL (2 studies, 39 participants); and immediate functional ability in ADL (5 studies, 158 participants); nor on persisting standardised neglect assessments (1 study, 16 participants) or immediate neglect assessments (5 studies, 154 participants).
Body awareness interventions versus any control
We found very low‐certainty evidence suggesting there may be benefit from body awareness interventions based on measures of persisting functional ability in ADL (5 studies, 125 participants). In addition to the very small number of participants, not one of these studies reported an adequate allocation process. We similarly found very low‐quality evidence from the same studies suggesting there may be benefit based on persisting standardised neglect assessments. There was also marked clinical heterogeneity, with a range of different interventions delivered in these studies.
We found very low‐certainty evidence suggesting there may be no benefit or detriment of body awareness interventions based on immediate functional ability in ADL (7 studies, 221 participants) nor on immediate neglect assessments (eleven studies, 357 participants).
Mental function interventions versus any control
We found no evidence suggesting there may be benefit or detriment of mental function interventions based on measures of persisting functional ability in ADL or on neglect assessments. We found very low‐quality evidence suggesting there may be no benefit or detriment of mental function interventions on measures of immediate functional ability in ADL (1 study, 24 participants) nor on immediate neglect assessments (3 studies, 60 participants).
Movement interventions versus any control
We found no evidence suggesting there may be benefit or detriment of movement interventions based on measures of persisting functional ability in ADL or on neglect assessments. We found very low‐quality evidence suggesting there may be benefit of movement interventions based on measures of immediate functional ability in ADL (3 studies, 75 participants); we similarly found very low‐quality evidence suggesting there may be benefit based on immediate neglect assessments (2 studies, 58 participants).
Non‐invasive brain stimulation versus any control
We found very low‐certainty evidence suggesting there may be no benefit nor detriment of NIBS based on measures of persisting functional ability in ADL (3 studies, 92 participants). In addition to the very small number of participants, we were concerned about risk of bias in two studies that delivered different types of NIBS. We found very low‐quality evidence suggesting there may be benefit from NIBS based on immediate functional ability in ADL (6 studies, 160 participants). We found very low‐quality evidence suggesting there may be benefit of NIBS based on persisting standardised neglect assessments (3 studies, 102 participants) or on immediate neglect assessments (10 studies, 244 participants). We had concerns about the accuracy of data reported in three studies included in these analyses.
Electrical stimulation versus any control
We found no evidence suggesting there may be benefit or detriment of electrical stimulation based on measures of persisting functional ability in ADL or neglect assessments, or on immediate functional ability in ADL. We found very low‐quality evidence suggesting there may be benefit from electrical stimulation based on immediate neglect assessments (2 studies, 60 participants). In addition to the very small number of participants, these studies were at high risk of bias and explored different types of stimulation.
Acupuncture versus any control
We found no evidence suggesting there may be benefit or detriment of acupuncture based on measures of persisting functional ability in ADL or neglect assessments. We found very low‐quality evidence suggesting there may be benefit from acupuncture based on measures of immediate functional ability in ADL and immediate neglect assessments (2 studies, 104 participants). In addition to the very small number of participants, these studies were judged to be at high risk of bias for blinding.
Key findings from this updated review
Sixty‐five RCTs (1951 participants) evaluated a range of eight types of non‐pharmacological interventions for people with neglect after adult‐acquired brain injury, all of which included stroke survivors. Most studies measured outcomes using standardised neglect assessments. Many reported immediate effects on ADL, but few reported persisting effects on functional ability in ADL over one month. We acknowledge and welcome an increase in use of persisting ADL assessments since the previous version of this review. Other meaningful outcomes such as discharge destination, falls, mood, quality of life, and adverse events were rarely or never reported
Methodological quality was generally poor or poorly described, and sample sizes were universally underpowered to detect plausible and important clinical effects. Some were explicitly reported as feasibility or pilot studies, but none has yet resulted in the publication of a moderately sized or large trial
Interventions were generally well described, and trialists were helpful in providing additional unpublished methodological details. We were able to describe many of the interventions using the Template for Intervention Description and Replication (TIDieR)
Very low‐quality evidence suggests that certain types of interventions may have persisting benefit based on functional ability in ADL and neglect severity (body awareness interventions, based on 5 studies; NIBS, based on 10 studies; movement interventions, based on 3 studies; electrical stimulation, based on 2 studies; acupuncture, based on 2 studies). These types of interventions may warrant prioritisation for further research focus but would benefit from further feasibility/pilot trials, with strong patient and public involvement, before proceeding to costly definitive RCTs
Despite 65 completed studies, evidence remains insufficient to permit conclusions about the clinical effects of any non‐pharmacological interventions for patients with spatial neglect, because as yet, no adequately powered, appropriately designed trials have been undertaken to answer these important questions. Further research must ensure adequate sample size, minimise risk of bias, and evaluate outcomes of importance to patients
We found no reports of patient and public involvement in any included study
Overall completeness and applicability of evidence
Methods
All studies had small underpowered samples, limiting our ability to make generalisations. We observed no trends in sample size over years, with most studies failing to address issues of statistical power. Available studies should provide sufficient data to enable power calculations for future studies, and we urge researchers to design appropriately powered studies.
Authors of both included and excluded studies were helpful in providing unpublished data. This review therefore presents a considerable quantity of unpublished data and previously unpublished clarification of methods used by the original authors. In contrast to problems of methodological reporting, the reporting quality of the rehabilitation approach used has generally improved since the last version of this review.
Participants
Almost all participants in the included studies had right hemisphere stroke, and most studies were completed in inpatient settings. Therefore, it is appropriate to generalise from the results of these studies only to the population of inpatients with neglect following right hemisphere stroke. We did not extract data on stroke severity, which again limits generalisation. Rehabilitation for people with long‐term persisting neglect may be different for those at earlier stages of recovery from stroke versus other types of adult‐acquired brain injury.
Interventions
Included studies investigated a variety of rehabilitation interventions; thus we have not treated them as a single entity. Although studies differed in number, frequency, and duration of therapy sessions, these were generally well described and interventions were similar enough to enable grouping, providing evidence applicable to clinical settings.
Comparisons
Fifty‐two of the 65 included studies included usual care, sham, no‐treatment, or attention control groups. These comparisons are appropriate for evaluating the effectiveness of interventions, providing results that should be generalisable. However we found considerable variation in what constituted usual care across study settings; future studies should provide sufficient detail to allow replication of control interventions.
Nine of the included studies compared multiple interventions with no specific control. Considerable heterogeneity and variation among interventions make it difficult to allow general conclusions from these studies. Further research is clearly required to identify the relative effectiveness of different non‐pharmacological interventions. In theory, a network meta‐analysis may allow indirect comparison to prioritise classes of intervention for further research. In practice, such an approach would require extreme caution, given the clinical heterogeneity of experimental and control interventions both within and between these classes.
Outcomes
A majority (51 out of 65) of studies reported a measure of functional ability in ADL, but only 16 reported these outcomes at follow‐up (our primary outcome of interest). This lack of follow‐up data on functional ability in ADL limited our ability to determine the persistence or maintenance of functional recovery. Almost all (63 out of 65) of the studies reported a standardised neglect assessment. Seven studies reported no usable data and presented results in graphs or gave P values only. Trialists are encouraged to provide appropriate data in accordance with CONSORT guidance to aid interpretation of study results.
We found very few data on other outcomes, such as discharge destination, falls, or depression. These are known to be of importance to stroke survivors, and including these in future research would improve the completeness of the evidence base.
Quality of the evidence
For this updated review, we judged the quality of evidence using the GRADE approach. We judged all evidence included within meta‐analyses to be of very low quality. We were unable to carry out sensitivity analysis because no studies met our pre‐planned criteria. Key factors contributing to downgrading of evidence within these comparisons included the following.
Risk of bias
We identified concerns about the methods used in a majority of included studies. The method of randomisation used was generally poorly conducted or described, for example, use of unconcealed lists or tombola systems. We assessed 18 of the included studies to be at high risk of bias due to inadequate allocation concealment, and information on 23 further studies was insufficient. We assessed a majority of studies (60 out of 65) to have inadequate evidence of blinding of outcome assessment (see Characteristics of included studies). We did not examine funnel plots because, as pre‐specified in our methods, studies for any one comparison were insufficient to make this worthwhile.
Imprecision
Included studies had small sample sizes, from 4 to 69 participants. Only 8 of the 65 studies had more than 50 participants overall (Dolkun 2019; Fong 2007; Kalra 1997; Kutlay 2018; Nyfeller 2019; Ten‐Brink 2017; Wilkinson 2014; Yang 2017), and none had 50 participants per arm (our minimum size for a phase 3 trial adequately powered to investigate longer‐term clinical effectiveness). A large quantity of study data could not be combined within analyses due to variations in study design and the fact that the maximum number of participants contributing to a single analysis was 311 (Analysis 3.4). Most studies were unclear about the intended study phase, with few specifying they were pilot studies. The small samples available for inclusion in meta‐analysis limit any conclusions drawn from this evidence.
Indirectness
A number of factors contributed to indirectness of the data included within meta‐analyses, particularly the following.
Population: whilst all studies recruited patients after stroke and only 1 included patients with brain injury from other causes, there remained considerable differences in populations such as time post stroke and baseline differences such as stroke severity. No studies acknowledged the impact of other stroke‐related impairments on inclusion, and many studies excluded participants on the basis of previous dementia or stroke, or current cognitive or communication problems, on the grounds that these would adversely affect responsiveness to therapy. These variations contributed to decisions to downgrade the quality of evidence.
Interventions: we synthesised evidence into categories related to a wide range of interventions for neglect to be of greatest use for those in clinical practice. However, this meant there were substantial variations in the interventions within these different categories. For example, our pooled visual interventions include paper‐based scanning training, computer‐based eye movement training, hemi‐field eye patching, and face‐to‐face scanning training. Studies were too few to warrant subgroup analyses for individual interventions, so the variety of interventions included in each comparison limits confidence in the pooled result.
Outcomes: there was substantial variation in measures used for each of our outcomes and how they were reported. For example, studies that included target cancellation as a standardised neglect assessment used a variety of tests involving cancellation of stars, lines, hearts, letters, numbers, cats, balloons, or bells. There was also variation in whether the number of items cancelled or not cancelled was reported. This variation in type of cancellation test alone highlights limitations when data from individual studies are pooled. Equally, whilst we have seen an increase in use of ADL assessments since the previous version of this review, these are subject to similar levels of heterogeneity, thus limiting certainty in our results.
To summarise, we judged the quality of the evidence synthesised within this review to be very low, which limits our certainty in the results. Future research needs to address factors that contribute to the quality of evidence, particularly around eligibility criteria, risk of bias, and choice of outcome measures, to produce results that are useful and meaningful.
Potential biases in the review process
Publication bias
We are confident that we have identified all relevant published studies due to our search methods, which included liaising with authors of relevant Cochrane Reviews; however there is always the potential for human error when screening by title. We sought to obtain unpublished data from study authors and trial registers when appropriate. We last searched trials registers in October 2020; however there may be newly published studies that we did not identify.
Categorisation of interventions
We categorised interventions into broad types to be of greatest utility for clinicians. We devised and assigned studies to categories through discussion between review authors whose professional backgrounds include psychology, occupational therapy, and optometry, which should limit bias in our categorisation. However, we acknowledge that substantial differences between interventions within each category may reduce the applicability of results. Future updates of this review should pre‐plan categories and identify interventions that are clinically relevant to combine. Involvement of key stakeholders is recommended to facilitate this process.
Outcomes
The primary outcome for this review was persisting functional ability in ADL, measured via standardised assessments. We identified six studies that used measures of ADL not included on our pre‐defined list of measures and thus excluded their data from meta‐analyses. These standardised measures could be considered for use in future updates of this review.
For this update and for previous versions of this review, we used the Behavioural Inattention Test (BIT) behavioural subtest as a measure of neglect but not the total BIT nor the conventional BIT subtest, and we excluded study data that did not allow calculation of the behavioural subtest. We did this because this subtest is most relevant to functional outcomes. We believe inclusion of total BIT and conventional BIT in future review updates would be of value, as both include cancellation tests and line bisection (our secondary outcomes).
We noted considerable heterogeneity in outcome assessments used (see Quality of the evidence). We believe consensus is needed between stroke survivors, their families and carers, health professionals, and researchers regarding core outcomes used in trials of interventions for neglect. This would contribute to more meaningful evidence synthesis and meta‐analysis.
Agreements and disagreements with other studies or reviews
Agreements and disagreements between this updated version and previous version
Our conclusions from the 2013 review were as follows.
Limited evidence suggests that cognitive rehabilitation may have an immediate effect on neglect impairment. However, considerable heterogeneity and evidence indicates that this effect was not sustained when studies with high risk of bias were removed.
Some evidence shows subgroup differences between studies with and without an attention control group, highlighting the need for attention control in rehabilitation research.
Evidence is insufficient to permit generalised conclusions about effects of cognitive rehabilitation interventions on functional ability in ADL or on standardised neglect assessments.
Key changes in the methods of this update include the following.
Broadened scope of the review to include any non‐pharmacological intervention.
Amendment of inclusion criteria to include participants with any adult‐acquired brain injury.
Updated searches, increasing the number of included studies from 23 to 65.
Use of the GRADE approach to systematically assess quality of evidence in this updated version.
These changes have increased uncertainty around previous limited evidence.
Limited very low‐quality evidence suggests that certain types of interventions may have benefit for persisting functional ability in ADL. Further research is very likely to have an effect on these conclusions.
Evidence remains insufficient to permit generalised conclusions about effects of non‐pharmacological interventions on functional ability in ADL or on standardised neglect assessments.
Agreements and disagreements with other published reviews
The UK National Clinical Guidelines for Stroke used evidence provided by the previous version of this review plus three studies now included in this update to conclude, "there is insufficient high‐quality evidence to recommend any specific interventions to increase independence" (ISWP 2016). This updated review is in agreement with this guideline. The guidelines also state, "there is some very limited evidence that cognitive rehabilitation may have an immediate beneficial effect on tests of neglect" (ISWP 2016); this is based on evidence from the previous version of this review; this update has highlighted further uncertainty regarding effects of any non‐pharmacological interventions on neglect assessments.
The National Institute for Clinical Excellence (NICE) stroke rehabilitation guidelines do not recommend any specific intervention and suggest "use [of] interventions for visual neglect after stroke that focus on the relevant functional tasks, taking into account the underlying impairment" (NICE 2013). This updated review is in agreement with this guideline.
The Scottish Intercollegiate Guideline Network (SIGN) guidelines for stroke rehabilitation (last updated in 2010) state, "there is insufficient evidence to reach conclusions relating to the effectiveness of any interventions for visual neglect" (SIGN 2010). These guidelines also state, based on evidence from four systematic reviews, that "visual scanning training appears to be the intervention with the most supporting evidence" (SIGN 2010). Our updated review does not directly support this recommendation.
Our review differs from three recent systematic reviews of non‐pharmacological interventions for neglect following stroke. A meta‐analysis of eight studies of differing intervention types (all of which are included in this update) concluded that intervention had a short‐term effect on cognitive function, and that NIBS showed the largest effect size (Kwon 2018). Kwon 2018 analysed studies together in one meta‐analysis. We deliberately did not combine different interventions (e.g. NIBS with prism adaptation) because the interventions are too different. Cotoi 2018 conducted a meta‐analysis of nine studies using theta‐burst stimulation and found improvement but acknowledged that evidence is limited and of low quality. Cotoi 2018 included one cross‐over study and one study that we classified as awaiting assessment due to uncertainty around methods. Salazar 2018 conducted a meta‐analysis of 10 NIBS studies (including three cross‐over studies excluded from this review) and concluded that NIBS is effective; we cannot conclude that NIBS is effective based on uncertainty of the evidence. We are confident that these differences do not impact the conclusions of this updated review.
Authors' conclusions
Implications for practice.
As the effectiveness of non‐pharmacological interventions for reducing disabling effects of neglect and increasing independence remains unproven, no specific rehabilitation approach can be supported or refuted on the basis of current randomised controlled trials. Until robust evidence is available, clinical practice should follow national clinical guidelines (where these exist). Clinical decisions should always be based on an assessment of the individual stroke survivor and informed by knowledge and critical evaluation of the full range of evidence related to treatment for people with spatial neglect. People with neglect should continue to receive general stroke or neurological rehabilitation services and should have the opportunity to take part in high‐quality research. Clinicians are strongly encouraged to participate in high‐quality trials. Funding agencies, clinical educators, and policy makers should encourage and facilitate research into spatial neglect to improve clinical practice and outcomes. Appropriate resources are required (e.g. staff, time commitment, data management) to successfully deliver large, long‐term trials. The costs of high‐quality rehabilitation trials can be recouped, as effective interventions reduce long‐term care needs and improve quality of life for people with spatial neglect.
Implications for research.
Our implications for research are unchanged from those found in the previous version of this review. Evidence is still sufficiently compelling to encourage further trials of non‐pharmacological interventions for neglect; however these trials need careful thought. We have identified 65 small underpowered feasibility studies; however before similar studies can be conducted, research and funding are needed to establish what will work in clinical practice, what is important to stroke survivors, and what outcome measures are appropriate to further this field.
A shift in focus to the person rather than the impairment may be required; stroke survivors with cognitive impairments such as neglect are often excluded from general rehabilitation studies. Trialists are encouraged to include these patients in general rehabilitation trials and to include measures of neglect. In addition, we identified 23 studies delivering multiple or combined interventions. Combination interventions may warrant further investigation to establish by means of pragmatic trials whether multiple interventions, such as NIBS plus scanning, provide an advantage over a single intervention.
Future studies must improve on current methodological and reporting issues.
Prior registration of future trials is essential to allow full assessment. Protocols that sufficiently describe procedural aspects, such as randomisation, concealment, completeness of follow‐up, and blinding of assessors, should be made available. Trialists should refer to the Cochrane Handbook (Chapter 8) for a description of acceptable methods of randomisation.
Future studies must avoid using non‐random allocation methods (such as matching) and tombola systems that preclude verification of the allocation process.
Trialists are encouraged to assess and report whether any attempted blinding of outcome assessors is achieved in practice. By its nature, rehabilitation for neglect is likely to be restricted to single‐blind trials (of outcome assessors), as blinding of participants and therapists is not usually achievable.
Cross‐over trials are not appropriate for rehabilitation for cognitive impairments, as effects of one approach may contaminate the next; the aim of rehabilitation is to promote independence and maintain treatment effects rather than 'washout' treatment effects.
Future trials should state their intended purpose (e.g. pilot, feasibility, definitive); a minority of included studies stated they were pilot/feasibility studies. Proof‐of‐concept studies are essential before studies of effectiveness.
Adequate statistical power is essential to detect a clinically meaningful difference in definitive trials and will require multi‐centre collaborations. There is no justification for claims that trials of complex interventions are not appropriate or possible or are too difficult, and suggestions that they would be too expensive should be balanced against long‐term care costs.
Future trials should provide adequate sample description and theoretical justification, and should consider using stratified randomisation to avoid imbalance of any factors likely to confound the trial. Neglect is a heterogeneous condition, and it is unlikely that a single rehabilitation approach is appropriate for all patients with neglect.
Complete follow‐up and intention‐to‐treat analysis are necessary, as a high dropout rate may be an important indication of effectiveness. Information is provided in the Cochrane Handbook (Chapter 6).
Researchers must expand the aim of studies; trials aiming to treat or compensate for neglect to improve ADL require different study designs and outcome measures.
More information about usual care is required, including time and detailed type of therapy received by participants in rehabilitation trials, as this is likely to influence outcomes.
Whilst we acknowledge an increase in use of ADL assessments since the previous version of this review, trials must assess both functional activities of daily living and neglect at a follow‐up assessment at least one month post intervention (i.e. persisting effects). Maintenance of function is of key importance to stroke survivors.
Trialists should also assess other outcomes that are of importance to stroke survivors, including falls and quality of life.
Future studies should use patient and public involvement to ensure study design, interventions, and outcomes are acceptable to stroke survivors.
This review is ongoing, and the review authors would be grateful to receive information on ongoing studies for a future update.
What's new
| Date | Event | Description |
|---|---|---|
| 12 May 2021 | New citation required but conclusions have not changed | Despite the inclusion of 65 RCTs, the effectiveness of non‐pharmacological interventions for reducing the disabling effects of neglect and increasing independence remains unproven and largely unstudied despite numerous small trials. No rehabilitation intervention for spatial neglect can be supported or refuted based on current evidence |
| 12 May 2021 | New search has been performed | We added 44 new trials to 21 of the 23 trials that we included in the previous version. Sixty‐five trials (1951 participants) are now included. We excluded 2 previously included studies as either fewer than 50% of participants had neglect, or we were unable to confirm participants had neglect. We have re‐written all sections using standard Cochrane sub‐headings. We have expanded the inclusion criteria to include any non‐pharmacological intervention. Our primary outcome has changed to persisting effects on functional disability to reflect the importance of this outcome for people with stroke. We have changed the comparisons: for this version of the review, we changed the presentation of statistical comparisons using 8 broad treatment types. We have included Patient, Carer, and Public Involvement in Research by consulting with stroke survivors |
History
Protocol first published: Issue 2, 2002 Review first published: Issue 2, 2002
| Date | Event | Description |
|---|---|---|
| 17 April 2013 | New citation required but conclusions have not changed | Despite the addition of 11 further trials, the key conclusions of this review have not changed greatly since the 2006 version: The effectiveness of cognitive rehabilitation for reducing the disabling effects of neglect and increasing independence remains unproven. No rehabilitation approach can be supported or refuted from current randomised controlled trials |
| 23 September 2012 | New search has been performed | We added 11 new trials to the 12 trials that we included in the previous version. Twenty‐three trials (628 participants) are now included. We have rewritten the Discussion section using standard Cochrane sub‐headings. We have expanded the outcomes: previous versions of the review had functional disability, neglect assessments, and discharge destination as outcomes. For this update, we added a number of secondary outcomes that had been identified as important to stroke survivors. This brings this review in line with other reviews of visual problems after stroke. We have changed the comparisons: for this version of the review, we changed the presentation of statistical comparisons. In particular, we amended the sub‐group comparisons of bottom‐up and top‐down approaches, so that analyses included sub‐groups of types of treatment |
| 4 August 2008 | Amended | Converted to new review format |
| 26 April 2006 | New search has been performed | For this updated review, we excluded several previously included non‐randomised trials to reduce bias. We added several new, or newly identified, randomised controlled trials (RCTs), resulting in a review of 306 participants from 12 RCTs |
Acknowledgements
We would like to thank the principal investigators for many of the included and excluded studies who provided additional information to that published. We are especially indebted to Hazel Fraser and Josh Cheyne at the Cochrane Stroke Group for their continued support and specialist guidance. We would like to thank Bernhard Elsner and Jan Mehrholz for sharing information about the Cochrane Review of brain stimulation after stroke. We would also like to thank our Patient Carer and Public Involvement (PCPI) group members Ann Bamford, Peter Dawson, and Margery Savin.
Searches for the first version of this review were funded by grants to Nadina Lincoln from the Stroke Association and the UK NHS Research and Development Programme for Physical and Complex Disabilities. Michael Dewey provided statistical input to the first published version of this review, for which we are very grateful. Christine Hazelton's time on this review was funded in part by the RNIB (Royal National Institute for Blind People) and the Stroke Association. The Stroke Association funded Audrey Bowen's time in part.
Verity Longley's time was supported by the National Institute for Health Research (NIHR Development and Skills Enhancement Award, NIHR300762). Claire Mitchell's time and PCPI work were supported by NIHR Cochrane Review Incentive Scheme funding (Award Reference Number: NIHR130742). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research, or the Department of Health and Social Care.
Appendices
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor: [Cerebrovascular Disorders] this term only #2 MeSH descriptor: [Basal Ganglia Cerebrovascular Disease] explode all trees #3 MeSH descriptor: [Brain Ischemia] explode all trees #4 MeSH descriptor: [Carotid Artery Diseases] explode all trees #5 MeSH descriptor: [Cerebrovascular Trauma] explode all trees #6 MeSH descriptor: [Intracranial Arterial Diseases] this term only #7 MeSH descriptor: [Intracranial Arteriovenous Malformations] explode all trees #8 MeSH descriptor: [Intracranial Embolism and Thrombosis] explode all trees #9 MeSH descriptor: [Intracranial Hemorrhages] explode all trees #10 MeSH descriptor: [Intracranial Hemorrhage, Hypertensive] this term only #11 MeSH descriptor: [Stroke] this term only #12 MeSH descriptor: [Brain Infarction] explode all trees #13 MeSH descriptor: [Stroke, Lacunar] this term only #14 MeSH descriptor: [Vasospasm, Intracranial] this term only #15 MeSH descriptor: [Vertebral Artery Dissection] this term only #16 MeSH descriptor: [Hypoxia, Brain] explode all trees #17 (stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc or cva or apoplex or SAH):ti,ab,kw #18 ((brain* or cerebr* or cerebell* or intracran* or intracerebral) near/5 (isch?emi* or infarct* or thrombo* or emboli* or occlus*)):ti,ab,kw #19 ((brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid) near/5 (haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed*)):ti,ab,kw #20 MeSH descriptor: [Hemiplegia] this term only #21 MeSH descriptor: [Paresis] explode all trees #22 (hemipleg* or hemipar* or paresis or paretic):ti,ab,kw #23 ((unilateral or visual or hemispatial or attentional or spatial) near/5 neglect):ti,ab,kw #24 ((cerebral or brain or subarachnoid) near/5 (haemorrhage* or haemorrhage* or haematoma* or hematoma* or bleed)):ti,ab,kw #25 ((trauma* or acquired) near/5 brain injur*):ti,ab,kw #26 MeSH descriptor: [Brain Damage, Chronic] explode all trees #27 MeSH descriptor: [Brain Injuries] this term only #28 MeSH descriptor: [Brain Concussion] explode all trees #29 MeSH descriptor: [Brain Hemorrhage, Traumatic] explode all trees #30 MeSH descriptor: [Brain Injury, Chronic] this term only #31 MeSH descriptor: [Diffuse Axonal Injury] this term only #32 MeSH descriptor: [Craniocerebral Trauma] this term only #33 MeSH descriptor: [Head Injuries, Closed] explode all trees #34 MeSH descriptor: [Intracranial Hemorrhage, Traumatic] explode all trees #35 MeSH descriptor: [Brain Abscess] explode all trees #36 MeSH descriptor: [Central Nervous System Infections] explode all trees #37 MeSH descriptor: [Encephalitis] explode all trees #38 MeSH descriptor: [Meningitis, Viral] explode all trees #39 (encephalitis or meningitis):ti,ab,kw #40 MeSH descriptor: [Brain Neoplasms] explode all trees #41 ((brain or cerebr*) near/5 (neoplasm* or lesion* or tumor* or tumour*)):ti,ab,kw #42 {OR #1‐#41} #43 MeSH descriptor: [Perceptual Disorders] explode all trees #44 MeSH descriptor: [Perception] explode all trees #45 MeSH descriptor: [Attention] this term only #46 MeSH descriptor: [Extinction, Psychological] this term only #47 (hemineglect or hemi‐neglect):ti,ab,kw #48 (unilateral or spatial) near/5 neglect):ti,ab,kw #49 (perception or inattention or hemi‐inattention or attention or extinction):ti,ab,kw #50 ((perceptual or visuo?spatial or visuo?perceptual or attentional) near/5 (disorder* or deficit* or impairment* or abilit*)):ti,ab,kw #51 ((perceptual or visuo?spatial or visuo?perceptual or attention* or cognit* or scanning*) near/5 (training or re‐training or rehabilitation or intervention or therapy)):ti,ab,kw #52 {or #43‐#51} #53 #42 AND #52
Appendix 2. MEDLINE (Ovid) search strategy
1. Cerebrovascular disorders/ or exp basal ganglia cerebrovascular disease/ or exp brain ischemia/ or exp carotid artery diseases/ or exp cerebrovascular trauma/ or exp intracranial arterial diseases/ or exp intracranial arteriovenous malformations/ or exp "intracranial embolism and thrombosis"/ or exp intracranial hemorrhages/ or stroke/ or exp brain infarction/ or stroke, lacunar/ or vasospasm, intracranial/ or vertebral artery dissection/ or exp hypoxia, brain/ 2. (stroke$ or poststroke or post‐stroke or apoplex$ or cerebral vasc$ or cerebrovasc$ or cva or SAH).tw. 3. ((brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw. 4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw. 5. exp hemiplegia/ or exp paresis/ 6. (hemipleg$ or hemipar$ or paresis or paretic).tw. 7. ((cerebral or brain or subarachnoid) adj5 (haemorrhage or haemorrhage or haematoma or hematoma or bleed)).tw. 8. ((trauma$ or acquired) adj5 brain injur$).tw. 9. exp brain damage, chronic/ or brain injuries/ or exp brain concussion/ or exp brain haemorrhage, traumatic/ or brain injury, chronic/ or diffuse axonal injury/ 10. craniocerebral trauma/ or exp head injuries, closed/ or exp intracranial haemorrhage, traumatic/ 11. exp brain abscess/ or exp central nervous system infections/ or exp encephalitis/ or exp meningitis, viral/ 12. (encephalitis or meningitis).tw. 13. exp brain neoplasms/ 14. ((brain or cerebr$) adj5 (neoplasm$ or lesion$ or tumor$ or tumour$)).tw. 15. or/1‐14 16. exp Perceptual Disorders/ 17. exp perception/ 18. Attention/ 19. "Extinction (psychology)"/ 20. (hemineglect or hemi‐neglect).tw. 21. ((unilateral or spatial) adj5 neglect).tw. 22. (perception or inattention or hemi‐inattention or attention or extinction).tw. 23. ((perceptual or visuo?spatial or visuo?perceptual or attentional) adj5 (disorder$ or deficit$ or impairment$ or abilit$)).tw. 24. ((perceptual or visuo?spatial or visuo?perceptual or attention$ or cognit$ or scanning$) adj5 (training or re‐training or rehabilitation or intervention or therapy)).tw. 25. or/16‐24 26. Randomized Controlled Trials as Topic/ 27. Random Allocation/ 28. Controlled Clinical Trials as Topic/ 29. control groups/ 30. clinical trials as topic/ or clinical trials, phase i as topic/ or clinical trials, phase ii as topic/ or clinical trials, phase iii as topic/ or clinical trials, phase iv as topic/ 31. double‐blind method/ 32. single‐blind method/ 33. Placebos/ 34. placebo effect/ 35. cross‐over studies/ 36. randomized controlled trial.pt. 37. controlled clinical trial.pt. 38. (clinical trial or clinical trial phase i or clinical trial phase ii or clinical trial phase iii or clinical trial phase iv).pt. 39. (random$ or RCT or RCTs).tw. 40. (controlled adj5 (trial$ or stud$)).tw. 41. (clinical$ adj5 trial$).tw. 42. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw. 43. (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw. 44. ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw. 45. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw. 46. (cross‐over or cross over or crossover).tw. 47. (placebo$ or sham).tw. 48. trial.ti. 49. (assign$ or allocat$).tw. 50. controls.tw. 51. or/26‐50 52. 15 and 25 and 51
Appendix 3. Embase (Ovid) search strategy
1. cerebrovascular disease/ or brain disease/ or exp basal ganglion hemorrhage/ or exp brain hemangioma/ or exp brain hematoma/ or exp brain hemorrhage/ or exp brain infarction/ or exp brain ischemia/ or exp carotid artery disease/ or exp cerebral artery disease/ or exp cerebrovascular accident/ or exp cerebrovascular malformation/ or exp intracranial aneurysm/ or exp occlusive cerebrovascular disease/ or exp vertebrobasilar insufficiency/ 2. (stroke$ or poststroke or post‐stroke or apoplex$ or cerebral vasc$ or cerebrovasc$ or cva or SAH).tw. 3. ((brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw. 4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw. 5. paralysis/ or exp hemiplegia/ or exp paresis/ 6. (hempar$ or hemipleg$ or paresis or paretic).tw. 7. ((trauma$ or acquired) adj5 brain injur$).tw. 8. exp brain damage, chronic/ or brain Injuries/ or exp brain concussion/ or exp brain hemorrhage, traumatic/ or brain injury, chronic/ or diffuse axonal injury/ or craniocerebral trauma/ or exp head injuries, closed/ or exp intracranial hemorrhage, traumatic/ or exp brain abscess/ or exp central nervous system infections/ or exp encephalitis/ or exp meningitis, viral/ 9. (encephalitis or meningitis).tw. 10. exp brain neoplasms/ 11. ((brain or cerebr$) adj5 (neoplasm$ or lesion$ or tumor$ or tumour$)).tw. 12. or/1‐11 13. exp perception disorder/ 14. exp perception/ 15. exp attention/ 16. visual deprivation/ 17. (hemineglect or hemi‐neglect).tw. 18. ((unilateral or spatial or hemi?spatial) adj5 neglect).tw. 19. (perception or inattention or hemi‐inattention or attention or extinction).tw. 20. ((perceptual or visuo?spatial or visuo?perceptual or attentional) adj5 (disorder$ or deficit$ or impairment$ or abilit$ or dysfunction)).tw. 21. ((perceptual or visuo?spatial or visuo?perceptual or attention$ or cognit$ or scanning$) adj5 (training or retraining or rehabilitation or intervention or therapy)).tw. 22. or/13‐21 23. Randomized Controlled Trial/ or "randomized controlled trial (topic)"/ 24. Randomization/ 25. Controlled clinical trial/ or "controlled clinical trial (topic)"/ 26. control group/ or controlled study/ 27. clinical trial/ or "clinical trial (topic)"/ or phase 1 clinical trial/ or phase 2 clinical trial/ or phase 3 clinical trial/ or phase 4 clinical trial/ 28. Crossover Procedure/ 29. Double Blind Procedure/ 30. Single Blind Procedure/ or triple blind procedure/ 31. placebo/ or placebo effect/ 32. (random$ or RCT or RCTs).tw. 33. (controlled adj5 (trial$ or stud$)).tw. 34. (clinical$ adj5 trial$).tw. 35. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw. 36. (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw. 37. ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw. 38. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw. 39. (cross‐over or cross over or crossover).tw. 40. (placebo$ or sham).tw. 41. trial.ti. 42. (assign$ or allocat$).tw. 43. controls.tw. 44. or/23‐43 45. 12 and 22 and 44
Appendix 4. CINAHL (Ebsco) search strategy
S1(MH "Cerebrovascular Disorders") OR (MH "Basal Ganglia Cerebrovascular Disease+") OR (MH "Carotid Artery Diseases+") OR (MH "Cerebral Ischemia+") OR (MH "Cerebral Vasospasm") OR (MH "Intracranial Arterial Diseases+") OR (MH "Intracranial Embolism and Thrombosis") OR (MH "Intracranial Hemorrhage+") OR (MH "Stroke") OR (MH "Vertebral Artery Dissections") S2(MH "Stroke Patients") OR (MH "Stroke Units") S3TI ( stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc or cva or apoplex or SAH ) or AB ( stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc or cva or apoplex or SAH ) S4TI ( brain* or cerebr* or cerebell* or intracran* or intracerebral ) or AB ( brain* or cerebr* or cerebell* or intracran* or intracerebral ) S5TI ( ischemi* or ischaemi* or infarct* or thrombo* or emboli* or occlus* ) or AB ( ischemi* or ischaemi* or infarct* or thrombo* or emboli* or occlus* ) S6S4 and S5 S7TI ( brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid ) or AB ( brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid ) S8TI ( haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed* ) or AB ( haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed* ) S9S7 AND S8 S10(MH "Hemiplegia") S11TI ( hemipleg* or hemipar* or paresis or paretic ) or AB ( hemipleg* or hemipar* or paresis or paretic ) S12(MH "Brain Injuries") OR (MH "Brain Concussion") OR (MH "Brain Neoplasms+") OR (MH "Brain Damage, Chronic") OR (MH "Head Injuries") OR (MH "Brain Abscess") S13TI (brain or head or intracran* or cerebr* or cerebell*) N5 (injur* or contusion* or hypoxi* or damage* or inflamm* or concussion or trauma$ or fractur* or neoplasm* or lesion* or tumor* or tumour* or cancer* or infection*) S14(MH "Meningitis") OR (MH "Encephalitis") S15S1 OR S2 OR S3 OR S6 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 S16(MH "Perceptual Disorders+") S17(MH "Perception+") S18(MH "attention") S19(MH "Unilateral Neglect (Saba CCC)") or (MH "Unilateral Neglect (NANDA)") S20TI (hemineglect or hemi‐neglect) or AB (hemineglect or hemi‐neglect) S21TI (unilateral or spatial) or AB (unilateral or spatial) S22TI (neglect) or AB (neglect) S23S21 AND S22 S24TI (perception or inattention or hemi‐inattention or attention or extinction) or AB (perception or inattention or hemi‐inattention or attention or extinction) S25TI (perceptual or visuo#spatial or visuo#perceptual or attentional) or AB (perceptual or visuo#spatial or visuo#perceptual or attentional) S26TI (disorder* or deficit* or impairment* or abilit*) or AB (disorder* or deficit* or impairment* or abilit*) S27S25 and S26 S28TI (perceptual or visuo#spatial or visuo#perceptual ot attention* or cognit* or scanning*) or AB (perceptual or visuo#spatial or visuo#perceptual ot attention* or cognit* or scanning*) S29TI ( training or re‐training or rehabilitation or intervention or therapy) or AB (training or re‐training or rehabilitation or intervention or therapy) S30S28 AND S29 S31S16 OR S17 OR S18 OR S19 OR S20 OR S23 OR S24 OR S27 OR S30 S32(MH "Randomized Controlled Trials") or (MH "Random Assignment") or (MH "Random Sample+") S33(MH "Clinical Trials") or (MH "Intervention Trials") or (MH "Therapeutic Trials") S34(MH "Double‐Blind Studies") or (MH "Single‐Blind Studies") or (MH "Triple‐Blind Studies") S35(MH "Control (Research)") or (MH "Control Group") or (MH "Placebos") or (MH "Placebo Effect") S36(MH "Crossover Design") OR (MH "Quasi‐Experimental Studies") S37PT (clinical trial or randomized controlled trial) S38TI (random* or RCT or RCTs) or AB (random* or RCT or RCTs) S39TI (controlled N5 (trial* or stud*)) or AB (controlled N5 (trial* or stud*)) S40TI (clinical* N5 trial*) or AB (clinical* N5 trial*) S41TI ((control or treatment or experiment* or intervention) N5 (group* or subject* or patient*)) or AB ((control or treatment or experiment* or intervention) N5 (group* or subject* or patient*)) S42((control or experiment* or conservative) N5 (treatment or therapy or procedure or manage*)) or AB ((control or experiment* or conservative) N5 (treatment or therapy or procedure or manage*)) S43TI ((singl* or doubl* or tripl* or trebl*) N5 (blind* or mask*)) or AB ((singl* or doubl* or tripl* or trebl*) N5 (blind* or mask*)) S44TI (cross‐over or cross over or crossover) or AB (cross‐over or cross over or crossover) S45TI (placebo* or sham) or AB (placebo* or sham) S46TI trial S47TI (assign* or allocat*) or AB (assign* or allocat*) S48TI controls or AB controls S49TI (quasi‐random* or quasi random* or pseudo‐random* or pseudo random*) or AB (quasi‐random* or quasi random* or pseudo‐random* or pseudo random*) S50S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 S51S15 AND S31 AND S50
Appendix 5. PsycINFO (Ovid) search strategy
1. cerebrovascular disorders/ or cerebral hemorrhage/ or exp cerebral ischemia/ or cerebrovascular accidents/ or subarachnoid hemorrhage/ 2. (stroke$ or post stroke or poststroke or post‐stroke or apoplex$ or cerebral vasc$ or cerebrovasc$ or cva or SAH).tw. 3. ((brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw. 4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw. 5. exp brain damage/ or traumatic brain injury/ or exp brain concussion/ or exp head injuries/ 6. ((brain or cerebr$) adj5 (injur$ or hypoxi$ or damage$ or concussion or trauma$ or neoplasm$ or lesion$ or tumor$ or tumour$ or cancer$ or infection$)).tw. 7. exp encephalitis/ or exp meningitis/ 8. (encephalitis or meningitis).tw. 9. exp brain neoplasms/ 10. ((brain or cerebr$) adj5 (neoplasm$ or lesion$ or tumor$ or tumour$)).tw. 11. or/1‐10 12. exp perceptual disturbances/ or exp perceptual distortion/ or exp sensory neglect/ 13. exp perception/ 14. exp "Extinction (Learning)"/ 15. (hemineglect or hemi‐neglect).tw. 16. ((unilateral or spatial) adj5 neglect).tw. 17. (perception or inattention or hemi‐inattention or attention or extinction).tw. 18. ((perceptual or visuo?spatial or visuo?perceptual or attentional) adj5 (disorder$ or deficit$ or impairment$ or abilit$)).tw. 19. ((perceptual or visuo?spatial ro visuo?perceptual or attention$ or cognit$ or scanning$) adj5 (training or re‐training or rehabilitation or intervention or therapy)).tw. 20. or/12‐19 21. clinical trials/ or treatment effectiveness evaluation/ or placebo/ 22. (random$ or RCT or RCTs).tw. 23. (controlled adj5 (trial$ or stud$)).tw. 24. (clinical$ adj5 trial$).tw. 25. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw. 26. (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw. 27. ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw. 28. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw. 29. (cross‐over or cross over or crossover).tw. 30. (placebo$ or sham).tw. 31. trial.ti. 32. (assign$ or allocat$).tw. 33. controls.tw. 34. or/21‐33 35. 11 and 20 and 34
Appendix 6. US National Institutes of Health Ongoing Trials Register search strategy
( neglect OR hemispatial OR unilateral ) AND AREA[StudyType] EXPAND[Term] COVER[FullMatch] "Interventional" AND AREA[ConditionSearch] ( Vertebral Artery OR Brain Infarction OR Intracranial Hemorrhages OR Carotid Artery Diseases OR Brain Ischemia OR Cerebral Hemorrhage OR Cerebrovascular Disorders OR Stroke ) AND AREA[StudyFirstPostDate] EXPAND[Term] RANGE[02/01/2017, 03/25/2020]
Basic search: neglect AND stroke OR hemispatial AND stroke OR neglect AND brain OR hemispatial AND brain OR neglect AND cerebral OR hemispatial AND cerebral
Appendix 7. World Health Organization International Clinical Trials Registry Platform search strategy
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch)
Basic search: neglect AND stroke OR hemispatial AND stroke OR neglect AND brain OR hemispatial AND brain OR neglect AND cerebral OR hemispatial AND cerebral
Appendix 8. Previous review search strategy
Searching other resources
For the purpose of this and other reviews (Lincoln 2001; Das Nair 2007), we originally searched simultaneously for trials in four areas of stroke rehabilitation (cognitive rehabilitation, occupational therapy, speech therapy, and treatment for mood disorders) using online computerised bibliographic databases: MEDLINE (1966 to 1998), BIDS Embase (1980 to 1998), CINAHL (1983 to 1998), PsycLIT (1974 to 1998), and CLINPSYCH (1980 to November 1994). We conducted these computerised searches using combinations of the following descriptors/key words: stroke/cerebrovascular accidents/neurological disability and randomised controlled/clinical trials/random allocation/double blind method and rehabilitation/remedial therapy/treatment/intervention and cognitive/unilateral neglect/visuospatial/visuoperceptual/memory/attention span/concentration/hemianopia/attentional deficits/activities of daily living/occupational therapy/leisure/dressing/self‐care/domiciliary rehabilitation.
To ensure that studies not listed in the above databases were not overlooked, in 1999 we handsearched all volumes of the journals listed below. The 1999 handsearch included a broad range of journals, as it covered studies in four areas of rehabilitation, only one of which (neglect) was relevant to this specific review. Therefore, for the 2006 update, we checked the Master List of journals that is searched by the Cochrane Collaboration (www.cochrane.us/masterlist.asp). We found that the journals relevant to neglect had been handsearched. The resulting studies would be found from the search of the Cochrane Central Register of Controlled Trials (CENTRAL) carried out quarterly by the Cochrane Stroke Group, and we did not wish to duplicate effort:
American Journal of Occupational Therapy (1947 to 1998);
Aphasiology (1987 to 1998);
Australian Occupational Therapy Journal (1965 to 1998);
British Journal of Occupational Therapy (1950 to 1998);
British Journal of Therapy and Rehabilitation (1994 to 1998);
Canadian Journal of Occupational Therapy (1970 to 1998);
Clinical Rehabilitation (1987 to 1998);
Disability Rehabilitation (1992 to 1998), formerly International Disability Studies (1987 to 1991), formerly International Rehabilitation Medicine (1979 to 1986);
International Journal of Language & Communication Disorders (1998), formerly European Journal of Disorders of Communication (1985 to 1997), formerly British Journal of Disorders of Communication (1977 to 1984);
Journal of Clinical Psychology in Medical Settings (1994 to 1998), formerly Journal of Clinical Psychology (1944 to 1994);
Journal of Developmental and Physical Disabilities (1992 to 1998), formerly Journal of the Multihandicapped Person (1989 to 1991);
Journal of Rehabilitation (1963 to 1998);
International Journal of Rehabilitation Research (1977 to 1998);
Journal of Rehabilitation Science (1989 to 1996);
Neuropsychological Rehabilitation (1987 to 1998);
Neurorehabilitation (1991 to 1998);
Occupational Therapy International (1994 to 1998);
Physiotherapy Theory and Practice (1990 to 1998), formerly Physiotherapy Practice (1985 to 1989);
Physical Therapy (1988 to 1998);
Rehabilitation Psychology (1982 to 1998); and
The Journal of Cognitive Rehabilitation (1988 to 1998), formerly Cognitive Rehabilitation (1983 to 1987).
The pre‐1999 searching and selection activities were carried out simultaneously for four reviews.
The National Research Register was searched for the 2012 review; however it has since been archived and not superseded.
We used the three citation index databases Science Citation Index (SCI), Social Sciences Citation Index (SSCI), and Arts and Humanities Citation Index (A&HCI) for citation tracking of relevant included studies.
Selection of studies
At least two review authors (NBL, AB for 1999 and 2006 versions; NBL, AB, CH, and AP for 2013 version) independently selected studies to be included in this review using the four inclusion criteria (types of trials, participants, interventions, and outcome measures). We independently assessed the methodological quality of studies, with reference to the Cochrane Handbook for Systematic Reviews of Interventions (Cochrane Handbook), and selected, entered, and cross‐checked data for analysis. We resolved disagreements by discussion.
Data and analyses
Comparison 1. Visual interventions versus any control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Activities of daily living: persisting effects | 2 | 55 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.57, 0.49] |
| 1.1.1 CBS | 1 | 21 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐0.86, 0.86] |
| 1.1.2 FIM | 1 | 34 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.75, 0.62] |
| 1.1.3 BI | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 1.2 Activities of daily living: immediate effects | 3 | 75 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.15 [‐0.60, 0.30] |
| 1.2.1 CBS | 2 | 36 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.64, 0.67] |
| 1.2.2 FIM | 1 | 39 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐0.94, 0.33] |
| 1.3 Neglect outcomes: persisting effects | 5 | 98 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.33, 0.48] |
| 1.3.1 Target cancellation | 2 | 33 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.41 [‐0.30, 1.11] |
| 1.3.2 Line bisection | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 1.3.3 BIT behavioural subtest | 3 | 65 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.59, 0.40] |
| 1.4 Neglect outcomes: immediate effects | 7 | 142 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.26, 0.42] |
| 1.4.1 Target cancellation | 3 | 46 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.58, 0.60] |
| 1.4.2 Line bisection | 1 | 28 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.71 [‐0.06, 1.48] |
| 1.4.3 BIT behavioural subtest | 3 | 68 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐0.64, 0.35] |
Comparison 2. Prism adaptation versus any control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Activities of daily living: persisting effects | 2 | 39 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.29 [‐0.93, 0.35] |
| 2.1.1 CBS | 2 | 39 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.29 [‐0.93, 0.35] |
| 2.1.2 BI | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 2.1.3 FIM | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 2.2 Activities of daily living: immediate effects | 5 | 158 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.12, 0.51] |
| 2.2.1 CBS | 5 | 158 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.12, 0.51] |
| 2.2.2 BI | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 2.2.3 FIM | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 2.3 Neglect outcomes: persisting effects | 1 | 16 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.96, 1.06] |
| 2.3.1 Target cancellation | 1 | 16 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.96, 1.06] |
| 2.3.2 Line bisection | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 2.3.3 BIT behavioural subtest | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 2.4 Neglect outcomes: immediate effects | 5 | 154 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.28 [‐0.05, 0.60] |
| 2.4.1 Target cancellation | 4 | 120 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.31 [‐0.07, 0.68] |
| 2.4.2 Line bisection | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 2.4.3 BIT behavioural subtest | 1 | 34 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.17 [‐0.50, 0.85] |
Comparison 3. Body awareness interventions versus any control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Activities of daily living: persisting effects | 5 | 125 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.61 [0.24, 0.97] |
| 3.1.1 CBS | 2 | 65 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.34 [‐0.15, 0.83] |
| 3.1.2 FIM | 2 | 48 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.83 [0.23, 1.43] |
| 3.1.3 BI | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 3.1.4 mRS | 1 | 12 | Std. Mean Difference (IV, Fixed, 95% CI) | 1.50 [0.14, 2.86] |
| 3.2 Activities of daily living: immediate effects | 7 | 221 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.26 [‐0.01, 0.53] |
| 3.2.1 CBS | 2 | 76 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.35 [‐0.10, 0.80] |
| 3.2.2 FIM | 3 | 91 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.39 [‐0.04, 0.82] |
| 3.2.3 BI | 1 | 42 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.29 [‐0.91, 0.32] |
| 3.2.4 mRS | 1 | 12 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.68 [‐0.51, 1.88] |
| 3.3 Neglect outcomes: persisting effects | 5 | 125 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.36 [0.00, 0.72] |
| 3.3.1 Target cancellation | 2 | 49 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.50 [‐0.08, 1.08] |
| 3.3.2 Line bisection | 1 | 22 | Std. Mean Difference (IV, Fixed, 95% CI) | 1.09 [0.18, 2.00] |
| 3.3.3 BIT behavioural subtest | 2 | 54 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.55, 0.53] |
| 3.4 Neglect outcomes: immediate effects | 10 | 311 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.16 [‐0.07, 0.39] |
| 3.4.1 Target cancellation | 7 | 227 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.16, 0.37] |
| 3.4.2 Line bisection | 1 | 22 | Std. Mean Difference (IV, Fixed, 95% CI) | 1.33 [0.39, 2.27] |
| 3.4.3 BIT behavioural subtest | 2 | 62 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.48, 0.52] |
| 3.5 Discharge destination (home) | 1 | 50 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.45, 4.35] |
| 3.6 Adverse events | 2 | 130 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.36 [0.05, 2.61] |
Comparison 4. Mental function interventions versus any control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Activities of daily living: persisting effects | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 4.1.1 CBS | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 4.1.2 FIM | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 4.1.3 BI | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 4.2 Activities of daily living: immediate effects | 1 | 24 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.49, 1.12] |
| 4.2.1 CBS | 1 | 24 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.49, 1.12] |
| 4.2.2 FIM | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 4.2.3 BI | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 4.3 Neglect outcomes: persisting effects | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 4.3.1 Target cancellation | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 4.3.2 Line bisection | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 4.3.3 BIT behavioural subtest | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 4.4 Neglect outcomes: immediate effects | 3 | 84 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.32, 0.53] |
| 4.4.1 Target cancellation | 3 | 84 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.32, 0.53] |
| 4.4.2 Line bisection | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 4.4.3 BIT behavioural subtest | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 4.5 Adverse events | 1 | 10 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.39 [0.15, 372.38] |
4.1. Analysis.

Comparison 4: Mental function interventions versus any control, Outcome 1: Activities of daily living: persisting effects
4.3. Analysis.

Comparison 4: Mental function interventions versus any control, Outcome 3: Neglect outcomes: persisting effects
4.5. Analysis.

Comparison 4: Mental function interventions versus any control, Outcome 5: Adverse events
Comparison 5. Movement intervention versus any control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Activities of daily living: persisting effects | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 5.1.1 CBS | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 5.1.2 FIM | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 5.1.3 BI | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 5.2 Activities of daily living: immediate effects | 3 | 75 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.57 [0.09, 1.04] |
| 5.2.1 CBS | 3 | 75 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.57 [0.09, 1.04] |
| 5.2.2 FIM | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 5.2.3 BI | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 5.3 Neglect outcomes: persisting effects | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 5.3.1 Target cancellation | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 5.3.2 Line bisection | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 5.3.3 BIT behavioural subtest | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 5.4 Neglect outcomes: immediate effects | 2 | 58 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.57 [0.04, 1.10] |
| 5.4.1 Target cancellation | 2 | 58 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.57 [0.04, 1.10] |
| 5.4.2 Line bisection | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 5.4.3 BIT behavioural subtest | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 5.5 Adverse events | 1 | 38 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
5.1. Analysis.

Comparison 5: Movement intervention versus any control, Outcome 1: Activities of daily living: persisting effects
5.3. Analysis.

Comparison 5: Movement intervention versus any control, Outcome 3: Neglect outcomes: persisting effects
5.5. Analysis.

Comparison 5: Movement intervention versus any control, Outcome 5: Adverse events
Comparison 6. NIBS versus any control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Activities of daily living: persisting effects | 4 | 92 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.35 [‐0.08, 0.77] |
| 6.1.1 CBS | 3 | 64 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.56 [0.04, 1.08] |
| 6.1.2 FIM | 1 | 28 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.83, 0.65] |
| 6.1.3 BI | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 6.2 Activities of daily living: immediate effects | 8 | 160 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.61 [0.27, 0.94] |
| 6.2.1 CBS | 6 | 120 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.55 [0.17, 0.93] |
| 6.2.2 FIM | 1 | 28 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.43 [‐0.33, 1.18] |
| 6.2.3 BI | 1 | 12 | Std. Mean Difference (IV, Fixed, 95% CI) | 2.59 [0.90, 4.29] |
| 6.3 Neglect outcomes: persisting effects | 5 | 102 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.77 [0.29, 1.24] |
| 6.3.1 Target cancellation | 4 | 75 | Std. Mean Difference (IV, Fixed, 95% CI) | 1.44 [0.83, 2.05] |
| 6.3.2 Line bisection | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 6.3.3 BIT behavioural subtest | 1 | 27 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐1.04, 0.48] |
| 6.4 Neglect outcomes: immediate effects | 13 | 244 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.75 [0.47, 1.04] |
| 6.4.1 Target cancellation | 10 | 174 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.72 [0.37, 1.06] |
| 6.4.2 Line bisection | 2 | 42 | Std. Mean Difference (IV, Fixed, 95% CI) | 2.18 [1.37, 2.98] |
| 6.4.3 BIT behavioural subtest | 1 | 28 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐1.02, 0.47] |
| 6.5 Adverse events | 0 | 0 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
6.5. Analysis.

Comparison 6: NIBS versus any control, Outcome 5: Adverse events
Comparison 7. Electrical stimulation versus any control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Activities of daily living: persisting effects | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 7.1.1 CBS | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 7.1.2 FIM | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 7.1.3 BI | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 7.2 Activities of daily living: immediate effects | 1 | 20 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.54 [‐1.44, 0.36] |
| 7.2.1 CBS | 1 | 20 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.54 [‐1.44, 0.36] |
| 7.2.2 FIM | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 7.2.3 BI | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 7.3 Neglect outcomes: persisting effects | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 7.3.1 Target cancellation | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 7.3.2 Line bisection | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 7.3.3 BIT behavioural subtest | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 7.4 Neglect outcomes: immediate effects | 2 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.99 [0.44, 1.53] |
| 7.4.1 Target cancellation | 2 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.99 [0.44, 1.53] |
| 7.4.2 Line bisection | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 7.4.3 BIT behavioural subtest | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
7.1. Analysis.

Comparison 7: Electrical stimulation versus any control, Outcome 1: Activities of daily living: persisting effects
7.2. Analysis.

Comparison 7: Electrical stimulation versus any control, Outcome 2: Activities of daily living: immediate effects
7.3. Analysis.

Comparison 7: Electrical stimulation versus any control, Outcome 3: Neglect outcomes: persisting effects
Comparison 8. Acupuncture versus any control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Activities of daily living: persisting effects | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 8.1.1 CBS | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 8.1.2 FIM | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 8.1.3 BI | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 8.2 Activities of daily living: immediate effects | 2 | 104 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.65 [0.26, 1.05] |
| 8.2.1 CBS | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 8.2.2 FIM | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 8.2.3 BI | 2 | 104 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.65 [0.26, 1.05] |
| 8.3 Neglect outcomes: persisting effects | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 8.3.1 Target cancellation | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 8.3.2 Line bisection | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 8.3.3 BIT‐behavioural subtest | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 8.4 Neglect outcomes: immediate effects | 2 | 104 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.57 [0.18, 0.97] |
| 8.4.1 Target cancellation | 1 | 64 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.52 [0.03, 1.02] |
| 8.4.2 Line bisection | 1 | 40 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.65 [0.01, 1.29] |
| 8.4.3 BIT behavioural subtest | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
8.1. Analysis.

Comparison 8: Acupuncture versus any control, Outcome 1: Activities of daily living: persisting effects
8.3. Analysis.

Comparison 8: Acupuncture versus any control, Outcome 3: Neglect outcomes: persisting effects
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aparicio‐Lopez 2016.
| Study characteristics | ||
| Methods | RCT Setting: Spain |
|
| Participants | 28 right‐hemisphere stroke patients Single‐treatment = 15, combined treatment = 13 Diagnosis of neglect: suggestive of VSN in the neuropsychological exploration protocol used to assess visuospatial attention Mean age, years: single treatment = 51, combined treatment = 46 Sex (men/women): single treatment = 9/3, combined treatment = 8/5 Days from stroke to admission: single treatment = 80, combined treatment = 85 Exclusion: severe language alteration, significant visual acuity impairment, pre‐morbid history of other neurological disease, psychiatric disorder, drug abuse | |
| Interventions | ST group followed a cognitive rehabilitation programme. Exercises included attention, memory, and executive function tasks. In all cases, adequate performance of assigned tasks required visual processing of stimuli homogeneously distributed across the screen. CT group carried out the same cognitive treatment as ST group, combined with RHEP. RHEP was implemented by using non‐prescription glasses specially made for the study. These glasses had a completely opaque right half‐field for each eye. This group wore these glasses during all cognitive treatment sessions | |
| Outcomes | For assessing visuospatial attention
|
|
| Notes | Breakdown of treatment by sex does not add up to total N | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A simple randomisation procedure was performed according to a computer‐generated random number table based on a uniform distribution (0, 1) |
| Allocation concealment (selection bias) | Low risk | The research assistant who generated the allocation scheme was not clinically involved in the study (neither in assessment nor in administration of treatment to patients) |
| Blinding of participants | High risk | Not possible to blind |
| Blinding of personnel | High risk | Not possible to blind |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Before the start of treatment and afterwards, the neuropsychological exploration protocol described in the Instruments section was administered. The researcher in charge of exploration was the same person responsible for planning and monitoring of treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes were reported equally |
| Selective reporting (reporting bias) | High risk | 10 primary outcomes |
| Other bias | Low risk | No baseline imbalance |
Bang 2015.
| Study characteristics | ||
| Methods | Pilot RCT Setting: Republic of Korea |
|
| Participants | 12 patients unilateral visuospatial neglect admitted to W. University Hospital tDCS + FT (combined) = 6, FT (control) = 6 Diagnosis of neglect: 15% deviation to the right from centre in line bisection test Mean age, years: combined = 66, control = 66 Sex (men/women): combined = 2/4, control = 2/4 Weeks from stroke to treatment: combined = 7, control = 7 Exclusion criteria: severe cognitive impairment rendering a person unable to understand instructions given by therapist, contraindications for intervention, unstable medical or neurological condition | |
| Interventions | Each participant performed a training programme consisting of 15 sessions lasting 50 minutes/d, 5 days a week, for 3 weeks Participants in the tDCS + feedback training group received tDCS for 20 minutes, then performed feedback training Both groups received feedback training for 30 minutes a day, 5 times a week, for 3 weeks. Feedback training used a vertical mirror held parallel to the sagittal plane to provide visual feedback on participants’ neglected side body. Participants were asked to look at the centre of the mirror, so they could see the reflection of visual input coming from the left side of the body | |
| Outcomes |
Measured immediately post treatment |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “They were randomly divided into two groups” |
| Allocation concealment (selection bias) | Unclear risk | “They were randomly divided into two groups” |
| Blinding of participants | High risk | No attempt at blinding described |
| Blinding of personnel | High risk | No attempt at blinding described |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No attempt at blinding described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants completed the entire study |
| Selective reporting (reporting bias) | Low risk | No suggestion of this |
| Other bias | Low risk | No baseline imbalance |
Cazzoli 2012.
| Study characteristics | ||
| Methods | Hybrid 3‐arm design. Here, combining first 2 arms “cTBS then sham” and “sham then cTBS” to create 2‐arm parallel design without cross‐over Setting: Switzerland, neurorehabilitation clinic | |
| Participants | 24 first‐stroke patients with left‐sided neglect and normal or corrected‐to‐normal vision cTBS‐sham = 16, control = 8 Diagnosis of neglect: deficits in at least 2 out of 3 classes of paper‐pencil tests Sex (all patients): 17 men, 7 women Mean age (all patients), years = 58 Stroke type: 14 ischaemic, 10 haemorrhagic Mean (SE) between stroke and treatment = 27 (4.4) days Exclusion criteria: history of epilepsy, prior head trauma, drug and alcohol abuse, major psychiatric disorder | |
| Interventions | Continuous TBS was applied by means of a MagPro X100 stimulator 60 mm outer radius (Magnetic Coil Transducer MC‐125). Continuous TBS was delivered with the same protocol described previously (Nyffeler et al, 2008, 2009; Cazzoli et al, 2009a, b). In brief, the continuous TBS protocol comprised 801 pulses, delivered in a continuous train and consisting of 267 bursts. Each burst contained 3 pulses at 30 Hz, repeated at 6 Hz. The total duration of 1 single, continuous TBS train was 44 seconds. Overall, 8 continuous TBS trains were applied over 2 days. Four continuous TBS trains were applied on Day 1 (2 continuous TBS trains with an interval of 15 minutes, third and fourth trains 60 and 75 minutes after first continuous TBS train, respectively; see Nyffeler et al, 2009), and 4 continuous TBS trains on Day 2 (same time intervals as for Day 1). Continuous TBS was applied over P3, according to the International 10–20 EEG System. This site overlies the posterior parietal cortex in proximity of the intraparietal sulcus (Hilgetag et al, 2001). The coil was held tangentially to the scalp, with the handle pointing posteriorly, the current flowing clockwise as viewed from above. Patients were asked to close their eyes during continuous TBS application. Continuous TBS was delivered at 100% of patients’ individual resting motor threshold. Sham was applied with the same protocol as described above, except for use of a sham coil (Magnetic Coil Transducer MC‐P‐B70) Control group received treatment as usual |
|
| Outcomes |
Measured immediately post treatment |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “were randomly allocated”. Split 16:8 could be lucky but suggests structure |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants | High risk | Blinding only within groups combined here |
| Blinding of personnel | High risk | Not clear whether personnel blinded within combined groups, but not applicable to this combined comparison |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessment by “four independent raters who were responsible for the care of each particular patient”. Unclear how they could have been blinded for this combined comparison |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | “All patients included completed the study protocol…all patients were assessed with all tests”, with limited exceptions |
| Selective reporting (reporting bias) | Low risk | All reported with equal (low) detail |
| Other bias | Low risk | No evidence of this |
Cha 2016.
| Study characteristics | ||
| Methods | 2‐group parallel Setting: South Korea, neurophysiotherapy outpatient clinic | |
| Participants | 30 stroke patients with
rTMS = 15, control = 15 Sex (women/men): rTMS = 8/7, control = 6/9 Age, mean (SD), years: rTMS = 64 (12), control = 63 (12) Time from stroke to treatment, mean (SD): rTMS = 4.1 (1.1), control = 3.9 (0.8) Neglect severity pre‐treatment, using LBT mean (SD): rTMS = 35.9 (8.1), control = 38.2 (4.7) |
|
| Interventions | Participants in the experimental group received rTMS and conventional rehabilitation therapy for a total of 50 minutes (rTMS: 20 minutes, conventional rehabilitation therapy: 30 minutes) per day, with a 10‐minute rest period halfway through the session. Participants in the experimental group received training 5 days per week for 4 weeks. Conventional rehabilitation therapy, consisting of neurodevelopmental facilitation techniques, was administered by therapists blinded to the study protocol and to participants’ assignment to groups. The objectives of stroke rehabilitation were to improve patients’ functional abilities, such as dressing, transfer, ambulation, and balance, and to provide education to caregivers, so as to help patients achieve earlier and/or greater independence in activities of daily living Participants in the control group received sham therapy and conventional rehabilitation therapy for a total of 50 minutes (sham therapy: 20 minutes, conventional rehabilitation therapy: 30 minutes) per day on the same day |
|
| Outcomes |
Measured immediately post treatment |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Assuming tombola system |
| Allocation concealment (selection bias) | High risk | No oversight of selection order |
| Blinding of participants | Low risk | Sham treatment |
| Blinding of personnel | High risk | Physician aware of allocation |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Separate physicians for treatment and assessment but unclear how possible to monitor success of ‘blind’ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | ADL not recorded |
| Other bias | Low risk | No evidence of this |
Cherney 2002.
| Study characteristics | ||
| Methods | RCT: no further information provided Setting: USA | |
| Participants | 4 right hemisphere stroke survivors with clinical evidence of neglect at least 6 months post onset Experimental: n = 2, control: n = 2 Mean age (SD), years: experimental = 69.5 (23.3), control = 62.0 (5.7) Sex (men): experimental = 2, control = 1 Side of damage (RBD): experimental = 2, control = 2 Mean months post onset (SD): experimental = 16 (12.7), control = 7.5 (0.7) Inclusion: right‐handedness, right hemisphere stroke, persisting neglect after 6 months, spoke English as a primary language, passed pure tone audiometry in the better ear, corrected visual acuity sufficient to read newsprint | |
| Interventions | Visual scanning training, practising letter and word cancellation tasks (to address the assumed underlying impairment of selective visual attention) vs repetitive practice of a functional task: oral reading (to represent an approach commonly used in rehabilitation) Both groups received 20 sessions. Frequency of sessions is not known Both scanning and reading training included use of visual, verbal, and tactile cues to attend to the left. In both training conditions, task difficulty gradually increased if the participant achieved 90% success (scanning) or 100% success (reading). In reading training, the cues were gradually removed (NB: scanning is coded as 'experimental' in this review) | |
| Outcomes | Study collected 4 types of outcomes, pre‐training and post training
The latter task was to identify 5 names from a local telephone book; there was a time limit of 3 minutes per name. BIT was scored in 3 ways: conventional subtests; behavioural subtests; and total. It is assumed this was measured immediately post training For comparability with other studies, this review used only BIT behavioural subtests post training Measured immediately post treatment |
|
| Notes | Comparison of 2 treatments. Intended as a small preliminary study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Unclear risk | No details of randomisation provided. Paper states "randomly assigned" |
| Blinding of participants | High risk | Blinding not possible |
| Blinding of personnel | High risk | Blinding not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not stated ‐ unlikely to be blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None reported |
| Selective reporting (reporting bias) | Low risk | Outcomes reported consistently |
| Other bias | Low risk | No evidence of this |
Choi 2016.
| Study characteristics | ||
| Methods | 2‐group parallel design Setting: South Korea | |
| Participants | 38 first‐time, right hemisphere stroke
Robot = 20, control = 18
Age, mean (SD), years: robot = 60 (12.5), control = 63 (11.1)
Sex (women/men): robot = 8/12, control = 10/8
Type of stroke: robot = 13 ischaemic, 7 haemorrhagic; control = 12 ischaemic, 6 haemorrhagic
Time between stroke and treatment, mean (SD), days: robot = 37 (15.9), control = 38 (16.9)
Neglect diagnosis: when bisection deviated 5 mm or more to the right side in the line bisection test Exclusion criteria: past medical history of brain damage, stroke, and other neurological or neuropsychiatric disease. Also, those who could not undergo robot treatment or hemi‐spatial neglect tests due to severe cognitive impairment. Patients with below second‐grade left upper extremity muscle strength in a manual muscle test, those who had any visual field defect, those with a seriously declined sitting balance interfering with upper extremity rehabilitation robot treatment in a sitting position on a chair with a back and armrests |
|
| Interventions | The Neuro‐X system was used for robotic treatment of hemi‐spatial neglect. During treatment, each patient sat on the right side of the robot, so the monitor was located to the left side of the patient. In this position, the patient could focus continuously on the left side. The robot treatment programme was implemented through games that induce passive and active assistive exercises of the wrist, elbow, and shoulder joints; games consisted of 2 types of isometric exercises and 2 types of range of motion exercises. Isometric exercises comprised an archery game, which was programmed to hit apples appearing on left and right sides of the monitor without any determined order, and a goalkeeper game, which was programmed to block a ball randomly approaching bottom left and right sides of the monitor. Range of motion exercises were conducted in a passive or an active assistive mode and consisted of a dolphin circus game and a skateboard game. All game programmes prompted participants’ concentration through sound effects During robotic treatment, occupational therapists monitored patients for diligently following progression of the robot programmes, measured patients’ muscle strength before robotic programmes began, and helped patients when games had to be changed from time to time Control group received treatment as usual |
|
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “patients were randomly assigned” |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants | High risk | Blinding not possible |
| Blinding of personnel | High risk | Blinding not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | “therapists who did not participate first hand in the treatment”; not clear how possible to validate or prevent communication |
| Incomplete outcome data (attrition bias) All outcomes | High risk | > 20% attrition from controls. All dropout informative – either early discharge or medical decline. Baseline data not reported for these participants |
| Selective reporting (reporting bias) | Low risk | Outcomes presented equally |
| Other bias | Low risk | No evidence of this |
Choi 2019.
| Study characteristics | ||
| Methods | 3‐group parallel RCT Setting: hospital, South Korea | |
| Participants | Inclusion: individual with diagnosis of unilateral neglect from a medical doctor and number of lines neglected in Albert test > 70%; individual without brain lesions other than stroke; individual with less than 3 months since stroke; individual with Korean version of Mini‐Mental Status Examination (K‐MMSE) score ≥ 20, who can follow directions and does not have hearing or vision impairment
Age: mean, SD
Sex: 17 women, 13 men Hemisphere damaged: not specified Time since stroke: 1 to 3 months |
|
| Interventions | This study has 3 intervention groups
‐ Group A received 30 minutes of conventional occupational therapy, followed by FES application on upper limb on the affected side and PA treatment for 20 minutes, for a total of 50 minutes. Conventional occupational therapy was conducted for 30 minutes and included joint movement, task‐oriented training, and daily life activity training. Joint movement was conducted and included passive joint movement, active adjuvant joint movement, and active joint movement. Task‐oriented training considered functional level of patients and used tools to sequentially conduct activities such as cup‐stacking and skateboarding. Daily life activity training included using the restroom, eating a meal, performing personal hygiene activities, wearing and taking off clothes, and transferring to chair or bed. Participants wore prism glasses that deflect the axis of vision to the right by 15 degrees, with the proximal surface shaped like a triangle facing the left. For FES, a product from Microstim was used. One channel was used and was set to apply, in shifts, 10 seconds of rest and 10 seconds of stimulation. It was attached below the elbow on the affected side. Although an intensity of 20 Hz is normally recommended, the threshold for electrical stimulation is different for each participant. Therefore, it was set to contract muscles enough to produce sufficient finger and wrist movements ‐ Group B received 30 minutes of conventional occupational therapy, followed by PA on the upper limb on the affected side for 20 minutes, for a total of 50 minutes ‐ Group C received 30 minutes of conventional occupational therapy, followed by FES application for 20 minutes, for a total of 50 minutes |
|
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | No detail offered. Exactly 10 per group |
| Allocation concealment (selection bias) | High risk | No detail offered. Exactly 10 per group |
| Blinding of participants | High risk | Outcome group: all Blinding not possible |
| Blinding of personnel | High risk | Outcome group: all Blinding not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome group: all Blinding not possible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | No suggestion of this |
| Other bias | Low risk | Not obvious |
Cottam 1987.
| Study characteristics | ||
| Methods | 2‐group parallel RCT Setting: rehabilitation centre, USA | |
| Participants | 12 stroke rehabilitation inpatients with left hemi‐spatial neglect Experimental: n = 6, control = 6 Mean age, years: experimental = 66.2, control = 71.3 Sex (men/women): 7/5 Side of damage: all had right middle cerebral artery lesions Time post onset, mean, weeks: experimental = 6, control = 16.3 Inclusion: right‐handedness; visual acuity > 20/100 corrected on Snellen's; oriented in person, place, and time; evidence of left hemi‐spatial neglect on ≥ 3 of the tests used; either WAIS‐R VIQ > 80 or minimum scaled score = 8 on 4/6 verbal subtests; arm and leg able to propel wheelchair | |
| Interventions | 3‐phase intervention, each phase consisting of 5 half‐hour sessions per day
vs no information other than participants were inpatients at a rehabilitation facility and were assessed after same periods as experimental group |
|
| Outcomes | Study collected 3 types of outcomes:
Assessed pre‐intervention, after each phase (5 days), and at follow‐up 6 weeks post discharge from hospital This review used only cancellation data, immediate and persisting effects |
|
| Notes | Single‐letter cancellation outcome data are entered as left‐sided omissions (i.e. low score is better outcome) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | No detail given; exactly 6 per group |
| Allocation concealment (selection bias) | High risk | No detail given; exactly 6 per group |
| Blinding of participants | High risk | Blinding not possible |
| Blinding of personnel | High risk | Blinding not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not stated. Not mentioned so unlikely to be blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 control lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Comprehensive dissertation report with massive multiplicity. Apparently post‐hoc combinations of quintiles (far left, left, centre, right, far right) of areas on visual tasks |
| Other bias | Low risk | Nothing obvious |
Dolkun 2019.
| Study characteristics | ||
| Methods | RCT, 2‐group parallel Setting: outpatient department and hospital ward, China |
|
| Participants | Patients with left hemiplegia after first stroke who met diagnostic criteria for unilateral spatial neglect of stroke. Patients with first cerebral infarction with course of disease within 2 weeks to 3 months. Muscle strength of the affected hand was reduced to at least level 4 and > 48 hours. Motor function of upper limbs was restored at the time of enrolment, and muscle strength at proximal end of the upper limbs was > grade 1. Right‐handedness (according to Chinese handedness) Age: intervention = range 37 to 80, mean 61 ± 13; control = range 41 to 79, mean 63 ± 12 Sex: intervention = 23/9 men/women; control = 22/10 men/women Hemisphere damaged: right Time since stroke: 2 weeks to 3 months post stroke | |
| Interventions | Intervention group received acupuncture at specific points. Acupoints selection: Bai Hui, Feng Fu, Feng Chi, Xuan Zhong, Nie San Zhen. Operation: patient was in the supine position, and local skin was routinely disinfected. Acupuncture needles of 0.25 mm × 25 mm or 0.25 mm × 40 mm were used. After needle insertion at the acupoint Bai Hui, horizontal insertion subcutaneous 15~20 mm. Insert into Feng Fu to jaw direction slowly 15~25 mm. After inserting the needle at the acupoint Feng Chi, towards throat direction oblique insert 15~25 mm. Insert into Xuan Zhong straight 15~30 mm. Temporal Three Needles: acupoint 1, 2 cun above tip of ear; acupoint 2, 1 cun forward acupoint 1; acupoint 3, 1 cun backward acupunct 1; when the needle is inserted, the tip of the needle is downward at an angle of 15°~20° with the scalp, slowly twirling and piercing into 25~30 mm. After insertion into acupoints, the needle is twisted and is retained for 30 minutes after De Qi Control group received standard acupuncture. Both groups received acupuncture at 10:00 to 13:00 Beijing time, once a day, 5 times per course of treatment, for a total of 4 courses of treatment |
|
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Statistical software cited for sequence generation |
| Allocation concealment (selection bias) | Low risk | "Opaque craft envelopes with serial numbers” |
| Blinding of participants | High risk | No mention and not straightforward |
| Blinding of personnel | High risk | No mention and not straightforward |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention and not straightforward |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | Tables for all presented in equal detail |
| Other bias | Low risk | Nothing obvious |
Edmans 2000.
| Study characteristics | ||
| Methods | RCT Setting: UK | |
| Participants | 42 (see Notes) stroke patients with visual neglect from those with general perceptual problems admitted to an inpatient SU Experimental: n = 24, control: n = 18 Mean age (SD), years: experimental = 69.17 (11.35), control = 66.61 (14.5) Sex (men/women): experimental = 10/14, control = 8/10 Mean time post onset: 37 days Inclusion: a subset of those with neglect from those with general perceptual problems from consecutive admissions to a stroke unit trial. SU trial criteria were medically stable, able to transfer with maximum 2 nurses, no discharge date planned, able to tolerate 30‐minute treatments, able to carry out some independent ADL pre‐stroke | |
| Interventions | ToT approach to treat the 'cause of the perceptual problem'. Underlying assumption is that practising a perceptual task will treat the underlying impairment and if successful will improve performance of other tasks that depend on the skills. Personal communication suggests that cueing and feedback were used to teach participants to compensate vs FA to treat the 'symptom rather than the cause' and involved practising ADL tasks Both groups received 2.5 hours per week for 6 weeks in addition to standard OT (NB: ToT is coded as experimental in this review) | |
| Outcomes | The broader study of perceptual problems completed the following measures by different assessors immediately after the 6‐week treatment: an independent blinded assessor completed the BI, Edmans ADL Scale, and RPAB. This assessor completed the ADL scales following interviews with unblinded nursing staff. The unblinded ward OT also completed the BI and Edmans ADL Scale. An unblinded physiotherapist completed the RMA gross motor scale. Additionally, assessments by other clinical staff were analysed: speech and language therapists, psychologists, physiotherapists. For comparability with other studies, this review used only the RPAB letter cancellation subtest score (number correctly cancelled) and the blinded assessor's BI | |
| Notes | Personal communication supplied further data and clarification of methods. Study authors provided unpublished data on 42 neglect patients from a larger RCT of 80 left and right (35) hemisphere strokes with perceptual problems, who was themselves taken from the stroke unit admission arm (n = 158) of an RCT of stroke unit vs general medical care. No pre‐randomisation differences between groups, except that the ToT group was a little longer post stroke (40/33 days) than the FA group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables |
| Allocation concealment (selection bias) | Low risk | The researcher used random number tables to prepare sequentially numbered opaque sealed envelopes. The random number tables were then returned; due to the large number randomised (80 to the full perception trial), it was unlikely that the sequence would be remembered. The envelopes were opened only in the presence of a witness. Random number tables were used. Concealment was highly likely to have been achieved, although this could not be guaranteed |
| Blinding of participants | High risk | Blinding not possible |
| Blinding of personnel | High risk | Blinding not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Assessor blinded but required to discuss with ward staff |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "No patients withdrew from the study but one patient (in the functional approach group) died before completing his six weeks of perceptual treatment." Data from this patient are included in analyses |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported equally |
| Other bias | Low risk | No evidence of this |
Fanthome 1995.
| Study characteristics | ||
| Methods | RCT Setting: UK | |
| Participants | 18 (see Notes) RH stroke patients admitted to hospital Experimental: n = 9, control: n = 9 (The following data describe the 18 initial participants: see Notes) Mean age (SD), years: experimental = 66.3 (10.7), control = 71.1 (7.6) Sex (men/women): experimental = 6/3, control = 6/3 Time post onset (mean months): experimental = 1.0, control = 0.6 Inclusion: not blind, < 80 years of age, no history of dementia or psychiatric problems, not ill, right‐handedness, score > 6 on Abbreviated Mental Test, RH stroke, score < 130 on BIT | |
| Interventions | 4 weeks (2 hours 40 minutes per week) of feedback on eye movements (wearing specially adapted glasses with auditory signal) vs 4 weeks of no treatment | |
| Outcomes | Study collected 3 types of outcomes: eye movements, conventional BIT subtests, and behavioural BIT subtests, immediately post treatment (4 weeks) and 4 weeks later (8 weeks) For this review, we used the 4‐week single‐letter cancellation test (for immediate outcomes) and 8‐week BIT summary behavioural subtest scores (for persisting outcomes) | |
| Notes | Personal communication supplied group data on BIT subtests for all but 1 control participant at 4 weeks (missing data; therefore n = 18 ‐ 1) and the information that assessor was blinded to allocation. BIT behavioural data are for all 18 at 4 weeks but for only 13 at 8 weeks. 8 weeks = post start of treatment, i.e. 4‐week follow‐up post end of treatment Single‐letter cancellation data are for number cancelled, i.e. higher numbers indicate better outcomes Experimental and control groups appeared adequately matched on demographic and clinical data, although control group was slightly older than experimental group; no baseline BIT data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sealed opaque envelopes prepared from random number tables |
| Allocation concealment (selection bias) | High risk | Concealment of allocation cannot be guaranteed, as this was not done by a third party. The combination of a small sample size with no external randomisation meant there was potential risk to concealment |
| Blinding of participants | High risk | Impossible to blind |
| Blinding of personnel | High risk | Impossible to blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessor stated, although no detail given |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1 participant was recruited but was not included, as "he could not move his eyes to the fixation points". 1 participant from the control group was excluded, as he was discharged home outside the area of the hospital |
| Selective reporting (reporting bias) | Low risk | Outcomes were reported equally |
| Other bias | Low risk | Groups appeared similar at baseline, and no significant differences were found |
Ferreira 2011.
| Study characteristics | ||
| Methods | RCT Setting: Brazil | |
| Participants | 10 ischaemic, right cerebral hemisphere stroke > 3/12 duration Mental practice = 5, visual scanning = 5 Detection of neglect: score < 129 (out of 146) on BIT Sex (women/men): mental practice = 2/3, visual scanning = 3/2 Age (range), years: mental practice = 46 to 73, visual scanning = 62 to 80 Time between stroke and treatment, range, months: mental practice = 3 to 62, visual scanning = 4 to 132 Exclusion criteria: locomotor problems or ataxia interfering with task completion, dysphasia, Parkinson’s disease, dementia, any neurodegenerative condition | |
| Interventions | Group 1: visual scanning Group 2: mental practice | |
| Outcomes |
Intervention groups were assessed at end of intervention period and at 3 months |
|
| Notes | "Five patients not willing to participate in the experimental protocols were submitted to a follow‐up exam 2 months later and were included in a control group." We did not include this group in analysis because it was non‐randomised; data only from the 2 intervention groups are presented We used imputation to calculate post‐intervention scores using 3 of the 5 values provided in each group: minimum, median, maximum | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Ten patients were randomly allocated” |
| Allocation concealment (selection bias) | Low risk | Randomisation (information from study authors): "Concealed envelopes for every patient (0 or 1). Then patients as they were recruited/included and subsequently randomised by the same method" |
| Blinding of participants | High risk | Not possible |
| Blinding of personnel | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | States: "the evaluations were always done by a physical therapist not directly involved in patients’ treatment." However, correspondence with study authors confirms: "there were two therapists involved, each one directly responsible for a different treatment strategy (mental practice or visual scanning). For instance, whenever a patient was randomised to mental practice, treatment was done by one and assessments by the other therapist. Hence, the assessor was always the therapist who would not be involved in treatment but he always knew the treatment allocation" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All complete |
| Selective reporting (reporting bias) | High risk | Total FIM reported more briefly than ‘significant’ subscale (self‐care items) |
| Other bias | Low risk | Groups appeared similar at baseline, and no significant differences were found |
Fong 2007.
| Study characteristics | ||
| Methods | 3‐arm RCT Setting: rehabilitation hospital, Hong Kong | |
| Participants | 60 participants Experimental 1: n = 20; experimental 2: n = 20; control: n = 20 Number lost to follow‐up: immediate post treatment (Day 30) assessments on 19, 20, and 15, respectively Also lost 5, 0, and 3, respectively to follow‐up (Day 60), so final analysis of 14, 20, and 12 Adequacy of matching at baseline? yes: P values are reported for all demographics and for baseline data ‐ there are no significant differences Mean age, mean (SD): experimental 1 = 69.9 (11.0), experimental 2 = 69.9 (9.8), control = 73.8 (9.9) Sex (men/women): 34/20 Side of damage: all had right brain damage Time post onset, days (SD): experimental 1 = 12.1 (9.4), experimental 2 = 11.6 (5.1), control = 12.1 (7.1) Inclusion criteria: first or second unilateral right lesion stroke confirmed by imaging and examination, admitted to rehabilitation hospital, < 8 weeks since stroke onset, right‐handedness, left visual inattention or neglect diagnosed by < 51/54 on Star Cancelled of BIT and GCS = 15 at recruitment Exclusion criteria: severe aphasia, significantly impaired visual acuity, hemianopia Visual sensory deficit: hemianopia and visual acuity assessed (method of assessment not stated) | |
| Interventions | Experimental 1: voluntary trunk rotation
1 hour per day, 5 days per week for 30 days = 30 hours; OT present throughout
Each hour composed of 15 minutes ADL + 45 voluntary trunk rotations with setup equipment (supine, unsupported sitting, and standing frame) reaching with ipsilateral hand into contralateral space and therefore rotating upper body/trunk by 15 to 35 degrees from midline. Used setup apparatus (pegboard or shoulder arc). Voluntary or if necessary therapist‐provided verbal or motor prompting for 15 minutes Experimental 2: voluntary trunk rotation and half‐field eye‐patching Same amount and content as experimental group 1 but wearing half‐field eye‐patches to ipsilesional (right) hemi‐field wearing patches on plastic goggles (over own glasses if necessary) Control: same amount of time as experimental groups 1 and 2. Conventional OT for hemiplegia (15 minutes ADL + 45 minutes training upper extremity). No mention of any neglect‐specific treatment, implying treated as if had only hemiplegia For analysis, voluntary trunk rotation with half‐field eye‐patching was classed as the experimental condition, and control as the control condition Profession of outcome provider: OT |
|
| Outcomes | Used 3 (some with multiple subtests) at 2 follow‐up time points (Day 30 immediately post therapy + Day 60)
Did not measure serious adverse events; excluded anyone re‐hospitalised or with deteriorating health |
|
| Notes | "Recruitment hypothesis" target both spatial representation and motor intentional deficits of personal and peri‐personal space ‐ this is the voluntary rotation plus eye‐patches "Inexpensive and easily integrated into use in day‐to‐day rehabilitation" Lack of intention‐to‐treat analysis, no baseline data for those allocated, baseline data for those followed up suggests pre‐therapy differences described in 'Risk of bias' table below | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Patients were "allocated to different groups according to their orders of admission to the study" |
| Allocation concealment (selection bias) | High risk | Personal communication with study authors: "we didn't have concealment of allocation of participants from the person who was recruiting" |
| Blinding of participants | High risk | Not mentioned and not practicable |
| Blinding of personnel | High risk | "The investigators were not blinded to group membership, and were also responsible for the intervention as allocated by the data manager” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Two independent blinded assessors, who were blinded to group membership, were responsible for all repeated measures throughout the duration of the study" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Although reasons for post‐randomisation exclusions are stated, it would have been preferable if all participants had been included in intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Low risk | P values reported for all demographic and baseline data ‐ no significant differences |
Fong 2013.
| Study characteristics | ||
| Methods | Multi‐centre, randomised, sham‐controlled RCT Setting: rehabilitation hospitals, Hong Kong | |
| Participants | Stroke patients: (1) cerebral vascular disease diagnosed by computed tomography scan or magnetic resonance imaging in a medical report and compatible with unilateral hemispherical involvement; (2) evidence of unilateral neglect from neurological testing or Behavioural Inattention Test (BIT) conventional subtest score < 129; (3) right‐handedness; (4) within 8 weeks after stroke; (5) ability to understand verbal instructions and to follow 1‐step commands; (6) severe to moderate unilateral upper limb paresis, defined as levels 1 to 5 in the Functional Test for the Hemiplegic Upper Extremity (FTHUE) with the range of some beginning voluntary motion of the hemiplegic shoulder and elbow to beginning ability of the hand to combine components of strong mass flexion and strong mass extension patterns Age, years: intervention = 66.2 ± 14.8, control = 68.6 ± 10.6 Sex: men/women: intervention = 16 (84.2)/3 (15.8), control = 9 (56.2)/7 (43.8) Hemisphere damaged: right, basal ganglia, internal capsule, corona radiate, or other Time since stroke, mean and SD, days: intervention = 24.3 ± 18.5, control = 22.3 ± 12.0 | |
| Interventions | Experimental group wore a wristwatch device emitting vibration cue with actometer for 3 consecutive waking hours on weekdays for 3 weeks. In the experimental group, patients had to press the acknowledgement button on the device with their right hand as soon as possible after each cue. Patients were told to follow every sensory cue with customary consecutive movements of the hemiplegic arm. They were instructed to perform the movement consecutively 5 times after each sensory cue. Cues came at intervals of 5 minutes for 3 hours. There were 2 kinds of customary movements tailored for participants according to the severity of their arm impairment: patients in levels 3 to 5 of the FTHUE who had partial use of their shoulders or arms were instructed to flex or extend their elbows; those in levels 2 to 3 of the FTHUE who had some voluntary motion of the shoulder were told to flex or abduct their shoulders Control group wore a sham wristwatch device with actometer |
|
| Outcomes |
Outcomes were reported as follow‐up but only 3 weeks following end of intervention, and therefore not meeting our definition of ‘persisting’ for this review |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Computerised random number generators” |
| Allocation concealment (selection bias) | Low risk | “Allocation to treatment sequences [was] concealed from all investigators” |
| Blinding of participants | High risk | Sham clearly ineffective: lost 20% of controls and none from active group for “lost interest” |
| Blinding of personnel | High risk | Ineffective sham |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Ineffective sham |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Lost 45% of control group before follow‐up assessment |
| Selective reporting (reporting bias) | Low risk | Consistent reporting of key outcomes |
| Other bias | Low risk | Nothing obvious |
Fu 2017.
| Study characteristics | ||
| Methods | RCT Setting: Korea, inpatient rehabilitation unit | |
| Participants | 13 right‐handed patients who had a first‐ever stroke in the right hemisphere and VSN with normal or corrected‐to‐normal vision rTMS = 7, control = 6 Diagnosis of neglect: average rightward bias of 12% Age, years: intervention = 60.17 ± 14.05, control = 62.00 ± 9.78 Sex: 3 women Time post stroke, days: intervention = 41.83 ± 20.56, control = 36.17 ± 17.50 | |
| Interventions | cTBS group received continuous TBS with the coil placed tangentially to the scalp at P3 over the left posterior parietal cortex (according to the 10–20 electrode position system of the American Electroencephalographic Association). Magnitude of the pulses was maintained at 80% resting motor threshold. On each day for 10 consecutive days, 4 sessions of stimulation were delivered, with an interval of 15 minutes between every 2 sessions. Each session lasted 40 seconds and contained 600 pulses delivered in 200 bursts at 5 Hz (theta rhythm). Each burst included 3 pulses delivered at 30 Hz | |
| Outcomes |
Measured immediately post treatment |
|
| Notes | Fu (2017) and Cao (2016) used the same participants but reported different outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail beyond “patients were randomly assigned” |
| Allocation concealment (selection bias) | Unclear risk | As above |
| Blinding of participants | Unclear risk | "Patients were blinded to the frequency of cTBS used" Clearly attempted with sham treatment but in direct contact with unblinded staff |
| Blinding of personnel | High risk | All/staff needed to know to set up |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome group: imaging Not clear when or how ‘regions of interest’ were identified. Looks more like hypothesis‐generating (exploratory) than hypothesis‐testing Outcome group: clinical Not clear how successful blinding attempt was or whether personnel administering tasks were the same as those involved in treatment, or otherwise had knowledge of group assignment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Cao 2016 contains additional participant omitted without explanation from Fu 2017 |
| Selective reporting (reporting bias) | High risk | Cao 2016 cites t‐tests for comparison at baseline but non‐parametric tests for comparison at outcome. Suggests absence of prospective or coherent analysis plan |
| Other bias | High risk | Massive multiplicity issues in imaging data, e.g. 78 hypothesis tests reported in each of Tables 1 and 2 (and these only in defined ‘regions of interest’) |
Goedert 2020.
| Study characteristics | ||
| Methods | RCT Setting: inpatient rehabilitation facility, USA | |
| Participants | Less than 60 days post stroke, first clinical stroke, unilateral right brain Event as confirmed by clinical computed tomography or magnetic resonance imaging, and BIT score at screening indicative of neglect (< 129) Age, years: 65.6 control, 61.8 prism Sex: 5 men/4 women = control, 4/4 = prism Hemisphere damaged: right Time since stroke: 9 to 50 days post stroke | |
| Interventions | Prism adaptation. Those randomised to the prism group received prism adaptation treatment once a day for 10 days (5 days per week for 2 weeks). Prism adaptation sessions were timed and each lasted approximately 15 to 20 minutes. Control group received usual care | |
| Outcomes |
Outcomes were measured up to 24 weeks post intervention. For comparability with other studies, we used outcomes at week 6 post intervention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information on process used despite detailed appendix |
| Allocation concealment (selection bias) | Unclear risk | Administrative (likely junior?) staff member tasked with list. Unblinded allocation and possibly post‐hoc evaluation “approximately half‐way through data collection” imply absence of proper quality control process |
| Blinding of participants | High risk | Not possible |
| Blinding of personnel | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not attempted |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Omission of 2 (11%) cases from prism arm, who did not (could not?) do more than 4 of planned 10 sessions |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Unclear risk |
|
Iwanski 2020.
| Study characteristics | ||
| Methods | Setting: Poland, inpatient or outpatient rehabilitation | |
| Participants | Inclusion criteria: (1) MRI or CT (in case of contraindications to MRI) confirming a first‐ever stroke in the right hemisphere; (2) time after onset 2 to 12 weeks (early subacute stroke; Bernhardt et al, 2017); (3) severe to moderate VSN recognised in a neuropsychological assessment; (4) age 18 to 75 years Age, mean ± SD, years: intervention = 65 ± 7.5, control = 64.6 ± 7.7 Sex (men/women): intervention: 11/3, control: 11/3 Days since stroke, mean ± SD: intervention = 49.2 ± 27, control = 35.4 ± 17 | |
| Interventions | Inhibiting stimulation parameters were chosen according to safety guidelines for rTMS (Rossi, Hallett, Rossini, & Pascual‐Leone, 2009). Stimulation was applied at 90% of the RMT at 1 Hz frequency. A total of 1800 pulses were generated during a 30‐minute session. Control group received sham stimulation performed with a sham coil that looked and sounded similar to real stimulation. To target the left angular gyrus, we positioned the coil on the scalp using the neuronavigation system and Talairach coordinates (x: –41; y: –66; z: 38; Cattaneo, Silvanto, Pascual‐Leone, & Battelli, 2009). During the long‐lasting rTMS, accuracy of the stimulation was constantly monitored by neuronavigation, while coil position error was recorded every 10 pulses. Deviation of up to 4 mm from the target was considered acceptable. For every participant, the percentage of pulses “in target” was estimated for each session Behavioral therapy of visuospatial neglect VSN therapy was focused mainly on visuospatial scanning with active and purposeful direction of sight to the left visual field in cognitive tasks performed in 2 computer programmes: RehaCom (HASOMED GmbH, Magdeburg, Germany) and CogniPlus (SCHUHFRIED GmbH, Modling, Austria). Additionally, paper‐and‐pencil tasks were used to improve visual scanning. Patients were asked to draw, copy, and analyse complex visual stimuli. Visual‐scanning training was guided by verbal instruction, contralesional cues (e.g. visual stimuli), and therapist feedback to orient attention to the neglected part of space |
|
| Outcomes |
Measured up to 3 months post intervention |
|
| Notes | Study authors reported median scores only for persisting neglect assessment. We imputed median for mean and used highest observed scores for SD | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Bespoke minimisation routine |
| Allocation concealment (selection bias) | Unclear risk | Insufficient detail; from correspondence with study author: "we allocated participants using Excel sheet. The file was protected by a password, which was known only for researchers (KP, ML), who were responsible for performing rTMS/sham sessions" |
| Blinding of participants | Unclear risk | Stated no previous experience and unaware of allocation but without evidence |
| Blinding of personnel | High risk | “Group assignments were known to the researchers who administered rTMS” |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome group: all “The neuropsychologist responsible for the cognitive assessment and leading therapy (SI) was blind to all patient treatment allocation” Assumes no communication within research team and success of participant blinding. Communication with study author reveals the following: "the neuropsychologist responsible for cognitive assessment and leading visuospatial scanning therapy was blind to rTMS/sham allocation. Participants also were not informed about the rTMS/sham allocation. Only two researchers knew the allocation because they administered the stimulation. The cooperation in the research team was close but due to blinding procedure information of allocation of the participants was known only form researchers who perform rTMS/sham procedure" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 1 loss to follow‐up (death) |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes identified |
| Other bias | High risk | Data‐driven analyses seemingly according to misunderstanding of ‘non‐significant’ and required assumptions for methods |
Kalra 1997.
| Study characteristics | ||
| Methods | RCT Setting: UK | |
| Participants | 50 (see Notes) stroke patients with visual neglect admitted to an SU The following data are for the 47 surviving patients: Experimental: n = 24, control: n = 23 Mean age (SD), years: experimental = 78 (9), control = 76 (10) Sex (male): experimental = 11, control = 9 Side of damage (RBD): experimental = 16, control = 17 Median time post onset, days (range): 6 (2 to 14) Inclusion: infarcts; partial anterior circulation, known to be sensitive to rehabilitation on basis of impairment of power, balance, proprioception, and cognition at 1 to 2 weeks after stroke Exclusion: TIAs, reversible neurological deficits, hemianopsia, severe dysphasia | |
| Interventions | Spatio‐motor cueing based on 'attentional‐motor integration' model and early emphasis on restoration of function vs conventional therapy input concentrating on restoration of tone, movement pattern, and motor activity before addressing skilled functional activity | |
| Outcomes | Study collected 6 types of outcomes:
This review used only BI, RPAB letter cancellation subtest, and discharge home. All were analysed as immediate effects |
|
| Notes | Principle behind approach: movement of affected limb in the deficit hemi‐space led to summation of activation of affected receptive fields of 2 distinct but linked spatial systems for personal and extrapersonal space, resulting in improvement in attention skills and appreciation of spatial relationships on the affected side. Personal communication supplied further data and clarification of methods No differences between groups in demographic variables or initial impairment or disability including BI Outcome data for 47 of 50 stroke patients with visual neglect admitted to an SU: experimental: n = 24 (+ 1 died), control: n = 23 (+ 2 died). For the 'destination discharge' outcome, the total figure of 50 was used in this review, as deaths were entered as not going home | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Low risk | External randomisation, using random permuted block technique in groups of 10, allocated by telephone by clerical staff using computer‐generated random numbers |
| Blinding of participants | High risk | Not possible to blind |
| Blinding of personnel | High risk | Not possible to blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Independent observer |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 lost to follow‐up: 1 intervention and 2 control. All died, so low risk of bias |
| Selective reporting (reporting bias) | High risk | Selective reporting of multiple subtests on RPAB |
| Other bias | High risk | "Treatment of patients in each group was undertaken by different therapists of the unit to prevent 'crossover' of treatment techniques”. Impossible to distinguish effect of therapy from effect of therapists. NB: recognised as preliminary study to inform design rather than to answer questions |
Karner 2019.
| Study characteristics | ||
| Methods | RCT Setting: rehabilitation hospital, Germany | |
| Participants | Minimum age of 60 years and diagnosis of first stroke of the right hemisphere occurring within previous 3 months, with hemi‐neglect of the left side, ability to sit, no major cognitive impairment Age, years (SD): intervention = 74.21 (6.53), control = 73.34 (8.13) Sex (women/men): intervention = 10/11, control = 12/6 Hemisphere damaged: right Time since stroke, mean (SD), days: intervention = 49.24 (29.12), control = 55.17 (22.75) | |
| Interventions | Intervention group received treatment using a therapeutic stimulation robot. PARO is an interactive robot in the shape of a baby seal. Each treatment began with providing information to the patient. This was done verbally as well as by initial physical contact on the left upper arm: “I am now on the left side of your body, the side affected by your stroke” PARO was placed on the neglected side, so it was possible for the patient to see and grasp it. The task for the patient was focusing attention on the robot. As soon as the patient had fixed his or her attention on PARO, it was successively moved further to the neglected side Control group was classified as attention control, with the researcher giving physical contact to the patient on the arm with verbal information as per the intervention. A book was also given for the patient to see and grasp. The patient was then read aloud from the book |
|
| Outcomes |
Participants were followed up for 2 weeks post intervention; therefore this does not meet our definition of 'persisting' effects of the intervention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Unclear risk | Recruitment of study participants and assignment to study groups were carried out by the researcher |
| Blinding of participants | High risk | Not possible to blind |
| Blinding of personnel | High risk | Not possible to blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Attempted blinding of neuropsychologist for neglect measures and others for ADL |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost 8 (17%), but reasons given and not markedly different between groups |
| Selective reporting (reporting bias) | Low risk | Outcomes reported in adequate detail |
| Other bias | Low risk | Nothing obvious |
Katz 2005.
| Study characteristics | ||
| Methods | Parallel control trial Setting: rehabilitation hospital, Israel. | |
| Participants | 19 patients with first right hemispheric stroke and persistent USN VR group = 11, control group = 8 Mean age, years: VR group = 62, control = 63 Sex (men/women): VR = 7/4, control = 5/3 Hemisphere: right Mean days between stroke and treatment: VR = 48, control = 36 | |
| Interventions | A street crossing virtual environment was programmed via Superscape’s 3D Webmaster and run on a desktop computer, with successively graded levels of difficulty that provide users with an opportunity to decide when it is safe to cross a virtual street. The level of difficulty was graded by the number and velocity of cars that approach the pedestrian cross‐walk, as well as the side (right or left) from which they approach, thus increasing attentional demands on the user. In addition other destructors were included such as commercial signs, blinking lights, etc. Virtual reality training protocol continued for 4 weeks, with 3 sessions per week, each of 45 minutes' duration, for a total of 9 hours. Timing of the control group computer scanning training protocol was identical. ?? Is this a control group or another active intervention? |
|
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | First 8 participants were randomly assigned to either VR training group (experimental) or computer visual scanning tasks group (control); remaining 3 participants were assigned to VR group to increase the number of participants who experienced the experimental condition |
| Allocation concealment (selection bias) | High risk | See above |
| Blinding of participants | High risk | No information about blinding provided |
| Blinding of personnel | High risk | No information about blinding provided |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No information about blinding provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | High risk | Multiple outcomes, none primary; no multiple testing adjustment. 1‐tailed test not justified |
Kerkhoff 2012.
| Study characteristics | ||
| Methods | RCT Setting: rehabilitation clinic, Germany | |
| Participants | 6 stroke patients with left‐sided visual and auditory neglect who were "enrolled in our clinic" Mean age, years: optokinetic stimulation (OKS) group = 62.3, SCAN group = 56.3 Inclusion criteria: single right‐hemispheric lesion due to stroke (infarction or haemorrhage); evidence of left‐sided visual neglect in at least 2 out of 4 screening tests, pathological rightward shift in ASMP | |
| Interventions | Group 1 ‐ OKS: repetitive leftward OKS stimulation with active pursuit eye movements. Participants were instructed to look at a computer screen (17") and make pursuit eye movements to the left (contralesional) side while looking at moving dot displays of 100 to 200 stimuli (mean velocity = 5° to 30°) Group 2 ‐ visual scanning training: participants viewed identical visual stimuli on the same computer monitor as the OKS group, but these patterns were always static. These participants were instructed to make systematic scanning eye movements to the left side and explore visual stimuli on the screen, just as in conventional visual scanning therapy Both groups received 20 treatment sessions of around 50 minutes, 5 sessions per week, 1 session per workday |
|
| Outcomes | Auditory neglect: ASMP Visual neglect: measured by the following 3 tests: number cancellation, horizontal line bisection, and paragraph reading All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | Data presented as single subjects in graph form. This paper contains 2 studies; study 1 was excluded, as it did not report outcomes of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Drawing lots, no possibility of validation |
| Allocation concealment (selection bias) | High risk | "The patients were randomly allocated to either an OKS (N = 3) or a SCAN (N = 3) treatment group by having a person neither involved in the study nor associated with the clinic draw concealed papers from an envelope containing 6 sheets of paper stating either 'OKS' or 'SCAN'" |
| Blinding of participants | High risk | Not possible to blind |
| Blinding of personnel | High risk | Not possible to blind |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not stated whether outcome assessor was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 6 participants recruited; none lost |
| Selective reporting (reporting bias) | Low risk | No suggestion of this |
| Other bias | Low risk | No suggestion of this |
Kerkhoff 2014.
| Study characteristics | ||
| Methods | RCT; 2‐group parallel Setting: Germany | |
| Participants | Single right‐hemisphere stroke, visual neglect in 2 screening tests (horizontal line bisection, number cancellation), and ability to execute daily neglect training for 30 minutes Age, mean, years (SD): intervention 1 = 64 (3), intervention 2 = 64 (3) Sex (men/women): intervention 1 = 7/5, intervention 2 = 8/4 Hemisphere damaged: right Time since stroke, mean (SD), days: intervention 1 = 37 (5), intervention 2 = 30 (4) | |
| Interventions | Participants received visual scanning training (VST) or smooth pursuit training (SPT). During VST, patients viewed stationary displays of stimuli implemented in the same software. Stimuli were geometrical objects (circles, triangles, squares, etc.), stars, letters, or digits (see Figure 1 for an example). The number of stimuli (5 to 60) and their size (1° to 2.5°), colour, and spatial arrangement were varied (systematic vs unordered, with/without line numbering, with/without subsidiary horizontal reference lines, with/without a red vertical “anchor line” on the leftmost side of the display). Patients were trained to scan systematically from left to right and from top to bottom, naming all objects, or counting certain stimuli. The therapist kept the patient’s head in a straight position for either treatment to promote eye instead of head movement. She watched continuously from the side whether the patient made smooth pursuit eye movements to the contralesional side (SPT) or saccadic eye movements (VST). If patients did not execute appropriate eye movements, instructions were repeated. If patients were tired, a short break (2 minutes) was given, adjusted to patients’ individual requirements During SPT, stimuli were random displays of 20 to 60 identically coloured and sized squares, moving horizontally from right to left at constant velocity, providing a coherent stimulus pattern (see Figure 1 for exemplary display). The colour, size (1° to 2.5°), and velocity (3.1° to 12.6°/s) of the stimuli were varied from time to time. The patient was encouraged to conduct smooth pursuit eye movements, repeatedly following the stimulus pattern from right to left, without head movement |
|
| Outcomes |
Participants were followed up 2 weeks post intervention; therefore this does not meet our definition of 'persisting' effects of the intervention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | “Randomly allocated to SPT or VST (by a person not involved in the study who drew lots from a sealed envelope)” |
| Allocation concealment (selection bias) | High risk | See above. No validation possible |
| Blinding of participants | High risk | Not possible |
| Blinding of personnel | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Attempted assessor blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | Consistent reporting |
| Other bias | Low risk | Nothing obvious |
Kim 2011.
| Study characteristics | ||
| Methods | RCT Setting: rehabilitation department, South Korea | |
| Participants | Stroke patients who were diagnosed with unilateral spatial neglect VR group = 12, control = 12 Mean age, years: VR = 62, control = 67 Sex (men/women): VR = 9/3, control = 5/7 Mean days from stroke to treatment: VR = 23, control = 26 Exclusions: patients with severe cognitive impairment or aphasia who could not understand instructions given by therapists, patients with such severely damaged sitting balance that they could not sit down on a chair with a back and armrests, patients with problems in cervical movement due to orthopaedic impairment, patients who could not recognise objects on a computer screen due to severely damaged eyesight | |
| Interventions | Physical therapy, occupational therapy, and cognitive therapy of the same intensity and time were applied to all patients. In addition, 2 occupational therapists conducted treatment for unilateral spatial neglect. One therapist conducted conventional rehabilitation programmes for the control group, such as visual tracking, reading and writing, drawing and copying, and puzzles; the other conducted virtual reality treatment on the VR group. Such treatments were applied for 30 minutes a day, once a day, 5 days a week for 3 weeks. The VR system consists of a monitor, a video camera, computer‐recognising gloves, and virtual objects. The video camera recognises movements | |
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding of participants | High risk | Unlike other double‐blind assessments, guardians knew about treatment of their patients, which means this study was not completely double‐blind |
| Blinding of personnel | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "Those tests were conducted by a therapist who was not involved in the treatment and did not know the state of the patients" However, CBS was filled out by guardians under supervision of the therapist |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only "seven subjects in the control group and three subjects in the VR group accurately performed the line bisection test and were included in the analysis" |
| Selective reporting (reporting bias) | Low risk | Outcomes were reported with equal detail |
| Other bias | High risk | 9 women and 3 men in VR groups; differences not accounted for |
Kim 2013.
| Study characteristics | ||
| Methods | RCT Setting: Korea, hospital | |
| Participants | First‐time cerebral stroke in the cortical or subcortical area; right cerebral ischaemic or haemorrhagic stroke. Scored > 15% deviation to the right from centre in line bisection Age, years: intervention 1 = 68.6 ± 14.4, intervention 2 = 64.1 ± 10.3, control = 68.3 ± 6.5 Number of men: intervention 1 = 5, intervention 2 = 4, control = 6 Time since stroke, days: intervention 1 = 14.2 ± 4.7, intervention 2 = 14.3 ± 3.6, control = 16.4 ± 8.5 | |
| Interventions | A physiatrist performed rTMS using a Magstim Super Rapid Magnetic Stimulatora with a 70‐millimeter, air‐cooled coil in the shape of a figure 8. The coil was held with the handle posterior and oriented sagittally and positioned on the scalp according to the 10e20 system, which is an internationally recognised method to describe the relation between location of scalp electrodes and underlying areas of the cerebral cortex The rTMS stimulation site corresponded with position P3, which is localised over the left PPC, and position P4, which is localised over the right PPC. Patients were seated in a comfortable chair with foam earplugs. We determined the motor threshold of the right first dorsal interossei muscle as the stimulus intensity required to produce motor‐evoked potentials of more than 100 microvolt peak‐to‐peak amplitude in 3 of 5 consecutive trials. For low‐frequency rTMS, 1‐Hz stimulation at a 90% motor threshold was delivered over the left (non‐lesioned) P3 in 4 trains of 5‐minute duration, each separated by 1 minute. This resulted in a total stimulation period of 20 minutes and total delivery of 1200 pulses For high‐frequency rTMS, 10‐Hz stimulation at a 90% motor threshold was delivered over the right (lesioned) P4 in 20 trains of 5 seconds' duration, each separated by 55 seconds. This resulted in a total stimulation period of 20 minutes and total delivery of 1000 pulses |
|
| Outcomes |
Measured immediately post treatment |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants | Unclear risk | Outcome group: all Use of sham but no evaluation of success nor discussion of process to ensure blinding |
| Blinding of personnel | High risk | Not practical to blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | “All evaluations were performed by a single experienced occupational therapist who was blinded to the study” No discussion of process to ensure success |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 6 participants excluded from all results due to early discharge, which may plausibly be treatment related |
| Selective reporting (reporting bias) | Low risk | All outcomes reported in equal detail |
| Other bias | Unclear risk | Unclear |
Kim 2015.
| Study characteristics | ||
| Methods | RCT, parallel 2‐group Setting: Korea, hospital | |
| Participants | Patients with hemi‐spatial neglect among hospitalised patients with stroke Age, years: intervention 1 = 62.3 ± 11.2, intervention 2 = 66.7 ± 6.9 Men/women: intervention 1 = 10/9, intervention 2 = 5/10 Time since stroke, months: intervention 1 = 19.11 ± 12.39, intervention 2 = 15.73 ± 12.33 | |
| Interventions | Group 1 had low‐frequency rTMS only once. rTMS was conducted a total of 1200 times for 20 minutes at the frequency of 1 Hz in the left P3 side, based on International 10–20 EEG Electrode System with 90% intensity of resting motor threshold Group 2 had a total of 10 times of rTMS, 5 times a week, for 2 weeks. rTMS are per intervention group 1 |
|
| Outcomes |
Measured immediately post treatment |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “We randomly divided the patients into two groups” |
| Allocation concealment (selection bias) | Unclear risk | No mention |
| Blinding of participants | High risk | No indication of attempt to blind |
| Blinding of personnel | High risk | No indication of attempt to blind |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No indication of attempt to blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No indication of attrition |
| Selective reporting (reporting bias) | Low risk | Outcomes reported in equal detail |
| Other bias | Low risk | Nothing obvious |
Kim 2018.
| Study characteristics | ||
| Methods | RCT, 3‐group parallel Setting: Korea, 'patients receiving rehabilitation' | |
| Participants | Patients with left hemi‐spatial neglect due to first stroke, right hemisphere stroke, no cognitive decline, muscle strength > 2, no visual defect, sitting balance to perform intervention Age, years: intervention 1 = 70.3 ± 9.6, intervention 2 = 66.6 ± 12.2, intervention 3 = 62.5 ± 16.5 Men/women: intervention 1 = 5/5, intervention 2 = 5/5, intervention 3 = 5/5 Time post stroke, days: intervention 1 = 19.2 ± 13.4, intervention 2 = 24.5 ± 22.4, intervention 3 = 15.3 ± 9.8 | |
| Interventions | Intervention 1: rTMS therapy with a coil stimulator shaped like a figure 8 at diameter of 70 mm using MagPro (MagVenture Inc., Farum, Denmark). Session included 900 stimuli applied over contralesional posterior parietal cortex at an intensity of 95% motor thresholds and a frequency of 0.9 Hz Intervention 2: patients in the robot group received additional treatment for hemi‐spatial neglect using a rehabilitation robot (Neuro‐X; Apsun Inc., Seoul, Korea) for upper limbs. During robot therapy, patients sat on the right side of the robot with the robot’s monitor on their left side. Robot therapy programme was conducted through games that induced passive and active assistive range of motion of the wrist, elbow, and shoulder joints. These games consisted of 2 isometric exercises and 2 range of motion exercises. The 2 isometric exercises used wrist extension and wrist flexion, in which the default muscle strength for wrist extension and wrist flexion were measured quantitatively before the start of the game, so the game was continued only when a force exceeding a certain level of strength was applied Intervention 3: rTMS + upper limb robot |
|
| Outcomes |
Measured before and after intervention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation table |
| Allocation concealment (selection bias) | High risk | No mention of concealment, but blocks of size 3 highly predictable |
| Blinding of participants | High risk | No sham for either intervention |
| Blinding of personnel | High risk | No sham for either intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | “Occupational therapist who did not directly participate in the treatment”, but patient clearly aware |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Early discharges excluded from analyses |
| Selective reporting (reporting bias) | Low risk | Outcomes reported in equal detail |
| Other bias | Low risk | Nothing obvious |
Koch 2012.
| Study characteristics | ||
| Methods | RCT, 2‐group parallel Setting: Italy, neurorehabilitation unit | |
| Participants | Right hemisphere subacute ischaemic stroke and affected by hemi‐spatial neglect, as confirmed by radiological (CT or MRI) and clinical examination | |
| Interventions | A MagStim Super Rapid magnetic stimulator (Magstim Company, Whitland, Wales, UK), connected with a figure‐of eight coil with a diameter of 70 mm, was used to deliver cTBS. In every session; 3‐pulse bursts at 50 Hz repeated every 200 msec for 40 s were delivered at 80% of the active motor threshold (AMT) over the left PPC (600 pulses). We used a neuronavigation system (Softaxic, E.M.S., Bologna, Italy) to precisely position the coil over the left PPC, using individual anatomical MRI; this technique has been described in detail previously. Individual coordinates of each stimulation site were normalised a posteriori into the Montreal Neurological Institute (MNI) coordinate system and averaged. To target the left PPC, the coil was positioned in the angular gyrus (AG) in the posterior portion of the inferior parietal lobule (IPL), close to a posterior part of the adjoining intraparietal sulcus (cIPS). The centre of the coil was positioned tangentially to the skull, with the handle pointing downward and slightly posteriorly. Sham stimulation was delivered with the coil angled at 90°, with only the edge of the coil resting on the scalp. Stimulus intensity, expressed as a percentage of maximum stimulator output, was set at 80% AMT for the FDI, inducing the same acoustic sensation as for real TBS Control: sham cTBS |
|
| Outcomes |
Assessed pre‐intervention and post intervention and at 2‐week follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly assigned to real or sham” |
| Allocation concealment (selection bias) | Unclear risk | "Patients were randomly assigned to real or sham” |
| Blinding of participants | Low risk | “Patients were unaware of their group assignment; all were only told that they had been enrolled in rehabilitation treatment for their spatial attention deficits” |
| Blinding of personnel | High risk | Inevitable that providers were aware |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | “Therapists were also blinded in respect to the type of intervention” “Evaluation of BIT was performed by blinded raters” Unclear scope for contact between study personnel, therapists, and raters. And no discussion of effectiveness of blinding effort |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One post‐randomisation exclusion from each group due to protocol violation. Unlikely to affect clear results |
| Selective reporting (reporting bias) | Low risk | Several apparently data‐driven analyses, but all outcome component scores tabulated |
| Other bias | Low risk | Nothing obvious |
Kutlay 2018.
| Study characteristics | ||
| Methods | Assessor‐blinded randomised controlled clinical study. Setting: inpatient rehabilitation, Turkey |
|
| Participants | “stroke patients with UN who were admitted for rehabilitation in the Department of Physical Medicine and Rehabilitation, Ankara University Medical Faculty, from February 2013 to December 2014 were screened” Age, years: intervention = 62 (54.5 to 67), control = 63 (54 to 70.75) Sex: intervention = 15/10 (m/f), control = 17/11 Hemisphere damaged: right Time since stroke, months: intervention = 4 (2 to 10.5), control = 3 (2 to 4.75) |
|
| Interventions | The Kinesthetic Ability Trainer (KAT; LLC, Vista, CA, USA) is a balance and training system that provides visual feedback to control body posture on a movable platform. The KAT system works by altering the stability of a movable platform, on which an individual stands, and/or by varying the degree to which the individual alters his or her base of support by shifting weight in response to visual feedback provided by a personal computer, in addition to the therapist’s guidance, encouragement, and feedback. Participants in the intervention group received a 4‐week balance training programme 5 times per week with session duration of 20 to 30 minutes. Control participants received usual care | |
| Outcomes | 1. Full BIT 2. FIM All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An independent research assistant (who was unaware of the baseline data) carried out the randomisation procedure with a block size of 4 using computer software |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes were used to conceal the randomisation sequence |
| Blinding of participants | High risk | Impossible to blind |
| Blinding of personnel | High risk | Impossible to blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The rehabilitation team evaluating patients was blinded to group assignment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | During the study, 4 patients from the control group and 7 from the KAT group dropped out for several reasons. A final total of 28 patients in the control group and 25 in the KAT group completed the study |
| Selective reporting (reporting bias) | Low risk | Outcomes were reported with equal detail |
| Other bias | Low risk | Nothing obvious |
Learmonth 2020.
| Study characteristics | ||
| Methods | Prospective randomised open blinded endpoint (PROBE) trial; feasibility study Setting: Scotland, inpatient hospital, expanded recruitment to outpatients due to low recruitment | |
| Participants | Participants were eligible if they were aged 18 years or older; had a clinical diagnosis of stroke with brain imaging compatible with right hemisphere intracerebral haemorrhage or ischaemic stroke; had a modified Rankin score estimated as 0 to 3; and had persistent hemi‐spatial neglect ≥ 4 weeks post stroke Age, median, years: intervention 1 = 66, intervention 2 = 67, intervention 3 = 70, control = 62 Men/women: intervention 1 = 3/3, intervention 2 = 4/2, intervention 3 = 2/4, control = 4/2 Time post stroke, median, days: intervention 1 = 282, intervention 2 = 47, intervention 3 = 60, control = 268 | |
| Interventions | Intervention 1: transcranial direct current stimulation (tDCS) Intervention 2: behavioural training. Participants were seated at a table in front of a mat measuring 140 × 30 cm. Nine black squares labelled A through I were positioned on the left side of the mat, and were used as starting positions for each trial. Three wooden rods of different lengths (50, 75, and 100 cm ‐ all 1.1 cm in diameter) were placed in front of the participant. At the start of each trial, participants were asked to pick up one of the rods (short, medium, or long) and place the left end of the rod at 1 of the 9 starting positions on the mat. They then were instructed to pick up the rod at its midpoint with their right hand using a pincer grip, and to assess whether the rod was balanced at its midpoint. If they felt that it was unbalanced, they were instructed to place the rod back down at its starting position and to adjust their grip (usually leftwards) until the rod was balanced. Training was intended for 15 min and involved roughly 54 trials Intervention 3: both tDCS and behavioural training were administered simultaneously. Behavioural training began as soon as the tDCS equipment had fully ramped up to 1 mA Control: control training was identical to behavioural training, but participants were instructed to lift up the rod at its rightmost end rather than at its midpoint. They thus performed a motor task, yet did not receive corrective proprioceptive nor visual feedback on their actions |
|
| Outcomes |
Assessed pre‐intervention and post intervention and at 6‐month follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Conducted by independent trials unit (Robertson Centre) |
| Allocation concealment (selection bias) | Low risk | Conducted by independent trials unit (Robertson Centre) |
| Blinding of participants | High risk | “Participants and the Research Assistant delivering the treatment were aware of the group allocation” |
| Blinding of personnel | High risk | “Participants and the Research Assistant delivering the treatment were aware of the group allocation” |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | “Allocations were concealed from outcome assessors. This concealment was maintained throughout the trial” No further detail on or discussion of success |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 10 (42%) lost before follow‐up |
| Selective reporting (reporting bias) | Low risk | All data reported |
| Other bias | Low risk | Nothing obvious |
Li 2017.
| Study characteristics | ||
| Methods | RCT Setting: China, rehabilitation unit | |
| Participants | (1) People between 40 and 70 years old; (2) course of disease 2 to 4 months; (3) for the first time, brain CT or MRI confirmed that lesion was located in the right hemisphere of the brain; (4) by line bisection test, line segment marking test, bell drawing test, plane graph copying test, and other unilateral space neglect scale and clinical examination to confirm the existence of left space neglect; (5) patients' condition is stable, clear, focused, and directional, and there are no obvious memory, emotional, or intellectual barriers. Patients understand the requirements of the examination and are able to cooperate; All are right‐handed, with no obvious visual impairment Age, years: intervention = 40 to 67 (53 ± 9), control = 40 to 69 (53 ± 8) Sex (men/women): intervention = 17/3, control = 18/2 Time post stroke, months: intervention = 2 to 4 (2.9 ± 0.6), control = 2 to 4 (2.9 ± 0.7) | |
| Interventions | Acupuncture on ”Xingshen Yisui Kaiqiao” acupoints Acupoint selection: Bai Hui, Si Shen Cong, Shen Ting, Ben Shen, Shen Men, Tong Li, Tai Xi, Da Zhong, Da Ling, Nei Guan. On the basis of the 8 acupoints of Bai Hui, Si Shen Cong, Shen Ting, Ben Shen, about 10 acupoints were alternately taken from upper and lower limbs on both sides every day. All acupoints were treated with 0.30 mm × 25 mm disposable acupuncture needles. Head acupoints were applied by the oblique needle shallow acupuncture method, and the needle body was inserted straightly. The needle was retained for 30 minutes Control group received treatment as usual |
|
| Outcomes |
Assessed pre‐intervention and post intervention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Prepared by statistics team |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, sealed opaque envelopes |
| Blinding of participants | High risk | No blinding |
| Blinding of personnel | High risk | Not practical |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessors; no info on success of process |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | Outcomes reported in equal detail |
| Other bias | Low risk | Nothing obvious |
Luukkainen‐Markkula 2009.
| Study characteristics | ||
| Methods | RCT, single site; comparing 2 active interventions Setting: Finland |
|
| Participants | 12 participants with left hemi‐spatial neglect due to a first single right hemisphere stroke occurring a maximum of 6 months previously Experimental 1: n = 6, experimental 2: n = 6 Number lost to follow‐up: none; however data for 1 person from each group for some measures and time points were missing There were baseline differences in the CBS OT score ‐ arm activation group, mean 9.4 (SD 2.3) and visual scanning group, mean 13.5 (SD 7.8) ‐ based on data from 10 participants Age, years, mean (SD): experimental 1 = 59.5 (8.4), experimental 2 = 57.8 (11.8) Sex (male/female): experimental 1 = 3/3, experimental 2 = 2/4 Side of damage: right hemisphere stroke Method of diagnosing stroke: CT or MRI; neurologist and radiologist Method of diagnosing neglect: For acute phase (< 3 months post stroke) – at least 2 of the following: score ≤ 100 on BIT conventional subtests (BIT C); ≥ 2 of the BIT subtests under the cutoff point; or CBS OT score of 10 to 30 points For subacute phase (3 to 6 months post stroke) – at least 2 of the following: score ≤ 129 on BIT C subtests; ≥ 1 BIT C subtest under the cutoff; or CBS OT score ≥ 2 Time post onset, days: experimental 1 = 81.0 (64.6), experimental 2 = 95.5 (63.2) Inclusion criteria: diagnosis of single right hemisphere stroke within 6 months, right‐handed with no other co‐existing disease causing cognitive decline. Visual sensory deficit (method of assessment): experimental 1 = 1 with complete hemianopia, experimental 2 = 3 with complete hemianopia |
|
| Interventions | Arm activation training 20 to 30 hours of left arm activation – amount determined by observation of subjective needs of individuals Content determined by individual WMFT performance: 1 patient had constraint‐induced movement therapy (intensive exercise of affected arm while unaffected arm was restrained with a sling). 5 patients without sufficient left arm mobility had modified arm activation therapy, all with left arm in left space and right arm resting on right side (50% passive arm activation FES with a glove/or for spasticity stretching by a therapist + 50% voluntary shoulder motor training in push‐pull equipment in left hemi‐space) vs Visual scanning training: 10 hours traditional visual scanning training – aimed for 1 hour, 4×/week of visual scanning combined with 2 daily physiotherapy sessions + 1 hour per day of OT/group therapy achieved for 1 hour, 5×/week during 3 weeks Content: 3 procedures (half‐hour on 1, then half‐hour on 2 or 3)
Profession of intervention provider: arm‐activation ‐ constraint‐induced movement therapist Visual scanning ‐ clinical psychologist |
|
| Outcomes | Several outcomes were measured. These are given along with details (where provided) of the time point of measurement, and the profession of the person performing the measure
Also reported 1 person with recurrent stroke |
|
| Notes | "Sufficient amount of active or passive left arm activation in the left half space combined with simultaneous visual tasks or while doing daily activities is likely to ameliorate visual and behavioural neglect" Confounding factors may be due to baseline imbalance on CBS or to Beck Depression Inventory (effect on engagement in therapy) and multiple assessments Group 1 received a lot more arm activation than Group 2 during visual scanning training. Group 2 received more OT and group therapy than group 1. Correspondence with study author states this difference is to keep total hours of therapy received by participants in each group comparable |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Personal communication with study author: "the method of randomization was carried out as follows: A clerk of the rehabilitation ward offered a pair of brown envelopes to an entering patient. One envelope included the AA group and the other envelope contained the VS group. The first patient picked one of the envelopes and the following patient entering the study was randomized automatically into the other group. This arrangement of paired randomization was necessary for the resources of the ward." Consequently allocation of the second patient would be known to researchers |
| Allocation concealment (selection bias) | High risk | See above |
| Blinding of participants | High risk | Not possible |
| Blinding of personnel | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Of the 13 assessments, a number were carried out by those who did not participate in rehabilitation. These outcome measures were visual and behavioural neglect, BIT C, and CBS. However, although assessments were carried out by someone who did not participate in rehabilitation, these people were not blinded to treatment group |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data for 1 person from each group for some measures and time points were missing |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | High risk | There were baseline differences between groups, with CBS and Beck Depression Inventory scores appearing higher and more variable for visual scanning group. There was no adjustment for baseline differences for CBS |
Machner 2012.
| Study characteristics | ||
| Methods | RCT Setting: hospital, Germany | |
| Participants | 23 patients with left spatial neglect after acute (< 14 days) right hemisphere stroke Experimental = 11, control = 10 Diagnosis of neglect: neglect if patients showed pathological performance on ≥ 2 tests of a neuropsychological test battery consisting of the following paper–pencil tests: line bisection, star cancellation, text reading, Bells cancellation, and Ogden figure copying task Age, years, mean (SD): experimental = 69 (3), control = 39 (3) Sex (men/women): experimental = 8/3, control = 6/4 Days between stroke and treatment, mean (SD): experimental = 3 (1), control = 5 (1) ADL before treatment CBS, mean (SD): experimental = 17 (3), control = 18 (3) Exclusion: previous stroke, neurodegenerative disease, inability to give informed consent | |
| Interventions | Patients in the treatment group received HEPOKS in addition to usual stroke care (physio, speech, and occupational therapy), whereas patients in the control group had usual care only. HEP was applied by spectacle frames containing non‐corrective lenses for which the right half was patched with dark non‐translucent tape. Participants were instructed to wear the glasses all day for 7 days and to remove them only for the OKS treatment sessions. Investigators, care providers, and patients’ relatives regularly checked on correct use of the glasses. Daily OKS sessions (15 minutes each) were applied at the bedside. Seventy coloured geometric objects were coherently moving on an 18.4″ notebook monitor from right to left at varying speeds (8° to 12°/s) | |
| Outcomes | 2 primary outcome measures: (1) mean performance (accuracy) on neuropsychological test battery, (2) neglect‐related functional disability measured by Catherine Bergego Scale Secondary outcome measures were Barthel Index, modified Rankin scale, National Institutes of Health Stroke Scale Participants were assessed at 3 time points (Figure 1): baseline (Day 1), post treatment (Day 8), and follow‐up (Day 30) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The principal investigator sent a fax including identification parameters of the eligible patient (no name and initials) to the IMBS. A staff member at the IMBS with no clinical involvement in the trial randomised the patient online using a computerised permuted block technique with varying block size and assigned the unique patient identification number (PID). The randomisation result and the PID were documented on the fax and sent back to the investigator |
| Allocation concealment (selection bias) | Low risk | See above |
| Blinding of participants | High risk | Due to the nature of a cognitive intervention trial, both investigators and patients were aware (not “blind”) of the allocated arm throughout the study |
| Blinding of personnel | High risk | See above |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Unclear if blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear |
| Selective reporting (reporting bias) | Low risk | Secondary outcomes are in data supplement |
| Other bias | Unclear risk | At baseline, study groups did not differ significantly in demographic, clinical, and neuropsychological characteristics, except for 1 paper–pencil subtest (Table). Lesion overlap analyses are provided in Figure II in the online‐only Data Supplement |
Mancuso 2012.
| Study characteristics | ||
| Methods | Setting: outpatient, Italy | |
| Participants | Outpatients with left visual neglect resulting from right hemisphere vascular lesion. All patients were right‐handed, had left hemiplegia or hemiparesis from ischaemic or haemorrhagic brain injury. All patients were selected in accordance with tests for neglect; those who had abnormal scores on ≥ 2 tests were enrolled. No patient had visual field deficits, which could preclude the proper performance of tests or exercises, or severe symptoms of cognitive impairment (MMSE score ≥ 21 of total 28, excluding tests in reading and drawing) Age, years: intervention = 70.2 (8.8), control = 62.3 (13.1) Sex (men/women): intervention = 7/6, control = 4/5 Hemisphere damaged: right Mean time since stroke (SD), days: intervention = 180.153 (301.485), control = 129.00 (132.799) | |
| Interventions | Intervention group received prism adaptation training with 5 rehabilitation sessions, lasting about 30 minutes each, from Monday to Friday for 1 week in the morning, by the same investigator, at each centre. Control group received the same treatment with neutral lenses | |
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After enrollment, patients were randomized by pilot center and assigned to two different groups 'A' or 'B'” |
| Allocation concealment (selection bias) | High risk | Randomisation done by ‘pilot centre’, suggesting high risk |
| Blinding of participants | High risk | In no case was specific information on the lens applied provided to the patient. Frames used for prismatic lenses were identical to those for neutral lenses. Nevertheless, patients likely to be able to tell that glasses are not doing anything. No assessment of success of 'blinding' attempt |
| Blinding of personnel | High risk | No attempt at blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessor not blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | “Of the 29 patients enrolled, there were 6 dropouts caused by deterioration in health, and one outlier, that is a patient who presented very different statistical characteristics to the rest of the group.” Excluding outlier without justification |
| Selective reporting (reporting bias) | Low risk | Similar reporting detail for all mentioned outcomes |
| Other bias | Low risk | No evidence of this |
Mizuno 2011.
| Study characteristics | ||
| Methods | RCT; multi‐centre, double‐blind Setting: rehabilitation departments, Japan | |
| Participants | 38 participants (444 screened) Experimental group (prisms): n = 20; control group: n = 18 Recruited from rehabilitation departments from 8 hospitals in Japan Age, years, mean (SD): experimental = 66.0 (11.5), control = 66.6 (7.7) Time from stroke, days, mean (SD): experimental = 67.1 (18.4), control = 64.4 (20.9) Inclusion criteria: within 3 months of first‐ever right hemisphere stroke, 42 to 89 years old, neglect as assessed by BIT behavioural test Exclusion criteria: unable to sit in wheelchair, aphasia or cognitive impairment resulting in inability to understand task, inability to understand Japanese, impaired vision or hearing, impaired right upper limb, previous brain injury 34 participants completed intervention and follow‐up; 4 dropouts (1 control, 3 prisms) ‐ 2 stroke relapse, 1 refused, 1 with delirium 31 participants completed follow‐up BIT | |
| Interventions | 2 daily training sessions, lasting 20 minutes, 5 days per week, for 2 weeks, for a total of 20 sessions Training ‐ pointing at targets, whilst sitting at a table Experimental group: prisms (shifting visual field 12° to right, Fresnel lens). Pointing task ‐ 30 times without prisms; 90 times with; 60 times without Control group: neutral plastic glasses. Pointing task as for experimental group Routine stroke rehabilitation provided as usual | |
| Outcomes |
Outcomes were recorded at baseline, after the 2‐week intervention, and immediately before hospital discharge. We used immediate effects only for comparability with other studies |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly allocated to intervention or control group, with a computerised block randomisation scheme |
| Allocation concealment (selection bias) | Low risk | Computerised block randomisation, with pre‐stratification according to BIT behavioural test (dichotomised to ≥ 55 or < 55) and participating hospital. All data were sent to the central office at the Department of Preventive Medicine and Public Health, School of Medicine, Keio University, before allocation assignment |
| Blinding of participants | High risk | Prism lenses; sham control not convincing |
| Blinding of personnel | High risk | See above |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Outcome assessor was masked to treatment allocation and otherwise uninvolved in the participant's treatment"; no evidence of success of this though |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 3 missing in prism group, 1 in control group |
| Selective reporting (reporting bias) | High risk | SIAS reported less |
| Other bias | Low risk | None obvious |
Nyfeller 2019.
| Study characteristics | ||
| Methods | RCT Setting: Switzerland, neurorehabilitation centre |
|
| Participants | 60 patients with a first, right hemispheric stroke participated in the study Age, years: sham = 70.6 ± 11.44, 8cTBS = 67.8 ± 10.13, 16cTBS = 74.3 ± 10.23 Sex (men/women): sham = 7/3, 8cTBS = 5/5, 16cTBS = 6/4 Time post stroke, days: sham = 25.8 ± 11.26, 8cTBS = 26.8 ± 20.89, 16cTBS = 22.9 ± 10.34 | |
| Interventions | In brief, the cTBS protocol comprised 801 pulses, delivered in a continuous train of 267 bursts. Each burst consisted of 3 pulses at 30 Hz, repeated at 6 Hz. Duration of 1 single cTBS train was therefore 44 seconds In the 16cTBS group, the same daily protocol was repeated 4 times, i.e. 16 cTBS trains were applied over 4 days In the 8cTBS group, 8 cTBS trains were applied over 2 days. Four cTBS trains were applied on Day 1 (2 cTBS trains with an interval of 15 minutes, third and fourth cTBS trains 60 and 75 minutes after the first one, respectively (Cazzoli et al, 2012), and 4 cTBS trains on Day 2 ‐ same time intervals as for Day 1, repeated after 24 hours) Sham stimulation was applied with the same 8cTBS protocol as described above, except for use of a sham coil |
|
| Outcomes |
Assessed pre‐intervention, post intervention, and 3 months post intervention |
|
| Notes | We entered this study as Nyfeller 2019 8c TBS and Nyfeller 2019 16c TBS and spilt the control group across entries | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation procedure was carried out by a blinded collaborator (TP), using a computerised block randomisation protocol to ensure equal group sizes (https://www.random.org/ integer‐sets) |
| Allocation concealment (selection bias) | Low risk | Treatment allocation was concealed from trained observers |
| Blinding of participants | Low risk | “Double‐blind” |
| Blinding of personnel | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | CBS was completed by rehabilitation nurses taking care of patients on a daily basis, who were blind with respect to the experimental protocol, and who observed patients performing different ADL. Unknown whether blinding was successful |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 3 dropped out at T2, unclear from which group though |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | Nothing obvious |
Nyfeller 2019 16c TBS.
| Study characteristics | ||
| Methods | See Nyfeller 2019 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation procedure was carried out by a blinded collaborator (TP), using a computerised block randomisation protocol to ensure equal group sizes (https://www.random.org/ integer‐sets) |
| Allocation concealment (selection bias) | Low risk | Treatment allocation was concealed from trained observers |
| Blinding of participants | Low risk | “Double‐blind” |
| Blinding of personnel | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | CBS was completed by rehabilitation nurses taking care of patients on a daily basis, who were blind with respect to the experimental protocol, and who observed patients performing different ADL. Unknown whether blinding was successful |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 3 dropped out at T2; unclear from which group though |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | Nothing obvious |
Nyfeller 2019 8c TBS.
| Study characteristics | ||
| Methods | See Nyfeller 2019 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Nys 2008.
| Study characteristics | ||
| Methods | RCT; single‐blind randomised controlled design Setting: stroke units, Netherlands | |
| Participants | 16 participants with neglect from 3 stroke units Experimental: n = 10, control: n = 6 Adequacy of matching at baseline? Yes Number lost to follow‐up: not clear ‐ only those who completed were included in the report. Also excluded 1 patient with deterioration of neurological condition during treatment phase, which probably should have been a loss to follow‐up rather than exclusion Mean age, years, mean (SD): experimental = 63.6 (13.8), control = 61.5 (11.0) Sex (men/women): experimental = 7/3, control = 3/3 Time post onset, days: experimental 1 = 8.8 (5.3), control = 11.2 (6.4) Side of damage: right Method of diagnosing stroke: not stated; based on referral by a stroke physician on admission to SU Method of diagnosing neglect: ≥ 2 subtests (out of 4): BIT subtests below cutoff. The 4 tests were Star Cancellation (cutoff ≤ 51), line bisection (cutoff ≤ 7), figure copying (cutoff ≤ 2), and representational drawing (cutoff ≤ 2) Inclusion criteria: inpatient in SU with neglect, within 4 weeks post stroke. All participants had to demonstrate an after effect of at least 3 visual degrees to the left of the landing position after the first prism adaptation; this would apply only to the active treatment group, but none were excluded for this reason Exclusion criteria: ocular problems, disturbed consciousness or too limited attention span (participants excluded during screening) Visual sensory deficit: 2 in the experimental group had hemianopia, diagnosed by confrontation comparing cueing and non‐cueing conditions by a stroke neurologist | |
| Interventions | Prism adaptation: "an extended version of that used by Rosetti et al 1998". While wearing goggles with prisms inducing a rightward optical shift of 10°, participants made 100 fast pointing movements to 2 visual targets presented 10° to the left and right of the body midline. Sessions of 30 minutes were conducted 4 days in a row vs placebo ‐ as above, but wearing goggles with no optical shift. Sessions of 30 minutes were conducted 4 days in a row Profession of intervention provider not stated |
|
| Outcomes |
Measured up to 1 month post intervention. |
|
| Notes | Postulated mechanism of action: not clear, but stated there was a "neural basis for the therapeutic effect" and treated early because the brain is most sensitive to rehabilitative treatment early after stroke | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | According to a randomisation procedure in SPSS |
| Allocation concealment (selection bias) | Unclear risk | Insufficient details "according to a randomisation procedure in SPSS" |
| Blinding of participants | High risk | Nature of prism glasses, no details given |
| Blinding of personnel | High risk | Nature of prism glasses, no details given |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Only 1 measure, scene copying, appears to have been scored retrospectively by an independent rater. Not stated whether outcome assessor was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | Nothing obvious |
Pandian 2014.
| Study characteristics | ||
| Methods | Prospective, open, blinded endpoint (PROBE design) RCT Setting: hospital, India | |
| Participants | 48 stroke patients with thalamic and parietal lobe lesions within 48 hours of stroke onset who had upper limb weakness Treatment = 27, control = 21 Diagnosis of neglect: star cancellation = 51 or fewer stars cancelled by the patient LBT: cutoff score for unilateral visual neglect was an error > 1.4 cm left or right Age, mean (SD), years: treatment = 63 (11), control = 64 (12) Sex (men/women): treatment = 14/13, control = 14/7 Hemisphere damaged (right/left): treatment = 21/6, control = 16/5 Exclusion criteria: Glasgow Coma Scale score < 7 | |
| Interventions | During the MT, patients sat near a table on which a mirror box (35 × 3 × 35 cm) was placed vertically. The affected hand was hidden behind the mirror, and the unaffected hand was placed in front of the mirror. Patients were asked to see only the unaffected hand in the mirror. Patients were instructed to perform flexion and extension movements of the non‐paretic wrist and fingers while looking into the mirror. Thus, they were seeing the reflection of the unaffected hand as movement of the affected hand in the mirror. During the session, while they were moving the non‐paretic hand, patients were asked to do the same movements in the paretic hand Control group carried out similar exercises for the same time period but used the non‐reflecting side of the mirror. The paretic hand was hidden from their sight. Control therapy was given by the same physiotherapist. Both treatment and control groups received limb activation |
|
| Outcomes | Primary outcomes
Secondary outcomes
Measured up to 6 months post intervention |
|
| Notes | Study authors did not give SDs for neglect outcomes. We imputed the SD for baseline at outcome. We attempted to impute mean from change scores that were provided; however the presented change scores require further explanation, as they imply perfection at follow‐up (a score of 53 on star cancellation, on which the maximum is 52), and because the magnitude of difference given the SD appears extreme. We are yet to receive a response from study authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | All eligible participants were randomised to the MT group or the control group (sham MT). A random allocation sequence was made using random digits generated by RALOC (random allocation) software and was conveyed to investigators by sealed numbered envelope |
| Allocation concealment (selection bias) | Low risk | See above |
| Blinding of participants | High risk | Not possible to blind |
| Blinding of personnel | High risk | Not possible to blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Physiotherapist who was unaware of group assignments assessed outcomes at 1, 3, and 6 months. No evidence suggests that this assumption was tested |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Very little attrition ‐ 1 each group |
| Selective reporting (reporting bias) | Unclear risk | 3 primary outcomes |
| Other bias | High risk | There was some imbalance in stroke lesions, manual dexterity, and stage of motor recovery between randomised groups Use of LOCF ("missing values on outcomes were imputed using last observation carried forward method") |
Park 2015.
| Study characteristics | ||
| Methods | RCT Setting: South Korea | |
| Participants | Inclusion criteria for participation were as follows: (1) left hemiparesis with onset duration > 6 months; (2) patient with unilateral neglect (> 6.3 mm deviation of the true centre of the line in the line bisection test); (3) cognition (> 23 points on the Korean version of Mini‐Mental Status Examination); (4) no hemianopsia or apraxia; and (5) imagination ability (average score < 3 in the Vividness of Movement Imagery Questionnaire) Age, years, mean (SD): intervention = 61.5 (5.1), control = 63.6 (6.0) Sex (men/women): intervention = 8/7, control = 6/9 Hemisphere damaged: right Time since stroke, months: intervention = 6.8 (0.9), control = 6.9 (1.0) | |
| Interventions | Participants received a mental practice intervention or usual care. During mental practice, experimental group (EG) participants mentally practised positioning and movement of the left upper limb as intensively as possible in a repetitive fashion. EG participants sat comfortably and leaned back against the back rest with feet on the floor and imagined the scene while listening to the voice of the researcher for 10 minutes with eyes closed. Contents of mental practice were to pick up a baseball, a pencil, and a coin at the centre of a body using the left hand, respectively, then move them into a basket lying on the left side. Verbal feedback provided by participants assured correct execution of imagery tasks. Each task was repeated up to 10 times per session. At the beginning of each task, break time was given to patients to induce relaxation and concentration internally on the left arm. EG participants received mental practice for additional 10 minutes (5 days a week for 4 weeks) | |
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Based on a computer‐generated randomisation programme by a research assistant under the blind condition |
| Allocation concealment (selection bias) | Unclear risk | No detail given |
| Blinding of participants | High risk | No detail given |
| Blinding of personnel | High risk | No detail given |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | All clinical measures were administered by the blinded assessor, but no detail was given |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No incomplete data apparent |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | Nothing obvious |
Park 2015b.
| Study characteristics | ||
| Methods | Setting: rehabilitation centre, South Korea | |
| Participants | Inclusion criteria for participation were (1) onset duration > 6 months, (2) right hemisphere stroke with UN, (3) Mini Mental State Examination score > 24, (4) ability to imagine (average score on Vividness of Movement Imagery Questionnaire < 3), and (5) active wrist muscle strength > 2 on Medical Research Council (MRC) Scale Exclusion criteria were (1) an implanted cardiac pacemaker, (2) skin lesion on affected side or hypersensitivity at the electrode site, (3) history of seizure or epilepsy, and (4) unstable medical conditions Age, years: intervention = 67.5 ± 10.3, control = 62.2 ± 10.2 Sex (men/women): intervention = 10/6, control = 8/9 Hemisphere damaged: right Time since stroke, months: intervention = 3.3 ± 1.3, control = 3.5 ± 1.6 | |
| Interventions | Experimental group (n = 16) received MP‐EMG ES in addition to conventional rehabilitation therapy (CRT: physical therapy and occupational therapy), whereas control group (n = 17) received cyclical ES in addition to the same CRT. Mentamove (Mentamove Deutschland GmbH, Munich, Germany) was used to apply MP‐EMG ES in the experimental group. Surface electrodes were attached to the wrist extensor muscle, and a reference electrode was attached at the lateral side of the forearm. The site of electrode placement was marked using a permanent marker throughout the intervention. During motor imagery training, electrical potentials were generated in the affected arm and were recorded using EMG. When potentials reached a pre‐set threshold, the induced electrical stimulation would contract the targeted muscle. The Mentamove process consisted of 3 stages: (1) motor imagery (approximately 12 seconds), (2) electrical stimulation (approximately 6 seconds), and (3) relaxation (approximately 12 seconds). Motor imagery used in this study was vigorous waving of the affected whole arm. This imagery was selected because the EMG was not able to detect electrical stimulation induced by motor imagery of simple extension of the wrist or elbow. The EMG pick‐up threshold was set afresh for each patient in every session. If the patient repeatedly reached the threshold during MP‐EMGES, the threshold was automatically increased slightly. Instructions were as follows: first, relax in a comfortable position. Imagine that your left arm moves rapidly and intensely when you see “motor imagery” in the tool window. If your performance is successful, you will experience an electrical stimulation in your forearm. If your performance fails, maintain the relaxed state. Cyclical ES (Mendel GmbH, Germany) without the EMG function was used to apply electrical stimulation in the control group. Electrodes also were attached to the wrist extensor muscle. With either instrument, biphasic pulses with frequency of 35 Hz and pulse width of 200 μS were applied for 12 seconds. Stimulation intensity led to a clear extension of the wrist (average 20 to 30 mA) | |
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Low risk | Randomly allocated to the 2 groups by block randomisation using opaque envelopes containing a code specifying the group |
| Blinding of participants | High risk | No details given |
| Blinding of personnel | High risk | No details given |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No details given |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None incomplete |
| Selective reporting (reporting bias) | Low risk | Outcomes reported in equal detail |
| Other bias | Low risk | No evidence of this |
Polanowska 2009.
| Study characteristics | ||
| Methods | RCT, single site and double‐blinded Setting: Poland | |
| Participants | 40 participants with first‐ever stroke and hemi‐neglect
Experimental: n = 20, control: n = 20
Adequacy of matching at baseline? No, although age, sex, BI, and MMSE are well balanced at baseline, accuracy on neglect tests seems lower in experimental vs control group
Number lost to follow‐up: study authors confirm no losses to follow‐up Mean age, years, mean (SD): experimental = 61.6 (8.3), control = 58.3 (12.9) Sex (men/women): experimental = 11/9, control = 14/6 Side of damage: right Method of diagnosing stroke: confirmed by neuroimaging and neurological exam (CT) Method of diagnosing neglect: confirmed by neuropsychological exam as fulfilling 2 of 3 criteria: ≥ 4 omissions of left‐sided targets in subtest A of Balloons test; marked rightward bias (cutoff score of 7) on line bisection; spontaneous behaviours specific to neglect (e.g. ipsilesional deviation of head, eyes, trunk); attending to ipsilesional side; neglect dyslexia and dysgraphia with tendency to initiate search on right of stimulus sheet Time post onset, days: experimental = 44.4 (27.3), control = 46.6 (26.2) Inclusion criteria: first right hemisphere stroke, left visuospatial neglect, recruited from single rehabilitation unit, 2 to 12 weeks post stroke, right‐handedness, 25 to 75 years of age, informed consent obtained Reasons for exclusion: if electrical stimulation contraindicated, history of dementia, neurological or psychiatric disorders; if communication or other problems meant unable to co‐operate Visual sensory deficit: 'visual sensory deficit': experimental = 13/20, control = 13/20; and 'hemianopia': experimental = 6/20, control = 9/20, as assessed by "standard neurological assessment" |
|
| Interventions | Electrical somatosensory stimulation of the left hand combined with conventional visual scanning training, 1 month duration of 20 session of 45 minutes duration each, 5 days per week. This stimulation lasted for the first 30 of the 45 minutes. Electrical stimulation was provided by 2 electrodes on the hand, giving a maximum intensity of 15 mA. Visual scanning used 2 programmes from RehaCom computerised system to get active purposeful exploration of visual field (1 ‐ saccadic training ‐ seek stimuli within detailed background; 2 ‐ attention and concentration ‐ detect and identify stimuli, then seek their counterpart on the opposite side within a detailed background). Visual scanning also used some paper‐and‐pencil tasks to improve scanning when reading and writing; drawing and copying; and analysing form and content of complex visual stimuli. Verbal and visual cues and instructions given, as was feedback on achievements and errors vs visual scanning training as above, with placebo stimulation when electrodes were applied to the hand but without "current intensity" Visuospatial scanning training was conducted by a neuropsychologist, and electrostimulation was supervised by a neurologist |
|
| Outcomes |
Also measured after only 1 day of stimulation but excluded those results in favour of the more meaningful 1 month results, which are immediate post rehabilitation – so no maintenance/follow‐up outcomes were measured |
|
| Notes | Postulated mechanism of action: visual scanning training aims to remind and motivate participants to scan to the left to build the habit of voluntarily scanning their neglected space. Requires awareness by the participant, which is not always present, hence use of passive (non‐volitional) physiological approaches such as sensory stimulation. Assumes manipulated sensory inputs are linked to auto levels of orientation behaviour. But effects seem transitory, so this study attempts to combine active training of visual scanning with passive stimulation to enhance activation of right hemisphere attention system and to improve visual exploration of extra‐personal space All participants received visual scanning training ‐ the only difference was electrical stimulation Study authors state in the paper that 11 participants reported a tingling sensation during a trial electrostimulation period. During the study itself, however, only 1 participant noted such a sensation; afterwards, it was noted this person was in the sham group |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Blocked randomisation was performed by 1 person unblinded to group allocations and was based on random number tables. For each 10 subjects, numbers 1‐5 meant that patients would be in group E, the numbers 6‐10 meant that patients would be in Group C with the constraint that in each block of 10 there would be 5 in group E and 5 in group C" |
| Allocation concealment (selection bias) | Low risk | "Allocations were stored in sealed, numbered envelopes that were opened only at the time of recruitment and the author has confirmed all envelopes were prepared before recruitment began by someone other than the recruiter" |
| Blinding of participants | Low risk | "Simulated stimulation was used for the controls" |
| Blinding of personnel | Low risk | "Both the psychologist who conducted the assessment and the person who supervised rehabilitation and evaluated therapy outcome were blinded to each patient’s group assignment. A third person who knew patient allocation controlled the generation of current during stimulation and ensured that the patients and other researchers remained blinded to the level of current delivered" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | States outcome assessor blinded, but not evidenced |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Study authors advise that all randomised participants were followed up on all variables, and there were no post‐randomisation exclusions |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | High risk | Control group had significantly better scanning accuracy at baseline. No adjustment was made for differences in scanning accuracy |
Raghavan 2017.
| Study characteristics | ||
| Methods | RCT Setting: UK, community hospital | |
| Participants | Inclusion criteria: (1) spatial and/or object neglect as identified by asymmetry scores on the Hearts Cancellation test of the Oxford Cognitive Screen (OCS); (2) neglect diagnosis confirmed by multi‐disciplinary team (MDT); (3) between 1 week and within 6 months of the stroke event; (4) medically fit; (5) able to comprehend instructions and provide informed consent as per the opinion of the MDT; (6) ability to concentrate for 20 to 30 minutes as judged by the MDT; (7) no co‐morbid psychological or neurological disorders (e.g. depression, dementia) as judged by the MDT; (8) no contraindications for rTMS administration upon administration of a screening questionnaire Age, years, mean: intervention = 75. 2, SD = 8.5; control = 80.08, SD = 7.1 Sex: intervention 3 women, control 1 woman Time post stroke, days: screening was done on average 19 days (SD = 9 days) after stroke for Intervention group, and 27 days (SD = 21 days) after stroke for control group | |
| Interventions | Magstim Super Rapid magnetic stimulator (Magstim Company, Whitland, Wales, UK) connected to a figure of 8 coil was used to deliver rTMS. The resting motor threshold was defined as lowest intensity of stimulation required to elicit 5 visible motor twitches in the relaxed right hand's first dorsal interosseous muscle, in response to 10 consecutive stimuli. To identify this threshold, the optimal "hotspot‟ in each patient's motor cortex was identified and stimulated (Rossini et al, 2015). rTMS was then provided at 90% of this identified resting motor threshold. Intervention group received 20 minutes of rTMS at 1 Hz (1200 pulses) to the left inferior parietal lobe (P3) of the intact hemisphere Control group received sham stimulation |
|
| Outcomes |
Follow‐up testing on the same cognitive test battery as at baseline was conducted both in the short term, i.e. less than 1 month post rTMS, and in the long term, i.e. at 6 or more months post rTMS |
|
| Notes | Data are from Chapter 5 of thesis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Based on computerized randomization" only detail |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants | Unclear risk | No details |
| Blinding of personnel | High risk | Different placement of probe suggests not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 dropped out of intervention group, 1 from control group |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | Nothing obvious. Multiple testing adjustments made |
Robertson 1990.
| Study characteristics | ||
| Methods | RCT Setting: hospital, UK | |
| Participants | 30 (see Notes) inpatients of Edinburgh hospitals who showed left visual field neglect on BIT Experimental: n = 17, control: n = 13 (The following data describe the 36 initial participants: see Notes) Mean age, years (SD): experimental = 64.2 (12.6), control = 63.1 (9.6) Sex (men/women): experimental = 9/11, control = 10/6 Onset of neglect, weeks (SD): experimental = 19.2 (21.1), control = 10.8 (6.3) Inclusion: presence of neglect (failure on at least 3/9 behavioural tests), oriented for time and place, ability to consent, ability to concentrate sufficiently to sit at computer‐based task for at least 15 minutes | |
| Interventions | 15½ hours (14 sessions of 75 minutes each, 2×/week for 7 weeks) computerised scanning and attention training (intensive briefing about nature of participant's problems, feedback on left and right latencies, trainer reinforcement and encouragement) vs 11.4 hours recreational computing (to minimise scanning and timed attention tasks, without any potential neuropsychological mechanism to improve cognitive function, but exposed to computer activities such as games, quizzes, and simple logical games) | |
| Outcomes | Study collected several types of outcomes
The BIT was the principal outcome measure. (Although not explicitly stated, it is assumed from the description on page 664 and the low scores in Table 10 that only the BIT behavioural subtests were given.) Outcomes were given immediately after training and after 6 months. Study also collected data on several other tests, including the GHQ and the FAI, to ensure matching of groups (see Notes). These were collected at each time point. This review used the BIT, immediately and after 6 months |
|
| Notes | This review entered n = 30 of initial 36 (33 with CVA, 2 with HI, 1 had surgery for excision of meningioma). 3/36 not followed up immediately, and 9/36 not seen at 6 months, but no information on which group these were from, so data entered into this review subtracted 3 and 9 from each group at first (n = 30) and second assessments, respectively. Information on allocation concealment provided by personal communication. 6 months' follow‐up Exclusion: participants with BIT score > 70 Cancellation data reported as errors rather than correct performance Review could not include FAI data as these were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation restricted in blocks of patients with severe or mild neglect; therefore stratified by severity |
| Allocation concealment (selection bias) | Low risk | External randomisation. Randomisation restricted in blocks of patients with severe or mild neglect; therefore stratified by severity. Randomisation was carried out by a third party |
| Blinding of participants | High risk | No information given |
| Blinding of personnel | High risk | No information given |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessor stated but not evidenced |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 3/36 not followed up immediately and 9/36 not seen at 6 months, but no information on which group these participants were assigned to |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | Slight difference in letter cancellation errors and Wisconsin at baseline. Adjustment not necessary |
Robertson 2002.
| Study characteristics | ||
| Methods | RCT Setting: UK | |
| Participants | 40 randomised but 36 seen for immediate outcome assessment (see Notes); recruited from London hospital and community rehabilitation teams; had left visual neglect on cancellation or bisection tests (The following data describe the initial 40 participants: see Notes) Experimental: n = 19, control: n = 21 Mean age, years (SD): experimental = 69.3 (9), control = 67 (9.4) Sex (male/female): experimental = 13/6, control = 16/5 Onset of neglect, days (SD): experimental = 152.8 (142.4), control = 152.1 (117.9) Inclusion: right hemisphere stroke, younger than 80 years, right‐handedness, no history of major psychiatric/disease/disability that would prevent participation or contaminate results | |
| Interventions | LAT wearing (on the wrist/leg/shoulder) an active limb activation device during perceptual training. The device emitted an auditory tone if no left‐sided movement was made; vs perceptual training wearing an inactive (no tone) limb activation device Both groups received training at their residence (usually own home) for 12 weeks for approximately 45 minutes per week Perceptual training for both groups involved working on visuoperceptual puzzles and reading tasks that implicitly but not explicitly involved advice to scan to the left | |
| Outcomes | Outcomes:
For comparability with other studies, this review used only the following time points: immediate and 6 months |
|
| Notes | Attrition: 36/40 followed up immediately (experimental = 17, control = 19); 32 at 6 months, 26 at 18 to 24 months Groups appeared appropriately matched for demographic and clinical baseline variables No information on number per group at 6 months. Known that 4 were lost, but not whether all were from a single group, so assumed worst case and subtracted 4 per group, i.e. conservative sample estimate of 28 not 32 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail given |
| Allocation concealment (selection bias) | Low risk | Robertson 2002 confirmed that recruiters were unaware of and were unable to predict allocation concealment. Study authors confirmed randomisation but did not specify the method used. Concealment was highly likely to have been achieved, although this could not be guaranteed |
| Blinding of participants | High risk | Nature of intervention |
| Blinding of personnel | High risk | No detail given |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessor; no more detail given |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4 (2 from each group) dropped out during treatment. 36 participants were followed up at 3 months, and 32 at 6 months. Of the 4 who dropped out at 6‐month follow‐up, 2 had a further CVA, 1 died, and 1 refused. Low risk; loss to follow‐up unlikely to affect outcomes |
| Selective reporting (reporting bias) | Low risk | 'Selected variables' chosen for table, but no evidence of bias |
| Other bias | Low risk | Nothing obvious |
Rode 2015.
| Study characteristics | ||
| Methods | Double‐blind RCT Setting: rehabilitation unit, France | |
| Participants | 20 single‐stroke patients with left SN at least 1 month following ischaemic event (aged 18 to 90) Prism = 10, control = 10 Definition neglect: LBT, balloon, copy of a drawing, dictation, and reading of a text Age, years, mean (SD): prism = 56 (12), control = 62 (13) Sex (men/women): prism = 5/4, control = 5/4 Days, mean (SD), between stroke and treatment: prism = 77 (38), control = 70 (38) Exclusion: existence of multiple brain lesions; temporospatial disorientation; psychiatric disorders; associated, non‐stabilised pathology | |
| Interventions | In the ‘prism' group, PA was carried out by wearing a pair of glasses producing a 108 rightward optical deviation of the visual field. Prismatic lenses were composed of 2 superimposed, curved, point‐to‐point lenses fitted with a ‘‘glacier’’ frame containing lateral leather protectors designed to avoid access to non‐shifted vision. Prisms covered a total visual field of 105% in which each monocular field represented 75 degrees, and the central visual binocular field represented 45 degrees. During prism exposure, the patient had to execute 80 rapid pointing movements towards visual targets located 10 degrees to the left or to the right of the middle of her/his body, with targets made to pseudo‐randomly alternate. In spite of repeated instructions to carry out rapid movements, movements produced in brain damaged patients generally remain too slow as to allow visual retroaction, and errors committed by our patients did not necessarily reflect the amplitude of optical deviation or the phase of adaptation. However, their degree of rapidity remained compatible with the development of actual sensory‐motor adaptation by reducing the strategic components of compensation. Pointing movements were performed with a pause of 30 seconds after each series of 20, thereby favouring an increased number of errors at the start of the following series. During exposure, the patient did not see the initial position of her/his hand, which entered the visual field only once the movement was approximately 30% to 50% complete, in such a way as to favour proprioceptive‐visual coding of the movement. All in all, prism exposure lasted from 6 to 10 minutes Although 'control' group patients carried out this visuomotor task under the same conditions, they were wearing a pair of placebo glasses fitted out with neutral lenses of the same weight consisting of two 5‐degree prismatic lenses set up so as not to produce any optical deviation Each patient carried out the exposure task (with prismatic glasses or neutral lenses) 4 times: at D0 (Expo1), at D + 7 (Expo2), at D + 14 (Expo3), and at D + 21 (Expo4) All exposure sessions took place under the same conditions and with the same operators |
|
| Outcomes | Primary outcome measure of the study was functional improvement in daily life activities following rehabilitation, assessed by the Functional Independence Measure (FIM) Secondary outcome measure was total score on the Behavioural Inattention Test (BIT) Measurement with regard to the primary endpoint was carried out 4 times: in pre‐tests and in post‐tests at 1 (M1), 3 (M3), and 6 (M6) months after the initial PA session. BIT evaluations were performed twice: in pre‐test, and then in post‐test at 6 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation and drawing by lots of the patients into 'prism' or 'control' groups were carried out by Denis Pelisson, director of the ImpAct team, in the Lyon Neuroscience Research Centre. Randomisation was produced at 2 levels, first by selection of patients for the 'prism' or 'control' group; second, by selection of patients according to severity of the initial SN assessed by BIT score, with the objective that the ratio of patients with severe neglect and patients with moderate neglect is comparable in the 2 groups |
| Allocation concealment (selection bias) | Low risk | See above |
| Blinding of participants | Low risk | Double‐blind; justified in text |
| Blinding of personnel | Low risk | See above |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Examiners carrying out the evaluation (GR, SL, EM) did not know whether a given patient had undergone PA. They were distinct from examiners performing the task of exposure to prismatic or neutral glasses (YR, SJC, LP). The double‐blind procedure was facilitated by the fact that SN patients were not aware of the disturbance induced by prism deviation and did not present the vegetative reactions expected during the appearance of motor errors when prisms were worn for the first time. Consequently, they could be assigned without their knowledge to the 'prism' and 'control' groups. This also entailed that examiners performing the assessment did not receive information from patients. All of this might have compromised the double‐blind trial |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition of only 1 in each group |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | Nothing obvious |
Rossit 2019.
| Study characteristics | ||
| Methods | Controlled prospective study using a single‐blind design Setting: hospital, UK | |
| Participants | Inclusion criteria: stroke lesions as identified by brain imaging report, hemi‐spatial neglect symptoms (in line bisection, BIT, or balloons test), ability to follow instructions, and medical fitness to participate Exclusion criteria were previous or concomitant neurological (e.g. brain tumour, dementia), visual (e.g. cataract), or motor (e.g. arthritis) disease unrelated to the current stroke Age, mean, years (SD): intervention = 65.6 (2.8), control = 64.9 (2.5) Sex (men/women): intervention = 3/7, control = 8/2 Hemisphere damaged: right Time since stroke, months (SD): intervention = 3.1 (0.9), control = 3.2 (0.5) |
|
| Interventions | Visuomotor feedback training (VFT) is a neglect rehabilitation technique that involves simple, inexpensive, and feasible training of grasping to lift rods at the centre. Patients in the intervention group were asked to reach for and grasp the rod with a pincer grip (using the forefinger and the thumb) and to try to lift it up at its centre, so it would be balanced. If they felt that it was not balanced after lifting it, they could repeat the trial until satisfied. Feedback was provided only from the tilting rod; the experimenter did not comment on performance. Patients in the control group were instructed to simply reach for and grasp the rod with a pincer grip (using the forefinger and the thumb) by its non‐neglected end (usually the right) and to lift it up from the mat on that side and place it back down again. Training was delivered for 2 sessions by an experimenter; then patients self‐administered it for 10 sessions over 2 weeks | |
| Outcomes |
Outcomes were measured up to 4 months post intervention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | High risk | Patients randomly assigned to intervention or control group as determined in the order of a list (complete/unrestricted randomisation); order of the list not hidden |
| Blinding of participants | Low risk | "Patients, carers and scorers of our outcome measures remained blind to group assignment throughout the trial, except for the Stroke Impact Scale" |
| Blinding of personnel | High risk | It seems instructions for the 2 arms are different; therefore it is impossible for the staff not to know which people belong to which group |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "The outcome assessment was performed by the experimenter (except the SIS) who also delivered the treatment. However, all measures were scored by a treatment‐blinded researcher" However (see above), it seems unlikely that these could be blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition equal in each group |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | Nothing obvious |
Rusconi 2002.
| Study characteristics | ||
| Methods | RCT Setting: Italy | |
| Participants | 24 randomised (see Notes), but outcome data collected on 20 (The following data describe the 20 participants) Experimental: n = 12, control: n = 8 (experimental is Type 1 and control is Type 2: see Interventions) Mean age, years: experimental = 69.8, control = 65.1 Sex (men/women): experimental = 5/7, control = 3/5 Mean weeks post stroke: experimental = 6.92, control = 8.38 Inclusion: unilateral right hemisphere stroke assessed by CT scan, right‐handedness, symptoms of unilateral neglect, admission to hospital for rehabilitation 5 weeks post stroke Exclusion: dementia | |
| Interventions | Study compared more than 2 interventions. First, there is a comparison of 2 types of cognitive training: Type 1 vs Type 2. Each 'type' is then subdivided into whether or not TENS is added (see Notes) Type 1 vs Type 2: both consist of 5 × 1‐hour sessions per week for 2 consecutive months (40 sessions) using 4 procedures requiring participants to actively scan the visual field (reading sentences and stories, doing line drawing on a dot matrix, assembling 3D cubes, matching cards containing the name and visual image of an object). Types 1 and 2 differed in that only Type 1 involved verbal and visuospatial cueing and verbal feedback. Although Type 2 used the same 4 procedures, it did not involve cueing or feedback, i.e. aspects of the training designed to improve awareness and encourage compensation | |
| Outcomes | Assessments were classified as 'functional and neurological' (i.e. BI, standard clinical neurological examination) or 'neuropsychological' (i.e. line cancellation, letter cancellation, line bisection, sentence reading, o'clock test, judgement of drawings, anosognosia, RCPM, facial recognition, position deficit). These were taken at 4 time points: on admission for neurorehabilitation at least 5 weeks post stroke (T0); 1 month later (T1), after which eligibility was determined and participants were randomised; after 1 month of intervention (T2); and after 2 months of intervention (T3) For comparability with other studies, this review used only T3 letter cancellation and BI. As intervention continued for 2 months, T3 is coded in this review as immediate effects | |
| Notes | Study author provided clarification and raw data by personal communication 24 people were randomised: 12 to Type 1 and 12 to Type 2. Study authors excluded 4 from the final evaluation because of "clinical worsening that prevented the conclusion of the treatment". These 4 were allocated to Type 2 Cancellation scores were for the numbers correctly cancelled. Separate scores were given for left and right space, but this review used total score. Line bisection data were for mean deviation in millimetres left (negative) or right (positive) of the midpoint. Line cancellation data could not be used, as the experimental group's SD was 0 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | High risk | Paper states "randomly assigned"; no details provided Subsequent information states allocations stored in sequentially numbered, sealed, opaque envelopes. Concealment of allocation is unlikely |
| Blinding of participants | High risk | No detail given |
| Blinding of personnel | High risk | No detail given |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No detail given |
| Incomplete outcome data (attrition bias) All outcomes | High risk | None reported in paper, but study authors reported 24 people were randomised: 12 to Type 1 and 12 to Type 2. Study authors excluded 4 from final evaluation because of "clinical worsening that prevented the conclusion of the treatment". These 4 were allocated to Type 2. No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | Nothing obvious |
Schroder 2008.
| Study characteristics | ||
| Methods | RCT, 3‐arm study Setting: Germany | |
| Participants | 30 right‐handed participants with right brain damage, moderate left neglect
Experimental 1: n = 10, experimental 2: n = 10, control: n = 10
Number lost to follow‐up: none
Adequacy of matching at baseline? Yes, no significant differences at baseline
Mean age, years, mean (SD): experimental 1 = 68.4, experimental 2 = 60.6, control = 67.3
Sex (men/women): experimental 1 = 7/3, experimental 2 = 5/5, control = 6/4
Time post onset, days, mean (SD): experimental 1 = 43.8 (23.6), experimental 2 = 24.6 (9.6), control = 36.2 (24.2)
Side of damage: right
Method of diagnosing stroke: not stated
Method of diagnosing neglect
No details of cutoffs provided Inclusion criteria: right‐handedness, less than 90 days post stroke, left brain damage, at least moderate neglect Exclusion criteria: not stated Visual sensory deficit: not stated |
|
| Interventions | Visual exploration and TENS: 20 therapy sessions, each lasting 25 to 40 minutes over 4 weeks (TENS: 100 Hz, over left trapezius, applied throughout exploration training) vs visual exploration and OKS 20 therapy sessions, each lasting 25 to 40 minutes over 4 weeks (OKS: small randomly spaced squares moving slowly to the left across a screen, 2 × 10‐minute periods of OKS separated by 10 to 20 minutes of exploration training) vs visual exploration (control) using the ELEX apparatus (stimuli patterns were presented on a screen that subtended 53° vertically and 40° horizontally: after initial fixation, participants had to shift fixation to a yellow stimulus) Profession of the intervention provider not stated |
|
| Outcomes |
Measured up to 1 week post intervention |
|
| Notes | TENS: "a non‐specific activation of the right hemisphere or a directional effect on the egocentric coordinates of extrapersonal space" OKS "activates multiple cortical (temporoparietal and vestibular cortex, the insula) and subcortical structures (basal ganglia) involved in multisensory integration" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly assigned"; no other details |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of participants | High risk | No details given |
| Blinding of personnel | High risk | No details given |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No details given |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | None reported |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Low risk | For the few variables given, groups appear comparable at baseline |
Seniow 2016.
| Study characteristics | ||
| Methods | Setting: rehabilitation unit, Poland | |
| Participants | 29 right‐handed Polish‐speaking patients with left‐sided hemi‐spatial neglect, who were admitted to the Neurorehabilitation Unit during a 3‐year period, were enrolled in the study Inclusion criteria were as follows: (1) adults 75 years of age, to avoid enrolling patients who would have difficulty actively participating in daily therapy and/or patients with age‐related cognitive decline; (2) first‐ever right hemisphere ischaemic stroke; (3) clear signs of hemi‐spatial neglect in the visual modality, as confirmed through a neuropsychological assessment; (4) time since stroke: 3 weeks to 6 months; (5) good general condition, to actively participate in rehabilitation programme; (6) provided written informed consent Exclusion criteria were as follows: (1) previous brain damage and non‐stroke neurological and psychiatric diseases that influence cognitive–behavioural functioning (e.g. dementia, addiction, depression); (2) impaired primary visual perception; (3) using medications that affect cortical excitability (e.g. antiepileptics, benzodiazepines); (4) contraindications to electrostimulation Age, years, mean (SD): intervention = 63.4 (7.7), control = 60.2 (9) Sex (men/women): intervention = 7/7, control = 8/7 Hemisphere damaged: right Time since stroke, days (range): intervention = 40.5 (25 to 140), control = 34.5 (27 to 45) | |
| Interventions | Intervention group patients received a therapeutic programme combining conventional visual scanning training with TENS applied by a mesh glove on the left hand. Control participants received the same treatment with sham TENS The 3‐week hemi‐spatial neglect rehabilitation programme comprised 15 consecutive individual therapeutic sessions (5/week) with active or sham electrostimulation applied during the first 30 minutes of the 45 minutes of visual scanning training |
|
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail given |
| Allocation concealment (selection bias) | Unclear risk | No detail given |
| Blinding of participants | Low risk | Member of the research team blinded to groups applied the same montage of electrodes to the left (contralesional) hand of each patient during each therapeutic session |
| Blinding of personnel | Unclear risk | No detail given |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Hemi‐spatial neglect severity was assessed twice by the same experienced clinical neuropsychologist (KP), blinded to group, on the day preceding the rehabilitation programme (baseline measurement) and on the day after its completion (post treatment) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No detail given |
| Selective reporting (reporting bias) | Low risk | Nothing obvious |
| Other bias | Low risk | Nothing obvious |
Sesh 2018.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Patients within 2 weeks following acute right MCA territory ischaemic stroke with clinical features suggestive of visual and/or sensory neglect Fully conscious, oriented without any significant aphasia (should have normal/useful level of comprehension and communicative capabilities) Age > 18 and < 80 years Age, years: intervention group = 56 ± 12.03, control group = 61 ± 6.6 Sex (men): intervention = 3, control = 6 Time post stroke: not reported, although < 2 weeks in inclusion criteria | |
| Interventions | Stimulate patients with hemi‐neglect using visual stimuli (optokinetic drum), cutaneous sensory stimuli (alarm bell), and auditory stimuli (using music played from a mobile phone) Control group: usual care |
|
| Outcomes |
Assessed pre‐intervention, post intervention, and 3 months post intervention |
|
| Notes | Study author reported median scores only for mRS assessments. We imputed the median for the mean and calculated SD to match t‐tests given in the paper | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Full details given |
| Allocation concealment (selection bias) | High risk | Open label |
| Blinding of participants | High risk | No details |
| Blinding of personnel | High risk | No details |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 2 dropped out of treatment group, 0 dropped out of control group |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | High risk | Baseline imbalance in NIHSS not accounted for in methods |
Song 2009.
| Study characteristics | ||
| Methods | Pilot RCT Setting: China, rehabilitation hospital | |
| Participants | Inclusion criteria: patients with right brain haemorrhage or cerebral infarction confirmed by computerised tomography (CT) or magnetic resonance imaging (MRI) and with VSN according to line cancellation and line bisection tests Exclusion criteria: recurrent stroke, epilepsy, serious heart disease, serious physical disease, in vivo metal implants such as cardiac pacemakers, increased intracranial pressure, obvious aphasia and understanding obstacles, use of tricyclic antidepressants or tranquilisers, pregnancy, younger than 18 years of age Age, years, mean: intervention = 56.14 (SD 8.9), control = 64.43 (SD 12.57) Sex (men/women): intervention = 2/5, control = 6/1 Time post stroke, days: intervention = mean 38.43 (SD 15.20), control = mean 31.57 (SD 11.47) |
|
| Interventions | Repetitive, low‐frequency stimuli were delivered with the patient lying on his or her back and the coil oriented with the handle pointing upwards. Stimulus intensity was set to 90% of the individual motor threshold and frequency was set to 0.5 Hz. The site of stimulation was the contralateral posterior parietal cortex corresponding to P3 with regard to electroencephalogram (EEG) 10–20. Each treatment session was 15 minutes long, and treatments were performed twice a day for 2 consecutive weeks. Control group received usual care | |
| Outcomes |
Study duration was 6 weeks. All participants performed line bisection and cancellation tests every 2 weeks, providing a total of 4 time points of evaluation |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding of participants | High risk | Control notably different from intervention |
| Blinding of personnel | High risk | No details given |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | “Evaluation at clinical testing was blinded”; no further detail |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Outcomes reported in equal detail |
| Other bias | High risk | Gender differences between groups |
Ten‐Brink 2017.
| Study characteristics | ||
| Methods | RCT Setting: rehabilitation centre, Netherlands | |
| Participants | Stroke patients with clinically diagnosed symptomatic stroke (first or recurrent, ischaemic, or intracerebral haemorrhagic lesion) admitted consecutively. Patients had to be aged between 18 and 85 years and had to have sufficient comprehension and communication skills. Patients were not included in cases of interfering psychiatric disorders or substance abuse, when they were physically or mentally unable to participate, or when expected discharge was < 3 weeks Age, median, years (IQR): intervention = 59.31 (14.45), control = 61.48 (13.37) Sex (men): intervention = 74%, control = 69% Hemisphere damaged: lesion side, %: intervention = left 21, right 77, bilateral 3; control = left 21, right 73, bilateral 6 Time since stroke, median days: intervention = 41.50 (39.00), control = 37.00 (37.00) | |
| Interventions | Prism adaptation or plain lenses. PA procedure was adapted from Rossetti et al. Patients wore a pair of goggles fitted with wide‐field point‐to‐point prismatic lenses, inducing an ipsilesional optical shift of 10° (PA) or goggles with plain lenses (SA). Exposure consisted of ±100 fast‐pointing movements to 3 stimuli (red, yellow, blue) presented on a horizontal axis at a distance of ±65 cm. Left and right stimuli were located 10° away from the body midline. The investigator indicated which stimulus was the target. A board was held under the chin to prevent viewing of the hand at its starting position but allowing an unobstructed view of targets and terminal errors. The co‐ordinates of the touch responses were recorded | |
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Before the start of the study, the investigator put 70 printed cards with the treatment condition (35 PA and 35 SA) in envelopes. After completion of the baseline assessment, the investigator opened an envelope and allocated the patient based on the treatment written on the card." Insufficient detail on randomisation and allocation |
| Allocation concealment (selection bias) | Unclear risk | See above |
| Blinding of participants | Low risk | Patients could not be (completely) blinded to treatment because they had to wear the goggles. However, patients were not explicitly told which treatment they had received, and none of them expressed any awareness of assigned condition (after informal enquiry) |
| Blinding of personnel | High risk | Nurses, physical therapists, and occupational therapists who filled in the CBS were blinded to treatment conditions (low risk of bias) The investigator (AFTB) who treated and tested patients regarding secondary outcomes was not blinded to treatment because she had to put on the goggles (high risk of bias) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | As above |
| Incomplete outcome data (attrition bias) All outcomes | High risk | All 4 dropouts in intervention arm |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | Nothing obvious |
Tsang 2009.
| Study characteristics | ||
| Methods | RCT Setting: rehabilitation hospital, Hong Kong | |
| Participants | 35 participants (1 dropout during the trial) Experimental: n = 17, control: n = 17 Adequacy of matching at baseline? Yes Number lost to follow‐up: 1; no details as to which group ‐ no data included in analyses Mean age, years, mean (SD): experimental = 70.47 (9.30), control = 71.82 (5.26) Sex (men/women): experimental = 12/5, control = 9/8 Time post onset, days, mean, (SD): experimental = 22.18 (15.87), control = 21.50 (21.67) Side of damage: right (experimental right 11, basal ganglia 0, other 6; control right 11, basal ganglia 2, other 4) Method of diagnosing stroke: CT or MRI Method of diagnosing neglect: BIT conventional subtest < 129 Inclusion criteria: subacute inpatients with right hemisphere stroke, undergoing rehabilitation, left visual field inattention, right‐handedness, within 8 weeks after onset of stroke, Glasgow coma scale of 15 Exclusion criteria: severe dysphasia, TIA, or reversible neurological deficit; significant impairment in visual acuity caused by cataracts, diabetic retinopathy, and glaucoma; history of other neurological disease, psychiatric disorder, or alcoholism Visual sensory deficit: visual acuity screened for; no other method of assessing visual fields, etc., noted | |
| Interventions | Right half‐field eye‐patching glasses: 4 weeks of conventional OT with right half‐field eye‐patching during OT session (conventional OT = 30 minutes ADL training and 30 minutes upper limb training using neurodevelopmental therapy ‐ this seems to be the standard procedure, rather than a record of what participants actually got; there was no mention of deviation from this amount). Other standard care received was 5 physiotherapy sessions of 60 minutes/week, speech and language therapy, and psychological counselling as indicated; skilled nursing care; daily medical round vs control (4 weeks of conventional OT as described above, without patching). Other standard care received was 5 physiotherapy sessions of 60 minutes/week, speech and language therapy, and psychological counselling as indicated, skilled nursing care, daily medical round Profession of intervention provider: OT |
|
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | "Concentrates the patients' attention on the contralesional space by blocking the ipsilesional visual field, and hence lessens the disinhibition of the orienting mechanism of the ipsilesional side resulting from interhemispheric imbalance" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomly assigned, by a designated person ... using consecutively numbered sealed envelopes for each group (according to random permuted blocks of four that were derived from the block of 4 randomisation table)" |
| Allocation concealment (selection bias) | Low risk | The designated person was the case therapist, and envelopes were prepared by a different person ‐ an OT |
| Blinding of participants | Unclear risk | States 'single‐blind' study but gives no details |
| Blinding of personnel | High risk | As stated single‐blind, safe to assume personnel were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Correspondence with study author states, "An occupational therapist, who was the blinded assessor and did not know the group allocation, was responsible for all the outcome measures, both pre and posttests", but assumption was not tested |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 1 participant dropped out but was not included in the analysis. Both baseline and outcome assessments include only the 34 who completed the study. Therefore no intention‐to‐treat analysis was performed |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Low risk | Study is free from systematic differences |
Turton 2010.
| Study characteristics | ||
| Methods | RCT, single‐blind, pilot, 2 sites Setting: hospital, UK | |
| Participants | 37 participants consented following screening; 1 person excluded post recruitment but pre‐randomisation for failing to complete assessments, so 36 randomised Experimental: n = 17, control: n = 19 Adequacy of matching at baseline? Yes, although large variation in severity of neglect Number lost to follow‐up: overall 34 of the 36 randomised remained at 4 days and 28 at 8 weeks Mean age, years, mean (SD): experimental = 72 (14), control = 71 (14) Sex (men/women): experimental = 8/8, control = 11/7 Time post onset, days, mean (SD): experimental 1 = 45 (23), control = 47 (39) Side of damage: right Method of diagnosing stroke: not specified Method of diagnosing neglect: star cancellation task and/or line bisection test of BIT Inclusion criteria: right hemisphere stroke, at least 20 days before entry to study; self‐care problems due to neglect identified by OT (from consecutive hospital admissions); ability to sit and point with the unaffected hand; ability to understand and follow instructions; medical fitness to participate Exclusion criteria: neglect prior to this stroke Visual sensory deficit: sensory score at baseline given Hemianopia: experimental = 3/16, control = 4/18 Assessed by Nottingham Sensory Assessment and confrontation | |
| Interventions | Prism adaptation training (repeated pointing movements to targets using the right 'unaffected' hand while wearing prism glasses; prism power of 10 diopters that shifted the field of view 6° to the right; training once per day, each working day for 2 weeks) vs sham treatment (same pointing procedure wearing plain glasses) Once a day for each working day for 2 weeks Profession of intervention provider: OT | |
| Outcomes |
|
|
| Notes | Conflict between proprioception and vision occurs when pointing wearing prisms and they mis‐point to the right, and there is subsequent adaptation. "Treatment triggers a realignment of the egocentric coordinate system that is responsible for the localisation of the body in space and of object position in relation to the body" Therapy and control were well tolerated, with only 1% and 3%, respectively, of sessions missed by participants due to illness |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A secretary who was located outside of the stroke services administered the randomisation procedure |
| Allocation concealment (selection bias) | Low risk | "A minimisation method using a 4:1 element of chance was implemented and automated using Microsoft Excel for pseudo‐random allocation to groups" The participant’s group was revealed, via telephone, to the occupational therapist who delivered the intervention |
| Blinding of participants | High risk | Prism lenses; sham not convincing |
| Blinding of personnel | High risk | See above |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Outcome assessments were carried out with assessors blind to group allocation" but not evidenced |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts accounted for |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | Nothing obvious |
Van Wyk 2014.
| Study characteristics | ||
| Methods | RCT Setting: rehabilitation centre, South Africa | |
| Participants |
Exclusions
Age: not reported Sex: not reported Hemisphere damaged: not reported Time since stroke: not reported |
|
| Interventions | Group 1 received saccadic eye movement training with visual scanning exercises integrated with task‐specific activities; group 2 received task‐specific activities only. Only the guideline of the interventions is given because principles were adapted to each participant’s functional ability. VSEs integrated with task‐specific activities consisted of dual‐task activities, which require the ability to allocate information‐processing resources between 2 tasks, and to maintain sufficient attention on visual scanning task during dual‐task performance | |
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Participants were matched and allocated on the basis of their scores on the SAS to ensure that participants in the 2 groups were comparable with regard to their level of functional activity. The first participant who was eligible for participation in the study was allocated to group 1 (experimental group). Participants who matched a previous participant’s score on the SAS were automatically placed in the second group (control group). If a participant had a score that did not match another participant’s SAS score, the participant was randomly allocated to either group 1 or group 2 using a formula on a Microsoft Excel programme to randomly allocate participants. The allocation process was repeated until 12 participants had been allocated to each group |
| Allocation concealment (selection bias) | High risk | As above |
| Blinding of participants | Low risk | Participants from group 1 and group 2 were blinded to the group they were assigned to. Participants in groups 1 and 2 were treated in separate venues to control blinding of participants throughout the study |
| Blinding of personnel | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | To ensure reliability of research data, a skilled assessor who was blinded to groups conducted all assessments of participants in the trial |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | If a participant dropped out of the study for any reason, another participant was recruited to replace him or her during the 4 weeks of the study |
| Selective reporting (reporting bias) | Low risk | All 3 outcomes results reported in detail. No primary? |
| Other bias | Low risk | No statistical difference was noted between groups at baseline (P = 0.24). Based on interpretation of the SAS, the motor function of participants from group 1 and group 2 was similar at the beginning of the intervention period. It can be concluded that the 2 groups were comparable to each other regarding motor function and level of functional activity prior to intervention |
Varalta 2019.
| Study characteristics | ||
| Methods | Single‐center, pilot RCT Setting: Italy | |
| Participants | Inclusion criteria: age > 18 years; presence of ischaemic or haemorrhagic stroke (as documented by computerised tomography or magnetic resonance imaging scan) that had occurred at least 6 months earlier; presence of hemi‐spatial neglect (Star Cancellation Test score < 50); ability to actively rotate the head toward the left in a closed‐eyes condition (absence of musculoskeletal disorders) Exclusion criteria: participation in other trials; dementia (Mini Mental State Examination correct score < 23.80); presence of severe comprehension deficits, psychiatric disorders, deficits of somatic sensation involving the cervical dermatome map (C3–C5), or visual field deficits as assessed by neurological examination; other neurological or orthopaedic conditions involving the neck and visual ability Age, years, mean (SD): intervention = 65.5 (10.2), control = 67.0 (11.5) Sex (men/women): intervention = 2/5, control = 4/1 Hemisphere damaged: not reported Time since stroke, mean months (SD): intervention = 19.7 (27.7), control = 28.0 (40.6) |
|
| Interventions | Neck taping or sham neck taping. For the intervention group, tape was placed according to Kenzo Kase's Kinesio Taping Method by an experienced physiotherapist. The tape strip was applied from the mastoid bone to the clavicle (rostrocaudal direction) with the sternocleidomastoid kept in a position of maximum stretching. Two I‐strips were applied: the first placed on the medial (sternal) head, and the second on the lateral (clavicular) head, of the sternocleidomastoid muscle, with 15% to 25% tension (paper‐off tension) For the control group, smaller I‐strips were used. To eliminate the specific therapeutic elements of elastic taping (i.e. longitudinal stretch, start and ending points of tape application), the strips were applied. All patients wore the tape for 30 days |
|
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Balanced (restricted) randomisation scheme”; only detail |
| Allocation concealment (selection bias) | Low risk | We used an allocation concealment mechanism (sequentially sealed numbered containers). Another investigator checked for correct patient allocation according to the randomisation list. After unmasking at the end of the study, we checked that no allocation errors had been made |
| Blinding of participants | Unclear risk | All participants were taped by the same investigator, who was not involved in the outcome assessment |
| Blinding of personnel | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All patients were evaluated by the same investigator, who was blinded to group allocation. The success of blinding was tested by asking the assessor to make an educated guess |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None |
| Selective reporting (reporting bias) | Low risk | Outcomes reported with equal detail |
| Other bias | Low risk | Nothing obvious |
Vatanparasti 2019.
| Study characteristics | ||
| Methods | RCT, pilot Setting: Iran, stroke unit | |
| Participants | Stroke patients with neglect, diagnosis of whom was verified by magnetic resonance imaging and clinical examination, right‐handed Age, years: intervention 1 PA = 65.5 ± 10.2, intervention 2 PA + cTBS = 67.5 ± 8.4 Sex (men/women) no. (%): intervention 1 PA = 5 (70), 2 (30); intervention 2 PA + cTBS = 5 (70), 2 (30) Time since stroke onset, no unit of measurement specified: subacute no. (%): intervention 1 PA = 3 (42.9), intervention 2 PA + cTBS = 3 (42.9) Time since stroke onset, no unit of measurement specified: chronic no. (%): intervention 1 PA = 4 (57.1), intervention 2 PA + cTBS = 4 (57.1) | |
| Interventions | Prism adaptation + cTBS Intervention 1: all patients were asked to wear a pair of prism glasses with a rightward prismatic shift of 10° when patients were asked to actively move their intact hand in front of a vertical mirror box for 20 minutes. Sham TMS followed the same protocol except the coil was positioned at a 90° angle to the skull, and a small part of the coil was resting on the skull Intervention 2: in addition to prisma adaptation, 1 group of patients received 10 sessions of TMS over the intact left posterior parietal cortex |
|
| Outcomes |
Assessed pre‐intervention and post intervention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants | Low risk | “Patients were unaware of the group assignments; they were informed that they are going to undergo the treatment for their visuospatial neglect of left side of their body” |
| Blinding of personnel | High risk | However, therapist was aware about patients’ group allocation |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No details given |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No details given |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Low risk | Nothing obvious |
Volkening 2016.
| Study characteristics | ||
| Methods | Double‐blind RCT Setting: clinic, Germany | |
| Participants | 29 first‐ever right hemispheric, right‐handed stroke patients with signs of left‐sided spatial neglect (age 18+) Cathode left = 8, cathode right = 8, sham = 8 Neglect test: according to a cutoff score criterion of ≤ 135 for mild neglect or suspicion of neglect on the Neglect test (NET, adapted German version of the BIT) Age, mean (range): cathode left = 71 (55 to 80), right = 73 (61 to 83), sham = 70 (45 to 82) Sex (men/women): cathode left = 2/6, right = 4/4, sham = 4/4 Days between stroke and treatment, mean (range): cathode left = 1.9 (1.1 to 3.9), right = 1.3 (0.4 to 2.2), sham = 1.0 (0.7 to 1.5) Exclusion: any metal implants; brain tumour, previous epileptic seizure, craniotomy, degenerative or psychiatric disorder, unable to perform the NET | |
| Interventions | As standardised therapy, all patients received smooth pursuit eye movement training (SPT) and visual scanning training (VST). Both training programmes were presented on a 14.1‐inch laptop monitor (60 Hz refresh rate). For SPT, computer‐generated random displays of 350 dots (blue on a white background) moving coherently towards the left hemi‐space (speed: 6.9°/s) were presented. Patients were instructed to look at the displays and to make smooth pursuit eye movements towards the direction of motion and return to the rightward side of the screen whenever they had reached the leftward border of the screen. For VST, different training exercises from the therapy programme Cogpack were used to facilitate exploration of the left hemi‐space. VST programmes and their difficulty levels were adjusted individually depending on each patient’s capabilities. In each session, patients first received 2 to 4 runs of SPT, followed by VST Simultaneously, patients received GVS or sham stimulation. Bilateral bipolar GVS was delivered by a battery‐driven, direct current stimulator (neuroConn Ilmenau, Germany). Two electrodes (anode and cathode) were inserted into natrium‐chloride‐soaked sponges (30 cm² each) and placed over both mastoids. Polarity placements were changed for each of the 3 stimulation conditions: for CL‐G VS, the cathode was placed on the left and the anode on the right mastoid. This electrode setup was reversed for CRGVS. For CL‐ and CR‐GVS, the current was ramped up (in steps of 0.1 mA/s) to 1.5 mA, kept there for 20 minutes, and ramped down again (in steps of 0.1 mA/ s). Conforming to established safety limits, patients were stimulated for only 20 minutes with a current intensity of 1.5 mA. Apart from the intervention, patients received occupational therapy and physiotherapy but no other specific neglect training |
|
| Outcomes | Primary outcome measures
Secondary outcome measures: subjective visual (SVV) and haptic vertical (SHV) were used to assess verticality perception. All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 17 out of 24 patients were randomly allocated to treatment groups by the research co‐ordinator, who drew cards from a sealed envelope. Since patients with more severe spatial neglect might respond differently to interventions than those with milder impairments, we allocated 7 patients using minimisation (see Scott, McPherson, Ramsay, & Campbell, 2002, for further details). Minimisation was based on NET scores. The NET score range for inclusion was subdivided into 3 strata: 0 to 45, 46 to 90, 91 to 135. Minimisation was performed by a post‐doctoral researcher otherwise not involved in the study |
| Allocation concealment (selection bias) | Low risk | See above |
| Blinding of participants | Low risk | Patients were also blinded to the allocated add‐on intervention (GVS) |
| Blinding of personnel | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Outcome measures were assessed by trained neuropsychologists, masked to treatment allocation and not otherwise involved in patients’ treatment." Assumption of unawareness was not tested |
| Incomplete outcome data (attrition bias) All outcomes | High risk | For SVV and SHV, there were more missing data points because some patients were not able to perform tasks at baseline (in total, SVV = 9; SHV = 5) due to impaired comprehension. Baseline measurements were therefore substituted with the group mean. Except for 1 case, all patients were able to perform the tasks after the intervention. Accordingly, LOCF was applied for missing data for the following time points |
| Selective reporting (reporting bias) | Unclear risk | Several primary outcomes |
| Other bias | High risk | Use of LOCF |
Welfringer 2011.
| Study characteristics | ||
| Methods | RCT, designed as a feasibility study Setting: Germany | |
| Participants | 30 participants with right hemisphere stroke, less than 6 months previously Inclusion criteria: diagnosis of right hemispheric stroke dated less than 6 months earlier; no history of major psychiatric problems and no other coexisting disease/disability; showed unilateral left visuospatial neglect symptoms as defined by a score ≤ 54 on the Letter Cancellation Test; no diagnosis of hemianopia; sufficient sensory, physical, and cognitive capacities to follow instructions for more than 30 minutes and no additional verbal‐memory deficits as defined by a percentage rank > 16 in the story recall subtest of the Wechsler Memory Scale‐Revised (WMS‐R); aged between 20 and 75 years; right‐handed; provided informed consent Experimental: n = 15; mean age = 56.3 years (SD 11.2); mean time since stroke = 3.2 months (SD 1.5) Control: n = 15; mean age = 57.3 years (SD 11.3); mean time since stroke = 3.4 months (SD 2.8) | |
| Interventions | Visuomotor‐imagery therapy (2 daily half‐hour sessions of visuomotor‐imagery therapy as add‐on treatment over a period of 3 weeks; participants mentally practised positions and movements of the contralesional upper limb in a repetitive fashion and as vividly and intensively as possible; over the course of the 3‐week intervention period, they participated in 28 to 30 training sessions; a total of 4 positions and 6 sequences (simple and complex movements) were imagined, with 1 exercise repeated up to 10 times per session) vs no supplementary intervention All participants received standardised rehabilitation therapies including 45 minutes of exploration training 4 times per week |
|
| Outcomes |
Measured immediately post treatment For analyses within this review, we used neglect ‐ Bells Cancellation test |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation sequences have been generated by study personnel prior to beginning the trial using a web‐based randomisation generator (http://www.randomization.com) |
| Allocation concealment (selection bias) | Low risk | Blocked randomisation, in blocks of 10; computer‐generated sequence, delivered by person independent of intervention |
| Blinding of participants | High risk | Impossible to blind |
| Blinding of personnel | High risk | Impossible to blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | States: "outcome measures were assessed by a blinded tester." although no detail given |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All reported with equal detail |
| Other bias | Low risk | Nothing obvious |
Wiart 1997.
| Study characteristics | ||
| Methods | RCT Setting: hospital, France | |
| Participants | 22 people within 3 months of onset of stroke and severe left unilateral neglect, hospitalised in 2 neurorehabilitation hospitals, positive for neglect on 3 tests (see Outcomes) Experimental: n = 11, control: n = 11 Mean age, years: experimental = 66, control = 72 Sex (men/women): experimental = 6/5, control = 6/5 Time post onset, mean days: experimental = 35, control = 30 Exclusions: history of stroke, alteration of general status, cognitive difficulties incompatible with rehabilitation | |
| Interventions | 1 hour per day for 20 days of experimental treatment followed by traditional rehabilitation (1 to 2 hours physiotherapy and 1 hour OT); experimental treatment is Bon Saint Come method: participant wears a thoracolumbar vest with attached metal pointer above the head; participant points to target on mobile wooden panel; audible and luminous signals provide biofeedback effect when targets are touched; initially conducted when sitting, this progresses to standing; the therapist participates actively during the session, stimulating, guiding, and correcting vs 3 to 4 hours of traditional rehabilitation per day | |
| Outcomes | Study collected 2 types of outcomes
These assessments were conducted 3 times: Day 0, Day 30 (after therapy), and Day 60 This review used only data from line bisection and FIM. Both 30‐day (immediate) and 60‐day (persisting) data were used in this review |
|
| Notes | The paper consists of 2 studies. These data refer to Study 1 only The experimental group was younger and had a higher initial FIM score (66) than the control group (54) Cancellation data were reported as errors rather than correct performance. Only 1 set of cancellation data (lines not bells) were entered in this review to avoid entering the same group of participants twice into the meta‐analysis Line bisection scores are % deviation to the right Control group had more, but not significantly so, omissions on line cancellation (control 16, experimental 14) and right deviations on line bisection (control 53%, experimental 50%) at baseline compared with experimental group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | They were randomly divided into 2 groups (using a randomisation table) |
| Allocation concealment (selection bias) | High risk | Information on allocation concealment unclear; random number tables |
| Blinding of participants | High risk | No detail given; participants unlikely to be blinded due to nature of intervention |
| Blinding of personnel | Unclear risk | No detail given |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. Assessment done by 'one of us (LW)'; different from person delivering therapy |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No incomplete data |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | High risk | Control group older and more disabled – no correction made |
Wilkinson 2014.
| Study characteristics | ||
| Methods | RCT Setting: rehabilitation units, UK | |
| Participants | Inclusion criteria
Exclusion criteria
Age, years, mean (SD): group 1 = 66.9 (10.6), group 2 = 66.0 (9.37), group 3 = 65.7 (8.72) Sex (women/men): group 1 = 3/12, group 2 = 6/12, group 3 = 3/13 Hemisphere damaged: right Time since stroke, days (median IQR): group 1 = 68 (39 to 229), group 2 = 75 (41 to 479), group 3 = 94 (39 to 534) |
|
| Interventions | Repeated sessions of galvanic vestibular stimulation. Participants received 1, 5, or 10 sessions, each lasting 25 minutes, of subsensory, left‐anodal right‐cathodal noisy direct current (mean amplitude = 1 mA) | |
| Outcomes |
Taken up to 1 month post intervention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was conducted using a secure, remote randomisation facility independent of the research team |
| Allocation concealment (selection bias) | Low risk | See above |
| Blinding of participants | Low risk | Treatment allocation was double‐blind; since GVS was subsensory, participants did not know their allocation, and a stimulation protocol (active or sham) pre‐determined by the randomisation officer was naively administered by the experimenter by typing a 4‐digit code (which changed every time) into the stimulation device. Participants’ in‐patient neglect treatment (typically visual scanning therapy but sometimes limited to informal reminders given by occupational therapy staff to look left during functional activities) was suspended while they remained on‐study |
| Blinding of personnel | Low risk | See above |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | BIT and BI were administered by the experimenter |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2, 1, 0 dropouts in each arm |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | No evidence of this |
Wu 2013.
| Study characteristics | ||
| Methods | Single‐blinded, randomised pre‐test and post‐test control group design Setting: rehabilitation clinics and medical centres, Taiwan | |
| Participants | 27 patients with right side cerebral stroke and neglect CIT + EP = 9, CIT = 9, control = 9 Neglect definition: results on 2 or more of 4 tests (double simultaneous stimulation test, line bisection test, random shape cancellation test, random Chinese word cancellation test) Age, years, mean (SD): CIT + EP = 56.1 (14.5), CIT = 65.5 (9.8), control = 61.3 (11.2) Sex (men/women): CIT + EP = 5/2, CIT = 5/3, control = 7/2 Time between stroke and treatment, months, mean (SD): CIT + EP = 13.0 (13.9), CIT = 10.1 (10.4), control = 13.7 (14.1) Exclusion: no excessive spasticity in the affected arm, including shoulder, elbow, wrist, and fingers; no severe cognitive impairment by showing awareness and ability to respond to oral instructions; no severe impairment of visual acuity after rectification; no participation in any experimental rehabilitation or drug studies during the study period | |
| Interventions | All participants received 2 hours of therapy, 5 days/week for 3 weeks, with 1‐to‐1 supervision. Interventions were provided at participating hospitals by occupational therapists who were trained in administration of the 3 protocols by investigators and who completed a written competency test before they administered treatment. Treating therapists were not blinded to group allocation. All other routine rehabilitation, such as physical therapy or speech therapy, proceeded as usual Constraint‐induced therapy (CIT) + eye‐patching (EP) group. Participants in this group received CIT + EP. CIT addressed forced use of the affected UE and restricted the unaffected UE during training. Shaping skills were delivered while participants were forced to use their affected UE in the mass practice of functional tasks such as drinking water and opening a jar. Participants wore a mitt on their unaffected hand and wrist for 6 hours/d during the 3‐week training and reported their compliance in a daily log. Home skill activities were assigned to promote this training in daily life, and problems were discussed to aid participants in overcoming barriers they encountered. Participants were also asked to wear glasses with a patch on the right lens to block the visual stimuli from the right side and to force them to receive stimuli from the left visual field. CIT group. The intervention in the CIT group resembled the intervention in the CIT + EP group, except participants did not wear the EP glasses Control group. The control group received traditional occupational therapy matched in intensity and duration with that of the other groups. The training programme for the affected UE included stretching and weight bearing, improving range of motion, muscle strengthening, and practising tasks used for functional training that might involve the unaffected UE assisting the affected UE, for example, stabilising a bottle while opening its lid or moving pegs into holes on a board Control group received usual care |
|
| Outcomes |
All taken immediately post intervention with no longer‐term follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Eligible participants were randomly assigned to CIT + EP, CIT, or conventional intervention in accordance with a random number table. When a new participant was enrolled, the study co‐ordinator gave a sealed opaque envelope identifying the participant’s group to therapists, and they were informed of group allocation and delivered therapy accordingly |
| Allocation concealment (selection bias) | Low risk | See above |
| Blinding of participants | High risk | Single‐blinded |
| Blinding of personnel | High risk | Treating therapists were not blinded to group allocation |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Three certified occupational therapists blind to group allocation were trained to provide the evaluations before and after a 3‐wk intervention. The same rater administered all the study measurements to each participant at baseline and after the 3‐wk intervention." Not enough detail to evidence lack of communication between team members |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 dropped out of one group, 1 from another |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | Nothing obvious |
Yang 2015.
| Study characteristics | ||
| Methods | Pilot RCT Setting: Taiwan, patients receiving routine rehabilitation | |
| Participants | Inclusion criteria: patients between 18 and 80 years of age; (2) first‐stroke patients (cerebral infarction or haemorrhage) confirmed by computed tomography (CT) or magnetic resonance imaging (MRI) and in recovery time within 60 to 180 days; (3) USN confirmed by line bisection test, star cancellation test, or clinical examination; (4) patients without serious heart, lung, and kidney disease or epilepsy; (5) patients without metallic implant of diamagnetic substance Age, years: intervention 1 = 46.72 ± 13.11, intervention 2 = 48.01 ± 12.25, intervention 3 = 49.45 ± 10.78, control = 47.70 ± 11.81 Sex (number of men): intervention 1 = 6, intervention 2 = 4, intervention 3 = 5, control = 7 Time since stroke: within 60 to 180 days | |
| Interventions | rTMS Intervention 1: stimulation parameter in the 1‐Hz group was 1 Hz, and stimulus duration for each sequence was 8 seconds; repeated 82 sequences with a total of 656 pulse number Intervention 2: stimulation frequency in the 10‐Hz group was 10 Hz, with a total pulse number of 1000 and stimulation interval of 55 seconds Intervention 3: continuous TBS group parameter was 801 pulses, in bursts of 3 pulses at 30 Hz, repeated every 100 milliseconds (5 Hz, θ rhythm) Control: sham stimulation | |
| Outcomes |
2 weeks before treatment (designated as time point 1), beginning of treatment (time point 2), end of treatment (time point 3), 1 month after treatment (time point 4) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail given |
| Allocation concealment (selection bias) | Unclear risk | No detail given |
| Blinding of participants | Unclear risk | No detail given |
| Blinding of personnel | High risk | No detail given |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Mentions assessor was blinded, although unclear if blinding achieved |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Although tables for 2 out of 3 outcomes are presented (the significant 2), unsure if this constitutes high bias |
| Other bias | Low risk | No evidence of this |
Yang 2015 10Hz.
| Study characteristics | ||
| Methods | See Yang 2015 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail given |
| Allocation concealment (selection bias) | Unclear risk | No detail given |
| Blinding of participants | Unclear risk | No detail given |
| Blinding of personnel | High risk | No detail given |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Mentions assessor was blinded, although unclear if blinding achieved |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropout |
| Selective reporting (reporting bias) | Low risk | Although tables for 2 out of 3 outcomes are presented (the significant 2), unsure if this constitutes high bias |
| Other bias | Low risk | No evidence of this |
Yang 2015 1Hz.
| Study characteristics | ||
| Methods | See Yang 2015 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Yang 2015 cTBS.
| Study characteristics | ||
| Methods | See Yang 2015 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Yang 2017.
| Study characteristics | ||
| Methods | RCT Setting: China, rehabilitation ward | |
| Participants | Inclusion criteria: (1) diagnosis of right hemispheric stroke through neurological examination and CT or MRI scans; (2) duration since onset longer than 1 week; (3) presenting with unilateral neglect confirmed by conventional subtests of the Behavioural Inattention Test with cutoff score of 129; (4) unilateral neglect as a result of recent acute stroke; (5) aged 18 or over; (6) Mini Mental State Examination score > 17.1 Age, years, mean: all participants = 58.0 ± 12.3 Sex (men/women): intervention 1 = 14/6, intervention 2 = 12/8, control = 17/ 3 Time post stroke, days: intervention 1 = 36.6 ± 33.2, intervention 2 = 37.5 ± 26, control = 42.5 ± 30.6 | |
| Interventions | Intervention 1: rTMS and sensory cueing groups were exposed to low‐frequency repetitive magnetic pulses generated by the TMS stimulator for 2 weeks. Patients were asked to wear the sensory cueing device on their left wrist for 3 hours a day, 5 times a week, over the 2 weeks. The cue was given every 5 minutes in the form of vibration (196 Hz, similar to the vibration of a cell phone) generated from the device; participants were required to press the acknowledgement button on the device to stop the cueing each time it was emitted Intervention 2: rTMS only Control: usual care | |
| Outcomes |
Measured up to 1 month post intervention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation table according to random permuted blocks of 4 |
| Allocation concealment (selection bias) | Unclear risk | Allocation‐to‐treatment sequences were concealed from all investigators responsible for carrying out the training or from patients involved |
| Blinding of participants | High risk | No detail given |
| Blinding of personnel | High risk | No detail given |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Investigators were blinded from all assessments carried out; unknown how this worked in practice |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1, 1, and 2 lost in each group |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | Nothing obvious |
Yi 2016.
| Study characteristics | ||
| Methods | RCT Setting: South Korea, hospital | |
| Participants | 30 participants with left visuospatial neglect diagnosed as right cerebral ischaemic or haemorrhagic stroke 10 anodal, 10 cathodal, 10 sham Mean age, years: anodal = 63, cathodal = 62, sham = 62 Sex (men/women): anodal = 7/3, cathodal = 8/2, sham = 6/4 Cause of neglect (haemorrhagic/ischaemic): anodal = 1/9, cathodal = 1/9, sham = 2/8 Neglect defined as > 6.33 mm average deviation from the centre line on the line bisection test (LBT) Exclusions: severe cognitive dysfunction or aphasia, contraindications for tDCS, systemic disease, ongoing neoplasia | |
| Interventions | Transcranial direct current stimulation (tDCS) applied over posterior parietal cortex: anodal, cathodal, or sham 15 sessions of tDCS. Sessions were 5 times per week for 3 weeks. A direct current was delivered by 2 sets of battery‐powered devices using 2 pairs of saline‐soaked sponge electrodes(5 cm × 5 cm). Stimulation was delivered while the patient was receiving conventional occupational therapy All patients received conventional physical therapy throughout the duration of the 3‐week tDCS protocol | |
| Outcomes |
Assessed pre‐treatment and post treatment |
|
| Notes | We entered this study into meta‐analysis as 2 studies: Yi (2016) anodal, and Yi (2016) cathodal | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were identified by a number assigned by a centralized computer‐generated randomization code" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient detail to confirm |
| Blinding of participants | Low risk | "Sham stimulation was performed in the same way as active stimulation, but the stimulator was turned off after 30 seconds. This ensured that subjects could feel the initial itching sensation at the beginning of tDCS and allowed for a successful blinding of the subjects to their stimulation condition" |
| Blinding of personnel | High risk | "Sham stimulation was performed in the same way as active stimulation, but the stimulator was turned off after 30 seconds" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropout seemingly |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | Nothing obvious |
Yi 2016 anodal.
| Study characteristics | ||
| Methods | See Yi 2016 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were identified by a number assigned by a centralized computer‐generated randomization code" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient detail to confirm |
| Blinding of participants | Low risk | "Sham stimulation was performed in the same way as active stimulation, but the stimulator was turned off after 30 seconds. This ensured that subjects could feel the initial itching sensation at the beginning of tDCS and allowed for a successful blinding of the subjects to their stimulation condition" |
| Blinding of personnel | High risk | "Sham stimulation was performed in the same way as active stimulation, but the stimulator was turned off after 30 seconds" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropout seemingly |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Low risk | Nothing obvious |
Yi 2016 cathodal.
| Study characteristics | ||
| Methods | See Yi 2016 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Zeloni 2002.
| Study characteristics | ||
| Methods | RCT Setting: Italy | |
| Participants | 8 randomised (see Notes) Experimental: n = 4, control: n = 4 Mean age, years: experimental = 68.8, control = 76.3 Sex (men/women): experimental = 4/0, control = 2/2 Mean months post stroke: experimental = 11.25, control = 4.5 Inclusion: "post‐acute" patients with right hemisphere vascular lesions and neglect, admitted to hospital, right‐handed, left hemiplegic Exclusions: normally wore glasses | |
| Interventions | Wearing plastic goggles for 1 week, removing them only to go to sleep (the right side of each lens was blinded) vs no goggles All 8 participants were involved in the hospital's daily activities including usual treatment for neglect, tasks to train compensation for faulty scanning | |
| Outcomes | Participants were assessed on 3 occasions: at recruitment, after the experimental group had received 1 week of hemi‐blinding goggles, and again 1 week after goggle treatment ended. Controls were assessed at the same time points but never wore the hemi‐blinding goggles. Testing was performed without goggles. Outcomes used were line, letter, and bell cancellation, copy drawing, line bisection For this version of the review, we used single letter cancellation outcome data only. We used data from the third time point; as this was only 1 week after intervention; it is coded in this review as 'immediate' effects | |
| Notes | Personal communication from study authors confirmed the methods used and provided data. The 8 randomised participants are numbers 1 to 4 in treatment and control groups as listed in the study authors' Table 9, page 196. The original study recruited 11 participants. The first 8 were randomised as described above. The other 3 were non‐randomly added to the groups (1 to treatment and 2 to control). This review used only the 8 randomised participants Cancellation tests were scored as number correct. Line bisection was scored as % correct, decreasing for rightward deviation. Study authors provided raw data (%) for the 8 participants on line bisection. Mean (SD) values were as follows: experimental = 62.5 (35.2), control = 73.8 (22.2). These data were used in the 2006 version of this review, but for this version, the number of neglect outcomes was reduced and the line bisection data removed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | See below |
| Allocation concealment (selection bias) | High risk | For the first 8 participants, group allocation was performed by randomly selecting a label from a pre‐printed set of 8 (see Notes). Label preparation was performed by a member of the trial team, but selection was performed by a student who had no previous or later involvement in the trial. Although allocation was done externally, the method used did not permit verification |
| Blinding of participants | High risk | Blinding not possible |
| Blinding of personnel | High risk | Blinding not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcomes |
| Selective reporting (reporting bias) | Low risk | Outcomes reported equally |
| Other bias | Unclear risk | No baseline adjustments made ‐ controls seem somewhat older, although sample was very small |
ADL: activities of daily living. ASMP: auditory subjective median plane. BI: Barthel Index. BIT: Behavioural Inattention Test. CBS: Catherine Bergego Scale occupational therapist’s evaluation score. cm: centimetre. CT: computerised tomography. CVA: cerebrovascular accident. FA: functional approach. FAI: Frenchay Activities Index. FIM: Functional Independence Measure. FT: feedback training. GHQ: General Health Questionnaire. GVS: Galvanic Vestibular Stimulation. HFVS: Harrington Flocks Visual Screener. HHA: homonymous hemianopia. HI: head injury. IQR: interquartile range. LAT: limb activation training. LBT: line bisection test. mm: millimetre. MMSE: Mini Mental Status Exam. MVPT: Motor‐Free Visual Perception Test. N/A: not applicable. Nottingham EADL: extended ADL index. OKS: optokinetic stimulation. OT: occupational therapy/therapist. RBD: right brain damage. RCPM: Raven's Coloured Progressive Matrices. RCT: randomised controlled trial. Rey CFT: Rey Osterreith Complex Figure Test. RH: right hemisphere. RMA: Rivermead Motor Assessment. RPAB: Rivermead Perceptual Assessment Battery. rTMS: repetitive transcranial magnetic stimulation. SCT: star cancellation test. SD: standard deviation. SEM: standard error of the mean. SIAS: Social Interaction Anxiety Scale. SIS: Stroke Impact Scale. SU: stroke unit. tDCS: transcranial direct current stimulation. TENS: transcutaneous electrical nerve stimulation. TIA: transient ischaemic attack. ToT: transfer of training. VN: visual neglect. WAIS‐R: Revised Weschler Adult Intelligence Scale. WMFT: Wolf Motor Function Test. WRAT: Wide Range Achievement Test.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Akinwuntan 2010 | Study does not include a neglect population. It is a study of 3 types of attention problems (selective attention, divided attention, speed of processing) that would affect driving ability. Refers to visual problems, but these are not neglect. No neglect measures are used |
| Al Mahasneh 1991 | Extreme difficulties with recruitment and participant attrition. 14 participants with neglect consented. These were unevenly assigned to experimental (9) and control (5) groups. Only 5 participants completed 3 weeks of treatment. Review authors did not feel the data were adequate for meta‐analysis, e.g. missing data, no SDs |
| Angeli 2004 | Not an RCT |
| Bar‐Haim 2011 | The method of allocation was not fully randomised. Clarification from study author stated, "the first individual was assigned randomly to 1 of the 3 groups (by assigning numbers to the groups, 1‐3, and drawing a number for that patient). From that point on, each new participant was assigned to the next group consecutively" |
| Beis 1999 | Controlled trial but not RCT: allocation by fixed order of presentation of participants, i.e. first to group 1, second to group 2, etc. Outcome assessors were blinded to allocation. Personal communication provided FIM data, confirmed allocation method, and revealed that assessments were carried out by 2 blinded researchers |
| Butter 1992 | Clarification of randomisation sought but not obtained. Appropriate results (means and SDs) not reported. Review authors were not sure that the trial was actually evaluating a treatment for spatial neglect |
| Carter 1980 | Clarification of randomisation sought but not obtained. Separate data for stroke patients also requested but not obtained. Appropriate data (means, SDs) not reported |
| Chen 2014 | Clarification of randomisation sought; study author confirmed allocation not randomised |
| Cubelli 1993 | Identified as a potential RCT of spatial neglect for the 2006 version. As further information could not be obtained, this was added to studies awaiting classification. As further details have still not been obtained, it has been moved to Excluded studies. We will re‐consider this study for inclusion if further information becomes available |
| Diller 1974 | Reported data inadequate for review. No reply to our letter of 9 February 1999, asking for difficult‐to‐extract data |
| EEG‐NF 2009 | Not a cognitive rehabilitation approach |
| Facchin 2019 | Cross‐over |
| Frassinetti 2002 | Controlled clinical trial: non‐random allocation (n = 13). Controls at different hospital. Assessment of outcomes not clear (probably non‐blind) |
| Gordon 1985 | Controlled trial: quasi‐randomisation based on rehabilitation service to which participant was assigned. Experimental and control conditions alternated every 6 months between the 2 services. Not randomised |
| Harvey 2003 | Controlled trial: non‐randomised, initial recruits allocated by date of admission to hospital ward, later recruits allocated by attempting to match groups on their scores on pre‐intervention neglect assessments. Study author provided clarification and unpublished data by personal communication |
| Harvey 2010 | Not an RCT |
| Jacquin‐Courtois 2010 | Did not collect outcomes of relevance to this review |
| Kang 2009 | Not specific to neglect |
| Keller 2006 | Although the English abstract states that participants were "randomly assigned", the full German paper does not state random allocation, and it appears that this study is not a randomised study |
| Keller 2009 | Cross‐over |
| Kerkhoff 2005 | Not randomised. States that participants were "consecutively collected and matched for clinical and demographic variables as well as neglect severity" and "all subjects were treated in a single‐subject baseline design" |
| Kerkhoff 2012b | The intervention involved a single treatment session (i.e. this was not a rehabilitation programme) |
| Klos 2005 | Personal communication from an expert in the field reported that Klos had completed an unpublished RCT of prism adaptation therapy for neglect. Excluded from review, as no reply to request for clarification of methods and data. Will reconsider for inclusion in next update if further information becomes available |
| Ladavas 2013 | Not randomised |
| Lesniak 2013 | Not neglect |
| Lincoln 1985 | RCT of patients with general perceptual problems. Problems are likely to have included neglect, but this subgroup could not be separately identified |
| Loverro 1988 | Controlled trial: reported as randomly assigned but allocation based on bed availability; outcome assessors blinded to purpose of the study |
| Nakamura 2015 | Cross‐over |
| Niemeier 1998 | Controlled trial: not randomised, selected in order of consecutive admissions and on documented left or right neglect. No information on concealment |
| Osawa 2010 | No mention of randomisation and appears that group allocation was based on whether or not they happened to have family |
| Paolucci 1996 | Controlled trial: abstract states randomly assigned but allocated on the basis of bed number (odd or even); bed number had been assigned by Hospital Administration; odd numbers got immediate training, even numbers got training after 2 months (delayed training); neglect screening assessment done after allocation by psychologist unaware of purpose of study; outcome assessor blinded to purpose of the study; after 8 weeks, the delayed group received training and the immediate group received control treatment (broad cognitive stimulation) |
| Patole 2015 | No comparison group, pre‐post study |
| Pizzamiglio 2004 | Non‐random controlled trial (n = 22): alternate allocation. Blind assessment of outcome on BI (functional outcome). Not clear if outcome assessed blind on impairment measures |
| Rossetti 1998 | Controlled trial: further data from study author confirm it was not randomised. First 6 consecutive cases were allocated to experimental group and next 6 to control. Outcome assessors were not blinded. The trial is the second of 2 experiments reported in the paper |
| Rossetti 2005 | Ongoing pharmacological study |
| Rossi 1990 | Less than 50% of participants had neglect |
| Schindler 2002 | Non‐randomised cross‐over controlled trial. First 10 participants were randomised to 1 of 2 groups, but the data on these 10 were not available at the time of this version of this review. It would be considered for inclusion at the next update if study authors could provide randomised data |
| Schmidt 2013 | Cross‐over |
| Serino 2006 | Not randomised |
| Serino 2009 | Non‐randomised controlled trial. After the first 5 participants, allocation is by alternation in blocks of 4 |
| Svaerke 2019 | Cross‐over |
| Tham 1997 | Non‐random controlled trial. First 7 participants assigned to novel treatment group, second 7 participants to conventional treatment group |
| Toglia 2009 | RCT of assessment methods ‐ dynamic vs static |
| Trudell 2003 | Published abstract suggested this may be an eligible study. Excluded from review, as no information with which to confirm methods. No further information has become available |
| Turgut 2018 | Cross‐over |
| Vaes 2016 | Communication with study author confirmed study not randomised: “We did not look at the nature of neglect for assigning patients to the experimental or control group. Because the time post‐stroke could be a factor that influences treatment results, we took the number of days post‐stroke into account and tried to match this between the groups. However we did not use a tool or statistical method” |
| Van Kessel 2013 | Cross‐over |
| Van Os 1991 | Not randomised (confirmed by native Dutch speaker) |
| Van Puymbroeck 2014 | Not specific to neglect, not an RCT |
| Webster 2001 | Controlled clinical trial: 40 assigned, 1 excluded, and matched participant excluded, n = 38. 20 controls were from a previous study, not simultaneous. Non‐blind assessment of outcomes. Wheelchair navigation (functional measure) as outcome; no impairment measures |
| Weinberg 1977 | Patients did not necessarily have neglect |
| Weinberg 1979 | Clarification of randomisation procedure sought but not obtained, and unlikely to be, given the age of this article. The time scale of publication (and a statement in the results) suggests that participants in this study were not in the Weinberg 1977 study; however, this has not been confirmed by study authors. On the other hand, the 1979 paper does not explicitly mention 'neglect' and may instead be a trial of visual perception. Given the amount of uncertainty about this study's fit to the inclusion criteria, inability to obtain confirmation and clarification about this old study and lack of detail on randomisation, we decided to exclude the 1979 article |
| Weinberg 1982 | Confirmation regarding randomisation sought from trialist but not obtained. No SD reported |
| Young 1983 | Controlled trial: not randomised. Divided into 3 groups matched for age, education, time since onset, and degree of deficit: no further information provided other than assessor blinded to group's membership |
BI: Barthel Index. FIM: Functional Independence Measure. RCT: randomised controlled trial. SD: standard deviation.
Characteristics of studies awaiting classification [ordered by study ID]
Cazzoli 2015.
| Methods | RCT |
| Participants | Left‐sided, hemi‐spatial neglect after subacute right hemispheric stroke |
| Interventions | cTBS was applied at 100% of patients' individual resting motor threshold of the right small hand muscles. Sham stimulation was applied according to the same protocol, with the exception that a sham coil was connected to output from the stimulator |
| Outcomes |
|
| Notes | Report analyses data from 13 patients. Five were “randomly allocated” (no further detail) to active or sham intervention. Remaining 3 received first sham, and then, within 5 days, active. Absence of statistically significant differences between data for these 3 and allocated groups was misinterpreted by study authors as “comparable in all these respects”. All analyses are done as if allocated groups were each n = 8 |
Chan 2013.
| Methods | Before‐and‐after trial |
| Participants | 40 patients with stroke and associated unilateral neglect |
| Interventions | 12‐session visual scanning programme for 4 weeks, whereas patients in the control group received standard rehabilitation services only |
| Outcomes | Modified BI, MMSE, and 2 neglect‐related measures, namely, Behavioural Inattention Test ‐ Conventional subtests, and Catherine Bergego Scale |
| Notes | We will include in future updates if deemed eligible |
Chan 2017.
| Methods | Randomised double‐blind controlled trial |
| Participants | Inclusion criteria: first or second stroke (haemorrhagic or ischaemic) confirmed by computer axial tomography scan or magnetic resonance imaging Neurological representation compatible with unilateral right lesion involvement (i.e. left hemiplegic); exhibited left visual field inattention or neglect by following any of the following criteria: obtaining a total score of star cancellation subtest in the conventional battery of the Behavioural Inattention Test < 51 (out of 54), obtaining a total score of line bisection subtest in the conventional battery of the Behavioural Inattention Test < 7 (out of 9), score on Catherine Bergego Scale ≥ 1, right‐handed, less than 6 months since onset of stroke at study entry, able to follow simple command Exclusion criteria: patients with severe dysphasia (either expressive or comprehensive) that restricts communication; history of other neurological disease, psychiatric disorder, or alcoholism; significant impairment in visual acuity caused by cataracts, diabetic retinopathy, glaucoma, or hemianopia; any additional medical or psychological condition that would affect ability to comply with the study protocol Ages eligible: child, adult, and senior Sexes eligible: all |
| Interventions | Experimental: TMS and trunk rotation Sham comparator: sham TMS and trunk rotation |
| Outcomes | Primary: BIT ‐ Chinese version Secondary: Catherine Bergego Scale, FTHUE‐HK, UE‐Fugl Meyer, FIM, SA‐SIP 30 |
| Notes | End date: 1 June 2019; unable to obtain further information |
Hauer 2007.
| Methods | 3‐arm trial |
| Participants | 18 participants with visuospatial neglect |
| Interventions | Prism adaptation. Group 1 had 1 daily treatment, Group 2 had 2 daily treatments, and Group 3 had none |
| Outcomes | Symptoms of neglect |
| Notes | Unsure if fully random allocation ‐ awaiting translation |
Iwata 2017.
| Methods | |
| Participants | Inclusion criteria: (1) scoring less than cutoff value in the line cancellation task, (2) no severe cognitive impairment (MMSE > 15) Exclusion criteria: (1) inability to understand the task because of aphasia or other cognitive impairment, (2) inability to sit on a wheelchair, (3) inability to recognise objects on a screen due to severely damaged eyesight, (4) inability to reach with upper limb extremity because of restricted range of motion, (5) inability to give informed consent form Age minimum: 20 years old Age maximum: 85 years old Gender: men and women |
| Interventions | Patients were attached to a head‐mounted display (HMD) and presented 3‐dimensional virtual reality space where multiple objects were installed. First, they answer aloud the objects' name of far space in 3‐dimensional virtual reality space with HMD. Second, they touch the objects of near space with 1 hand that is synchronised in 3‐dimensional virtual reality space with HMD. At this time, they are promoted attentional disengagement from the ipsilesional stimuli by blocking visual stimuli to direct attention and attentional movement from the ipsilesional to the contralesional side by expanding the visible area to the contralesional side. This took about 6 minutes Patients were seated at a desk. They conducted visual scanning training on the desk. The task of patients is to answer the objects' name that is pointed by the therapist. Objects were installed on the desk. This took about 6 minutes Patients were seated at a desk. They conducted visual scanning training on the screen. The screen is installed in front of the patient. The task of patients is to answer the name of the object that is pointed to by the therapist. Objects were installed on the screen. This took about 6 minutes Patients were attached to a head‐mounted display (HMD) and presented 3‐dimensional virtual reality space, where multiple objects were installed. They answer aloud the name of objects of far space in 3‐dimensional virtual reality space with HMD. At this time, patients' attention is inducted to neglect side of an object. This took about 13 minutes |
| Outcomes | Primary: line cancellation, line bisection, star cancellation, letter cancellation task Secondary: not stated |
| Notes | Status ‐ not yet recruiting Status seems unusual given the start date; we have been unable to gain further information |
Lim 2017.
| Methods | Single‐blind RCT |
| Participants | Inclusion criteria: presence of hemi‐spatial neglect as defined by Behavioral Inattention Test score of 129 or worse (maximum score 146) Exclusion criteria: presence of aphasia at time of testing, recent seizures, major psychiatric illness, prior unrelated neurological disease |
| Interventions | 1/2 patients receive visual stimulation with rehabilitation glasses. 1/2 patients receive control stimulation with rehabilitation glasses |
| Outcomes | Primary: BIT Secondary: none stated |
| Notes | Status: completed; we have been unable to gain further information |
Marandola 2020.
| Methods | RCT |
| Participants | 30 patients with ischaemic stroke and diagnosis of hemi‐neglect |
| Interventions | Modified constraint‐induced movement therapy (mCIMT) or conventional therapy |
| Outcomes | Catherine Bergego Scale (CBS) for assessment hemi‐neglect; Fugl‐Meyer tests for the motor function of lower and upper limb, and BI and modified Rankin scale for the rest of objectives |
| Notes | We will include this study in future updates if eligible |
Mueller‐Planitz 2017.
| Methods | RCT |
| Participants | Inclusion criteria: 18 years old or older; demonstrated visual/spatial neglect, as demonstrated by NIH Stroke Scale (NIHSS), and deficits in assessing tactile extinction and visuospatial neglect done on admission Exclusion criteria: severe pain or skin disease at the posterior neck, severe atherosclerosis of carotid arteries by an ultrasonic evaluation Ages eligible: 18 years of age and older Sexes eligible: all |
| Interventions | Experimental: vibration to upper posterior neck muscles. Treatment will be performed by occupational therapist practitioners prior to regular occupational therapy session using a vibration tool Active comparator: standard of care Regular occupational therapy session |
| Outcomes | Primary: BIT Secondary: Catherine Bergego Scale (CBS, Activity Measure for Post‐Acute Care (AM‐PAC)) |
| Notes | End date: 12 April 2018 Study terminated early due to poor enrolment |
Park 2021.
| Methods | RCT |
| Participants | Inclusion criteria
|
| Interventions | Robot‐assisted hand training Type: experimental Classification: behavioural Descriptions: exercises were carried out as follows: (1) grasp and release training (digital joint flexion/extension exercise from the thumb to the fifth finger) for 15 minutes; (2) count training (count a number sequence from 1 to 5) for 15 minutes |
| Outcomes | Outcome name: Line Bisection Test
Metric/method of measurement: hemi‐spatial neglect
Time point: before and after the 20 sessions Outcome name: Albert's test Metric/method of measurement: hemi‐spatial neglect Time point: before and after the 20 sessions Outcome name: Catherine Bergego Scale Metric/method of measurement: hemi‐spatial neglect Time point: before and after the 20 sessions |
| Notes | We will include this study in future updates if eligible |
Saevarsson 2010.
| Methods | Setting: rehabilitation hospital and community, Germany |
| Participants | Main inclusion criteria: right hemisphere injury, intact left hemisphere, intact cerebellum, overall stable health condition, significantly impaired performance on more than 3 of 9 neuropsychological neglect tests Age: ages reported individually Sex (women/men): 5/7 Hemisphere damaged: right Time since stroke: time since stroke reported individually |
| Interventions | Participants received either neck vibration (NV) or neck vibration plus prism adaptation (NVPA) NV was applied for 20 minutes on the left posterior neck muscle of the patient. The location at the neck was found by asking patients to monitor a small green light 2 metres in front of them. While the apparatus was adjusted, patients were asked openly if they noticed any changes in their perception of the light. If a patient reported an alteration (e.g. the light point moving to the right side at the time of stimulation and to the left side when the NV module is removed), the NV module was applied at that exact location. The NV module was glued with medical tape to patients’ neck muscles. Both groups of patients underwent NV while seated in front of an adaptation box. The NVPA group underwent PA treatment simultaneously to the NV. Patients in this group were asked to perform rapid pointing movements approximately 4 times per minute while wearing 10° right‐shifted prism glasses. Participants were able to see their pointing only for the last 1 to 2 cm before their finger reached the dots of the adaptation box. Pointing errors reduced with repeated pointing until the landing point was aligned with the dots |
| Outcomes | |
| Notes | We are awaiting details on randomisation to check eligibility and will include the study if eligible in future updates |
Seo 2017.
| Methods | Double‐blind RCT |
| Participants | Inclusion criteria: (1) first‐ever stroke on the right hemisphere, (2) right‐handedness, (3) left hemi spatial neglect (Line Bisection Test = 15% to right side), (4) patients over 18 years old who gave informed consent, (5) stroke onset within the last 6 months Exclusion criteria: (1) medically unstable patients, (2) general contraindication of tDCS (pacemaker, implantable cardioverter‐defibrillator, metal implants in brain), (3) pregnancy, (4) history of seizure or brain surgery, (5) severe skin lesion on stimulation sites, (6) severe cognitive impairment (MMSE < 10) Age minimum: 18 years Age maximum: no limit Gender: both |
| Interventions | Experimental group receives 2.0 mA cathodal tDCS 5 times a week for 2 weeks (10 times). Each treatment takes 20 minutes. Control group receives sham tDCS |
| Outcomes | Primary: line bisection test |
| Notes | Status: not yet recruiting, unable to obtain further information |
Toglia 2020.
| Methods | Randomised controlled proof‐of‐concept pilot |
| Participants | 40 patients with left‐sided neglect after right brain stroke were included |
| Interventions | Multi‐context treatment approach using a protocol of spatial exploration strategy training in 1 brief session (20 to 30 minutes) |
| Outcomes | Spatial Neglect Assessment Battery |
| Notes | We will include this study in future updates if eligible |
Vilimovsky 2021.
| Methods | RCT |
| Participants | 34 stroke patients receiving inpatient rehabilitation |
| Interventions | Prism adaptation training |
| Outcomes |
|
| Notes | We will include this study in future updates if deemed eligible |
Zigiotto 2020.
| Methods | Pilot study |
| Participants | 20 USN stroke patients |
| Interventions | 2‐week treatment (20 sessions, twice per day) of intensive audiovisual multi‐sensory stimulation compared with prismatic adaptation |
| Outcomes | Neuropsychological clinical tests (target cancellation, line bisection, sentence reading, personal neglect, complex drawing) and the Catherine Bergego Scale for functional disability |
| Notes | We will include this study in future updates if eligible |
BI: Bathel Index. BIT: Behavioural Inattention Test. HADS: Hospital Anxiety and Depression Scale. MMSE: Mini Mental State Examination. RCT: randomised controlled trial. TUG: timed up and go,
Characteristics of ongoing studies [ordered by study ID]
Elshout 2018.
| Study name | |
| Methods | RCT |
| Participants | Inclusion criteria
Exclusion criteria: patients who recovered from neglect between inclusion and start of training (i.e. no signs of neglect anymore on all baseline measurements) will be excluded |
| Interventions | 15 neglect patients will receive visual scanning therapy 15 neglect patients will receive visual scanning training combined with congruent hand movements Outcome measures for each training group will be compared to 15 stroke patients without neglect and 15 age‐matched healthy controls |
| Outcomes | Primary outcomes
Secondary outcomes
|
| Starting date | |
| Contact information | |
| Notes | End date: 31/05/19. Study author confirms in write‐up phase |
ISRCTN88395268.
| Study name | A feasibility study for attention loss after stroke (SPATIAL) |
| Methods | Feasibility RCT |
| Participants | Participant inclusion criteria (current participant inclusion criteria as of 10/02/2020) Patient participants
Carer participants
Staff participants
|
| Interventions | Trialists are testing how sensible and practical it is to use PAT as part of an occupational therapy session to inform a larger trial. This will be done in multiple hospitals. Patients will be split into 2 groups at random: 1 will receive PAT in addition to normal occupational therapy, the other will receive just normal occupational therapy. The entire study will be evaluated to find out what it was like for everyone who was involved. The study will also test whether PAT helps people participate in occupational therapy. The study has been designed in collaboration with stroke service users For participants in the intervention group, prism adaptation training (PAT) will be offered at the start of a standardised session of OT for up to 3 weeks, 5 days a week. PAT takes no more than 5 minutes plus setup time (seating participants and fitting glasses). To perform PAT, participants will be seated at a table in front of a training box that has open ends. Participants will be fitted with 12.5° prism glasses, and the occupational therapist will hold up targets at the opposite end of the box and will ask participants to reach to the target; this will be repeated a maximum of 90 times, or for a maximum of 5 minutes, whichever is shorter When prism glasses have been removed, the session will continue with standardised OT. The effect of prism adaptation training is strongest in the hours soon after treatment; reducing the spatial inattention for long enough to take part in usual OT that aims to increase independence in activities of daily living. OT staff will record the time that PAT took place, the number of repetitions of pointing, and length and type of therapy intervention |
| Outcomes | Primary outcome measure
Secondary outcome measures
|
| Starting date | 1 July 2018 |
| Contact information | Prof Audrey Bowen SPATIALstroke@manchester.ac.uk |
| Notes | End date: 30 June 2020 |
Luvizutto 2017.
| Study name | A clinical study of non‐invasive brain stimulation in unilateral spatial neglect after stroke |
| Methods | Randomised double‐blind placebo‐controlled trial; parallel, with 2 arms |
| Participants | Inclusion criteria: diagnosis of stroke of either sex, 18 to 85 years of age, ischaemia or bleeding in the right parietal lobe, confirmed by computed tomography or magnetic resonance imaging, objective diagnosis of unilateral spatial neglect Exclusion criteria: metal into cranial cavity, injuries in the area of electrode placement, clinical instability, severe cognitive impairment, global aphasia, previous visual disturbances, other neurological disease |
| Interventions | Transcranial direct‐current stimulation (tDCS): applied through current stimulator battery powered using sponge pair of surface electrodes (5 cm × 5 cm) soaked in saline solution. A constant current of 2 mA of intensity will be applied for 20 minutes based on security guidelines in the right posterior parietal lobe. For stimulation of the posterior parietal lobe, will be placed on the anode P4 point (international electroencephalogram system) and the cathode in the left supraorbital area after cleaning the areas with alcohol. After stimulation, areas of electrode placement will be checked Control group (sham): patient is placed in the same room and position of tDCS group with the same device programming for 20 minutes, and the current will be delivered by first 10 seconds and off by 19 minutes and 50 seconds Each group will consist of 20 participants, and the tDCS will be performed for 15 sessions, 3 times a week, for 5 weeks |
| Outcomes | Primary: Catherine Bergego Scale Secondary: Barthel Index, modified Rankin Scale, European (5D) Quality of Life Scale |
| Starting date | 1 July 2016 |
| Contact information | Gustavo Luvizutto Av. Prof. Montenegro, Distrito de Rubião Junior, sem número 18.618‐97 Botucatu Brazil gluvizutto@gmail.com Affiliation: Hospital das Clínicas da Faculdade de Medicina de Botucatu |
| Notes | End date: 31 January 2020 |
NCT00989430.
| Study name | Prism adaptation therapy for spatial neglect |
| Methods | Randomised double‐blind controlled trial |
| Participants | Inclusion criteria: participants
Exclusion criteria: participant has or had a serious brain condition other than stroke |
| Interventions | Experimental: prism adaptation treatment: 2 weeks of prism adaptation treatment followed by 4 weekly assessments and long‐term follow‐ups at 3rd and 6th months No Intervention: control: standard rehabilitation care: participants will continue with their standard inpatient rehabilitation care. They will be assessed with cognitive and functional scales for tracking their recovery |
| Outcomes | Primary: improvement in spatial neglect (method not stated) Secondary: not stated |
| Starting date | October 2012 |
| Contact information | Anna M Barrett, MD Kessler Institute for Rehabilitation, West Orange, New Jersey, United States, 07052 |
| Notes | End date: October 2020 |
NCT02213640.
| Study name | |
| Methods | Randomised double‐blind controlled trial |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Transcranial direct current stimulation (tDCS) vs placebo stimulation |
| Outcomes | Primary: Behavioural Inattention Test (BIT) Secondary: Negligence Battery Test (BTN), Functional Independence Scale (FIM), Catherine Bergego Scale (CBS), Jamar |
| Starting date | |
| Contact information | |
| Notes | Confirmed ongoing by study author in analysis |
NCT02680171.
| Study name | Feasibility and effectiveness study of implementing prism adaptation as a treatment for spatial neglect after stroke |
| Methods | Randomised double‐blind controlled trial |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Experimental: prism goggles with 10‐degree rightward deviating prism lenses will be used to implement prism adaptation treatment, in addition to standard care Sham comparator: non‐shifting goggles (sham) will be worn by patients in the control condition. These goggles do not shift patients' visual field |
| Outcomes | Primary: Sunnybrook Neglect Assessment Procedure (SNAP) Secondary: Johnny Shirt Visual Scanning Task, Behavioural Inattention Test ‐ Behaviour subtests (BIT‐B), Catherine Bergego Scale (CBS), Halifax Neglect Severity Scale, Functional Independence Measure (FIM), Frenchay Activities Index, length of inpatient stay at the Rehabilitation Centre, discharge destination, proprioceptive and visuo‐motor pointing midline tasks |
| Starting date | Feburary 2016 |
| Contact information | Gail A Eskes, PhD gail.eskes@dal.ca |
| Notes | Champod AS, Taylor K, Eskes GA. Development of a new computerized prism adaptation procedure for visuo‐spatial neglect. Journal of Neuroscience Methods 2014;30;235:65‐75. doi: 10.1016/j.jneumeth.2014.05.023. Epub 2014 Jun 19 End date: 30 June 2019. PI confirms study is ongoing |
NCT03168360.
| Study name | Effect of intensive cognitive rehabilitation in subacute stroke patient |
| Methods | RCT |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Intensive cognitive rehabilitation by cognitive therapist for 1 hour on every working day during subacute stroke phase |
| Outcomes | Primary outcome measure
|
| Starting date | 1 November 2016 |
| Contact information | Contact: Won Hyuk Chang, MD, PhD02‐3410‐2818; wh.chang@samsung.com |
| Notes | End date: 31 December 2021 |
NCT03317860.
| Study name | Improving measurement and treatment of post‐stroke neglect |
| Methods | Participants will receive both conditions (active and sham transcranial direct current stimulation paired with arm rehabilitation training (repetitive task‐specific practice)) in this cross‐over design study. Individuals will be randomised to determine which condition they receive first, and the participant and the treatment therapist and assessor will be blinded to the order that the interventions are delivered. The PI will oversee randomisation, so that each patient is randomised and is assigned a unique 5‐digit code. When this code is entered on the tDCS device, the device will automatically assign the patient to receive either real or sham stimulation. Because sham stimulation provides a ramp up/ramp down stimulation for 15 seconds at the start and end of the session, the participant may perceive the sham stimulation as active stimulation |
| Participants | Inclusion criteria
|
| Interventions | Single session of bilateral active parietal cortex tDCS (2.0 mA for 30 minutes) paired with repetitive task‐specific practice (RTP) |
| Outcomes | Primary outcome measures Excitability of fronto‐parietal connectivity measured by paired pulse twin coil transcranial magnetic stimulation (TMS) test. In each session, the difference in excitability of fronto‐parietal connectivity between pre‐stimulation and post stimulation will be measured
Secondary outcome measures Kinematic assessment will be conducted to assess changes in motor impairment Neglect assessment (conventional subtests) will be conducted to assess changes in attentional impairment. Total scores range from 0 to 146, with lower scores indicating greater impairment
Other outcome measures This neglect assessment will be administered to examine the impact of neglect on performance of daily activities. Total scores range from 0 to 30, with higher scores indicating greater impairment This neglect assessment (behavioural subtests) will be administered to examine the impact of neglect on performance of daily activities. Total scores range from 0 to 81, with lower scores indicating greater impairment This neglect assessment will be administered to examine the impact of neglect on performance of daily activities. Each item has a score of 0 to 6, with lower scores indicating greater impairment. The Lateralized Attention Score (LAS) is difference between contralateral and ipsilateral proportions of items. Higher LAS scores indicate greater impairment
|
| Starting date | 2 July 2018 |
| Contact information | grattan@musc.edu |
| Notes | End date: 3 July 2023 |
NCT03402906.
| Study name | Family‐clinician collaboration to Improve neglect and rehabilitation outcome after stroke |
| Methods | RCT |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Experimental group will be performing the Family‐Clinician Collaboration Programme. Family members will work closely with the clinician to understand the status and goals of the stroke survivor, and family members will integrate family‐mediated treatment procedures into their time spent with the patient Intervention: behavioural ‐ family‐clinician collaboration programme; behavioural ‐ standard care at KIR Family‐mediated treatment activities and collaboration between clinician and family members Other name: FCC Participants will receive standard care provided at Kessler Institute for Rehabilitation Arm Intervention/treatment Experimental: family‐clinician collaboration programme; behavioural: standard care at KIR |
| Outcomes | Primary outcome measures: assessment of overall functional independence
|
| Starting date | 30 September 2017 |
| Contact information | Peii Chen, PhD, Kessler Foundation |
| Notes | Active, no longer recruiting End date: 29 September 2020 |
NCT03451708.
| Study name | Optokinetic stimulation for the treatment of hemi‐spatial neglect ‐ safety and efficacy studies |
| Methods | Cross‐over |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Optokinetic stimulation will be displayed on a see‐through liquid crystal display lens placed in front of participants |
| Outcomes | Primary outcome measures: performance on Center of Cancellation Test, performance on Behavioural Inattention Test, visual acuity, reading speed
Secondary outcome measures: line bisection score, grip strength, extinction score, gait assessment, balance assessments
|
| Starting date | 1 May 2018 |
| Contact information | Principal investigator: Chun Lim, MD, Beth Israel Deaconess Medical Center |
| Notes | End date: 31 August 2022 |
NCT03458611.
| Study name | Virtual Reality Attention Training in stroke patients (VRAT) |
| Methods | Study design is a mix of within‐subject manipulation of placebo and active intervention conditions and between‐subject manipulation of the order of these 2 within‐subject conditions. To clarify, a placebo and an active version of VR game‐based attention training will be administered to each patient. The order of these 2 within‐subject conditions is counterbalanced between subjects to account for differences in order between the 2 treatment conditions |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | An audiovisual expanding (looming) stimulus is presented repeatedly to patients during the intervention. During the game, a disk is presented to the player. This disk expands and contracts in size. Presentation of the disk coincides with presentation of a sound that matches in frequency. The disk predicts the location where the next target will be presented. The player must discriminate between 2 types of target stimuli that are presented at the centre of the disk. To discriminate between the 2 targets, the player receives a limited time window. The locations of the disk and target stimuli are adjusted in real time as a function of the player's performance. The primary goal of this algorithm is to present multi‐sensory looming stimuli more frequently in the contralesional field than in the ipsilesional field |
| Outcomes | Primary outcome measure: the measure of spatial asymmetry will be the difference in accuracy for target detection between left and right visual fields (visual L‐R score)
Secondary outcome measures While patients play the VR game, their head orientation is logged at a fixed rate. The cumulative time a patient's head is oriented towards the left or right side during moments in the VR intervention that there are no target stimuli presented will be calculated. The difference between time with the head oriented towards the left vs the right will be used as an index of spatial asymmetry in the VR environment (VR L‐R score) Difference between percentage of cumulative fixation duration for left and right visual fields as measured with an eye tracker during a visual computer task Difference between percentages of the direction of the first saccade in each trial of the task as measured with an eye tracker during a visual computer task Accuracy for auditory signals presented to the left and right ear is measured with a computerised task. Accuracy difference for left and right signals will be calculated Hemi‐spatial neglect symptoms in daily life are measured with the Catherina Bergego Scale (Azouvi et al, 2003). This scale has 10 items of behaviour that are observed and are given a score from 0 (= no signs of neglect) to 3 (= patient always shows signs of neglect or does not correct for it). The sum of individual scores is the outcome index
|
| Starting date | 1 September 2018 |
| Contact information | celine.gillebert@kuleuven.be |
| Notes | End date: February 2020 |
NCT03854487.
| Study name | Effect of mirror therapy on unilateral neglect for patients after stroke |
| Methods | Single‐blinded randomised controlled trial to investigate effects of mirror therapy, with reference to sham mirror (a glass wall) and control (a covered mirror), in reducing unilateral neglect for patients with stroke |
| Participants | Inclusion criteria
|
| Interventions | Mirror therapy |
| Outcomes |
|
| Starting date | July 2016 |
| Contact information | |
| Notes | Study author confirmed ended and in write‐up stages |
NCT03887962.
| Study name | Virtual Environment Rehabilitation for Patients With Motor Neglect Trial (VERMONT) |
| Methods | RCT |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Participants will be instructed to walk on a treadmill, moving at a constant speed, following a "virtual path" displayed on a flat screen in front of them. In this group, the gait task may involve avoiding virtual obstacles on the screen in the path or stepping on targets as determined by the therapist |
| Outcomes | Primary outcome measures
Secondary outcome measures
|
| Starting date | 1 May 2017 |
| Contact information | Principal Investigator: Nicholas GN Shenker, MD, Cambridge University Hospitals, NHS Foundation Trust |
| Notes | End date: 1 November 2020 |
NCT04080999.
| Study name | Repetitive transcranial magnetic stimulation in spatial attention after stroke (r‐TMS) |
| Methods | RCT |
| Participants | Ages eligible for study: 18 years to 80 years (adult, older adult)
Sexes eligible for study: all
Accepts healthy volunteers: no Inclusion criteria
Exclusion criteria
|
| Interventions | Device: r‐TMS Interventions have a total administration time of 75 minutes per day. For TMS stimulation, the coil will be positioned tangentially on the target area. Each r‐TMS session will last 15 minutes and will be administered every other day (e.g. Monday‐Wednesday‐Friday, Monday‐Wednesday‐Friday, Monday). Visual scanning treatment involves the presence of a therapist, who administers various visual scanning tasks, used to increase patient's awareness and to teach strategies to improve spatial exploration abilities (Pizzamiglio et al, 1992). Trainings include 3 increasing levels of difficulty (9 possible combinations). Each level of difficulty will be exercised until the patient reaches a level of accuracy of 75%. The CCT will be carried out in 50‐minute sessions for 5 days a week within 15 days (11 sessions in total). On the days when r‐TMS is also administered, administration of the CCT will immediately follow brain stimulation |
| Outcomes | Primary outcome measures: battery for assessment of cognitive and behavioural symptoms in LHSN
Secondary outcome measures: battery for assessment of LHSN symptoms in activity of daily living. Two subtests will be executed ‐ "alertness" and "visual field/neglect" ‐ to assess attentive functions. The motor subscale will be executed to assess motor independence. A test will assess motor impairment in stroke patients. A test to assess ability to control the trunk after stroke. Psychophysiological index of inter‐hemispheric transmission. Psychophysiological index of inter‐hemispheric imbalance in a visual‐spatial attention task
|
| Starting date | 5 December 2018 |
| Contact information | Contact: Emanuela Casanova, MD, 3398999147; e.casanova@ausl.bologna.it Contact: Francesco Di Gregorio, PhD, 3290762585; francesco.digregorio@ku.de |
| Notes | End date: 1 March 2021 |
NCT04227132.
| Study name | Evaluation of an adaptive computerized training for rehabilitation of spatial neglect in stroke survivors (MULTITASK) |
| Methods | Randomised cross‐over. Both experimental and control trainings will be administered consecutively to all patients. Each type of training will be delivered for 10 sessions, with order of training randomised across participants |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Patients will receive at first the Labyrinth training for 10 sessions of 45 minutes, delivered 4 days per week. Then, they will undergo standard training for 10 sessions of 45 minutes, for around 4 days per week. Before and after each training, patients will be tested for primary and secondary outcomes with standardised tests Patients sit in front of a computer monitor and play the adaptive video game with a joystick. The game requires to orient and move inside a maze, and it includes phases that engage multi‐tasking abilities. The level and speed of the game are adapted online to patients' performance Experimental: Labyrinth training, then standard training device: adaptive computer game training |
| Outcomes | Primary outcome measures Diagnostic test for spatial neglect, composed of different subtests of spatial attention Test for everyday functional outcome
Secondary outcome measures Computerised test on spatial monitoring and multi‐tasking abilities Test for allocentric and egocentric spatial neglect
|
| Starting date | 16 December 2019 |
| Contact information | Contact: Francesca Meneghello, MD, 0412207183 ext 0039; francesca.meneghello@ospedalesancamillo.net |
| Notes | End date: 31 December 2021 |
NCT04273620.
| Study name | Combined optokinetic stimulation and cueing‐based reading therapy to treat hemi‐spatial neglect following stroke (OKS‐READ) |
| Methods | This study will be a monocentric, randomised, controlled clinical trial. Using a cross‐over design with 2 arms, patients will receive the intervention therapy first, then the control treatment, or they will start in the control arm and will then switch to the intervention arm |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Behavioural: optokinetic stimulation and cueing‐based reading therapy (OKS‐READ) Each intervention session starts with optokinetic stimulation (OKS) of at least 15 minutes' duration. A pattern of squares, dots, triangles, and stars will coherently and continuously move to the left on a computer screen in front of patients. Patients are instructed to choose 1 stimulus and follow it with the eyes until it has reached the left side of the screen, then jump to the right edge of the screen and start again The second part of each intervention session is the cueing‐based reading therapy (READ), which will also last at least 15 minutes. The task of patients is to read out loud words or a text presented on a paper in front of them. We will use exogenous (e.g. the therapist highlights words when they are omitted) and endogenous cues (verbal instructions that require intrinsic action by patients) to facilitate attentional shifts to the left. The intensity of cueing will be matched to the actual severity of neglect (adaptive therapy) Behavioural: general neuropsychological treatment As a control treatment, patients will receive neuropsychological treatment without targeting visuospatial attention. Examples for components implemented are supporting conversations, diagnostic assessments (e.g. memory diagnostics), and training of memory and executive functions |
| Outcomes | Primary outcome measures Composite score of different established computerised tests assessing spatial neglect (minimum 0%, maximum 100%; higher score means better outcomes) Clinical score of neglect‐related functional disability (Catherine Bergego Scale, CBS; minimum 0, maximum 30; higher score means worse outcomes)
Secondary outcome measures Performance in the Menu reading task of the Behavioural Inattention Test battery (minimum 0 correct words (worst outcome), maximum 24 correct words (best outcome)) Bias of the Center of Cancellation (CoC) during the Bells test (values between ‐1 (strongest leftward bias), 0 (no bias), and +1 (strongest rightward bias)) Bias of the Center of Fixation (CoF) during free viewing of naturalistic photographs as measured with an infrared remote eye tracker (values between ‐1 (strongest leftward bias), 0 (no bias), and +1 (strongest rightward bias)) Differences between investigator‐assessed CBS score and patients' self‐assessed CBS score Barthel Index (minimum 0, maximum 100; higher score means better outcomes) Functional Independence Measure (18‐item scale with scores between 0 and 7 points; higher scores mean better outcomes)
|
| Starting date | 22 January 2020 |
| Contact information | bjoern.machner@neuro.uni-luebeck.de |
| Notes | End date: 21 February 2022 |
NL8145.
| Study name | Modulating connectivity with non‐invasive brain stimulation during spatial neglect rehabilitation |
| Methods | RCT |
| Participants |
|
| Interventions | We will combine evidence‐based visual scanning training with 40 minutes of (active or sham) dual‐site tACS at theta (6 Hz) and gamma (80 Hz) frequencies. The intervention is administered 5 times a week for a duration of 2 weeks |
| Outcomes | Primary outcome: performance on digitalised Star Cancellation Test Secondary outcomes
|
| Starting date | 9 October 2019 |
| Contact information | olof.vanderwerf@maastrichtuniversity.nl |
| Notes | End date: 1 June 2022 |
Olson 2020.
| Study name | Caloric vestibular stimulation for treatment of unilateral neglect |
| Methods | Unknown |
| Participants | Unknown |
| Interventions | Unknown |
| Outcomes | Unknown |
| Starting date | Unknown |
| Contact information | catrina.olson@und.edu |
| Notes |
RCT: randomised controlled trial.
Differences between protocol and review
This review was initiated in 1999 and has undergone many changes. Differences between the previous 2013 version and this update are outlined below.
Review title
Previous versions of this review were titled "Cognitive rehabilitation for spatial neglect following stroke". We decided to broaden the scope of this update beyond cognitive rehabilitation due to the variety of interventions used to rehabilitate this cognitive impairment.
Included patients
Previous versions of this review were confined to trials of participants with stroke. For this updated review, this was expanded to include participants with neglect following any adult‐acquired non‐progressive brain injury. We expected the majority of such to be stroke patients.
Types of interventions
Previous versions of this review included only cognitive rehabilitation interventions; however, for this update, we expanded inclusion to any non‐pharmacological intervention and thus re‐considered any studies previously excluded for this reason. In previous versions of this review, we categorised the type of intervention according to cognitive theory as either a bottom‐up or a top‐down processing rehabilitation approach. For this update, we categorised interventions into eight broad types based on their approach. Through our knowledge of the field, we were aware of the development since initiation of this review of many non‐pharmacological interventions that may not have fallen under the umbrella of cognitive rehabilitation. We therefore expanded our inclusion to be more relevant to clinical practice.
Types of outcome measures
For previous versions of this review, we were interested in outcomes at two time points: (1) immediately after completion of an intervention, and (2) persisting beyond completion of an intervention (i.e. follow‐up outcome).
For this 2021 update, we designated (1) persisting beyond completion of an intervention (i.e. follow‐up outcome) as the primary outcome, and (2) immediately after completion of an intervention as a secondary outcome, to reflect the importance of these outcomes to people with stroke.
In previous versions of the review, we defined the primary outcome as 'ratings on measures of functional disability: activities of daily living (ADL) scales: Barthel Index (BI), Functional Independence Measure (FIM), Frenchay Activities Index (FAI), or neglect‐specific ADL measures'. As this was not a comprehensive list of functional disability measures, we extended the scales listed for the 2013 update to be more comprehensive and to avoid having to make decisions after identification of studies. We checked back through the studies included previously and found that this clarification did not lead to any changes to outcomes included from those studies.
Analysis
For this 2021 review update, we analysed outcomes only by subgroup (intervention type), and we omitted analysis of all studies versus any control, as intervention types were not comparable. For all previous versions of this review, we used data recorded at the time of hospital discharge as persisting effects. We re‐evaluated this decision for this update and omitted these data from meta‐analysis, as they are process dependent.
Contributions of authors
The original review, initiated by Nadina Lincoln (published by Lincoln, Bowen, and Dewey in 2002), has been updated several times with input from various review authors. The current (2021) extensive expansion and update was led by Audrey Bowen and was enabled by funding awarded to Verity Longley, Audrey Bowen, Alex Pollock, Christine Hazelton, Claire Mitchell, Calvin Heal, and Andy Vail. Verity Longley conducted most of the updated searches, data collection, analysis, and reporting. Christine Hazelton and Calvin Heal contributed significantly to searches, data collection, and reporting. Gorana Pobric took responsibility for the non‐invasive brain stimulation studies. Alex Pollock and Andy Vail led on methodological decision‐making and statistical analyses. Claire Mitchell contributed to searches, data collection, and Patient, Carer, and Public Involvement. Kate Woodward‐Nutt took responsibility for Patient, Carer, and Public Involvement. All co‐authors approved the final report.
Sources of support
Internal sources
No sources of support provided
External sources
-
NIHR DSE award, UK
Funded Verity Longley's time and training
-
NIHR NETSCC Incentive award, UK
Awarded for the current update
-
The Stroke Association, UK
Part‐funded Audrey Bowen's post through a readership award
-
The RNIB (Royal National Institute for Blind people), UK
Funded Christine Hazelton's time on this update.
-
NHS Executive Research and Development Programme Physical and Complex Disabilities, UK
Awarded for the original 2002 review
-
The Stroke Association, UK
Part funded Christine Hazelton's time via a non‐clinical Lectureship award.
Declarations of interest
Verity Longley: none known. Christine Hazelton: payment for a fellowship: my time on this review has been funded in part by a non‐clinical lectureship funded by the Stroke Association. Work as a health professional: clinical work as an Optometrist, Glasgow Caledonian University ‐ only a very small amount of this clinical work touches on the topic of interest in this review. Calvin Heal: none known. Alex Pollock: none known. Kate Woodward‐Nutt: none known. Claire Mitchell: none known. Gorana Pobric: none known. Andy Vail: none known. Audrey Bowen: grants and contracts: (1) funding for this review update, NIHR NETSCC Incentive Funding; (2) funding for primary research on the topic of this review (e.g. the SPATIAL feasibility study), NIHR RfPB, awarded to SRFT NHS Trust rather than to my University as per NIHR arrangements. Payment for a fellowship: fellowship for Dr Longley under my mentorship, NIHR Development and Skills Enhancement Award, awarded to MMU, where Dr Longley secured an academic post. Published opinions in medical journals, the public press, broadcast and social media relevant to interventions in the work: I have published journal papers and book chapters, and I have edited national guidelines that include the topic of this review (e.g. ICSWP National Clinical Guideline for Stroke 2016, awarded to SRFT NHS Trust rather than to my University as per NIHR arrangements). If you were involved in conducting a study that is eligible for inclusion in this review, what was the funding source for that study? Bowen A (CI), et al. A feasibility study of prisms and therapy in attention loss after stroke (SPATIAL feasibility). NIHR RfPB 249K, 2018‐2020.
The work presented here represents the views of the authors and not necessarily those of the funding bodies.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Aparicio‐Lopez 2016 {published data only}
- Aparicio-López C, García-Molina A, García-Fernández J, López-Blázquez R, Enseñat-Cantallops A, Sánchez-Carrión R, et al. Combination treatment in the rehabilitation of visuo-spatial neglect. Psicothema 2016;28(2):143–9. [DOI] [PubMed] [Google Scholar]
- Aparicio-López C, García-Molina A, García-Fernández J, Lopez-Blazquez R, Enseñat-Cantallops A, Sánchez-Carrión R, et al. Cognitive rehabilitation with right hemifield eye-patching for patients with sub-acute stroke and visuo-spatial neglect: a randomized controlled trial. Brain Injury 2015;29(4):501-7. [DOI] [PubMed] [Google Scholar]
Bang 2015 {published data only}
- Bang D-H, Bong S-Y. Effect of combination of transcranial direct current stimulation and feedback training on visuospatial neglect in patients with subacute stroke: a pilot randomized controlled trial. Journal of Physical Therapy Science 2015;27:2759–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cazzoli 2012 {published data only}
- Cazzoli D, Muri RM, Schumacher R, Arx S, Chaves S, Gutbrod K, et al. Theta burst stimulation reduces disability during the activities of daily living in spatial neglect. Brain 2012;135:3426–39. [DOI] [PubMed] [Google Scholar]
Cha 2016 {published data only}
- Cha HG, Kim MK. Effects of repetitive transcranial magnetic stimulation on arm function and decreasing unilateral spatial neglect in subacute stroke: a randomized controlled trial. Clinical Rehabilitation 2016;30(7):649–56. [DOI] [PubMed] [Google Scholar]
Cherney 2002 {published data only}
- Cherney LR, Halper AS, Papachronis D. Two approaches to treating unilateral neglect after right hemisphere stroke: a preliminary investigation. Topics in Stroke Rehabilitation 2003;9(4):22-33. [DOI] [PubMed] [Google Scholar]
Choi 2016 {published data only}
- Choi YS, Lee KW, Lee JH, Kim SB, Park GT, Lee SJ. The effect of an upper limb rehabilitation robot on hemispatial neglect in stroke patients. Annals of Rehabilitation Medicine 2016;40(4):611-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Choi 2019 {published data only}
- Choi HS, Kim DJ, Yang YA. The effect of a complex intervention program for unilateral neglect in patients with acute-phase stroke: a randomized controlled trial. Osong Public Health and Research Perspectives 2019;10(5):265-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cottam 1987 {published data only}
- Cottam GL. Visual Scanning Training for Right Hemispheric Stroke Patients Exhibiting Hemispatial Neglect [Dissertation]. Oxford, Mississippi: University of Mississippi, 1987. [Google Scholar]
Dolkun 2019 {published data only}
- Dolkun R, Li YK, Guo H, Liu ZY. Zhishen Tiaosui acupuncture on the unilateral spatial neglect after stroke: a randomized controlled trial. Chinese Acupuncture & Moxibustion 2019;39(10):1041-5. [DOI] [PubMed] [Google Scholar]
Edmans 2000 {published and unpublished data}
- Edmans JA, Webster J, Lincoln NB. A comparison of two approaches in the treatment of perceptual problems after stroke. Clinical Rehabilitation 2000;14(3):230-43. [DOI] [PubMed] [Google Scholar]
Fanthome 1995 {published and unpublished data}
- Fanthome Y, Lincoln N, Drummond A, Walker M. The treatment of visual neglect using feedback of eye movements: a pilot study. Disability Rehabilitation 1995;17(8):413-7. [DOI] [PubMed] [Google Scholar]
Ferreira 2011 {published data only}
- Ferreira HP, Lopes MAL, Luiz RR, Cardoso L, Andre C. Is visual scanning better than mental practice in hemispatial neglect? Results from a pilot study. Topics in Stroke Rehabilitation 2011;18(2):155-61. [DOI] [PubMed] [Google Scholar]
Fong 2007 {published and unpublished data}
- Fong KNK, Chan MKL, Ng PPK, Tsang MHN, Chow KKY, Lau CWL, et al. The effect of voluntary trunk rotation and half-field eye-patching for patients with unilateral neglect in stroke: a randomized controlled trial. Clinical Rehabilitation 2007;21:729-41. [DOI] [PubMed] [Google Scholar]
Fong 2013 {published data only}
- Fong KNK, Yang NYH, Chan MKL, Chan DYL, Lau AFC, Chan DYW, et al. Combined effects of sensory cueing and limb activation on unilateral neglect in subacute left hemiplegic stroke patients: a randomized controlled pilot study. Clinical Rehabilitation 2013;27(7):628-37. [DOI] [PubMed] [Google Scholar]
Fu 2017 {published data only}
- Cao L, Fu W, Zhang Y, Huo S, Du J, Zhu L, et al. Intermittent θ burst stimulation modulates resting-state functional connectivity in the attention network and promotes behavioral recovery in patients with visual spatial neglect. NeuroReport 2016;27:1261–5. [DOI] [PubMed] [Google Scholar]
- Fu W, Cao L, Zhang Y, Huo S, Du J, Zhu L, Song W. Continuous theta-burst stimulation may improve visuospatial neglect via modulating the attention network: a randomized controlled study. Topics in Stroke Rehabilitation 2017;24(4):236-41. [DOI] [PubMed] [Google Scholar]
Goedert 2020 {published and unpublished data}
- Goedert KM, Chen P, Foundas AL, Barrett AM. Frontal lesions predict response to prism adaptation treatment in spatial neglect: a randomised controlled study. Neuropsychological Rehabilitation 2020;30(1):32-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Iwanski 2020 {published data only}
- Iwanski S, Lesniak M, Polanowska K, Bembenek J, Czepiel W, Seniow J. Neuronavigated 1 Hz rTMS of the left angular gyrus combined with visuospatial therapy in post-stroke neglect. NeuroRehabilitation 2020;46:83-93. [DOI] [PubMed] [Google Scholar]
Kalra 1997 {published and unpublished data}
- Kalra L, Perez I, Gupta S, Whittink M. Effects of visual neglect on stroke rehabilitation. Proceedings of the Challenge of Stroke. The Lancet Conference; 15-16 October 1998; Geneva, Switzerland. Abstract 92.
- Kalra L, Perez I, Gupta S, Wittink M. The influence of visual neglect on stroke rehabilitation. Stroke 1997;28(7):1386-91. [DOI] [PubMed] [Google Scholar]
Karner 2019 {published data only}
- KarnerS, Stenner H, Spate M, Behrens J, Krakow K. Effects of a robot intervention on visuospatial hemineglect in postacute stroke patients: a randomized controlled trial. Clinical Rehabilitation 2019;33(12):1940-8. [DOI] [PubMed] [Google Scholar]
Katz 2005 {published data only}
- Katz N, Ring H, Naveh Y, Kizony R, Feintuch U, Weiss PL. Interactive virtual environment training for safe street crossing of right hemisphere stroke patients with unilateral spatial neglect. Disability and Rehabilitation 2005;27(20):1235-44. [DOI] [PubMed] [Google Scholar]
Kerkhoff 2012 {published data only}
- Kerkhoff G, Keller I, Artinger F, Hildebrandt H, Marquardt C, Reinhart S, et al. Recovery from auditory and visual neglect after optokinetic stimulation with pursuit eye movements - transient modulation and enduring treatment effects. Neuropsychologia 2012;50(6):1164-77. [DOI] [PubMed] [Google Scholar]
Kerkhoff 2014 {published data only}
- Kerkhoff G, Bucher L, Brasse M, Leonhart E, Holzgraefe M, Volzke V, et al. Smooth pursuit "bedside" training reduces disability and unawareness during the activities of daily living in neglect: a randomized controlled trial. Neurorehabilitation and Neural Repair 2014;28(6):554-63. [DOI] [PubMed] [Google Scholar]
Kim 2011 {published data only}
- Kim YM, Chun MH, Gi Yun GJ, Song YJ, Young HE. The effect of virtual reality training on unilateral spatial neglect in stroke patients. Annals of Rehabilitation Medicine 2011;35:309-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2013 {published data only}
- Kim BR, Chun MH, Kim DY, Lee SJ. Effect of high- and low-frequency repetitive transcranial magnetic stimulation on visuospatial neglect in patients with acute stroke: a double-blind, sham-controlled trial. Archives of Physical Medicine and Rehabilitation 2013;94(5):803-7. [DOI] [PubMed] [Google Scholar]
Kim 2015 {published data only}
- Kim YK, Jung JH, Shin SH. A comparison of the effects of repetitive transcranial magnetic stimulation (rTMS) by number of stimulation sessions on hemispatial neglect in chronic stroke patients. Experimental Brain Research 2015;233:283-9. [DOI] [PubMed] [Google Scholar]
Kim 2018 {published data only}
- Kim SB, Lee KW, Lee JH, Lee SJ, Park JG, Lee JB. Effect of combined therapy of robot and low-frequency repetitive transcranial magnetic stimulation on hemispatial neglect in stroke patients. Annals of Rehabilitation Medicine 2018;42(6):788-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koch 2012 {published data only}
- Koch G, Bonnì S, Giacobbe V, Bucchi G, Basile B, Lupo F, et al. θ-burst stimulation of the left hemisphere accelerates recovery of hemispatial neglect. Neurology 2012;78:24-30. [DOI] [PubMed] [Google Scholar]
Kutlay 2018 {published data only}
- Kutlay S, Genç A, Gök H, Öztuna D, Küçükdeveci A. Kinaesthetic ability training improves unilateral neglect and functional outcome in patients with stroke: a randomized control trial. Journal of Rehabilitation Medicine 2018;50(2):159-64. [DOI] [PubMed] [Google Scholar]
Learmonth 2020 {unpublished data only}
- Learmonth G, Benwell CSY, Märker G, Dascalu D, Checketts M, Santosh C, et al. Non-invasive brain stimulation in stroke patients (NIBS): a prospective randomized open blinded end-point (PROBE) feasibility trial using transcranial direct current stimulation (tDCS) in post-stroke hemispatial neglect. Neuropsychological Rehabilitation 2020;online:1-25. [DOI: 10.1080/09602011.2020.1767161] [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2017 {published data only}
- Li Y, Xu J, Liu L, Li M, Lu H, Chen H, et al. Post-stroke unilateral spatial neglect treated with acupuncture and rehabilitation: a randomized controlled trial. Zhongguo Zhen Jiu 2017;37(9):913-7. [DOI] [PubMed] [Google Scholar]
Luukkainen‐Markkula 2009 {published and unpublished data}
- Luukkainen-Markkulaa R, Tarkkaa IM, Pitkanena K, Siveniusa J, Hamalainen H. Rehabilitation of hemispatial neglect: a randomized study using either arm activation or visual scanning training. Restorative Neurology and Neuroscience 2009;27:663-72. [DOI] [PubMed] [Google Scholar]
Machner 2012 {published and unpublished data}
- Machner B, Könemund I, Sprenger A, Gablentz J, Helmchen C. Randomized controlled trial on hemifield eye patching and optokinetic stimulation in acute spatial neglect. Stroke 2014;45:2465-8. [DOI] [PubMed] [Google Scholar]
Mancuso 2012 {published data only}
- Mancuso M, Pacini M, Gemignani P, Bartalini B, Agostini B, Ferroni L, et al. Clinical application of prismatic lenses in the rehabilitation of neglect patients. A randomized controlled trial. European Journal of Physical and Rehabilitation Medicine 2012;48(2):197-208. [PubMed] [Google Scholar]
Mizuno 2011 {published data only}
- Mizuno K, Tsuji T, Takebayashi T, Fujiwara T, Hase K, Liu M. Prism adaptation therapy enhances rehabilitation of stroke patients with unilateral spatial neglect: a randomized, controlled trial. Neurorehabilitation and Neural Repair 2011;25(8):711-20. [DOI] [PubMed] [Google Scholar]
Nyfeller 2019 {published and unpublished data}
- Nyffeler TT, Vanbellingen T, Kaufmann BC, Pflugshaupt T, Bauer D, Frey J, et al. Theta burst stimulation in neglect after stroke: functional outcome and response variability origins. Brain 2019;142(4):992-1008. [DOI] [PubMed] [Google Scholar]
Nyfeller 2019 16c TBS {published data only}
- Nyffeler TT, Vanbellingen T, Kaufmann BC, Pflugshaupt T, Bauer D, Frey J, et al. Theta burst stimulation in neglect after stroke: functional outcome and response variability origins. Brain 2019;142(4):992-1008. [DOI] [PubMed] [Google Scholar]
Nyfeller 2019 8c TBS {published data only}
- Nyffeler TT, Vanbellingen T, Kaufmann BC, Pflugshaupt T, Bauer D, Frey J, et al. Theta burst stimulation in neglect after stroke: functional outcome and response variability origins. Brain 2019;142(4):992-1008. [DOI] [PubMed] [Google Scholar]
Nys 2008 {published data only (unpublished sought but not used)}
- Nys GMS, De Haan EHF, Kunneman A, De Kort PLM, Dijkerman HC. Acute neglect rehabilitation using repetitive prism adaptation: a randomized placebo-controlled trial. Restorative Neurology and Neuroscience 2008;26:1-12. [PubMed] [Google Scholar]
Pandian 2014 {published data only}
- Pandian JD, Arora R, Kaur P, Sharma D, Vishwambaran DK, Arima H. Mirror therapy in Unilateral neglect after STroke (MUST trial). A randomized controlled trial. American Academy of Neurology 2014;83:1012–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Park 2015 {published data only}
- Park J-H, Lee J-H. The effects of mental practice on unilateral neglect in patients with chronic stroke: a randomized controlled trial. Journal of Physical Therapy Science 2015;27(12):3803-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Park 2015b {published data only}
- Park J-S, Choi J-B, Kim W-J, Jung N-H, Chang M. Effects of combining mental practice with electromyogram-triggered electrical stimulation for stroke patients with unilateral neglect. Journal of Physical Therapy Science 2015;27(11):3499-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
Polanowska 2009 {published and unpublished data}
- Polanowska K, Seniówa J, Paprota E, Leśniaka M, Członkowskaa A. Left-hand somatosensory stimulation combined with visual scanning training in rehabilitation for post-stroke hemineglect: a randomised,double-blind study. Neuropsychological Rehabilitation 2009;19(3):364-82. [DOI] [PubMed] [Google Scholar]
Raghavan 2017 {published data only}
- Raghavan C. Hemispatial Neglect: An Evaluation of Novel Assessment Methods and Rehabilitation [PhD Thesis]. Oxford: University of Oxford, 2017. [Google Scholar]
Robertson 1990 {published and unpublished data}
- Robertson I, Gray J, Pentland B, Waite L. Microcomputer-based rehabilitation for unilateral left visual neglect: a randomised controlled trial. Archives of Physical Medicine and Rehabilitation 1990;71:663-8. [PubMed] [Google Scholar]
Robertson 2002 {published data only}
- Robertson IH, McMillan TM, MacLeod E, Edgeworth J, Brock D. Rehabilitation by limb activation training reduces left-sided motor impairment in unilateral neglect patients: a single-blind randomised control trial. Neuropsychological Rehabilitation 2002;12(5):439-54. [Google Scholar]
Rode 2015 {published data only}
- Rode G, Lacour S, Jacquin-Courtois S, Pisella L, Michel C, Revol P, et al. Long-term sensorimotor and therapeutical effects of a mild regime of prism adaptation in spatial neglect. A double-blind RCT essay. Annals of Physical and Rehabilitation Medicine 2014;58:40–53. [DOI] [PubMed] [Google Scholar]
Rossit 2019 {published data only}
- Rossit S, Benwell CSY, Szymanek L, Learmonth G, McKernan-Ward L, Corrigan E, et al. Efficacy of home-based visuomotor feedback training in stroke patients with chronic hemispatial neglect. Neuropsychological Rehabilitation 2019;29(2):251-72. [DOI] [PubMed] [Google Scholar]
Rusconi 2002 {published data only}
- Rusconi ML, Meinecke C, Sbrissa P, Bernardini B. Different cognitive trainings in the rehabilitation of visuo-spatial neglect. Europa Medicophysica 2002;38:159-66. [Google Scholar]
Schroder 2008 {published data only}
- Schroder A, Wist ER, Homberg V. TENS and optokinetic stimulation in neglect therapy after cerebrovascular accident: a randomized controlled study. European Journal of Neurology 2008;15:922-7. [DOI] [PubMed] [Google Scholar]
Seniow 2016 {published data only}
- Seniow J, Polanowska K, Lesniak M, Czlonkowska A. Adding transcutaneous electrical nerve stimulation to visual scanning training does not enhance treatment effect on hemispatial neglect: a randomized, controlled, double-blind study. Topics in Stroke Rehabilitation 2016;23(6):377-83. [DOI] [PubMed] [Google Scholar]
Sesh 2018 {published data only}
- Sesh S. Effect of Combined Visual-Auditory-Sensory Stimulation in Hemineglect Syndrome Following Right Hemispheric Ischemic Strokes: A Randomized Control Trial [Thesis]. Thiruvananthapuram: Sree Chitra Tirunal Institute for Medical Sciences and Technology, 2018. [Google Scholar]
Song 2009 {published data only}
- Song W, Du B, Xu Q, Hu J, Wang M, Luo Y. Low-frequency transcranial magnetic stimulation for visual spatial neglect: a pilot study. Journal of Rehabilitation Medicine 2009;41:162-5. [DOI] [PubMed] [Google Scholar]
Ten‐Brink 2017 {published data only}
- Ten Brink AF, Visser-Meily JMA, Schut MJ, Kouwenhoven M, Eijsackers ALH, Nijboer TCW. Prism adaptation in rehabilitation? No additional effects of prism adaptation on neglect recovery in the subacute phase poststroke: a randomized controlled trial. Neurorehabilitation and Neural Repair 2017;31(12):1017-28. [DOI] [PubMed] [Google Scholar]
Tsang 2009 {published and unpublished data}
- Tsang MHM, Sze KH, Fong KNK. Occupational therapy treatment with right half-field eye-patching for patients with subacute stroke and unilateral neglect: a randomised controlled trial. Disability and Rehabilitation 2009;31(8):630-7. [DOI] [PubMed] [Google Scholar]
Turton 2010 {published and unpublished data}
- Turton AJ, O'Leary K, Gabb J, Woodward R, Gilchrist I. A single blinded randomised controlled pilot trial of prism adaptation for improving self-care in stroke patients with neglect. Neuropsychological Rehabilitation 2010;20(2):180-96. [DOI] [PubMed] [Google Scholar]
Van Wyk 2014 {published data only}
- Van Wyk A, Eksteen CA, Rheeder P. The effect of visual scanning exercises integrated into physiotherapy in patients with unilateral spatial neglect poststroke: a matched-pair randomized control trial. Neurorehabilitation and Neural Repair 2014;28(9):856-73. [DOI] [PubMed] [Google Scholar]
Varalta 2019 {published data only}
- Varalta V, Munari D, Pertile L, Fonte C, Vallies G, Chemello E, et al. Effects of neck taping in the treatment of hemispatial neglect in chronic stroke patients: a pilot, single blind, randomized controlled trial. Medicina 2019;55(4):108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vatanparasti 2019 {published data only}
- Vatanparasti S, Kazemnejad A, Yoonessi A, Oveisgharan S. The effect of continuous theta-burst transcranial magnetic stimulation combined with prism adaptation on the neglect recovery in stroke patients. Journal of Stroke & Cerebrovascular Diseases 2019;28(11):1-8. [DOI] [PubMed] [Google Scholar]
Volkening 2016 {published data only}
- Volkening K, Kerkhoff G, Keller I. Effects of repetitive galvanic vestibular stimulation on spatial neglect and verticality perception - a randomised sham-controlled trial. Neuropsychological Rehabilitation 2016;7:1-18. [DOI] [PubMed] [Google Scholar]
Welfringer 2011 {published data only}
- Welfringer A, Leifert-Fiebach G, Babinsky R, Brandt T. Visuomotor imagery as a new tool in the rehabilitation of neglect: a randomised controlled study of feasibility and efficacy. Disability and Rehabilitation 2011;33:2033-43. [DOI] [PubMed] [Google Scholar]
Wiart 1997 {published and unpublished data}
- Wiart L, Bon Saint Come A, Debellaix X, Petit H, Joseph PA, Mazaux JM, et al. Unilateral neglect syndrome rehabilitation by trunk rotation and scanning training. Archives of Physical Medicine and Rehabilitation 1997;78:424-9. [DOI] [PubMed] [Google Scholar]
Wilkinson 2014 {published data only}
- Wilkinson D, Zubko O, Sakel M, Coulton S, Higgins T, Pullicino P. Galvanic vestibular stimulation in hemi-spatial neglect. Frontiers in Integrative Neuroscience 2014;8(4):1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2013 {published data only}
- Wu C-Y, Wang T-N, Chen Y-T, Lin K-C, Chen Y-A, Li H-T, et al. Effects of constraint-induced therapy combined with eye patching on functional outcomes and movement kinematics in poststroke neglect. American Journal of Occupational Therapy 2013;67:236-45. [DOI] [PubMed] [Google Scholar]
Yang 2015 {published data only}
- Yang W, Liu T-T, Song X-B, Zhang Y, Li Z-H, Cui Z-H, et al. Comparison of different stimulation parameters of repetitive transcranial magnetic stimulation for unilateral spatial neglect in stroke patients. Journal of the Neurological Sciences 2015;359:219-25. [DOI] [PubMed] [Google Scholar]
Yang 2015 10Hz {published data only}
- Yang W, Liu T-T, Song X-B, Zhang Y, Li Z-H, Cui Z-H, et al. Comparison of different stimulation parameters of repetitive transcranial magnetic stimulation for unilateral spatial neglect in stroke patients. Journal of the Neurological Sciences 2015;359:219-25. [DOI] [PubMed] [Google Scholar]
Yang 2015 1Hz {published data only}
- Yang W, Liu T-T, Song X-B, Zhang Y, Li Z-H, Cui Z-H, et al. Comparison of different stimulation parameters of repetitive transcranial magnetic stimulation for unilateral spatial neglect in stroke patients. Journal of the Neurological Sciences 2015;359:219-25. [DOI] [PubMed] [Google Scholar]
Yang 2015 cTBS {published data only}
- Yang W, Liu T-T, Song X-B, Zhang Y, Li Z-H, Cui Z-H, et al. Comparison of different stimulation parameters of repetitive transcranial magnetic stimulation for unilateral spatial neglect in stroke patients. Journal of the Neurological Sciences 2015;359:219-25. [DOI] [PubMed] [Google Scholar]
Yang 2017 {published data only}
- Yang NY, Fong KN, Li-Tsang CW, Zhou D. Effects of repetitive transcranial magnetic stimulation combined with sensory cueing on unilateral neglect in subacute patients with right hemispheric stroke: a randomized controlled study. Clinical Rehabilitation 2017;31(9):1154-63. [DOI] [PubMed] [Google Scholar]
- Zhang RG, Liu SX, Wang FY, Ma XC, Yang YH. Treatment of unilateral neglect using repetitive transcranial magnetic stimulation (rTMS) and sensory cueing (SC) in stroke patients. Journal of Sichuan University, Medical Science Edition 2017;48(2):309‐13. [PubMed] [Google Scholar]
Yi 2016 {published data only}
- Yi YG, Chun MH, Do KH, Sung EJ, Kwon YG, Kim DY. The effect of transcranial direct current stimulation on neglect syndrome in stroke patients. Annals of Rehabilitation Medicine 2016;40(2):223-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yi 2016 anodal {published data only}
- Yi YG, Chun MH, Do KH, Sung EJ, Kwon YG, Kim DY. The effect of transcranial direct current stimulation on neglect syndrome in stroke patients. Annals of Rehabilitation Medicine 2016;40(2):223-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yi 2016 cathodal {published data only}
- Yi YG, Chun MH, Do KH, Sung EJ, Kwon YG, Kim DY. The effect of transcranial direct current stimulation on neglect syndrome in stroke patients. Annals of Rehabilitation Medicine 2016;40(2):223-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zeloni 2002 {published data only}
- Zeloni G, Farne A, Baccini M. Viewing less to see better. Journal of Neurology Neurosurgery and Psychiatry 2002;73:195-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Akinwuntan 2010 {published data only}
- Akinwuntan A, Devos H, Verheyden G, Baten G, Kiekens C, Feys H, et al. Retraining moderately impaired stroke survivors in driving-related visual attention skills. Topics in Stroke Rehabilitation 2010;17(5):328-36. [DOI] [PubMed] [Google Scholar]
Al Mahasneh 1991 {published data only}
- Al Mahasneh SM. Nursing Interventions to Reduce Unilateral Neglect in Right Hemisphere Stroke Patients [Dissertation]. Ann Arbor, Michigan: University of Michigan, 1991.
Angeli 2004 {published data only}
- Angeli V. Recovery of oculo-motor bias in neglect patients after prism adaptation. Neuropsychologia 2004;42(9):1223-34. [DOI] [PubMed] [Google Scholar]
Bar‐Haim 2011 {unpublished data only}
- Bar-Haim Erez A, Soroker N, Averbuch S. Phasic alerting combined with visual search training: a novel therapeutic approach for unilateral spatial neglect. Data on file.
Beis 1999 {published and unpublished data}
- Beis J-M, Andre JM, Baumgarten A, Challier B. Eye patching in unilateral spatial neglect: efficacy of two methods. Archives of Physical Medicine and Rehabilitation 1999;80:71-6. [DOI] [PubMed] [Google Scholar]
Butter 1992 {published data only}
- Butter C, Kirsch N. Combined and separate effects of eye patching and visual stimulation on unilateral neglect following stroke. Archives of Physical Medicine and Rehabilitation 1992;73:1133-9. [PubMed] [Google Scholar]
Carter 1980 {published data only}
- Carter L, Caruso J, Languirand M, Berard M. Cognitive skill remediation in stroke and non-stroke elderly. Clinical Neuropsychology 1980;2(3):109-13. [Google Scholar]
Chen 2014 {published data only}
- Chen P, Goedert K, Shah P, Foundas A, Barrett A. Integrity of medial temporal structures may predict better improvement of spatial neglect with prism adaptation treatment. Brain Imaging and Behavior 2014;8(3):346-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cubelli 1993 {published data only}
- Cubelli R, Inzaghi MG, De Tanti A. The rehabilitation of unilateral spatial neglect: experimental verification of its effectiveness [La rieducazione della negligenza spaziale unilaterale: verifica sperimentale della sua efficacia]. Europa Medicophysica 1993;29:111-21. [Google Scholar]
Diller 1974 {published data only}
- Diller L, Ben Yishay Y, Gerstman LJ, Goodki R, Gordon W, Weinberg J. Studies in cognition and rehabilitation in hemiplegia. In: Rehabilitation Monograph No. 50. New York: New York University, 1974. [Google Scholar]
EEG‐NF 2009 {published data only}
- Smithard D. A novel neurofeedback-based intervention to reduce neglect and improve function in stroke patients. UK Clinical Research Network Portfolio Database, 2012 (http://public.ukcrn.org.uk/search/).
- Smithard D. Electroencephalogram-neurofeedback (EEG-NF) to improve neglect in stroke patients. Current Controlled Trials, 2009 (http://www.controlled-trials.com/).
Facchin 2019 {published data only}
- Facchin AE, Sartori CL, De Galeazzi A, Beschin N. Effect of prism adaptation on neglect hemianesthesia. Cortex 2019;113:298-311. [DOI] [PubMed] [Google Scholar]
Frassinetti 2002 {published data only}
- Frassinetti A, Angeli V, Meneghello F, Avanzi S, Ladavas E. Long-lasting amelioration of visuospatial neglect by prism adaptation. Brain 2002;125:608-23. [DOI] [PubMed] [Google Scholar]
Gordon 1985 {published data only}
- Gordon W, Hibbard M, Egelko S, Diller L. Perceptual remediation in patients with right brain damage: a comprehensive programme. Archives of Physical Medicine and Rehabilitation 1985;66:353-9. [PubMed] [Google Scholar]
Harvey 2003 {published data only}
- Harvey M, Hood B, North A, Robertson IH. The effects of visuomotor feedback training on the recovery of hemispatial neglect symptoms: assessment of a 2-week and follow-up intervention. Neuropsychologia 2003;41:886-93. [DOI] [PubMed] [Google Scholar]
Harvey 2010 {published and unpublished data}
- Harvey M, Muir K, Rossit S. Long term improvements in activities of daily living in patients with hemispatial neglect. Behavioural Neurology 2010;23:249-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jacquin‐Courtois 2010 {published data only}
- Jacquin-Courtois S, Rode G, Pavani F, O'Shea J, Giard MH, Boisson D, et al. Effect of prism adaptation on left dichotic listening deficit in neglect patients: glasses to hear better? Brain 2010;133(3):895-908. [DOI] [PubMed] [Google Scholar]
Kang 2009 {published data only}
- Kang SH, Kim DY, Seo KM, Kwang C-A, Yoo JY, Sung SY, et al. A computerized visual perception rehabilitation programme with interactive computer interface using motion tracking technology – a randomized controlled, single-blinded, pilot clinical trial study. Clinical Rehabilitation 2009;23:434-44. [DOI] [PubMed] [Google Scholar]
Keller 2006 {published data only}
- Keller I, Beer AL, Kerkhoff G. Optokinetic stimulation in visual neglect [Optokinetische stimulation bei visuellem neglect]. Neurologie und Rehabilitation 2003;9(6):272-9. [Google Scholar]
Keller 2009 {published data only}
- Keller I, Lefin-Rank G, Lösch J, Kerkhoff G. Combination of pursuit eye movement training with prism adaptation and arm movements in neglect therapy: a pilot study. Neurorehabilitation and Neural Repair 2009;23(1):58-66. [DOI] [PubMed] [Google Scholar]
Kerkhoff 2005 {unpublished data only}
- Kerkhoff G, Keller I, Ritter V, Marquandt C. Repetitive optokinetic stimulation induces lasting recovery from visual neglect. Restorative Neurology and Neuroscience 2006;24:357-68. [PubMed] [Google Scholar]
- Kerkhoff G. Personal communication 2005.
Kerkhoff 2012b {published data only}
- Kerkhoff G, Keller I, Artinger F, Hildebrandt H, Marquardt C, Reinhart S, et al. Recovery from auditory and visual neglect after optokinetic stimulation with pursuit eye movements - transient modulation and enduring treatment effects. Neuropsychologia 2012;50(6):1164-77. [DOI] [PubMed] [Google Scholar]
Klos 2005 {unpublished data only}
- Klos T. Personal communication, 2005.
Ladavas 2013 {published data only}
- Ladavas E, Giulietti S, Avenanti A, Bertini C, Lorenzini E, Quinquinio C, et al. a-tDCS on the ipsilesional parietal cortex boosts the effects of prism adaptation treatment in neglect. Restorative Neurology and Neuroscience 2015;33(5):647-62. [DOI] [PubMed] [Google Scholar]
Lesniak 2013 {published data only}
- Lesniak M, Polanowska K, Seniów J. Repeated anodal tDCS coupled with cognitive training for patients with severe traumatic brain injury - a pilot RCT. Clinical Neurophysiology 2013;124(10):179-80. [DOI] [PubMed] [Google Scholar]
Lincoln 1985 {published data only}
- Lincoln N, Whiting S, Cockburn J, Bhavnani G. An evaluation of perceptual retraining. International Rehabilitation Medicine 1985;7:99-110. [DOI] [PubMed] [Google Scholar]
Loverro 1988 {published data only}
- Loverro J, Reding M. Bed orientation and rehabilitation outcome for patients with stroke hemianopsia or visual neglect. Journal of Neurologic Rehabilitation 1988;2:147-50. [Google Scholar]
Nakamura 2015 {published data only}
- Nakamura J, Kita Y, Ikuno K, Kojima K, Okada Y, Shomoto K. Influence of the stimulus parameters of galvanic vestibular stimulation on unilateral spatial neglect. NeuroReport 2015;26(8):462-6. [DOI] [PubMed] [Google Scholar]
Niemeier 1998 {published data only}
- Niemeier JP. The Lighthouse Strategy: use of a visual imagery technique to treat visual inattention in stroke patients. Brain Injury 1998;12(5):399-406. [DOI] [PubMed] [Google Scholar]
Osawa 2010 {published data only}
- Osawa A, Maeshima S. Family participation can improve unilateral spatial neglect in patients with acute right hemispheric stroke. European Neurology 2010;63:170-5. [DOI] [PubMed] [Google Scholar]
Paolucci 1996 {published and unpublished data}
- Antonucci G, Guariglia C, Judica A, Magnotti L, Paolucci S, Pizzamiglio L, et al. Effectiveness of neglect rehabilitation in a randomised group study. Journal of Clinical and Experimental Neuropsychology 1995;17(3):383-9. [DOI] [PubMed] [Google Scholar]
- Paolucci S, Antonucci G, Guariglia C, Magnotti L, Pizzamiglio L, Zoccolotti P. Facilitatory effect of neglect rehabilitation on the recovery of left hemiplegic stroke patients: a cross-over study. Journal of Neurology 1996;243:308-14. [DOI] [PubMed] [Google Scholar]
Patole 2015 {published data only}
- Patole RR, Kulkarni VN, Rairikar SA, Shyam AK, Sancheti PK. Effect of task specific treatment in patients with unilateral neglect. Indian Journal of Physiotherapy and Occupational Therapy 2015;9(1):74-7. [Google Scholar]
Pizzamiglio 2004 {published data only}
- Pizzamiglio L, Fasotti L, Jehkonen M, Antonucci G, Magnotti L, Boelen D, et al. The use of opto-kinetic stimulation in rehabilitation of the hemi-neglect disorder. Cortex 2004;40:441-50. [DOI] [PubMed] [Google Scholar]
Rossetti 1998 {published and unpublished data}
- Rossetti Y, Rode G, Pisella L, Farne A, Li L, Boisson D, et al. Prism adaptation to a rightward optical deviation rehabilitates left hemispatial neglect. Nature 1998;395(6698):166-9. [DOI] [PubMed] [Google Scholar]
Rossetti 2005 {unpublished data only}
- Rossetti Y. Personal communication, 2005.
Rossi 1990 {published data only}
- Rossi P, Kheyfets S, Reding M. Fresnel prisms improve visual perception in stroke patients with homonymous hemianopia or unilateral visual neglect. Neurology 1990;40:1597-9. [DOI] [PubMed] [Google Scholar]
Schindler 2002 {published data only}
- Schindler I, Kerkhoff G, Karnath H-O, Keller I, Goldenberg G. Neck muscle vibration induces lasting recovery in spatial neglect. Journal of Neurology, Neurosurgery and Psychiatry 2002;73:412-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schmidt 2013 {published data only}
- Schmidt L, Keller I, Utz KS, Artinger F, Stumpf O, Kerkhoff G. Galvanic vestibular stimulation improves arm position sense in spatial neglect: a sham-stimulation-controlled study. Neurorehabilitation and Neural Repair 2013;27(6):497-506. [DOI] [PubMed] [Google Scholar]
Serino 2006 {published data only}
- Serino A, Angeli V, Frassinetti F, Ladavas E. Mechanisms underlying neglect recovery after prism adaptation. Neuropsychologia 2006;44:1068-78. [DOI] [PubMed] [Google Scholar]
Serino 2009 {published data only}
- Serino A, Barbiani M, Rinaldesi ML, Ladavas E. Effectiveness of prism adaptation in neglect rehabilitation: a controlled trial study. Stroke 2009;40:1392-8. [DOI] [PubMed] [Google Scholar]
Svaerke 2019 {published data only}
- Svaerke KW, Omkvist KV, Havsteen IB, Christensen HK. Computer-based cognitive rehabilitation in patients with visuospatial neglect or homonymous hemianopia after stroke. Journal of Stroke & Cerebrovascular Diseases 2019;28(11):1-9. [DOI] [PubMed] [Google Scholar]
Tham 1997 {published data only}
- Tham K, Tegner R. Video feedback in the rehabilitation of patients with unilateral neglect. Archives of Physical Medicine and Rehabilitation 1997;78:410-3. [DOI] [PubMed] [Google Scholar]
Toglia 2009 {published data only}
- Toglia J, Cermak SA. Dynamic assessment and prediction of learning potential in clients with unilateral neglect. American Journal of Occupational Therapy 2009;63(5):569-79. [DOI] [PubMed] [Google Scholar]
Trudell 2003 {published data only}
- Trudell C, Bodian L, Demaio JH, Cheskes BE, Reding M. Comparison of hemi-field fresnel prisms versus patching for visual neglect after stroke. Archives of Physical Medicine and Rehabilitation 2003;84:A9. [Google Scholar]
Turgut 2018 {published data only}
- Turgut N, Möller L, Dengler K, Steinberg K, Sprenger A, Eling P, et al. Adaptive cueing treatment of neglect in stroke patients leads to improvements in activities of daily living: a randomized controlled, crossover trial. Neurorehabilitation & Neural Repair 2018;32(11):988-98. [DOI] [PubMed] [Google Scholar]
Vaes 2016 {published data only}
- Vaes N, Nys G, Lafosse C, Dereymaeker L, Oostra K, Hemelsoet D, et al. Rehabilitation of visuospatial neglect by prism adaptation: effects of a mild treatment regime. A randomised controlled trial.. Neuropsychological Rehabilitation 2016;28(6):899-918. [DOI] [PubMed] [Google Scholar]
Van Kessel 2013 {published data only}
- Van Kessel ME, Geurts ACH, Brouwer WH, Fasotti L. Visual scanning training for neglect after stroke with and without a computerized lane tracking dual task. Frontiers in Human Neuroscience 2013;7:358. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Os 1991 {published data only}
- Van Os ES, Driessen M-J, Wagenaar RC. Visual scanning training in stroke patients. Nederlands Tijdschrift voor Ergotherapie 1991;19:47-53. [Google Scholar]
Van Puymbroeck 2014 {published data only}
- Van Puymbroeck M, Allsop J, Miller KK, Schmid AA. Improvements in ICF components in individuals with chronic stroke following a yoga-based intervention. American Journal of Recreation Therapy 2014;95(10):24. [Google Scholar]
Webster 2001 {published data only}
- Webster JS, McFarland PT, Rapport LJ, Morrill B, Roades LA, Abadee PS. Computer-assisted training for improving wheelchair mobility in unilateral neglect patients. Archives of Physical Medicine and Rehabilitation 2001;82:769-75. [DOI] [PubMed] [Google Scholar]
Weinberg 1977 {published data only}
- Weinberg J, Diller L, Gordon W, Gerstman L, Lieberman A, Lakin P, et al. Visual scanning training effect on reading-related tasks in acquired right brain damage. Archives of Physical Medicine and Rehabilitation 1977;58:479-86. [PubMed] [Google Scholar]
Weinberg 1979 {published data only}
- Weinberg J, Diller L, Gordon W, Gerstman L, Lieberman A, Lakin P, et al. Training sensory awareness and spatial organisation in people with right brain damage. Archives of Physical Medicine and Rehabilitation 1979;60:491-7. [PubMed] [Google Scholar]
Weinberg 1982 {published data only}
- Weinberg J, Piasetsky E, Diller L, Gordon W. Treating perceptual organisation deficits in nonneglecting RBD stroke patients. Journal of Clinical Neuropsychology 1982;4(1):59-75. [DOI] [PubMed] [Google Scholar]
Young 1983 {published data only}
- Young G, Collins D, Hren M. Effect of pairing scanning training with block design training in the remediation of perceptual problems in left hemiplegics. Journal of Clinical Neuropsychology 1983;5(3):210-2. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Cazzoli 2015 {published data only}
- Cazzoli D, Rosenthal CR, Kennard C, Zito GA, Hopfnere S, Muri RM, et al. Theta burst stimulation improves overt visual search in spatial neglect independently of attentional load. Cortex 2015;73:317-29. [DOI] [PubMed] [Google Scholar]
Chan 2013 {published data only}
- Chan DYK, ManDWK. Unilateral neglect in stroke: a comparative study. Topics in Geriatric Rehabilitation: 2013;29(2):126-34. [Google Scholar]
Chan 2017 {unpublished data only}
Hauer 2007 {published and unpublished data}
- Hauer B, Qirbach A. Unilateral neglect: prism adaptation as an economic and effective therapy? [Unilateraler Neglect: Prismenadaptation als ökonomische und effefktive Therapie?]. Zeitschrift für Neuropsychologie 2007;18(3):171-81. [Google Scholar]
Iwata 2017 {unpublished data only}JPRN‐UMIN000020114
Lim 2017 {unpublished data only}
Marandola 2020 {published data only}
- Marandola MM, Jimenez-Martin I, Rodriguez-Yanez M, Arias-Rivas S, Santamaria-Calavid M, Castillo J. Constraint-induced movement therapy in the rehabilitation of hemineglect after a stroke. Revista de Neurologia 2020;70(4):119-26. [DOI] [PubMed] [Google Scholar]
Mueller‐Planitz 2017 {unpublished data only}
Park 2021 {published data only}
- Park JH. The effects of robot-assisted left-hand training on hemispatial neglect in older patients with chronic stroke. Medicine (Baltimore) 2021;100(9):e24781. [DOI] [PMC free article] [PubMed] [Google Scholar]
Saevarsson 2010 {published data only}
- Saevarsson S, Kristjánsson Á, Halsband U. Strength in numbers: combining neck vibration and prism adaptation produces additive therapeutic effects in unilateral neglect. Neuropsychological Rehabilitation 2010;20(5):704–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Seo 2017 {unpublished data only}KCT0001601
Toglia 2020 {published data only}
- Toglia J, Chen P. Spatial exploration strategy training for spatial neglect: a pilot study. Neuropsychological Rehabilitation 2020;online:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vilimovsky 2021 {published data only}
- Vilimovsky T, Chen P, Hoidekrova K, Petioky J, Harsa P. Prism adaptation treatment to address spatial neglect in an intensive rehabilitation program: a randomized pilot and feasibility trial. PLoS ONE 2021;16(1):1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zigiotto 2020 {published data only}
- Zigiotto L, Damora A, Albini F, Casati C, Scrocco G, Mancuso M, et al. Multisensory stimulation for the rehabilitation of unilateral spatial neglect. Neuropsychological Rehabilitation 2020;online:1. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Elshout 2018 {published data only}
- Elshout JA, Nijboer TCW, Van Der Stigchel S. Is congruent movement training more effective than standard visual scanning therapy to ameliorate symptoms of visuospatial neglect? Study protocol of a randomised control trial. BMJ Open 2019;9(12):1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
ISRCTN88395268 {published data only}http://www.isrctn.com/ISRCTN88395268
- ISRCTN88395268. A feasibility study for attention loss after stroke [A feasibility study of prisms and therapy in attention loss after stroke (SPATIAL feasibility)]. https://www.isrctn.com/ISRCTN88395268 (first received 8 January 2019).
Luvizutto 2017 {unpublished data only}RBR‐78jvzx
- Luvizutto GJ, Rizzati GRS, Fogaroli MO, Rodrigues RT, Ribeiro PW, Carvalho Nunes HR, et al. Treatment of unilateral spatial neglect after stroke using transcranial direct current stimulation (ELETRON trial): study protocol for a randomized controlled trial. Trials 2016;17(1):479. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT00989430 {unpublished data only}
- NCT00989430. Prism adaptation therapy for spatial neglect [Prism adaptation therapy for spatial neglect: theoretical and practical outcomes]. https://clinicaltrials.gov/ct2/show/NCT00989430 (first received 5 October 2009).
NCT02213640 {unpublished data only}
- NCT02213640. Potentiation of the effects of prismatic adaptation by transcranial direct current stimulation (tDCS): evaluation of functional interest in negligence rehabilitation (PRIStiM1). https://clinicaltrials.gov/ct2/show/NCT02213640 (first received 11 August 2014).
NCT02680171 {unpublished data only}
- NCT02680171. Feasibility and effectiveness study of implementing prism adaptation as a treatment for spatial neglect after stroke [Feasibility and effectiveness study of implementing prism adaptation as a treatment for spatial neglect after right hemisphere stroke]. https://clinicaltrials.gov/ct2/show/NCT02680171 (first received 11 February 2016).
NCT03168360 {published data only}
- NCT03168360. Effect of intensive cognitive rehabilitation in subacute stroke patient. https://clinicaltrials.gov/ct2/show/NCT03168360 (first received 30 May 2017).
NCT03317860 {published data only}
- NCT03317860. Improving measurement and treatment of post-stroke neglect. https://clinicaltrials.gov/ct2/show/NCT03317860 (first received 23 October 2017).
NCT03402906 {published data only}
- NCT03402906. Family-clinician collaboration to improve neglect and rehabilitation outcome after stroke. https://clinicaltrials.gov/ct2/show/NCT03402906 (first received 18 January 2018).
NCT03451708 {published data only}
- NCT03451708. OKS for the treatment of hemispatial neglect [Optokinetic stimulation for the treatment of hemispatial neglect - safety and efficacy studies]. https://clinicaltrials.gov/ct2/show/NCT03451708 (first received 2 March 2018).
NCT03458611 {published data only}
- NCT03458611. Virtual Reality Attention Training in stroke patients (VRAT) [Virtual reality attention training in stroke patients]. https://clinicaltrials.gov/ct2/show/NCT03458611 (first received 8 March 2018).
NCT03854487 {published data only}
- NCT03854487. Effect of mirror therapy on unilateral neglect for patients after stroke. https://clinicaltrials.gov/ct2/show/NCT03854487 (first received 26 February 2019).
NCT03887962 {published data only}
- NCT03887962. Virtual environment rehabilitation for patients with motor neglect trial (VERMONT) [Trial of virtual reality biofeedback in patients with motor neglect from chronic pain or cerebrovascular disease]. https://clinicaltrials.gov/ct2/show/NCT03887962 (first received 25 March 2019).
NCT04080999 {published data only}
- NCT04080999. Repetitive transcranial magnetic stimulation in spatial attention after stroke (r-TMS) [Efficacy of repetitive transcranial magnetic stimulation (r-TMS) combined with conventional cognitive treatment on cognitive-behavioral symptoms of left hemispatial neglect in right-stroke patients within three months post-onset compared to conventional cognitive treatment only: a randomized controlled trial]. https://clinicaltrials.gov/ct2/show/NCT04080999 (first received 6 September 2019).
NCT04227132 {published data only}
- NCT04227132. Evaluation of an adaptive computerized training for rehabilitation of spatial neglect in stroke survivors (MULTITASK) [Modulation of visuospatial awareness during multi-tasking in right hemisphere stroke patients: towards novel behavioural and neurofunctional predictors of impairments and recovery of the attentional network]. https://clinicaltrials.gov/ct2/show/NCT04227132 (first received 13 January 2020).
NCT04273620 {published data only}
- NCT04273620. Combined optokinetic stimulation and cueing-based reading therapy to treat hemispatial neglect following stroke (OKS-READ) [Randomized controlled trial of combined optokinetic stimulation and cueing-based reading therapy to treat hemispatial neglect following stroke (OKS-READ study)]. https://clinicaltrials.gov/ct2/show/NCT04273620 (first received 18 February 2020).
NL8145 {published data only}
- NL8145. Modulating connectivity with non-invasive brain stimulation during spatial neglect rehabilitation. https://www.trialregister.nl/trial/8145 (first received 10 September 2019).
Olson 2020 {unpublished data only}
- Caloric vestibular stimulation for treatment of unilateral neglect. Ongoing study. Unknown. Contact author for more information.
Additional references
Azouvi 1996
- Azouvi P, Marchal F, Samuel C, Morin L, Renard C, Louis-Dreyfus A, et al. Functional consequences and awareness of unilateral neglect: study of an evaluation scale. Neuropsychological Rehabilitation 1996;6(2):133-50. [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4:561-71. [DOI] [PubMed] [Google Scholar]
Berg 1992
- Berg K, Wood-Dauphine SL, Williams JL, Gayton D. Measuring balance in the elderly: validation of an instrument. Canadian Journal of Public Health 1992;S2:7-11. [PubMed] [Google Scholar]
Bosma 2020
- Bosma MS, Nijboer TCW, Caljouw MAA, Achterberg WP. Impact of visuospatial neglect post-stroke on daily activities, participation and informal caregiver burden: a systematic review. Annals of Physical and Rehabilitation Medicine 2020;63(4):344-58. [DOI] [PubMed] [Google Scholar]
Bowen 2011
- Bowen A, Knapp P, Gillespie D, Nicolson DJ, Vail A. Non-pharmacological interventions for perceptual disorders following stroke and other adult-acquired, non-progressive brain injury. Cochrane Database of Systematic Reviews 2011, Issue 4. Art. No: CD007039. [DOI: 10.1002/14651858.CD007039.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bush 2006
- Bush JW, Kaplan RM. The quality of well-being scale (formerly the index of well-being). In: McDowell I, editors(s). Measuring Health. A Guide to Rating Scales and Questionnaires. 3rd edition. New York: Oxford University Press, 2006:675–83. [Google Scholar]
Checketts 2020
- Checketts M, Mancuso M, Fordell H, Chen P, Hreha K, Eskes GA, et al. Current clinical practice in the screening and diagnosis of spatial neglect post-stroke: findings from a multidisciplinary international survey. Neuropsychological Rehabilitation 2020;online:1-33. [DOI] [PubMed] [Google Scholar]
Cochrane Handbook
- Higgins JT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Collin 1988
- Collin C, Wade D, Davies S, Horne V. The Barthel ADL Index: a reliability study. International Disability Studies 1988;10:61-3. [DOI] [PubMed] [Google Scholar]
Cotoi 2018
- Cotoi A, Mirkowski M, Iruthayarajah J, Anderson R, Teasell R. The effect of theta-burst stimulation on unilateral spatial neglect following stroke: a systematic review. Clinical Rehabilitation 2019;33(2):183-94. [DOI] [PubMed] [Google Scholar]
Das Nair 2007
- Das Nair R, Lincoln N. Cognitive rehabilitation for memory deficits following stroke. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No: CD002293. [DOI: 10.1002/14651858.CD002293.pub2] [DOI] [PubMed] [Google Scholar]
Duncan 1990
- Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. Journal of Gerontology 1990;45(6):192-7. [DOI] [PubMed] [Google Scholar]
Edmans 1997
- Edmans JA, Webster J. The Edmans ADL Index: validity and reliability. Disability and Rehabilitation 1997;19(11):465-76. [DOI] [PubMed] [Google Scholar]
Elsner 2020
- Elsner B, Kugler J, Pohl M, Mehrholz J. Transcranial direct current stimulation (tDCS) for improving activities of daily living, and physical and cognitive functioning, in people after stroke. Cochrane Database of Systematic Reviews 2020, Issue 11. Art. No: CD009645. [DOI: 10.1002/14651858.CD009645.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Flanagan 1978
- Flanagan JC. A research approach to improving our quality of life. American Psychologist 1978;33:138-47. [Google Scholar]
Goldberg 1970
- Goldberg DP, Blackwell B. Psychiatric illness in general practice. A detailed study using a new method of case identification. British Medical Journal 1970;1:439-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Graf 2008
- Graf C. The Lawton instrumental activities of daily living scale. American Journal of Nursing 2008;108(4):52-62. [DOI] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction - GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383-94. [DOI] [PubMed] [Google Scholar]
Hammerbeck 2019
- Hammerbeck U, Gittins M, Vail A, Paley L, Tyson SF, Bowen A. Spatial neglect in stroke: identification, disease process and association with outcome during inpatient rehabilitation. Brain Sciences 2019;9(374):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Heilman 2003
- Heilman KM, Watson RT, Valenstein E. Neglect and related disorders. In: Heilman KM, Valenstein E, editors(s). Clinical Neuropsychology. 4th edition. New York: Oxford University Press, 2003:296-346. [Google Scholar]
Hill 1996
- Hill KD, Bernhardt J, McGann AM, Maltese D, Berkovits D. New test of dynamic standing balance for stroke patients: reliability, validity and comparison with healthy elderly. Physiotherapy Canada 1996;48(4):257-62. [Google Scholar]
Hoffman 2014
- Hoffmann T, Glasziou P, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2017;348(g1687):1-12. [DOI] [PubMed] [Google Scholar]
Holbrook 1983
- Holbrook M, Skilbeck CE. An activities index for use with stroke patients. Age and Ageing 1983;12(2):166-70. [DOI] [PubMed] [Google Scholar]
Hou 2020
- Hou Y, Liu Y, Li M, Ning B, Wen Z, Fu W. Acupuncture plus rehabilitation for unilateral neglect after stroke: a systematic review and meta-analysis. Evidence-Based Complementary and Alternative Medicine 2020;2020:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
ISWP 2016
- Intercollegiate Stroke Working Party. National Clinical Guideline for Stroke. 5th edition. London: Royal College of Physicians, 2016. [Google Scholar]
Jehkonen 2006
- Jehkonen M, Laihosalo M, Kettunen JE. Impact of neglect on functional outcome after stroke: a review of methodological issues and recent research findings. Restorative Neurology and Neuroscience 2006;24:209-15. [PubMed] [Google Scholar]
Katz 1963
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. Journal of the American Medical Association 1963;185:914-9. [DOI] [PubMed] [Google Scholar]
Keith 1987
- Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. Advances in Clinical Rehabilitation 1987;1:6-18. [PubMed] [Google Scholar]
Kwon 2018
- Kwon J-S. Therapeutic intervention for visuo-spatial neglect after stroke: a meta-analysis of randomized controlled trials. Osong Public Health and Research Perspectives 2018;9(2):59-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lincoln 1990
- Lincoln NB, Edmans JA. A re-validation of the Rivermead ADL scale for elderly patients with stroke. Age and Ageing 1990;19(1):19-24. [DOI] [PubMed] [Google Scholar]
Lincoln 2001
- Lincoln NB, Majid MJ, Weyman N. Cognitive rehabilitation for attention deficits following stroke. Cochrane Database of Systematic Reviews 2001, Issue 3. Art. No: CD002842. [DOI: 10.1002/14651858.CD002842] [DOI] [PubMed] [Google Scholar]
Loetscher 2019
- Loetscher T, Potter KJ, Wong D, das Nair R. Cognitive rehabilitation for attention deficits following stroke. Cochrane Database of Systematic Reviews 2019, Issue 11. Art. No: CD002842. [DOI: 10.1002/14651858.CD002842.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Luvizutto 2015
- Luvizutto GJ, Bazan R, Braga GP, Resende LADL, Bazan SGZ, El Dib R. Pharmacological interventions for unilateral spatial neglect after stroke. Cochrane Database of Systematic Reviews 2015, Issue 11. Art. No: CD010882. [DOI: 10.1002/14651858.CD010882.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Müri 2013
- Müri RM, Cazzoli D, Nef T, Mosimann UP, Hopfner S, Nyffeler T. Non-invasive brain stimulation in neglect rehabilitation: an update. Frontiers in Human Neuroscience 2013;7(248):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
NICE 2013
- National Institute for Health and Care Excellence. Stroke Rehabilitation in Adults. Clinical Guideline CG162. Manchester: NICE, 2013. [PubMed] [Google Scholar]
Nijboer 2013
- Nijboer T, Van de Port I, Schepers V, Post M, Visser-Meily A. Predicting functional outcome after stroke: the influence of neglect on basic activities in daily living. Frontiers in Human Neuroscience 2013;7:182. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nouri 1987
- Nouri FM, Lincoln NB. An extended activities of daily living scale for stroke patients. Clinical Rehabilitation 1987;1:301-5. [Google Scholar]
Podsiadlo 1991
- Podsiadlo D, Richardson S. The timed “Up & go”: a test of basic functional mobility for frail elderly persons. Journal of the American Geriatrics Society 1991;39:142-8. [DOI] [PubMed] [Google Scholar]
Rode 2017
- Rode G, Pagliari C, Huchon L, Rossetti Y, Pisella L. Semiology of neglect: an update. Annals of Physical and Rehabilitation Medicine 2017;60(3):177-85. [DOI] [PubMed] [Google Scholar]
Rossetti 1998
- Rossetti Y, Rode G, Pisella L, Farné A, Li L, Boisson D, et al. Prism adaptation to a rightward optical deviation rehabilitates left hemispatial neglect. Nature 1998;395(6698):166-9. [DOI] [PubMed] [Google Scholar]
Salazar 2018
- Salazar APS, Vaz PG, Marchese RR, Stein C, Pinto C, Pagnussat AS. Noninvasive brain stimulation improves hemispatial neglect after stroke: a systematic review and meta-analysis. Archives of Physical Medicine and Rehabilitation 2018;99(2):355-66. [DOI] [PubMed] [Google Scholar]
SIGN 2010
- Scottish Intercollegiate Guidelines Network. Sign Guideline 118. Management of patients with stroke: rehabilitation, prevention and management of complications, and discharge planning: a national clinical guideline. Edinburgh: NHS Quality Improvement Scotland, 2010. [Google Scholar]
Song 2005
- Song FJ, Jerosch-Herold CJ, Harvey I, Drachler M, Holland R, Mares K. Can parametric statistical methods be used to analyse and present ordinal Barthel data in trials of post-stroke interventions? In: Proceedings of the European Stroke Conference. 2005.
Towle 1991
- Towle D, Lincoln NB. Development of a questionnaire for detecting everyday problems in stroke patients with unilateral visual neglect. Clinical Rehabilitation 1991;5(2):135-40. [Google Scholar]
Van Bennekom 1995
- Van Bennekom CA, Jelles F, Lankhorst GJ. Rehabilitation Activities Profile: the ICIDH as a framework for a problem-oriented assessment method in rehabilitation medicine. Disability and Rehabilitation 1995;17(3-4):169-75. [DOI] [PubMed] [Google Scholar]
Wade 1985
- Wade D, Skilbeck C, David R, Langton-Hewer R. Stroke: A Critical Approach to Diagnosis, Treatment and Management. London: Chapman and Hall, 1985. [Google Scholar]
Ware 1992
- Ware JE Jr, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36). I. Conceptual framework and item selection. Medical Care 1992;30:473-83. [PubMed] [Google Scholar]
Wilson 1987
- Wilson B, Cockburn J, Halligan P. Development of a behavioral test of visuospatial neglect. Archives of Physical Medicine and Rehabilitation 1987;68:98-102. [PubMed] [Google Scholar]
Wilson 2005
- Wilson LJT, Hareendran A, Hendry A, Potter J, Bone I, Muir KW. Reliability of the Modified Rankin Scale across multiple raters: benefits of a structured interview. Stroke 2005;36:777-81. [DOI] [PubMed] [Google Scholar]
Yardley 2005
- Yardley L, Beyer N, Hauer K. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age and Ageing 2005;34:614-9. [DOI] [PubMed] [Google Scholar]
Yesavage 1983
- Yesavage A, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. Journal of Psychiatric Research 1983;17:37-49. [DOI] [PubMed] [Google Scholar]
Zigmond 1983
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica 1983;67:361-70. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Bowen 2013
- Bowen A, Hazelton C, Pollock A, Lincoln NB. Cognitive rehabilitation for spatial neglect following stroke. Cochrane Database of Systematic Reviews 2013, Issue 7. Art. No: CD003586. [DOI: 10.1002/14651858.CD003586.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]


