Abstract
Background:
The retrosigmoid approach represents a crucial surgical route to address different lesions in the cerebellopontine angle but cerebrospinal fluid (CSF) leak still remains the most frequent complication after this approach. Here, we analyzed the impact of different factors in CSF leak development after a retrosigmoid approach. Identifying risk factors related to a specific approach may help the surgeon to tailor the perioperative management and to appropriately counsel patients regarding their risk profile.
Methods:
We retrospectively reviewed the clinical, surgical, and outcome data of 103 consecutive patients (M/F, 47/56; mean follow-up 35.6 ± 23.9 months) who underwent a retrosigmoid approach for different cerebellopontine angle pathologies and studied the impact of different factors on the occurrence of a CSF leak to univariate and multivariate analysis.
Results:
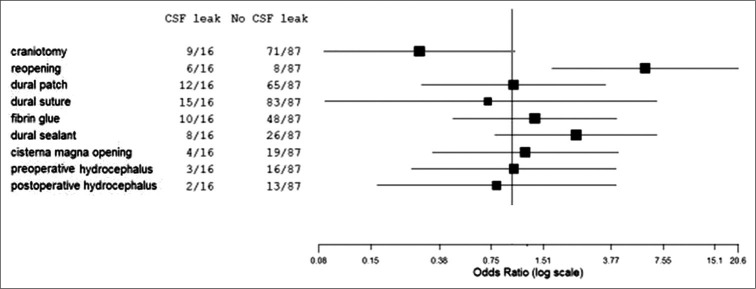
Seventy-nine patients (76.7%) were operated for tumors growing in the cerebellopontine angle. Twenty-four patients (23.2%) underwent microvascular decompression to treat a drug-resistant trigeminal neuralgia. Sixteen patients (15.5%) developed CSF leak in the postoperative course of which six underwent surgical revision. Performing a craniectomy as surgical procedure (P = 0.0450) and performing a reopening procedure (second surgery; P = 0.0079) were significantly associated to a higher risk of developing CSF leak. Moreover, performing a reopening procedure emerged as an independent factor for CSF developing on multivariate analysis (P = 0.0156).
Conclusion:
Patients submitted to craniectomy and patients who underwent a second surgery showed an higher CSF leak rate. Ongoing improvement of biomaterial technology may help neurosurgeons to prevent this potentially life-threatening complication.
Keywords: Craniotomy, Cerebrospinal fluid leak, Craniectomy, Neurovascular conflict, Retrosigmoid approach, Vestibular schwannoma

INTRODUCTION
The retrosigmoid approach represents an excellent surgical route to address various tumors and vascular lesions in the cerebellopontine angle.[6,17,18,20,24] Despite the continuous evolution and refinements of the surgical technique, the recent introduction of new biomaterials for dural and bone reconstruction, along with the growing awareness and experience of the neurosurgeons, cerebrospinal fluid (CSF) leak still remains the most frequent complication after this approach, with a reported overall rate up to 22%.[8,9,17] This complication negatively affects patients outcome, being associated with risk of meningitis, need for reoperation, increased hospital stay, and increased costs.[4,5,7,14,15,25,26] The majority of studies on this topic have investigated the risk factors for CSF leak in the surgery of the vestibular schwannoma.[3,7,12,13,26] However, the surgery of a vestibular schwannoma carries specific problems which may directly impact on the developing of specific complications such as CSF leak. Moreover, most of these series were focused on comparing the results of the retrosigmoid and the translabyrinthine approaches in that particular surgical scenario. Thus, the aim of our study was to analyze the impact of different factors in CSF leak development after a retrosigmoid approach regardless the pathology treated. Identifying risk factors related to a specific approach may help the surgeon to tailor the perioperative management and to appropriately counsel patients regarding their risk profile.
MATERIALS AND METHODS
We retrospectively reviewed the clinical, surgical and outcome data of 103 consecutive patients (M/F, 47/56) who underwent a retrosigmoid approach for cerebellopontine angle pathologies between February 2013 and December 2019 at our department. The mean age was 53.6 ± 15.4 years and the mean follow-up was 35.6 ± 23.9 months. We studied the role of factors such as age, sex, the type of pathology, the evidence of preoperative and postoperative hydrocephalus, and the type of surgical procedure (craniotomy/craniectomy) or if the procedure was a reopening (second surgery), the cisterna magna opening during surgery, the use of dural suture, dural patch, fibrin glue, and other dural sealants during surgery on the occurrence of a CSF leak (subcutaneous collection, incisional leak, CSF rhinorrhea, and CSF otorrhea) in the postoperative course of these patients. The surgical procedures were performed by different neurosurgeons thus the closure techniques varied according to the surgeon’s preference. The dura was sutured either with a 3–0 silk suture (40 cases) or with a 4–0 nylon suture (58 cases). An artificial dural substitute was used in all cases of dural patch (77 cases). For patients in whom CSF leak occurred, the type of treatment was also recorded. Statistical comparison of categorical variables was performed by χ2 statistic, using the Fisher exact test. A multivariate logistic regression model was used to estimate the odds ratio of developing a CSF leak, while adjusting for baseline variables. Differences were considered significant at P < 0.05. Statistical analyses were done using StatView version 5 software (SAS Institute Inc.).
RESULTS
Data of patients are summarized in Table 1. Briefly, 79 patients (76.7%) were operated for tumors growing in the cerebellopontine angle (62 vestibular schwannoma, three trigeminal schwannoma, three mixed nerve schwannoma, one facial schwannoma, seven meningioma, and three other tumors). Twenty-four patients (23.2%) underwent microvascular decompression to treat a drug-resistant trigeminal neuralgia. Nineteen out of 103 patients had hydrocephalus at presentation. Postoperative CSF leak was noted in 16 patients (15.5%), of which nine presented with a subcutaneous CSF collection, three with an incisional CSF leak, and four with CSF rhinorrhea. No CSF otorrhea was recorded. Six patients required a reoperation for the CSF leak [Table 2]. On univariate analysis, we found that performing a craniectomy as surgical procedure (P = 0.0450) and performing a reopening procedure (P = 0.0079) were significantly associated to a higher risk of developing CSF leak. The reopening procedure emerged as an independent factor for CSF developing on multivariate analysis (P = 0.0156; Table 3 and Figure 1).
Table 1:
Clinical and outcome data of patients submitted to retrosigmoid approach for cerebellopontine angle surgery.
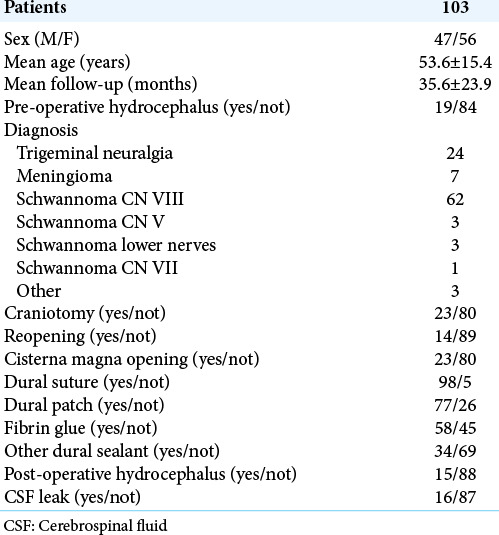
Table 2:
Treatment of patients who developed CSF leak after a retrosigmoid approach.
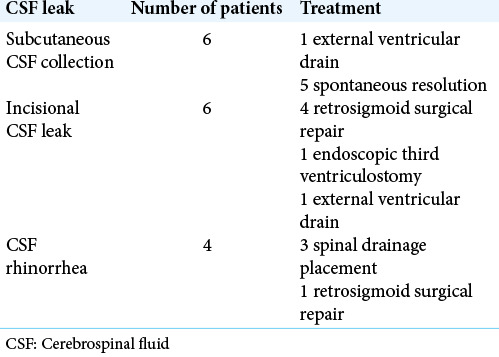
Table 3:
Multivariate analysis (logistic regression model) of factors possibly influencing the onset of CSF leak.
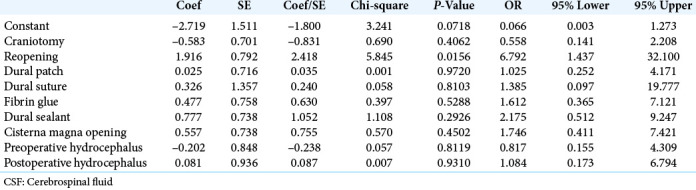
Figure 1:
Forest plot of multivariate logistic regression analysis demonstrating the reopening as the only independent prognostic factor for cerebrospinal fluid leak development.
DISCUSSION
The retrosigmoid approach to the cerebellopontine angle, first popularized in the 1930s by Dandy,[9] remains a crucial route in the surgical management of various pathologies. Despite several important modifications introduced through the following decades, this approach still remains associated with high rates of postoperative CSF leak. The aim of this study was to evaluate which factors were significantly associated with the developing of CSF leak in the retrosigmoid approach. To do this we studied different preoperative features, intraoperative technical nuances and postoperative findings of patients submitted to this approach. Several factors potentially contributing to the development of a postoperative CSF leak following retrosigmoid approach have been described. While age, sex and the evidence of a pre- and post-operative hydrocephalus have been reported associated with CSF leak,[3,4,7,27] these factors did not correlate with an increased risk of leakage in our series. Moreover, we included in our analysis many different pathologies operated through the retrosigmoid approach most of which were vestibular schwannoma and neurovascular conflicts. Even if in our series the kind of pathology operated did not correlate with an increased risk of leakage, it has been reported that resecting a vestibular schwannoma may carry adjunctive risks because of the need of drilling the petrous bone of the internal auditory canal to obtain a gross total resection of the tumor. This maneuver may expose the petrous air cells which can potentially result in CSF rhinorrhea.[26,27] In our series, we found that performing a craniotomy as surgical procedure was significantly associated with a lower risk of CSF leak. The previous studies[10,16,29] reported an increased risk of leakage in patients submitted to retrosigmoid craniectomy compared with cases submitted to retrosigmoid craniotomy. For example, Legnani et al.,[16] in a series of 152 patients, reported a complication rate associated to craniotomy significantly lower than in the craniectomy group (7% vs. 33%) and Teo and Eljamel[29] observed a CSF leak rate of 6.6% in craniotomy group and 20% in craniectomy group, respectively. Probably replacing the bone flap between the dura and the muscles, could prevent the adhesion and traction between the two different layers, thereby reducing the risk of dural tearing.[10] However, the use of some biomaterial such as the polymethylmethacrylate cement,[21,23] the hydroxyapatite bone cement,[1] and the demineralized bone matrix[22] has been reported effective in reducing the CSF leak after a retrosigmoid craniectomy. Nonetheless no case of CSF leak in a recent series of 86 patients submitted to the replacement of bone flap with primary dural closure without the use of allo- or autografts has been recently reported.[30] Performing a reopening procedure significantly increased the risk to have a CSF leak in the postoperative course of our patients. Duong et al. found a significantly higher CSF leak rate up to 50% after a second surgery in patients submitted to a retrosigmoid approach.[11] The possible mechanism might be related to the fact that a second surgery is a more difficult procedure requiring a longer operative time. This could lead to an accumulation of more blood and proteinaceous debris in CSF thereby inhibiting the normal CSF circulation postoperatively.[7] Moreover, in second surgeries a scarred and hardened dura with impaired physiological microcirculation could have a decreased healing tendency and could be prone to dural tears.[27] In patients operated for a vestibular schwannoma recurrence an adjunctive mechanism has been proposed. In these cases, CSF leak could be related to the opening of air cells at the internal auditory canal opened in a previous surgery and obstructed only partly by postoperative scarring. Thus, a broader covering of the internal auditory canal with autologous fat tissue and fibrin glue has been proposed to prevent the leakage in these cases.[27] Regardless the mechanisms involved in CSF leak occurrence, it is crucial its rapid identification and treatment due to the possibility of developing a life-threatening meningitis. In our series, 83.3% of patients with subcutaneous collections resolved spontaneously without need for any treatment [Table 2]. On the other hand, all patients with incisional leak and rhinorrhea required a treatment (40% of cases resolved after a CSF drainage and 60% required a reoperation, respectively; Table 2). However, no further complications were recorded in patients with CSF leak, confirming previous results.[27]
Our study has some limitations due to the retrospective nature of data. For this reason, we were not able to study the impact of body mass index which might affect the complication rate in this type of surgery.[2,28] In addition, although we studied many different surgical nuances, we did not perform a subgroup analysis of different biomaterials used in our series to create more homogeneous groups to enhance the statistical power.
CONCLUSION
In our study, we identified subgroups of patients who were at risk for CSF leak occurrence after a retrosigmoid approach for the treatment of different pathologies. Patients submitted to craniectomy and patients who underwent a second surgery showed an higher CSF leak rate. Ongoing improvement of biomaterial technology[19] may help neurosurgeons to prevent this potentially life-threatening complication.
Footnotes
How to cite this article: Montano N, Signorelli F, Giordano M, D’Onofrio GF, Izzo A, D’Ercole M, et al. Factors associated with cerebrospinal fluid leak after a retrosigmoid approach for cerebellopontine angle surgery. Surg Neurol Int 2021;12:258.
Contributor Information
Nicola Montano, Email: nicolamontanomd@yahoo.it.
Francesco Signorelli, Email: francesco.signorelli1984@gmail.com.
Martina Giordano, Email: msmgiordano@gmail.com.
Federica Ginevra D’Onofrio, Email: ginevra.f.donofrio@gmail.com.
Alessandro Izzo, Email: izzo.alessandro88@gmail.com.
Manuela D’Ercole, Email: manuela.dercole@policlinicogemelli.it.
Eleonora Ioannoni, Email: e.ioannoni@libero.it.
Giovanni Pennisi, Email: giovannipennisi91@gmail.com.
Anselmo Caricato, Email: anselmo.caricato@unicatt.it.
Roberto Pallini, Email: roberto.pallini@unicatt.it.
Alessandro Olivi, Email: alessandro.olivi@policlinicogemelli.it.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Aldahak N, Dupre D, Ragaee M, Froelich S, Wilberger J, Aziz KM. Hydroxyapatite bone cement application for the reconstruction of retrosigmoid craniectomy in the treatment of cranial nerves disorders. Surg Neurol Int. 2017;8:115. doi: 10.4103/sni.sni_29_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bamgbade OA, Rutter TW, Nafiu OO, Dorje P. Postoperative complications in obese and nonobese patients. World J Surg. 2007;31:556–61. doi: 10.1007/s00268-006-0305-0. [DOI] [PubMed] [Google Scholar]
- 3.Brennan JW, Rowed DW, Nedzelski JM, Chen JM. Cerebrospinal fluid leak after acoustic neuroma surgery: Influence of tumor size and surgical approach on incidence and response to treatment. J Neurosurg. 2001;94:217–23. doi: 10.3171/jns.2001.94.2.0217. [DOI] [PubMed] [Google Scholar]
- 4.Bryce GE, Nedzelski JM, Rowed DW, Rappaport JM. Cerebrospinal fluid leaks and meningitis in acoustic neuroma surgery. Otolaryngol Head Neck Surg. 1991;104:81–7. doi: 10.1177/019459989110400115. [DOI] [PubMed] [Google Scholar]
- 5.Chern A, Hunter JB, Bennett ML. Cost analysis of cerebrospinal fluid leaks and cerebrospinal fluid leak prevention in patients undergoing cerebellopontine angle surgery. Otol Neurotol. 2016;38:147–51. doi: 10.1097/MAO.0000000000001252. [DOI] [PubMed] [Google Scholar]
- 6.Ciric I, Zhao JC, Rosenblatt S, Wiet R, O’Shaughnessy B. Suboccipital retrosigmoid approach for removal of vestibular schwannomas: Facial nerve function and hearing preservation. Neurosurgery. 2005;56:560–70. doi: 10.1227/01.neu.0000154059.34990.b8. [DOI] [PubMed] [Google Scholar]
- 7.Copeland WR, Mallory GW, Neff BA, Driscoll CL, Link MJ. Are there modifiable risk factors to prevent a cerebrospinal fluid leak following vestibular schwannoma surgery? J Neurosurg. 2015;122:312–6. doi: 10.3171/2014.10.JNS14432. [DOI] [PubMed] [Google Scholar]
- 8.Cueva RA, Mastrodimos B. Approach design and closure techniques to minimize cerebrospinal fluid leak after cerebellopontine angle tumor surgery. Otol Neurotol. 2005;26:1176–81. doi: 10.1097/01.mao.0000176174.94764.3b. [DOI] [PubMed] [Google Scholar]
- 9.Dandy WE. Removal of cerebellopontine (acoustic) tumors through a unilateral approach. Arch Surg. 1934;29:337–44. [Google Scholar]
- 10.Della Pepa GM, Montano N, Lucantoni C, Alexandre AM, Papacci F, Meglio M. Craniotomy repair with the retrosigmoid approach: The impact on quality of life of meticulous reconstruction of anatomical layers. Acta Neurochir (Wien) 2011;153:2255–8. doi: 10.1007/s00701-011-1113-3. [DOI] [PubMed] [Google Scholar]
- 11.Duong DH, O’Malley S, Sekhar LN, Wright DG. Postoperative hydrocephalus in cranial base surgery. Skull Base Surg. 2000;10:197–200. doi: 10.1055/s-2000-9331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Falcioni M, Romano G, Aggarwal N, Sanna M. Cerebrospinal fluid leak after retrosigmoid excision of vestibular schwannomas. Otol Neurotol. 2008;29:384–6. doi: 10.1097/MAO.0b013e31816021e3. [DOI] [PubMed] [Google Scholar]
- 13.Fishman AJ, Marrinan MS, Golfinos JG, Cohen NL, Roland JT., Jr Prevention and management of cerebrospinal fluid leak following vestibular schwannoma surgery. Laryngoscope. 2004;114:501–5. doi: 10.1097/00005537-200403000-00022. [DOI] [PubMed] [Google Scholar]
- 14.Hoffman RA. Cerebrospinal fluid leak following acoustic neuroma removal. Laryngoscope. 1994;104:40–58. doi: 10.1288/00005537-199401000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Khrais TH, Falcioni M, Taibah A, Agarwal M, Sanna M. Cerebrospinal fluid leak prevention after translabyrinthine removal of vestibular schwannoma. Laryngoscope. 2004;114:1015–20. doi: 10.1097/00005537-200406000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Legnani FG, Saladino A, Casali C, Vetrano IG, Varisco M, Mattei L, et al. Craniotomy vs craniectomy for posterior fossa tumors: A prospective study to evaluate complications after surgery. Acta Neurochir (Wien) 2013;155:2281–6. doi: 10.1007/s00701-013-1882-y. [DOI] [PubMed] [Google Scholar]
- 17.Ling PY, Mendelson ZS, Reddy RK, Jyung RW, Liu JK. Reconstruction after retrosigmoid approaches using autologous at graft-assisted Medpor Titan cranioplasty: Assessment of postoperative cerebrospinal fluid leaks and headaches in 60 cases. Acta Neurochir (Wien) 2014;156:1879–88. doi: 10.1007/s00701-014-2190-x. [DOI] [PubMed] [Google Scholar]
- 18.Mangham CA., Jr Retrosigmoid versus middle fossa surgery for small vestibular schwannomas. Laryngoscope. 2004;114:1455–61. doi: 10.1097/00005537-200408000-00026. [DOI] [PubMed] [Google Scholar]
- 19.Montano N, Giordano M, Caccavella VM, Ioannoni E, Polli FM, Papacci F, et al. Hemopatch® with fibrin glue as a Dural sealant in cranial and spinal surgery. A technical note with a review of the literature. J Clin Neurosci. 2020;79:144–7. doi: 10.1016/j.jocn.2020.07.011. [DOI] [PubMed] [Google Scholar]
- 20.Ojemann RG. Retrosigmoid approach to acoustic neuroma (vestibular schwannoma) Neurosurgery. 2001;48:553–8. doi: 10.1097/00006123-200103000-00018. [DOI] [PubMed] [Google Scholar]
- 21.Ou C, Chen Y, Mo J, Wang S, Gai S, Xing R, et al. Cranioplasty using polymethylmethacrylate cement following retrosigmoid craniectomy decreases the rate of cerebrospinal fluid leak and pseudomeningocele. J Craniofac Surg. 2019;30:566–70. doi: 10.1097/SCS.0000000000005168. [DOI] [PubMed] [Google Scholar]
- 22.Pabaney AH, Reinard KA, Asmaro K, Malik GM. Novel technique for cranial reconstruction following retrosigmoidcraniectomy using demineralized bone matrix. Clin Neurol Neurosurg. 2015;136:66–70. doi: 10.1016/j.clineuro.2015.05.034. [DOI] [PubMed] [Google Scholar]
- 23.Park JS, Kong DS, Lee JA, Park K. Intraoperative management to prevent cerebrospinal fluid leakage after microvascular decompression: Dural closure witha plugging muscle method. Neurosurg Rev. 2007;30:139–42. doi: 10.1007/s10143-006-0060-6. [DOI] [PubMed] [Google Scholar]
- 24.Samii M, Gerganov VM, Samii A. Functional outcome after complete surgical removal of giant vestibular schwannomas. J Neurosurg. 2010;112:860–7. doi: 10.3171/2009.7.JNS0989. [DOI] [PubMed] [Google Scholar]
- 25.Selesnick SH, Liu JC, Jen A, Newman J. The incidence of cerebrospinal fluid leak after vestibular schwannoma surgery. Otol Neurotol. 2004;25:387–93. doi: 10.1097/00129492-200405000-00030. [DOI] [PubMed] [Google Scholar]
- 26.Shew M, Muelleman T, Harris M, Li M, Sykes K, Staecker H, et al. Petrous apex pneumatization: Influence on postoperative cerebellopontine angle tumor cerebrospinal fluid fistula. Ann Otol Rhinol Laryngol. 2018;127:604–7. doi: 10.1177/0003489418781934. [DOI] [PubMed] [Google Scholar]
- 27.Stieglitz LH, Wrede KH, Gharabaghi A, Gerganov VM, Samii A, Samii M, et al. Factors affecting postoperative cerebrospinal fluid leaks after retrosigmoidal craniotomy for vestibular schwannomas. J Neurosurg. 2009;111:874–83. doi: 10.3171/2009.2.JNS081380. [DOI] [PubMed] [Google Scholar]
- 28.Sugerman HJ, DeMaria EJ, Felton WL, 3rd, Nakatsuka M, Sismanis A. Increased intra-abdominal pressure and cardiac filling pressures in obesity-associated pseudotumor cerebri. Neurology. 1997;49:507–11. doi: 10.1212/wnl.49.2.507. [DOI] [PubMed] [Google Scholar]
- 29.Teo MK, Eljamel MS. Role of craniotomy repair in reducing postoperative headaches after a retrosigmoid approach. Neurosurgery. 2010;67:1286–91. doi: 10.1227/NEU.0b013e3181f0bbf1. [DOI] [PubMed] [Google Scholar]
- 30.Venable GT, Roberts ML, Lee RP, Michael LM 2nd. Primary dural closure for retrosigmoid approaches. J Neurol Surg B Skull Base. 2018;79:330–4. doi: 10.1055/s-0037-1607455. [DOI] [PMC free article] [PubMed] [Google Scholar]