Dear Editor,
The coronavirus disease 2019 (COVID-19) pandemic originated from China's Wuhan and has currently become a global threat [1], affecting more than 200 countries with over 100 million infected cases and over 2 million deaths [2]. Presentations of COVID-19 have ranged from asymptomatic/mild symptoms to severe illness and mortality.
In response to the COVID-19 outbreak, the Taiwanese government set up the central emergency command center in January 2020 to formulate policies involving tourist restriction, community surveillance, social distancing, promoting mask usage, handwashing, and respiratory hygiene. Expansion of testing and hospital capacity, increasing material inventories, requisitioning facilities, patient diversion, and transfers were undertaken to prevent unnecessary emergency department (ED) overcrowding.
Taiwan recorded its first case on January 20 which surged to over 400 by April 19, 2020. Until early May of 2020, the spread had slowed down. Taiwan has reported <1,000 confirmed cases until February this year and was recognized with one of the most successful epidemic prevention protocol and implementation.
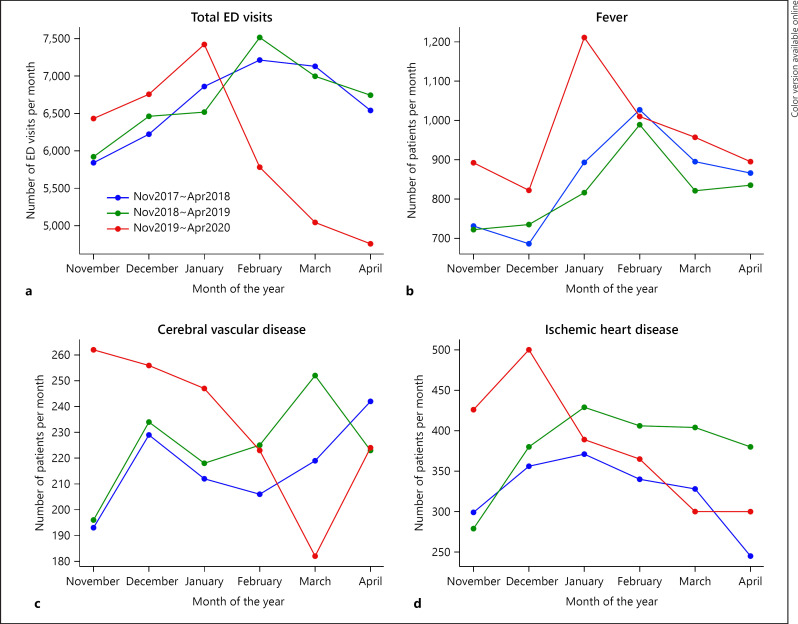
Since the ED was flooded with COVID-19 patients, the noninfected regular patients sought treatment at alternative outpatient centers. Some experts were concerned and contemplated on the long-lasting public health consequences if people were scared to visit hospitals. We aimed to analyze the changes in ED visits at the Kaohsiung Chang Gung Memorial Hospital, the largest tertiary medical center in southern Taiwan with an average of 72,000 ED visits per year. All adult nontrauma patients visiting the EDs from November to April in the last 3 years were included in the analysis. The number of total ED visits was down by 25–30% from February to April 2020 (Fig. 1a). Though a slight increase was observed in the ED visits for fever from March to April 2020 (Fig. 1b), a decrease of about 15% in patients visiting EDs for cerebrovascular diseases was seen in March 2020 (Fig. 1c). The ED visits for ischemic heart disease were similar for the last 3 years but also reduced in March 2020 (Fig. 1d). The proportion of patients needing intensive care unit admission or intubation in ED was comparable for the last 3 years.
Fig. 1.
Number of visits recorded at the ED of the Kaohsiung Chang Gung Memorial Hospital each week from November to April for the past 3 years. Total ED visits (a); ED visits for fever (b); ED visits for cerebrovascular disease (c); ED visits for ischemic heart disease (d). ED, emergency department.
Many noncritical patients or patients with mild illnesses avoid unnecessary ED visits during the COVID-19 crisis, and therefore, a decrease in ED visits for cerebrovascular disease and ischemic heart diseases was observed. Similar phenomenon was also observed in the Western countries [3]; however, ED visits should not be delayed in patients experiencing a serious health crisis such as a potential stroke or heart attack [4].
Conflict of Interest Statement
The authors declare that they have no competing interests.
Funding Sources
This research was not supported by any grant or external funding.
Author Contributions
All contributors have had input and agree on the final manuscript.
Acknowledgement
We appreciate the support provided for statistics at the Biostatistics Center of the Kaohsiung Chang Gung Memorial Hospital.
References
- 1.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395((10229)):1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization WHO coronavirus disease (COVID-19) dashboard. Available from: https://covid19.who.int/
- 3.Schwarz V, Mahfoud F, Lauder L, Reith W, Behnke S, Smola S, et al. Decline of emergency admissions for cardiovascular and cerebrovascular events after the outbreak of COVID-19. Clin Res Cardiol. 2020;109((12)):1500–6. doi: 10.1007/s00392-020-01688-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herlitz J, Wireklintsundström B, Bång A, Berglund A, Svensson L, Blomstrand C. Early identification and delay to treatment in myocardial infarction and stroke: differences and similarities. Scand J Trauma Resusc Emerg Med. 2010;18:48. doi: 10.1186/1757-7241-18-48. [DOI] [PMC free article] [PubMed] [Google Scholar]