Abstract
Coronavirus disease (COVID-19) is highly contagious and is now a tragic pandemic. Maintenance hemodialysis (MHD) patients are susceptible to COVID-19 and more prone to develop into severe cases because of the older age, heavy comorbidities, and impaired immunity. Patients who receive in-center dialysis have to travel to and from dialysis centers; patients have to share the dialysis hall with others during dialysis, making the prevention and control of COVID-19 in dialysis centers different from that in community and more difficult. This article provides key points in coping with COVID-19 in dialysis centers during this pandemic based on experience: (1) enforcing infection control management of dialysis centers, (2) training of hemodialysis patients and medical staffs, (3) screening for COVID-19 among patients and medical staffs, and (4) providing graded isolated dialysis to close contacts, suspected cases, and confirmed cases of COVID-19. We hope our single-center experience can be referenced by other dialysis centers around the world in coping with the COVID-19 pandemic.
Keywords: Coronavirus disease 2019, Hemodialysis, End-stage kidney disease, Pandemic, Preventive measures
Background
The new coronavirus (severe acute respiratory syndrome coronavirus (SARS-CoV-2)) is more contagious than the other 2 coronaviruses, SARS-CoV, which caused 8096 cases [1], and the Middle East respiratory syndrome coronavirus, which caused 2,229 laboratory-confirmed cases between 2012 and 2018 [2]. The World Health Organization (WHO) declared the coronavirus disease (COVID-19) a pandemic on March 11, 2020. The WHO director-general said at the media briefing on March 23, 2020, [3]: “The pandemic is accelerating. It took 67 days from the first reported case to reach the first 100,000 cases, 11 days for the second 100,000 cases, and just 4 days for the third 100,000 cases.” Globally, by January 22, 2021, there have been 96,267,473 confirmed cases, including 2,082,745 deaths worldwide [4].
Maintenance hemodialysis (MHD) patients are susceptible to microbial attack because of their older age, impaired immune system, high frequency of complications, and comorbidities [5, 6]. They are more prone to develop into severe cases [7]. The first 2 deaths in the USA were MHD patients [8]. MHD patients have to stay in a densely populated hall during their repeated 4-hour dialysis sessions, so they are likely to be exposed to droplet-borne disease [9]. Medical staff in the facility also suffer a high risk of infection.
In the first publication [9] on COVID-19 in dialysis centers, after the first COVID-19 was diagnosed, intensive measures including COVID-19 case isolation, personal protective equipment (PPE) upgradation, and screening of COVID-19 among other MHD patients were undertaken from January 14 to February 17, 2020, during which 37 out of 230 MHD patients and 4 medical staff were diagnosed to have COVID-19. No new case was diagnosed thereafter. It means although COVID-19 could spread quickly in dialysis centers, it could be effectively prevented and controlled by adequate measures.
In mid-January 2020, immediately after the first case of COVID-19 outside Wuhan was reported, our hemodialysis (HD) center at the Peking University People's Hospital began to implement strict measures. On February 18, 2020, one COVID-19 case was found in our MHD patient who got the virus from the patient's daughter or son-in-law. The patient was transferred to a designated hospital on the same day. Although some of the other patients and medical staff had been in close contact, none of them got COVID-19 after 14 days of observation, thanks to strict measures. This further implicates that the strict management process inside dialysis centers can effectively minimize the risk of cross-infection.
Several Chinese associations published their recommendations for management of dialysis centers during this COVID-19 pandemic [10, 11]. The EUDIAL working group of ERA-EDTA and the American Society of Nephrology also published their recommendations [6, 12].
This article refers to the above suggestions and draws on our experience to explain the key points in preventing COVID-19 and mitigating risks of COVID-19 in dialysis centers during this pandemic. We focus on preventive measures for non-COVID-19 designated dialysis centers. This is a single-center experience, but we hope our experience will be useful to other dialysis centers worldwide.
Managing Dialysis Center
Preplanning for Possible Urgent Situation
COVID-19-infected MHD patients should receive HD treatment at designated hospitals or dialysis centers. In Wuhan, China, 8 dialysis centers in the urban area and 5 in the suburbs were designated as facilities for COVID-19-infected MHD patients to ensure their treatment. Areas with a high number of COVID-19 cases should preplan as a whole to designate dialysis centers for MHD patients with COVID-19.
Urgent plans should be prepared when a COVID-19 case is confirmed, including rescheduling treatments for all patients and isolation of all close contacts as well as medical staff.
Providing Training to Healthcare Team
Online training via online meeting, online continued medical education programs, and WeChat group notices should be provided to all medical staff. The content should include the following:
1. Knowledge of COVID-19;
2. Classification of cleanliness of different areas (polluted area, semi-polluted area, and nonpolluted area);
3. Proper usage of different types of face masks;
4. Procedures for effective hand hygiene;
5. Healthy habits: keeping distance from others when talking or eating, washing working coats frequently, less gathering, no eating and drinking in polluted or semi-polluted areas;
6. Proper selections of PPE for different conditions in daily works.
Providing Training to MHD Patients and Their Companions
1. During the epidemic, self-isolation at home is essential for MHD patients [11]. They should be instructed to stay at home while off dialysis. They should avoid taking public transportation to get the dialysis or using elevators as much as possible. They also should avoid unnecessary close contact with others.
2. Companions to a MHD patient should be fixed and be without epidemiological history. The companion should not be allowed to enter the dialysis treatment center when the shift is ongoing.
3. Measures should be taken to improve patients' compliance. Patients should be notified of shift changes. During the epidemic, several conditions will possibly prolong the dialysis interval: waiting for COVID-19 laboratory test results and shift changes because of a new case of COVID-19. Patients should be instructed to strictly control their diet, water, salt, potassium, and phosphorus intake in case of sudden prolongation of the inter-dialysis period.
4. Patients and companions should wear medical surgical face masks or N95 masks without ventilation valve all the time during dialysis treatment, and maintain a safe distance of no less than 2 m away from others. Patients and companions should be trained about how to properly wear face masks.
5. Patients should be provided with instructions about hand hygiene and proper cough etiquette.
Adjusting Dialysis Shifts to Contain Possible COVID-19 Cases
During the COVID-19 pandemic, close contacts of a suspected or confirmed COVID-19 case should be isolated. The dialysis shift schedules should be adjusted and main shift crossovers should be avoided to limit patients' possible exposure.
MHD patients usually have 6 shifts every 2 weeks with a fixed time schedule per week. They are divided into 4 groups. Monday, Wednesday, and Friday patients never see Tuesday, Thursday, and Saturday patients and will not be exposed to infection after effective terminal disinfection. However, morning and afternoon patients in the same day may expose to each other, so rules should be made to avoid their contact.
Some MHD patients with 4, 5, 7, or 8 shifts per 2 weeks should be adjusted to fit into the 4 main groups. Shifts that cannot be adjusted should be performed separately. If possible, medical staff can be adjusted according to actual needs.
Strict Screening for COVID-19 in MHD Patients and Medical Staff
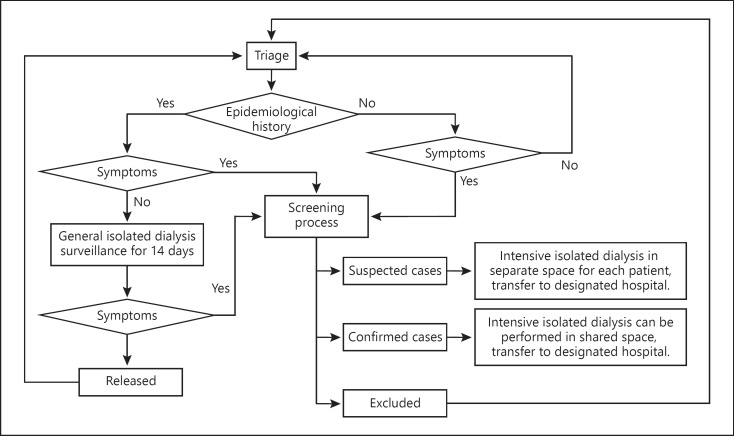
MHD patients and medical staff intermittently come to the dialysis center and meet other patients and other medical staff in the center. They also come into contact with other people or family members on transportations or at home. During the pandemic, nobody knows when they may get infected with COVID-19 which has a latent period of 1–14 days or even longer and is contagious during this period [13]. Asymptomatic COVID-19 cases are also contagious since a large number of viruses can be detected from their nasopharynx swab test. Dialysis centers should differentiate high-risk patients, COVID-19 suspected and confirmed patients as soon as possible by screening, and set different levels of isolation (Fig. 1). These are very important for dialysis centers to reduce the outbreak of infection.
Fig. 1.
Flowchart for identification and isolated dialysis of COVID-19 close contacts, and suspected and diagnosed cases based on triage results. COVID-19, coronavirus disease.
Reporting of Epidemiological History
All patients and medical staff should be well-informed about their responsibility of reporting any epidemiological history according to the Law of the People's Republic of China on the Prevention and Treatment of Infectious Diseases.
Monitoring Daily Health of Medical Staff and MHD Patients
An established daily physical health monitoring program should include the history of close contacts, body temperature, and suspicious symptoms in medical staff, patients, and patients' companions. Medical staff should report every day whether they have fevers or suspected symptoms. For patients and patients' companions, their health-related information should be acquired by telephone or other remote methods on inter-dialysis days. On the day of dialysis, triage should be performed before patients enter the dialysis hall.
Screening for COVID-19 before Entering
Trained medical staff should ask patients and their companions (1) if they have histories of travel to or residence in the epidemic area or other case-reporting communities within the last 14 days; (2) whether they have contacted subject(s) with fever or respiratory symptoms within the last 14 days; (3) whether they have been exposed to clustered fever cases; (4) whether they have been exposed to suspected or confirmed COVID-19 cases within the last 14 days; (5) whether they have suspicious symptoms, including fever, dry cough, and fatigue (which are the main manifestations of COVID-19 cases); nasal congestion, runny nose, sore throat, myalgia, and diarrhea (manifestations in some COVID-19 cases); and dyspnea and/or hypoxemia (manifestations in severe COVID-19 cases) [13].
As some patients may conceal epidemiological history or self-administer antipyretic drugs to cover their symptoms, medical staff should find other ways to get accurate information. In China, some validated smart phone applications will keep track of the user's location in the recent 14 days.
Patients' body temperatures should be taken every time before they enter the HD hall. If the temperature taken from the forehead exceeds 37.3°C using a remote infrared thermometer, axillary temperature should be taken using a mercury thermometer. The procedures for COVID-19 screening (chest CT scan and one of nasopharynx swab test for SARS-CoV-2 RNA or serum SARS-CoV-2 antibody) should be activated if the axillary temperature exceeds 37.3°C.
Patients Initiating First Dialysis
A patient initiating dialysis should be screened for COVID-19 before the first dialysis.
Adjusting Dialysis Shifts Based on Triage Results
Dialysis shifts should be adjusted according to clinical symptoms and epidemiological history.
Asymptomatic MHD Patients without Epidemiological History
They should receive regular dialysis treatment as usual and perform routine daily monitoring and triage before entering the dialysis hall.
Asymptomatic MHD Patients with Epidemiological History
Arrangements should be made for these patients to receive general isolated dialysis or separate continuous renal replacement therapy, and the patients should be observed for at least 14 days.
General isolated dialysis should be provided to each of these MHD patients in a separate space; it can also be performed in a shared space during shortage of medical resources. The shift should be the last one during the day or an additional shift after the daily regular shift to avoid contact with other MHD patients. The patients should be supervised to take body temperature test twice a day and report suspicious symptoms. Their body temperature should be monitored during dialysis treatment. Patients should wear medical surgical masks or N95 fitted masks without ventilation valve during the whole process. Medical staff should wear working coats, hair caps, eye shields or goggles, N95 masks, gloves, and isolation gowns. After each session of dialysis treatment, terminal disinfection should be performed (see Performing Terminal Disinfection after Each Dialysis Shifts).
During the 14-day observed isolation, if the patient is suspected or confirmed, the procedures for suspected or confirmed cases should be activated (see COVID-19 Suspected or Confirmed MHD Patients). If no suspicious symptoms are found and the screening results are negative after 14 days, the patient should be scheduled to return to his/her routine dialysis station and shift.
Symptomatic MHD Patients with or without Epidemiological History
They should be screened for COVID-19. Patients should receive intensive isolated dialysis or separate CRRT until COVID-19 is confirmed or ruled out. Medical staff should upgrade their PPE when taking care of these patients.
If COVID-19 is suspected or confirmed by screening, the procedures for suspected or confirmed cases should be followed (see COVID-19 Suspected or Confirmed MHD Patients). If the screening results do not match the diagnosis of COVID-19, the patient without epidemiological history should be scheduled to return to his/her routine dialysis station and shift. Those with epidemiological histories should be arranged to receive general isolated dialysis.
To avoid sharing space and passage with other patients, intensive isolated dialysis should be provided in a separate space and in an additional shift after the daily routine shifts. Medical staff should upgrade PPE in response. All other measures used in general isolated dialysis should apply to the intensive isolated dialysis.
COVID-19 Suspected or Confirmed MHD Patients
Dialysis centers should report suspected or confirmed cases to the corresponding institution according to local requirements within a time limit. The patient should be transferred to the designated hospital for dialysis service.
Before being transferred, the suspected or confirmed patient should be dialyzed in a shared area but should be away from other MHD patients. Each of the COVID-19 suspected patients should be dialyzed in a separate room.
Identified close contacts including other MHD patients, family members, and medical staff should be isolated for at least 14 days from the time of last exposure to the suspected or confirmed patients. Close contact patients should follow the process for patients with positive epidemiological history. The facility should perform terminal disinfection. The dialysis center should activate emergency plans to adjust manpower and arrange follow-up work.
Performing Terminal Disinfection after Each Dialysis Shift
During the COVID-19 pandemic, terminal disinfection should be performed after each shift. If it is not feasible, terminal disinfection should be performed after each general isolated dialysis, intensive isolated dialysis, and after a new case is suspected or confirmed [14, 15]. The terminal disinfection should be carried out in the following sequence: air disinfection, dirt collection, object surface disinfection, and medical supplies disinfection. Dialysis centers should change the bedsheets and covers after each shift.
Summaries
Although our dialysis center was exposed to 1 COVID-19 patient last year during the first round of the pandemic, no new case emerged because of upgraded infection control management of dialysis centers, comprehensive training of MHD patients and medical staff, strict screening for COVID-19 among MHD patients and medical staff, and grouped management of MHD patients. The aim of the MHD patient grouping was to limit the number of close contacts, thus avoiding an outbreak of COVID-19 in the dialysis center. In the past year, COVID-19 has not been effectively controlled worldwide; China has also experienced and is experiencing repeated epidemics. COVID-19 may still exist for years. Strict preventive and control measures have been proven to be effective. Our experience can be adapted to meet local needs by other dialysis centers around the world during this COVID-19 pandemic before vaccination-induced herd immunity is achieved.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors did not receive any funding.
Author Contributions
Liangying Gan drafted the manuscript; Li Zuo made revision; and Bing Yang, Yan Wang, and Ying Wang provided suggestions and manuscript discussion.
References
- 1.World Health Organization Summary of probable SARS cases with onset of illness from 1 November 2002 to 31. July 2003. Available from: https://www.who.int/csr/sars/country/en/
- 2.World Health Organization WHO MERS global summary and assessment of risk. Available from: https://www.who.int/csr/disease/coronavirus_infections/risk-assessment-august-2018.pdf?ua=1&ua=1&ua=1.
- 3.World Health Organization WHO Director-General's opening remarks at the media briefing on COVID-19 − 23. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—23-march-2020.
- 4.World Health Organization WHO Coronavirus Disease (COVID-19) Dashboard. Available from: https://covid19.who.int/
- 5.Zoccali C, Vanholder R, Massy ZA, Ortiz A, Sarafidis P, Dekker FW, et al. The systemic nature of CKD. Nat Rev Nephrol. 2017 Jun;13((6)):344–58. doi: 10.1038/nrneph.2017.52. [DOI] [PubMed] [Google Scholar]
- 6.Basile C, Combe C, Pizzarelli F, Covic A, Davenport A, Kanbay M, et al. Recommendations for the prevention, mitigation and containment of the emerging SARS-CoV-2 (COVID-19) pandemic in hemodialysis centres. Nephrol Dial Transplant. 2020 Mar 20;35:737–41. doi: 10.1093/ndt/gfaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang T, Du Z, Zhu F, Cao Z, An Y, Gao Y, et al. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet. 2020 Mar 21;395((10228)):e52. doi: 10.1016/S0140-6736(20)30558-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Medscape Medical News Dialysis should continue despite COVID-19. Available from: https://www.medscape.com/viewarticle/926720?nlid=134518_1502&src=WNL_mdplsfeat_200317_mscpedit_neph&uac=169159SV&spon=44&impID=2314992&faf=1#vp_1.
- 9.Ma Y, Diao B, Lv X, Zhu J, Liang W, Liu L, et al. 2019 novel coronavirus disease in hemodialysis (HD) patients: report from one HD center in Wuhan, China. medRxiv [Google Scholar]
- 10.Expert term of Chinese Society of Blood Purification Administration Recommendations for prevention and control of novel coronavirus infection in blood purification center (room) Chin J Blood Purif. 2020;19((2)):73–6. [Google Scholar]
- 11.COVID-19 Expert Team of Chinese Society of Nephrology Recommendations for prevention and control of novel coronavirus infection in blood purification center (room) from the Chinese Medical Association Nephrology Branch. Chinese J Nephrol. 2020;36((2)):82–4. [Google Scholar]
- 12.Kliger AS, Silberzweig J. Mitigating risk of COVID-19 in dialysis facilities. Clin J Am Soc Nephrol. 2020 Mar 20;15((5)):707–9. doi: 10.2215/CJN.03340320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Health Commission of the People's Republic of China Diagnosis and treatment of COVID-19 (trial version 7) Available from: http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989/files/ce3e6945832a438eaae415350a8ce964.pdf. [DOI] [PMC free article] [PubMed]
- 14.Beijing Hospital Infection Management Quality Control and Improvement Center Medical institutions daily and during epidemic (COVID-19) environmental cleaning and disinfection checklist. 2020 Feb 10 [Google Scholar]
- 15.Ministry of Health of the People's Republic of China Regulation of disinfection technique in healthcare setting. 2012 Apr 5 [Google Scholar]