Abstract
Introduction
The COVID-19 pandemic resulted in significant healthcare reorganizations, potentially striking standard medical care. We investigated the impact of the COVID-19 pandemic on acute stroke care quality and clinical outcomes to detect healthcare system's bottlenecks from a territorial point of view.
Methods
Crossed-data analysis between a prospective nation-based mandatory registry of acute stroke, Emergency Medical System (EMS) records, and daily incidence of COVID-19 in Catalonia (Spain). We included all stroke code activations during the pandemic (March 15–May 2, 2020) and an immediate prepandemic period (January 26–March 14, 2020). Primary outcomes were stroke code activations and reperfusion therapies in both periods. Secondary outcomes included clinical characteristics, workflow metrics, differences across types of stroke centers, correlation analysis between weekly EMS alerts, COVID-19 cases, and workflow metrics, and impact on mortality and clinical outcome at 90 days.
Results
Stroke code activations decreased by 22% and reperfusion therapies dropped by 29% during the pandemic period, with no differences in age, stroke severity, or large vessel occlusion. Calls to EMS were handled 42 min later, and time from onset to hospital arrival increased by 53 min, with significant correlations between weekly COVID-19 cases and more EMS calls (rho = 0.81), less stroke code activations (rho = −0.37), and longer prehospital delays (rho = 0.25). Telestroke centers were afflicted with higher reductions in stroke code activations, reperfusion treatments, referrals to endovascular centers, and increased delays to thrombolytics. The independent odds of death increased (OR 1.6 [1.05–2.4], p 0.03) and good functional outcome decreased (mRS ≤2 at 90 days: OR 0.6 [0.4–0.9], p 0.015) during the pandemic period.
Conclusion
During the COVID-19 pandemic, Catalonia's stroke system's weakest points were the delay to EMS alert and a decline of stroke code activations, reperfusion treatments, and interhospital transfers, mostly at local centers. Patients suffering an acute stroke during the pandemic period had higher odds of poor functional outcome and death. The complete stroke care system's analysis is crucial to allocate resources appropriately.
Keywords: Stroke, Emergency medical services, Organization, Coronavirus disease 2019
Introduction
In December 2019, the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of coronavirus disease 2019 (COVID-19), was first identified in Wuhan, China [1]. High transmissibility rates led to a quick worldwide spread, and the World Health Organization declared a pandemic outbreak on March 11, 2020. Spain was one of the countries more heavily stricken by SARS-CoV-2 at the beginning of the pandemic and adopted unprecedented measures such as large-scale social isolation, closing borders, and nationwide lockdown.
The COVID-19 pandemic resulted in a significant reorganization of emergency care facilities to accommodate the additional workload [2, 3]. Worldwide, the restructuring of health staff and hospital resources towards the COVID-19 emergency is inevitably leading to severe impairment of standard medical care [4], particularly for time-dependent diseases [5, 6]. Several groups in Europe [7, 8, 9, 10, 11, 12], Asia [13], Latin America [14], and the USA [15, 16] reported marked and unexplained decreases in stroke's volume of patients and reperfusion therapies. The American Heart Association/American Stroke Association (AHA/ASA) provided temporary emergency guidance for stroke centers during the current crisis [17].
Acute stroke care continues to be crucial at emergency facilities, even amid a pandemic or crisis, and highly organized healthcare systems are vital to provide life-saving procedures in the briefest time from stroke onset [18, 19]. We aimed to detect stroke care system bottlenecks during COVID-19 pandemic. For this, we performed a detailed analysis of crossed data between nation-based registries of COVID-19 pandemic and stroke care in Catalonia, a region especially afflicted with around 25% of the total number of cases and deaths in Spain.
Materials and Methods
Individual deidentified patient data not provided in the article are available in a trusted data repository at other investigators' requests to replicate procedures and results.
Data Collection
In Catalonia (total population of 7.5 million inhabitants), acute stroke care is provided through a network of 28 acute hospitals, including 6 comprehensive stroke centers (CSCs), 8 primary stroke centers (PSCs), and 14 telestroke centers (TSCs) [20, 21]. TSCs are IVT-ready centers through telemedicine connection to an on-call neurologist, PSCs are IVT-ready centers with neurologists on-site and equipped Stroke Unit, and CSCs are MT-capable centers. No significant changes in stroke pathways or IVT and MT eligibility criteria were made during the COVID-19 outbreak. The Stroke Code protocol was implemented in Catalonia in 2006, and activation criteria are nondisabled or with minor disability patients with suspicion of acute stroke of <8 h from onset or unknown time of onset. The Emergency Medical System (EMS), with single centralized coordination, is the Stroke Code's primary activator. All stroke code activations in Catalonia are prospectively recorded and stored in CICAT (Codi Ictus Catalunya), a government-mandated, population-based registry. Mortality and clinical outcome (Rankin scale) at 90 days during both study periods were centrally assessed by a blinded evaluator of the Catalan Stroke Program. Per protocol, only patients receiving reperfusion therapies (IVT and/or MT) and stroke code patients scoring RACE ≥4 at EMS assistance are evaluated at 90 days. The Catalan Health Department provided daily new confirmed COVID-19 cases per geographical region. The EMS provided prospectively collected data on the number of total daily calls per geographical region and stroke care prehospital workflow times during the study period.
Study Design
We compared prospective data collected from 2 periods of 7 weeks: the pandemic period, corresponding to the period after lockdown implementation on March 15, 2020, through May 2, 2020, when the national de-escalation plan started (7 weeks), and the comparable prior time, called the prepandemic control period (January 26, 2020, to March 14, 2020). Baseline characteristics, stroke care workflow times, clinical and radiological features, and reperfusion treatments were compared. Prehospital workflow times included the stroke onset to EMS alert, defined by the moment when the need of the resource was recorded; the EMS alert to EMS assistance, defined by the moment when the EMS arrived at the scene; and the time from stroke onset to hospital arrival. The number of EMS alerts and new COVID-19 confirmed cases was extracted for crossed-data correlation analysis. Data were totaled per week and geographical health areas. Poor clinical outcome at 90 days was defined as mRS ≥ 2.
Outcomes
The primary objectives were to compare differences in the number of stroke codes and reperfusion therapies administered between study periods. Secondary outcomes included differences in clinical characteristics, stroke care workflow metrics, correlation analysis to evaluate the impact of EMS collapse on stroke code activation and prehospital stroke metrics and the impact of COVID-19 infection rate on stroke code activation and in-hospital stroke care workflow. We assessed whether the differences observed globally were different across the types of stroke centers (CSCs, PSCs, and TSCs). We also evaluated the impact of differences between study periods on mortality and clinical outcome at 90 days.
Statistical Analysis
Demographic, baseline, and clinical characteristics and stroke care metrics were described and compared between the pandemic and prepandemic cohorts. Continuous variables were shown as mean (SD) or median (interquartile intervals) and compared with the Student t test, Mann-Whitney, or Kruskal-Wallis tests as appropriate. Categorical variables were presented as counts and percentages and were compared with the χ2 or Fisher exact tests. Significance was considered when 2-sided p values were <0.05. The weekly number of stroke activations, reperfusion treatments, and median workflow time metrics during the study period was calculated for each Catalonia healthcare region. The influence of weekly regional incidence of COVID-19 cases and EMS alerts per 100,000 habitants in main outcomes was tested with Spearman's rho correlation. Statistical analyses were done with IBM SPSS version 23.3 (Chicago, IL, USA) and Python 3.7.6 with the Pandas, Matplotlib, and Seaborn libraries.
Results
A total of 805 (17 per day) stroke code activations were reported in Catalonia during the pandemic period, compared to 1,033 (21 per day) during the prepandemic control period, representing a decline of 22% of stroke code activations (shown in Fig. 1 and online suppl. Table 1; for all online suppl. material, see www.karger.com/doi/10.1159/000516309). This decline was mainly derived from a reduction in ischemic strokes (24% reduction) and stroke mimics (47% reduction). The number of reperfusion therapies also declined, 304 (6 per day) administered during the prepandemic period compared to 215 (4 per day) during the pandemic (29% reduction). No differences in age, stroke severity, or proportion of large vessel occlusion (LVO) were seen, while unwitnessed strokes increased by 9%. The source of stroke code activation changed during the pandemic period, with an increase of stroke codes delivered by EMS without prenotification and a lower proportion of stroke code activations at emergency departments of patients arriving by their own means.
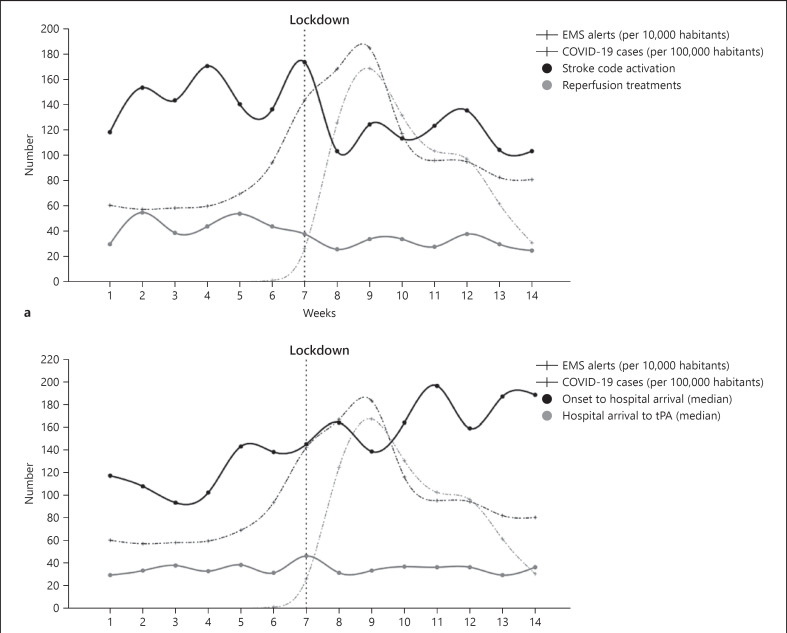
Fig. 1.
Temporal trends in EMS calls, COVID-19 cases, and stroke-related activity. a Course of COVID-19 cases, EMS alerts, and the number of stroke code activations and reperfusion treatments. Note the sharp increase of EMS alerts and COVID-19 cases around the lockdown implementation date and the subsequent decrease in the number of stroke code activations and reperfusion treatments. b Course of COVID-19 cases, EMS alerts, and stroke care delays. The time from stroke onset to hospital door increased during the pandemic, whereas the time to rtPA initiation did not. EMS, Emergency Medical System; rtPA, recombinant tissue plasminogen activator.
Prehospital workflow metrics were critically affected during the pandemic period (shown in Fig. 1; Table 1). Time from symptom onset to hospital arrival was increased by 53 min (120 min for patients arriving by private transport and 35 min for patients transferred by the EMS). There was a massive increase in the number of total calls to the EMS, and the time from stroke onset to the EMS alert increased by 42 min. This time encompasses the patient or witness's alert and the handling of the call by the EMS. Once the EMS was alerted, the prehospital delays remained stable. Temporal trends in EMS calls, COVID cases, and stroke-related activity showed higher affliction in stroke code activation and delays of prehospital stroke time metrics during the first 4 weeks while the number of COVID-19 was growing weekly (shown in Fig. 1).
Table 1.
Prehospital stroke workflow times in minutes
| Control period | Pandemic | Difference | p value | |
|---|---|---|---|---|
| All stroke code patients | ||||
| Onset to hospital arrival, min | 118 [63–284] | 171 [78–540] | +53 | <0.001 |
| Patients arriving at the ED by private transport | ||||
| Onset to hospital arrival, min | 118 [62–285] | 238 [119–583] | + 120 | <0.001 |
| Patients transferred by EMS | ||||
| Onset to EMS alert, min | 47 [15–170] | 89 [20–329] | +42 | 0.003 |
| Onset to EMS assistance, min | 56 [23–177] | 101 [29–338] | +45 | 0.004 |
| EMS alert to EMS assistance, min | 8 [5–12] | 8 [5–11] | 0 | 0.791 |
| Onset to hospital arrival, min | 115 [61–248] | 150 [76–504] | +35 | <0.001 |
Data are presented as median [interquartile range]. ED, emergency department; EMS, emergency medical system.
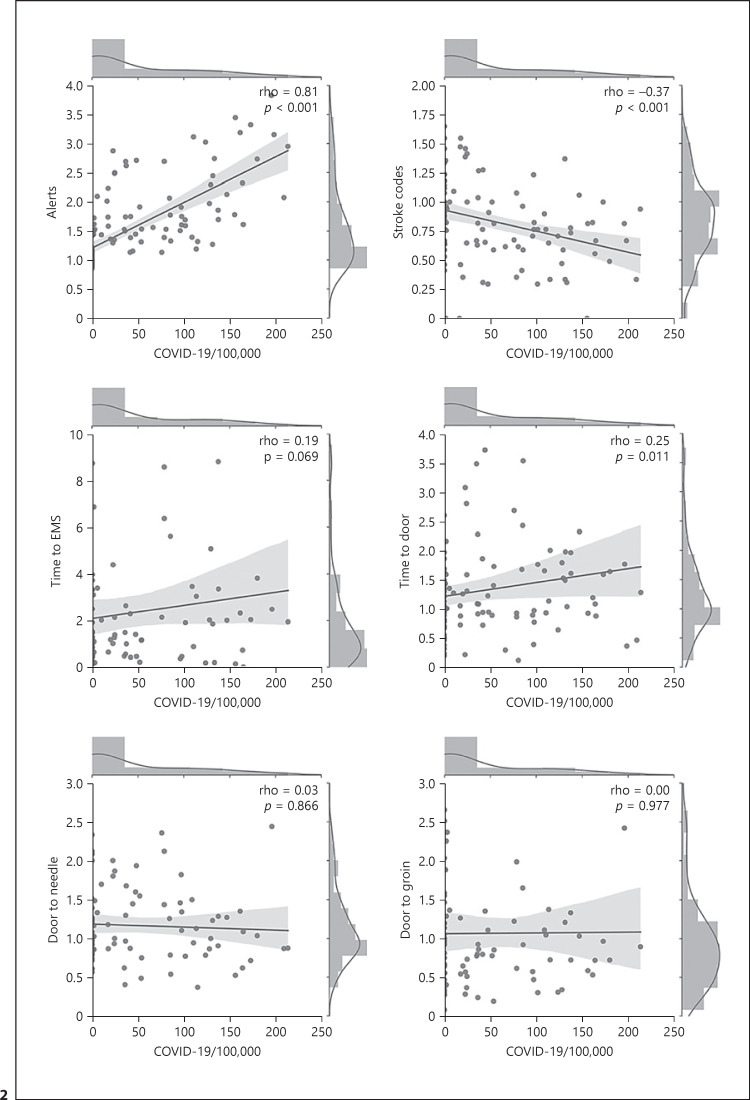
When comparing regions and weeks with varying degrees of saturation due to COVID-19, there were significant correlations of increasing weekly numbers of COVID-19 cases and more EMS calls (rho = 0.81, p < 0.001), less stroke code activations (rho = −0.37, p < 0.001), and longer prehospital delays (rho = 0.25, p = 0.011). In contrast, the number of COVID-19 cases in each region was unrelated to in-hospital delays to systemic thrombolysis or endovascular thrombectomy (Fig. 2).
Fig. 2.
Relationship between the frequency of COVID-19 cases and several aspects of stroke care compared to the prepandemic period. Joint plots showing the univariate distributions and the relationships, with Spearman's rho correlations, between weekly cases of COVID-19 and several aspects of stroke care at the main sanitary regions in Catalonia. The figures show points representing weekly ratios in each region relative to median values during the prepandemic period, with the linear regression fit line and bootstrap confidence intervals for the regression estimate. Note the strong correlation of COVID-19 cases with EMS alerts, the moderate negative correlation with the stroke code activations, and the slight correlation with times from onset to hospital door. In contrast, the number of COVID-19 cases and intrahospital delays to reperfusion treatments was uncorrelated. EMS, emergency medical services.
Stroke code activations and reperfusion therapies dropped across all types of centers (Table 2). TSCs were afflicted with higher falls in stroke code activations, thrombolytic treatments, and referrals to MT-capable CSCs. In-hospital workflow assessed by the door to needle and door to groin times remained mostly stable at all CSCs and PSCs but were especially affected in TSCs with a 17-min delay in the door to needle time.
Table 2.
Reperfusion therapies and in-hospital workflow times
| Control period | Pandemic | Difference | p value | |
|---|---|---|---|---|
| All centers | N = 1,033 | N = 805 | −22% | |
| Reperfusion treatment, n | 304 | 215 | −29% | 0.580 |
| IVT | 167 | 113 | −32% | |
| IVT + MT | 43 | 33 | −23% | |
| MT alone | 94 | 69 | −27% | |
| Door to needle (IVT), min | 35 [25–51] | 34 [26–50] | −1 min | 0.847 |
| Onset to needle (IVT), min | 118 [85–180] | 138 [91–210] | +20 min | 0.024 |
| Door to groin (MT), min | 80 [54–150] | 93 [60–130] | +13 min | 0.461 |
| Onset to groin (MT), min | 213 [130–409] | 267 [162–663] | +54 min | 0.007 |
| TSCs | N = 110 | N = 70 | −36% | |
| IVT, n | 22 | 10 | −55% | 0.328 |
| Door to needle (IVT), min | 42 [32–58] | 59 [39–74] | +17 min | 0.109 |
| Referred to MT center, n | 38 | 18 | −53% | 0.212 |
| PSCs | N = 303 | N = 213 | −29% | |
| IVT, n | 72 | 42 | −42% | 0.276 |
| Door to needle (IVT), min | 34 [24–54] | 33 [25–49] | −1 min | 0.714 |
| Referred to MT center, n | 40 | 29 | −28% | 0.892 |
| CSCs | N = 620 | N = 522 | −16% | |
| Reperfusion treatment, n | 193 | 150 | −22% | 0.755 |
| IVT | 81 | 63 | −23% | |
| IVT + MT | 35 | 31 | −6% | |
| MT alone | 77 | 56 | −27% | |
| Door to needle (IVT), min | 34 [24–50] | 33 [26–49] | −1 min | 0.876 |
| Door to groin (MT), min | 70 [48–96] | 82 [56–115] | +12 min | 0.056 |
Data are presented as n for categorical variables and as median [interquartile range] for continuous variables. TSCs are IVT-ready centers through telemedicine connection to an on-call neurologist, PSCs are IVT-ready centers with the neurologist on-site and Stroke Unit equipped. CSCs are MT-capable centers. IVT, intravenous thrombolysis; MT, mechanical thrombectomy; min, minutes; CSCs, comprehensive stroke centers; PSCs, primary stroke centers; TSCs, telestroke centers.
Mortality and clinical outcome at 90 days was assessed in 334 patients of the control period (32.3%) and 362 patients of the pandemic period (45%). Clinical characteristics of 90-day assessed patients are shown in online suppl. material (Table 2). After adjustment by clinical covariates associated with clinical outcome such as age, baseline NIHSS and mRS, time from onset to arrival, and LVO, suffering a stroke during the pandemic period remained as an independent predictor of mortality (OR 1.6 [1.05–2.4], p 0.03) and worse functional outcome (mRS ≤2 at 90 days: OR 0.6 [0.4–0.9], p 0.015).
Discussion
This crossed-data nation-based cohort analysis allowed us to identify causative dysfunctions in acute stroke management during the COVID-19 pandemic at Catalonia. The collapse of the prehospital EMS and a decline in stroke-related activity, especially in TSCs, appear as the main bottlenecks for decreased stroke code activations, reperfusion treatments, and interhospital transfers in Catalonia. Deficiencies during the pandemic period led to higher mortality rates and worse functional outcomes.
Previous studies reporting substantial falls in the number of acute stroke patients [8, 9, 10, 12, 15], number of emergency reperfusion therapies [7, 22], and delay in stroke care times [13, 23] during the COVID-19 pandemic provided few insights on why this phenomenon was happening and which points of the stroke care continuum should be reinforced to assure healthcare quality and equality to all stroke patients during the pandemic crisis. Most reports were focused on the results of the patients treated in one hospital or small groups of hospitals, most of them being CSCs [11]. Stroke incidence and reperfusion treatment rates at a population level are more meaningful and genuine quality indicators of the healthcare system's performance.
We report a 22% reduction in stroke code activations. Previous reports attributed this fall to a significant decrease in TIAs and minor strokes [14], while we observed no changes in TIA incidence or stroke severity, and the proportion of LVO strokes during the 2 periods was similar. Unwitnessed strokes increased by 9%, probably secondary to home isolation due to lockdown policies. Patients reduced mobility by private transport and arrived 2 h later to hospitals than usual. We observed an increase of stroke codes delivered by EMS with no prenotification and a significant delay (+42 min) in the time from symptom onset to EMS alert, which reverberated in all ulterior stroke metrics. Patients not coming to the hospital or seeking late aid might not have been the main limiting factors as previous reports highlighted [6, 16], since we did not detect changes in stroke characteristics, and the collapse of the EMS call center was directly related to enlarged prehospital delays (Fig. 2). We observed positive correlations between the number of COVID-19 cases and the number of total EMS alerts and delays to first EMS assistance and arrival at the hospitals. These observations suggest that, rather than not seeking medical help, often patients or people who witnessed the stroke could not effectively contact the EMS call center during the first weeks of the pandemic. It is worth highlighting that once the EMS received the alert, the time of EMS assistance remained stable, suggesting that the most conflictive point was the difficulty to contact the EMS system more than the availability of mobile units. Although stroke education and divulgation should always be present, especially during times when going to a hospital might be perceived as a threat, we encourage to focus resources on emphasizing EMS facilities to assure first stroke assistance to be as fast and efficient as always.
Getting the patient to the right hospital becomes even more critical in the days of the COVID-19 crisis. Although there are still insufficient data on the preferable transport circuit for stroke patients [21], we probably should consider adjusting transport pathways depending on hospital saturation. Amid a pandemic where mobility is restricted, telemedicine might be a powerful tool to ensure healthcare in remote areas. The AHA/ASA temporary emergency guidance [17] for stroke centers during the COVID-19 crisis encouraged to step down admissions in non-ICU units for stable stroke patients and to use stroke telemedicine. Catalonia has an extensive and well-established telestroke system across the territory [20]. Unfortunately, TSCs appeared to be the most vulnerable part of the stroke care system, reducing one-third of stroke code activations and >50% of thrombolytic treatments and referrals to CSCs, resulting in a decline of endovascular treatment opportunities. Emergent stroke care in TSCs is provided by emergency physicians guided through telemedicine by an on-call neurologist, whilst PSCs and CSCs had on-site neurologists. Although on-call telestroke neurologists were fully available during COVID-19 outbreak, emergency physicians had all resources and attention focused on the pandemic which failed in detecting stroke codes and resulted in less reperfusion therapies and interhospital referrals. We also detected a decline of reperfusion therapies in PSCs, but CSC referrals were less affected in this case. At CSCs, a proportioned decline in reperfusion treatments according to the reduction of stroke codes was observed. We also observed longer in-hospital delay until IVT initiation in TSCs, but not in PSCs and CSCs. During a pandemic crisis, stroke circuits should balance best stroke care and restricted mobility to avoid disease spread. Considering our observations, TSCs or PSCs severely restructured with stroke care affliction should be reinforced to ensure stroke treatment opportunities throughout the territory, or if not possible, we should consider bypassing TSCs to the closest higher-level stroke center (PSCs or CSCs) to provide equal stroke care even amid a pandemic.
Working fast but safely should be a significant cornerstone of the stroke care system [24]. All stroke care workers should wear preventive personal protective equipment, and COVID-19 testing should be performed to all stroke patients [17, 25]. The concern of contact with possible COVID-19-positive patients may result in delayed in-hospital workflows as already reported [13, 23]. We observed an additional delay of 20 min from symptom onset to intravenous thrombolysis administration and 54 min from symptom onset to groin puncture in patients undergoing endovascular treatment. This delay was mainly driven by a significant increase in prehospital workflow times since no significant delays of in-hospital metrics were observed.
Higher mortality rates and worse functional outcome are reported during the pandemic period. Larger workflow times and lower reperfusion therapies rates might be clue but not essential as suffering a stroke in the pandemic period remained as an independent predictor of poor outcome when adjusted by covariates. Pandemic deficiencies and changes afflict stroke care entirely. Constant and dynamic analysis of the holistic system care becomes imperative in health crisis to assure stroke care quality.
Regarding the study's limitations, the massive workload during the pandemic might have hampered the case notification and correct information collection in the registry. Nonetheless, the CICAT registry is a prospective government-mandatory registry that has been closely monitored during the pandemic to minimize this potential bias. The analysis is based on data from a regional stroke healthcare system. Organization and resource distribution might differ from other stroke healthcare systems, so our results should be carefully extrapolated to other regions. Details on the reasons for the initial delay at first telephone contact are missing and would have been optimal. Mortality and clinical outcome are not assessed in all patients, which would have been of great interest. However, the assessment was equally defined per protocol in both study periods. In turn, our study's main strengths are prospective data of the population-based registry that reflect all healthcare levels in a whole territory and the analysis of crossed data of stroke, EMS collapse, and COVID-19 infection rate.
Conclusions
The COVID-19 outbreak pushed stroke care systems to the limit. Territorial analysis of the complete stroke care system is crucial for researchers and healthcare policymakers to allocate resources appropriately and recognize weak infrastructural points in local healthcare systems. Such analysis showed that Catalonia's most vulnerable points were the collapse of the prehospital EMS and a decline in stroke code activations, reperfusion treatments, and interhospital transfers, which was higher at TSCs. The pandemic deficiencies resulted in higher mortality and worse clinical outcomes.
Statement of Ethics
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The study was approved by the Ethical Review Board of Hospital Germans Trias i Pujol and extended to the rest of the participating centers (PI-20-115). The need for written informed consent was waived by the Ethics Committee of Hospital Germans Trias i Pujol.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors thank the support of the Spanish Ministry of Economy and Competitiveness for grants RETICS-INVICTUS-PLUS to Dr. Pérez de la Ossa (RD0016/0019/0020), Dr. Purroy (RD16-0019-0017), Dr. Martí-Fàbregas (RD16-0019-0010), and Dr. Roquer (RD0016/0019/0002) funded by Instituto de Salud Carlos III and cofunded by the European Regional Development Fund (ERDF). Dr. Ramos-Pachón received funding from Instituto de Salud Carlos III with a Grant for Health Research (CM18/00021). Dr. Urra was sponsored by the Instituto de Salud Carlos III, Reference No. INT19/00020, and by the European Social Fund (The ESF − Investing in your future). Dr. Purroy was funded by the Government of Catalonia-Agència de Gestió d'Ajuts Universitaris i de Recerca (2017 SGR 1628). Dr. Gómez-Choco was funded by the Department of Health of the Generalitat de Catalunya (grant SLT008/18/00032).
Author Contributions
Anna Ramos-Pachon, Álvaro García-Tornel, Natàlia Pérez de la Ossa, and Xabier Urra contributed to the study design, data analysis and interpretation, writing and revision of the report. The rest of the coauthors contributed to data collection, edition, and revision of the manuscript. Corresponding authors had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Acknowledgement
All the authors acknowledge the excellent and tireless work done by the Emergency Medical System and the whole National Health System in Catalonia during this unprecedented pandemic.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382((8)):727–33. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aguiar de Sousa D, van der Worp HB, Caso V, Cordonnier C, Strbian D, Ntaios G, et al. Maintaining stroke care in Europe during the COVID-19 pandemic: results from an international survey of stroke professionals and practice recommendations from the European Stroke Organisation. Eur Stroke J. 2020 Sep;5((3)):230–6. doi: 10.1177/2396987320933746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bersano A, Kraemer M, Touzé E, Weber R, Alamowitch S, Sibon I, et al. Stroke care during the COVID-19 pandemic: experience from three large European countries. Eur J Neurol. 2020 Sep;27((9)):1794–800. doi: 10.1111/ene.14375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Markus HS, Brainin M. COVID-19 and stroke: a global World Stroke Organization perspective. Int J Stroke. 2020;15((4)):361–4. doi: 10.1177/1747493020923472. [DOI] [PubMed] [Google Scholar]
- 5.Jahan R, Saver JL, Schwamm LH, Fonarow GC, Liang L, Matsouaka RA, et al. Association between time to treatment with endovascular reperfusion therapy and outcomes in patients with acute ischemic stroke treated in clinical practice. JAMA. 2019;322((3)):252–63. doi: 10.1001/jama.2019.8286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51((7)):1996–2001. doi: 10.1161/STROKEAHA.120.030225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pop R, Quenardelle V, Hasiu A, Mihoc D, Sellal F, Dugay MH, et al. Impact of the Covid-19 outbreak on acute stroke pathways − insights from the Alsace region in France. Eur J Neurol. 2020 Sep;27((9)):1783–7. doi: 10.1111/ene.14316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Montaner J, Barragán-Prieto A, Pérez-Sánchez S, Escudero-Martínez I, Moniche F, Sánchez-Miura JA, et al. Break in the stroke chain of survival due to COVID-19. Stroke. 2020;51((8)):2307–14. doi: 10.1161/STROKEAHA.120.030106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rudilosso S, Laredo C, Vera V, Vargas M. Renú A, Llull L, et al. Acute stroke care is at risk in the era of COVID-19: experience at a comprehensive stroke center in Barcelona. Stroke. 2020;51((7)):1991–5. doi: 10.1161/STROKEAHA.120.030329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meza HT, Gil Á L, Saldaña AS, Martínez-Zabaleta M, Juez PR, Martínez EL, et al. Impact of COVID-19 outbreak on ischemic stroke admissions and in-hospital mortality in North-West Spain. Int J Stroke. 2020 Oct;15((7)):755–62. doi: 10.1177/1747493020938301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoyer C, Ebert A, Huttner HB, Puetz V, Kallmünzer B, Barlinn K, et al. Acute stroke in times of the COVID-19 pandemic: a Multicenter Study. Stroke. 2020;51((7)):2224–7. doi: 10.1161/STROKEAHA.120.030395. [DOI] [PubMed] [Google Scholar]
- 12.Rinkel LA, Prick JCM, Slot RER, Sombroek NMA, Burggraaff J, Groot AE, et al. Impact of the COVID-19 outbreak on acute stroke care. J Neurol. 2021 Feb;268((2)):403–8. doi: 10.1007/s00415-020-10069-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teo K-C, Leung WCY, Wong YK, Liu RKC, Chan AHY, Choi OMY, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020;51((7)):2228–31. doi: 10.1161/STROKEAHA.120.030105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diegoli H, Magalhães PSC, Martins SCO, Moro CHC, França PHC, Safanelli J, et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Stroke. 2020;51((8)):2315–21. doi: 10.1161/STROKEAHA.120.030481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsiao J, Sayles E, Antzoulatos E, Stanton RJ, Sucharew H, Broderick JP, et al. Effect of COVID-19 on emergent stroke care: a regional experience. Stroke. 2020;51((9)):e2111–4. doi: 10.1161/STROKEAHA.120.030499. STROKEAHA120030499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Uchino K, Kolikonda MK, Brown D, Kovi S, Collins D, Khawaja Z, et al. Decline in stroke presentations during COVID-19 surge. Stroke. 2020;51((8)):2544–7. doi: 10.1161/STROKEAHA.120.030331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lyden P. Temporary emergency guidance to US Stroke centers during the coronavirus disease 2019 (COVID-19) pandemic: on Behalf of the American Heart Association/American Stroke Association Stroke Council Leadership. Stroke. 2020;51:1910–2. doi: 10.1161/STROKEAHA.120.030023. [DOI] [PubMed] [Google Scholar]
- 18.Goyal M, Menon BK, Van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387((10029)):1723–31. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 19.Saver JL, Goyal M, Van Der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016;316((12)):1279–88. doi: 10.1001/jama.2016.13647. [DOI] [PubMed] [Google Scholar]
- 20.López-Cancio E, Ribó M, Cardona P, Serena J, Purroy F, Palomeras E, et al. Telestroke in Catalonia: increasing thrombolysis rate and avoiding interhospital transfers. Cerebrovasc Dis. 2018;46((1–2)):66–71. doi: 10.1159/000492124. [DOI] [PubMed] [Google Scholar]
- 21.Abilleira S, Pérez de la Ossa N, Jiménez X, Cardona P, Cocho D, Purroy F, et al. Transfer to the local stroke center versus direct transfer to endovascular center of acute stroke patients with suspected large vessel occlusion in the catalan territory (RACECAT): study protocol of a cluster randomized within a cohort trial. Int J Stroke. 2019;14((7)):734–44. doi: 10.1177/1747493019852176. [DOI] [PubMed] [Google Scholar]
- 22.Kerleroux B, Fabacher T, Bricout N, Moïse M, Testud B, Vingadassalom S, et al. Mechanical thrombectomy for acute ischemic stroke amid the COVID-19 outbreak: decreased activity, and increased care delays. Stroke. 2020;51((7)):2012–7. doi: 10.1161/STROKEAHA.120.030373. [DOI] [PubMed] [Google Scholar]
- 23.Yang B, Wang T, Chen J, Chen Y, Wang Y, Gao P, et al. Impact of the COVID-19 pandemic on the process and outcome of thrombectomy for acute ischemic stroke. J Neurointerv Surg. 2020;12((7)):664–8. doi: 10.1136/neurintsurg-2020-016177. [DOI] [PubMed] [Google Scholar]
- 24.Pedicelli A, Valente I, Pilato F, Distefano M, Colosimo C. Stroke priorities during COVID-19 outbreak: acting both fast and safe. J Stroke Cerebrovasc Dis. 2020;29((8)):104922–7. doi: 10.1016/j.jstrokecerebrovasdis.2020.104922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salahuddin H, Castonguay AC, Zaidi SF, Burgess R, Jadhav AP, Jumaa MA. Interventional stroke care in the era of COVID-19. Front Neurol. 2020;11:468–8. doi: 10.3389/fneur.2020.00468. [DOI] [PMC free article] [PubMed] [Google Scholar]