Abstract
Background
Older adults—classified as a high‐risk group—are highly likely to experience increased loneliness due to the implementation of various policies designed to prevent the spread of COVID‐19. Accordingly, this study aims to examine the effects of a pilot social prescribing project for elderly people in rural area of South Korea during the COVID‐19 pandemic.
Methods
Using the PRECEDE‐PROCEED model, the effectiveness of the pilot project was verified through pre‐ and post‐impact and outcome evaluation.
Results
According to the results of the impact evaluation, loneliness reduced significantly, while the social participation attitude score increased. Although the average score of self‐efficacy increased, it was not statistically significant. Moreover, it was found that self‐esteem increased significantly. In the outcome evaluation, depression reduced considerably.
Conclusion
To conclude, the pilot social prescribing project was effective in reducing depression and loneliness for the elderly in rural areas of Korea. It was also confirmed that there is potential to develop a new health promotion project that can improve the self‐esteem of the elderly, and expand their social activities. Second, the pilot project was carried out in an integrated manner by utilizing resources in communities with good accessibility. Therefore, it is expected to be used as a new “Integrated community care model” to improve the mental health of the elderly in rural areas. Third, during the COVID‐19 pandemic, the elderly tend to experience increasing feelings of depression, isolation, and loneliness due to “social distancing.” Therefore, it is expected that social prescribing programs for the elderly in rural areas would become a new alternative for relieve mental disorder of the seniors.
Keywords: COVID‐19, depression, elderly, rural area, social prescribing
1. INTRODUCTION
Since COVID‐19's beginning in Wuhan, Hubei Province, China, in December 2019, the virus has now spread worldwide. On March 12, 2020, the World Health Organization (WHO) issued its highest warning level, declaring COVID‐19 “a pandemic”. 1 The first confirmed case of COVID‐19 was reported in the Republic of Korea on January 20, 2020, when a 35‐year‐old Chinese woman tested positive for the virus. As of September 18, the total number of confirmed cases in Korea was 22 783, and the total number of deaths was 377. 2 This historically unprecedented pandemic has put individuals in a situation where they are disconnected from one another due to social distancing protocols, the inability to gather in public places, and the closure of educational institutions. According to the WHO, such situations have had a considerable negative effect on people, threatening their mental health. 3 The U.S. Centers for disease control and prevention (CDC) also reported that such situations attributable to COVID‐19 may induce considerable fear, anxiety, and stress in people, which can develop into symptoms of depression and affect their mental health. 4 And some research reflected both the physical and psychological pressure of the current COVID‐19 pandemic on people working in medical place. 5 In particular, older adults—classified as a high‐risk group—are highly likely to experience increased loneliness due to the implementation of various policies designed to prevent the spread of COVID‐19. 6 , 7 Accordingly, the need for COVID‐19 management programs for older adults is rising.
In 2016, the UK's National Health Service (NHS) administered a “social prescribing” program to reduce the burden on general practitioners (GPs), and address depression and loneliness among UK citizens. Social prescribing refers to providing a service that goes beyond medical treatment for a disease, linking patients with nonmedical community services. 8 A new concept based on the belief in social determinants of health, it is thought that health is greatly influenced by socioeconomic factors. 9 Nonmedical services provided in a community are diverse, including arts, physical activities, learning, volunteering, fellowship meetings, self‐help groups, social security benefits, and educational opportunities. 10 Professor Andy Haines of the United Kingdom predicted that the physical and mental health of vulnerable groups of people, such as the elderly, would be gravely affected by such situations as the COVID‐19 pandemic, in which social anxiety increases, and people are further isolated. Haines argued that social prescribing, while utilizing community resources would be an effective way to address the problem. 11 A study reported that a social prescribing program using community resources could be an option when the fatigue of healthcare personnel is rising from the prolonged COVID‐19 pandemic. 12 In Ontario, Canada, social prescribing guidelines and programs to cope with COVID‐19 have been newly formulated, 13 whereas the UK is implementing social prescribing programs centered around community NGOs. 14 In Korea, it has been suggested that it is necessary to develop a “Social prescribing program” that includes strategies such as keeping social distance, tele counselling in a pandemic era and online distance learning for health education. Taiwan is also discussing social prescribing as a way to cope with the pandemic. 15 It is thus clear that social prescribing programs for people suffering from the impact of COVID‐19 are being developed worldwide.
Accordingly, this study was conducted to identify the effectiveness of the social prescribing model in the COVID‐19 pandemic era by investigating its impact on depression, loneliness, and attitudes toward social participation, self‐efficacy, and self‐esteem in elderly people in South Korea.
2. METHODS
2.1. Study design
It was hypothesized that the interventions administered in the pilot social prescribing project would improve subjects' health status by modifying environmental and ecological factors. The effectiveness of the pilot project was tested by utilizing the PRECEDE‐PROCEED model, and conducting pre‐and post‐impact evaluations (Figure 1). 16
FIGURE 1.
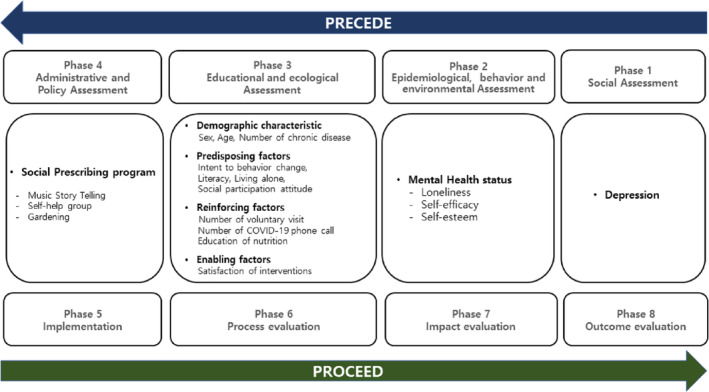
Research design
2.2. Interventions
The interventions were administered once a week for approximately 10 weeks from May 1 to July 10, 2020. The specific contents of the interventions are shown in Table 1. The interventions consisted of three parts: music storytelling, a self‐help group, and gardening. Two coordinators participated in all intervention programs, and interventions for the program were applied to the subjects in a parallel method.
TABLE 1.
Intervention activities in social prescribing program
| Intervention | Activities | Location | Time |
|---|---|---|---|
| Music storytelling |
|
Community library | One per a week (90 minutes) |
| |||
| |||
| Self‐help group (School of Hunjang) a |
|
Community library | One per a week (60 minutes) |
| |||
| |||
| |||
| |||
| Gardening |
|
Community garden | One per a week (30 minutes) |
| |||
| |||
| |||
| COVID‐19 prevention |
|
‐ | Three per a week |
|
Four per a week | ||
|
One per a week |
Hunjang: The teacher or headmaster of the seodang was called the hunjang.
The range of social prescribing services provided by the UK's NHS National Social Prescribing Network includes interventions of music, sports, arts, clubs, green activities, volunteering, learning, education, and so on (Karen et al., 2017). 17 , 18 The Music Storytelling program is a social prescribing that improves people's quality of life and alleviates mental health through artistic intervention in health (Philip et al., 2019). 19 , 20 Green activity in Social Prescribing program is such as gardening and horticulture, and through contact with nature, people become healthier physically and mentally (Karen et al, 2017). 18 Self‐help groups and volunteering, learning, and education programs have clear health benefits, and support for each other can increase social connectivity (Lee & Brudney, 2008; NHS England & NHS Improvement, 2016). 21 , 22 , 23
2.2.1. Music storytelling
Music storytelling refers to discovering stories that individuals have within through music therapy techniques to help them live better lives. 24 The contents of the music storytelling program are shown in Table 2. Including activities to strengthen seven domains (ie, cognition, sensation, language, physical functioning, ego, mind and body, and sociability), the program was led by two experts with the assistance of 17 university student volunteers. The volunteers were recruited from three universities located in the study area, and received 1‐week training prior to their participation. The music storytelling program was offered in the Heungeop community Library for 90 minutes every Wednesday, from May 1 to July 10, 2020.
TABLE 2.
Music story telling program
| Time | Theme | RFL (rhythm for life) | GIM (guide image music) | MIC (movement improvisation circle) |
|---|---|---|---|---|
| 1 to 3 Week | “I” | Rhythm of self‐introduction | “I” | Healthy clapping |
| Rhythm of self‐presentation | Making a story book (praise for completion) | Body tapping, massage | ||
| Rhythm of my hometown | Expressing my hometown | Healthy breathing | ||
| 4 to 6 Week | “You” | Rhythm of improvisation | “You” | Healthy clapping |
| Imitative and open Rhythm | Making a story book (drawing hand of my friend) | Healthy gymnastics (Hand in hand) | ||
| Expressing Rhythm with friends | Pleasure moments with friends | Healthy gymnastics (I like you) | ||
| 7 to 9 week | “We” | Rhythm of our hometown | “Our town” | Moving as a group |
| Song writing with “A‐ri‐rang” melody | Making a story book (10 rainbow healthy life rules) | Massaging with each other | ||
| Making a song of our town using “A‐ri‐rang” melody | Making a knot with each other | Dance a Waltz with each other | ||
| 10 week | Active | Group activity presentation (Ganggangsuwolrae) | Making a story book (with Korean Flag) | Group dance |
2.2.2. Self‐help group
The goals of self‐help groups are to provide older adults with mutual aid rather than a one‐directional service benefit, and establish a social support system. Self‐help groups have a positive impact on the self‐esteem of older adults and the formation of social networks. 25 In this study, a self‐help group was organized by utilizing the Heungup Township Community Library, one of the resources available in the study area. The group met for 60 minutes every Friday, and participants were encouraged to attend the program voluntarily. Program activities included making natural soaps, facemasks for the prevention of COVID‐19, and creating natural diffusers. Additionally, songs for healing were written for the community suffering due to COVID‐19, and education on healthy fruits and diets was provided under the theme of “stay healthy until the age of 100.” To improve understanding and keeping in mind the elderly participants' literacy levels, figures and photographs were utilized in the educational and nutritional material distributed.
2.2.3. Gardening
The American Horticultural Therapy Association (AHTA) defined horticultural therapy as the process of enhancing individuals' social, psychological, and physical adaptabilities through plants and gardening activities to promote physical, mental, and spiritual healing. 26 In this study, a community garden was created in collaboration with the Korea National Agricultural Extension Center, a community resource. A feeling of achievement was fostered among participants through productive activities such as growing sweet potatoes, peppers, cherry tomatoes, and corn. The program was conducted every week on Fridays, and participants were instructed to manage the garden in partnership with university student volunteers.
2.3. Study subjects
The program participants were 16 adults aged 65 or older, recommended by the Administrative and Welfare Office in a rural area in Gangwon Province. They consented to participate in the study's interventions over 10 weeks. Of the 16 participants, 10 attended all 10 program sessions, and these participants were selected as the study subjects. Arrangements were made for the subjects to visit a public health doctor at the community public health center for one‐on‐one, in‐person examinations pre‐ and post‐intervention. The doctor's medical statement contained information on clinical health status (including underlying disease), a neuropsychiatric evaluation regarding mood disorders and dementia status, and a physician's opinion on future treatment.
2.4. Data collection and the description of variables
The survey used in this study was comprised of items addressing socio‐demographics, depression, loneliness, social participation, self‐efficacy, and self‐esteem. The reliability and validity of the instruments were analyzed by a PhD in public health and a statistician. The survey was administered twice, before and after the interventions. To administer the survey, 13 survey takers were recruited and trained by the PhD student and statistician on the survey items and the administration method over 2 days, for approximately, 1 hour per day. The trained survey takers met in person with the subjects to whom they were allocated, and administered the survey in a one‐on‐one interview setting. The survey took an average of 15 minutes to complete.
2.4.1. Depression
As an instrument to measure the change in depression pre‐ and post‐intervention, the geriatric depression scale (GDS) was chosen, 27 and the Geriatric Depression Scale‐Korean Version (GDS‐K) was used, 28 keeping in mind the Korean‐speaking elderly subjects of the study. The GDS‐K consists of 30 items, and a score under 13 points is classified as normal, whereas a score of 14 to 18 indicates mild depression, a score of 19 to 21 indicates moderate depression, and a score over 22 signifies severe depression. The value of Cronbach's α, an index for reliability, was .84 in the GDS‐K validation study and .82 in this study, suggesting that the GDS‐K is a reliable instrument.
2.4.2. Loneliness
Loneliness was assessed using a scale revised from the UCLA Loneliness Scale translated into Korean. 29 Ten items that fit in with Korea's situation, five positive and five negative, were used in this study. The instrument used in the study had a Cronbach's α value of .70.
2.4.3. Social participation attitude
To examine the level of older adults' social participation in a variety of interpersonal relationships, the social participation scale for the elderly living alone was used. 30 The instrument consists of eight items evaluated on a five‐point scale. The Cronbach's α of the instrument was .90 in a previous study, and .85 in the present study.
2.4.4. Self‐efficacy
Self‐efficacy refers to a person's belief in his or her competence to perform successfully in producing a certain outcome. 31 To assess self‐efficacy, the Korean Adaptation of the General Self‐Efficacy Scale was used; it was based on the general self‐efficacy scale (GSE) developed by Schwarzer, 32 and tested for internal reliability. 33
2.4.5. Self‐esteem
Self‐esteem is the evaluative element in self‐perception and refers to a person's acceptance of self as a positive and worthwhile being. 34 In this study, self‐esteem was assessed with a Korean translation of the Rosenberg Self‐Esteem Scale. 35 , 54 The instrument consists of 10 items—five regarding positive self‐esteem and five regarding negative self‐esteem. All items were evaluated on a five‐point scale. Scores range from 10 to 50 and the higher the score, the higher one's self‐esteem. Cronbach's α for the entire instrument was .84.
2.5. Statistical analysis
The data were analyzed using SPSS Statistics (25.0 version). A Wilcoxon signed‐rank test was conducted for impact and outcome evaluations of the social prescribing programs. Specifically, the statistical analysis proceeded as follows. First, means and standard deviations were computed, and a frequency analysis was performed to examine subjects' sociodemographic, epidemiological, behavioral, and environmental factors, and assess the predisposing, reinforcing, and enabling factors. Second, the Wilcoxon signed‐rank test was conducted to examine changes before and after implementation of the social prescribing programs with respect to depression, loneliness, social participation attitude, self‐efficacy, and self‐esteem.
2.6. Ethical approval
This research protocal has been reviewed and approved by the Institutional Review Board (IRB) of Yonsei University Mirae Campus (number: 1041849‐202 010‐SB‐146‐04).
3. RESULTS
3.1. PRECEDE assessment before implementation of social prescribing programs
Results from the PRECEDE assessment phases are shown in Table 3. First, regarding the social assessment phase, all 10 subjects were female (100%). The mean age was 82.0 years, with six subjects (60.0%) responding that they were over 80, and four (40.0%) responding that they were under 80. Regarding the number of chronic illnesses, three was the most common answer (70.0%), followed by one (20.0%) and two (10.0%). Regarding the score for depression measured using the GDS‐K, six subjects (60.0%) scored 13 or lower (classified as normal); this category was the largest. The second largest category was mild depression, with two subjects (20.0%) whose scores were between 14 and 18, followed by one subject (10.0%) each falling in the categories of moderate depression (19‐21) and severe depression (22 and up).
TABLE 3.
PRECEDE assessment before social prescribing program (N = 10)
| Category | N | % | ||
|---|---|---|---|---|
| Social assessment | Demographic characteristics | |||
| Sex | Female | 10 | 100.0 | |
| Age | <80 | 4 | 40.0 | |
| ≥80 | 6 | 60.0 | ||
| Average | 82.0 (SD 5.9) | |||
| Number of chronic disease | 1 | 2 | 20.0 | |
| 2 | 1 | 10.0 | ||
| ≥ 3 | 7 | 70.0 | ||
| Depression (GDS‐K) | ||||
| GDS‐K score | ≤13 | 6 | 60.0 | |
| 14 ≤ 18 | 2 | 20.0 | ||
| 19 ≤ 21 | 1 | 10.0 | ||
| ≥22 | 1 | 10.0 | ||
| Epidemiological, behavior, and environmental assessment | Mental health status | |||
| Loneliness | ≤24 | 4 | 40.0 | |
| 25 ≤ 29 | 5 | 50.0 | ||
| ≥30 | 1 | 10.0 | ||
| Self‐efficacy | ≤22 | 5 | 50.0 | |
| 23 ≤ 26 | 3 | 30.0 | ||
| ≥28 | 2 | 20.0 | ||
| Self‐esteem | ≤31 | 3 | 30.0 | |
| 32 ≤ 36 | 6 | 60.0 | ||
| ≥37 | 1 | 10.0 | ||
| Diagnosis from doctor | ||||
| DSM‐5 (major depressive disorder) | Yes | 1 | 10.0 | |
| No | 9 | 90.0 | ||
| K‐MMSE (cognitive function decline) | Yes | 2 | 20.0 | |
| No | 8 | 80.0 | ||
| Predisposing factors | Social participation attitude | ≤ 31 | 3 | 30.0 |
| 32 ≤ 36 | 6 | 60.0 | ||
| ≥ 37 | 1 | 10.0 | ||
| Literacy | Yes | 3 | 30.0 | |
| No | 7 | 70.0 | ||
| Living alone | Yes | 9 | 90.0 | |
| No | 1 | 10.0 | ||
| Reinforcing factors | Voluntary visit (per a week) | Yes | 0 | 0.0 |
| No | 10 | 100.0 | ||
| COVID‐19 phone call (per a week) | Yes | 0 | 0.0 | |
| No | 10 | 100.0 | ||
| Education of healthy nutrition | Yes | 0 | 0.0 | |
| No | 10 | 100.0 | ||
| Enabling factors | Scale of happiness (total score: 100) | Average | 54.40 (SD 6.9) | |
In the epidemiological, behavioral, and environmental assessment phases, the scores for loneliness, self‐efficacy, and self‐esteem, as well as the Diagnostic and Statistical Manual of Mental Disorders (DSM‐5), and the Korea Mini‐Mental State Examination (K‐MMSE) test results, were analyzed. Regarding loneliness, the majority of subjects (n = 5, 50.0%) had a score between 25 and 29. The second most common score range was under 24 (n = 4, 40.0%), followed by a score over 30 (n = 1, 10.0%). In regard to self‐efficacy, the majority of subjects (n = 5, 50.0%) had a score under 22, followed by scores ranging from 23 to 26 (n = 3, 30.0%), and over 28 (n = 2, 20.0%). With regard to self‐esteem, the most common score range was 32 to 36 (n = 6, 60.0%), followed by a score under 31 (n = 3, 30.0%) and over 37 (n = 1, 10.0%). Regarding the DSM‐5 (major depressive disorder) test results, nine subjects (90.0%) were classified as “normal,” and one subject was classified as “requiring consultation with a psychiatrist.” Lastly, regarding the K‐MMSE (dementia status) test results, eight subjects (80.0%) were classified as normal, and two subjects (20.0%) as requiring consultation with a psychiatrist for cognitive competence.
For predisposing factors, social participation attitude and literacy were examined, as well as whether a subject lived alone. Regarding the score for social participation attitude, the largest group of subjects (n = 6, 60.0%) scored between 23 and 36. The second common score range was under 31 (n = 3, 30.0%) and over 37 (n = 1, 10.0%). In terms of literacy, seven subjects (70.0%) responded that they were illiterate; there were thus more illiterate subjects than literate subjects (n = 3, 30.0%). Of the 10 subjects, nine (90.0%) lived alone, and one subject (10.0%) lived with family members. For reinforcing factors, the following was chosen: the (weekly) number of visits by volunteers, the (weekly) number of phone calls regarding COVID‐19 prevention, and the number of times the subject received nutritional education. It was found that none of the subjects had these experiences. As an enabling factor, satisfaction with the social prescribing programs was examined using a scale for happiness before and after intervention. The mean happiness score was 54.40 (SD 6.9).
3.2. Progress evaluation after social prescribing programs
Results from the progress evaluation phase pre‐ and post‐implementation of the social prescribing pilot project are shown in Table 4. In the study, three social prescribing programs were executed as interventions, namely music storytelling, a self‐help group, and gardening. For reinforcing factors, the (weekly) number of visits by volunteers, the (weekly) number of phone calls regarding COVID‐19 prevention, and the number of times the subjects received nutritional education during the duration of the interventions were selected. None of the subjects had experienced any of the reinforcing factors prior to the intervention. After the interventions, the (weekly) number of visits by volunteers was three, the (weekly) number of phone calls regarding COVID‐19 prevention was four, and the number of sessions for nutritional education was six. As an enabling factor, satisfaction with the social prescribing programs was evaluated by measuring the level of happiness pre‐ and post‐intervention; for the predisposing factor, the attitude toward social participation was measured. The mean happiness score was 54.40 (SD 6.9) before intervention, and 83.20 (SD 6.4) after. Mean scores for the attitude toward social participation were 29.90 (SD 5.7) and 35.10 (SD 3.3) before and after intervention, respectively.
TABLE 4.
Progress evaluation after social prescribing program (N = 10)
| Category | Before | After | ||
|---|---|---|---|---|
| M ± SD | ||||
| Reinforcing factors | Number of voluntary visit (per a week) | 0 | 3 | |
| Number of COVID‐19 phone call (per a week) | 0 | 4 | ||
| Education of healthy nutrition | 0 | 6 | ||
| Enabling factors | Satisfaction of social prescribing program | Scale of happiness (total score: 100) | 54.40 (SD 6.9) | 83.20 (SD 6.4) |
| Predisposing factors | Social participation attitude change | 29.90 (SD 5.7) | 35.10 (SD 3.3) | |
| Progress evaluation | Mental health | Loneliness | 25.60 (SD 2.5) | 22.20 (SD 5.0) |
| Self‐efficacy | 23.40 (SD 4.8) | 27.00 (SD 6.3) | ||
| Self‐esteem | 31.80 (SD 4.2) | 38.40 (SD 6.3) | ||
| Depression (GDS‐K) | 13.60 (SD 5.0) | 10.00 (SD 3.7) | ||
In the progress evaluation phase, subjects' characteristics were evaluated. According to the findings, the mean loneliness score was 25.60 (SD 2.5) before intervention, and 22.20 (SD 5.0) after. Regarding self‐efficacy, the mean pre‐intervention score was 23.40 (SD 4.8), and the mean post‐intervention score was 27.00 (SD 6.3). Regarding self‐esteem, the mean pre‐intervention score was 31.80 (SD 4.2), and the mean post‐intervention score was 38.40 (SD 6.3). Lastly, the mean pre‐intervention depression score, measured with the GDS‐K, was 13.60 (SD 5.0), and the mean post‐intervention score was 10.00 (SD 3.7).
3.3. Impact and outcome evaluation after the social prescribing project
The Wilcoxon signed‐rank test was performed to evaluate the pre‐ and post‐impact and outcome of the pilot social prescribing project and the results are presented in Table 5. To evaluate the impact of the pilot project, pre/post changes in loneliness, social participation attitude, self‐efficacy, and self‐esteem were analyzed. First, loneliness tended to decrease statistically (Z = −1.684, P < .1). Furthermore, the attitude toward social participation statistically and significantly increased (Z = −2.173, P < .05) after intervention. The mean self‐efficacy score improved post‐intervention, although the increase was not statistically significant. Self‐esteem was statistically and significantly elevated (Z = −2.521, P < .05) after intervention. For the outcome evaluation of the pilot project, the change in depression was examined, and it was found that depression had significantly decreased (Z = −2.829, P < .01; Figure 2).
TABLE 5.
Impact and outcome evaluation after social prescribing program (N = 10)
| Category | N | Mean Rank | Sum of Ranks | z | ||
|---|---|---|---|---|---|---|
| Impact evaluation | Loneliness a | (−) Rank | 7 | 6.29 | 44.00 | −1.684* |
| (+) Rank | 3 | 3.67 | 11.00 | |||
| Ties | 0 | |||||
| Social participation b | (−) Rank | 1 | 2.50 | 2.50 | −2.173** | |
| (+) Rank | 7 | 4.79 | 33.50 | |||
| Ties | 2 | |||||
| Self‐efficacy b | (−) Rank | 3 | 4.67 | 14.00 | −1.011 | |
| (+) Rank | 6 | 6 | 31.00 | |||
| Ties | 1 | |||||
| Self‐esteem b | (−) Rank | 0 | 0 | 0 | −2.521** | |
| (+) Rank | 8 | 4.5 | 36.00 | |||
| Ties | 2 | |||||
| Outcome evaluation | Depression (GDS‐K) a | (−) Rank | 10 | 5.50 | 55.00 | −2.829*** |
| (+) Rank | 0 | 0 | 0 | |||
| Ties | 0 | |||||
Reference: (+) Rank.
Reference: (−) Rank.
P < .1.
P < .05.
P < .01.
FIGURE 2.
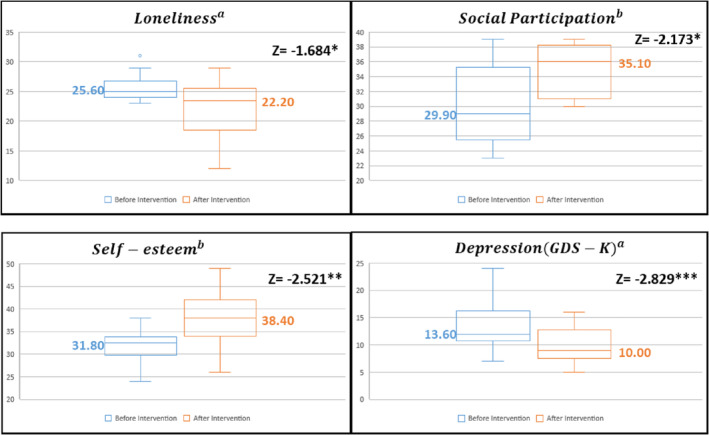
Impact and outcome evaluation boxplot
4. DISCUSSION
For the subjects who participated in all three social prescribing intervention programs (music storytelling, the self‐help group, and gardening), scores for both depression and loneliness decreased statistically and significantly, whereas social participation attitude and self‐esteem statistically and significantly increased. Previous studies have found that social prescribing programs had the effect of lowering depression, 36 , 37 and, along with related activities, were effective in easing loneliness and the feeling of isolation in older adults. 38 , 39 , 40 In addition, according to Munford, 10 who studied the effect of a social prescribing program for adults aged 65 or older with a chronic illness in Salford, northern England, and the use of a community‐based social prescribing program enhanced their overall quality of life, positive moods, interpersonal relationships, and self‐esteem. It also lowered helplessness and fatigue indices. In particular, social prescribing programs that are developed utilizing community assets, and designed to fit the unique features of the community and individual situations, have better potential for success. 41 In the present study, the social prescribing program was executed for older adults in a rural area using community assets, such as the Community Library, and positive findings were obtained (similar to those of previous studies). Additionally, each subject's health status was examined by a public health doctor before and after intervention, and subjects participated in the program based on the doctor's recommendation. Accordingly, the study was structured similarly to the UK's social prescribing model. 17 In social prescribing programs, patients are diagnosed by a doctor, and customized social prescriptions are supported through a social prescription coordinator (Link Worker). Primary care clinician makes a social prescription—a referral—after fulsome discussions and connected to social and community supports. These social prescribing programs can reduce the burdensome work of doctors through connection to nonpharmaceutical treatment in the community rather than drug treatment, and can be effective in solving chronic diseases and mental health problems. In addition, it can be a way to reduce the burden of medical expenses due to excessive medical use. 42
On the other hand, it has been stated that for a social prescribing intervention program to be successful, the program should generally involve subjects' productive participation and transformation, a community‐based approach, and should be implemented in an integrative manner. 43 The social prescribing intervention programs in this study had all of these features. Regardless of how beneficial an activity might be, if depressed lonely older adults perceive it as something for “lonely older people,” they immediately regard it as an undesirable or unhelpful service, and their participation rate drops precipitously. 44 The participation rate was high in the present study because opportunities for voluntary participation were made available to study subjects through the self‐help group and programs that were familiar to them, owing to the active use of community resources. Further, as subjects were engaged in productive outdoor activities via the gardening program, interpersonal relationships improved, while self‐esteem and feelings of achievement increased. One of the primary effects of horticultural therapy and gardening is increased self‐esteem. Goals of music storytelling include the reinforcement of cognitive competence and sensations, linguistic competence improvement, a calm mind and body, increased sociability, self‐discovery, and enhanced physical functioning. In the present study, music and stories were combined, and psychological counselling techniques were utilized in music storytelling. A previous study found that a music storytelling program for older adults in rural areas had the effects of “joy from participating,” “vitality from intergenerational exchanges,” and “expanded interpersonal relationships”. 37 Another study reported that social prescribing and the use of music had the positive impacts of reducing stress and increasing social participation. 19 Based on the current study findings, it seems that a social prescribing program is effective in lessening depression and loneliness in older adults in rural areas; additionally, self‐esteem is positively influenced and social participation can be expected to increase. Accordingly, the findings show that it would be feasible to develop a social prescribing program for a new rural‐type health promotion project in South Korea.
Social prescribing can be an option to manage the mental health of rural community residents during the COVID‐19 pandemic. 45 The WHO recommends that efforts be made to stay physically “active” in order to maintain physical and mental capacities for recovery, even though the COVID‐19 situation is worsening. 46 In the COVID‐19 pandemic, older adults are experiencing heightened feelings of depression, loneliness, and social isolation from being alone. 47 The United Kingdom is providing social prescribing interventions to strengthen primary healthcare during the COVID‐19 pandemic by utilizing community health and welfare workers. 48 In this study too, social prescribing programs were implemented during the pandemic, and such activities as the transmission of accurate information on COVID‐19 via promotional data, social prescribing through telecommunication (via telephone), and the delivery of COVID‐19 protection gear were supported. It was anticipated that a social prescribing program would be more effective in a crisis because of its basis: an asset‐based community development (ABCD) model approach, formulated according to the theory of salutogenesis, integrated with customized nonmedical service. 45 , 49 As the COVID‐19 pandemic persists, many complications have been arising, to the extent of coining the term “Corona Blues”. 50 Policy solutions, however, are lacking. The US CDC stated that a conscious effort to reinforce communities would be needed to cope with stress and loneliness resulting from COVID‐19, 4 and many studies warn that drinking, smoking, and drug use may further exacerbate depression. 51 , 52 , 53 Accordingly, to solve the mental health problems of older adults in rural areas during the COVID‐19 pandemic, it is necessary to formulate an integrative community care model for social prescribing, appropriate for the current pandemic situation in the use and linking of community assets, while public health centers responsible for primary healthcare and Administrative and Welfare offices also play a central role. On the basis of the study results, it is believed that such social prescribing programs can provide an effective psychological defense for the rural elderly, who may tend to become easily withdrawn as indoor activity increases because of the social distancing policy for COVID‐19 prevention.
There are also several limitations in this study. First, this study only analyzed participants who attended all 10 weeks in the social prescribing program. Because the high average of the subjects led to manage and coordinate the attendance difficulty. Therefore, it is necessary to consider how to manage the dropout rate of research subjects in future social prescription programs. Second, since research related to social prescribing is a process that requires finding an integrated basis for a wide variety of intervention programs, not only quantitative studies but also qualitative studies are important. 43 Therefore, in future studies, it is necessary to evaluate the effectiveness using a research method that combines not only quantitative studies but also qualitative studies. Third, the social prescribing pilot project conducted in Korea left some weaknesses. This study is small‐scale, does not have a control group, much of the evidence available is qualitative, and relies on self‐reported outcomes. However, there is a growing body of evidence that social prescribing can lead to a range of positive health and wellbeing outcomes. If the social prescribing project is expanded in integrated with local communities and local social enterprises, more sophisticated scientific research will be possible.
5. CONCLUSION
First, the social prescribing programs were effective in reducing depression and loneliness in elderly people in rural area. Additionally, it was confirmed that it is feasible to develop such programs for a new health promotion project in which self‐esteem is positively influenced, and greater social participation of older adults can be expected.
Second, the pilot social prescribing project was executed in an integrative manner, utilizing community resources with excellent accessibility. Hence, it is anticipated that the project could be used as a new integrated community care model to promote mental health in elderly people in rural area.
Third, as indoor activity increases because of social distancing and other policies in the COVID‐19 pandemic era, it is expected that social prescribing programs would be a new alternative to equip elderly people in rural areas—who would typically withdraw from social participation and feel increasingly more depressed, isolated, and lonely—with an effective psychological defense.
CONFLICT OF INTEREST
All authors declare that they have no conflict of interest to declare.
AUTHOR CONTRIBUTIONS
Conceptualization: Ji Eon Kim, Eun Woo Nam, Dong Eun Shin
Data Curation: Si Chen, Yan Wang
Funding Acquisition: Eun Woo Nam, Jin Hee Choi
Investigation: Ji Eon Kim, Yu Lim Lee, Min Ah Chung, Hye Jin Yoon, Sangheon Lee
Methodology: Ji Eon Kim, Eun Woo Nam
Project Administration: Eun Woo Nam, Hae Kyung Kim
Resources: Ji Eon Kim, Eun Woo Nam, Dong Eun Shin
Supervision: Eun Woo Nam
Writing—Original Draft Preparation: Ji Eon Kim
Writing—Review & Editing: Ji Eon Kim, Eun Woo Nam
All authors have read and approved the final version of the manuscript.
Eun Woo Nam had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
TRANSPARENCY STATEMENT
The lead author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Kim JE, Lee YL, Chung MA, et al. Effects of social prescribing pilot project for the elderly in rural area of South Korea during COVID‐19 pandemic. Health Sci Rep. 2021;4:e320. 10.1002/hsr2.320
Funding information National Research Foundation of Korea, Grant/Award Number: NRF‐2018S1A5A2A03039636; Ministry of Education of the Republic of Korea
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the findings of this study are available within the article supplementary materials.
REFERENCES
- 1. WHO . Stay physically active during self‐quarantine; 2020a. https://www.euro.who.int/en/health‐topics/health‐emergencies/coronavirus‐covid‐19/technical‐guidance/stay‐physically‐active‐during‐self‐quarantine
- 2. COVID‐19 Dashboard . 2020. https://coronaboard.kr/
- 3. WHO . Looking after our mental health; 2020b. https://www.who.int/news‐room/campaigns/connecting‐the‐world‐to‐combat‐Coronavirus/healthyathome/healthyathome‐mental‐health?gclid=Cj0KCQjwn7j2BRDrARIsAHJkxmyuL1b2BYDtck3UvORx2Tcif_bQBCQnFBmC4B6OXm7YoSb3iXIbzXsaAhGHEALw_wcB
- 4. Centers for Disease Control and Prevention (CDC) . Coronavirus Disease 2019 (COVID‐19); 2020. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html
- 5. Amerio A, Bianchi D, Santi F, et al. Covid‐19 pandemic impact on mental health: a web‐based cross‐sectional survey on a sample of Italian general practitioners. Acta Bio‐Med. 2020;91(2):83‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. American Psychological Association . COVID‐19 isn't just a danger to older people's physical health; 2020. https://www.apa.org/news/apa/2020/03/covid-19-danger-physical-health
- 7. Miller G. Social distancing prevents infections, but it can have unintended consequences. Science. 2020;1. 10.1126/science.abb7506. [DOI] [Google Scholar]
- 8. National Academy for Social Prescribing . A social revolution in wellbeing; 2020. https://tinyurl.com/y7b8mav4
- 9. Drinkwater C, Wildman J, Moffatt S. Social prescribing. BMJ. 2019;364:l1285. [DOI] [PubMed] [Google Scholar]
- 10. Munford LA, Panagioti M, Bower P, Skevington SM. Community asset participation and social medicine increases qualities of life. Soc Sci Med. 2020;259:113149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Haines A, de Barros EF, Berlin A, Heymann DL, Harris MJ. National UKprogramme of community health workers for COVID‐19 response. Lancet. 2020;395(10231):1173‐1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID‐19 among front‐line health‐care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475‐e483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alliance for Healthier Communities . 2020. https://www.allianceon.org/news/Ontarios-Social-Prescribing-pilot-project-shows-strength-community-health-interventions
- 14. Elemental UK Ltd . 2020. https://elementalsoftware.co/strengthening‐community‐support‐through‐digital‐social‐prescribing‐during‐covid‐19/
- 15. Hung T. Strengthening Communicable Disease Control in Communities with Social Prescriptions. Thinking Taiwan. 2020. https://www.thinkingtaiwan.com/content/8192
- 16. Green L, Kreuter M. The Precede–Proceed Model. Health Promotion Planning: an Educational Approach. 3rd ed. Mountain View, CA: Mayfield Publishing Company; 1999:32‐43. [Google Scholar]
- 17. Polley M, Fleming J, Anfilogoff T, et al. Making sense of social prescribing; 2017. https://www.westminster.ac.uk/patient-outcomes-in-health-research-group/projects/social-prescribing-network
- 18. STEADMAN Karen, THOMAS Rosemary, DONNALOJA Victoria, The Work Foundation . Social prescribing: a pathway to work?. Social Care Institute for Excellence (SCIE). 2017. https://www.scie.org.uk/prevention/research‐practice/getdetailedresultbyid?id=a11G000000PYsKCIA1. [Google Scholar]
- 19. Fleischer S, Grehan M. The arts and health: moving beyond traditional medicine. J Appl Arts Health. 2016;7(1):93‐105. [Google Scholar]
- 20. Philip K, Lewis A, Hopkinson NS. Music and dance in chronic lung disease. Breathe. 2019;15(2):116‐120. 10.1183/20734735.0007-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lancu I, Olmer A. The minimental state examination—an up‐to‐date review. Harefuah. 2006;145(9):687‐701. [PubMed] [Google Scholar]
- 22. Lee Y‐J, Brudney JL. The impact of volunteering on successful ageing: a review with implications for programme design. The journal of the Institute for Volunteering Research. 2008;9(1):21‐36. [Google Scholar]
- 23. England N.H.S., & Improvement, N.H.S . NHS operational planning and contracting guidance 2017‐2019, 2016. [Google Scholar]
- 24. Korean Intellectual Property Office . n.d. No. 41‐0270261.
- 25. Cho SH, Kim HS. A study on depression of low‐income elderly people who live alone—focusing on the moderating effect of social support. Crisis. 2015;11(11):55‐71. [Google Scholar]
- 26. American Horticultural Therapy Association . American Horticultural Therapy Association Definitions and Positions. Washington, DC: American Horticultural Therapy Association; 2013. [Google Scholar]
- 27. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17(1):37‐49. [DOI] [PubMed] [Google Scholar]
- 28. Gi BS, Lee CW. A preliminary study for the standardization of geriatric depression scale in Korea. Psychiatry Investig. 1995;129(6):1875‐1885. [Google Scholar]
- 29. Russell D, Peplau LA, Cutrona CE. The revised UCLA loneliness scale: concurrent and discriminant validity evidence. J Pers Soc Psychol. 1980;39(3):472‐480. [DOI] [PubMed] [Google Scholar]
- 30. Cho SH, Yoo YS. The effects of participation in social activity on life satisfaction in low‐income aged people living alone: focusing on the mediating effects of loneliness. Korean Soc Gerontol Soc Welfare. 2016;71(4):35‐59. [Google Scholar]
- 31. Bandura Albert. Social Foundations of Thought and Action. Englewood Cliffs, NJ; 1986:23‐28. [Google Scholar]
- 32. Schwarzer R. General perceived self‐efficacy in 14 cultures. Self‐Self‐Efficacy assessment; 1999. http://userpage.fu-berlin.de/~gesund/publicat/ehps_cd/health/world14.htm
- 33. Lee YM, Schwarzer R, & Jerusalem M. Korean adaptation of the general self‐efficacy scale; 1994.
- 34. Taft LB. Self‐esteem in later life: a nursing perspective. Adv Nurs Sci. 1985;8(1):77‐84. 10.1097/00012272-198510000-00009. [DOI] [PubMed] [Google Scholar]
- 35. Rosenberg M. Rosenberg self‐esteem scale (RSE). Acceptance and Commitment Therapy. Measures Package. 1965;61(52):18. [Google Scholar]
- 36. Kimberlee R. What is the value of social prescribing? Adv Soc Sci Res J. 2016;3(3):29‐35. 10.14738/assrj.33.1889. [DOI] [Google Scholar]
- 37. Geu‐Rum S, Hye‐Yeon J, Eun‐Woo N. Effects of a social prescribing program on the depressive status of elderly people in a rural area of Gangwon‐do. Korean Publ Health Assoc. 2019;45(4):77‐87. [Google Scholar]
- 38. Kellezi B, Wakefield JRH, Stevenson C, et al. The social cure of social prescribing: a mixed‐methods study on the benefits of social connectedness on quality and effectiveness of care provision. BMJ Open. 2019;9(11):e033137. 10.1136/bmjopen-2019-033137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Stall NM, Savage RD, Rochon PA. Loneliness in older adults. CMAJ. 2019;191(17):E476‐E476. 10.1503/cmaj. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Woodall J, Trigwell J, Bunyan M‐A, et al. Understanding the effectiveness and mechanisms of a social prescribing service: a mixed methods analysis. BMC Health Serv Res. 2018;18:604. 10.1186/s12913-018-3437-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wildman JM, Valtorta N, Moffatt S, Hanratty B. ‘What works here doesn't work there’: the significance of local context for sustainable and replicable asset‐based community intervention aimed at promoting social interaction in later life. Health Soc Care Commun. 2019;27:1102‐1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Dronina Y, Ndombi GO, Kim JE, Nam EW. Financing mechanisms of social prescribing projects: a systematic review. Health Policy and Management. 2020;30(4):513‐521. [Google Scholar]
- 43. Gardiner C, Geldenhuys G, Gott M. Interventions to reduce social isolation and loneliness among older people: an integrative review. Health Soc Care Community. 2018;26(2):147‐157. [DOI] [PubMed] [Google Scholar]
- 44. Kharicha K, Iliffe S, Manthorpe J, et al. What do older people experiencing loneliness think about primary care or community based interventions to reduce loneliness? A qualitative study in England. Health Soc Care Community. 2017;25(6):1733‐1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Nam EW. Overcome social isolation and depression of COVID‐19 outbreak era. Korean Journal of Health Education and Promotion. 2020;37(1):113‐116. 10.14367/kjhep.2020.37.1.113. [DOI] [Google Scholar]
- 46. WHO . WHO announces COVID‐19 outbreak a pandemic; 2020c. https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic
- 47. Berg‐Weger M, Morley JE. Loneliness and social isolation in older adults during the Covid‐19 pandemic: implications for gerontological social work. J Nutr Health Ageing. 2020;24(5):456‐458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Razai MS, Oakeshott P, Kankam H, Galea S, Stokes‐Lampard H. Mitigating the psychological effects of social isolation during the covid‐19 pandemic. BMJ. 2020;369:1‐5. [DOI] [PubMed] [Google Scholar]
- 49. Howarth M, Griffiths A, da Silva A, Green R. Social prescribing: a ‘natural’ community‐based solution. Br J Community Nurs. 2020;25(6):294‐298. [DOI] [PubMed] [Google Scholar]
- 50. The Kukmin Daily . 2020. http://news.kmib.co.kr/article/view.asp?arcid=0014987129&code=61121111
- 51. Satre DD, Hirschtritt ME, Silverberg MJ, Sterling SA. Addressing problems with alcohol and other substances among older adults during the COVID‐19 pandemic. Am J Geriatr Psychiatry. 2020;28(7):780‐783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Sharp LA. Looking after your mental health during the COVID‐19 pandemic. Aust Nurs Midwifery J. 2020;26(11):4. [Google Scholar]
- 53. Stanton R, To QG, Khalesi S, et al. Depression, anxiety and stress during COVID‐19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020;17(11):4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Jon BJ. Self‐esteem: a test of its measurability. Yonsei J. 1974;11:107‐129. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article supplementary materials.


