Abstract
Background:
The purpose of the current study is to identify the correlations between the most important preoperative clinical factors and the outcome of surgery of spinal meningiomas (SM).
Methods:
We performed a retrospective analysis of the medical history, clinical, paraclinical, neuroimaging, and surgical protocol data in 31 patients with SM who underwent surgical resection at our institution from January 2011 to July 2020. The degree of resection was assessed on the Simpson scale. The modified McCormick scale was used to monitor the effect and outcome of treatment at admission, discharge, and at further follow-up.
Results:
The average age of the patients was 65 years (37-78). Vertebral pain and motor deficits were the most common initial symptoms that occurred in 26 (89.6%) and 29 (93.5%) patients, respectively. Sphincter disorders were found in 9 (29%) patients. Total resection (Simpson Grade I – II) was achieved in 29 patients (93.5%). We achieved a favorable outcome (McCormick Gr. I to III) in 93.3% of patients. The degree of the neurological deficit (P = 0.026) and the presence of sphincter disorders (P = 0.009) were the preoperative clinical factors that most significantly correlated with the outcome of treatment.
Conclusion:
The outcome from the surgical treatment of SM correlated significantly with the degree of the preoperative neurological deficit. Therefore, patients presenting with more severe symptoms are expected to have worse outcomes.
Keywords: Myelopathy, Outcome, Risk factors, Spinal meningioma, Surgery

INTRODUCTION
Spinal meningiomas (SM) represent about 1–2% of all meningiomas and 25–45% of all intradural extramedullary spinal tumors.[22] Annual incidence of SM is 0,62 per 100,000 people.[8] Most SMs are solitary and entirely intradural, but in about 10% of cases, they can be intra-extradural, and in extremely rare cases, purely extradural or intramedullary.[4] SM are observed in all age groups but occur mostly between the 5th and 7th decade of life, with 75% of cases occurring in women, and approximately 80% are located in the thoracic spine.[6,19]
The upper cervical spine and foramen magnum are also common sites for SM occurrence.[15] Subaxial cervical and lumbar meningiomas are relatively rare.[30] SMs are slow-growing neoplasms that cause clinical symptoms when reaching a size that causes compression to the spinal cord and/or nerve roots.[31] The typical clinical presentation begins with pain followed by sensory deficits, gait disturbance, and sphincter dysfunction.[18] Their size, ventral localization, and presence of calcifications still pose a challenge to neurosurgeons in successfully treating SMs.[28]
The purpose of the current study is to identify the correlations between the most important preoperative clinical factors and the outcome of surgery of SM.
MATERIALS AND METHODS
This study was approved by the Ethics Committee of St Georgi University Hospital. The patient data from medical histories, clinical presentation, paraclinical tests, diagnostic imaging, and surgical protocols were retrospectively collected. Attention was paid to the symptoms at onset, clinical presentation at admission, neuroimaging data, localization, type of surgical intervention, histology, and outcome of the disease. The degree of resection was assessed on the Simpson scale.[32] The neurological deficit before and after surgical treatment was assessed by the Modified McCormick scale based on a retrospective chart review. The scale has five grades: (i) normal neurological status with or without minimal dysesthesia; (ii) mild motor or sensory deficit; (iii) moderate deficit with a slightly limited function, independent of foreign aid; (iv) severe motor or sensory deficit, dependent on foreign aid, and (v) paraplegia/ quadriplegia.[19] The long-term outcome was also assessed by the Modified McCormick scale during outpatient visits. For statistical analysis, the modified McCormick Grades I – III were considered favorable, while Grades IV – V were deemed unfavorable.[14] Follow-up ranged from 1 to 105 months, median of 43 months, most were discontinued after 24 months.
Statistical analysis
The Chi-square test was used to compare categorical data and the nonparametric Mann–Whitney U test to compare variables grouped in rank scales. The bilateral significance level was determined to be P < 0.05.
RESULTS
Thirty-one patients underwent 32 surgical interventions for SM at our institution from January 2011 to July 2020 (29 women [93.5%] and 2 men [6.5%] aged between 37 and 78 years, mean age 65 years). One patient underwent surgery for meningioma recurrence 4 years after the first operation. Twenty-eight (90.3%) of the tumors were intradural extramedullary, two (6.5%) had extradural extension, and one (3.2%) was intramedullary.
In 26 (83.9%) patients, the disease debuted with low back and/or back pain, and 29 (93.5%) patients had additional motor deficits that gradually progressed over time. Twenty-one of the patients (67.7%) had lower extremity paraparesis, 3 (9.7%) had lower extremity paraplegia, 4 (12.9%) had quadriparesis, and one (3.2%) had unilateral lower extremity paresis. Sphincter disorders were found in 9 (29%) patients. The period from the disease onset to its diagnosis varied from 1 to 36 months (median 6.0 months; IQR = 8.0). The clinical symptoms, the localization, and SM’s location relative to the axial section of the spinal cord and cauda equina are presented in [Tables 1 and 2].
Table 1:
Clinical symptoms at admission of patients with spinal meningiomas.
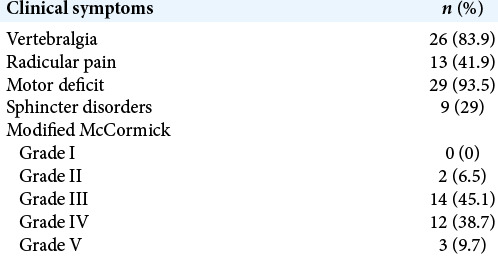
Table 2:
Localization and axial location of spinal meningiomas.
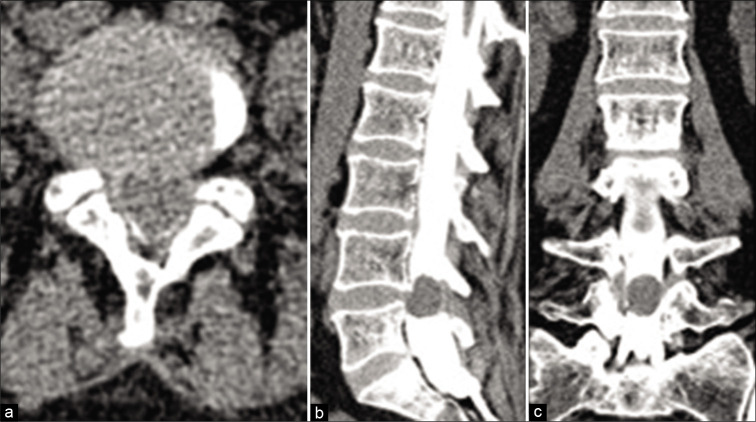
In 1 patient who was contraindicated to magnetic resonance imaging (MRI) investigation, the diagnosis was achieved by computed tomography (CT)-assisted myelography [Figure 1]. In the remaining 30 patients, MRI was used to confirm the diagnosis [Figures 2-5].
Figure 1:
CT-assisted myelography in a patient with a meningioma at the level of L4-L5: (a) CT axial projection; (b and c) sagittal and coronal reconstructions.
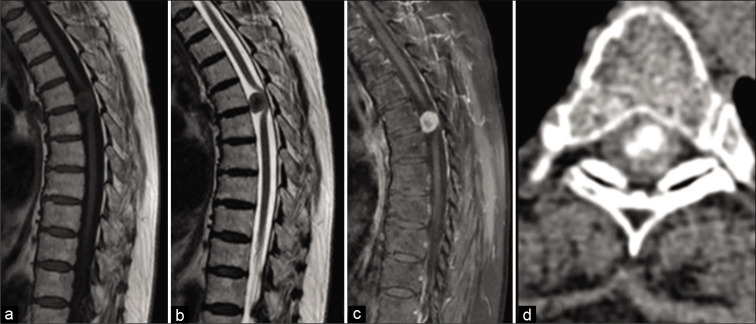
Figure 2:

Sagittal MRI of spinal meningioma at the level of T9 vertebra. (a) T1-weighted image; (b) T2-weighted image.
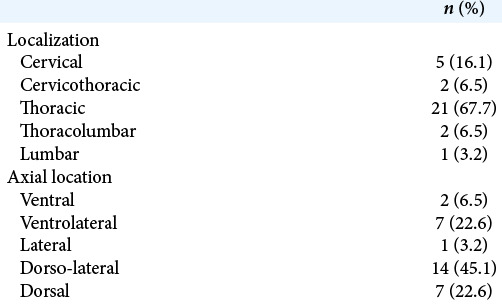
Figure 5:
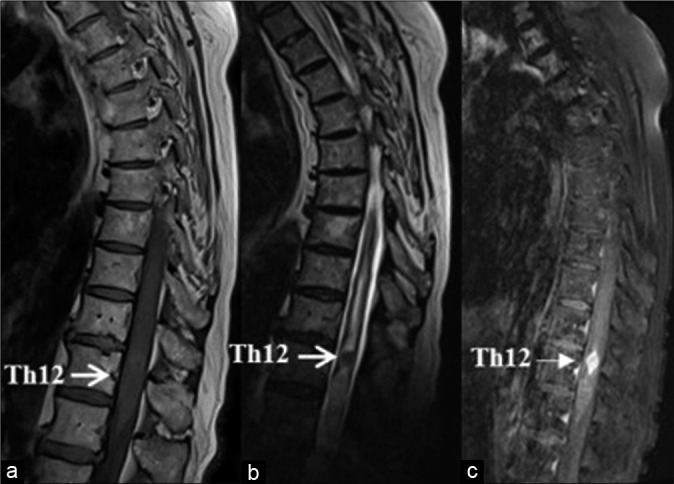
Sagittal MRI of a patient with an intramedullary meningioma (white arrow) (a) T1-weighted image shows an isointense lesion with a spindle-shaped expansion of the medulla; (b) T2-weighted image demonstrates ovoid hypointense lesion with associated hydromyelia; (c) Enhanced T1-weighted image shows a homogeneous accumulation of the contrast media by the tumor.
Figure 3:

Sagittal MRI of ventrolateral meningioma at the level of T3 vertebra. (a) T1 without enhancement – isointense signal; (b) T1 with gadolinium enhancement – homogeneous accumulation of contrast that demonstrated the presence of “dural tail sign” (white arrow).
We used posterior or posterolateral surgical access in all operated patients. The goal of surgery was total tumor removal. In 30 patients (96.8%), the access used was laminectomy and in one – hemilaminectomy. Total resection (Simpson Grade I and II) was achieved in 29 patients (93.5%) [Figure 6]. Subtotal resection was performed in one patient with high cervical meningioma that extended to the foramen magnum and engulfed the vertebral artery. Another patient underwent Simpson Grade III resection because the lesion was located intra- and extradurally, with infiltration and destruction of surrounding bone structures. Intraoperative neurophysiological monitoring (IONM) was used in one patient with thoracic intramedullary meningioma [Figure 5].
Figure 6:
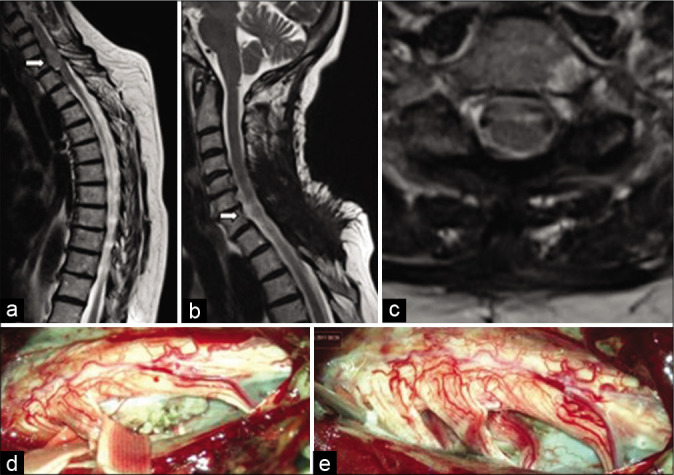
(a) Preoperative sagittal T2 MRI – ventrolateral meningioma at the level of C7 vertebra (white arrow); (b and c) postoperative sagittal and axial MRI confirms total tumor removal; (d and e) intraoperative images at the beginning and the end of the surgical procedure.
The histological result in 29 patients revealed WHO Grade I psammomatous type of meningioma. In one patient, the tumor had pronounced adjacent bone metaplasia [Figure 7]. In the rest two patients, the meningiomas were atypical (WHO Grade II) [Figure 8].
Figure 7:
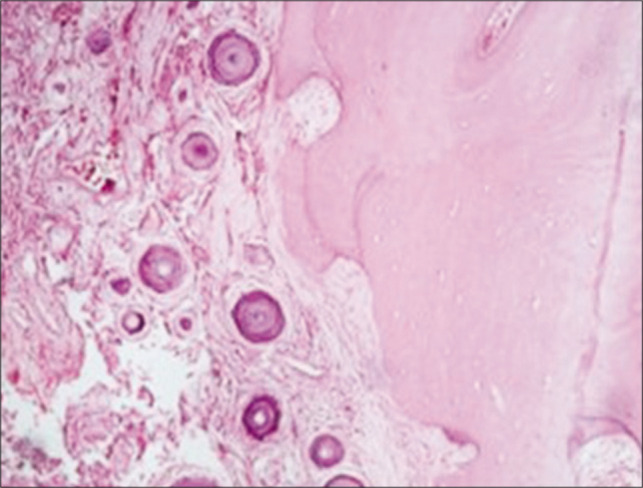
Psammomatous meningioma with adjacent bone metaplasia. Psammoma bodies are visible on the left, an area with bone metaplasia is outlined on the right (hematoxylin-eosin, ×200).
Figure 8:
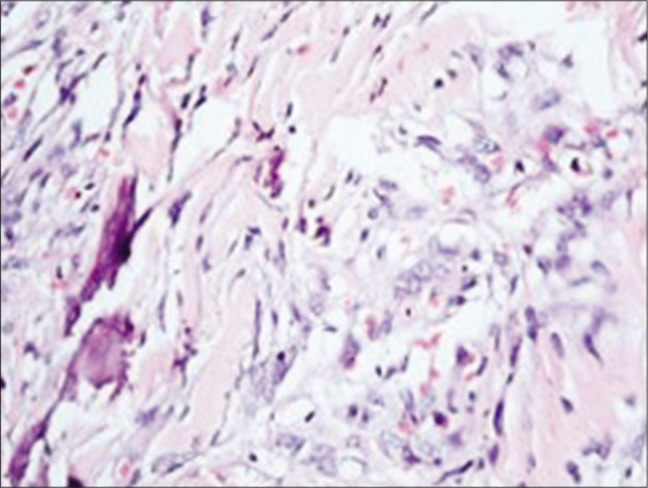
Atypical meningioma with bone metaplasia. Bone septs are visible on the left, an area of the tumor with pronounced cellular atypism is outlined on the right (hematoxylin-eosin, ×200).
In 30 patients (96.8%), the postoperative period was uneventful. All patients had improvement in their neurological status. One patient developed hemorrhagic stroke at the second postoperative day, which spontaneously resorbed after conservative treatment for 17 days. The median hospital stay was 14.5 days (Min = 9.0; Max = 30.0; IQR = 10.25).
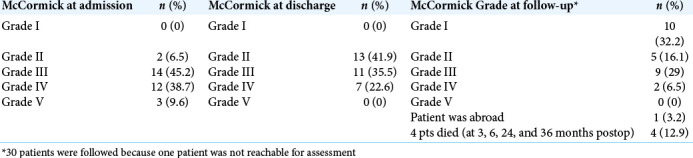
Preoperatively, the patients with McCormick Grade I-III were 16 (51.6%), while the remaining 15 (48.4%) were with McCormick Grade IV-V. After treatment, the number of patients with McCormick Grade I-III increased to 24 (77.4%), while those with McCormick Grade IV-V decreased to 7 (22.6%), and during follow-up, their number further decreased to 2 (6.4%). At the time of admission and discharge, none of the patients had an intact neurological function and normal gait. At follow-up, there were 10 such patients (32.2%) [Table 3].
Table 3:
Degree of neurological deficit measured by the Modified McCormick scale of patients with SMs at admission, discharge, and follow-up.
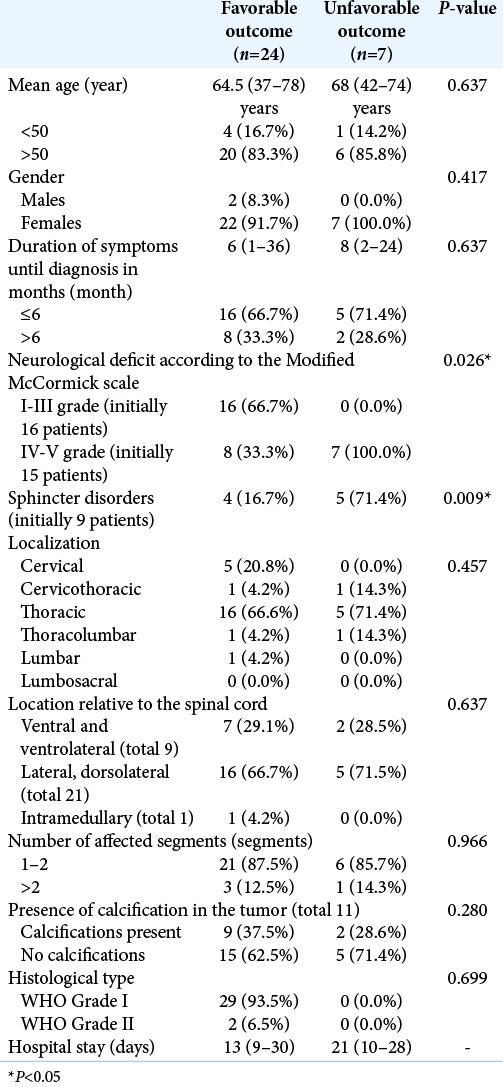
The statistical analysis found that only the degree of preoperative neurological deficit (P = 0.026) and the presence of sphincter disorders (P = 0.009) were significantly correlated to the outcome after treatment [Table 4].
Table 4:
Correlations between the preoperative factors and the treatment outcome in patients with spinal meningiomas.
DISCUSSION
SMs can be found along the entire spine axis, but primarily in the thoracic region and have a frequency of 0.5–2 per 100,000 people per year.[31] Sixty-four percent to 84% of SM are localized in the thoracic region with dorsal, dorsolateral, or lateral location; in 14–27%, they are localized in the cervical region, but with predominant ventral location, and in only 2–14% – in the lumbar region.[33] As seen in [Table 2], our results are consistent with this statement.
SMs with an intradural and extradural spread are observed in 5–6% of cases, while the intramedullary and purely epidural variants are extremely rare.[21,36] In our series, the first variant was observed in two of the cases (7.1%), while the intramedullary localization was found in 1 case (3.6%).
Our series confirms that SMs can be observed in all age groups. Twenty-three of the patients (79.3%) were between the 5th and 7th decade of their life, with 15 (51.7%) of them being older than 65 years. Due to the influence of specific sex hormones in tumorogenesis, meningiomas are much more common in women, with a female-to-male ratio ranging from 4:1 to 10:1.[2] In our series, women with meningiomas were 93.5% or the female-to-male was 14.5:1.
In general, SMs are manifested clinically by symptoms of progressive radiculopathy and/or myelopathy.[21] In 26 (83.9%) of our patients, the disease debuted with low back and/or back pain and gradually progressing motor deficit. According to Kleklamp and Samii, sphincter dysfunction is a late symptom that occurs in 15% to 40% of patients, a fact also observed in 29% of our patients.[13] The time from the onset of complaints to the diagnosis varies from 12 to 24 months, but in the current series, this period averaged 10 months.[23] MRI is the diagnostic tool of choice, with the ability to visualize the localization, size and axial position of the lesion, as well as the presence of concomitant spinal malformations, edema, or syrinx.[21] Typically, SMs in the current series appeared isointense or hypointense on T1 and T2 sequences, and enhanced homogeneously after gadolinium administration. As for others, we also found that the “dural tail sign” was present in about 50% of cases.[21] The presence of calcifications in the tumor elicits “dark” signal on the T2 sequence, but they are better visualized by CT [Figure 4].[3] Due to the extreme rarity of intramedullary meningiomas, their imaging characteristics have not been well studied, but in most cases they are isointense or hypointense on T1 and T2 sequences, with a homogeneous postgadolinium enhancement, as demonstrated here.[27] Meningiomas are subdivided into 15 histological and cytomorphological subtypes, nine of which correspond to WHO Grade I, three to WHO Grade II, and another three to WHO Grade III meningiomas.[16] We confirmed the statement of Tsai et al. that the most common subtype of SM is the psammomatous variant.[34] The treatment of SMs is primarily surgical and aims at radical resection. The surgical access and technique depend on the tumor attachment zone. The most commonly employed approach is the posterior or posterolateral route through one-level laminectomy or hemilaminectomy at one or two levels with lateral expansion if needed to reach ventrally or ventrolaterally located tumors and avoid spinal cord retraction. This standard approach which is used in about 100% of cases.[31] was also utilized by us. According to Pereira et al., total resection of the SM is achieved in 82% to 98% of patients, with low rates of morbidity and mortality.[21] We achieved total resection (Simpson Grades I and II) in 29 patients (93.5%) which was consistent with the results from other reported series.[1,12,25,29,35]
Figure 4:
MRI and CT of a patient with ventrolateral meningioma at the level of T5. (a) Sagittal T1 MRI image – the tumor elicits isointense signal; (b) sagittal T2 MRI image – a central area with a more pronounced hypointense “dark” signal is visualized that is consistent with intratumoral calcification; (c) sagittal T1 MRI image with gadolinium enhancement – lack of accumulation of the contrast in the central calcified area; (d) axial CT – the presence of calcifications is well visible.
While IONM for intramedullary tumors has become a standard in neurosurgical practice, IONM for intradural extramedullary tumors is still under debate.[7] Some authors question the real benefit from the use of IONM during intradural extramedullary tumor resection,[10] while others point that it is a valuable tool that minimizes surgical morbidity, especially in cases with tumors located in the craniovertebral junction or in anterior or anterolateral position and even in cases with tumors adherent to the spinal cord without a clear cleavage plane.[5,11] We applied IONM in only one patient from the current series who harbored intramedullary meningioma. Nevertheless, we favor the use of IONM during resection of intradural extramedullary tumors because of its potential to guarantee safer surgery and better outcomes.
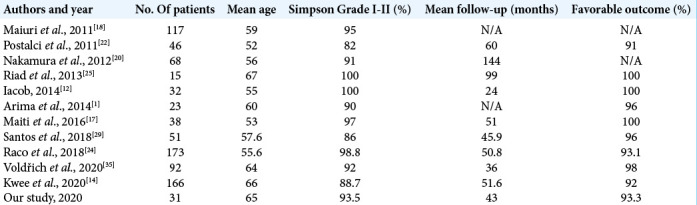
Good or excellent outcome can be achieved in 79% to 98% of cases.[20] Of the 26 patients followed, we achieved a favorable outcome in 93.3% (McCormick I – 38.5%, McCormick II – 19.2%, and McCormick III – 34.6%). A brief overview of results and outcomes of treatment of SMs from the current and other published studies is presented in [Table 5].
Table 5:
Overview of results and outcomes of treatment of spinal meningiomas.
Previous studies have found that factors such as ventral or ventrolateral axial tumor location, large tumor size, T2 cord signal changes, the presence of extensive calcifications, prolonged presentation before diagnosis, WHO grade > I, Simpson resection grade II, or higher can negatively affect the outcome because are associated with an increased risk of long-term morbidity.[9,17,20,24,26]
Despite the retrospective design, a relatively small number of patients and the data that were not statistically analyzed through multivariate analysis, this study found that the outcome of SM treatment was significantly correlated to the degree of the preoperative neurological deficit and the presence of sphincter disorders. A potential discrepancy in the current study is the fact that it demonstrated that more severe preoperative symptoms were associated with the poorer outcome while the length of time with symptoms had no significant effect on outcome.
CONCLUSION
Spinal surgeons should be aware of the insidious natural evolution of SM. Despite being benign lesions, SM can lead to permanent disability if left untreated. The outcome of surgical treatment of SMs is strongly correlated to the severity of the preoperative neurological deficit. Therefore, patients presenting with more severe symptoms are expected to have worse outcomes. However, further prospective studies, which include larger number of patients, are needed to elucidate the identified correlations.
Footnotes
How to cite this article: Davarski A, Kitov B, Apostolov G, Kehayov I, Stoyanova R. Correlations between preoperative clinical factors and treatment outcome of spinal meningiomas – A retrospective study of a series of 31 cases. Surg Neurol Int 2021;12:236.
Contributor Information
Atanas Davarski, Email: atanas.davarski@gmail.com.
Borislav Kitov, Email: borislavkitov@yahoo.com.
Georgi Apostolov, Email: apostolovgeorgi00@gmail.com.
Ivo Kehayov, Email: dr.kehayov@gmail.com.
Rumyana Stoyanova, Email: rumi_stoqnova@abv.bg.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Arima H, Takami T, Yamagata T, Naito K, Abe J, Shimokawa N. Surgical management of spinal meningiomas: A retrospective case analysis based on preoperative surgical grade. Surg Neurol Int. 2014;5(Suppl 7):333–9. doi: 10.4103/2152-7806.139642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bloomer CW, Ackerman A, Bhatia AG. Imaging for spine tumors and new applications. Top Magn Reson Imaging. 2006;17:69–87. doi: 10.1097/RMR.0b013e31802bb38f. [DOI] [PubMed] [Google Scholar]
- 3.Caroli E, Acqui M, Roperto R, Ferrante L, D’Andrea G. Spinal en plaque meningiomas: a contemporary experience. Neurosurgery. 2004;55:1275–9. doi: 10.1227/01.neu.0000143611.28034.b2. [DOI] [PubMed] [Google Scholar]
- 4.Cheng C, Wang J, Zhao S, Tao B, Bai S, Shang A. Intramedullary thoracic meningioma: A rare case report and review of the literature. World Neurosurg. 2019;129:176–80. doi: 10.1016/j.wneu.2019.05.172. [DOI] [PubMed] [Google Scholar]
- 5.Cofano F, Giambra C, Costa P, Zeppa P, Bianconi A, Mammi M, et al. Management of extramedullary intradural spinal tumors: The impact of clinical status, intraoperative neurophysiological monitoring and surgical approach on outcomes in a 12-year double-center experience. Front Neurol. 2020;11:598619. doi: 10.3389/fneur.2020.598619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gezen F, Kahraman S, Canakci Z, Beduk A. Review of 36 cases of spinal cord meningioma. Spine. 2000;25:727–31. doi: 10.1097/00007632-200003150-00013. [DOI] [PubMed] [Google Scholar]
- 7.Ghadirpour R, Nasi D, Iaccarino C, Giraldi D, Sabadini R, Motti L, et al. Intraoperative neurophysiological monitoring for intradural extramedullary tumors: Why not? Clin Neurol Neurosurg. 2015;130:140–9. doi: 10.1016/j.clineuro.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 8.Ghaffari-Rafi A, Mehdizadeh R, Ghaffari-Rafi S, Leon-Rojas J. Demographic and socioeconomic disparities of benign and malignant spinal meningiomas in the United States. Neurochirurgie. 2021;67:112–8. doi: 10.1016/j.neuchi.2020.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Gilard V, Goia A, Ferracci FX, Marguet F, Magne N, Langlois O, et al. Spinal meningioma and factors predictive of post-operative deterioration. J Neurooncol. 2018;140:49–54. doi: 10.1007/s11060-018-2929-y. [DOI] [PubMed] [Google Scholar]
- 10.Harel R, Schleifer D, Appel S, Attia M, Cohen ZR, Knoller N. Spinal intradural extramedullary tumors: The value of intraoperative neurophysiologic monitoring on surgical outcome. Neurosurg Rev. 2017;40:613–9. doi: 10.1007/s10143-017-0815-2. [DOI] [PubMed] [Google Scholar]
- 11.Hohenberger C, Gugg C, Schmidt NO, Zeman F, Schebesch KM. Functional outcome after surgical treatment of spinal meningioma. J Clin Neurosci. 2020;77:62–6. doi: 10.1016/j.jocn.2020.05.042. [DOI] [PubMed] [Google Scholar]
- 12.Iacob G. Spinal meningiomas. Personal experience and review of literature. Rom Neurosurg. 2014;21:146–60. [Google Scholar]
- 13.Kleklamp J, Samii M. Surgery of Spinal Tumors. 1st ed. Berlin, Heidelberg: Springer-Verlag; 2007. Extramedullary tumors; pp. 248–60. [Google Scholar]
- 14.Kwee LE, Harhangi BS, Ponne GA, Kros JM, Dirven CM, Dammers R. Spinal meningiomas: Treatment outcome and long-term follow-up. Clin Neurol Neurosurg. 2020;198:106238. doi: 10.1016/j.clineuro.2020.106238. [DOI] [PubMed] [Google Scholar]
- 15.Levy WJ, Jr, Bay J, Dohn D. Spinal cord meningioma. J Neurosurg. 1982;57:804–12. doi: 10.3171/jns.1982.57.6.0804. [DOI] [PubMed] [Google Scholar]
- 16.Louis DN, Perry A, Reifenberger G, von Deimling A, FigarellaBranger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: A summary. Acta Neuropathol. 2016;131:803–20. doi: 10.1007/s00401-016-1545-1. [DOI] [PubMed] [Google Scholar]
- 17.Maiti TK, Bir SC, Patra DP, Kalakoti P, Guthikonda B, Nanda A. Spinal meningiomas: clinicoradiological factors predicting recurrence and functional outcome. Neurosurg Focus. 2016;41:E6. doi: 10.3171/2016.5.FOCUS16163. [DOI] [PubMed] [Google Scholar]
- 18.Maiuri F, De Caro ML, de Divitiis O, Vergara P, Mariniello G. Spinal meningiomas: Age-related features. Clin Neurol Neurosurg. 2011;113:34–8. doi: 10.1016/j.clineuro.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 19.McCormick PC, Post KD, Stein BM. Intradural extramedullary tumors in adults. Neurosurg Clin N Am. 1990;1:591–608. [PubMed] [Google Scholar]
- 20.Nakamura M, Tsuji O, Fujiyoshi K, Hosogane N, Watanabe K, Tsuji T, et al. Long-term surgical outcomes of spinal meningiomas. Spine (Phila Pa 1976) 2012;37:E617–23. doi: 10.1097/BRS.0b013e31824167f1. [DOI] [PubMed] [Google Scholar]
- 21.Pereira CU, Dias LA, Dezena RA. Spinal Meningiomas: Report of 14 cases and literature review. J Bras Neurocirurg. 2015;26:110–5. [Google Scholar]
- 22.Postalci L, Tugcu B, Gungor A, Guclu G. Spinal meningiomas: Recurrence in ventrally located individuals on long-term follow-up; a review of 46 operated cases. Turk Neurosurg. 2011;21:449–53. [PubMed] [Google Scholar]
- 23.Raco A, Pesce A, Miscusi M. Surgical treatment of spinal meningiomas. In: Signorelli F, editor. From Bench to Bedside Trauma, Tumors, Spine, Functional Neurosurgery. London: InTechOpen; 2016. pp. 99–110. [Google Scholar]
- 24.Raco A, Pesce A, Toccaceli G, Domenicucci M, Miscusi M, Delfini R. Factors leading to a poor functional outcome in spinal meningioma surgery: Remarks on 173 cases. Neurosurgery. 2018;80:602–9. doi: 10.1093/neuros/nyw092. [DOI] [PubMed] [Google Scholar]
- 25.Riad H, Knafo S, Segnarbieux F, Lonjon N. Spinal meningiomas: Surgical outcome and literature review. Neurochirurgie. 2013;59:30–4. doi: 10.1016/j.neuchi.2012.10.137. [DOI] [PubMed] [Google Scholar]
- 26.Ruggeri AG, Fazzolari B, Colistra D, Cappelletti M, Marotta N, Delfini R. Calcified spinal meningiomas. World Neurosurg. 2017;102:406–12. doi: 10.1016/j.wneu.2017.03.045. [DOI] [PubMed] [Google Scholar]
- 27.Sahni D, Harrop JS, Kalfas IH, Vaccaro AR, Weingarten D. Exophytic intramedullary meningioma of the cervical spinal cord. J Clin Neurosci. 2008;15:1176–9. doi: 10.1016/j.jocn.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 28.Sandalcioglu IE, Hunold A, Muller O, Stolke D, Asgari S. Spinal meningiomas: Critical review of 131 surgically treated patients. Eur Spine J. 2008;17:1035–41. doi: 10.1007/s00586-008-0685-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Santos RC, de Amoreira Gepp R. Benefits of spinal meningioma resection. Surg Neurol Int. 2019;9:16. doi: 10.4103/sni.sni_409_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schwarts TH, McCormick PC. Spinal cord tumors in adults. In: Winn HR, editor. Youmans Neurological Surgery. Vol. 4. Philadelphia, PA: Saunders; 2004. pp. 4817–34. [Google Scholar]
- 31.Setzer M, Vatter H, Marquardt G, Seifert V, Vrionis FD. Management of spinal meningiomas: surgical results and a review of the literature. Neurosurg Focus. 2007;23:E14. doi: 10.3171/FOC-07/10/E14. [DOI] [PubMed] [Google Scholar]
- 32.Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatr. 1957;20:22–39. doi: 10.1136/jnnp.20.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Traul DE, Shaffrey ME, Schiff D. Part I: Spinal-cord neoplasms intradural neoplasms. Lancet Oncol. 2007;8:35–45. doi: 10.1016/S1470-2045(06)71009-9. [DOI] [PubMed] [Google Scholar]
- 34.Tsai EC, Butler J, Benzel EC. Spinal meningiomas. In: Lee JH, editor. Meningiomas. London: Springer; 2009. pp. 529–39. [Google Scholar]
- 35.Voldřich R, Netuka D, Beneš V. Spinal meningiomas: Is Simpson grade II resection radical enough? Acta Neurochir. 2020;162:1401–8. doi: 10.1007/s00701-020-04280-2. [DOI] [PubMed] [Google Scholar]
- 36.Yuan D, Liu D, Yuan XR, Xi J, Ding X. Intramedullary thoracic spinal cord meningioma: A rare case report and review of the literature. J Neurol Surg A Cent Eur Neurosurg. 2013;74(Suppl 1):e136–9. doi: 10.1055/s-0032-1330959. [DOI] [PubMed] [Google Scholar]