Abstract
Aims
To conduct a systematic literature review to identify recent epidemiological, biomarker, genetic and clinical evidence that expands our understanding of nonalcoholic fatty liver disease (NAFLD) as a metabolic disorder.
Materials and Methods
We performed a literature search using PubMed to identify trials, observational studies and meta‐analyses published in the past 5 years.
Results
A total of 95 publications met prespecified inclusion criteria and reported on the interplay between NAFLD/nonalcoholic steatohepatitis (NASH) and metabolic dysfunction, in terms of disease burden and/or epidemiology (n = 10), pathophysiology, risk factors and associated conditions (n = 29), diagnosis and biomarkers (n = 34), and treatment approaches (n = 22). There is a growing body of evidence on the links between NAFLD/NASH pathogenesis and mechanisms of metabolic dysfunction, through liver lipid accumulation, insulin resistance, inflammation, apoptosis, and fibrogenic remodelling within the liver. The frequent co‐occurrence of NAFLD with obesity, metabolic syndrome and type 2 diabetes supports this premise. Therapeutic approaches originally envisaged for type 2 diabetes or obesity (such as glucagon‐like peptide‐1 receptor agonists, sodium‐glucose co‐transporter‐2 inhibitors, insulin sensitizers and bariatric surgery) have shown promising signs of benefit for patients with NAFLD/NASH.
Conclusions
Given the complex interplay between NAFLD and metabolic dysfunction, there is an urgent need for multidisciplinary collaboration and established protocols for care of patients with NAFLD that are individualized and ideally support reduction of overall metabolic risk as well as treatment for NASH.
Keywords: fatty liver disease, GLP‐1, insulin resistance, pharmaco‐epidemiology, type 2 diabetes
1. INTRODUCTION
Nonalcoholic fatty liver disease (NAFLD) is a chronic and increasingly common liver disorder among adults in Western countries. 1 , 2 NAFLD encompasses a heterogeneous spectrum of disease, but is histologically categorized into nonalcoholic fatty liver, characterized as ≥5% liver steatosis with no evidence of injury to hepatocytes and no evidence of fibrosis, 1 and nonalcoholic steatohepatitis (NASH), 1 , 2 defined as ≥5% liver steatosis including inflammation and injury to hepatocytes with or without fibrosis, although fibrosis is typically observed. 1 , 2 , 3 NASH is associated with increased risk of cirrhosis, hepatocellular carcinoma (HCC), and liver‐related mortality, especially when fibrosis is present. 1 , 2 , 3 Advancing fibrosis stage exponentially increases the risk of liver‐related mortality. 4
Diagnosis of NAFLD requires detection of liver steatosis, exclusion of other liver diseases, and absence of alcoholic causes. 5 NAFLD is often identified by abdominal ultrasonography during routine health checks, and ultrasonography is an acceptable screening procedure for steatosis. 5 However, liver biopsies remain the only definitive technique to determine and then monitor the stage and severity of NAFLD. 6 Biopsies are invasive, costly, and allow for considerable sampling error 5 , 6 ; thus, noninvasive diagnostic and staging methods are under continued investigation. Vibration‐controlled one‐dimensional transient elastography, also known as Fibroscan®, provides a liver stiffness measurement and controlled attenuation parameter, which can indicate the level of liver fibrosis and steatosis, respectively. 7 This method is considered an effective noninvasive procedure for NAFLD screening. 7 Development of the XL probe has also improved Fibroscan® reliability in patients with obesity. 7 The commercial biomarker panels SteatoTest, ActiTest, NashTest‐2 and FibroTest have been validated for diagnosis of NAFLD, NASH and/or fibrosis; however, the validation cohorts only included a minority of patients with type 2 diabetes mellitus (T2DM). 8 All panels were found to underperform in a population of patients with T2DM, suggesting that studies in nondiabetic populations should not be directly extrapolated to patients with T2DM. 8 Other proposed methods for detecting and assessing fibrosis stage in patients with NAFLD include various biomarkers and composite scores of clinical assessments such as NAFLD fibrosis score, fibrosis‐4 index and the aspartate transaminase (AST) to platelet ratio index; studies assessing these have found varying performance. 9 , 10 , 11 The National Institute for Health and Care Excellence has recommended the Enhanced Liver Fibrosis score for assessing advanced fibrosis in NAFLD. 12 Noninvasive imaging methods, such as magnetic resonance imaging‐derived proton density fat fraction and magnetic resonance elastography (MRE), have been suggested for liver fat and fibrosis detection, respectively. 13 , 14 Recently, combining liver stiffness measurement and controlled attenuation parameter by Fibroscan® with AST level, known as FibroScan‐AST (FAST), demonstrated good performance in identifying patients at risk of progressive NASH (NASH with NAFLD Activity Score ≥4 and fibrosis stage ≥2). 15 The positive predictive value for FAST was 83% in the prospective UK derivation cohort, and 69% in the pooled global validation cohorts. 15 The MRE combined with FIB‐4 (MEFIB) index (MRE ≥3.3 kPa and FIB‐4 ≥1.6) demonstrated positive predictive values of 97% and 91% for detection of fibrosis stage ≥2 in the University of California at San Diego derivation cohort and Japan validation cohort, respectively. 16
Accumulating evidence supports a bidirectional association between NAFLD and components of metabolic syndrome (MetS). 1 , 17 , 18 NAFLD is accompanied by a number of pathophysiological changes: (i) increased de novo lipogenesis (DNL) and very low‐density lipoprotein production; (ii) reduced hepatic fatty acid oxidation; (iii) unrestrained lipolysis in adipose tissue; and (iv) impaired insulin‐mediated suppression of hepatic glucose production, leading to liver steatosis, hypertriglyceridaemia, and hyperglycaemia. 19 , 20 At the molecular level, selective hepatic insulin resistance (IR) is thought to be a common factor driving these processes, resulting in development of both hepatic and peripheral metabolic dysfunction. 21
The prevalence and incidence of IR, obesity, T2DM and NAFLD are also closely linked. 22 NAFLD and T2DM share multiple cardiometabolic risk factors and proinflammatory and profibrotic pathways. 23 The prevalence of comorbid conditions with NASH has been reported in a meta‐analysis to be 82% for obesity, 72% for hyperlipidaemia, 71% for MetS (various definitions were included), 68% for hypertension, and 44% for T2DM. 17 Patients with T2DM frequently also have NAFLD and have a higher risk of developing NASH, suggesting there is a bidirectional interplay of risk factors between NAFLD and T2DM. 24
While NAFLD was formally described over 40 years ago, it is only in recent years that NAFLD has become recognized as an urgent unmet medical need, and an appropriate histological classification, regulatory pathway and clinical endpoints have been in place to enable effective clinical research and drug development. 25 As yet there are no approved treatments for NAFLD or NASH, but a consensus workshop between the American Association for Study of Liver Diseases and the US Food and Drug Administration (FDA), published in 2015, established a framework for critical components of the drug development process enabling more rapid progress. 26 This literature review focuses on the current evidence supporting NAFLD as a metabolic disease and part of a process of systemic metabolic dysfunction, the efforts to establish noninvasive diagnostic techniques, particularly in patients with NAFLD and T2DM or obesity, and the current evidence supporting pharmacological therapies under investigation for NAFLD or NASH that target metabolic dysfunction.
2. METHODS
The objective of the literature review was to identify evidence that advances the understanding of NAFLD, including NASH, and its relationships with components of MetS, with a focus on the most recent evidence generated in the past 5 years.
2.1. Search strategy
A literature search of the PubMed electronic database was conducted on 16 November 2020 to identify clinical studies, clinical trials, comparative studies, controlled clinical trials, meta‐analyses, observational studies and randomized controlled trials, restricted to human participants only and in English language, published from January 2014. The full search strategy is presented in the Supplementary Appendix S1. Articles outside of the PubMed search were also included, if relevant.
2.2. Study selection
Articles were included in the full‐text review if they reported on disease burden, epidemiology, association with metabolic abnormalities or other diseases (eg, cancer), pathophysiology, diagnosing methods, and treatment and management of NAFLD or NASH.
3. RESULTS
A total of 168 articles and abstracts underwent full‐text review from the PubMed search (Figure 1). After removal of 73 ineligible articles, there remained 95 articles that met the criteria for inclusion in this review (Table S1), and 84 are further discussed. Selected articles (Figure 1) were categorized according to the type of data they reported, as follows: disease burden and/or epidemiology (10 references); the interplay with metabolic abnormalities and/or relationships with other diseases (29 references); diagnosis and biomarkers (34 references); and treatment (22 references).
FIGURE 1.
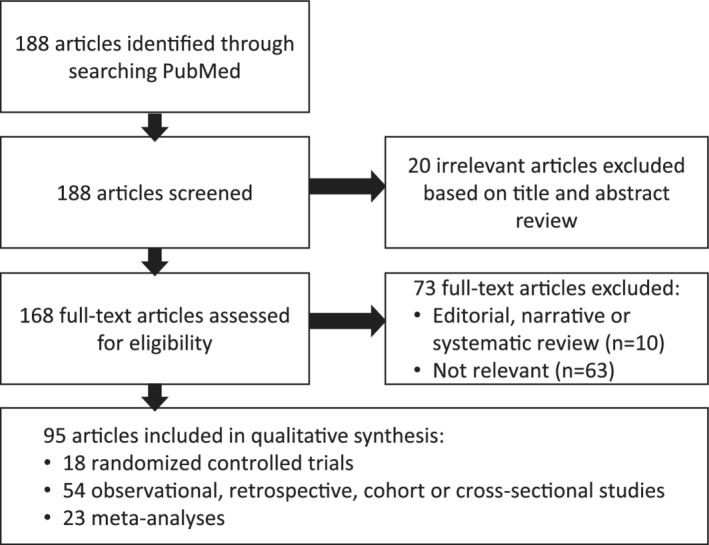
Diagram of included and excluded publications
3.1. Global burden of NAFLD and NASH
The prevalence of NAFLD has grown consistently over the last three decades in the United States, in line with similar increases in the prevalence of obesity and T2DM. 27 Seven of the retrieved studies reported on the burden of NAFLD in the context of metabolic abnormalities. A cross‐sectional analysis of 1948 adults in China identified a prevalence of NAFLD of 35.5% during general health checks. 28 A large, well‐designed meta‐analysis of 24 studies including 35 599 patients with T2DM reported a pooled prevalence of NAFLD of 59.7%. 29 This finding is consistent with the prevalence of NAFLD in three recent observational studies in populations with metabolic risk factors: 65.7% in South Indian patients with morbid obesity undergoing bariatric surgery (of which 33.6% had histological features of NASH), 30 64.5% in premenopausal women who have overweight/obesity from Greece, 31 and 64.7% in patients with T2DM from Bangladesh. 32 Parameters of metabolic dysfunction (including body mass index [BMI], waist‐hip ratio, glycated haemoglobin [HbA1c], fasting plasma glucose, low‐density lipoprotein [LDL] cholesterol, triglycerides, total cholesterol, and hypertension) were consistently found to be significantly associated with an increased prevalence of NAFLD across the studies identified. 28 , 29 , 30 , 31 , 32 , 33 , 34 The 34 retrieved studies related to the diagnosis and monitoring of NAFLD and NASH are discussed in the Supplementary Appendix S1.
3.2. Metabolic risk factors and the pathophysiology of NAFLD
The current view of NAFLD pathogenesis encompasses abnormal lipid metabolism, apoptosis, hepatic inflammation, and fibrogenic remodelling in the liver and has been an active area of research in recent years (Figure 2).
FIGURE 2.

Potential mechanisms by which nonalcoholic steatohepatitis (NASH) causes hepatic and extrahepatic metabolic dysfunction and current metabolic therapeutic targets. Acetyl‐CoA, acetyl co‐enzyme A; GLP‐1, glucagon‐like peptide‐1; HR, hormone receptor; NAFLD, non‐alcoholic fatty liver disease; PPAR, peroxisome proliferator‐activated receptor; SGLT2, sodium‐glucose co‐transporter‐2; T2DM, type 2 diabetes mellitus
3.2.1. Metabolic dysfunction
A number of meta‐analyses carried out in the past 5 years have evaluated the interplay between metabolic diseases and NAFLD, and what is now understood to be a “vicious cycle” between NAFLD and T2DM, in which NAFLD increases the risk of incident T2DM and then T2DM increases the risk of liver fibrosis. Many of the publications identified reinforce the association of NAFLD with components of MetS and IR first reported 20 years ago, 35 , 36 although few studies evaluated longitudinal changes in liver histology.
Large meta‐analyses consistently demonstrate that patients with NAFLD have a significant risk of T2DM and MetS. 37 , 38 Currently it is uncertain whether the incidence of T2DM increases with worsening severity of liver disease in NAFLD. An updated meta‐analysis that incorporated a total of 19 observational studies in nearly 296 500 individuals (30% with NAFLD diagnosed via imaging) and captured nearly 16 000 cases of incident T2DM over a median follow‐up of 5 years concluded that NAFLD was associated with an approximate doubling of risk of T2DM (random‐effects hazard ratio 2.22, 95% confidence interval [CI] 1.84‐2.60). 23 In this study, risk of T2DM appeared to increase further with greater severity of NAFLD in the four eligible studies that used either noninvasive fibrosis scores or ultrasonographic severity of steatosis. In a cohort study of 12 853 South Koreans a significantly increased risk of incident T2DM at 5‐year follow‐up was reported among patients with baseline fatty liver on ultrasonography (odds ratio 2.42, 95% CI 1.74‐3.36; P <0.0001), even after adjustment for established risk factors. 39 There is also some evidence of worsening metabolic dysfunction with increasing severity of NAFLD in patients with MetS. 40 The IT‐DIAB observational study in patients with prediabetes found that the Fatty Liver Index (a proxy of liver steatosis comprising triglycerides, gamma glutamyl‐transferase [GGT], BMI, and waist circumference) was associated with new‐onset diabetes independent of age, gender, diabetes risk score, HbA1c, and fasting plasma glucose. 41 Besides T2DM, patients with obesity also have an increased risk of NAFLD. 42 , 43 Finally, it should be noted that NAFLD can occur in lean individuals, especially in Asian populations, who display increased visceral adipose tissue and IR at lower BMI thresholds (see below). 44
On the other side of the coin, several studies have demonstrated that metabolic diseases, especially T2DM, are independent factors of the severity of NAFLD. A recent prospective cohort study designed to reflect the full spectrum of disease and overcome potential lead time bias by including patients with NAFLD, borderline NASH and definite NASH has provided insights into liver histology over a mean of 4.9 years between biopsies, reporting that MetS was significantly associated with progression to advanced fibrosis (P = 0.03). 45 Moreover, T2DM is an independent risk factor for severe steatosis (relative risk 2.04, 95% CI 1.10‐3.76; P = 0.023) and severe fibrosis (relative risk 4.57, 95% CI 1.37‐15.20; P = 0.013) compared with patients without T2DM. 46 A meta‐analysis found that T2DM was associated with a more than twofold increased risk of incident severe liver disease events in the general population at risk of NAFLD or with diagnosed NAFLD (adjusted hazard ratio 2.25, 95% CI 1.83‐2.76; P <0.001). 47 In the same study, obesity as defined by BMI alone had a less marked association with increased risk of incident severe liver disease outcomes (adjusted hazard ratio 1.20, 95% CI 1.12‐1.28; P <0.001). 47 A separate meta‐analysis found that BMI‐defined obesity was significantly associated with liver fibrosis in patients with NAFLD (odds ratio 3.22, 95% CI 2.13‐4.87; P <0.001), but not necessarily with advanced fibrosis. 48
In light of the association between NAFLD and metabolic disorders, an international panel of experts proposed that defining fatty liver disease based on the presence or absence of metabolic dysfunction, independent of alcohol consumption, may be more relevant to the condition. 49 Metabolic dysfunction‐associated fatty liver disease (MAFLD) has been suggested as an alternative term to better represent patient heterogeneity, 49 , 50 and to account for the possibility of coexisting liver diseases which may be associated with alcohol consumption. 49 It is also suggested that a higher alcohol intake threshold should be considered when enrolling patients into clinical trials, to address the current difficulties faced in patient recruitment. 49 The proposed key diagnostic criteria for MAFLD comprise hepatic steatosis together with at least one of the following: overweight/obesity; T2DM; or two or more metabolic risk abnormalities. 49 The presence of metabolic risk factors in the absence of overweight/obesity enables diagnosis of MAFLD in the nonobese or lean population.
A recent meta‐analysis confirmed that BMI should not be a mandatory criterion for MAFLD/NAFLD diagnosis, with approximately 40% of global NAFLD cases classified as nonobese and approximately 20% as lean. 51 Obese and lean NAFLD share many pathophysiological characteristics. For example, some individual components of MetS, such as high blood pressure, plasma glucose levels and serum triglycerides, appear to be similar between patients with obese or lean NAFLD, although MetS overall is more prevalent in obese cases. 52 The frequency of NASH and stage ≥2 fibrosis in nonobese NAFLD is 40% and 30%, respectively, 51 and neither appear to correlate with obesity. 48 However, obese NAFLD may predict worse long‐term prognosis due to higher transaminase levels, a higher degree of hepatic steatosis, and increased risk of metabolic complications and fibrosis, relative to nonobese NAFLD. 48 Lean NAFLD appears to be more common in Asian populations and possible predisposing factors include visceral adiposity, fructose‐ and cholesterol‐rich diets, and genetic components. 44 , 53 Indeed, presence of the G allele of PNPLA3 rs738409 appears to be more frequent in nonobese NAFLD than in obese cases. 48 Evidence for effective pharmacological treatment approaches in lean NAFLD is lacking 44 and inclusion of lean NAFLD individuals in clinical trials for pharmacological treatment of NAFLD is recommended. 48 , 51 In terms of current disease management, similar approaches to those taken for NAFLD patients with obesity are suggested, such as weight loss in those individuals with visceral obesity and dietary restrictions (also see below). 44 , 53
3.2.2. Pathological mechanisms
Multiple parallel events are thought to lead to the pathogenesis of NAFLD, starting with accumulation of fatty acids and triglycerides and development of IR both in the liver and in adipose and skeletal muscle. Through a combination of multiple‐stable‐isotope analysis and liver biopsies, sources of intrahepatic triglycerides have been attributed mainly to circulating fatty acids (approximately 59%), DNL (approximately 26%) and dietary fatty acids (approximately 15%) in NAFLD. 54 , 55 DNL is estimated to be threefold higher in NAFLD compared with controls, whereas the production of fatty acids from adipose tissue has not been found to be significantly different. 55 It has been proposed that all individuals may have a genetic and environmentally determined limit to their capacity for adipose tissue expansion and that, once this is reached, lipids accumulate in other tissues, and this promotes IR and inflammation both within and outside of the liver in a process known as lipotoxicity. 56 A cross‐sectional study in 137 normoglycaemic participants from Mexico reported that disruption in regulation of acylcarnitines and amino acids predicts development of inflammation, obesity, NAFLD, and IR. 57 IR is thought to exacerbate lipotoxicity through stimulation of lipolysis in adipose tissue and a process of positive feedback that escalates the metabolic imbalance, for example, through accumulation of ceramides, long‐chain acylcarnitines and diacylglycerols (DAGs) that promote inflammation and impact further on insulin signalling. 58 , 59 Adipose tissue macrophages are thought to be key contributors to IR and impaired adipose tissue function. 60 Increased fatty acid levels activate toll‐like receptor 4 (TLR4) signalling in adipose tissue macrophages, resulting in polarization from an anti‐inflammatory M2 state into the proinflammatory M1 phenotype. 61 M1 macrophages produce the cytokines tumour necrosis factor‐α and interleukin (IL)‐6, both of which are associated with development of IR. 62 Adipose tissue hypertrophy can result in reduced oxygen supply to the tissue; hypoxia has also been implicated in the infiltration of adipose tissue by M1 macrophages and as a potential mechanism of IR. 60 , 62 Insights into the relationship between metabolic dysfunction and NAFLD from genome‐wide analyses in recent years are discussed in the Supplementary Appendix S1.
3.2.3. Inflammation, oxidative and endoplasmic reticulum stress, and apoptosis
Insulin resistance and lipid accumulation in the liver trigger a cascade of mitochondrial dysfunction and activation of cytochrome p450 2E1‐mediated lipid peroxidation that generates reactive oxygen species and degrades mitochondria and other hepatocellular structures. 63 Mitochondrial damage decreases cellular energy production and increases accumulation of metabolic intermediates, which adds to the stress on endoplasmic reticulum caused by excess free cholesterol. These processes lead to release of proinflammatory cytokines, hepatocellular injury, apoptosis and fibrogenesis, which can ultimately progress to fibrosis and cirrhosis. 63 Several studies have assessed the key putative mechanisms responsible for hepatic IR and hepatic lipid accumulation. Hepatic lipid accumulation has been implicated in the development of IR, but translational evidence in humans is limited. 64 Intracellular lipid metabolites, such as DAG, ceramides and acylcarnitines, are claimed to be involved in the pathogenesis of IR in skeletal muscle. 65 The severity of liver cell injury and degree of NAFLD activity are also thought to contribute to hepatic IR independent of the amount of intrahepatic triglycerides and lipid intermediates. 65 Studies have consistently shown the key role of hepatocellular DAG and protein kinase Cε (PKCε) activation in the pathogenesis of IR in humans. 64 , 65 , 66 DAG in hepatic cytosol has been shown to be a predictor for insulin inhibition of glucose production, and DAG‐associated IR is characterized by PKCε translocation. 64 , 65 , 66 In a study of the human liver lipidome in 125 liver biopsy samples, PNPLA3 I148M variant allele carriers had significantly higher liver fat content and no features of IR (as determined from homeostatic model assessment of IR [HOMA‐IR], serum lipids and adiponectin concentrations), compared with noncarriers. 67 IR in the human liver is associated with increased concentrations of saturated and monounsaturated free fatty acids and triacylglycerols (TAGs) as well as ceramides from the de novo ceramide synthetic pathway. 67 This is not observed in NAFLD with the PNPLA3 I148M variant, which instead is characterized by increased concentrations of polyunsaturated TAGs that can be attributed to known functions of the I148M variant in in vitro studies. 67
Several identified studies highlighted the relationship between inflammation and NAFLD. 68 , 69 , 70 In a cross‐sectional analysis, patients with NAFLD had significantly lower circulating levels of anti‐inflammatory mediators such as adiponectin, endogenous soluble receptor for advanced glycation end products, and IL‐10, and high concentrations of proinflammatory oxidized LDL, CD40 ligand, and endogenous thrombin potential compared with patients without NAFLD, suggesting that the inflammation may be accelerated by the presence of MetS. 68 Leukocyte cell‐derived chemotaxin‐2 (LECT2) has been identified as a secretory protein that modulates inflammatory responses, but is also implicated as playing a key role in IR. 71 Significantly higher plasma levels of LECT2 were found in patients with NAFLD versus those without, and were associated with obesity, lipid profile and high‐sensitivity C‐reactive protein (hsCRP) in individuals with MetS.
It is thought that sublethal lipid‐induced hepatocyte stress and dysfunction is able to trigger proinflammatory cascades through the generation of undead hepatocytes (which includes ballooned hepatocytes and hepatocytes with Mallory‐Denk bodies' inclusions) and extracellular vesicle release. 72 This generates a feed‐forward loop, intensifying hepatocyte injury and maintaining a proinflammatory microenvironment within the liver. 72 Decreased liver fat and heat shock factor 1 may impair heat shock protein−70‐dependent anti‐inflammation, further exacerbating inflammation leading to oxidative stress during progression of the disease. 70 Adipose tissue secretes regulatory proteins known as adipokines that may play a role in development of MetS and NASH through involvement in the hepatic and systemic inflammatory response and in IR. Patients with NAFLD have decreased levels of circulating anti‐inflammatory adipokine adiponectin 73 and underexpression of adiponectin receptors in visceral fat, while overexpression of adiponectin receptors in the liver appears to be associated with the degree of liver damage. 74 A systematic review assessed the relationship between novel adipokines and liver histology in patients with NAFLD, including 31 cross‐sectional studies evaluating seven adipokines. 75 Chemerin, resistin, and adipocyte‐fatty‐acid‐binding protein (also known as FABP‐4) were identified as potentially being involved in NAFLD pathogenesis and/or progression, warranting further evaluation.
Inflammasomes are large multiprotein complexes that promote or sustain inflammation, and intriguing evidence in a mouse model of NASH suggests that saturated fatty acids can upregulate the inflammasome in hepatocytes. 76 Elevated serum uric acid (UA), an end product of purine metabolism, is a feature of inflammasome activation that has been observed in MetS and cardiovascular (CV) disease. The associations between UA, components of MetS, obesity and NAFLD were assessed in a cross‐sectional study in 10 069 Chinese participants. 77 The prevalence of NAFLD was significantly higher among individuals with elevated UA across subgroups of patients with BMI <25 and ≥25 kg/m2, and there was a strong additive interaction between obesity and elevated UA to increase the risk of NAFLD. 77
3.2.4. Impact on CV disease
As T2DM occurs very frequently with NAFLD, and T2DM is an established risk factor, it has been uncertain until recently whether the presence of co‐existing T2DM confounds the relationship between NAFLD and CV disease. Wild et al 78 recently performed a retrospective cohort analysis using linked population‐based routine data for people aged 40 to 89 years diagnosed with T2DM in Scotland between 2004 and 2013 who had one or more hospital admission records. Adjusted hazard ratios for NAFLD versus no record of liver disease were 1.70 (95% CI 1.52‐1.90) for CV disease and 1.60 (95% CI 1.40‐1.83) for all‐cause mortality. Moreover, a recent meta‐analysis showed that NAFLD was independently associated with a higher incidence of CV disease in patients with T2DM, 79 providing evidence that T2DM is unlikely to confound the relationship between NAFLD and CV disease, as a similar strength of relationship between NAFLD and CV disease exists in patients both with and without T2DM. Another meta‐analysis found a significant association between presence of NAFLD and diastolic cardiac dysfunction, suggesting the need for careful observation for CV comorbidities in patients with NAFLD. 80 The risk of atrial fibrillation (AF) has been found to be doubled in cross‐sectional studies of patients with NAFLD, independent of other risk factors for AF; this risk was elevated even further in those with T2DM. 81 It has been suggested that the relationship between NAFLD and AF is likely attributable to shared risk factors and pathological mechanisms such as obesity, activation of the renin‐angiotensin system and proinflammatory and oxidative states. 82 A causal relationship between the two, however, has not been confirmed. 81 , 82 In a retrospective analysis of the longitudinal CARDIA cohort, NAFLD was shown to correlate with subclinical myocardial remodelling and dysfunction, resulting in left ventricular stiffness that was independent of established risk factors for heart failure, suggesting common pathophysiological links perhaps via IR, systemic inflammation, and/or myocardial lipotoxicity. 83 In a prospective observational study, NAFLD was significantly correlated with systemic markers of inflammation and higher all‐cause mortality in patients with heart failure with preserved ejection fraction. 84 Another study found that NAFLD incidence was significantly higher among patients with versus those without coronary artery disease (P = 0.013), and greater degrees of liver steatosis were observed in patients with Grade 3 versus those with Grade 0 to 1 coronary artery disease (P = 0.038). 85 However, a cohort study including 30 239 participants in the United States reported no clear association between NAFLD and risk of ischaemic stroke, suggesting that although the risk factors for stroke, atherosclerosis, and coronary disease are similar, the role of liver inflammation across the spectrum of atherosclerotic CV diseases remains to be clarified. 86
3.2.5. Impact on oncogenesis
Nonalcoholic fatty liver disease is associated with an elevated risk of HCC, colorectal adenoma and colorectal cancer, with the risk increasing with NAFLD severity, potentially as a result of excess advanced glycation end products and proinflammatory cytokines that can elicit oxidative stress and hepatic stellate cell activation. 87 A retrospective, long‐term analysis of outcomes in Japanese patients with NAFLD found that incidences of HCC and both liver and nonliver‐related mortality were increased in individuals with advanced fibrosis compared with those with mild fibrosis. 88 In a meta‐analysis of 21 observational studies, NAFLD was associated with increased risk of incident colorectal adenoma/colorectal cancer, while severe NAFLD also elevated the risk of incident colorectal adenoma/colorectal cancer compared with mild and/or moderate NAFLD. 87 A cohort study in 1793 participants from China reported that NAFLD and MetS were independently associated with elevated risk of colorectal neoplasm (P = 0.001 and P = 0.001, respectively) and colorectal cancer (P = 0.005 and P = 0.001, respectively), and the authors suggested that patients with NAFLD and MetS should undergo regular colonoscopy assessments. 89 Another meta‐analysis found that NAFLD may elevate the risk of developing cholangiocarcinoma, particularly intrahepatic cholangiocarcinoma. 90 Finally, a meta‐analysis of 19 studies including 168 571 participants without cirrhosis reported that patients with NASH have a higher risk of developing HCC compared with patients with other aetiologies of liver diseases. 91
3.3. Managing NAFLD and NASH by treating liver disease and targeting metabolic risk: Current and emerging strategies
Lifestyle modification consisting of diet, exercise and weight loss is advocated for patients with NAFLD. 1 , 92 , 93 Assessment of dietary and physical activity habits is part of comprehensive NAFLD screening 2 ; however, no recommendations exist on any particular type of diet or intensity, volume and type of exercise required. 1 , 92 , 93 Exercise may independently improve hepatic steatosis without weight loss, but weight loss is usually required for NASH resolution. 92 , 93 There is evidence of reversal of liver fibrosis with weight loss, but the effect is dependent on the degree of weight reduction and baseline BMI. A 7% to 10% decrease in body weight is thought to be required for resolution of NAFLD in patients with obesity; however, only 10% to 20% of individuals are able to achieve a weight loss of ≥10% with lifestyle change over 1 to 2 years. 94 It should be underlined that similar weight loss is less effective in reaching NASH resolution in people with diabetes compared with those without diabetes. 95
In terms of exercise, a study in 32 patients with NAFLD found that 8 weeks of individualized aerobic training improved some metabolic variables, and in particular decreased alanine transaminase (ALT) and AST levels. 96 Conversely, a randomized controlled trial in 24 patients with NASH found that 12 weeks of exercise without weight loss had no significant effect on inflammation or fibrosis markers including ALT and AST, or on noninvasive scores of liver disease. The study did, however, report significant reductions in hepatic and circulating triglycerides, and visceral fat, after the 12‐week programme. 97 Interestingly, a cross‐sectional study found that individuals with NASH are physically deconditioned, with significantly reduced aerobic power and capacity in NASH patients with obesity and overweight, compared with untrained sedentary control subjects. 98 NASH subjects in this study had fitness levels comparable to those of the least fit subset of control subjects. 98 Regarding diet, a meta‐analysis reported that a carbohydrate‐restricted diet may be more effective in reduction of hepatic steatosis than simply a low‐fat diet, 99 possibly due to reduced fructose content. 55 Excessive consumption of fructose has been implicated in the development of NAFLD through increased plasma triglycerides and hepatic DNL. 55 , 100 Increased fatty acid consumption in the form of omega‐3 polyunsaturated fatty acids (PUFA) has been linked to reduced hepatic steatohepatitis, triglyceride content and IR. 100 , 101 However, a randomized controlled trial reported no histological improvement in NASH after 1 year of N‐3 PUFA treatment, despite a reduction in hepatic fat content. 102 However, the inconsistent effects of omega‐3 fatty acids on NAFLD and/or NASH may depend on the composition and purity of omega‐3 fatty acids used in the study and on the severity of liver disease. Previous studies have often used mixtures of eicosapentanoic (EPA) and docosahexanoic acid (DHA) with different degrees of purification. Sanyal et al 103 showed no improvement of NAFLD Activity Score after supplementation with purified EPA in patients with NASH. Only one clinical trial, the WELCOME study (Wessex Evaluation of fatty Liver and Cardiovascular markers in NAFLD with OMacor thErapy), has assessed erythrocyte EPA and DHA enrichment to assess compliance during the study. 104 Using erythrocyte DHA percentage enrichment or erythrocyte EPA percentage enrichment, the authors were able to test the specific contribution of each omega‐3 fatty acid. Thus, it was possible to test associations between percentage DHA enrichment (or percentage EPA enrichment), and changes in liver fat percentage measured by magnetic resonance spectroscopy. In this study, the authors showed an independent association between a decrease in liver fat percentage and enhanced erythrocyte DHA enrichment, but not with erythrocyte EPA enrichment, with purified omega‐3 fatty acid treatment. High‐fibre diets have demonstrated benefits in NAFLD subjects and so are recommended for improvement. 100 , 101 Dietary supplements and homeopathic remedies are also discussed in the Supplementary Appendix S1.
3.3.1. Potential pharmacological treatment approaches targeting metabolic dysfunction
There are currently no FDA‐approved pharmaceutical treatments for patients with NAFLD or NASH; however, some international guidelines do recommend some therapeutic approaches (Supplementary Appendix S1). To date, none of the treatments assessed in NASH have provided efficacy across the heterogeneous patient population and the lack of simple inexpensive tests to assess treatment response and predictors of likelihood of response is a major challenge for drug development.
Treatment approaches for NAFLD based on a range of metabolic targets have been evaluated, including glucagon‐like peptide (GLP)‐1 receptor agonists, sodium‐glucose co‐transporter‐2 (SGLT2) inhibitors, dipeptidyl peptidase‐4 (DPP‐4) inhibitors, insulin sensitizers and the inhibitor of gluconeogenesis metformin, fibroblast growth factor (FGF)‐21 and FGF‐19 agonists and analogues, and an acetyl‐CoA carboxylase (ACC) inhibitor. While insulin therapy could be useful to inhibit adipose tissue lipolysis and thereby reduce liver steatosis, 105 insulin often promotes weight gain in patients with T2DM, so delayed introduction or intensification of insulin is preferred in patients with NAFLD or obesity. 106 Given the ongoing challenges in identifying and categorizing NAFLD, the current basis for drug development is to identify clinically meaningful outcomes and optimal surrogates for disease regression.
3.3.2. Insulin sensitizers and metformin
Thiazolidinediones directly bind to and activate the peroxisome proliferator‐activated receptor (PPAR)‐γ and have been evaluated in a number of studies in NASH. 107 A meta‐analysis including patients with biopsy‐confirmed NASH found that pioglitazone was significantly associated with reversed advanced fibrosis and resolution of NASH, regardless of the presence of T2DM. 108 Another recent meta‐analysis comparing antidiabetic drug classes in patients with NAFLD reported that only the thiazolidinediones and liraglutide have shown an improvement in liver histology. 109 However, thiazolidinediones are associated with weight gain, and their use (and associated risks and benefits) needs to be carefully considered in patients with NASH. 108 , 110 Other adverse events associated with first‐generation thiazolidinediones include bone fractures, congestive heart failure, cancer, hypoglycaemia and lower‐limb oedema. 107 , 108 , 110 MSDC‐0602K, a second generation of thiazolidinedione that targets the mitochondrial pyruvate carrier, did not demonstrate significant effects on primary and secondary liver histology endpoints in a randomized, double‐blind, placebo‐controlled phase 2b study. 107 However, the effects on noninvasive measures of liver cell injury and glucose metabolism support further exploration of the safety and potential efficacy of MSDC‐0602K in patients with T2DM and liver injury. 107 Adverse events typically associated with thiazolidinediones were not observed more frequently with MSDC‐0602K than placebo. 107 A phase 3 study assessing resolution of NASH with MSDC‐0602K in patients with NASH and T2DM (NCT03970031) is planned.
Other next‐generation insulin sensitizers, such as elafibranor and seladelpar, which act via the PPAR family, showed initial promise in NAFLD but have not been able to demonstrate significant improvements in liver histology to date, 107 , 111 , 112 , 113 and clinical development of elafibranor (a dual PPAR‐α/‐δ agonist) and seladelpar (a PPAR‐δ agonist) in NAFLD has halted. Lanifibranor, a pan‐PPAR agonist, was evaluated for the treatment of NASH in the phase 2b NATIVE study. 114 A press release in June 2020 announced that significantly more patients achieved a decrease of ≥2 points in the Steatosis Activity Fibrosis score (combining assessments of hepatocellular inflammation and ballooning) from baseline with lanifibranor 1200 mg/d versus placebo (49% vs 27%; P = 0.004). 115 Resolution of NASH and no worsening of fibrosis was also observed in 45% of patients receiving lanifibranor 1200 mg/d versus 19% receiving placebo (P < 0.001). 115 Modest weight increase and peripheral oedema were observed with lanifibranor treatment. 115 On the basis of these promising results, a phase 3 programme is planned for lanifibranor in NASH.
Pemafibrate is a highly selective PPAR‐α agonist that promotes the induction of genes involved in fatty acid oxidation, lipid mobilization and energy metabolism. 116 , 117 In a clinical trial in patients with T2DM and hypertriglyceridaemia over 24 weeks, pemafibrate was shown to significantly reduce fasting serum triglycerides (P <0.001) and HOMA‐IR score (0.4 mg/d, P <0.05; 0.2 mg/d, P <0.01) compared with placebo. 118 Incidence of adverse events was similar with pemafibrate or placebo. 118 Most clinical trials of pemafibrate have been in Japan, 116 including the ongoing phase 2, placebo‐controlled trial investigating the efficacy and safety of pemafibrate in patients with NAFLD (NCT03350165). The large‐scale phase 3 clinical trial, PROMINENT (NCT03071692), is investigating effects of pemafibrate on CV outcomes in patients with T2DM and combined dyslipidaemia across multiple countries worldwide.
Metformin has a modest benefit on weight loss and, in studies in NAFLD, has generally not demonstrated significant improvements over comparator therapy in serum markers of liver injury, liver fat content, or in histological inflammation and fibrosis. 119 In a study of 85 patients with T2DM and NAFLD, 24 weeks of either metformin or liraglutide significantly improved weight, BMI, and waist circumference versus gliclazide (all P <0.01) 120 ; however, there was a significant reduction in intrahepatic fat content with liraglutide versus gliclazide (P = 0.001), but not with metformin. 121 NS‐0200, a fixed‐dose combination of leucine, metformin, and sildenafil, has been assessed in a phase 2 randomized controlled trial of patients with NAFLD. No significant differences were seen versus placebo, but high‐dose NS‐0200 (1.1 g leucine/0.5 g metformin/1.0 mg sildenafil) twice weekly for 16 weeks significantly reduced hepatic fat content compared with placebo in a subgroup of patients with high baseline ALT (P <0.005). 122 Adverse events associated with metformin typically include gastrointestinal effects such as nausea and diarrhoea. 123 In patients with severe hepatic, renal or cardiac dysfunction, metformin use is discouraged due to subclinical increases in lactic acid and potential lactic acidosis in a small subset of patients. 123
3.3.3. GLP‐1 receptor agonists
Liraglutide, a once‐daily GLP‐1 receptor agonist, is licensed for T2DM (maximum dose: 1.8 mg/d) and weight management in adults with metabolic disorders who have overweight or obesity (maximum dose: 3.0 mg/d). Liraglutide was shown in the phase 2 Lira‐NAFLD study (dose: 1.2 mg/d) to significantly reduce body weight and liver fat content (P <0.0001) after 6 months of treatment in patients with NAFLD and T2DM. 124 In a meta‐analysis, patients with NASH (particularly those with T2DM) had improved liver histology, aminotransferase levels, and obesity in response to treatment with GLP‐1 receptor agonists liraglutide or exenatide. 125 In the phase 2 LEAN randomized controlled study, more patients treated with liraglutide achieved histological resolution of NASH compared with patients receiving placebo (P = 0.019), while fewer patients treated with liraglutide had progression of fibrosis compared with patients receiving placebo (P = 0.04). 126 Recently, the once‐weekly GLP‐1 receptor agonist semaglutide has also been shown to significantly reduce ALT and hsCRP levels in a dose‐dependent manner in patients with obesity or T2DM. 127 In a recent phase 2 trial of semaglutide in patients with NASH, the primary endpoint of NASH resolution with no worsening of liver fibrosis was met (P <0.001). 128 Significant reductions in ALT and AST have also been reported with the investigational dual GLP‐1 and glucose‐dependent insulinotropic polypeptide receptor agonist tirzepatide. 129 Adverse events associated with GLP‐1 receptor agonists are typically gastrointestinal, such as nausea, vomiting, diarrhoea, abdominal discomfort and appetite suppression. 125
A phase 2a study of the dual GLP‐1/glucagon receptor agonist cotadutide has demonstrated beneficial effects in patients with T2DM and excess body weight. 130 Over a 42‐day period, there were significant reductions in blood glucose levels (P <0.0001), body weight (P = 0.0008), and liver fat (P = 0.0172) with cotadutide treatment, compared with placebo. 130 Gastrointestinal disturbances and decreased appetite occurred more frequently with cotadutide than with placebo. 130 It is thought that the GLP‐1 receptor agonism effects of reducing plasma glucose should counterbalance any hyperglycaemic effects from glucagon receptor agonism, while allowing beneficial effects such as increased energy expenditure, satiety, hepatic lipolysis and fatty acid oxidation. 131 , 132
3.3.4. DPP‐4 inhibitors
Dipeptidyl peptidase‐4 is a serine protease involved in metabolism and immune function, and GLP‐1 is among its peptidase targets. 133 , 134 , 135 As such, DPP‐4 has been evaluated in relation to T2DM and NAFLD. A cross‐sectional study found significant correlations between DPP‐4 activity and ALT (r = 0.4637, P = 0.0038) and GGT (r = 0.4491, P = 0.0017) levels, and a direct correlation between DPP‐4 activity and HOMA2‐IR (r = 0.5295, P = 0.0026). 134 A more recent cross‐sectional study corroborated these findings by concluding that, not only do patients with NAFLD have increased DPP‐4 activity (P = 0.02) irrespective of obesity, but there is also a linear relationship between DPP‐4 activity and the severity of liver steatosis (P = 0.04) and lobular inflammation (P = 0.03). 133 DPP‐4 has therefore been identified as a possible marker of disease progression in NAFLD. 133 , 134 , 135 While it has been suggested in one small open‐label randomized controlled trial that sitagliptin, a DPP‐4 inhibitor, improved NAFLD Activity Score irrespective of diabetes status, 136 additional larger double‐blind randomized controlled trials are warranted to confirm the potential benefit of DPP‐4 inhibitors in NASH. DPP‐4 inhibitors have a good safety profile and the most frequent adverse events observed are nasopharyngitis and, more rarely, skin lesions (bullous pemphigoid). 137
3.3.5. SGLT2 inhibitors
The established antidiabetic SGLT2 inhibitors are known to reduce body weight and body fat, mainly by increasing urinary glucose excretion. In the EFFECT‐II study, the SGLT2 inhibitor dapagliflozin, in combination with omega‐3 carboxylic acids, significantly reduced liver fat content (P <0.05), and decreased markers of hepatocyte injury including plasma FGF‐21, compared with placebo. 138 Empagliflozin, another SGLT2 inhibitor, was shown in the E‐LIFT study to significantly reduce liver fat versus standard treatment (P <0.0001). 139 A recent phase 4 study provided evidence that empagliflozin effectively reduces liver fat content compared with placebo, but has no major effects on tissue‐specific insulin sensitivity. 140 Exploratory analyses also revealed a marked decrease in serum UA and a rise in serum high molecular weight adiponectin levels. 140 These effects occurred in the presence of moderate weight loss and despite only minor changes in glycaemia in a cohort of patients with metabolically well‐controlled T2DM and a short disease duration. 140 There is currently a need to better understand the mechanism of action of SGLT2 inhibitors in the liver and to further characterize potential benefit in patients with NAFLD, particularly on liver histology. The most common adverse effects associated with SGLT2 inhibitors are mycotic genital infections 141 and, particularly in individuals with type 1 diabetes, diabetic ketoacidosis. 142
3.3.6. Other potential pharmacological treatment approaches based on metabolic dysfunction
It has been proposed that combining GLP‐1 analogues with an SGLT2 inhibitor and/or a specific statin could potentially reduce the risk of CV‐related morbidity and mortality, as well as liver‐related morbidity in patients with NASH, 143 while combining GLP‐1 analogues such as liraglutide or exenatide with thiazolidinediones also has the capacity to reduce hepatic fat content in patients with NAFLD and T2DM. 144
The farnesoid X receptor (FXR), a metabolic nuclear receptor that is critically involved in regulating bile acid, lipid, and glucose metabolism, 145 , 146 is a potential therapeutic target because serum bile acid levels have been shown to correlate with disease severity in NAFLD. 147 Obeticholic acid, an FXR agonist, provided significant histological improvement in fibrosis versus placebo among patients with NASH and F2‐3‐stage fibrosis as part of a planned 18‐month interim analysis of a phase 3 REGENERATE randomized controlled trial (NCT02548351); this study is ongoing to assess clinical outcomes. 148 Pruritis and elevated LDL cholesterol have been reported as common adverse effects of obeticholic acid. 148 , 149 , 150 Given the association with elevated LDL cholesterol levels, combination of statins with obeticholic acid has been suggested. 150 The phase 2 CONTROL study found that coadministration with atorvastatin reversed the effects of obeticholic acid on LDL cholesterol concentration in patients with NASH and fibrosis. 150
Norursodeoxycholic acid is a synthetic bile acid homologue which has been assessed in a dose‐finding phase 2 trial in individuals with NAFLD. 151 A dose‐related reduction of serum ALT was reported after treatment with norursodeoxycholic acid, as were reductions in AST and GGT, compared with placebo. 151 The most common adverse events reported were headaches, infections and gastrointestinal effects. 151 A phase 2b trial on the safety and efficacy of norursodeoxycholic acid in NAFLD is currently underway (EudraCT number 2018‐003443‐31).
Fibroblast growth factor‐19 has been implicated in multiple metabolic pathways in the pathogenesis of NASH. Aldafermin (NGM282), an FGF19 analogue, has been shown in a phase 2 randomized controlled trial in patients with biopsy‐confirmed NASH to significantly reduce liver fat content (P <0.0001), ALT and AST (P <0.0001), and some fibrosis biomarkers (Pro‐C3 and TIMP‐1; P <0.05) versus placebo after 12 weeks. 152 Reported adverse events included injection site reactions, gastrointestinal symptoms and abdominal pain. 152 A phase 2b dose‐ranging study is ongoing to further assess the potential of aldafermin in patients with NASH and liver fibrosis (NCT03912532).
The intestinal cholesterol absorption inhibitor ezetimibe was assessed in a randomized controlled pilot study of 50 patients with biopsy‐confirmed NASH, but did not significantly improve liver fat, histology, enzymes, or stiffness versus placebo. 153 No significant side effects were found compared with the placebo arm. 153
Acetyl‐CoA carboxylase catalyses the rate‐limiting step in DNL. Firsocostat (GS‐0976), a small molecule inhibitor of ACC isoforms 1 and 2, has been shown to significantly reduce hepatic steatosis (P = 0.002), metalloproteinase 1 (a marker of fibrogenesis; P = 0.022), and multiple plasma acylcarnitine species (P <0.001‐0.009). 154 Commonly reported adverse events were nausea, abdominal pain and diarrhoea. 154 Firsocostat is currently being investigated in combination with antifibrotic agents in patients with NASH (NCT02781584).
Resmetirom, a selective thyroid hormone receptor‐β agonist, is the first thyroid hormone analogue investigated for use in treatment of NASH. 155 A phase 2 randomized, double‐blind study in patients with biopsy‐confirmed NASH reported significant reductions in hepatic fat after treatment with resmetirom compared with placebo (P <0.0001). 155 Resmetirom treatment also reduced levels of triglycerides, cholesterol and other lipids. 155 A higher incidence of transient mild diarrhoea and nausea was observed with resmetirom versus placebo. A phase 3 trial for the treatment of NASH with resmetirom is ongoing (NCT03900429).
The impact of bariatric surgery on NAFLD is discussed in the Supplementary Appendix S1.
4. CONCLUSIONS
Type 2 diabetes, obesity and MetS are well established as major global health challenges associated with significant economic impact. NAFLD very commonly co‐occurs with other metabolic disorders, meaning that patients typically have multiple health challenges and greatly increased risk of serious clinical consequences. Although not yet widely adopted, the term MAFLD has been proposed by an international expert panel when describing hepatic steatosis associated with metabolic dysfunction, in recognition of the specific characteristics of NAFLD in comparison with other liver diseases. 49 Many patients with NAFLD may be primarily under the care of nonhepatology specialists, including diabetologists, cardiologists, endocrinologists, and primary care physicians, and at this interface between metabolic and hepatic medicine, optimal patient care requires effective multidisciplinary collaboration and joint protocols. 156 It seems likely that a combined approach of pharmacotherapy (including systemic glucose and lipid management) with lifestyle and behavioural interventions will prove most successful, given the complex multifaceted nature of metabolic disorders. In the future, it would be preferable to establish treatment options with known benefits for both NAFLD and the other metabolic disorders with which patients typically present. The increased risk of CV complications and gastrointestinal tumours in addition to HCC suggests a need for proactive assessment and rapid intervention of comorbidities by the relevant specialist clinician. There is an opportunity to build on the chronic disease management approach that is already being implemented in some healthcare systems for patients with T2DM or obesity. Our growing understanding of the natural history and pathogenesis of NAFLD and NASH, focused efforts on new diagnostic and interventional approaches, and ability to deliver optimal multidisciplinary care provide opportunities to improve outcomes for patients with NAFLD and NASH and reduce the impact on healthcare systems.
CONFLICT OF INTEREST
B. C. reports grants and personal fees from Amgen, Regeneron and Sanofi, and personal fees from Abbott, Akcea, AstraZeneca, Bristol Myers Squibb, Genfit, Gilead, Eli Lilly and Company, Merck (MSD) and Novo Nordisk. R. L. serves as a consultant or advisory board member for 89bio, Alnylam, Arrowhead Pharmaceuticals, AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Cirius, CohBar, DiCerna, Galmed, Gilead, Glympse bio, Intercept, Ionis, Metacrine, NGM Biopharmaceuticals, Novo Nordisk, Pfizer, Sagimet and Viking Therapeutics. In addition, his institution has received grant support from Allergan, Boehringer Ingelheim, Bristol Myers Squibb, Eli Lilly and Company, Galmed Pharmaceuticals, Genfit, Gilead, Intercept, Inventiva, Janssen, Madrigal Pharmaceuticals, NGM Biopharmaceuticals, Novartis, Pfizer, pH Pharma and Siemens. He is also co‐founder of Liponexus, Inc. A. J. S. is President of Sanyal Biotechnology and has stock options in Genfit, Akarna, Tiziana, Indalo, Durect Inversago and Galmed. He has served as a consultant to AstraZeneca, Nitto Denko, Conatus, Nimbus, Salix, Tobira, Takeda, Janssen, Gilead, Terns, Birdrock, Merck, Valeant, Boehringer Ingelheim, Bristol Myers Squibb, Eli Lilly and Company, Hemoshear, Zafgen, Novartis, Novo Nordisk, Pfizer, Exhalenz and Genfit. He has been an unpaid consultant to Intercept, Echosens, Immuron, Galectin, Fractyl, Syntlogic, Affimune, Chemomab, Zydus, Nordic Bioscience, Albireo, Prosciento and Surrozen. His institution has received grant support from Gilead, Salix, Tobira, Bristol Myers Squibb, Shire, Intercept, Merck, AstraZeneca, Malinckrodt, Cumberland and Novartis. He receives royalties from Elsevier and UptoDate. C. D. B. discloses no conflicts of interest.
AUTHOR CONTRIBUTIONS
All authors participated in the drafting and revision of the manuscript. All authors reviewed and approved the final submitted version.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/dom.14322.
Supporting information
Appendix S1: Supporting Information
ACKNOWLEDGMENTS
Financial support for medical editorial assistance from Anna Bacon, of Articulate Science, was provided by Novo Nordisk. C. D. B. is supported in part by the Southampton NIHR Biomedical Research Centre (IS‐BRC‐20004), UK. R. L. receives funding support from National Institute of Environmental Health Sciences (5P42ES010337), NCATS (5UL1TR001442), NIDDK (R01DK106419, 1R01DK121378, R01 DK124318, P30DK120515), and DOD PRCRP (CA170674P2). A. J. S. receives funding support from National Center for Advancing Translational Sciences (UL1TR002649, KL2TR002648), NIDDK (RO1 DK 10596, 5UO1 DK61731), NIAAA (U01AA026979, AA026966, UH2AA026971), and NCI (CA183954).
Cariou B, Byrne CD, Loomba R, Sanyal AJ. Nonalcoholic fatty liver disease as a metabolic disease in humans: A literature review. Diabetes Obes Metab. 2021;23:1069–1083. 10.1111/dom.14322
Funding information Financial support for medical editorial assistance from Anna Bacon, of Articulate Science, was provided by Novo Nordisk. C. D. B. is supported in part by the Southampton NIHR Biomedical Research Centre (IS‐BRC‐20004), UK. R. L. receives funding support from National Institute of Environmental Health Sciences (5P42ES010337), NCATS (5UL1TR001442), NIDDK (R01DK106419, 1R01DK121378, R01 DK124318, P30DK120515), and DOD PRCRP (CA170674P2). A. J. S. receives funding support from National Center for Advancing Translational Sciences (UL1TR002649, KL2TR002648), NIDDK (RO1 DK 10596, 5UO1 DK61731), NIAAA (U01AA026979, AA026966, UH2AA026971), and NCI (CA183954).
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328‐357. [DOI] [PubMed] [Google Scholar]
- 2. European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO) . EASL‐EASD‐EASO clinical practice guidelines for the management of non‐alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388‐1402. [DOI] [PubMed] [Google Scholar]
- 3. Takahashi Y, Fukusato T. Histopathology of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J Gastroenterol. 2014;20(42):15539‐15548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dulai PS, Singh S, Patel J, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta‐analysis. Hepatology. 2017;65(5):1557‐1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hashimoto E, Taniai M, Tokushige K. Characteristics and diagnosis of NAFLD/NASH. J Gastroenterol Hepatol. 2013;28(4 Suppl):64‐70. [DOI] [PubMed] [Google Scholar]
- 6. Ratziu V, Charlotte F, Heurtier A, et al. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128(7):1898‐1906. [DOI] [PubMed] [Google Scholar]
- 7. Mikolasevic I, Orlic L, Franjic N, Hauser G, Stimac D, Milic S. Transient elastography (FibroScan®) with controlled attenuation parameter in the assessment of liver steatosis and fibrosis in patients with nonalcoholic fatty liver disease ‐ where do we stand? World J Gastroenterol. 2016;22(32):7236‐7251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bril F, McPhaul MJ, Caulfield MP, et al. Performance of the SteatoTest, ActiTest, NashTest and FibroTest in a multiethnic cohort of patients with type 2 diabetes mellitus. J Invest Med. 2019;67(2):303‐311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Subasi CF, Aykut UE, Yilmaz Y. Comparison of noninvasive scores for the detection of advanced fibrosis in patients with nonalcoholic fatty liver disease. Eur J Gastroenterol Hepatol. 2015;27(2):137‐141. [DOI] [PubMed] [Google Scholar]
- 10. Yang M, Jiang L, Wang Y, et al. Step layered combination of noninvasive fibrosis models improves diagnostic accuracy of advanced fibrosis in nonalcoholic fatty liver disease. J Gastrointestin Liver Dis. 2019;28(3):289‐296. [DOI] [PubMed] [Google Scholar]
- 11. Bril F, McPhaul MJ, Caulfield MP, et al. Performance of plasma biomarkers and diagnostic panels for nonalcoholic steatohepatitis and advanced fibrosis in patients with type 2 diabetes. Diabetes Care. 2020;43(2):290‐297. [DOI] [PubMed] [Google Scholar]
- 12. National Institute for Health and Care Excellence . Non‐alcoholic fatty liver disease (NAFLD): assessment and management. 2016. https://www.nice.org.uk/guidance/ng49/chapter/Recommendations. Accessed April, 2020. [PubMed]
- 13. Park CC, Nguyen P, Hernandez C, et al. Magnetic resonance elastography vs transient elastography in detection of fibrosis and noninvasive measurement of steatosis in patients with biopsy‐proven nonalcoholic fatty liver disease. Gastroenterology. 2017;152(3):598‐607.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hsu C, Caussy C, Imajo K, et al. Magnetic resonance vs transient elastography analysis of patients with nonalcoholic fatty liver disease: a systematic review and pooled analysis of individual participants. Clin Gastroenterol Hepatol. 2019;17(4):630‐637.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Newsome PN, Sasso M, Deeks JJ, et al. FibroScan‐AST (FAST) score for the non‐invasive identification of patients with non‐alcoholic steatohepatitis with significant activity and fibrosis: a prospective derivation and global validation study. Lancet Gastroenterol Hepatol. 2020;5(4):362‐373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jung J, Loomba RR, Imajo K, et al. MRE combined with FIB‐4 (MEFIB) index in detection of candidates for pharmacological treatment of NASH‐related fibrosis. Gut. 2020. 10.1136/gutjnl-2020-322976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease‐meta‐analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73‐84. [DOI] [PubMed] [Google Scholar]
- 18. Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015;62(1 Suppl):S47‐S64. [DOI] [PubMed] [Google Scholar]
- 19. Yki‐Jarvinen H. Non‐alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol. 2014;2(11):901‐910. [DOI] [PubMed] [Google Scholar]
- 20. Koliaki C, Szendroedi J, Kaul K, et al. Adaptation of hepatic mitochondrial function in humans with non‐alcoholic fatty liver is lost in steatohepatitis. Cell Metab. 2015;21(5):739‐746. [DOI] [PubMed] [Google Scholar]
- 21. Brown MS, Goldstein JL. Selective versus total insulin resistance: a pathogenic paradox. Cell Metab. 2008;7(2):95‐96. [DOI] [PubMed] [Google Scholar]
- 22. Savvidou S, Karatzidou K, Tsakiri K, Gagalis A, Hytiroglou P, Goulis J. Circulating adiponectin levels in type 2 diabetes mellitus patients with or without non‐alcoholic fatty liver disease: results of a small, open‐label, randomized controlled intervention trial in a subgroup receiving short‐term exenatide. Diabetes Res Clin Pract. 2016;113:125‐134. [DOI] [PubMed] [Google Scholar]
- 23. Mantovani A, Byrne CD, Bonora E, Targher G. Nonalcoholic fatty liver disease and risk of incident type 2 diabetes: a meta‐analysis. Diabetes Care. 2018;41(2):372‐382. [DOI] [PubMed] [Google Scholar]
- 24. Bril F, Cusi K. Management of nonalcoholic fatty liver disease in patients with type 2 diabetes: a call to action. Diabetes Care. 2017;40(3):419‐430. [DOI] [PubMed] [Google Scholar]
- 25. Ratziu V, Goodman Z, Sanyal A. Current efforts and trends in the treatment of NASH. J Hepatol. 2015;62(1 Suppl):S65‐S75. [DOI] [PubMed] [Google Scholar]
- 26. Sanyal AJ, Friedman SL, McCullough AJ, Dimick‐Santos L, American Association for the Study of Liver Diseases , United States Food and Drug Administration . Challenges and opportunities in drug and biomarker development for nonalcoholic steatohepatitis: findings and recommendations from an American Association for the Study of Liver Diseases‐U.S. Food and Drug Administration Joint Workshop. Hepatology. 2015;61(4):1392‐1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Younossi ZM, Stepanova M, Younossi Y, et al. Epidemiology of chronic liver diseases in the USA in the past three decades. Gut. 2019;69(3):564‐568. [DOI] [PubMed] [Google Scholar]
- 28. Lu ZY, Shao Z, Li YL, Wulasihan M, Chen XH. Prevalence of and risk factors for non‐alcoholic fatty liver disease in a Chinese population: an 8‐year follow‐up study. World J Gastroenterol. 2016;22(13):3663‐3669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dai W, Ye L, Liu A, et al. Prevalence of nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus: a meta‐analysis. Medicine (Baltimore). 2017;96(39):e8179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Praveenraj P, Gomes RM, Kumar S, et al. Prevalence and predictors of non‐alcoholic fatty liver disease in morbidly obese south Indian patients undergoing bariatric surgery. Obes Surg. 2015;25(11):2078‐2087. [DOI] [PubMed] [Google Scholar]
- 31. Vassilatou E, Vassiliadi DA, Salambasis K, et al. Increased prevalence of polycystic ovary syndrome in premenopausal women with nonalcoholic fatty liver disease. Eur J Endocrinol. 2015;173(6):739‐747. [DOI] [PubMed] [Google Scholar]
- 32. Kabir MA, Uddin MZ, Siddiqui NI, et al. Prevalence of non‐alcoholic fatty liver disease and its biochemical predictors in patients with type‐2 diabetes mellitus. Mymensingh Med J. 2018;27(2):237‐244. [PubMed] [Google Scholar]
- 33. Herath HMM, Kodikara I, Weerarathna TP, Liyanage G. Prevalence and associations of non‐alcoholic fatty liver disease (NAFLD) in Sri Lankan patients with type 2 diabetes: a single center study. Diabetes Metab Syndr. 2019;13(1):246‐250. [DOI] [PubMed] [Google Scholar]
- 34. Caussy C, Soni M, Cui J, et al. Nonalcoholic fatty liver disease with cirrhosis increases familial risk for advanced fibrosis. J Clin Invest. 2017;127(7):2697‐2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Marchesini G, Brizi M, Morselli‐Labate AM, et al. Association of nonalcoholic fatty liver disease with insulin resistance. Am J Med. 1999;107(5):450‐455. [DOI] [PubMed] [Google Scholar]
- 36. Sanyal AJ, Campbell‐Sargent C, Mirshahi F, et al. Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology. 2001;120(5):1183‐1192. [DOI] [PubMed] [Google Scholar]
- 37. Ballestri S, Zona S, Targher G, et al. Nonalcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta‐analysis. J Gastroenterol Hepatol. 2016;31(5):936‐944. [DOI] [PubMed] [Google Scholar]
- 38. Tokita Y, Maejima Y, Shimomura K, et al. Non‐alcoholic fatty liver disease is a risk factor for type 2 diabetes in middle‐aged japanese men and women. Internal Med. 2017;56(7):763‐771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sung KC, Jeong WS, Wild SH, Byrne CD. Combined influence of insulin resistance, overweight/obesity, and fatty liver as risk factors for type 2 diabetes. Diabetes Care. 2012;35(4):717‐722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gaharwar R, Trikha S, Margekar SL, Jatav OP, Ganga PD. Study of clinical profile of patients of non alcoholic fatty liver disease and its association with metabolic syndrome. J Assoc Physicians India. 2015;63(1):12‐16. [PubMed] [Google Scholar]
- 41. Wargny M, Smati S, Pichelin M, et al. Fatty liver index is a strong predictor of changes in glycemic status in people with prediabetes: the IT‐DIAB study. PLoS One. 2019;14(8):e0221524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Pang Q, Zhang JY, Song SD, et al. Central obesity and nonalcoholic fatty liver disease risk after adjusting for body mass index. World J Gastroenterol. 2015;21(5):1650‐1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Li L, Liu DW, Yan HY, Wang ZY, Zhao SH, Wang B. Obesity is an independent risk factor for non‐alcoholic fatty liver disease: evidence from a meta‐analysis of 21 cohort studies. Obesity Rev. 2016;17(6):510‐519. [DOI] [PubMed] [Google Scholar]
- 44. Albhaisi S, Chowdhury A, Sanyal AJ. Non‐alcoholic fatty liver disease in lean individuals. JHEP Rep. 2019;1(4):329‐341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kleiner DE, Brunt EM, Wilson LA, et al. Association of histologic disease activity with progression of nonalcoholic fatty liver disease. JAMA Netw Open. 2019;2(10):e1912565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Strey CBM, de Carli LA, Fantinelli M, et al. Impact of diabetes mellitus and insulin on nonalcoholic fatty liver disease in the morbidly obese. Ann Hepatol. 2018;17(4):585‐591. [DOI] [PubMed] [Google Scholar]
- 47. Jarvis H, Craig D, Barker R, et al. Metabolic risk factors and incident advanced liver disease in non‐alcoholic fatty liver disease (NAFLD): a systematic review and meta‐analysis of population‐based observational studies. PLoS Med. 2020;17(4):e1003100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lu FB, Hu ED, Xu LM, et al. The relationship between obesity and the severity of non‐alcoholic fatty liver disease: systematic review and meta‐analysis. Expert Rev Gastroenterol Hepatol. 2018;12(5):491‐502. [DOI] [PubMed] [Google Scholar]
- 49. Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction‐associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73(1):202‐209. [DOI] [PubMed] [Google Scholar]
- 50. Fouad Y, Waked I, Bollipo S, Gomaa A, Ajlouni Y, Attia D. What's in a name? Renaming 'NAFLD' to 'MAFLD'. Liver Int. 2020;40(6):1254‐1261. [DOI] [PubMed] [Google Scholar]
- 51. Ye Q, Zou B, Yeo YH, et al. Global prevalence, incidence, and outcomes of non‐obese or lean non‐alcoholic fatty liver disease: a systematic review and meta‐analysis. Lancet Gastroenterol Hepatol. 2020;5(8):739‐752. [DOI] [PubMed] [Google Scholar]
- 52. Sinha N, Mukhopadhyay S, Sau M. Metabolic syndrome is not uncommon among lean non‐alcoholic fatty liver disease patients as compared with those with obesity. Indian J Gastroenterol. 2020;39(1):75‐83. [DOI] [PubMed] [Google Scholar]
- 53. Kumar R, Mohan S. Non‐alcoholic fatty liver disease in lean subjects: characteristics and implications. J Clin Transl Hepatol. 2017;5(3):216‐223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Donnelly KL, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest. 2005;115(5):1343‐1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ter Horst KW, Serlie MJ. Fructose consumption, lipogenesis, and non‐alcoholic fatty liver disease. Nutrients. 2017;9(9):981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Virtue S, Vidal‐Puig A. Adipose tissue expandability, lipotoxicity and the metabolic syndrome – an allostatic perspective. Biochim Biophys Acta. 2010;1801(3):338‐349. [DOI] [PubMed] [Google Scholar]
- 57. Romero‐Ibarguengoitia ME, Vadillo‐Ortega F, Caballero AE, et al. Family history and obesity in youth, their effect on acylcarnitine/aminoacids metabolomics and non‐alcoholic fatty liver disease (NAFLD). Structural equation modeling approach. PLoS One. 2018;13(2):e0193138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Chen Z, Yu R, Xiong Y, Du F, Zhu S. A vicious circle between insulin resistance and inflammation in nonalcoholic fatty liver disease. Lipids Health Dis. 2017;16(1):203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Masarone M, Rosato V, Dallio M, et al. Role of oxidative stress in pathophysiology of nonalcoholic fatty liver disease. Oxid Med Cell Longev. 2018;2018:9547613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Russo L, Lumeng CN. Properties and functions of adipose tissue macrophages in obesity. Immunology. 2018;155(4):407‐417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lauterbach MAR, Wunderlich FT. Macrophage function in obesity‐induced inflammation and insulin resistance. Pflugers Arch. 2017;469(3–4):385‐396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Chylikova J, Dvorackova J, Tauber Z, Kamarad V. M1/M2 macrophage polarization in human obese adipose tissue. Biomedica Pap Med Fac Univ Palacky Olomouc Czech Repub. 2018;162(2):79‐82. [DOI] [PubMed] [Google Scholar]
- 63. Chakravarthy MV, Neuschwander‐Tetri BA. The metabolic basis of nonalcoholic steatohepatitis. Endocrinol Diabetes Metab. 2020;3(4):e00112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ter Horst KW, Gilijamse PW, Versteeg RI, et al. Hepatic diacylglycerol‐associated protein kinase Cε translocation links hepatic steatosis to hepatic insulin resistance in humans. Cell Rep. 2017;19(10):1997‐2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Magkos F, Su X, Bradley D, et al. Intrahepatic diacylglycerol content is associated with hepatic insulin resistance in obese subjects. Gastroenterology. 2012;142(7):1444‐1446.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Kumashiro N, Erion DM, Zhang D, et al. Cellular mechanism of insulin resistance in nonalcoholic fatty liver disease. Proc Natl Acad Sci U S A. 2011;108(39):16381‐16385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Luukkonen PK, Zhou Y, Sädevirta S, et al. Hepatic ceramides dissociate steatosis and insulin resistance in patients with non‐alcoholic fatty liver disease. J Hepatol. 2016;64(5):1167‐1175. [DOI] [PubMed] [Google Scholar]
- 68. Santilli F, Blardi P, Scapellato C, et al. Decreased plasma endogenous soluble RAGE, and enhanced adipokine secretion, oxidative stress and platelet/coagulative activation identify non‐alcoholic fatty liver disease among patients with familial combined hyperlipidemia and/or metabolic syndrome. Vascul Pharmacol. 2015;72:16‐24. [DOI] [PubMed] [Google Scholar]
- 69. Al Rifai M, Silverman MG, Nasir K, et al. The association of nonalcoholic fatty liver disease, obesity, and metabolic syndrome, with systemic inflammation and subclinical atherosclerosis: the multi‐ethnic study of atherosclerosis (MESA). Atherosclerosis. 2015;239(2):629‐633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Di Naso FC, Porto RR, Fillmann HS, et al. Obesity depresses the anti‐inflammatory HSP70 pathway, contributing to NAFLD progression. Obesity (Silver Spring). 2015;23(1):120‐129. [DOI] [PubMed] [Google Scholar]
- 71. Yoo HJ, Hwang SY, Choi JH, et al. Association of leukocyte cell‐derived chemotaxin 2 (LECT2) with NAFLD, metabolic syndrome, and atherosclerosis. PLoS One. 2017;12(4):e0174717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ibrahim SH, Hirsova P, Gores GJ. Non‐alcoholic steatohepatitis pathogenesis: sublethal hepatocyte injury as a driver of liver inflammation. Gut. 2018;67(5):963‐972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Gastaldelli A, Harrison SA, Belfort‐Aguilar R, et al. Importance of changes in adipose tissue insulin resistance to histological response during thiazolidinedione treatment of patients with nonalcoholic steatohepatitis. Hepatology. 2009;50(4):1087‐1093. [DOI] [PubMed] [Google Scholar]
- 74. Nannipieri M, Cecchetti F, Anselmino M, et al. Pattern of expression of adiponectin receptors in human liver and its relation to nonalcoholic steatohepatitis. Obes Surg. 2009;19(4):467‐474. [DOI] [PubMed] [Google Scholar]
- 75. Bekaert M, Verhelst X, Geerts A, Lapauw B, Calders P. Association of recently described adipokines with liver histology in biopsy‐proven non‐alcoholic fatty liver disease: a systematic review. Obes Rev. 2016;17(1):68‐80. [DOI] [PubMed] [Google Scholar]
- 76. Csak T, Ganz M, Pespisa J, Kodys K, Dolganiuc A, Szabo G. Fatty acid and endotoxin activate inflammasomes in mouse hepatocytes that release danger signals to stimulate immune cells. Hepatology. 2011;54(1):133‐144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Zhang Y, Wang J, Zhang Z, Lin W, Cao S, Liu Y. A clinical study of life quality with anxiety and depression self rating in patients of NAFLD affected by metabolic syndrome. Hepatol Int. 2017;11(1):S940‐S941. [Google Scholar]
- 78. Wild SH, Walker JJ, Morling JR, et al. Cardiovascular disease, cancer, and mortality among people with type 2 diabetes and alcoholic or nonalcoholic fatty liver disease hospital admission. Diabetes Care. 2018;41(2):341‐347. [DOI] [PubMed] [Google Scholar]
- 79. Zhou YY, Zhou XD, Wu SJ, et al. Synergistic increase in cardiovascular risk in diabetes mellitus with nonalcoholic fatty liver disease: a meta‐analysis. Eur J Gastroenterol Hepatol. 2018;30(6):631‐636. [DOI] [PubMed] [Google Scholar]
- 80. Wijarnpreecha K, Lou S, Panjawatanan P, et al. Association between diastolic cardiac dysfunction and nonalcoholic fatty liver disease: a systematic review and meta‐analysis. Dig Liver Dis. 2018;50(11):1166‐1175. [DOI] [PubMed] [Google Scholar]
- 81. Mantovani A, Dauriz M, Sandri D, et al. Association between non‐alcoholic fatty liver disease and risk of atrial fibrillation in adult individuals: an updated meta‐analysis. Liver Int. 2019;39(4):758‐769. [DOI] [PubMed] [Google Scholar]
- 82. Haghbin H, Gangwani MK, Ravi SJK, et al. Nonalcoholic fatty liver disease and atrial fibrillation: possible pathophysiological links and therapeutic interventions. Ann Gastroenterol. 2020;33(6):603‐614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. VanWagner LB, Wilcox JE, Colangelo LA, et al. Association of nonalcoholic fatty liver disease with subclinical myocardial remodeling and dysfunction: a population‐based study. Hepatology. 2015;62(3):773‐783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Yoshihisa A, Sato Y, Yokokawa T, et al. Liver fibrosis score predicts mortality in heart failure patients with preserved ejection fraction. ESC Heart Fail. 2018;5(2):262‐270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Friedrich‐Rust M, Schoelzel F, Maier S, et al. Severity of coronary artery disease is associated with non‐alcoholic fatty liver dis‐ease: a single‐blinded prospective mono‐center study. PLoS One. 2017;12(10):e0186720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Alexander KS, Zakai NA, Lidofsky SD, et al. Non‐alcoholic fatty liver disease, liver biomarkers and stroke risk: the reasons for geographic and racial differences in stroke cohort. PLoS One. 2018;13(3):e0194153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Chen J, Bian D, Zang S, et al. The association between nonalcoholic fatty liver disease and risk of colorectal adenoma and cancer incident and recurrence: a meta‐analysis of observational studies. Expert Rev Gastroenterol Hepatol. 2019;13(4):385‐395. [DOI] [PubMed] [Google Scholar]
- 88. Kogiso T, Sagawa T, Kodama K, Taniai M, Hashimoto E, Tokushige K. Long‐term outcomes of non‐alcoholic fatty liver disease and the risk factors for mortality and hepatocellular carcinoma in a Japanese population. J Gastroenterol Hepatol. 2020;35(9):1579‐1589. [DOI] [PubMed] [Google Scholar]
- 89. Pan S, Hong W, Wu W, et al. The relationship of nonalcoholic fatty liver disease and metabolic syndrome for colonoscopy colorectal neoplasm. Medicine. 2017;96(2):e5809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Wongjarupong N, Assavapongpaiboon B, Susantitaphong P, et al. Non‐alcoholic fatty liver disease as a risk factor for cholangiocarcinoma: a systematic review and meta‐analysis. BMC Gastroenterol. 2017;17(1):149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Stine JG, Wentworth BJ, Zimmet A, et al. Systematic review with meta‐analysis: risk of hepatocellular carcinoma in non‐alcoholic steatohepatitis without cirrhosis compared to other liver diseases. Aliment Pharmacol Ther. 2018;48(7):696‐703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Francque S, Lanthier N, Verbeke L, et al. The Belgian Association for study of the liver guidance document on the management of adult and paediatric non‐alcoholic fatty liver disease. Acta Gastroenterol Belg. 2018;81(1):55‐81. [PubMed] [Google Scholar]
- 93. Chitturi S, Wong VW‐S, Chan W‐K, et al. The Asia–Pacific working party on non‐alcoholic fatty liver disease guidelines 2017—part 2: management and special groups. J Gastroenterol Hepatol. 2018;33(1):86‐98. [DOI] [PubMed] [Google Scholar]
- 94. Hallsworth K, Adams LA. Lifestyle modification in NAFLD/NASH: facts and figures. JHEP Rep. 2019;1(6):468‐479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Vilar‐Gomez E, Martinez‐Perez Y, Calzadilla‐Bertot L, et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology. 2015;149(2):367‐378.e5; quiz e14‐15. [DOI] [PubMed] [Google Scholar]
- 96. Cevik Saldiran T, Mutluay FK, Yağci I, Yilmaz Y. Impact of aerobic training with and without whole‐body vibration training on metabolic features and quality of life in non‐alcoholic fatty liver disease patients. Ann Endocrinol (Paris). 2020;81(5):493‐499. [DOI] [PubMed] [Google Scholar]
- 97. Houghton D, Thoma C, Hallsworth K, et al. Exercise reduces liver lipids and visceral adiposity in patients with nonalcoholic steatohepatitis in a randomized controlled trial. Clin Gastroenterol Hepatol. 2017;15(1):96‐102.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Argo CK, Stine JG, Henry ZH, et al. Physical deconditioning is the common denominator in both obese and overweight subjects with nonalcoholic steatohepatitis. Aliment Pharmacol Ther. 2018;48(3):290‐299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Haghighatdoost F, Salehi‐Abargouei A, Surkan PJ, Azadbakht L. The effects of low carbohydrate diets on liver function tests in nonalcoholic fatty liver disease: a systematic review and meta‐analysis of clinical trials. J Res Med Sci. 2016;21:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. George ES, Forsyth A, Itsiopoulos C, et al. Practical dietary recommendations for the prevention and management of nonalcoholic fatty liver disease in adults. Adv Nutr. 2018;9(1):30‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Romero‐Gómez M, Zelber‐Sagi S, Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. 2017;67(4):829‐846. [DOI] [PubMed] [Google Scholar]
- 102. Argo CK, Patrie JT, Lackner C, et al. Effects of n‐3 fish oil on metabolic and histological parameters in NASH: a double‐blind, randomized, placebo‐controlled trial. J Hepatol. 2015;62(1):190‐197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Sanyal AJ, Abdelmalek MF, Suzuki A, Cummings OW, Chojkier M, EPE‐A Study Group . No significant effects of ethyl‐eicosapentanoic acid on histologic features of nonalcoholic steatohepatitis in a phase 2 trial. Gastroenterology. 2014;147(2):377‐384.e1. [DOI] [PubMed] [Google Scholar]
- 104. Scorletti E, Bhatia L, McCormick KG, et al. Effects of purified eicosapentaenoic and docosahexaenoic acids in nonalcoholic fatty liver disease: results from the Welcome* study. Hepatology. 2014;60(4):1211‐1221. [DOI] [PubMed] [Google Scholar]
- 105. Juurinen L, Tiikkainen M, Hakkinen AM, Hakkarainen A, Yki‐Jarvinen H. Effects of insulin therapy on liver fat content and hepatic insulin sensitivity in patients with type 2 diabetes. Am J Physiol Endocrinol Metab. 2007;292(3):E829‐E835. [DOI] [PubMed] [Google Scholar]
- 106. Tacelli M, Celsa C, Magro B, et al. Antidiabetic drugs in NAFLD: the accomplishment of two goals at once? Pharmaceuticals (Basel). 2018;11(4):121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Harrison SA, Alkhouri N, Davison BA, et al. Insulin sensitizer MSDC‐0602K in non‐alcoholic steatohepatitis: a randomized, double‐blind, placebo‐controlled phase IIb study. J Hepatol. 2020;72(4):613‐626. [DOI] [PubMed] [Google Scholar]
- 108. Musso G, Cassader M, Paschetta E, Gambino R. Thiazolidinediones and advanced liver fibrosis in nonalcoholic steatohepatitis: a meta‐analysis. JAMA Intern Med. 2017;177(5):633‐640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Mantovani A, Byrne CD, Scorletti E, Mantzoros CS, Targher G. Efficacy and safety of anti‐hyperglycaemic drugs in patients with non‐alcoholic fatty liver disease with or without diabetes: an updated systematic review of randomized controlled trials. Diabetes Metab. 2020;46(6):427‐441. [DOI] [PubMed] [Google Scholar]
- 110. Cariou B, Charbonnel B, Staels B. Thiazolidinediones and PPARgamma agonists: time for a reassessment. Trends Endocrinol Metab. 2012;23(5):205‐215. [DOI] [PubMed] [Google Scholar]
- 111. Genfit Corp . GENFIT: announces results from interim analysis of RESOLVE‐IT phase 3 trial of elafibranor in adults with NASH and Fibrosis. 2020. https://ir.genfit.com/news-releases/news-release-details/genfit-announces-results-interim-analysis-resolve-it-phase-3. Accessed 6 June, 2020.
- 112. CymaBay Therapeutics . CymaBay Therapeutics Halts clinical development of Seladelpar. 2019. https://www.globenewswire.com/news-release/2019/11/25/1951942/0/en/CymaBay-Therapeutics-Halts-Clinical-Development-of-Seladelpar.html. Accessed 6 June, 2020.
- 113. Ratziu V, Harrison SA, Francque S, et al. Elafibranor, an agonist of the peroxisome proliferator‐activated receptor‐α and ‐δ, induces resolution of nonalcoholic steatohepatitis without fibrosis worsening. Gastroenterology. 2016;150(5):1147‐1159.e1145. [DOI] [PubMed] [Google Scholar]
- 114. Sven MF, Pierre B, Manal FA, et al. A randomised, double‐blind, placebo‐controlled, multi‐centre, dose‐range, proof‐of‐concept, 24‐week treatment study of lanifibranor in adult subjects with non‐alcoholic steatohepatitis: design of the NATIVE study. Contemp Clin Trials. 2020;98:106170. [DOI] [PubMed] [Google Scholar]
- 115. INVENTIVA . Inventiva's lanifibranor meets the primary and key secondary endpoints in the Phase IIb NATIVE clinical trial in non‐alcoholic steatohepatitis (NASH). 2020. https://www.globenewswire.com/news-release/2020/06/15/2048284/0/en/Inventiva-s-lanifibranor-meets-the-primary-and-key-secondary-endpoints-in-the-Phase-IIb-NATIVE-clinical-trial-in-non-alcoholic-steatohepatitis-NASH.html. Accessed 22 July, 2020.
- 116. Yamashita S, Masuda D, Matsuzawa Y. Pemafibrate, a new selective PPARalpha modulator: drug concept and its clinical applications for dyslipidemia and metabolic diseases. Curr Atheroscler Rep. 2020;22(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Sasaki Y, Asahiyama M, Tanaka T, et al. Pemafibrate, a selective PPARalpha modulator, prevents non‐alcoholic steatohepatitis development without reducing the hepatic triglyceride content. Sci Rep. 2020;10(1):7818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Araki E, Yamashita S, Arai H, et al. Effects of pemafibrate, a novel selective PPARalpha modulator, on lipid and glucose metabolism in patients with type 2 diabetes and hypertriglyceridemia: a randomized, double‐blind, placebo‐controlled, phase 3 trial. Diabetes Care. 2018;41(3):538‐546. [DOI] [PubMed] [Google Scholar]
- 119. Pan CS, Stanley TL. Effect of weight loss medications on hepatic steatosis and steatohepatitis: a systematic review. Front Endocrinol (Lausanne). 2020;11:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Feng WH, Bi Y, Li P, et al. Effects of liraglutide, metformin and gliclazide on body composition in patients with both type 2 diabetes and non‐alcoholic fatty liver disease: a randomized trial. J Diabetes Investig. 2019;10(2):399‐407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Feng W, Gao C, Bi Y, et al. Randomized trial comparing the effects of gliclazide, liraglutide, and metformin on diabetes with non‐alcoholic fatty liver disease. J Diabetes. 2017;9(8):800‐809. [DOI] [PubMed] [Google Scholar]
- 122. Chalasani N, Vuppalanchi R, Rinella M, et al. Randomised clinical trial: a leucine‐metformin‐sildenafil combination (NS‐0200) vs placebo in patients with non‐alcoholic fatty liver disease. Aliment Pharmacol Ther. 2018;47(12):1639‐1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Flory J, Lipska K. Metformin in 2019. JAMA. 2019;321(19):1926‐1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Petit J‐M, Cercueil J‐P, Loffroy R, et al. Effect of liraglutide therapy on liver fat content in patients with inadequately controlled type 2 diabetes: the Lira‐NAFLD study. J Clin Endocrinol Metab. 2017;102(2):407‐415. [DOI] [PubMed] [Google Scholar]
- 125. Dong Y, Lv Q, Li S, et al. Efficacy and safety of glucagon‐like peptide‐1 receptor agonists in non‐alcoholic fatty liver disease: a systematic review and meta‐analysis. Clin Res Hepatol Gastroenterol. 2017;41(3):284‐295. [DOI] [PubMed] [Google Scholar]
- 126. Armstrong MJ, Gaunt P, Aithal GP, et al. Liraglutide safety and efficacy in patients with non‐alcoholic steatohepatitis (LEAN): a multicentre, double‐blind, randomised, placebo‐controlled phase 2 study. Lancet. 2016;387(10019):679‐690. [DOI] [PubMed] [Google Scholar]
- 127. Newsome P, Francque S, Harrison S, et al. Effect of semaglutide on liver enzymes and markers of inflammation in subjects with type 2 diabetes and/or obesity. Aliment Pharmacol Ther. 2019;50(2):193‐203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Newsome PN, Buchholtz K, Cusi K, et al. A placebo‐controlled trial of subcutaneous semaglutide in nonalcoholic steatohepatitis. N Engl J Med. 2020. 10.1056/NEJMoa2028395. [DOI] [PubMed] [Google Scholar]
- 129. Hartman ML, Sanyal AJ, Loomba R, et al. Effects of novel dual GIP and GLP‐1 receptor agonist tirzepatide on biomarkers of nonalcoholic steatohepatitis in patients with type 2 diabetes. Diabetes Care. 2020;43(6):1352‐1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Ambery P, Parker VE, Stumvoll M, et al. MEDI0382, a GLP‐1 and glucagon receptor dual agonist, in obese or overweight patients with type 2 diabetes: a randomised, controlled, double‐blind, ascending dose and phase 2a study. Lancet. 2018;391(10140):2607‐2618. [DOI] [PubMed] [Google Scholar]
- 131. Boland ML, Laker RC, Mather K, et al. Resolution of NASH and hepatic fibrosis by the GLP‐1R/GcgR dual‐agonist cotadutide via modulating mitochondrial function and lipogenesis. Nat Metab. 2020;2(5):413‐431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Sánchez‐Garrido MA, Brandt SJ, Clemmensen C, Müller TD, DiMarchi RD, Tschöp MH. GLP‐1/glucagon receptor co‐agonism for treatment of obesity. Diabetologia. 2017;60(10):1851‐1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Barchetta I, Ceccarelli V, Cimini FA, et al. Circulating dipeptidyl peptidase‐4 is independently associated with the presence and severity of NAFLD/NASH in individuals with and without obesity and metabolic disease. J Endocrinol Invest. 2020. 10.1007/s40618-020-01392-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Firneisz G, Varga T, Lengyel G, et al. Serum dipeptidyl peptidase‐4 activity in insulin resistant patients with non‐alcoholic fatty liver disease: a novel liver disease biomarker. PLoS One. 2010;5(8):e12226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Itou M, Kawaguchi T, Taniguchi E, Sata M. Dipeptidyl peptidase‐4: a key player in chronic liver disease. World J Gastroenterol. 2013;19(15):2298‐2306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Alam S, Ghosh J, Mustafa G, Kamal M, Ahmad N. Effect of sitagliptin on hepatic histological activity and fibrosis of nonalcoholic steatohepatitis patients: a 1‐year randomized control trial. Hepat Med. 2018;10:23‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Gallwitz B. Clinical use of DPP‐4 inhibitors. Front Endocrinol. 2019;10:389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Eriksson JW, Lundkvist P, Jansson PA, et al. Effects of dapagliflozin and n‐3 carboxylic acids on non‐alcoholic fatty liver disease in people with type 2 diabetes: a double‐blind randomised placebo‐controlled study. Diabetologia. 2018;61(9):1923‐1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Kuchay MS, Krishan S, Mishra SK, et al. Effect of empagliflozin on liver fat in patients with type 2 diabetes and nonalcoholic fatty liver disease: a randomized controlled trial (E‐LIFT trial). Diabetes Care. 2018;41(8):1801‐1808. [DOI] [PubMed] [Google Scholar]
- 140. Kahl S, Gancheva S, Straßburger K, et al. Empagliflozin effectively lowers liver fat content in well‐controlled type 2 diabetes: a randomized, double‐blind, phase 4, placebo‐controlled trial. Diabetes Care. 2020;43(2):298‐305. [DOI] [PubMed] [Google Scholar]
- 141. Pereira MJ, Eriksson JW. Emerging role of SGLT‐2 inhibitors for the treatment of obesity. Drugs. 2019;79:219‐230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Danne T, Garg S, Peters AL, et al. International consensus on risk management of diabetic ketoacidosis in patients with type 1 diabetes treated with sodium–glucose cotransporter (SGLT) inhibitors. Diabetes Care. 2019;42(6):1147‐1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Athyros VG, Katsiki N, Karagiannis A. Editorial: can glucagon like peptide 1 (GLP1) agonists or sodium‐glucose co‐transporter 2 (SGLT2) inhibitors ameliorate non‐alcoholic steatohepatitis in people with or without diabetes? Curr Vasc Pharmacol. 2016;14(6):494‐497. [DOI] [PubMed] [Google Scholar]
- 144. Tang W, Xu Q, Hong T, et al. Comparative efficacy of anti‐diabetic agents on nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus: a systematic review and meta‐analysis of randomized and non‐randomized studies. Diabetes Metab Res Rev. 2016;32(2):200‐216. [DOI] [PubMed] [Google Scholar]
- 145. Han CY. Update on FXR biology: promising therapeutic target? Int J Mol Sci. 2018;19(7):2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Lefebvre P, Cariou B, Lien F, Kuipers F, Staels B. Role of bile acids and bile acid receptors in metabolic regulation. Physioll Rev. 2009;89(1):147‐191. [DOI] [PubMed] [Google Scholar]
- 147. Bechmann LP, Kocabayoglu P, Sowa JP, et al. Free fatty acids repress small heterodimer partner (SHP) activation and adiponectin counteracts bile acid‐induced liver injury in superobese patients with nonalcoholic steatohepatitis. Hepatology. 2013;57(4):1394‐1406. [DOI] [PubMed] [Google Scholar]
- 148. Younossi ZM, Ratziu V, Loomba R, et al. Obeticholic acid for the treatment of non‐alcoholic steatohepatitis: interim analysis from a multicentre, randomised, placebo‐controlled phase 3 trial. Lancet. 2019;394(10215):2184‐2196. [DOI] [PubMed] [Google Scholar]
- 149. Neuschwander‐Tetri BA, Loomba R, Sanyal AJ, et al. Farnesoid X nuclear receptor ligand obeticholic acid for non‐cirrhotic, non‐alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo‐controlled trial. Lancet. 2015;385(9972):956‐965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Pockros PJ, Fuchs M, Freilich B, et al. CONTROL: a randomized phase 2 study of obeticholic acid and atorvastatin on lipoproteins in nonalcoholic steatohepatitis patients. Liver Int. 2019;39(11):2082‐2093. [DOI] [PubMed] [Google Scholar]
- 151. Traussnigg S, Schattenberg JM, Demir M, et al. Norursodeoxycholic acid versus placebo in the treatment of non‐alcoholic fatty liver disease: a double‐blind, randomised, placebo‐controlled, phase 2 dose‐finding trial. Lancet Gastroenterol Hepatol. 2019;4(10):781‐793. [DOI] [PubMed] [Google Scholar]
- 152. Harrison SA, Rinella ME, Abdelmalek MF, et al. NGM282 for treatment of non‐alcoholic steatohepatitis: a multicentre, randomised, double‐blind, placebo‐controlled, phase 2 trial. Lancet. 2018;391(10126):1174‐1185. [DOI] [PubMed] [Google Scholar]
- 153. Loomba R, Sirlin CB, Ang B, et al. Ezetimibe for the treatment of nonalcoholic steatohepatitis: assessment by novel magnetic resonance imaging and magnetic resonance elastography in a randomized trial (MOZART trial). Hepatology. 2015;61(4):1239‐1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Loomba R, Kayali Z, Noureddin M, et al. GS‐0976 reduces hepatic steatosis and fibrosis markers in patients with nonalcoholic fatty liver disease. Gastroenterology. 2018;155(5):1463‐1473.e1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Harrison SA, Bashir MR, Guy CD, et al. Resmetirom (MGL‐3196) for the treatment of non‐alcoholic steatohepatitis: a multicentre, randomised, double‐blind, placebo‐controlled, phase 2 trial. Lancet. 2019;394(10213):2012‐2024. [DOI] [PubMed] [Google Scholar]
- 156. Tanaka N, Kimura T, Fujimori N, Nagaya T, Komatsu M, Tanaka E. Current status, problems, and perspectives of non‐alcoholic fatty liver disease research. World J Gastroenterol. 2019;25(2):163‐177. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supporting Information
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


