Abstract
EUS-guided biliary drainage (EUS-BD) has emerged as an alternative to ERCP for distal biliary obstruction in expert hands. Various routes for EUS-guided access in distal biliary obstruction include EUS choledochoduodenostomy, EUS-guided rendezvous, and EUS-antegrade (EUS-AG) stent placement. While percutaneous transhepatic biliary drainage and ERCP are established modalities in management of malignant hilar biliary obstruction, the role of EUS-BD is emerging. Various methods of drainage in hilar obstruction include EUS hepaticogastrostomy, EUS hepaticoduodenostomy, EUS-guided bridging stent placement, and combined ERCP and EUS-guided biliary drainage. In this review, we discuss the role of EUS-BD in malignant hilar biliary obstruction with the currently available evidence, along with the limitations and challenges to the use of this modality in management of these patients.
Keywords: biliary drainage, EUS, hilar biliary obstruction, neoplasms
INTRODUCTION
ERCP is the primary modality for biliary drainage (BD) in hilar biliary obstruction secondary to benign and malignant conditions. Percutaneous transhepatic biliary drainage (PTBD) is the alternative in patients with obstruction in the proximal biliary tree and for those with failed ERCP.[1] EUS-BD was first described in 2001 by Giovanni et al., where choledochoduodenostomy was done with placement of a plastic stent in the common bile duct.[2] EUS-guided hepaticogastrostomy (EUS-HGS) was subsequently described in 2003 by Burmester et al. in a patient with Billroth II reconstruction.[3] EUS-BD is being increasingly used by experts as an alternative to PTBD in settings of failed ERCP in patients with distal biliary obstruction.[4] A recent meta-analysis by Jin et al. which included 4 comparative trials and over 300 patients showed that EUS-BD had similar efficacy (~95%) to ERCP as primary palliation for distal biliary obstruction, with similar rates of adverse events in expert hands.[5] EUS-BD had clinical advantages of reduced risk of pancreatitis, tumor ingrowth, or stent dysfunction. Another meta-analysis which included 10 studies (3 randomized and 7 retrospective) also showed comparable efficacy of EUS-BD to ERCP with similar rates of adverse events when used as primary modality for palliation.[6] However, data of EUS-BD in patients with hilar biliary obstruction are sparse with increasing use of this modality by experts. We hereby review the currently available literature on EUS-BD in patients with hilar biliary obstruction.
PRINCIPLES OF BILIARY DRAINAGE IN HILAR OBSTRUCTION
ERCP is the standard of care for BD. Previous studies suggested that draining more than 33% of the liver should suffice in patients with preserved liver function, while draining more than 50% was needed in patients with impaired liver function.[7] A previous multicenter study from France on assessment of BD by liver volumetry suggested that draining more than 50% of the liver was associated with improved survival than those with lesser than 50% volume of liver drained (119 vs. 59 days) in malignant hilar biliary obstruction.[8] Seventy-one percent is the optimal volume of liver to be drained for adequate chemotherapy to be given in patients with malignant hilar obstruction.[9]
A previous randomized trial demonstrated that bilateral drainage of liver was better than unilateral drainage, especially in higher blocks, with respect to clinical success, need for re-interventions, and median stent patency.[10] Xia et al. in their parallel multicenter study defined the optimal strategy for hilar biliary obstruction. They found that bilateral metal stent placement was better than unilateral with respect to patency, re-intervention, and overall survival. Metal stents were better than plastic with respect to clinical success, with rates being 98.9%, 83.5%, 71.4%, and 65.4% in the bilateral metal, unilateral metal, bilateral plastic, and unilateral plastic groups, respectively. Furthermore, rates of postprocedure cholangitis were much higher in the plastic stent group.[11] Bilateral metal stent placement can be achieved by side-by-side (SBS) placement or stent-in-stent (SIS) deployment. Naitoh et al. demonstrated that SBS was associated with higher patency, however, with increased risk of complications.[12] On the other hand, in a prospective randomized control trial, Lee et al. demonstrated similar efficacy and adverse event rates between SBS and SIS, with marginal increase in stent patency in the SIS group without statistical significance.[13] Endoscopic stent placement in complex anatomies is challenging, and PTBD has been the alternative for patients in this setting. However, EUS-BD may be a single-step procedure which can be used as stand-alone or add-on to other modalities for BD [Table 1].
Table 1.
Types of EUS-guided biliary drainage based on level of biliary obstruction
| Level of block | Type of EUS-BD |
|---|---|
| Distal biliary obstruction | CDS |
| HGS | |
| EUS-AG stenting | |
| EUS-RV in failed ERCP via left hepatic duct puncture | |
| Hilar biliary obstruction with communicating systems | HGS |
| HDS | |
| EUS-RV in failed ERCP via left hepatic duct puncture | |
| Hilar biliary obstruction with noncommunicating systems | Bridging procedure (HGS with stent placement draining right to left) |
| CERES (can include EUS-HGS with right biliary SEMS via ERCP or EUS-HDS with left biliary SEMS via ERCP) |
BD: Biliary drainage; CDS: Choledochoduodenostomy; HGS: Hepaticogastrostomy; AG: Antegrade; RV: Rendezvous; HDS: Hepaticoduodenostomy; CERES: Combined ERCP with EUS; SEMS: Self-expandable metal stent
EUS-BILIARY DRAINAGE IN HILAR BILIARY OBSTRUCTION – TECHNIQUES AND CHALLENGES
EUS-BD is indicated in patients who have failed ERCP or in situations where ERCP may not be feasible (surgically altered anatomy). In patients who have a failed re-intervention of occluded transpapillary stents, EUS-BD can be considered. EUS-BD is mainly used for inoperable patients, although EUS-rendezvous (EUS-RV) can be done in the preoperative setting. While EUS-BD can use intrahepatic and extrahepatic approaches, in case of hilar obstruction intrahepatic access is a must.[14] Unlike in ERCP, eventually, EUS-BD may use a route that may or may not traverse the stricture. Contraindications to EUS-BD are gross ascites, intervening blood vessels, coagulopathy, and patients unfit for endoscopic procedures.
The techniques used for drainage include EUS-HGS, EUS-guided hepaticoduodenostomy (EUS-HDS), bridging method, or a combination of ERCP and EUS (CERES).[15] The objective of all these modalities is to ensure the maximum volume of the liver is drained. In patients with right and left systems communicating with one another (Type I or II block), a single stent may suffice. In these situations, isolated EUS-HGS may be tried. EUS-HGS involves accessing the left hepatic duct through segment II or III. Covered metal stent is placed across the tract for draining the entire liver [Figures 1 and 2]. Giobor stent (Taewoong Medical Inc., South Korea), which has a variable segment of covered and uncovered portion, can also be used for EUS-HGS. On the other hand, EUS-HDS involves draining the right lobe of liver with puncture through the lateral wall of the duodenum [Figure 3]. Fully covered metal stent is placed across the tract. EUS-HGS and EUS-HDS are both modalities of intrahepatic BD. In patients where the right and left systems were noncommunicating, bridging technique can be used. This involves placement of an uncovered stent between the right and left systems to establish drainage into the left system. EUS-HGS can then be used to drain the left system [Figure 4].
Figure 1.
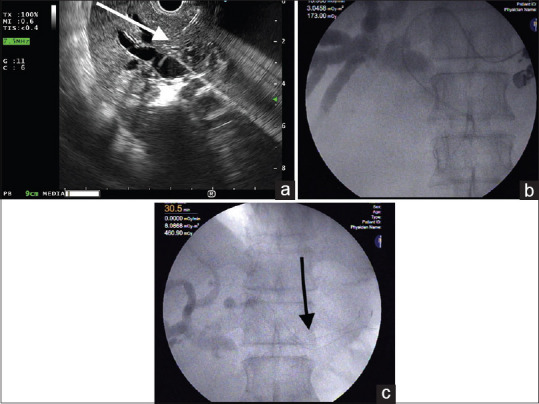
Steps of EUS-guided hepaticogastrostomy - (a) EUS-guided puncture into the segment 3 radicle in left lobe with 19G fine-needle aspiration needle (white arrow), (b) Guidewire passage into the common bile duct across the hilum, (c) Stent placement across the hepaticogastrostomy orifice created (black arrow)
Figure 2.
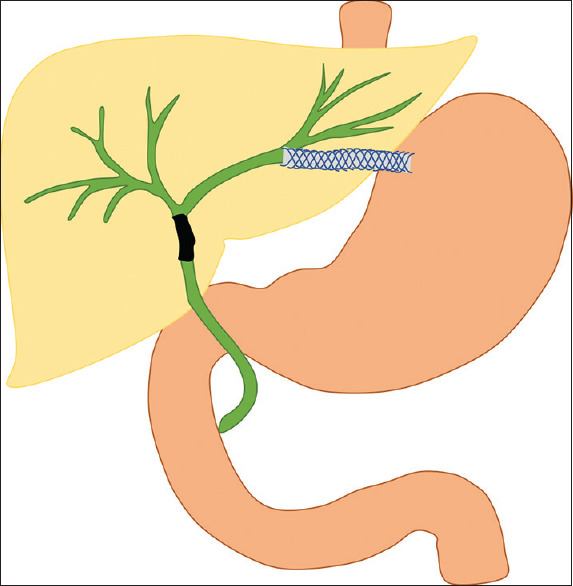
Graphical representation of EUS-guided hepaticogastrostomy
Figure 3.
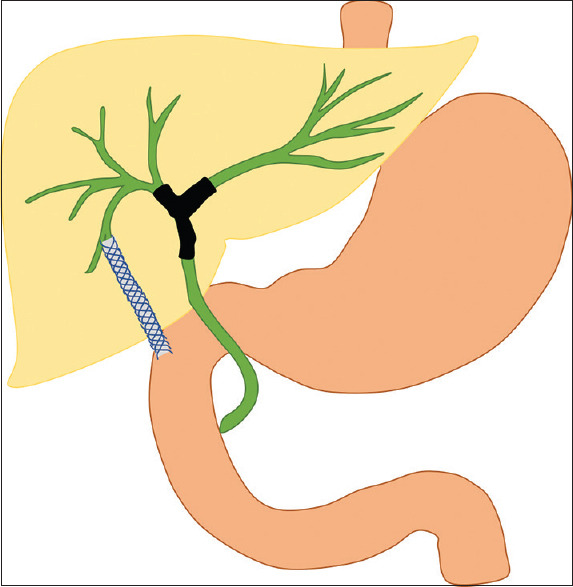
Graphical representation of EUS-guided hepaticoduodenostomy
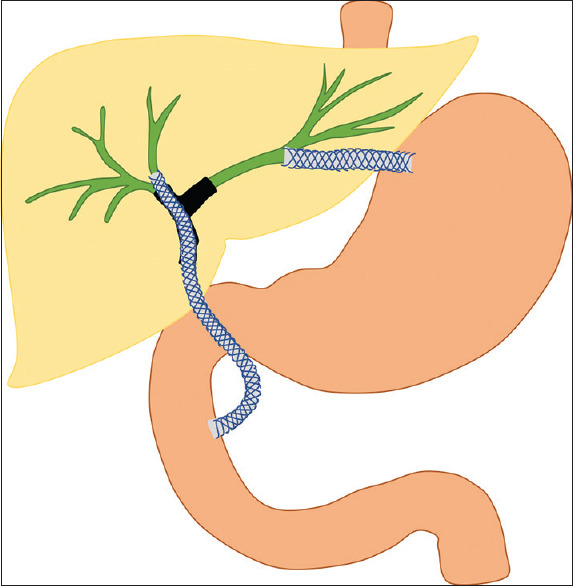
Figure 4.
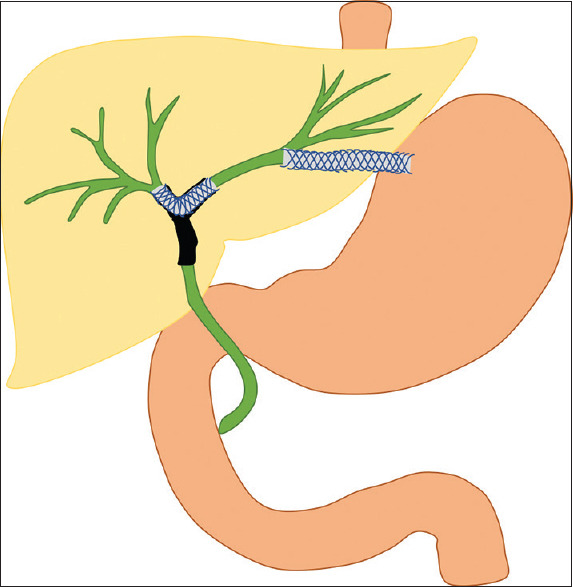
Graphical representation of EUS-guided bridging stent placement in hilar biliary obstruction with involvement of primary biliary confluence; uncovered self-expandable metal stent placed bridging the right and left systems with covered self-expandable metal stents placed across the EUS-HGS
CERES involves CERES for BD [Figure 5]. In patients where through the papilla the right system is accessed and drained, EUS-HGS can be used for draining the left system. On the other hand, where the left system is drained through the papilla, EUS-HDS can be used to access the right system. This is mainly done in situations where the right and left systems are noncommunicating. ERCP is usually attempted first in these situations in an attempt to ensure transpapillary drainage. EUS-BD is added when one system cannot be accessed through ERCP.
Figure 5.
Graphical representation of combined ERCP and EUS-guided biliary drainage in patients with hilar obstruction with involvement of primary biliary confluence; uncovered self-expandable metal stent placed via transpapillary route into the right hepatic duct and the left lobe drained using EUS-guided hepaticogastrostomy
EUS-RV can also be done in situations with failed ERCP through the transgastric route for proximal biliary obstruction. The left system can be punctured and a guidewire passed across the papilla. The scope is then exchanged to duodenoscope, and ERCP is performed by using the same guidewire for access.[16] EUS-antegrade (EUS-AG) stent placement can be done for patients with Type I Bismuth block with communicating systems, with single-stent placement through the left system. However, technical success is lower (77%) due to challenges in distal guidewire passage.[17]
EFFICACY OF EUS-BILIARY DRAINAGE IN MALIGNANT HILAR BILIARY OBSTRUCTION
No previous meta-analysis is available on the EUS-BD in hilar biliary obstruction. However, multiple case reports and retrospective series are available [Table 2]. The first large series was described by Bories et al. in 2007, which included 11 patients with failed ERCP for hilar biliary obstruction (8 malignant and 3 benign). Ten out of 11 (90.9%) patients successfully underwent EUS-HGS in this series, with placement of plastic and metal stents in 7 and 3 patients, respectively. The mean duration of follow-up was 213 days, with clinical success in 10 cases.[18] Ogura et al. described a series of 11 patients with obstructed right duct for which EUS-HDS (4/11) or bridging stent placement (7/11) was done.[19] Technical and clinical successes were achieved in all patients. Ogura et al. in another series described EUS-BD as a rescue after failed ERCP in 10 patients, with EUS-HGS in 8 patients and EUS-HDS in 2 patients.[20] Technical success was achieved in all patients; however, functional success was achieved in 90%. In another series by Moryoussef et al. in 2017, 18 patients with failed ERCP either due to surgical anatomy, impassable strictures, or duodenal stenosis with hilar biliary obstruction underwent EUS-HGS (14/18) or bridging stent placement (3/18).[21] Technical success was 94% with clinical success being 72% at 1 week and 68% at 30 days. The re-intervention rate was 16.4%. The type of block was Type I/II in 47%, Type III in 47%, and Type 4 in 6%. This may be the reason for the lower rate of clinical success.
Table 2.
Major studies of EUS-guided biliary drainage in hilar biliary obstruction
| Authors | Number of patients Mode of drainage | Technical success/clinical success | Adverse effects |
|---|---|---|---|
| Bories et al.[18] |
n=11 All HGS |
Technical and clinical 10/11 (90.9%) (7 plastic stents and 3 SEMS) | 1 stent block 1 transient ileus 1 biloma 1 cholangitis |
| Ogura et al.[19] |
n=11 7 bridging, 4 HDS |
Technical and clinical 11/11 (100%) | None |
| Ogura et al.[20] |
n=10 8 HGS, 2 HDS |
Technical success 10/10 (100%) Clinical success 90% |
None |
| Moryoussef et al.[21] |
n=18 18/18 HGS |
Technical success 17/18 (94.4%) Clinical success 72.2% (early - 7 days)/68% (late - 30 days) |
3/18 (16.7%) 1 severe hemorrhage 1 stent obstruction 1 stent migration |
| Minaga et al.[22] |
n=30 HGS 28/30, HDS 2/30 |
Technical success 29/30 (96.6%) Clinical success 22/29 (75.9%) |
Early - 10% (3/30) (mild peritonitis managed conservatively) Late - 23.3% (7/30) (cholangitis due to stent dysfunction) |
| Kongkam et al.[24] |
n=36 CERES (19) versus PTBD (17) ERCP+HGS=17 ERCP+HDS=1 ERCP+HGS+HDS=1 |
Technical success - CERES 84% (16/19) versus PTBD 100% (P<0.05) Clinical success - CERES 78.9% (15/19) versus 76.5% (13/17) |
CERES 26.3% (5/19) versus PTBD 35.5% (6/17) (P=0.56) Median time to re-intervention - CERES 92 days versus PTBD 40 days (P=0.006) Recurrent biliary obstruction at 3 and 6 months - CERES 26.7% and 22.2% versus PTBD 88.2% and 100% (P<0.01) |
HGS: Hepaticogastrostomy; SEMS: Self-expandable metal stent; HDS: Hepaticoduodenostomy; PTBD: Percutaneous transhepatic biliary drainage; CERES: Combined ERCP with EUS
The largest series of malignant hilar biliary obstruction managed using EUS-BD after failed ERCP for re-intervention was described by Minaga et al. in 2017. In their series of 30 patients, 40% had Type IV block, 43.3% had Type III block, and 16.6% had Type II block.[22] Technical success was 96.6% and clinical success in those with technical success was 75.4%. In this series, 28 patients underwent EUS-HGS and 2 patients underwent EUS-HDS. Bismuth Type IV block was the only factor associated with clinical ineffectiveness of EUS-BD on multivariate analysis. Stent patency was only 62.5 days, considering that the study included patients with advanced disease. A recent review on the efficacy of all types of EUS-BD showed a technical success rate of 91%, a clinical success rate of 86%, and a complication rate of 17%.[23]
Kongkam et al. in their series of CERES showed a technical success rate of 90%, a clinical success rate of 81%, and a complication rate of 18%.[15] In an open-label multicenter comparative study from Thailand, CERES had similar technical success, clinical success, and complication rates as compared to bilateral PTBD in patients with advanced hilar biliary obstruction (Bismuth Type III and IV). However, the risk of recurrent biliary obstruction and re-intervention was significantly lower in patients with CERES. The median period before development of recurrent biliary obstruction was 92 days and 40 days for CERES and bilateral PTBD, respectively (P = 0.006).[24] Although there are multiple studies on EUS-RV in patients with primarily distal biliary obstruction, no large-scale data in hilar obstruction is available.[16,25,26]
SAFETY OF EUS-BILIARY DRAINAGE IN MALIGNANT HILAR BILIARY OBSTRUCTION
Complications are known to occur in 8% of patients who undergo EUS-BD for hilar biliary obstruction.[14] In a previous study of 68 patients, complications are more likely to occur via the transhepatic route than the transduodenal route. Complications, although more common in proximal biliary obstruction than distal obstruction, did not reach significance.[27] Biliary peritonitis can occur during EUS-HGS and EUS-HDS. Hemorrhage can occur if there is an inadvertent intrahepatic vascular injury during the procedure. Stent malfunction occurs in 16%–23% of patients, needing re-intervention. The reasons include shortening, migration, or obstruction of the stent. Intraperitoneal stent migration may rarely occur, needing urgent surgical intervention. Mortality may occur due to complications of stent malfunction. Most of these procedures are done by experts, and there is a risk of publication bias with respect to complications.
Nakai et al. showed that in their series of 96 patients, the rate of recurrent biliary obstruction was 36% after a median duration of 6.8 months post EUS-BD. Of these, majority were EUS-HGS procedures. The cause was nontumor related with tissue hyperplasia, stent migration, sludge, and de novo stricture. Re-intervention was successful via EUS-BD that was performed in 89%.[28]
COMPARISON OF EUS-BILIARY DRAINAGE WITH PERCUTANEOUS TRANSHEPATIC BILIARY DRAINAGE
No comparative trials are available between EUS-BD and PTBD in hilar obstruction. However, EUS-BD has the benefits of a single-step procedure with likely longer stent patency as chances of ingrowth are lesser. However, technical factors including endoscopic expertise are a major factor determining success. PTBD, on the other hand, is associated with high technical success and clinical success. However, there is impaired quality of life with increased risk of hemobilia, cholangitis, and neoplastic seeding with increased re-intervention.[29]
Limitations
While EUS-BD seems attractive in patients with hilar biliary obstruction, there is a steep learning curve which poses a major challenge to routine use of these procedures. Various models such as the Mumbai EUS stereolithography/three-dimensional printing bile duct prototype and the Thai TAGE II model have been used for training in EUS-BD.[30,31] Major limitations also include the increased risk of complications, especially with the transhepatic approach, and the possibility of inadequate BD in higher blocks. Hence, these procedures should be performed by expert endoscopists in high-volume centers.
CONCLUSIONS
EUS-BD in patients with malignant hilar biliary obstruction is an alternative to PTBD in settings after failed ERCP or in postsurgical anatomy in expert hands. EUS-BD offers excellent technical success and reasonable clinical success with risk of complications such as biliary peritonitis and stent malfunction. Larger trials comparing EUS-BD in hilar biliary obstruction with transpapillary modalities are needed. In majority of cases, ERCP or EUS-BD or their combination will provide adequate BD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank Dr. Suprabhat Giri for assistance with making the illustrations for the manuscript.
REFERENCES
- 1.Moole H, Dharmapuri S, Duvvuri A, et al. Endoscopic versus percutaneous biliary drainage in palliation of advanced malignant hilar obstruction: A meta-analysis and systematic review. [Epub 2016 Aug 25];Can J Gastroenterol Hepatol 2016. 2016 doi: 10.1155/2016/4726078. 4726078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giovannini M, Moutardier V, Pesenti C, et al. Endoscopic ultrasound-guided bilioduodenal anastomosis: A new technique for biliary drainage. Endoscopy. 2001;33:898–900. doi: 10.1055/s-2001-17324. [DOI] [PubMed] [Google Scholar]
- 3.Burmester E, Niehaus J, Leineweber T, et al. EUS-cholangio-drainage of the bile duct: Report of 4 cases. Gastrointest Endosc. 2003;57:246–51. doi: 10.1067/mge.2003.85. [DOI] [PubMed] [Google Scholar]
- 4.Hathorn KE, Bazarbashi AN, Sack JS, et al. EUS-guided biliary drainage is equivalent to ERCP for primary treatment of malignant distal biliary obstruction: A systematic review and meta-analysis. Endosc Int Open. 2019;7:E1432–41. doi: 10.1055/a-0990-9488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jin Z, Wei Y, Lin H, et al. Endoscopic ultrasound-guided versus endoscopic retrograde cholangiopancreatography-guided biliary drainage for primary treatment of distal malignant biliary obstruction: A systematic review and meta-analysis. Dig Endosc. 2020;32:16–26. doi: 10.1111/den.13456. [DOI] [PubMed] [Google Scholar]
- 6.Han SY, Kim SO, So H, et al. EUS-guided biliary drainage versus ERCP for first-line palliation of malignant distal biliary obstruction: A systematic review and meta-analysis. Sci Rep. 2019;9:16551. doi: 10.1038/s41598-019-52993-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takahashi E, Fukasawa M, Sato T, et al. Biliary drainage strategy of unresectable malignant hilar strictures by computed tomography volu- metry. World J Gastroenterol. 2015;21:4946–53. doi: 10.3748/wjg.v21.i16.4946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vienne A, Hobeika E, Gouya H, et al. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: The role of liver volume assessment. Gastrointest Endosc. 2010;72:728–35. doi: 10.1016/j.gie.2010.06.040. [DOI] [PubMed] [Google Scholar]
- 9.Caillol F, Bories E, Zemmour C, et al. Palliative endoscopic drainage of malignant stenosis of biliary confluence: Efficiency of multiple drainage approach to drain a maximum of liver segments. United European Gastroenterol J. 2019;7:52–9. doi: 10.1177/2050640618803812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee TH, Kim TH, Moon JH, et al. Bilateral versus unilateral placement of metal stents for inoperable high-grade malignant hilar biliary strictures: A multicenter, prospective, randomized study (with video) Gastrointest Endosc. 2017;86:817–27. doi: 10.1016/j.gie.2017.04.037. [DOI] [PubMed] [Google Scholar]
- 11.Xia MX, Cai XB, Pan YL, et al. Optimal stent placement strategy for malignant hilar biliary obstruction: A large multicenter parallel study. Gastrointest Endosc. 2020;91:1117–280. doi: 10.1016/j.gie.2019.12.023. [DOI] [PubMed] [Google Scholar]
- 12.Naitoh I, Hayashi K, Nakazawa T, et al. Side-by-side versus stent-in-stent deployment in bilateral endoscopic metal stenting for malignant hilar biliary obstruction. Dig Dis Sci. 2012;57:3279–85. doi: 10.1007/s10620-012-2270-9. [DOI] [PubMed] [Google Scholar]
- 13.Lee TH, Moon JH, Choi JH, et al. Prospective comparison of endoscopic bilateral stent-in-stent versus stent-by-stent deployment for inoperable advanced malignant hilar biliary stricture. Gastrointest Endosc. 2019;90:222–30. doi: 10.1016/j.gie.2019.03.011. [DOI] [PubMed] [Google Scholar]
- 14.Nakai Y, Kogure H, Isayama H, et al. Endoscopic ultrasound-guided biliary drainage for unresectable hilar malignant biliary obstruction. Clin Endosc. 2019;52:220–5. doi: 10.5946/ce.2018.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kongkam P, Tasneem AA, Rerknimitr R. Combination of endoscopic retrograde cholangiopancreatography and endoscopic ultrasonography-guided biliary drainage in malignant hilar biliary obstruction. Dig Endosc. 2019;31(Suppl 1):50–4. doi: 10.1111/den.13371. [DOI] [PubMed] [Google Scholar]
- 16.Kawakubo K, Isayama H, Sasahira N, et al. Clinical utility of an endoscopic ultrasound-guided rendezvous technique via various approach routes. Surg Endosc. 2013;27:3437–43. doi: 10.1007/s00464-013-2896-5. [DOI] [PubMed] [Google Scholar]
- 17.Iwashita T, Doi S, Yasuda I. Endoscopic ultrasound-guided biliary drainage: A review. Clin J Gastroenterol. 2014;7:94–102. doi: 10.1007/s12328-014-0467-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bories E, Pesenti C, Caillol F, et al. Transgastric endoscopic ultrasonography-guided biliary drainage: Results of a pilot study. Endoscopy. 2007;39:287–91. doi: 10.1055/s-2007-966212. [DOI] [PubMed] [Google Scholar]
- 19.Ogura T, Sano T, Onda S, et al. Endoscopic ultrasound-guided biliary drainage for right hepatic bile duct obstruction: Novel technical tips. Endoscopy. 2015;47:72–5. doi: 10.1055/s-0034-1378111. [DOI] [PubMed] [Google Scholar]
- 20.Ogura T, Onda S, Takagi W, et al. Clinical utility of endoscopic ultrasound-guided biliary drainage as a rescue of re-intervention procedure for high-grade hilar stricture. J Gastroenterol Hepatol. 2017;32:163–8. doi: 10.1111/jgh.13437. [DOI] [PubMed] [Google Scholar]
- 21.Moryoussef F, Sportes A, Leblanc S, et al. Is EUS-guided drainage a suitable alternative technique in case of proxi- mal biliary obstruction? Therap Adv Gastroenterol. 2017;10:537–544. doi: 10.1177/1756283X17702614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Minaga K, Takenaka M, Kitano M, et al. Rescue EUS-guided intrahepatic biliary drainage for malignant hilar biliary stricture after failed transpapillary re-intervention. Surg Endosc. 2017;31:4764–72. doi: 10.1007/s00464-017-5553-6. [DOI] [PubMed] [Google Scholar]
- 23.Rimbaş M, Larghi A. Endoscopic ultrasonography-guided techniques for accessing and draining the biliary system and the pancreatic duct. Gastrointest Endosc Clin N Am. 2017;27:681–705. doi: 10.1016/j.giec.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 24.Kongkam P, Orprayoon T, Boonmee C, et al. ERCP plus endoscopic ultrasound-guided biliary drainage versus percutaneous transhepatic biliary drainage for malignant hilar biliary obstruction: A multicenter observational open-label study. Endoscopy. 2021;53:55–62. doi: 10.1055/a-1195-8197. [DOI] [PubMed] [Google Scholar]
- 25.Dhir V, Bhandari S, Bapat M, et al. Comparison of EUS-guided rendezvous and precut papillotomy techniques for biliary access (with videos) Gastrointest Endosc. 2012;75:354–9. doi: 10.1016/j.gie.2011.07.075. [DOI] [PubMed] [Google Scholar]
- 26.Iwashita T, Lee JG, Shinoura S, et al. Endoscopic ultrasound-guided rendezvous for biliary access after failed cannulation. Endoscopy. 2012;44:60–5. doi: 10.1055/s-0030-1256871. [DOI] [PubMed] [Google Scholar]
- 27.Dhir V, Artifon EL, Gupta K, et al. Multicenter study on endoscopic ultrasound-guided expandable biliary metal stent placement: Choice of access route, direction of stent insertion, and drainage route. Dig Endosc. 2014;26:430–5. doi: 10.1111/den.12153. [DOI] [PubMed] [Google Scholar]
- 28.Nakai Y, Ito Y, Yagioka H, et al. OR-THER-04: Long-term outcomes and reintervention of endoscopic ultrasound-guided biliary drainage for malignant biliary obstruction: A multicenter retrospective analysis of 96 cases. Endosc Ultrasound. 2017;6(Suppl 1):S8. [Google Scholar]
- 29.Wang L, Lin N, Xin F, et al. A systematic review of the comparison of the incidence of seeding metastasis between endoscopic biliary drainage and percutaneous transhepatic biliary drainage for resectable malignant biliary obstruction. World J Surg Oncol. 2019;17:116. doi: 10.1186/s12957-019-1656-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dhir V, Itoi T, Fockens P, et al. Novel ex vivo model for hands-on teaching of and training in EUS-guided biliary drainage: Creation of “Mumbai EUS” stereolithography/3D printing bile duct prototype (with videos) Gastrointest Endosc. 2015;81:440–6. doi: 10.1016/j.gie.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 31.Siripun A, Chantarojanasiri T, Ratanachuek T, et al. Su1276 development of non-fluoroscopic, all-artificial model for endoscopic ultrasound guided biliary drainage training (TAGE-2) Gastrointest Endosc. 2020;91:AB306–7. [Google Scholar]


