Abstract
Aim
Controversies on therapeutic strategy for large bowel obstruction by primary colorectal cancer mainly concern acute conditions, being essentially different from subacute obstruction. Clearly defining acute obstruction is important for design and interpretation of studies as well as for guidelines and daily practice. This systematic review aimed to evaluate definitions of obstruction by colorectal cancer in prospective studies.
Method
A systematic search was performed in PubMed, Embase and the Cochrane Library. Eligibility criteria included randomized or prospective observational design, publication between 2000 and 2019, and the inclusion of patients with an obstruction caused by colorectal cancer. Provided definitions of obstruction were extracted with assessment of common elements.
Results
A total of 16 randomized controlled trials (RCTs) and 99 prospective observational studies were included. Obstruction was specified as acute in 28 studies, complete/emergency in five, (sub)acute or similar terms in four and unspecified in 78. Five of 16 RCTs (31%) and 37 of 99 cohort studies (37%) provided a definition. The definitions included any combination of clinical symptoms, physical signs, endoscopic features and radiological imaging findings in 25 studies. The definition was only based on clinical symptoms in 11 and radiological imaging in six studies. Definitions included a radiological component in 100% of evaluable RCTs (5/5) vs. 54% of prospective observational studies (20/37, P = 0.07).
Conclusion
In this systematic review, the majority of prospective studies did not define obstruction by colorectal cancer and its urgency, whereas provided definitions varied hugely. Radiological confirmation seems to be an essential component in defining acute obstruction.
INTRODUCTION
Approximately 10% of patients with colorectal cancer present with acute large bowel obstruction. Different incidences have been reported [1], as the severity or degree of obstruction varies substantially and may significantly influence clinical decision‐making. Complete obstruction may lead to extensive bowel dilatation, even leading to caecal blow‐out, which increases the urgency of surgery or placement of a colonic self‐expandable metal stent (SEMS). In contrast, incomplete or imminent obstruction may allow for more conservative treatment including laxatives with subsequent surgery in a semi‐elective setting.
Clinical presentation of large bowel obstruction by primary colorectal cancer varies hugely in daily practice. Patients may present mainly with abdominal pain for several weeks, whereas others rapidly develop abdominal distention and might experience disproportionately mild symptoms. Conflicting results have been published regarding the degree of colorectal obstruction and SEMS success rates [2], which might be explained by variation in clinical presentation. Recently, a scoring system was developed by a Japanese group (the ColoRectal Obstruction Scoring System, CROSS) in order to evaluate the degree of colorectal obstruction and consequently aid in the choice of treatment of patients with obstructive colorectal cancer [3]. In their most recent guideline, the European Society of Gastrointestinal Endoscopy (ESGE) recommends against prophylactic SEMS placement in patients with a subacute obstruction [2], but without providing a clear definition.
A clear definition of obstruction by colorectal cancer might reduce overtreatment of patients with mild conditions, and focuses the need for emergency treatment towards patients with an acute presentation. In addition, literature on patients with obstructive colorectal cancer can be compared more effectively with more appropriate translation into clinical guidelines and daily practice. Furthermore, it enables clinical benchmarking. Therefore, the aim of this systematic review was to provide a literature overview of used definitions of obstruction by colorectal cancer in prospective studies, thereby serving as a basis for the development of a consensus definition.
METHODS
This systematic review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines [4]. No review protocol was registered.
Search strategy and data extraction
A systematic search was undertaken on MEDLINE/Pubmed, Embase and the Cochrane Library. The final search was performed on 13 March 2019. In MEDLINE/Pubmed, the following search terms were used: ((colon*[tiab] OR colorectal[tiab]) AND (cancer*[tiab] OR neoplasm*[tiab] OR malignan*[tiab]) AND obstructi*[tiab] AND english[language]). The first two authors (JV and KB) independently assessed titles and abstracts and subsequently full texts for eligibility. Reference lists of the included articles were manually cross‐searched for any additional studies. Any discrepancies were discussed and, in the case of disagreement, consensus was reached after consulting the senior author (PT).
Inclusion/exclusion criteria
Studies were included in the case of a randomized or prospective observational study design, a publication date between 1 January 2000 and 13 March 2019, and if describing patients with any sign of obstruction caused by either right‐sided colon cancer, left‐sided colon cancer or rectal cancer. Exclusion criteria were retrospective studies, reviews, letters, editorials, studies including patients <18 years old, animal studies and studies not written in English. Not providing a definition of obstructive colon cancer was not an exclusion criterion.
Outcomes of interest
Provided definitions of malignant colorectal obstruction or any related descriptions of the clinical condition and its urgency of included patients were extracted from each study. Definitions were evaluated based on whether or not they contained any of the following five elements: clinical symptoms, duration of symptoms, physical examination, endoscopic features and/or radiological imaging. Other extracted variables included study design, number of patients, terminology used for the studied clinical condition as mentioned in the Methods section, and whether or not a definition of obstructive colon cancer was provided in the Methods section.
RESULTS
Study selection
The literature search yielded a total of 6797 articles (Figure 1). After exclusion of 2768 duplicates, 4029 articles were screened on title and abstract, and 282 studies remained for full text screening. After exclusion based on study design (n = 123), 115 studies remained for final analysis including 16 randomized controlled trials (RCTs) (13.9%) and 99 prospective observational studies (86.1%). The studies are summarized in Table 1.
FIGURE 1.
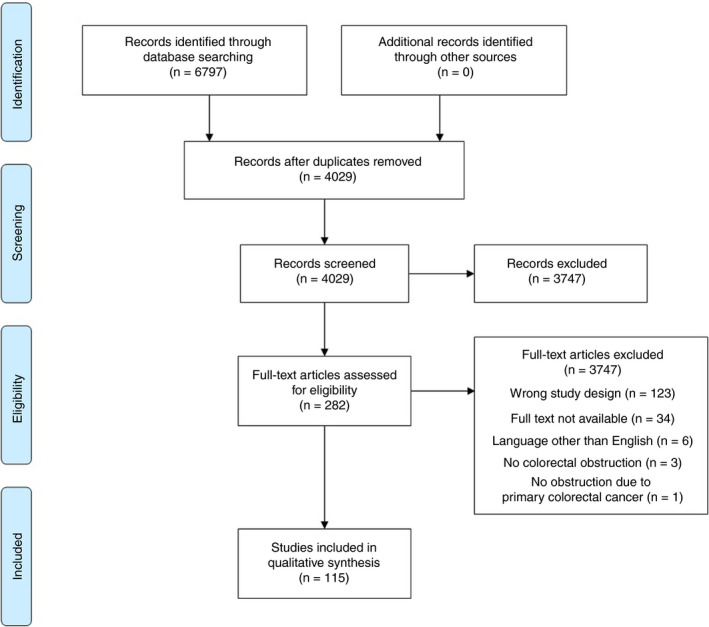
PRISMA flowchart
TABLE 1.
Study characteristics of all the included studies
| Author | Year | Title |
|---|---|---|
| Bayrak | 2019 | Stent experiences in emergency conditions in acute mechanical intestinal obstruction caused by colorectal cancer. |
| Fiori | 2018 | Endoscopic Stenting for Colorectal Cancer |
| Takahashi | 2018 | Oncological Assessment of Stent Placement for Obstructive Colorectal Cancer from Circulating Cell‐Free DNA and Circulating Tumor DNA Dynamics. |
| Yamashita | 2018 | Impact of endoscopic stent insertion on detection of viable circulating tumor cells from obstructive colorectal cancer. |
| Li | 2017 | Clinical application of transanal ileal tube placement using X‐ray monitoring. |
| Arezzo | 2016 | Colonic stenting as a bridge to surgery versus emergency surgery for malignant colonic obstruction: results of a multicentre randomised controlled trial (ESCO trial) |
| Enomoto | 2016 | Open surgery versus laparoscopic surgery after stent insertion for obstructive colorectal cancer. |
| Haraguchi | 2016 | Colonic stenting as a bridge to surgery for obstructive colorectal cancer: advantages and disadvantages. |
| Saito | 2016 | A prospective multicenter study on self‐expandable metallic stents as a bridge to surgery for malignant colorectal obstruction in Japan: efficacy and safety in 312 patients. |
| Wan | 2016 | Comparison of through‐the‐scope stent insertion with standard stent insertion for the management of malignant colorectal obstruction: a prospective study. |
| Achiam | 2015 | Perioperative Colonic Evaluation in Patients with Rectal Cancer; MR Colonography Versus Standard Care. |
| Lin | 2015 | Investigation of treatment methods in obstructive colorectal cancer. |
| Matsuzawa | 2015 | A Japanese prospective multicenter study of self‐expandable metal stent placement for malignant colorectal obstruction: short‐term safety and efficacy within 7 days of stent procedure in 513 cases. |
| Milek | 2015 | Implantation of a new enteral stent in obstructive colorectal cancer using interventional radiology in patients over 70 years of age. |
| Singh | 2015 | Role of CT Colonography in Colonic Lesions and Its Correlation with Conventional Colonoscopic Findings. |
| Young | 2015 | Improving Quality of Life for People with Incurable Large‐Bowel Obstruction: Randomized Control Trial of Colonic Stent Insertion. |
| Di Mitri | 2014 | The new nitinol conformable self‐expandable metal stents for malignant colonic obstruction: a pilot experience as bridge to surgery treatment. |
| Kamocki | 2014 | Own experiences of endoscopic self‐expandable stent placement for malignant colorectal ileus. |
| Kim | 2014 | Mmp‐9 expression after metallic stent placement in patients with colorectal cancer: association with in‐stent restenosis. |
| Kim | 2014 | Preoperative colonoscopy through the colonic stent in patients with colorectal cancer obstruction. |
| Krstic | 2014 | Hartmann's procedure vs loop colostomy in the treatment of obstructive rectosigmoid cancer. |
| Lo | 2014 | Protocol‐driven self‐expanding metallic stenting for malignant large‐bowel obstruction in a district hospital |
| Occhionorelli | 2014 | Colonic stent placement as a bridge to surgery in patients with left‐sided malignant large bowel obstruction. An observational study. |
| Ding | 2013 | A temporary self‐expanding metallic stent for malignant colorectal obstruction. |
| Ghazal | 2013 | Colonic endolumenal stenting devices and elective surgery versus emergency subtotal/total colectomy in the management of malignant obstructed left colon carcinoma. |
| Lamazza | 2013 | A new technique for placement of a self‐expanding metallic stent (SEMS) in patients with colon rectal obstruction: a prospective study of 43 patients. |
| Lee | 2013 | Novel method of stent insertion for malignant lower rectal obstruction with proximal releasing delivery system (with video). |
| Lim | 2013 | Preoperative colonoscopy for detection of synchronous neoplasms after insertion of self‐expandable metal stents in occlusive colorectal cancer: comparison of covered and uncovered stents. |
| Sumise | 2013 | Outcome of emergency one‐stage resection and anastomosis procedure for patients with obstructed colorectal cancer. |
| Warden | 2013 | Stenting as first‐line management for all patients with nonperforating left‐sided obstructing colorectal cancer. |
| Yoshida | 2013 | Feasibility of a new self‐expandable metallic stent for patients with malignant colorectal obstruction. |
| Angenete | 2012 | Stenting for colorectal cancer obstruction compared to surgery‐‐a study of consecutive patients in a single institution. |
| Bonfante | 2012 | Managing acute colorectal obstruction by "bridge stenting" to laparoscopic surgery: Our experience |
| Cennamo | 2012 | Colorectal stenting as a bridge to surgery reduces morbidity and mortality in left‐sided malignant obstruction: a predictive risk score‐based comparative study. |
| Chen | 2012 | Laparoscopic management for acute malignant colonic obstruction. |
| Cheung | 2012 | Outcome and safety of self‐expandable metallic stents for malignant colon obstruction: a Korean multicenter randomized prospective study. |
| Chou | 2012 | Dual‐design expandable colorectal stent for a malignant colorectal obstruction: preliminary prospective study using new 20‐mm diameter stents. |
| Ho | 2012 | Endoscopic stenting and elective surgery versus emergency surgery for left‐sided malignant colonic obstruction: a prospective randomized trial. |
| Inaba | 2012 | Phase II clinical study on stent therapy for unresectable malignant colorectal obstruction (JIVROSG‐0206). |
| JimenezFuertes | 2012 | Resection and primary anastomosis without diverting ileostomy for left colon emergencies: is it a safe procedure? |
| Larssen | 2012 | Long‐term outcome of palliative treatment with self‐expanding metal stents for malignant obstructions of the GI tract. |
| Meisner | 2012 | Self‐Expanding Metal Stenting for Palliation of Patients with Malignant Colonic Obstruction: Effectiveness and Efficacy on 255 Patients with 12‐Month's Follow‐up. |
| Song | 2012 | Usefulness of a guiding sheath for fluoroscopic colorectal stent placement. |
| Tominaga | 2012 | Favorable long‐term clinical outcome of uncovered D‐weave stent placement as definitive palliative treatment for malignant colorectal obstruction. |
| Yang | 2012 | Two‐stage resection for malignant colonic obstructions: the timing of early resection and possible predictive factors. |
| Alcantara | 2011 | Prospective, controlled, randomized study of intraoperative colonic lavage versus stent placement in obstructive left‐sided colonic cancer. |
| Chakraborty | 2011 | Malignant bowel obstruction: natural history of a heterogeneous patient population followed prospectively over two years. |
| Luigiano | 2011 | Through‐the‐scope large diameter self‐expanding metal stent placement as a safe and effective technique for palliation of malignant colorectal obstruction: a single center experience with a long‐term follow‐up. |
| Meisner | 2011 | Self‐expandable metal stents for relieving malignant colorectal obstruction: short‐term safety and efficacy within 30 days of stent procedure in 447 patients. |
| Milek | 2011 | Preliminary results of the use of self‐expanding nitinol stents in inoperable gastrointestinal cancers |
| Pirlet | 2011 | Emergency preoperative stenting versus surgery for acute left‐sided malignant colonic obstruction: a multicenter randomized controlled trial. |
| Sule | 2011 | Adult large bowel obstruction: a review of clinical experience. |
| van Hooft | 2011 | Colonic stenting versus emergency surgery for acute left‐sided malignant colonic obstruction: a multicentre randomised trial. |
| Williams | 2011 | Colorectal stenting in malignant large bowel obstruction: the learning curve. |
| Young | 2011 | Stenting large bowel obstruction avoids a stoma: consecutive series of 100 patients. |
| Achiam | 2010 | Differentiation between benign and malignant colon tumors using fast dynamic gadolinium‐enhanced MR colonography; a feasibility study. |
| Branger | 2010 | Management of acute malignant large‐bowel obstruction with self‐expanding metal stent. |
| Dakubo | 2010 | Colorectal carcinoma: an update of current trends in Accra. |
| Hisanaga | 2010 | Multicenter prospective study on efficacy and safety of octreotide for inoperable malignant bowel obstruction. |
| Li | 2010 | Management of acute malignant colorectal obstruction with a novel self‐expanding metallic stent as a bridge to surgery. |
| Moon | 2010 | Comparison of a newly designed double‐layered combination covered stent and D‐weave uncovered stent for decompression of obstructive colorectal cancer: a prospective multicenter study |
| Mukai | 2010 | Two‐stage treatment (Mukai's method) with hybrid 2‐port HALS (Mukai's operation) for complete bowel obstruction by left colon cancer or rectal cancer. |
| Nagula | 2010 | Quality of life and symptom control after stent placement or surgical palliation of malignant colorectal obstruction. |
| Park | 2010 | Comparison of efficacies between stents for malignant colorectal obstruction: a randomized, prospective study. |
| Tanaka | 2010 | Endoscopic balloon dilation for obstructive colorectal cancer: a basic study on morphologic and pathologic features associated with perforation. |
| Brehant | 2009 | Elective (planned) colectomy in patients with colorectal obstruction after placement of a self‐expanding metallic stent as a bridge to surgery: the results of a prospective study. |
| Cheung | 2009 | Endolaparoscopic approach vs conventional open surgery in the treatment of obstructing left‐sided colon cancer: a randomized controlled trial. |
| Kim | 2009 | Dual‐design expandable colorectal stent for malignant colorectal obstruction: comparison of flared ends and bent ends. |
| Maras‐Simunic | 2009 | Use of modified multidetector CT colonography for the evaluation of acute and subacute colon obstruction caused by colorectal cancer: a feasibility study. |
| Marelli | 2009 | Clinical utility of serum tumor markers in the diagnosis of malignant intestinal occlusion. A prospective observational study. |
| Reza | 2009 | Colorectal stenting for management of acute malignant bowel obstruction in advanced colorectal cancer in Iran. |
| Stenhouse | 2009 | Self expanding wall stents in malignant colorectal cancer: is complete obstruction a contraindication to stent placement? |
| Baraza | 2008 | Combination endo‐radiological colorectal stenting: a prospective 5‐year clinical evaluation. |
| Elsberger | 2008 | Self‐expanding metallic stent insertion in the proximal colon |
| Fregonese | 2008 | Ultraflex precision colonic stent placement as a bridge to surgery in patients with malignant colon obstruction. |
| Im | 2008 | Clinical outcomes and patency of self‐expanding metal stents in patients with malignant colorectal obstruction: a prospective single center study. |
| Jiang | 2008 | Primary vs. delayed resection for obstructive left‐sided colorectal cancer: impact of surgery on patient outcome. |
| Nagata | 2008 | PET/CT colonography for the preoperative evaluation of the colon proximal to the obstructive colorectal cancer. |
| Repici | 2008 | WallFlex colonic stent placement for management of malignant colonic obstruction: a prospective study at two centers. |
| Stipa | 2008 | Management of obstructive colorectal cancer with endoscopic stenting followed by single‐stage surgery: open or laparoscopic resection? |
| van Hooft | 2008 | Early closure of a multicenter randomized clinical trial of endoscopic stenting versus surgery for stage IV left‐sided colorectal cancer. |
| Varpe | 2008 | Adoption of self‐expanding metallic stents in the palliative treatment of obstructive colorectal cancerg‐look out for perforations! |
| Wong | 2008 | Tumor pathology and long‐term survival in emergency colorectal cancer |
| Alcantara | 2007 | Colorectal stenting as an effective therapy for preoperative and palliative treatment of large bowel obstruction: 9 years' experience. |
| Choi | 2007 | Interventional management of malignant colorectal obstruction: use of covered and uncovered stents. |
| Lee | 2007 | Comparison of uncovered stent with covered stent for treatment of malignant colorectal obstruction. |
| Mitchell | 2007 | Emergency room presentation of colorectal cancer: a consecutive cohort study. |
| Mucci‐Hennekinne | 2007 | Management of acute malignant large‐bowel obstruction with self‐expanding metal stent. |
| Olmi | 2007 | Acute colonic obstruction: endoscopic stenting and laparoscopic resection. |
| Repici | 2007 | Ultraflex precision colonic stent placement for palliation of malignant colonic obstruction: a prospective multicenter study. |
| Song | 2007 | A dual‐design expandable colorectal stent for malignant colorectal obstruction: results of a multicenter study. |
| Tsurumaru | 2007 | Self‐expandable metallic stents as palliative treatment for malignant colorectal obstruction. |
| McArdle | 2006 | The impact of blood loss, obstruction and perforation on survival in patients undergoing curative resection for colon cancer. |
| Ptok | 2006 | Palliative stent implantation in the treatment of malignant colorectal obstruction. |
| Vitale | 2006 | Preoperative colonoscopy after self‐expandable metallic stent placement in patients with acute neoplastic colon obstruction. |
| Davies | 2005 | Bowel function following insertion of self‐expanding metallic stents for palliation of colorectal cancer. |
| Gallardo‐Valverde | 2005 | Obstruction in patients with colorectal cancer increases morbidity and mortality in association with altered nutritional status. |
| Kim | 2005 | Complete single‐stage management of left colon cancer obstruction with a new device. |
| Lim | 2005 | Prospective, randomized trial comparing intraoperative colonic irrigation with manual decompression only for obstructed left‐sided colorectal cancer. |
| Poon | 2005 | Evaluation of P‐POSSUM in surgery for obstructing colorectal cancer and correlation of the predicted mortality with different surgical options. |
| Syn | 2005 | Metallic stents in large bowel obstruction: Experience in a District General Hospital |
| Villar | 2005 | Surgical options for malignant left‐sided colonic obstruction. |
| Balague | 2004 | Minimally invasive treatment for obstructive tumors of the left colon: endoluminal self‐expanding metal stent and laparoscopic colectomy. Preliminary results. |
| Law | 2004 | Palliation for advanced malignant colorectal obstruction by self‐expanding metallic stents: prospective evaluation of outcomes. |
| Maeda | 2004 | Successful treatment using a self‐expandable metallic stent in the palliation for unresectable malignant obstruction of the colon and rectum |
| Meisner | 2004 | Self‐expanding metal stents for colonic obstruction: experiences from 104 procedures in a single center. |
| Park | 2004 | Single‐stage procedure with intraoperative colonoscopy and colonic irrigation in patients with obstructing left‐sided colonic cancer. |
| Shim | 2004 | Through‐the‐scope double colonic stenting in the management of inoperable proximal malignant colonic obstruction: a pilot study. |
| Tekkis | 2004 | The Association of Coloproctology of Great Britain and Ireland study of large bowel obstruction caused by colorectal cancer. |
| Tomiki | 2004 | Comparison of stent placement and colostomy as palliative treatment for inoperable malignant colorectal obstruction. |
| Vanbiervliet | 2004 | Endoscopic palliative treatment of malignant colorectal stenosis with metallic stents: Results in 41 patients |
| Xinopoulos | 2004 | Stenting or stoma creation for patients with inoperable malignant colonic obstructions? Results of a study and cost‐effectiveness analysis. |
| Law | 2003 | Comparison of stenting with emergency surgery as palliative treatment for obstructing primary left‐sided colorectal cancer. |
| DeGregorio | 2002 | Use of an introducer sheath for colonic stent placement. |
| Martinez‐Santos | 2002 | Self‐expandable stent before elective surgery vs. emergency surgery for the treatment of malignant colorectal obstructions: comparison of primary anastomosis and morbidity rates. |
| Seymour | 2002 | Palliative stenting of malignant large bowel obstruction |
| Vrazas | 2002 | Stenting for obstructing colorectal malignancy: an interim or definitive procedure. |
| Wong | 2002 | Treatment of acute malignant colorectal obstruction with self‐expandable metallic stents. |
| Carraro | 2001 | Obstructing colonic cancer: failure and survival patterns over a ten‐year follow‐up after one‐stage curative surgery. |
| Mao | 2001 | Treatment of malignant digestive tract obstruction by combined intraluminal stent installation and intra‐arterial drug infusion. |
| Tanaka | 2001 | Endoscopic transanal decompression with a drainage tube for acute colonic obstruction: Clinical aspects of preoperative treatment |
| Camunez | 2000 | Malignant colorectal obstruction treated by means of self‐expanding metallic stents: effectiveness before surgery and in palliation. |
| Grunshaw | 2000 | Prospective evaluation of ultrasound in distal ileal and colonic obstruction |
| Laval | 2000 | The use of steroids in the management of inoperable intestinal obstruction in terminal cancer patients: do they remove the obstruction? |
| Law | 2000 | Self‐expanding metallic stent in the treatment of colonic obstruction caused by advanced malignancies. |
| Repici | 2000 | Covered metal stents for management of inoperable malignant colorectal strictures. |
| Tamim | 2000 | Experience with endoluminal colonic wall stents for the management of large bowel obstruction for benign and malignant disease. |
Terminology
Main terms for the clinical condition that were adhered to in the included studies were ‘obstruction/obstructing/obstructive’ (n = 105), ‘stricture’ (n = 5) and ‘occlusion’ (n = 2) (Table 1). ‘Ileus’ was not used in any of the included studies. In five studies, no specific terminology was provided in the Methods section. The urgency of the clinical condition was further specified in 34 studies: ‘acute’ (n = 28), ‘complete’ (n = 4), ‘emergency’ (n = 1), ‘imminent’ (n = 1). Three studies included patients of varying urgency (‘(sub)acute’, ‘(in)complete’, ‘(sub)occlusion’).
Definition of obstructive colorectal cancer
In total, 42 of the 115 included studies (36.5%) provided a definition of obstructive colorectal cancer: five of 16 RCTs (31.3%) and 37 of 99 prospective observational studies (37.4%) (Table 1). The definitions of these 42 studies are displayed in Table 2, thereby separating the used terms and descriptions for each of the five predefined elements. The definition was solely based on clinical symptoms in 11 studies [5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15] or solely on radiological imaging in six studies [16, 17, 18, 19, 20, 21] (Figure 2). In the remaining studies, a combination of clinical symptoms with or without duration, physical examination, endoscopic features or radiological imaging was incorporated into the definition of obstruction. A combination of symptoms and physical examination was used in four studies [22, 23, 24, 25], symptoms including duration and physical examination in two studies [23, 25], symptoms and endoscopic features in one study [26], symptoms including duration and endoscopic features in none of the studies, symptoms and radiological findings in six studies [27, 28, 29, 30, 31, 32], symptoms including duration and radiological findings in two studies [28, 29], symptoms, physical examination and endoscopic features in one study [33], and symptoms, physical examination and radiological findings in nine studies [34, 35, 36, 37, 38, 39, 40, 41, 42], with three of these also including duration of symptoms [34, 38, 41]. None of the studies included all five elements. A radiological component was incorporated in the used definitions in 100% of RCTs (5/5) vs. 54.1% of prospective observational studies (20/37, P = 0.07). No studies were identified that formally validated a definition of obstructive colorectal cancer.
TABLE 2.
Definitions provided for colorectal obstruction in prospective studies, divided into five predefined elements
| First author | Year | Clinical symptoms | Duration of symptoms | Physical examination | Endoscopic features | Radiological imaging | |
|---|---|---|---|---|---|---|---|
| 1 | Bayrak [34] | 2019 | No bowel movements during last 24 h, fecaloid vomiting | During last 24 h | Abdominal distention | NR | Enlarged colonic loops |
| 2 | Fiori [8] | 2018 | Symptoms of severe obstruction lasting for >3 months | >3 months | NR | NR | NR |
| 3 | Takahashi [45] | 2018 | Pain | NR | Abdominal distention | Severe colonic obstruction on endoscopic imaging | Dilatation of the colon on plain or enhanced abdominal CT scan |
| 4 | Saito [12] | 2016 | CROSS | NR | NR | NR | NR |
| 5 | Matsuzawa [43] | 2015 |
Complete obstruction: inability to pass flatus [50] Remaining cases: incomplete obstruction + CROSS |
NR | NR |
Complete obstruction: inability to endoscopically visualize the proximal lumen [50] Remaining cases: incomplete obstruction |
Complete obstruction: inability of water‐soluble contrast to pass proximal to the lesion [50] Remaining cases: incomplete obstruction |
| 6 | Di Mitri [6] | 2014 | Unable to pass stool and gas, vomiting, abdominal pain, paradoxical diarrhoea | NR | NR | NR | NR |
| 7 | Kim [33] | 2014 | Constipation | NR | Abdominal distention | Endoscopic features of colonic obstruction and colonoscope with diameter 12.2 or 13.2 mm could not pass through the stricture | NR |
| 8 | Ding [7] | 2013 | Symptoms resulting in difficulty in defaecation | NR | NR | NR | NR |
| 9 | Yoshida [44] | 2013 |
Complete obstruction: inability to pass flatus Remaining cases: incomplete obstruction [50] |
NR | NR |
Complete obstruction: lack of endoscopically visible proximal lumen Remaining cases: incomplete obstruction [50] |
Complete obstruction: lack of water‐soluble contrast passing proximally to the lesion Remaining cases: incomplete obstruction [50] |
| 10 | Cennamo [35] | 2012 | Abdominal pain, complete blockage of bowel transit and flatus | NR | Abdominal distention | NR | Dilated bowel proximal to the site of obstruction |
| 11 | Chou [5] | 2012 | Symptoms resulting in defaecation difficulty | NR | NR | NR | NR |
| 12 | Ho [37] | 2012 | Vomiting, abdominal pain, inability to pass stools | NR | Abdominal distention | NR | Dilated colon |
| 13 | Song [14] | 2012 | Symptoms that resulted in defaecation difficulty | NR | NR | NR | NR |
| 14 | Alcantara [21] | 2011 | NR | NR | NR | NR | Diagnosis of complete intestinal obstruction due to tumour in left colon using abdominal CT [48] |
| 15 | Chakraborty [36] | 2011 | Nausea, vomiting, pain [49] | NR | Abdominal distention [49] | NR | Corresponding findings on CT scan of abdomen and pelvis [49] |
| 16 | Marrelli [39] | 2011 | Abdominal pain, constipation | NR | Abdominal distention | NR | Air–fluid levels suggestive of mechanical ileus |
| 17 | Sule [42] | 2011 | Constipation, abdominal pain, nausea | NR | Abdominal distention | NR | Radiographic features of large bowel obstruction |
| 18 | Van Hooft [29] | 2011 | Clinical signs of severe colonic obstruction that had existed for less than 1 week | <1 week | NR | NR | Dilatation of the colon on either plain abdominal radiograph, with typical abnormalities on a gastrografin enema study, or contrast‐enhanced CT scan |
| 19 | Hisanaga [22] | 2010 | Nausea/vomiting or abdominal pain | NR | Abdominal distention | NR | NR |
| 20 | Nagula [24] | 2010 | Progressive constipation, multiple small bowel movements daily, abdominal pain, and nausea and vomiting | NR | Abdominal distention | NR | NR |
| 21 | Brehant [17] | 2009 | NR | NR | NR | NR | Colon distention, upstream malignant stenosis |
| 22 | Kim [10] | 2009 | Symptoms resulting in difficulty in defaecation | NR | NR | NR | NR |
| 23 | Maras‐Simunic [15] | 2009 | Altered bowel habits | NR | NR | NR | NR |
| 24 | Stenhouse [19] | 2009 | NR | NR | NR | NR |
Complete obstruction: no retrograde flow of gastrografin or bowel dilatation proximal to a transition zone followed by distal bowel collapse on CT Incomplete obstruction: partially obstructing lesion with retrograde flow of gastrografin |
| 25 | Fregonese [9] | 2008 | Abdominal/perianal pain, nausea, vomiting, bloating, decreased stool calibre, haematochezia, tenesmus, urgency, rectal bleeding, incontinence, melena | NR | NR | NR | NR |
| 26 | Nagata [18] | 2008 | NR | NR | NR | NR | Bowel distention in segments proximal vs. distal from the lesion |
| 27 | Repici [41] | 2008 | Inability to pass flatus or stool through the anus for more than 24 h | > 24 h | Bowel distention | NR | Radiographic evidence of ileus |
| 28 | Alcantara [16] | 2007 | NR | NR | NR | NR | Only provided for incomplete obstruction: bowel dilatation seen at CT with some contrast medium passing through the tumour |
| 29 | Lee [23] | 2007 | Obstipation or constipation >48 h, nausea, vomiting or cramping abdominal pain | > 48 h | Abdominal distention | NR | NR |
| 30 | Olmi [25] | 2007 | Symptoms such as severe constipation longer than 48 h, nausea, vomiting and cramping abdominal pain | > 48 h | Abdominal distention | NR | NR |
| 31 | Song [13] | 2007 | Difficulty in defaecation | NR | NR | NR | NR |
| 32 | Ptok [46] | 2006 | NR | NR | NR | Tumour stenosis that could not be passed with a normal colonoscope | Manifest ileus or prestenotic dilatation of the colon exceeding 6 cm |
| 33 | Kim [26] | 2005 |
Complete obstruction: NR Nearly complete obstruction: abdominal pain in bowel preparation for colon study |
NR | NR |
Complete obstruction: NR Nearly complete obstruction: complete colonoscopic examination was impossible because of narrowing |
NR |
| 34 | Lim [27] | 2005 | Delay of stool | NR | NR | NR | Large bowel distention on plain supine abdominal radiograph with confirmation on flexible sigmoidoscopy and/or CT of the abdomen or pelvis |
| 35 | Poon [40] | 2005 | Abdominal pain and constipation | NR | Abdominal distention | NR | Dilated bowel proximal to the site of obstruction |
| 36 | Shim [28] | 2004 | Constipation lasting longer than 48 h, vomiting or cramping abdominal pain | >48 h | NR | NR | Conventional radiographic evidence of colonic obstruction on a barium enema examination |
| 37 | Tekkis [32] | 2004 | Clinical or radiological evidence of distended large and/or small bowel secondary to colorectal cancer and presenting as an emergency | NR | NR | NR | Clinical or radiological evidence of distended large and/or small bowel secondary to colorectal cancer and presenting as an emergency |
| 38 | Tanaka [20] | 2001 | NR | NR | NR | NR | Bowel dilatation, formation of air–fluid level and presence of tumour with plain abdominal radiography and CT rather than contrast medium |
| 39 | Grunshaw [30] | 2000 | Clinical or radiological findings suggestive of distal small bowel or colonic obstruction | NR | NR | NR | Fluid or gas‐filled colon, terminating abruptly with collapsed colon distally, with or without the presence of a mass lesion |
| 40 | Laval [38] | 2000 | At least 3 criteria: vomiting at least twice a day, colicky abdominal pain, no flatus for 12 h or more, no stool for at least 4 days (excluding cases of faecal impaction) | At least 3 criteria: vomiting at least twice a day, colicky abdominal pain, no flatus for 12 h or more, no stool for at least 4 days (excluding cases of faecal impaction) | Intestinal distention | NR | Air–fluid levels or the absence of large bowel gas on abdominal X‐ray |
| 41 | Repici [11] | 2000 |
Complete obstruction: no passage of gas and faeces Incomplete obstruction: only passage of gas |
NR | NR | NR | NR |
| 42 | Tamim [31] | 2000 | Not passing stool or gas via the rectum | NR | NR | NR | Signs of complete obstruction on plain radiography, CT scan or contrast‐enhanced enema |
CROSS, ColoRectal Obstruction Scoring System; NR, not reported.
FIGURE 2.

Percentage of studies reporting each (combination of) element(s) within their definition
Clinical symptoms
The most frequently reported clinical symptoms included abdominal pain, inability to pass stool or flatus, nausea and/or vomiting. The CROSS score, which focuses on the level of oral intake along with symptoms of stricture, was used in two of 42 studies (4.8%) [12, 43]. In three of the studies [11, 43, 44], absence of flatus determined the degree of obstruction: if the patient was still able to pass flatus, the obstruction was incomplete. The required duration of symptoms for patients to be eligible for inclusion was reported in eight studies [8, 23, 25, 28, 29, 34, 38, 41]. Three studies mentioned >48 h as a minimum [23, 25, 28], whereas others used criteria such as symptoms for at least 12 h [38] or 24 h [34, 41], less than 1 week [29] or at least 3 months [8].
Physical examination
Findings during physical examination that were included in definitions of colorectal obstruction included abdominal distention in 13 studies [22, 23, 24, 25, 39, 40, 42, 45], bowel distention in one study [41] and intestinal distention in one study [38].
Endoscopic features
Endoscopic features were included in the definition of obstruction in six studies and were described as ‘the inability of the endoscopist to visualize the proximal lumen’ [43, 44], ‘a stenosis that could not be passed with a colonoscope’ [33, 46] or ‘severe colonic obstruction on endoscopic imaging’ [45]. One study specifically defined nearly complete obstruction using endoscopic features: ‘complete colonoscopic examination was impossible because of narrowing’ [26].
Radiological imaging
Descriptions of findings during radiological imaging as one of the elements of the definition of obstruction included ‘enlarged colonic loops’, ‘dilated colon proximally to the lesion’, ‘termination of a fluid‐ or gas‐filled colon by a collapsed colon distally’, ‘inability of contrast to pass proximal to the lesion’, ‘some contrast passing the tumour in case of incomplete obstruction’ and ‘air–fluid levels suggestive of ileus’.
DISCUSSION
The current systematic review reveals an important shortcoming in the available literature on large bowel obstruction by colorectal cancer regarding the definition of the relevant clinical condition, as well as the specification of the urgency of obstruction. Even after eligibility was confined to only randomized and prospective observational studies, we found that only 42 of the 115 included studies (36.5%) provided any definition of obstruction and only 34 studies (29.6%) specified the urgency. The proportion of studies providing any definition was similar for RCTs (31%) and non‐randomized observational cohort studies (37%). Definitions varied extensively regarding the terms and descriptions that were used, as well as the number and combinations of the five predefined elements that were incorporated. Most studies used a combination of clinical symptoms with or without duration and findings during radiological imaging to define malignant colorectal obstruction. All RCTs using a definition for obstruction incorporated radiological signs to confirm the presence of obstruction, while this was the case in only half of prospective observational studies. The required duration of symptoms for inclusion varied from 12 h up to 3 months.
Regarding the terminology of the clinical condition, ‘obstruction’ or similar words were mostly used. However, given the fact that this term can apparently be used independent of the degree of obstruction, it seems necessary to further specify this condition. Considering the desired relevance of the definition for therapeutic decision‐making, one should name the condition that indicates the necessity for an emergency intervention, either surgical or endoscopic. ‘Acute obstruction’ probably best expresses this clinical scenario, while ‘complete obstruction’ wrongly implies that one can reliably assess the degree of obstruction by any measure. If urgency was specified, ‘acute’ was used in the vast majority of studies.
Clinical symptoms that were included in the definitions were abdominal pain, nausea, vomiting and several words and phrases referring to problems with passing stools or flatus. Reporting these symptoms may vary between physicians according to differences in education, specialization and experience, besides geographical and psychosocial differences in the way patients present their symptoms, and thus be subject to inter‐observer variability. Some of the symptoms are relatively unspecific, such as abdominal pain and nausea. Vomiting is a more objective symptom, but only presents in the case of malignant obstruction if the small bowel dilates with insufficiency of the ileocaecal valve. Inability to pass stools or flatus might also be difficult to judge, and terms such as ‘constipation’, ‘change in bowel habits’ or ‘difficulty in defaecation’ do not seem to be appropriate to define acute obstruction.
Duration of symptoms was infrequently described and varied between 12 h and 3 months. Notably, several studies used a minimum of 24 h or even 12 h of not passing stools or flatus as a criterion for inclusion. However, this might also be the case in physiological circumstances, raising the question whether adding an interval of 24 h or less to the definition of colorectal obstruction regarding bowel movements is of any relevance. If one would consider including passage of stools or flatus as part of the definition of acute obstruction, the minimal duration should probably be at least 48 h.
Radiological confirmation of obstruction is probably one of the essential elements of the definition. However, in order to define the condition as an emergency, it also seems essential that symptoms should be included in a definition of acute obstruction in combination with at least the presence of abdominal distention during physical examination. The other way around, abdominal distention during physical examination in the absence of any related symptoms can contribute to defining acute colorectal obstruction.
In the case of emergency surgery, colonoscopy is often not performed before resection or construction of a decompressing stoma. This was confirmed by the current systematic review, in which endoscopic characteristics were infrequently part of the requirements for having obstructive colorectal cancer. Furthermore, endoscopic features such as inability to pass the endoscope might be observed in the absence of any clinical or radiological signs of obstruction. For these reasons, endoscopic features should probably not be included in the definition of acute obstruction. In contrast, a CT scan showing dilated colon proximal to a malignant appearing stenosis is probably one of the most reliable elements of a definition of obstruction [47]. The only difficulty for radiologists is to distinguish obstruction from colonic dilatation or pseudo‐obstruction, and a contrast enema can help to differentiate. Furthermore, the clinical diagnosis only fits into ‘acute obstruction’ in combination with at least one clinical criterion such as vomiting, distended abdomen or not passing stools or flatus for at least 48 h.
The required maximum interval between presentation and first intervention, reflecting urgency and severity of the obstruction, was reported even less frequently than duration of symptoms. In one RCT [29], patients had to be treated with either an SEMS or surgery within 24 h of randomization. Although such a criterion might add to the definition of acute obstruction, incorporating timing of subsequent therapeutic interventions is probably not the purest way of defining a clinical condition. Considering therapeutic consequences, it is also of relevance that the ESGE guideline of 2020 recommends against prophylactic colonic SEMS placement. According to the guideline, SEMS is only indicated in patients with both obstructive symptoms and radiological findings suspicious of malignant large bowel obstruction, because of the potential risks associated with colonic stenting [2]. An unclear distinction between acute and imminent obstruction may result in overtreatment of patients who might experience relief of mild symptoms by, for example, laxatives with subsequent semi‐elective surgery. This underlines the need to talk about ‘acute obstruction’, as mentioned before.
Recently, a scoring system CROSS was developed by a Japanese group in order to evaluate the degree of colorectal obstruction and consequently aid in the choice of treatment of patients with obstructive colorectal cancer [3]. This scoring system focuses on the level of oral intake along with symptoms of stricture, including abdominal pain or cramps, abdominal distention, nausea, vomiting, constipation and diarrhoea. The less able a patient is to eat soft solids, the lower the CROSS score. However, this scoring system is infrequently used in the literature. This was confirmed by the current systematic review, with only two of 42 studies (4.8%) adhering to the CROSS scoring system. A disadvantage of this scoring system is the lack of any radiological criteria. Before widespread implementation, such a scoring system has to be assessed regarding its relevance to therapeutic decision‐making and subsequent clinical outcome parameters. Subsequently, validation is required in different clinical settings.
The limitations of the present review are related to the selection of studies. Besides RCTs, we decided to include studies with a prospective study design. However, the term ‘prospective’ does not necessarily mean that a complete research protocol had been written before data collection and might only indicate that patients were prospectively identified. This might explain the low proportion of definitions provided, although the proportion was similar for RCTs. In addition, because of the rather long inclusion period, the methodological criteria of designing and reporting prospective studies as well as the diagnostic work‐up of such patients have probably changed over time. Furthermore, insight into the clinical relevance of the urgency of the obstruction might have increased.
In conclusion, obstruction by colorectal cancer was not clearly defined and its urgency was not specified in the majority of the included prospective studies in the current systematic review. Radiological imaging showing distended bowel proximal to a suspicious malignant stenosis seems an essential element of a definition of obstruction by colorectal cancer. If combined with a distended abdomen during physical examination with or without specific clinical symptoms, this can define the clinical condition of ‘acute obstruction’ with required relevance for therapeutic decision‐making. Consensus on one uniform definition is warranted, in order to reduce overtreatment of imminent obstruction, to improve comparability of the literature, to facilitate guideline development and to enable benchmarking within a clinical audit.
CONFLICT OF INTERESTS
J.V. Veld, K.J. Beek, E.C.J. Consten, H.L. van Westreenen, F. ter Borg, W.A. Bemelman, J.E. van Hooft and P.J. Tanis have no conflicts of interests or financial ties to disclose for this specific study. Outside of the submitted work, J.E. van Hooft received a grant from Cook Medicals and a consultancy fee from Boston Scientific and Medtronics.
ETHICAL APPROVAL
J.V. Veld, K.J. Beek, E.C.J. Consten, H.L. van Westreenen, F. ter Borg, W.A. Bemelman, J.E. van Hooft, and P.J. Tanis have no conflicts of interests or financial ties to disclose for this specific study.
Outside of the submitted work, J.E. van Hooft received a grant from Cook Medicals and a consultancy fee from Boston Scientific and Medtronics.
AUTHOR CONTRIBUTIONS
All authors contributed to the design, writing, and revision of this manuscript. JV and KB performed the literature search and wrote the initial draft. JV, KB, EC, FB, HW, WB, JH, and PT interpreted the results of the literature search.
FUNDING INFORMATION
This research did not receive any specific grant from funding agencies in the public, commercial or not‐for‐profit sectors.
Veld, JV , Beek KJ, Consten EC, et al. Definition of large bowel obstruction by primary colorectal cancer: A systematic review. American Colorectal Dis. 2021;23:787–804. 10.1111/codi.15479
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Jullumstro E, Wibe A, Lydersen S, Edna TH. Colon cancer incidence, presentation, treatment and outcomes over 25 years. Colorectal Dis. 2011;13(5):512–8. [DOI] [PubMed] [Google Scholar]
- 2. van Hooft JE, Veld JV, Arnold D, Beets‐Tan RGH, Everett S, Gotz M, et al. Self‐expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Update 2020. Endoscopy. 2020;52(5):389–407. [DOI] [PubMed] [Google Scholar]
- 3. Group JCSSPR . CROSS: ColoRectal Obstruction Scoring System, 2012. Available from: https://colon‐stent.com/001_mainpage_en.html. Accessed on July 6, 2020.
- 4. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12. [DOI] [PubMed] [Google Scholar]
- 5. Chou SQ, Song HY, Kim JH, Park JH, Fan Y, Lee H, et al. Dual‐design expandable colorectal stent for a malignant colorectal obstruction: preliminary prospective study using new 20‐mm diameter stents. Korean J Radiol. 2012;13(1):66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Di Mitri R, Mocciaro F. The new nitinol conformable self‐expandable metal stents for malignant colonic obstruction: a pilot experience as bridge to surgery treatment. ScientificWorldJournal. 2014;2014:651765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ding XL, Li YD, Yang RM, Li FB, Zhang MQ. A temporary self‐expanding metallic stent for malignant colorectal obstruction. World J Gastroenterol. 2013;19(7):1119–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fiori E, Lamazza A, Sterpetti AV, Schillaci A. Endoscopic stenting for colorectal cancer: lessons learned from a 15‐year experience. J Clin Gastroenterol. 2018;52(5):418–22. [DOI] [PubMed] [Google Scholar]
- 9. Fregonese D, Naspetti R, Ferrer S, Gallego J, Costamagna G, Dumas R, et al. Ultraflex precision colonic stent placement as a bridge to surgery in patients with malignant colon obstruction. Gastrointest Endosc. 2008;67(1):68–73. [DOI] [PubMed] [Google Scholar]
- 10. Kim JH, Song HY, Li YD, Shin JH, Park JH, Yu CS, et al. Dual‐design expandable colorectal stent for malignant colorectal obstruction: comparison of flared ends and bent ends. Am J Roentgenol. 2009;193(1):248–54. [DOI] [PubMed] [Google Scholar]
- 11. Repici A, Reggio D, De Angelis C, Barletti C, Marchesa P, Musso A, et al. Covered metal stents for management of inoperable malignant colorectal strictures. Gastrointest Endosc. 2000;52(6):735–40. [DOI] [PubMed] [Google Scholar]
- 12. Saito S, Yoshida S, Isayama H, Matsuzawa T, Kuwai T, Maetani I, et al. A prospective multicenter study on self‐expandable metallic stents as a bridge to surgery for malignant colorectal obstruction in Japan: efficacy and safety in 312 patients. Surg Endosc. 2016;30(9):3976–86. [DOI] [PubMed] [Google Scholar]
- 13. Song HY, Kim JH, Shin JH, Kim HC, Yu CS, Kim JC, et al. A dual‐design expandable colorectal stent for malignant colorectal obstruction: results of a multicenter study. Endoscopy. 2007;39(5):448–54. [DOI] [PubMed] [Google Scholar]
- 14. Song HY, Nam DH, Lee H. Usefulness of a guiding sheath for fluoroscopic colorectal stent placement. Korean J Radiol. 2012;13(Suppl 1):S83–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Maras‐Simunic M, Druzijanic N, Simunic M, Roglic J, Tomic S, Perko Z. Use of modified multidetector CT colonography for the evaluation of acute and subacute colon obstruction caused by colorectal cancer: a feasibility study. Dis Colon Rectum. 2009;52:489–95. [DOI] [PubMed] [Google Scholar]
- 16. Alcantara M, Serra X, Bombardo J, Falco J, Perandreu J, Ayguavives I, et al. Colorectal stenting as an effective therapy for preoperative and palliative treatment of large bowel obstruction: 9 years’ experience. Tech Coloproctol. 2007;11(4):316–22. [DOI] [PubMed] [Google Scholar]
- 17. Brehant O, Fuks D, Bartoli E, Yzet T, Verhaeghe P, Regimbeau JM. Elective (planned) colectomy in patients with colorectal obstruction after placement of a self‐expanding metallic stent as a bridge to surgery: the results of a prospective study. Colorectal Dis. 2009;11(2):178–83. [DOI] [PubMed] [Google Scholar]
- 18. Nagata K, Ota Y, Okawa T, Endo S, Kudo SE. PET/CT colonography for the preoperative evaluation of the colon proximal to the obstructive colorectal cancer. Dis Colon Rectum. 2008;51(6):882–90. [DOI] [PubMed] [Google Scholar]
- 19. Stenhouse GJ, Page B, Rowan A, Giles L, Macdonald A. Self expanding wall stents in malignant colorectal cancer: is complete obstruction a contraindication to stent placement? Colorectal Dis. 2009;11(8):854–8. [DOI] [PubMed] [Google Scholar]
- 20. Tanaka T, Furukawa A, Murata K, Sakamoto T. Endoscopic transanal decompression with a drainage tube for acute colonic obstruction: clinical aspects of preoperative treatment. Dis Colon Rectum. 2001;44(3):418–22. [DOI] [PubMed] [Google Scholar]
- 21. Alcantara M, Serra‐Aracil X, Falco J, Mora L, Bombardo J, Navarro S. Prospective, controlled, randomized study of intraoperative colonic lavage versus stent placement in obstructive left‐sided colonic cancer. World J Surg. 2011;35(8):1904–10. [DOI] [PubMed] [Google Scholar]
- 22. Hisanaga T, Shinjo T, Morita T, Nakajima N, Ikenaga M, Tanimizu M, et al. Multicenter prospective study on efficacy and safety of octreotide for inoperable malignant bowel obstruction. Jpn J Clin Oncol. 2010;40(8):739–45. [DOI] [PubMed] [Google Scholar]
- 23. Lee KM, Shin SJ, Hwang JC, Cheong JY, Yoo BM, Lee KJ, et al. Comparison of uncovered stent with covered stent for treatment of malignant colorectal obstruction. Gastrointest Endosc. 2007;66(5):931–6. [DOI] [PubMed] [Google Scholar]
- 24. Nagula S, Ishill N, Nash C, Markowitz AJ, Schattner MA, Temple L, et al. Quality of life and symptom control after stent placement or surgical palliation of malignant colorectal obstruction. J Am Coll Surg. 2010;210(1):45–53. [DOI] [PubMed] [Google Scholar]
- 25. Olmi S, Scaini A, Cesana G, Dinelli M, Lomazzi A, Croce E. Acute colonic obstruction: endoscopic stenting and laparoscopic resection. Surg Endosc. 2007;21(11):2100–4. [DOI] [PubMed] [Google Scholar]
- 26. Kim JH, Shon DH, Kang SH, Jang BI, Chung MK, Kim JH, et al. Complete single‐stage management of left colon cancer obstruction with a new device. Surg Endosc. 2005;19(10):1381–7. [DOI] [PubMed] [Google Scholar]
- 27. Lim JF, Tang CL, Seow‐Choen F, Heah SM. Prospective, randomized trial comparing intraoperative colonic irrigation with manual decompression only for obstructed left‐sided colorectal cancer. Dis Colon Rectum. 2005;48(2):205–9. [DOI] [PubMed] [Google Scholar]
- 28. Shim CS, Cho JY, Jung IS, Ryu CB, Hong SJ, Kim JO, et al. Through‐the‐scope double colonic stenting in the management of inoperable proximal malignant colonic obstruction: a pilot study. Endoscopy. 2004;36(5):426–31. [DOI] [PubMed] [Google Scholar]
- 29. van Hooft JE, Bemelman WA, Oldenburg B, Marinelli AW, Lutke Holzik MF, Grubben MJ, et al. Colonic stenting versus emergency surgery for acute left‐sided malignant colonic obstruction: a multicentre randomised trial. Lancet Oncol. 2011;12(4):344–52. [DOI] [PubMed] [Google Scholar]
- 30. Grunshaw ND, Renwick IG, Scarisbrick G, Nasmyth DG. Prospective evaluation of ultrasound in distal ileal and colonic obstruction. Clin Radiol. 2000;55(5):356–62. [DOI] [PubMed] [Google Scholar]
- 31. Tamim WZ, Ghellai A, Counihan TC, Swanson RS, Colby JM, Sweeney WB. Experience with endoluminal colonic wall stents for the management of large bowel obstruction for benign and malignant disease. Arch Surg. 2000;135(4):434–8. [DOI] [PubMed] [Google Scholar]
- 32. Tekkis PP, Kinsman R, Thompson MR, Stamatakis JD, Association of Coloproctology of Great Britain and Ireland . The Association of Coloproctology of Great Britain and Ireland study of large bowel obstruction caused by colorectal cancer. Ann Surg. 2004;240(1):76–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kim JS, Lee KM, Kim SW, Kim EJ, Lim CH, Oh ST, et al. Preoperative colonoscopy through the colonic stent in patients with colorectal cancer obstruction. World J Gastroenterol. 2014;20(30):10570–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bayrak S, Tatar C, Kinaci E, Cakar E, Colak S, Sevinc MM et al. Stent experiences in emergency conditions in acute mechanical intestinal obstruction caused by colorectal cancer. Videosurg Other Miniinvasive Tech. 2019;14(1):46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cennamo V, Luigiano C, Manes G, Zagari RM, Ansaloni L, Fabbri C, et al. Colorectal stenting as a bridge to surgery reduces morbidity and mortality in left‐sided malignant obstruction: a predictive risk score‐based comparative study. Dig Liver Dis. 2012;44(6):508–14. [DOI] [PubMed] [Google Scholar]
- 36. Chakraborty A, Selby D, Gardiner K, Myers J, Moravan V, Wright F. Malignant bowel obstruction: natural history of a heterogeneous patient population followed prospectively over two years. J Pain Symptom Manage. 2011;41(2):412–20. [DOI] [PubMed] [Google Scholar]
- 37. Ho KS, Quah HM, Lim JF, Tang CL, Eu KW. Endoscopic stenting and elective surgery versus emergency surgery for left‐sided malignant colonic obstruction: a prospective randomized trial. Int J Colorectal Dis. 2012;27(3):355–62. [DOI] [PubMed] [Google Scholar]
- 38. Laval G, Girardier J, Lassauniere JM, Leduc B, Haond C, Schaerer R. The use of steroids in the management of inoperable intestinal obstruction in terminal cancer patients: do they remove the obstruction? Palliat Med. 2000;14(1):3–10. [DOI] [PubMed] [Google Scholar]
- 39. Marrelli D, Caruso S, Neri A, Pedrazzani C, Capuano L, Mazzei MA, et al. Clinical utility of serum tumor markers in the diagnosis of malignant intestinal occlusion. A prospective observational study. Int J Biol Marker. 2011;26(1):58–64. [DOI] [PubMed] [Google Scholar]
- 40. Poon JT, Chan B, Law WL. Evaluation of P‐POSSUM in surgery for obstructing colorectal cancer and correlation of the predicted mortality with different surgical options. Dis Colon Rectum. 2005;48(3):493–8. [DOI] [PubMed] [Google Scholar]
- 41. Repici A, De Caro G, Luigiano C, Fabbri C, Pagano N, Preatoni P, et al. WallFlex colonic stent placement for management of malignant colonic obstruction: a prospective study at two centers. Gastrointest Endosc. 2008;67(1):77–84. [DOI] [PubMed] [Google Scholar]
- 42. Sule AZ, Ajibade A. Adult large bowel obstruction: a review of clinical experience. Ann Afr Med. 2011;10(1):45–50. [DOI] [PubMed] [Google Scholar]
- 43. Matsuzawa T, Ishida H, Yoshida S, Isayama H, Kuwai T, Maetani I, et al. A Japanese prospective multicenter study of self‐expandable metal stent placement for malignant colorectal obstruction: short‐term safety and efficacy within 7 days of stent procedure in 513 cases. Gastrointest Endosc. 2015;82(4):697–707 e1. [DOI] [PubMed] [Google Scholar]
- 44. Yoshida S, Watabe H, Isayama H, Kogure H, Nakai Y, Yamamoto N, et al. Feasibility of a new self‐expandable metallic stent for patients with malignant colorectal obstruction. Dig Endosc. 2013;25(2):160–6. [DOI] [PubMed] [Google Scholar]
- 45. Takahashi G, Yamada T, Iwai T, Takeda K, Koizumi M, Shinji S, et al. Oncological assessment of stent placement for obstructive colorectal cancer from circulating cell‐free DNA and circulating tumor DNA dynamics. Ann Surg Oncol. 2018;25(3):737–44. [DOI] [PubMed] [Google Scholar]
- 46. Ptok H, Meyer F, Marusch F, Steinert R, Gastinger I, Lippert H, et al. Palliative stent implantation in the treatment of malignant colorectal obstruction. Surg Endosc. 2006;20(6):909–14. [DOI] [PubMed] [Google Scholar]
- 47. Jaffe T, Thompson WM. Large‐bowel obstruction in the adult: classic radiographic and CT findings, etiology, and mimics. Radiology. 2015;275(3):651–63. [DOI] [PubMed] [Google Scholar]
- 48. Fielding LP, Stewart‐Brown S, Blesovsky L. Large‐bowel obstruction caused by cancer: a prospective study. Br Med J. 1979;2(6189):515–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Anthony T, Baron T, Mercadante S, Green S, Chi D, Cunningham J, et al. Report of the clinical protocol committee: development of randomized trials for malignant bowel obstruction. J Pain Symptom Manage. 2007;34(1 Suppl):S49–59. [DOI] [PubMed] [Google Scholar]
- 50. Small AJ, Coelho‐Prabhu N, Baron TH. Endoscopic placement of self‐expandable metal stents for malignant colonic obstruction: long‐term outcomes and complication factors. Gastrointest Endosc. 2010;71(3):560–72. [DOI] [PubMed] [Google Scholar]
- 51. Law WL, Chu KW, Ho JW, Tung HM, Law SY, Chu KM. Self‐expanding metallic stent in the treatment of colonic obstruction caused by advanced malignancies. Dis Colon Rectum. 2000;43(11):1522–7. [DOI] [PubMed] [Google Scholar]
- 52. Camunez F, Echenagusia A, Simo G, Turegano F, Vazquez J, Barreiro‐Meiro I. Malignant colorectal obstruction treated by means of self‐expanding metallic stents: effectiveness before surgery and in palliation. Radiology. 2000;216(2):492–7. [DOI] [PubMed] [Google Scholar]
- 53. Mao AW, Gao ZD, Xu JY, Yang RJ, Xiao XS, Jiang TH, et al. Treatment of malignant digestive tract obstruction by combined intraluminal stent installation and intra‐arterial drug infusion. World J Gastroenterol. 2001;7(4):587–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Carraro PG, Segala M, Cesana BM, Tiberio G. Obstructing colonic cancer: failure and survival patterns over a ten‐year follow‐up after one‐stage curative surgery. Dis Colon Rectum. 2001;44(2):243–50. [DOI] [PubMed] [Google Scholar]
- 55. Wong KS, Cheong DM, Wong D. Treatment of acute malignant colorectal obstruction with self‐expandable metallic stents. ANZ J Surg. 2002;72(6):385–8. [DOI] [PubMed] [Google Scholar]
- 56. Vrazas JI, Ferris S, Bau S, Faragher I. Stenting for obstructing colorectal malignancy: an interim or definitive procedure. ANZ J Surg. 2002;72(6):392–6. [DOI] [PubMed] [Google Scholar]
- 57. Seymour K, Johnson R, Marsh R, Corson J. Palliative stenting of malignant large bowel obstruction. Colorectal Dis. 2002;4(4):240–5. [DOI] [PubMed] [Google Scholar]
- 58. Martinez‐Santos C, Lobato RF, Fradejas JM, Pinto I, Ortega‐Deballon P, Moreno‐Azcoita M. Self‐expandable stent before elective surgery vs. emergency surgery for the treatment of malignant colorectal obstructions: comparison of primary anastomosis and morbidity rates. Dis Colon Rectum. 2002;45(3):401–6. [DOI] [PubMed] [Google Scholar]
- 59. DeGregorio B, Mainar A, Tejero E, Alfonso E, Gimeno MJ, Herrera M. Use of an introducer sheath for colonic stent placement. Eur Radiol. 2002;12(9):2250–2. [DOI] [PubMed] [Google Scholar]
- 60. Law WL, Choi HK, Chu KW. Comparison of stenting with emergency surgery as palliative treatment for obstructing primary left‐sided colorectal cancer. Br J Surg. 2003;90(11):1429–33. [DOI] [PubMed] [Google Scholar]
- 61. Xinopoulos D, Dimitroulopoulos D, Theodosopoulos T, Tsamakidis K, Bitsakou G, Plataniotis G, et al. Stenting or stoma creation for patients with inoperable malignant colonic obstructions? Results of a study and cost‐effectiveness analysis. Surg Endosc. 2004;18(3):421–6. [DOI] [PubMed] [Google Scholar]
- 62. Vanbiervliet G, Dumas R, Demarquay JF, Peten EP, Stef A, Adhoute G, et al. Endoscopic palliative treatment of malignant colorectal stenosis with metallic stents: results in 41 patients. Acta Endosc. 2004:327–34. [Google Scholar]
- 63. Tomiki Y, Watanabe T, Ishibiki Y, Tanaka M, Suda S, Yamamoto T, et al. Comparison of stent placement and colostomy as palliative treatment for inoperable malignant colorectal obstruction. Surg Endosc. 2004;18(11):1572–7. [DOI] [PubMed] [Google Scholar]
- 64. Park UC, Chung SS, Kim KR, Seong MK, Yoon WH, Kim YJ, et al. Single‐stage procedure with intraoperative colonoscopy and colonic irrigation in patients with obstructing left‐sided colonic cancer. Int J Colorectal Dis. 2004;19(5):487–92. [DOI] [PubMed] [Google Scholar]
- 65. Meisner S, Hensler M, Knop FK, West F, Wille‐Jorgensen P. Self‐expanding metal stents for colonic obstruction: experiences from 104 procedures in a single center. Dis Colon Rectum. 2004;47(4):444–50. [DOI] [PubMed] [Google Scholar]
- 66. Maeda K, Inoue T, Yashiro M, Nishihara T, Nishiguchi Y, Hirakawa K. Successful treatment using a self‐expandable metallic stent in the palliation for unresectable malignant obstruction of the colon and rectum. Dig Endosc. 2004;16(4):332–336. [Google Scholar]
- 67. Law WL, Choi HK, Lee YM, Chu KW. Palliation for advanced malignant colorectal obstruction by self‐expanding metallic stents: prospective evaluation of outcomes. Dis Colon Rectum. 2004;47(1):39–43. [DOI] [PubMed] [Google Scholar]
- 68. Balague C, Targarona EM, Sainz S, Montero O, Bendahat G, Kobus C, et al. Minimally invasive treatment for obstructive tumors of the left colon: endoluminal self‐expanding metal stent and laparoscopic colectomy. Preliminary results. Dig Surg. 2004;21(4):282–6. [DOI] [PubMed] [Google Scholar]
- 69. Villar JM, Martinez AP, Villegas MT, Muffak K, Mansilla A, Garrote D, et al. Surgical options for malignant left‐sided colonic obstruction. Surg Today. 2005;35(4):275–81. [DOI] [PubMed] [Google Scholar]
- 70. Syn WK, Patel M, Ahmed MM. Metallic stents in large bowel obstruction: experience in a District General Hospital. Colorectal Dis. 2005;7(1):22–6. [DOI] [PubMed] [Google Scholar]
- 71. Gallardo‐Valverde JM, Calanas‐Continente A, Baena‐Delgado E, Zurera‐Tendero L, Vazquez‐Martinez C, Membrives‐Obrero A, et al. Obstruction in patients with colorectal cancer increases morbidity and mortality in association with altered nutritional status. Nutr Cancer. 2005;53(2):169–76. [DOI] [PubMed] [Google Scholar]
- 72. Davies RJ, D'Sa IB, Lucarotti ME, Fowler AL, Tottle A, Birch P, et al. Bowel function following insertion of self‐expanding metallic stents for palliation of colorectal cancer. Colorectal Dis. 2005;7(3):251–3. [DOI] [PubMed] [Google Scholar]
- 73. Vitale MA, Villotti G, d'Alba L, Frontespezi S, Iacopini F, Iacopini G. Preoperative colonoscopy after self‐expandable metallic stent placement in patients with acute neoplastic colon obstruction. Gastrointest Endosc. 2006;63(6):814–9. [DOI] [PubMed] [Google Scholar]
- 74. McArdle CS, McMillan DC, Hole DJ. The impact of blood loss, obstruction and perforation on survival in patients undergoing curative resection for colon cancer. Br J Surg. 2006;93(4):483–8. [DOI] [PubMed] [Google Scholar]
- 75. Tsurumaru D, Hidaka H, Okada S, Sakoguchi T, Matsuda H, Matsumata T, et al. Self‐expandable metallic stents as palliative treatment for malignant colorectal obstruction. Abdom Imaging. 2007;32(5):619–23. [DOI] [PubMed] [Google Scholar]
- 76. Song HY, Kim JH, Shin JH, Kim HC, Yu CS, Kim JC, et al. A dual‐design expandable colorectal stent for malignant colorectal obstruction: results of a multicenter study. Endoscopy. 2007;39(5):448–54. [DOI] [PubMed] [Google Scholar]
- 77. Repici A, Fregonese D, Costamagna G, Dumas R, Kahler G, Meisner S, et al. Ultraflex precision colonic stent placement for palliation of malignant colonic obstruction: a prospective multicenter study. Gastrointest Endosc. 2007;66(5):920–7. [DOI] [PubMed] [Google Scholar]
- 78. Mucci‐Hennekinne S, Kervegant AG, Regenet N, Beaulieu A, Barbieux JP, Dehni N, et al. Management of acute malignant large‐bowel obstruction with self‐expanding metal stent. Surg Endosc. 2007;21(7):1101–3. [DOI] [PubMed] [Google Scholar]
- 79. Mitchell AD, Inglis KM, Murdoch JM, Porter GA. Emergency room presentation of colorectal cancer: a consecutive cohort study. Ann Surg Oncol. 2007;14(3):1099–104. [DOI] [PubMed] [Google Scholar]
- 80. Choi JS, Choo SW, Park KB, Shin SW, Yoo SY, Kim JH, et al. Interventional management of malignant colorectal obstruction: use of covered and uncovered stents. Korean J Radiol. 2007;8(1):57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Wong SK, Jalaludin BB, Morgan MJ, Berthelsen AS, Morgan A, Gatenby AH, et al. Tumor pathology and long‐term survival in emergency colorectal cancer. Dis Colon Rectum. 2008;51(2):223–30. [DOI] [PubMed] [Google Scholar]
- 82. Varpe P, Huhtinen H, Rantala A, Salminen P, Sarparanta H, Gronroos J. Adoption of self‐expanding metallic stents in the palliative treatment of obstructive colorectal cancer‐look out for perforations!. Surg Laparosc Endosc Percutan Tech. 2008;18(4):353–6. [DOI] [PubMed] [Google Scholar]
- 83. van Hooft JE, Fockens P, Marinelli AW, Timmer R, van Berkel AM, Bossuyt PM, et al. Early closure of a multicenter randomized clinical trial of endoscopic stenting versus surgery for stage IV left‐sided colorectal cancer. Endoscopy. 2008;40(3):184–91. [DOI] [PubMed] [Google Scholar]
- 84. Stipa F, Pigazzi A, Bascone B, Cimitan A, Villotti G, Burza A, et al. Management of obstructive colorectal cancer with endoscopic stenting followed by single‐stage surgery: open or laparoscopic resection? Surg Endosc. 2008;22(6):1477–81. [DOI] [PubMed] [Google Scholar]
- 85. Jiang JK, Lan YT, Lin TC, Chen WS, Yang SH, Wang HS, et al. Primary vs. delayed resection for obstructive left‐sided colorectal cancer: impact of surgery on patient outcome. Dis Colon Rectum. 2008;51(3):306–11. [DOI] [PubMed] [Google Scholar]
- 86. Im JP, Kim SG, Kang HW, Kim JS, Jung HC, Song IS. Clinical outcomes and patency of self‐expanding metal stents in patients with malignant colorectal obstruction: a prospective single center study. Int J Colorectal Dis. 2008;23(8):789–94. [DOI] [PubMed] [Google Scholar]
- 87. Elsberger B, Rourke K, Brush J, Glancy S, Collie M. Self‐expanding metallic stent insertion in the proximal colon. Colorectal Dis. 2008;10(2):194–6. [DOI] [PubMed] [Google Scholar]
- 88. Baraza W, Lee F, Brown S, Hurlstone DP. Combination endo‐radiological colorectal stenting: a prospective 5‐year clinical evaluation. Colorectal Dis. 2008;10(9):901–6. [DOI] [PubMed] [Google Scholar]
- 89. Reza F, Amir MA, Faramarz D, Shahrokh M, Mehrdad Z, Shivarani S, et al. Colorectal stenting for management of acute malignant bowel obstruction in advanced colorectal cancer in Iran. Asian Pac J Cancer Prevent. 2009;10(5):739–41. [PubMed] [Google Scholar]
- 90. Cheung HY, Chung CC, Tsang WW, Wong JC, Yau KK, Li MK. Endolaparoscopic approach vs conventional open surgery in the treatment of obstructing left‐sided colon cancer. Arch Surg. 2009;144(12):1127–32. [DOI] [PubMed] [Google Scholar]
- 91. Tanaka A, Sadahiro S, Yasuda M, Shimizu S, Maeda Y, Suzuki T, et al. Endoscopic balloon dilation for obstructive colorectal cancer: a basic study on morphologic and pathologic features associated with perforation. Gastrointest Endosc. 2010;71(4):799–805. [DOI] [PubMed] [Google Scholar]
- 92. Park S, Cheon JH, Park JJ, Moon CM, Hong SP, Lee SK, et al. Comparison of efficacies between stents for malignant colorectal obstruction: a randomized, prospective study. Gastrointest Endosc. 2010;72(2):304–10. [DOI] [PubMed] [Google Scholar]
- 93. Mukai M, Sekido Y, Hoshikawa T, Yazawa N, Fukumitsu H, Okada K, et al. Two‐stage treatment (Mukai's method) with hybrid 2‐port HALS (Mukai's operation) for complete bowel obstruction by left colon cancer or rectal cancer. Oncol Rep. 2010;24(1):25–30. [DOI] [PubMed] [Google Scholar]
- 94. Moon CM, Kim TI, Lee MS, Ko BM, Kim HS, Lee KM, et al. Comparison of a newly designed double‐layered combination covered stent and D‐weave uncovered stent for decompression of obstructive colorectal cancer: a prospective multicenter study. Dis Colon Rectum. 2010;53(8):1190–6. [DOI] [PubMed] [Google Scholar]
- 95. Li YD, Cheng YS, Li MH, Fan YB, Chen NW, Wang Y, et al. Management of acute malignant colorectal obstruction with a novel self‐expanding metallic stent as a bridge to surgery. Eur J Radiol. 2010;73(3):566–71. [DOI] [PubMed] [Google Scholar]
- 96. Dakubo JC, Naaeder SB, Tettey Y, Gyasi RK. Colorectal carcinoma: an update of current trends in Accra. West Afr J Med. 2010;29(3):178–83. [DOI] [PubMed] [Google Scholar]
- 97. Branger F, Thibaudeau E, Mucci‐Hennekinne S, Metivier‐Cesbron E, Vychnevskaia K, Hamy A, et al. Management of acute malignant large‐bowel obstruction with self‐expanding metal stent. Int J Colorectal Dis. 2010;25(12):1481–5. [DOI] [PubMed] [Google Scholar]
- 98. Achiam MP, Andersen LP, Klein M, Logager V, Chabanova E, Thomsen HS, et al. Differentiation between benign and malignant colon tumors using fast dynamic gadolinium‐enhanced MR colonography; a feasibility study. Eur J Radiol. 2010;74(3):e45–50. [DOI] [PubMed] [Google Scholar]
- 99. Young CJ, Suen MK, Young J, Solomon MJ. Stenting large bowel obstruction avoids a stoma: consecutive series of 100 patients. Colorectal Dis. 2011;13(10):1138–41. [DOI] [PubMed] [Google Scholar]
- 100. Williams D, Law R, Pullyblank AM. Colorectal stenting in malignant large bowel obstruction: the learning curve. Int J Surg Oncol. 2011;2011:917848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Pirlet IA, Slim K, Kwiatkowski F, Michot F, Millat BL. Emergency preoperative stenting versus surgery for acute left‐sided malignant colonic obstruction: a multicenter randomized controlled trial. Surg Endosc. 2011;25(6):1814–21. [DOI] [PubMed] [Google Scholar]
- 102. Milek T, Ciostek P, Wozniak W, Lewczuk A, Petryka R, Slowik J, et al. Preliminary results of the use of self‐expanding nitinol stents in inoperable gastrointestinal cancers. Polish J Surg. 2010;82(5):79–83. [Google Scholar]
- 103. Meisner S, Gonzalez‐Huix F, Vandervoort JG, Goldberg P, Casellas JA, Roncero O, et al. Self‐expandable metal stents for relieving malignant colorectal obstruction: short‐term safety and efficacy within 30 days of stent procedure in 447 patients. Gastrointest Endosc. 2011;74(4):876–84. [DOI] [PubMed] [Google Scholar]
- 104. Luigiano C, Ferrara F, Fabbri C, Ghersi S, Bassi M, Billi P, et al. Through‐the‐scope large diameter self‐expanding metal stent placement as a safe and effective technique for palliation of malignant colorectal obstruction: a single center experience with a long‐term follow‐up. Scand J Gastroenterol. 2011;46(5):591–6. [DOI] [PubMed] [Google Scholar]
- 105. Yang HY, Wu CC, Jao SW, Hsu KF, Mai CM, Hsiao KC. Two‐stage resection for malignant colonic obstructions: the timing of early resection and possible predictive factors. World J Gastroenterol. 2012;18(25):3267–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Tominaga K, Maetani I, Sato K, Shigoka H, Omuta S, Ito S, et al. Favorable long‐term clinical outcome of uncovered D‐weave stent placement as definitive palliative treatment for malignant colorectal obstruction. Dis Colon Rectum. 2012;55(9):983–9. [DOI] [PubMed] [Google Scholar]
- 107. Song HY, Nam DH, Lee H. Usefulness of a guiding sheath for fluoroscopic colorectal stent placement. Korean J Radiol. 2012;13(Suppl 1):S83–S88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Meisner S, Gonzalez‐Huix F, Vandervoort JG, Repici A, Xinopoulos D, Grund KE, et al. Self‐expanding metal stenting for palliation of patients with malignant colonic obstruction: effectiveness and efficacy on 255 patients with 12‐month's follow‐up. Gastroenterol Res Pract. 2012;2012:296347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Larssen L, Medhus AW, Korner H, Glomsaker T, Soberg T, Gleditsch D, et al. Long‐term outcome of palliative treatment with self‐expanding metal stents for malignant obstructions of the GI tract. Scand J Gastroenterol. 2012;47(12):1505–14. [DOI] [PubMed] [Google Scholar]
- 110. Jimenez Fuertes M, Costa Navarro D. Resection and primary anastomosis without diverting ileostomy for left colon emergencies: is it a safe procedure? World J Surg. 2012;36(5):1148–53. [DOI] [PubMed] [Google Scholar]
- 111. Inaba Y, Arai Y, Yamaura H, Sato Y, Kato M, Saito H, et al. Phase II clinical study on stent therapy for unresectable malignant colorectal obstruction (JIVROSG‐0206). Am J Clin Oncol. 2012;35(1):73–6. [DOI] [PubMed] [Google Scholar]
- 112. Cheung DY, Kim JY, Hong SP, Jung MK, Ye BD, Kim SG, et al. Outcome and safety of self‐expandable metallic stents for malignant colon obstruction: a Korean multicenter randomized prospective study. Surg Endosc. 2012;26(11):3106–13. [DOI] [PubMed] [Google Scholar]
- 113. Chen FM, Yin TC, Fan WC, Huang CJ, Hsieh JS. Laparoscopic management for acute malignant colonic obstruction. Surg Laparosc Endosc Percutan Tech. 2012;22(3):210–4. [DOI] [PubMed] [Google Scholar]
- 114. Bonfante P, D'Ambra L, Berti S, Falco E, Cristoni MV, Briglia R. Managing acute colorectal obstruction by "bridge stenting" to laparoscopic surgery: our experience. World J Gastrointest Surg. 2012;4(12):289–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Angenete E, Asplund D, Bergstrom M, Park PO. Stenting for colorectal cancer obstruction compared to surgery–a study of consecutive patients in a single institution. Int J Colorectal Dis. 2012;27(5):665–70. [DOI] [PubMed] [Google Scholar]
- 116. Warden C, Stupart D, Goldberg P. Stenting as first‐line management for all patients with nonperforating left‐sided obstructing colorectal cancer. Colorectal Dis. 2013;15(7):e389–95. [DOI] [PubMed] [Google Scholar]
- 117. Sumise Y, Yoshioka K, Okitsu N, Kamo H, Arakawa Y, Yamaguchi T, et al. Outcome of emergency one‐stage resection and anastomosis procedure for patients with obstructed colorectal cancer. J Med Investigat. 2013;60(3–4):249–55. [DOI] [PubMed] [Google Scholar]
- 118. Lim SG, Lee KJ, Suh KW, Oh SY, Kim SS, Yoo JH, et al. Preoperative colonoscopy for detection of synchronous neoplasms after insertion of self‐expandable metal stents in occlusive colorectal cancer: comparison of covered and uncovered stents. Gut Liver. 2013;7(3):311–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Lee KM, Lim SG, Shin SJ, Kim JH, Kang DH, Kim JK, et al. Novel method of stent insertion for malignant lower rectal obstruction with proximal releasing delivery system (with video). Gastrointest Endosc. 2013;78(6):930–3. [DOI] [PubMed] [Google Scholar]
- 120. Lamazza A, Fiori E, Schillaci A, Sterpetti AV. A new technique for placement of a self‐expanding metallic stent (SEMS) in patients with colon rectal obstruction: a prospective study of 43 patients. Surg Endosc. 2013;27(3):1045–8. [DOI] [PubMed] [Google Scholar]
- 121. Ghazal AH, El‐Shazly WG, Bessa SS, El‐Riwini MT, Hussein AM. Colonic endolumenal stenting devices and elective surgery versus emergency subtotal/total colectomy in the management of malignant obstructed left colon carcinoma. J Gastrointest Surg. 2013;17(6):1123–9. [DOI] [PubMed] [Google Scholar]
- 122. Occhionorelli S, Tartarini D, Cappellari L, Stano R, Vasquez G. Colonic stent placement as a bridge to surgery in patients with left‐sided malignant large bowel obstruction. An observational study. Il Giornale di chirurgia. 2014;35(11–12):283–9. [PMC free article] [PubMed] [Google Scholar]
- 123. Lo X, Li K, Fok BKL, Poon MCM, Cheung MHY, Li RSK, et al. Protocol‐driven self‐expanding metallic stenting for malignant large‐bowel obstruction in a district hospital. Surg Pract. 2014;18(3):122–127. [Google Scholar]
- 124. Krstic S, Resanovic V, Alempijevic T, Resanovic A, Sijacki A, Djukic V, et al. Hartmann's procedure vs loop colostomy in the treatment of obstructive rectosigmoid cancer. World J Emerg Surg. 2014;9(1):52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Kamocki ZK, Zareba KP, Bandurski R, Baniukiewicz A, Wroblewski E, Gryko M, et al. Own experiences of endoscopic self‐expandable stent placement for malignant colorectal ileus. Videosurg Other Miniinvas Techn. 2014;9(1):59–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Young CJ, De‐Loyde KJ, Young JM, Solomon MJ, Chew EH, Byrne CM, et al. Improving quality of life for people with incurable large‐bowel obstruction: randomized control trial of colonic stent insertion. Dis Colon Rectum. 2015;58(9):838–49. [DOI] [PubMed] [Google Scholar]
- 127. Singh K, Narula AK, Thukral CL, Singh NR, Singh A, Kaur H. Role of CT colonography in colonic lesions and its correlation with conventional colonoscopic findings. J Clin Diagn Res. 2015;9(4):TC14‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Milek T, Ciostek P. Implantation of a new enteral stent in obstructive colorectal cancer using interventional radiology in patients over 70 years of age. Videosurg Other Miniinvas Tech. 2015;10(2):155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Lin BQ, Wang RL, Li QX, Chen W, Huang ZY. Investigation of treatment methods in obstructive colorectal cancer. J BUON. 2015;20(3):756–61. [PubMed] [Google Scholar]
- 130. Achiam MP, Logager V, Lund Rasmussen V, Okholm C, Mollerup T, Thomsen HS, et al. Perioperative colonic evaluation in patients with rectal cancer; MR colonography versus standard care. Acad Radiol. 2015;22(12):1522–8. [DOI] [PubMed] [Google Scholar]
- 131. Wan Y, Zhu YQ, Chen NW, Wang ZG, Cheng YS, Shi J. Comparison of through‐the‐scope stent insertion with standard stent insertion for the management of malignant colorectal obstruction: a prospective study. Tech Coloproctol. 2016;20(10):707–14. [DOI] [PubMed] [Google Scholar]
- 132. Haraguchi N, Ikeda M, Miyake M, Yamada T, Sakakibara Y, Mita E, et al. Colonic stenting as a bridge to surgery for obstructive colorectal cancer: advantages and disadvantages. Surg Today. 2016;46(11):1310–7. [DOI] [PubMed] [Google Scholar]
- 133. Enomoto T, Saida Y, Takabayashi K, Nagao S, Takeshita E, Watanabe R, et al. Open surgery versus laparoscopic surgery after stent insertion for obstructive colorectal cancer. Surg Today. 2016;46(12):1383–6. [DOI] [PubMed] [Google Scholar]
- 134. Li D, Du H, Shao G, Xu Y, Li R, Tian Q. Clinical application of transanal ileal tube placement using X‐ray monitoring. Oncol Lett. 2017;13(1):137–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Yamashita S, Tanemura M, Sawada G, Moon J, Shimizu Y, Yamaguchi T, et al. Impact of endoscopic stent insertion on detection of viable circulating tumor cells from obstructive colorectal cancer. Oncol Lett. 2018; 15(1): 400–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Arezzo A, Balague C, Targarona E, Borghi F, Giraudo G, Ghezzo L, et al. Colonic stenting as a bridge to surgery versus emergency surgery for malignant colonic obstruction: results of a multicentre randomised controlled trial (ESCO trial). Surg Endosc. 2017; 31(8): 3297–305. [DOI] [PubMed] [Google Scholar]
- 137. Kim E‐Y, Song H‐Y, Kim JC, Yoon YS, Ye BD, Nam DH, et al. MMP‐9 expression after metallic stent placement in patients with colorectal cancer: association with in‐stent restenosis. Radiology. 2014; 271(3): 901–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


