Abstract
Introduction
Feelings of anger and irritability are prominent symptoms of bipolar disorder (BD) that may occur during hypomanic, depressive and, especially, during mixed mood states. We aimed to determine whether such constructs are associated with the conversion to BD in subjects with a history of unipolar depression.
Methods
Data were derived from the depressed participants of Netherlands Study of Depression and Anxiety with 9 years of follow‐up. Hypomania was ascertained using the Composite International Diagnostic Interview at 2, 4, 6, and 9 years follow‐up. Cross‐sectionally, we studied the association between prevalent hypomania and anger related constructs with the “Spielberger Trait Anger subscale,” the “Anger Attacks” questionnaire, the cluster B personality traits part of the “Personality Disorder Questionnaire,” and “aggression reactivity.” Prospectively, we studied whether aggression reactivity predicted incident hypomania using Cox regression analyses.
Results
Cross‐sectionally, the bipolar conversion group (n = 77) had significantly higher scores of trait anger and aggression reactivity, as well as a higher prevalence on “anger attacks,” “antisocial traits,” and “borderline traits” compared to current (n = 349) as well as remitted (n = 1159) depressive patients. In prospective analyses in 1744 participants, aggression reactivity predicted incident hypomania (n = 28), with a multivariate‐adjusted hazard ratio of 1.4 (95% confidence interval: 1.02–1.93; p = .037).
Conclusion
Anger is a risk factor for conversion from unipolar depression to BD. In addition, patients who converted to BD showed on average more anger, agitation and irritability than people with a history of unipolar depression who had not converted.
Keywords: aggression, anger, bipolar disorder, conversion, hypomania, irritability, prospective study
1. INTRODUCTION
Bipolar disorder (BD) is a severe and debilitating mood disorder, characterized by hypomanic and depressive episodes (Judd et al., 2003). Most patients with BD have experienced one or more episodes of depression before the onset of hypomania (Gilman et al., 2012; Perlis et al., 2005), and as a consequence are initially diagnosed with an unipolar depression. Since the treatment for unipolar depression is different from BD and may instigate hypomania (Bowden, 2005), earlier detection of a vulnerability to BD would benefit these patients. Moreover, risk factors for the conversion to BD may yield anchor points for psychological interventions, for early recognition and appropriate treatment.
Previous studies showed that a parental history of BD, more severe depression, comorbid psychotic symptoms, childhood trauma and atypical symptoms of depression were risk factors for a conversion from unipolar to BD (Dom & Moggi, 2014; Gilman et al., 2012; Perlis et al., 2006). Irritability and anger in unipolar depression appeared to be a robust clinical marker of undiagnosed or subthreshold BD, or so‐called bipolar spectrum illness (Benazzi & Akiskal, 2005; Benazzi, 2005). It is important to examine the association between anger and BD, because of its impact on the patient and family and loved ones. Knowing there is an association can help us to target treatment. It is also important to properly investigate whether experiencing irritability/anger would have predictive value in the development of BD.
Anger can be divided into feelings and expressions. The feeling of anger involves different constructs, encompassing: trait‐ and state anger (Deffenbacher et al., 1996; Spielberger, Reheiser et al., 1995). Trait anger is defined by the constant tendency to experience anger upon the slightest provocation. It is a chronic condition that is intertwined in one's personality. A high level of anger can be a personality trait (Williams, 2017). State anger is defined as the temporary psychological, emotional feeling at a particular time and situation that can vary in intensity from mild irritation to intense fury and rage. These angry feelings could lead to the expression of anger including anger attacks and aggression. Attacks are spells of anger of a sudden surge of autonomic arousal with symptoms, such as tachycardia, sweating, flushing, and a feeling of being out of control. They are experienced as uncharacteristic and may occur in inappropriate situations (Fava et al., 1990). Anger attacks are associated with verbal and physical aggression, which in turn can cause social avoidance to prevent a future anger attack and has certainly a negative impact on interpersonal relations (Fava et al., 1993). All emotional states of anger, agitation and irritability will be referred to as anger in the current paper.
Anger might be part of emotion regulation problems and it has been hypothesized that heightened emotionality is an enduring characteristic of BD (Henry et al., 2008). This suggests that people with BD experience more intense and more frequently fluctuating negative and positive emotions (apart from their mood episodes). This might increase their risk of developing mood episodes. Most previous studies found cross‐sectional associations between anger and bipolarity (Abrams & Taylor, 1980; Ballester et al., 2012; Benazzi & Akiskal, 2006; Mammen et al., 2004; Perlis et al., 2004). In one prospective study (255 BD, 85 non‐BP psychopathology and 84 healthy controls) BD patients reported persistently higher scores on self‐report questionnaires on anger and feelings of aggression compared to psychiatric and healthy controls across a four‐year follow‐up (Ballester et al., 2014). There are indications that people with BD show stronger emotional reactivity compared to healthy controls on self‐report questionnaires (Aas et al., 2015), or specifically report more anger and frustration during euthymic states (Dutra et al., 2014; Johnson & Carver, 2016), but contradictory findings have been reported as well (Edge et al., 2013).
Emotional instability in BD is often mistaken for comorbid personality disorder, since this is such a core characteristic of especially cluster B personality disorders. Ecological momentary assessments (EMA) studies have shown that BD patients in remission report more overall negative affect (Gruber et al., 2013; Havermans et al., 2010) and more fluctuations in both negative and positive emotionality compared to healthy controls (Knowles et al., 2007). Earlier cross‐sectional studies have found that some of the symptoms of BD (e.g., irritability, anger, and emotional instability) overlap with personality disorders, such as borderline personality disorder and antisocial personality disorder (Bauer & Pfennig, 2005; Kolla et al., 2017). In total, 44% of patients diagnosed with borderline personality disorder were found to meet strict diagnostic criteria for BD (Deltito et al., 2001). Moreover, 55% of newly diagnosed BD patients (without comorbid personality disorder) showed signs of juvenile antisocial behavior in a retrospective study (Barzman et al., 2007). These findings suggest that borderline and antisocial personality disorders have construct overlap with BD. Especially affective instability and impulsivity were traits that may link BD to personality disorders (Renaud et al., 2012).
In sum, the majority of the studies have shown a relation between BD and emotional instability, and specifically of anger, also in stable periods. In the current study, we investigated whether patients who converted to BD showed more feelings of anger, irritability and antisocial and borderline personality traits than people with a history of unipolar depression who did not convert. Second, we aimed to determine whether increased aggression reactivity increases the risk of conversion from depression to BD.
2. METHODS
2.1. Study sample
Data were derived from the Netherlands Study of Depression and Anxiety (NESDA) with measurement points at baseline and at the 2‐, 4‐, 6‐, and 9‐year follow‐up. NESDA is an ongoing longitudinal cohort study, consisting of 2,981 participants (18–65 years). Participants were recruited at baseline from community care (19%), primary care (54%), and specialized mental health care (27%) in the Netherlands. Individuals included in the NESDA study were participants with current or remitted depressive disorders and/or comorbid anxiety. The control group consisted of participants without lifetime psychiatric disorders. Exclusion criteria included (1) the presence of other psychiatric disorders (e.g., psychotic, obsessive–compulsive, bipolar, or severe addiction disorder) and (2) not being fluent in Dutch. Participants gave written informed consent before enrollment, and ethical approval was granted by all ethical committees of participating universities (VU University Medical Center, Leiden University Medical Center and University Medical Center Groningen). A detailed description of NESDA is given elsewhere (Penninx et al., 2008).
Specially trained research staff administered the diagnostic interviews using the Composite International Diagnostic Interview (CIDI; version 2.1) to assess remitted or current depressive disorders and incidents of hypomania which is indicative for BD. In the current study, we analyzed data cross‐sectionally and prospectively with survival analysis.
Cross‐sectional analysis sample: data on anger related questionnaires (i.e., trait anger, aggression reactivity, anger attacks, and personality traits associated with more anger) were gathered only at the fourth wave at 4‐year follow‐up. Therefore, we selected participants who completed the fourth wave (n = 2,402; 80.6%) to examine the construct of anger cross‐sectionally. Participants suffering from a remitted and current depressive disorder and BD patients who converted between baseline and 4 years of follow‐up were included. In a previous NESDA study (de Bles et al., 2019), healthy controls showed significantly less trait anger and had lowest prevalence of anger attacks compared with groups of depression with or without comorbid anxiety disorder. For this reason, healthy controls were excluded in the current study. Participants with missing data on questionnaires regarding (hypo)manic episodes, or on one of the anger‐related questionnaires were excluded, resulting in a total sample of 1585 (53.2%) of the 2,981 participants for the cross‐sectional analyses (see Flowchart in Figure 1).
Figure 1.
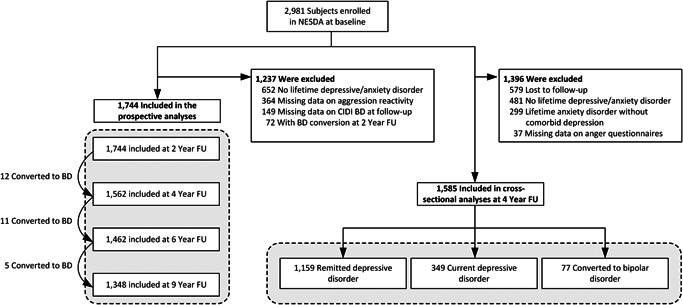
Flowchart of included participants in prospective and cross‐sectional analyses. BD, bipolar disorder; FU, follow up; NESDA, Netherlands Study of Depression and Anxiety
Prospective analysis sample: aggression reactivity questionnaire was the only measured anger related instrument at baseline. Therefore, aggression reactivity was used as the predictor for incident (hypo)mania during the 9 years of follow‐ups. We included 1744 (58.5%) of 2981 participants, with remitted or current depressive disorder with at least one follow‐up assessment (Figure 1).
2.2. Measures
2.2.1. Aggression reactivity
This questionnaire was used in prospective analysis as predictor and in cross‐sectional as one of the anger‐related constructs. It was measured with the aggression reactivity subscale of the Leiden index of depression sensitivity–revised (LEIDS‐R; Van der Does, 2002, 2005). The LEIDS‐R contains 34 items with six subscales. Aggression reactivity is one of these subscales and has six items (e.g., “In a sad mood, I do more things that I will later regret”; “When I feel bad, I feel like more breaking things”; “In a sad mood I'm more bothered by aggressive thoughts”; “When I feel down, I more easily become cynical or sarcastic”; “When I feel sad, I do more risky things”; “When feel down, I lose my temper more easily”). These items measure how people react in a sad mood. Items are answered on a five‐point Likert scale from 0 to 4, with total scores ranging from 0 to 24. The internal consistency (Cronbach's alpha) for the aggression reactivity subscale was 0.80 in the current NESDA sample.
2.2.2. CIDI hypomanic episodes
The CIDI (WHO version 2.1) is a comprehensive, fully standardized diagnostic interview to screen for mental disorders based on diagnostic and statistical manual of mental disorder‐fourth edition(DSM‐IV) criteria. The CIDI was used to assess remitted or current depressive disorders in the preceding 6 months. Incident cases of hypomanic episodes, which were indicative of BD, were ascertained using the CIDI “bipolar” section. The CIDI has high interrater reliability, (BDI: κ = 0.92, BDII: κ = 0.94; Wittchen et al., 1991) and is a valid instrument (diagnosis of a lifetime BD sensitivity 0.87 and specificity 0.89; Lecrubier et al., 1997) for yielding DSM‐IV diagnoses.
2.2.3. Trait anger
Trait anger was assessed via the Dutch adaption of the Spielberger state–trait anger scale (STAS; Spielberger 1980; Van der Ploeg et al., 1982) and was gathered at the fourth wave at 4‐year follow‐up. The STAS is divided into two subscales for state and trait anger, whereby only the latter was administered in the current study. Trait anger is described as anger proneness as a personality trait (Spielberger et al., 1988). The trait anger scale is a 10‐item, self‐report questionnaire. Participants score items on a four‐point Likert scale from 1 to 4. The total sum score ranges from 10 to 40. Psychometric properties have shown good item correlations, high test‐retest reliability, and high internal consistency values with Cronbach's alphas ranging from 0.75 to 0.91 (Spielberger 1980; Van der Ploeg et al., 1982). The internal consistency (i.e., Cronbach's alpha) in our sample was 0.89.
2.2.4. Anger attacks
The anger attacks questionnaire (Fava et al., 1993) is a self‐rated instrument used to measure the presence or absence of anger attacks during the previous 6 months. It was measured at the fourth wave at 4‐year follow‐up. Anger attacks are sudden spells of anger inappropriate to the situation, accompanied by irritability, a sense of being out of control, and autonomic arousal symptoms (Fava et al., 1993). To define who was experiencing anger attacks, the following criteria had to be met the previous 6 months: (1) irritability, (2) overreaction to minor annoyances, (3) inappropriate anger and rage directed at others, (4) incidence of at least one anger attack within the past month, and (5) presence of at least four or more of the following symptoms in at least one of the attacks: tachycardia, hot flashes, tightness of the chest, paresthesia, dizziness, shortness of breath, sweating, trembling, panic, feeling out of control, feeling like attacking others, attacking physically or verbally, and throwing or destroying objects.
2.2.5. Cluster B personality traits
Antisocial behavior was assessed with the Dutch adaptation of the personality disorder questionnaire (PDQ‐4; Hyler et al., 1988) and data was gathered at the fourth wave at 4‐year follow‐up. It was used to identify the key features or possible presence of a personality disorder. Items included in the PDQ‐4 were adapted from the diagnostic criteria for personality disorders of the DSM‐IV (APA, 1994). In the current study, a shortened version of the PDQ‐4 with 37 dichotomous (“true”/”false”) was assessed. Items were divided into three subcategories; borderline personality disorder (15 items; e.g., “I have difficulty controlling my anger or temper”); antisocial personality disorder (eight items; e.g., “I don't care if others get hurt so long as I get what I want”) and antisocial behavior before the age of fifteen (14 items; e.g. “I was considered a bully”). Based on items of the subscales for borderline and antisocial personality traits the presence or absence of these symptomatology and characteristics was assessed. The PDQ‐4 has a high sensitivity and moderate specificity (Cronbach's alpha = 0.97; Stringer et al., 2013), and a test–retest reliability of 0.67 (Furnham et al., 2014).
2.2.6. Covariates
Sociodemographic covariates were self‐reported age, gender, and level of education in years. Lifetime DSM IV‐based alcohol dependency and abuse and drug use were assessed using the CIDI. In addition, the severity of depression during the past week was assessed with the 30‐item self‐report inventory of depressive symptomatology (IDS; Rush et al., 1996). Items were scored on a four‐point Likert scale (0–3) with total sum score ranges from 0 to 84 (only 28 of the 30 items are rated) The IDS had good internal reliability (Cronbach's alpha = 0.85). This is a 21‐item self‐report inventory with an internal consistency (Cronbach's alpha) of 0.92 (Beck et al., 1988). Comorbid current anxiety use was assessed with CIDI.
2.3. Statistical analyses
Sociodemographic and clinical characteristics were summarized according to CIDI using descriptive statistics. Missing values of BMI and smoking status were imputed with the respective values from the previous wave.
2.3.1. Cross‐sectional analyses
The CIDI was used to assess remitted or current depressive disorders and incident hypomanic episodes in the previous two years for cross‐sectional analysis at the fourth wave at 4‐year follow‐up. Upon completing the CIDI, participants were categorized into one of the following two psychopathology groups: remitted‐ and current depression. In these two groups a number of participants had experienced a hypomanic episode between baseline and 4‐year follow‐up, thus being classified in the BD converted group. We used analysis of variance to compare the mean levels of the continuous variables trait anger and aggression reactivity, and chi‐squared tests were used to compare the prevalence of the dichotomous variables anger attacks, antisocial and borderline personality traits among the three psychopathology groups (i.e., remitted depression, current depression, converted BD group). Furthermore, analyses were repeated for marginal means, resulting from adjustment for gender, age, level of education, alcohol and drugs use, severity of depressive symptoms and comorbid anxiety disorder using analysis of covariance (ANCOVA) and multivariable logistic regression analyses, when appropriate. The results of these analyses were presented in forest plots.
Moreover, multivariate linear regression analysis was used to analyze all the individual items of all the anger constructs (i.e., trait anger, aggression reactivity, anger attacks, and personality traits associated with more anger). Individual items estimated betas (with error bars representing 95% confidence intervla [CI]) were summarized and presented in supplementary forest plots. These were sorted by the size of each estimated beta for each construct separately.
2.3.2. Prospective analyses
At baseline, patients with a self‐reported or with a professionally reported primary clinical diagnosis of BD were excluded. As the BD section of the CIDI was not conducted at baseline, we applied a lag‐time analysis of 2 years, excluding all incident cases of hypomanic cases based on the CIDI between baseline and 2‐year follow‐up. In 1744 participants, 28 experienced CIDI‐confirmed incident hypomania during follow‐up (between 2 and 9 years). Kaplan–Meier analysis was used to examine the relationship between baseline aggression reactivity and conversion to BD. Hazard ratios (HR) with 95% CI of conversion to BD were estimated by Cox proportional hazards models. The date of inclusion into the cohort was considered the baseline for each patient in the survival analysis. The primary endpoint consisted of all incident cases during the follow‐up period, the survival time, and the diagnoses at each time point based on the CIDI. All follow‐up losses as well as patients who did not experience a hypomanic episode were censored. We estimated three models: (a) a crude model that did not include any covariates, (b) an adjusted model that included gender, age, and level of education, and (c) a fully adjusted model that also included alcohol dependency, severity of depression symptoms and comorbid anxiety disorder. We tested for a linear trend across tertiles of incidents of hypomania.
Multivariable logistic and Cox regression analyses and ANCOVA were performed using IBM SPSS statistical software (version 25; IBM Corp.). The analyses regarding individual items and forest plots were computed using the R statistical software, version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria, 2016. URL: https://www.R-project.org/). A two‐sided p value was considered statistically significant at the 0.05 level.
3. RESULTS
3.1. Cross‐sectional results
Demographic and clinical characteristics on (hypo)manic episodes of wave 4 (at 4 years follow‐up) are shown in Table 1. Participants (N = 1585) were on average 46.3 years old (SD = 12.6) and 68.8% were female. There were 77 (4.9%) patients who had converted from unipolar depression to BD based on CIDI during the two through four year waves (Table 1). There were no notable differences found in the sociodemographic between the groups. Patients with current depressive disorder showed more severe symptoms of depression compared with the other two groups. The group of converted patients smoked more often and suffered more from alcohol dependency than the two other groups. These patients also used more benzodiazepines, selective serotonin reuptake inhibitors, and psychotropic medication compared to other groups.
Table 1.
Baseline characteristics of the study sample
| 4 year (wave 4) characteristic (N = 1585) | ||||
|---|---|---|---|---|
| Baseline characteristic (N = 1744) | Remitted depressive disorder (n = 1159) | Current depressive disorder (n = 349) | Converted group bipolar disorder (n = 77) | |
| All sociodemographic | ||||
| Female sex, no. (%) | 1,290 (68.3%) | 796 (68.7%) | 253 (72.5%) | 41 (53.2%) |
| Age in years, mean (SD) | 42.5 (12.6) | 46.2 (12.7) | 47.0 (12.3) | 44.8 (11.2) |
| Education, in years, mean (SD) | 12.1 (3.3) | 12.7 (3.3) | 12.2 (3.3) | 12.2 (3.3) |
| Body mass index (BMI), in kg/m2, mean (SD) | 25.7 (5.1) | 26.3 (5.0) | 26.4 (5.5) | 26.9 (5.7) |
| Smoking, no. (%) | 737 (39.0%) | 371 (32.0%) | 129 (37.0%) | 34 (44.2%) |
| Alcohol dependency, no. (%) | 549 (29.1%) | 75 (6.5%) | 42 (12.0%) | 11 (14.3%) |
| Clinical characteristics | ||||
| Severity depression IDS‐SR total score, mean (SD) | 33.03 (2.45) | 14.95 (9.79) | 29.45 (12.63) | 24.70 (13.55) |
| Medication use, no. (%) | ||||
| Benzodiazepines | 335 (17.7%) | 124 (10.7%) | 86 (24.6%) | 20 (26.0%) |
| Selective serotonin reuptake inhibitors | 411 (21.8%) | 186 (16.0%) | 65 (18.6%) | 17 (22.1%) |
| Tricyclic antidepressants | 63 (3.3%) | 30 (2.6%) | 17 (2.9%) | 5 (6.5%) |
| Other antidepressants | 129 (6.8%) | 64 (5.5%) | 46 (13.2%) | 8 (10.4%) |
Note: Data are means (with standard errors in parentheses) or number of participants (with percentages in parentheses).
Abbreviation: IDS‐SR, inventory of depressive symptomatology, self‐report.
Significant differences were present in the crude model for all anger constructs among the three groups (all p's < .001). The between differences persisted the adjusted models in continuous variables (see forest plot in Figure 2) with (F (2, 1582) = 8.20, p < .001 for trait anger; F (2, 1456) = 5.61, p = .004 for aggression reactivity. In the adjusted models, patients who were converted had the highest marginal mean levels on trait anger and aggression reactivity in comparison with remitted patients with a mean difference; (MD = 1.87, SE = 0.6, p = .001) for trait anger, and (MD = 1.76, SE = 0.5, p = .001) for aggression reactivity and current depressed patients (MD = 2.35, SE = 0.6, p < .001) for trait anger, (MD = 1.71, SE = 0.6, p = .002) for aggression reactivity.
Figure 2.
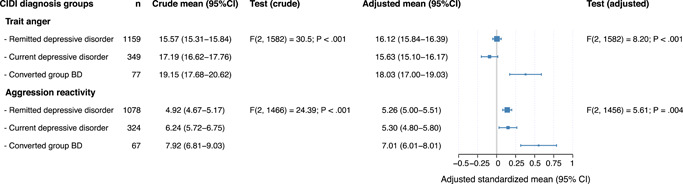
Forest plot showing the estimated marginal means (with 95% confidence interval [CI]) of trait anger and aggression reactivity according to three diagnoses groups. The adjusted analyses were adjusted for gender, age, level of education, alcohol dependency, drugs use, severity of depressive symptoms, and comorbid anxiety disorder
Results of adjusted analysis in categorical variables (see forest plot in Figure 3) were also significant with χ 2 (2) = 4.55, p = .041 for anger attacks; χ 2 (2) = 5.12, p = .02 for antisocial personality traits; and χ 2 (2) = 10.41, p = .001 for borderline personality traits. Furthermore, the converted group also had the highest prevalence of anger attacks (22.1%), antisocial personality traits (9.1%) and borderline personality traits (36.4%) compared to those with remitted and current depression.
Figure 3.
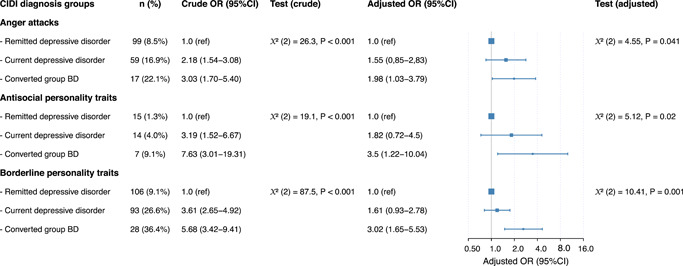
Forest plot showing (adjusted) odds ratios (OR) of anger attacks, antisocial and borderline personality traits according to three diagnoses groups. The adjusted analyses were adjusted for gender, age, level of education, alcohol dependency, drugs use, severity of depressive symptoms, and comorbid anxiety disorder. CI, confidence interval
Results of the individual items of constructs (Figures S1–S5) with estimated betas and 95% CI show that anger attack items measuring physical sensation and anger items were most strongly associated with hypomania. Moreover, almost all the items of PDQ borderline personality disorder‐subscale were statistically significantly associated with hypomania, and were more prominently associated than the other anger constructs. It was also notable that specifically the items that measure impulsiveness were strongly associated, rather than items that measure anti‐sociability, such as bullying or harming other people.
3.2. Prospective results
Baseline characteristics are summarized in Table 1. The subjects at baseline (n = 1744) were on average 42.5 years of age (SD = 12.6) and were predominantly female (68.3%). The sample consisted of 560 (29.7%) patients with remitted depressive and/or anxiety disorder and 1.328 (70.3%) patients with a current depressive and/or anxiety disorder. Based on CIDI 28 cases of hypomanic episodes were identified, signaling conversion to BD, from 2 to 9 years of follow‐up. Relatively smaller number of incident cases of (hypo)mania in prospective analysis compared with cross‐sectional analysis (28 vs. 77) is due to the exclusion of all the cases between baseline and 2 years of follow‐up in prospective analysis to exclude all prevalent cases from the prospective analysis.
Kaplan–Meier analysis of survival with the incident hypomanic episode as outcome showed that patients with higher levels of aggression reactivity had higher conversion rates compared to patients with lower levels of aggression reactivity (Figure 4). This association is also displayed in Table 2; showing that, compared to patients in the lower tertile of aggression reactivity (low is reference with HRs of 1 and intermediate with HRs of 1.34), those in the top tertile had a higher rate (HRs of 4.63) of incident cases of hypomania. In the fully adjusted model, aggression reactivity was a significant predictor, with an HRs 1.4 (95% CI, 1.02–1.93; p = .037) per 1‐SD increase in aggression reactivity.
Figure 4.
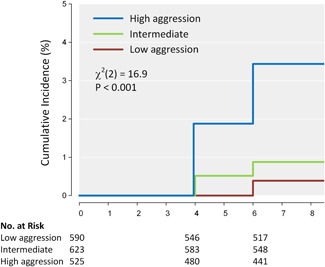
Kaplan–Meier curves of incident hypomania according to tertiles of aggression reactivity. p Value by log‐rank Mantel–Cox test
Table 2.
Tertiles of aggression reactivity as a predictor of incident of hypomania in sample of patients with depression and/or anxiety disorder
| Lower scores | Intermediate scores | Higher scores | p Value for trend a | |
|---|---|---|---|---|
| Tertiles of aggression reactivity | ||||
| Participants, no. | 590 | 623 | 525 | |
| Cases, no. (%) | 4 (0.7%) | 6 (1.0%) | 18 (3.4%) | |
| Hazard ratio (95% confidence interval) | ||||
| Crude | 1.0 (ref) | 1.41 (0.40–4.99) | 5.27 (1.79–15.6) | <.001 |
| Adjustedb | 1.0 (ref) | 1.37 (0.39–4.88) | 4.87 (1.63–14.6) | <.001 |
| Fully adjusted modelc | 1.0 (ref) | 1.34 (0.37–4.69) | 4.63 (1.54–13.9) | .037 |
| Continuous aggression reactivity (z‐value) | ||||
| Hazard ratio (95% confidence interval) | ||||
| Crude | 1.84 (1.41–2.41) | <.001 | ||
| Adjustedb | 1.78 (1.36–2.35) | <.001 | ||
| Fully adjusted modelc | 1.4 (1.02–1.93) | .037 | ||
Data obtained by an analysis of variance for trend, linear term.
Adjusted for gender, age, level of education.
Additionally adjusted for alcohol dependence and severity of depression symptoms (IDS).
4. DISCUSSION
The purpose of this study was first to examine the association of different constructs of anger with BD; and second to determine the predictive role of aggression reactivity in conversion to BD. Our study demonstrated a strong and consistent finding in the prospective as well as in the cross‐sectional analyses. We found that higher levels of anger in all its variants were consistently associated with bipolarity versus those with a history of unipolar depression. Second, we found that aggression reactivity was predictive of conversion to BD.
Cross‐sectionally, all the different constructs of anger and affective instability (i.e., trait anger, aggression reactivity, anger attacks, and personality traits associated with more anger) showed consistent associations, with the strongest association and highest prevalence in the converted group in comparison to the remitted and current depression groups. These results were in line with previous findings showing that BD patients scored higher on anger‐related measures (Dutra et al., 2014; Perlis et al., 2004) in comparison to unipolar depressed groups.
Regarding our prospective findings, we found that aggression reactivity was a risk factor for the conversion to BD in persons with a history of unipolar depression. Although two earlier prospective studies (Ballester et al., 2014; Dutra et al., 2014) showed that feelings of anger were more frequent during the follow‐up waves in BD patients in comparison with subjects with other psychiatric disorders and healthy controls, we are not aware of previous studies that examined the predictive value of an anger construct in relation to conversion to BD.
Affective instability and dysregulation in general seem to be distinctive factors for BD compared to unipolar depression in the current sample, since our results show that both antisocial‐ and borderline personality traits were more prevalent in the BD conversion group than in the currently depressed and remitted unipolar depression group. Results were most striking for the borderline traits, which is in line with previous findings showing that emotional instability is a core characteristic in both BD and borderline personality disorder. (Deltito et al., 2001) suggest that the current classification may fail to differentiate between the two disorders considering the complexity and heterogeneity within these patient groups and that perhaps borderline and bipolar might be the two extremes of the same spectrum (Deltito et al., 2001). Additionally, a longitudinal study showed that comorbid borderline and antisocial personality traits predicted the risk of aggression in BD, while controlling for potential confounding factors (Garno et al., 2008).
Whether emotion regulation problems are more characteristic for BD than unipolar depression is unclear, since the few studies into this topic had contradicting results (Becerra et al., 2015; Rive et al., 2015). We might carefully conclude, based on the current and previous findings, that especially anger and aggression dysregulation are the most distinct affective characteristics for BD when compared to unipolar depression. One important explanation for this finding might be the occurrence of mixed mood states. Although results are not fully conclusive, agitated depression or mixed depression (i.e., depressed episodes with the simultaneous presence of several manic symptoms, like irritability) in unipolar depression might be one of the early signs of conversion to BD since mixed episodes are more prevalent in BD (Vázquez et al., 2018). However, it is unclear to what extent the current and previous findings are associated with the increased occurrence of mixed mood states in BD patients.
Another potential explanation for the more distinct problems in regulation of anger in BD patients compared to unipolar depression patients might reside in differences in emotion regulation styles. Although most dysfunctional emotion regulation styles are comparable between BD and unipolar depression patients (e.g., rumination and catastrophizing) (Fletcher et al., 2013; Fuhr et al., 2014) there are indications for important differences. Both on the cognitive and behavioral levels, BD patients seem to have the tendency to upregulate activated mood states. For instance, (Kelly et al., 2011) showed that positive appraisal about activated states predicted BD (in a sample with BD, unipolar depression and healthy controls). BD patients also seem to have more extreme positive self‐relevant appraisals of the feelings of activation than healthy controls and unipolar depressed patients (Mansell et al., 2011; Tosun et al., 2015). Additionally, at least a subgroup of the bipolar patients are more likely to engage in stimulating and activating behavior that potentially induces a hypomanic episodes; (Lee, Lam, Mansell, & Farmer, 2010). Although previous studies focussed specifically on activated states, such as happiness or euphoria, anger can also be considered as an activated mood state as well.
Feelings of anger might be an important target for early recognition of illness and intervention in BD. Increased feelings of anger in unipolar patients in combination with some other known clinical characteristics, such as multiple brief depressed episodes, a lack of response to antidepressants, a family history of BD (Ghaemi et al., 2000) might help to signal an upcoming conversion to BD. In addition, agitated affective states in BD patients deserve attention for its own sake, as these may have negative consequences for their quality of life and that of their loved ones (Lee Mortensen et al., 2015). Since, BD patients experience extensive emotional instability even during euthymic states (Henry et al., 2008) and seem to use maladaptive strategies (Dodd et al., 2019), it is important that they learn to regulate such feelings in an appropriate way. Psychotherapy, social therapy, and group‐oriented approaches can help BD patients to prevent decompensation and to develop healthier social relationships. Other treatment strategies that may especially be apt to improve emotion regulation are dialectical behavior therapy and systems training for emotional predictability and problem solving program, which is based on cognitive behavioral therapy combined with emotional management skill training (Eisner et al., 2017; Van Dijk et al., 2013).
One of the strengths of this study is its longitudinal design and the inclusion of a large group of participants that oversampled patients with (preceding) depression. This is the first study that investigated prospectively the predictive value of feelings of anger in conversion to BD. In addition, this is the first study that examined five different constructs of anger in relation to BD, with strong and consistent findings. There are also limitations that need to be addressed. First, the primary focus of this prospective cohort study on unipolar rather than bipolar depression resulted in a relatively small sample of patients who experienced a hypomanic episode during follow‐up. Second, even though we adjusted for potential confounders, a family history of BD was not assessed and could not be included as cofounder. Third, the current use of antipsychotic medication and mood stabilizers might have had a dampening effect on anger and aggression, leading to an underestimation rather than an overestimation of our results (Masand et al., 2017). However, the group taking these medications was fairly small. Finally, participants who dropped out or missed scales at follow‐ups had probably higher risk of anger or irritability. Exclusion of this specific group might have led to underestimation of our results.
We can conclude that aggression reactivity is a robust risk factor for the conversion from unipolar to BD. In addition, patients who had experienced hypomania and thus had converted to BD showed more feelings of anger in comparison with unipolar depressive patients. Identifying the potential risk factors for the development of BD might have clinical value in earlier recognition, prevention of conversion into mania, and better targeted interventions.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
Supporting information
Supporting information.
ACKNOWLEDGMENTS
The infrastructure for the NESDA study (www.nesda.nl) is funded through the Geestkracht program of the Netherlands Organization for Health Research and Development (ZonMw, grant number 10‐000‐1002) and financial contributions by participating universities and mental health care organizations (VU University Medical Center, GGZ inGeest, Leiden University Medical Center, Leiden University, GGZ Rivierduinen, University Medical Center Groningen, University of Groningen, Lentis, GGZ Friesland, GGZ Drenthe, Rob Giel Onderzoekscentrum).
Mesbah R, de Bles N, Rius‐Ottenheim N, et al. Anger and cluster B personality traits and the conversion from unipolar depression to bipolar disorder. Depression Anxiety. 2021;38:671–681. 10.1002/da.23137
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Aas, M. , Aminoff, S. R. , Vik Lagerberg, T. , Etain, B. , Agartz, I. , Andreassen, O. A. , & Melle, I. (2014). Affective lability in patients with bipolar disorders is associated with high levels of childhood trauma. Psychiatry Research, 218(1‐2), 252–255. [DOI] [PubMed] [Google Scholar]
- Aas, M. , Pedersen, G. , Henry, C. , Bjella, T. , Bellivier, F. , Leboyer, M. , Kahn, J.‐P. , Cohen, R. F. , Gard, S. , Aminoff, S. R. , Lagerberg, T. V. , Andreassen, O. A. , Melle, I. , & Etain, B. (2015). Psychometric properties of the affective lability scale (54 and 18‐item version) in patients with bipolar disorder, first‐degree relatives, and healthy controls. Journal of Affective Disorders, 172, 375–380. [DOI] [PubMed] [Google Scholar]
- Abrams, R. , & Taylor, M. A. (1980). A comparison of unipolar and bipolar depressive illness. The American Journal of Psychiatry, 137(9), 1084–1087. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). [Google Scholar]
- Ballester, J. , Goldstein, B. , Goldstein, T. R. , Yu, H. , Axelson, D. , Monk, K. , Hickey, M. B. , Diler, R. S. , Sakolsky, D. J. , Sparks, G. , Iyengar, S. , Kupfer, D. J. , Brent, D. A. , & Birmaher, B. (2014). Prospective longitudinal course of aggression among adults with bipolar disorder. Bipolar Disorders, 16(3), 262–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballester, J. , Goldstein, T. , Goldstein, B. , Obreja, M. , Axelson, D. , Monk, K. , Hickey, M. , Iyengar, S. , Farchione, T. , Kupfer, D. J. , Brent, D. , & Birmaher, B. (2012). Is bipolar disorder specifically associated with aggression? Bipolar Disorders, 14(3), 283–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barzman, D. H. , DelBello, M. P. , Fleck, D. E. , Lehmkuhl, H. , & Strakowski, S. M. (2007). Rates, types, and psychosocial correlates of legal charges in adolescents with newly diagnosed bipolar disorder. Bipolar Disorders, 9(4), 339–344. [DOI] [PubMed] [Google Scholar]
- Bauer, M. , & Pfennig, A. (2005). Epidemiology of bipolar disorders. Epilepsia, 46(Suppl 4), 8–13. [DOI] [PubMed] [Google Scholar]
- Becerra, R. , Cruise, K. , Harms, C. , Allan, A. , Bassett, D. , Hood, S. , & Murray, G. (2015). Emotion regulation and residual depression predict psychosocial functioning in bipolar disorder: Preliminary study. Universitas Psychologica, 14(3), 855–864. [Google Scholar]
- Beck, A. T. , Epstein, N. , Brown, G. , & Steer, R. A. (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56(6), 893–897. [DOI] [PubMed] [Google Scholar]
- Benazzi, F. (2005). Possible bipolar nature of irritability in major depressive disorder. The Journal of Clinical Psychiatry, 66(8), 1072–1073. [DOI] [PubMed] [Google Scholar]
- Benazzi, F. , & Akiskal, H. (2005). Irritable‐hostile depression: Further validation as a bipolar depressive mixed state. Journal of Affective Disorders, 84(2‐3), 197–207. [DOI] [PubMed] [Google Scholar]
- Benazzi, F. , & Akiskal, H. S. (2006). Psychometric delineation of the most discriminant symptoms of depressive mixed states. Psychiatry Research, 141(1), 81–88. [DOI] [PubMed] [Google Scholar]
- Bowden, C. L. (2005). A different depression: Clinical distinctions between bipolar and unipolar depression. Journal of Affective Disorders, 84(2‐3), 117–125. [DOI] [PubMed] [Google Scholar]
- de Bles, N. J. , Rius Ottenheim, N. , van Hemert, A. M. , Pütz, L. E. H. , van der Does, A. J. W. , Penninx, B. W. J. H. , & Giltay, E. J. (2019). Trait anger and anger attacks in relation to depressive and anxiety disorders. Journal of Affective Disorders, 259, 259–265. [DOI] [PubMed] [Google Scholar]
- Deffenbacher, J. L. , Oetting, E. R. , Thwaites, G. A. , Lynch, R. S. , Baker, D. A. , Stark, R. S. , Thacker, S. , & Eiswerth‐Cox, L. (1996). State‐trait anger theory and the utility of the trait anger scale. Journal of Counseling Psychology, 43(2), 131–148. [Google Scholar]
- Deltito, J. , Martin, L. , Riefkohl, J. , Austria, B. , Kissilenko, A. , Corless, C. , & Morse, P. (2001). Do patients with borderline personality disorder belong to the bipolar spectrum? Journal of Affective Disorders, 67(1‐3), 221–228. [DOI] [PubMed] [Google Scholar]
- Dodd, A. , Lockwood, E. , Mansell, W. , & Palmier‐Claus, J. (2019). Emotion regulation strategies in bipolar disorder: A systematic and critical review. Journal of Affective Disorders, 246, 262–284. [DOI] [PubMed] [Google Scholar]
- Dom, G. , & Moggi, F. (2014). Co‐occurring addictive and psychiatric disorders: A practice‐based handbook from a European perspective. Springer. [Google Scholar]
- Dutra, S. J. , Reeves, E. J. , Mauss, I. B. , & Gruber, J. (2014). Boiling at a different degree: an investigation of trait and state anger in remitted bipolar I disorder. Journal of Affective Disorders, 168, 37–43. [DOI] [PubMed] [Google Scholar]
- Edge, M. D. , Miller, C. J. , Muhtadie, L. , Johnson, S. L. , Carver, C. S. , Marquinez, N. , & Gotlib, I. H. (2013). People with bipolar I disorder report avoiding rewarding activities and dampening positive emotion. Journal of Affective Disorders, 146(3), 407–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisner, L. , Eddie, D. , Harley, R. , Jacobo, M. , Nierenberg, A. A. , & Deckersbach, T. (2017). Dialectical behavior therapy group skills training for bipolar disorder. Behavior Therapy, 48(4), 557–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fava, M. , Anderson, K. , & Rosenbaum, J. F. (1990). “Anger attacks”: Possible variants of panic and major depressive disorders. The American Journal of Psychiatry, 147(7), 867–870. [DOI] [PubMed] [Google Scholar]
- Fava, M. , Rosenbaum, J. F. , Pava, J. A. , McCarthy, M. K. , Steingard, R. J. , & Bouffides, E. (1993). Anger attacks in unipolar depression, Part 1: Clinical correlates and response to fluoxetine treatment. The American Journal of Psychiatry, 150(8), 1158–1163. [DOI] [PubMed] [Google Scholar]
- Fletcher, K. , Parker, G. , & Manicavasagar, V. (2013). Behavioral activation system (BAS) differences in bipolar I and II disorder. Journal of Affective Disorders, 151(1), 121–128. [DOI] [PubMed] [Google Scholar]
- Fuhr, K. , Hautzinger, M. , & Meyer, T. D. (2014). Implicit motives and cognitive variables: Specific links to vulnerability for unipolar or bipolar disorder. Psychiatry Research, 215(1), 61–68. [DOI] [PubMed] [Google Scholar]
- Furnham, A. , Milner, R. , Akhtar, R. , & De Fruyt, F. (2014). A review of the measures designed to assess DSM‐5 personality disorders. Psychology, 5(14), 1646–1686. [Google Scholar]
- Garno, J. L. , Gunawardane, N. , & Goldberg, J. F. (2008). Predictors of trait aggression in bipolar disorder. Bipolar Disorders, 10(2), 285–292. [DOI] [PubMed] [Google Scholar]
- Ghaemi, S. N. , Nassir Ghaemi, S. , Boiman, E. E. , & Goodwin, F. K. (2000). Diagnosing bipolar disorder and the effect of antidepressants. The Journal of Clinical Psychiatry, 61(10), 804–808. [DOI] [PubMed] [Google Scholar]
- Gilman, S. E. , Dupuy, J. M. , & Perlis, R. H. (2012). Risks for the transition from major depressive disorder to bipolar disorder in the National Epidemiologic Survey on alcohol and related conditions. The Journal of Clinical Psychiatry, 73(6), 829–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber, J. , Kogan, A. , Mennin, D. , & Murray, G. (2013). Real‐world emotion? An experience‐sampling approach to emotion experience and regulation in bipolar I disorder. Journal of Abnormal Psychology, 122(4), 971–983. [DOI] [PubMed] [Google Scholar]
- Havermans, R. , Nicolson, N. A. , Berkhof, J. , & deVries, M. W. (2010). Mood reactivity to daily events in patients with remitted bipolar disorder. Psychiatry Research, 179(1), 47–52. [DOI] [PubMed] [Google Scholar]
- Henry, C. , Van den Bulke, D. , Bellivier, F. , Roy, I. , Swendsen, J. , M'Baïlara, K. , Siever, L. J. , & Leboyer, M. (2008). Affective lability and affect intensity as core dimensions of bipolar disorders during euthymic period. Psychiatry Research, 159(1‐2), 1–6. [DOI] [PubMed] [Google Scholar]
- Hyler, S. E. , Rieder, R. O. , Williams, J. B. W. , Spitzer, R. L. , Hendler, J. , & Lyons, M. (1988). The personality diagnostic questionnaire: Development and preliminary results. Journal of Personality Disorders, 2(3), 229–237. [Google Scholar]
- Johnson, S. L. , & Carver, C. S. (2016). Emotion‐relevant impulsivity predicts sustained anger and aggression after remission in bipolar I disorder. Journal of Affective Disorders, 189, 169–175. [DOI] [PubMed] [Google Scholar]
- Judd, L. L. , Akiskal, H. S. , Schettler, P. J. , Coryell, W. , Maser, J. , Rice, J. A. , Solomon, D. A. , & Keller, M. B. (2003). The comparative clinical phenotype and long term longitudinal episode course of bipolar I and II: A clinical spectrum or distinct disorders? Journal of Affective Disorders, 73(1‐2), 19–32. [DOI] [PubMed] [Google Scholar]
- Kelly, R. E. , Mansell, W. , Wood, A. M. , Alatiq, Y. , Dodd, A. , & Searson, R. (2011). Extreme positive and negative appraisals of activated states interact to discriminate bipolar disorder from unipolar depression and non‐clinical controls. Journal of Affective Disorders, 134(1‐3), 438–443. [DOI] [PubMed] [Google Scholar]
- Knowles, R. , Tai, S. , Jones, S. H. , Highfield, J. , Morriss, R. , & Bentall, R. P. (2007). Stability of self‐esteem in bipolar disorder: comparisons among remitted bipolar patients, remitted unipolar patients, and healthy controls 1. Bipolar Disorders, 9(5), 490–495. [DOI] [PubMed] [Google Scholar]
- Kolla, N. J. , Meyer, J. H. , Bagby, R. M. , & Brijmohan, A. (2017). Trait anger, physical aggression, and violent offending in antisocial and borderline personality disorders. Journal of Forensic Sciences, 62(1), 137–141. [DOI] [PubMed] [Google Scholar]
- Lecrubier, Y. , Sheehan, D. V. , Weiller, E. , Amorim, P. , Bonora, I. , Harnett Sheehan, K. , Janavs, J. , & Dunbar, G. C. (1997). The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry: The Journal of the Association of European Psychiatrists, 12(5), 224–231. [Google Scholar]
- Lee Mortensen, G. , Vinberg, M. , Lee Mortensen, S. , Balslev Jørgensen, M. , & Eberhard, J. (2015). Bipolar patients' quality of life in mixed states: A preliminary qualitative study. Psychopathology, 48(3), 192–201. [DOI] [PubMed] [Google Scholar]
- Lee, R. , Lam, D. , Mansell, W. , & Farmer, A. (2010). Sense of hyper‐positive self, goal‐attainment beliefs and coping strategies in bipolar I disorder. Psychological Medicine, 40(6), 967–975. [DOI] [PubMed] [Google Scholar]
- Mammen, O. K. , Pilkonis, P. A. , Chengappa, K. N. R. , & Kupfer, D. J. (2004). Anger attacks in bipolar depression: predictors and response to citalopram added to mood stabilizers. The Journal of Clinical Psychiatry, 65(5), 627–633. [PubMed] [Google Scholar]
- Mansell, W. , Paszek, G. , Seal, K. , Pedley, R. , Jones, S. , Thomas, N. , Mannion, H. , Saatsi, S. , & Dodd, A. (2011). Extreme appraisals of internal states in bipolar I disorder: A multiple control group study. Cognitive Therapy and Research, 35(1), 87–97. [Google Scholar]
- Masand, P. , Correll, C. U. , Yu, X. , Xiang, Y. , & Kane, J. M. (2017). Biological treatment of acute agitation or aggression with schizophrenia or bipolar disorder in the inpatient setting. Annals of Clinical Psychiatry: Official Journal of the American Academy of Clinical Psychiatrists, 29(2), 92–107. [PubMed] [Google Scholar]
- Penninx, B. W. J. H. , Beekman, A. T. F. , Smit, J. H. , Zitman, F. G. , Nolen, W. A. , Spinhoven, P. , Cuijpers, P. , De Jong, P. J. , Van Marwijk, H. W. J. , Assendelft, W. J. J. , Van Der Meer, K. , Verhaak, P. , Wensing, M. , De Graaf, R. , Hoogendijk, W. J. , Ormel, J. , Van Dyck, R. , & NESDA Research Consortium (2008). The Netherlands Study of Depression and Anxiety (NESDA): Rationale, objectives, and methods. International Journal of Methods in Psychiatric Research, 17(3), 121–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlis, R. H. , Brown, E. , Baker, R. W. , & Nierenberg, A. A. (2006). Clinical features of bipolar depression versus major depressive disorder in large multicenter trials. The American Journal of Psychiatry, 163(2), 225–231. [DOI] [PubMed] [Google Scholar]
- Perlis, R. H. , Delbello, M. P. , Miyahara, S. , Wisniewski, S. R. , Sachs, G. S. , Nierenberg, A. A. , & STEP‐BD investigators (2005). Revisiting depressive‐prone bipolar disorder: polarity of initial mood episode and disease course among bipolar I systematic treatment enhancement program for bipolar disorder participants. Biological Psychiatry, 58(7), 549–553. [DOI] [PubMed] [Google Scholar]
- Perlis, R. H. , Smoller, J. W. , Fava, M. , Rosenbaum, J. F. , Nierenberg, A. A. , & Sachs, G. S. (2004). The prevalence and clinical correlates of anger attacks during depressive episodes in bipolar disorder. Journal of Affective Disorders, 79(1‐3), 291–295. [DOI] [PubMed] [Google Scholar]
- Renaud, S. , Corbalan, F. , & Beaulieu, S. (2012). Differential diagnosis of bipolar affective disorder type II and borderline personality disorder: Analysis of the affective dimension. Comprehensive Psychiatry, 53(7), 952–961. [DOI] [PubMed] [Google Scholar]
- Rive, M. M. , Mocking, R. J. T. , Koeter, M. W. J. , van Wingen, G. , de Wit, S. J. , van den Heuvel, O. A. , Veltman, D. J. , Ruhé, H. G. , & Schene, A. H. (2015). State‐Dependent differences in emotion regulation between unmedicated bipolar disorder and major depressive disorder. JAMA Psychiatry, 72(7), 687–696. [DOI] [PubMed] [Google Scholar]
- Rush, A. J. , Gullion, C. M. , Basco, M. R. , Jarrett, R. B. , & Trivedi, M. H. (1996). The Inventory of depressive symptomatology (IDS): Psychometric properties. Psychological Medicine, 26(3), 477–486. [DOI] [PubMed] [Google Scholar]
- Spielberger, C. D. (1980). Preliminary manual for the state‐trait anger scale (STAS). University of South Florida Human Resources Institute. [Google Scholar]
- Spielberger, C. D. (1991). State‐trait anger expression inventory: Professional manual.
- Spielberger, C. D. , Krasner, S. S. , & Solomon, E. P. (1988). The experience, expression, and control of anger. In Janisse M. P. (Ed.), Individual Differences, Stress, and Health Psychology (pp. 89–108). Springer. [Google Scholar]
- Spielberger, C. D. , Reheiser, E. C. , & Sydeman, S. J. (1995). Measuring the experience, expression, and control of anger. Issues in Comprehensive Pediatric Nursing, 18(3), 207–232. [DOI] [PubMed] [Google Scholar]
- Stringer, B. , van Meijel, B. , Eikelenboom, M. , Koekkoek, B. , Licht, C. M. M. , Kerkhof, A. J. F. M. , Penninx, B. W. J. H. , & Beekman, A. T. F. (2013). Recurrent suicide attempts in patients with depressive and anxiety disorders: The role of borderline personality traits. Journal of Affective Disorders, 151(1), 23–30. [DOI] [PubMed] [Google Scholar]
- Tosun, A. , Maçkali, Z. , Çağin Tosun, Ö. , Kapucu Eryar, A. , & Mansell, W. (2015). Extreme appraisals of internal states and duration of remission in remitted bipolar patients. Noro Psikiyatri Arsivi, 52(4), 406–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Does, W. (2002). Different types of experimentally induced sad mood? Behavior Therapy, 33(4), 551–561. [Google Scholar]
- Van der Does, W. (2005). Thought suppression and cognitive vulnerability to depression. The British Journal of Clinical Psychology/the British Psychological Society, 44(Pt 1), 1–14. [DOI] [PubMed] [Google Scholar]
- Van der Ploeg, H. M. , Defares, P. B. , & Spielberger, C. D. (1982). Handleiding bij de Zelf‐analyse Vragenlijst. The Netherlands: Swets & Zeitlinger, Lisse. [Google Scholar]
- Van Dijk, S. , Jeffrey, J. , & Katz, M. R. (2013). A randomized, controlled, pilot study of dialectical behavior therapy skills in a psychoeducational group for individuals with bipolar disorder. Journal of Affective Disorders, 145(3), 386–393. [DOI] [PubMed] [Google Scholar]
- Vázquez, G. H. , Lolich, M. , Cabrera, C. , Jokic, R. , Kolar, D. , Tondo, L. , & Baldessarini, R. J. (2018). Mixed symptoms in major depressive and bipolar disorders: A systematic review. Journal of Affective Disorders, 225, 756–760. [DOI] [PubMed] [Google Scholar]
- Williams, R. (2017). Anger as a basic emotion and Its role in personality building and pathological growth: The neuroscientific, developmental and clinical perspectives. Frontiers in Psychology, 8, 1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen, H.‐U. , Robins, L. N. , Cottler, L. B. , Sartorius, N. , Burke, J. D. , Regier, D. , & Participants in the multicentre Who/Adamha Field Trials (1991). Cross‐cultural feasibility, reliability and sources of variance of the composite international diagnostic interview (CIDI). British Journal of Psychiatry, 159(5), 645–653. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


