Introduction
Osteoarthritis (OA) is the most common form of arthritis, affecting 350 million individuals worldwide (15% of the population)1. It is estimated that 32.5 million US adults have clinical OA of their knee, hip or hand2, with the most common sites being knee and hip. OA most likely represents a final common pathway of many different factors including genetics, environment, and biomechanical contributors3. OA is also associated with substantial individual and societal costs, and the occurrence of OA, as well as associated outcomes, can differ across populations. This article reviews racial/ethnic, socioeconomic and geographic disparities in the incidence, prevalence and outcomes of knee and hip OA.
Knee Osteoarthritis
Racial/ethnic disparities in knee OA
There has been little exploration of racial differences in knee OA incidence. Joint-based and person-based analyses of the Johnston County OA Project found no significant differences in the incidence of radiographic knee OA (with a Kellgren-Lawrence [K-L] score ≥ 2), symptomatic OA (having pain symptoms and radiographic knee OA in the same knee joint) and severe radiographic knee OA (K-L ≥ 3) between African Americans (AAs) and whites4,5.
Multiple US-based studies have found differences in the prevalence of knee OA between AAs and whites6–8. For example, in the Third National Health and Nutrition Examination Survey (NHANES-III), AAs were 50–65% more likely to have rKOA and sxKOA than whites6. In the Johnston County OA project, AAs had greater prevalence of severe radiographic knee OA (13.9% vs 6.6%) than whites, with no significant racial differences in overall radiographic and symptomatic OA8. Differences in KOA prevalence between AAs and whites seem to be more pronounced among women than men5,9,10. There have been few comparisons of knee OA prevalence in other racial and ethnic groups. Some research indicates that Chinese women have about 45% higher prevalence of radiographic and symptomatic knee OA than white women, with no difference between Chinese and white men11,12. In NHANES-III, there were no significant differences in knee OA prevalence between Mexican Americans and whites6
With regard to prevalence of specific radiographic features of knee OA, data from Johnston County OA project identified several racial differences.10 Compared with whites, AAs had more severe tibiofemoral radiographic knee OA, higher prevalence of tricompartmental radiographic knee OA, greater prevalence and severity of osteophytes and joint space narrowing, and higher likelihood of sclerosis. Analyses from the Osteoarthritis Initiative (OAI) showed that AAs were more likely than whites to have valgus thrust during walking, and this could contribute to the greater risk of lateral knee OA13.
Many studies have identified racial differences in OA-related outcomes, particularly pain and function14–26. Although some of these studies have included OA in other joints (particularly the hip), a focus has been on knee OA. A recent meta-analysis of racial/ethnic differences in OA pain and disability found higher pain severity in AAs than whites, with a standard mean difference of 0.57 (95% CI, 0.54 to 061) in studies using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) (Figure 1)27. AAs also had higher self-reported disability (0.38, 95% CI, 0.22 to 0.54) and poorer performance on functional tests (−0.5, −0.72 to −0.44). AAs with OA living below the poverty line may be at the greatest risk for poor pain and functional outcomes28.
Figure 1:
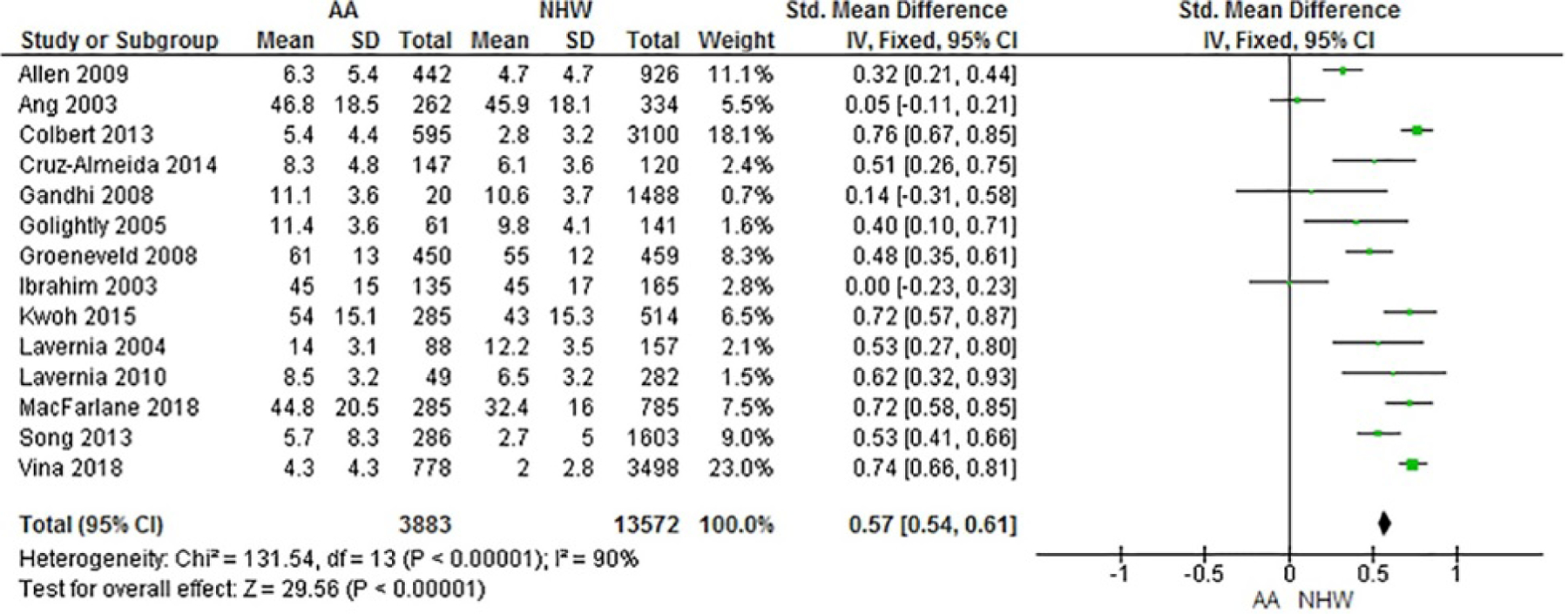
Forest plot of WOMAC pain measures. High scores = worse outcome/most severe pain
From Vaughn IA, Terry EL, Bartley EJ, Schaefer N, Fillingim RB. Racial-Ethnic Differences in Osteoarthritis Pain and Disability: A Meta-Analysis. J Pain. 2019;20(6):629–644.
Studies also have reported racial differences in pain sensitivity among individuals with knee OA29,30. For example, in a sample of patients with sxKOA, AAs exhibited greater sensitivity to both mechanical and heat-induced pain30. Other research has found greater experimental pain sensitivity among Asian Americans compared with Caucasian Americans with KOA31.
Many studies have explored potential factors underlying racial and ethnic differences in OA-related pain and function. Factors with evidence for explaining differences in pain and function between AAs and whites include: psychological resilience and perceived stress32, depressive symptoms16,33,34, low income and other socioeconomic factors33,35, pain coping patterns36, body mass index (BMI)16, and performance of physically demanding occupational tasks37. One study suggests that more depressive symptoms may contribute to greater pain sensitivity among Asian Americans compared to white Americans with knee OA31,38.
Socioeconomic disparities in knee OA
In the US, annual incidence rates of knee symptoms, radiographic knee OA, symptomatic knee OA, severe radiographic and symptomatic knee OA were estimated in longitudinal analyses of the Johnston County OA population5. Incidence rates for radiographic and severe radiographic knee OA were lower among individuals with higher levels of education but were only significantly different for severe radiographic knee OA (Table 1). In Spain, associations were examined in a retrospective ecological study of medical records for more than 5 million individuals in Catalonia between knee OA incidence with an area-based SES deprivation measure, the ecological MEDEA index (proportion of unemployed, temporary workers, manual workers, low educational attainment and low educational attainment among youngsters)39. Higher incidence rates of knee OA were found in areas that were deemed as most deprived (Table 1)40.
Table 1.
Summary of socioeconomic differences in the incidence, prevalence and outcomes of knee OA.
| SES Measure | Study Author and Year | Data Source | Country | Health Outcome | Selected Results Point estimate (95% CI) |
|---|---|---|---|---|---|
| Education | Murphy et al 20165 | Joco OA | US | IR per 100 person-years for knee symptoms, rKOA, severe rKOA, sxKOA, severe sxOA |
Severe rKOA: <high school vs ≥ high school IR=2.8 (2.3–3.4) |
| Hannan et al 199241 | NHANES-I | US | Prevalence rKOA, knee pain |
rKOA: ≤ 8 years vs ≥ 13 years aOR = 1.53 (1.09–2.23) knee pain: ≤ 8 years vs ≥ 13 years aOR = 1.34 (1.09–1.65) |
|
| Callahan et al 201044 | JoCo OA | US | Prevalence of rKOA, bilateral rKOA,sxKOA, bilateral sxKOA |
sxKOA: <12 years vs. ≥ 12 years aOR = 1.86 (1.20 – 2.87) |
|
| Callahan et al 201145 | JoCo OA | US | Prevalence of rKOA, bilateral rKOA, sxKOA, bilateral sxKOA |
rKOA: <12 years vs. ≥ 12 years aOR = 1.44 (1.20–1.73) sxKOA: <12 years vs. ≥ 12 years aOR = 1.66 (1.34–2.06) |
|
| Grotle et al 200842 | MSK pain survey | Norway | Prevalence self-reported KOA |
self-reported KOA: ≤ 9 years vs. > 12 years aOR =2.25 (1.43–3.57) 9–12 years vs. >12 years aOR = 2.32 (1.54–3.50) |
|
| Jorgensen et al 201143 | Danish National register | Denmark | Prevalence knee OA by ICD-8 code | Highest education vs. vocational/basic school Knee OA among women: RR = 0.62 (0.60–0.65) Knee OA among men: RR = 0.50 (0.48– 0.53) |
|
| Cleveland et al 201346 | JoCo OA | US | WOMAC function, pain, stiffness total in rKOA and sxKOA |
rKOA and WOMAC function: <12 years vs. ≥ 12 years aβ = 2.83 (0.38,5.28) |
|
| Feldman et al 201591 | AViKA TKR cohort | US | WOMAC pain and function, pain catastrophizing |
% with high pain (WOMAC >55) among people with knee rOA, adjusted: Less than college: 32.6% (21.3%, 43.9%) Some college: 29.9% (19.9%, 40.0%) College graduate: 21.1% (15.3%, 26.9%) |
|
| Kiadaliri et al 201748 | Malmӧ OA Study | Sweden | Knee pain, rKOA, KOOS pain, other symptoms, ADL, QOL, Swedish EQ-5D-3L | Education <9 years vs. 10–12 years vs. college Frequent knee pain: aRII = 0.71 (0.61–0.84) rKOA: aRII=0.53 (0.29–0.98) KOOS pain: aRII=0.61 (0.42–0.90) KOOS ADL: aRII=0.52 (0.36–0.77) |
|
| Hawker et al 200247 | Mail survey Ontario | Canada | Need for knee or hip arthroplasty | Likelihood for potential need for arthroplasty: <high school vs. ≥ high school aOR = 1.57 (1.17–2.11) | |
| Occupation | Callahan et al 201145 | JoCo OA | US | Prevalence of rKOA, bilateral rKOA, sxKOA, bilateral sxKOA | For all prevalence knee OA outcomes and non-managerial vs. managerial occupations: no significant independent association beyond educational attainment and community poverty |
| Cleveland et al 201346 | JoCo OA | US | WOMAC function, pain, stiffness total in rKOA and sxKOA | rKOA and WOMAC pain: managerial vs. non-managerial occupation aβ = 0.78 (0.08,1.48) | |
| Kiadaliri et al 201748 | Malmӧ OA Study | Sweden | Knee pain, rKOA, KOOS pain,other symptoms, ADL, QOL, Swedish EQ-5D-3L | Occupation: unskilled manual, skilled manual, low-level non-manual, intermediate non-manual, high-level non-manual Frequent knee pain: aRII = 0.70 (0.60–0.82) rKOA: aRII = 0.55 (0.31–0.98) KOOS pain: aRII=0.57 (0.39–0.83) KOOS ADL: aRII=0.49 (0.34–0.72) |
|
| Income | Murphy et al 20165 | Joco OA | US | IR per 100 person-years for knee symptoms, rKOA, severe rKOA, sxKOA, severe sxOA | Knee symptoms: <$15,000 vs ≥$35,000 IR = 7.4 (6.3–8.7) |
| Jorgensen et al 201143 | Danish National register | Denmark | Prevalence Knee OA by ICD-8 code | ≥150% vs. 75–124% average household income Knee OA among women: RR = 0.80 (0.77–0.83) Knee OA among men: RR = 0.77 (0.74–0.80) |
|
| Reichmann et al 201151 | NHANES-III OAI | US | Health Status – % poor/fair |
Among people with rKOA: NHANES-III: <$20,000 = 46.5% (36.8%, 56.10%) $50,000+ = 8.3% (1.9%, 14.8%) OAI: <$20,000 = 11.3% (7.5%, 15.10%) $50,000+ = 1.0% (0.0%, 2.3%) |
|
| Hawker et al 200247 | Mail survey Ontario | Canada | Need for knee or hip arthroplasty |
Likelihood of potential need for arthroplasty: ≤$20,000 vs > $40,000 aOR 1.83 (1.24–2.70) |
|
| Community Poverty | Callahan et al 201145 | JoCo OA | US | Prevalence of rKOA, bilateral rKOA, sxKOA, bilateral sxKOA |
rKOA: high poverty vs. low poverty aOR = 1.83 (1.43–2.36) sxKOA: high poverty vs low poverty aOR = 1.36 (1.00–1.83) |
| Cleveland et al 201346 | JoCo OA | US | WOMAC function, pain, stiffness total in rKOA and sxKOA |
sxKOA and WOMAC pain: high poverty vs. low poverty aβ = 1.35 (0,06, 2.64) |
|
| Area-level SES | Feldman et al 201591 | AViKA TKR cohort | US | WOMAC pain and function, pain catastrophizing) |
% with high pain (WOMAC >55) among people with knee rOA, adjusted Low area SES: 34.2% (25.3%, 43.1%) Mid area SES: 26.6% (17.0%, 34.2%) High area SES: 18.6% (11.8%, 25.5%) |
| Social Class | Peters et al 200550 | SASH | UK | New Zealand Score for knee pain and disability |
Knee pain and disability: lowest social class vs highest, adjusted mean difference = 8.3 (−1.8–18.3) |
| Deprivation | Reyes et al 201540 | SIDIAP | Spain | Incidence of knee OA by ICD-10 code |
Knee OA: Most vs. least deprived area aIRR = 1.23 (1.19–1.28) |
Abbreviations: aβ = adjusted parameter estimate, ADL = activities of daily living, aOR = adjusted odds ratio, aRII= adjusted relative index of inequality, AViKA = Adding Value in Knee Arthroplasty, CI= confidence interval, ICD = International Classification of Diseases, IR= annual incidence rate, IRR = incidence rate ratio, JoCo OA = Johnston County Osteoarthritis Project, KOOS = Knee Injury and Osteoarthritis Outcome Score, MSK = musculoskeletal, NHANES = National Health and Nutrition Examination Survey, QOL = quality of life, rKOA = radiographic knee osteoarthritis, RR = rate ratio, SASH = Somerset and Avon Survey of Health, SES = socioeconomic status, SIDIAP = System for the Development of Research in Primary Care, sxKOA = symptomatic knee osteoarthritis, UK = United Kingdom, US = United States, WOMAC= Western Ontario and McMaster Universities Osteoarthritis Index
Studies examining associations between SES measures and knee OA prevalence are more common. Using data from the NHANES-I in the early 1990s, education of ≤8 years compared with ≥13 years was significantly associated with radiographic knee OA and knee pain (Table 1)41. Findings from a population survey in Norway showed that compared to individuals with ≥12 years of education, individuals with ≤ 9 or 9–12 years were 25–30% more likely to have age-and sex-adjusted radiographic knee OA, or self-reported or doctor-diagnosed knee OA (Table 1)42. In a Danish study, the risk for knee OA was lower in women in a household with a higher education level and a higher risk of knee OA was associated with less income (Table 1)43.
Associations between low education levels with radiographic knee OA have also been observed in the Johnston County OA project44,45. One study examined associations of education dichotomized as < 12 versus ≥ 12 years with unilateral and bilateral radiographic and symptomatic knee OA44, adjusting for demographic and clinical covariates. Analyses were stratified by gender and also conducted in a subset of postmenopausal women. In men, only the association with symptomatic knee OA remained significant after covariate adjustment. In adjusted analyses in the total group of women, those with < 12 years of education were 50–85% more likely to have unilateral and bilateral radiographic and symptomatic knee OA. In the subset of postmenopausal women, these observations were partly explained by hormone replacement therapy. Analyses between education and radiographic and symptomatic OA in Johnston County OA cohort were expanded to explore independent relationships between education, and two other SES variables, occupation (defined as non-managerial or not), and household community poverty level (Table 1)45. When all three SES measures were analyzed simultaneously in adjusted models, < 12 years of education was significantly associated with unilateral and bilateral radiographic knee OA and symptomatic knee OA.
A number of studies have identified SES differences in health-related outcomes, particularly pain, disability and the need for arthroplasty, among people with knee OA in addition to the differences in the incidence or prevalence (Table 1)46–51. In a study of participants with radiographic knee OA in NHANES-III, lower income levels were associated with fair or poor self-reported health status in multivariable adjusted models51. In the Somerset and Avon Survey of Health, individuals who reported more pain and worse function at follow-up, lower social class, comorbidities and higher BMI were associated with greater deterioration50. In cross-sectional analyses of the Johnston County OA project, in individuals with knee OA, low education and higher community poverty rates were both significantly associated with worse pain and function46. Another study found socioeconomic gradients related to both frequent knee pain and knee OA as well as health related quality of life in favor of individuals with higher levels of SES48.
Geographic disparities in knee OA
According to the Global Burden of Disease 2010 study, the age-standardized prevalence of sxKOA is estimated at 3.8% globally52. Regional variations exist, where the prevalence of sxKOA is highest in the Asia Pacific high-income region, Oceania and North Africa/Middle East (Figure 2). Prevalence in the US and Europe falls in the middle range, and the lowest frequencies are reported in southern Asia.
Figures 2:
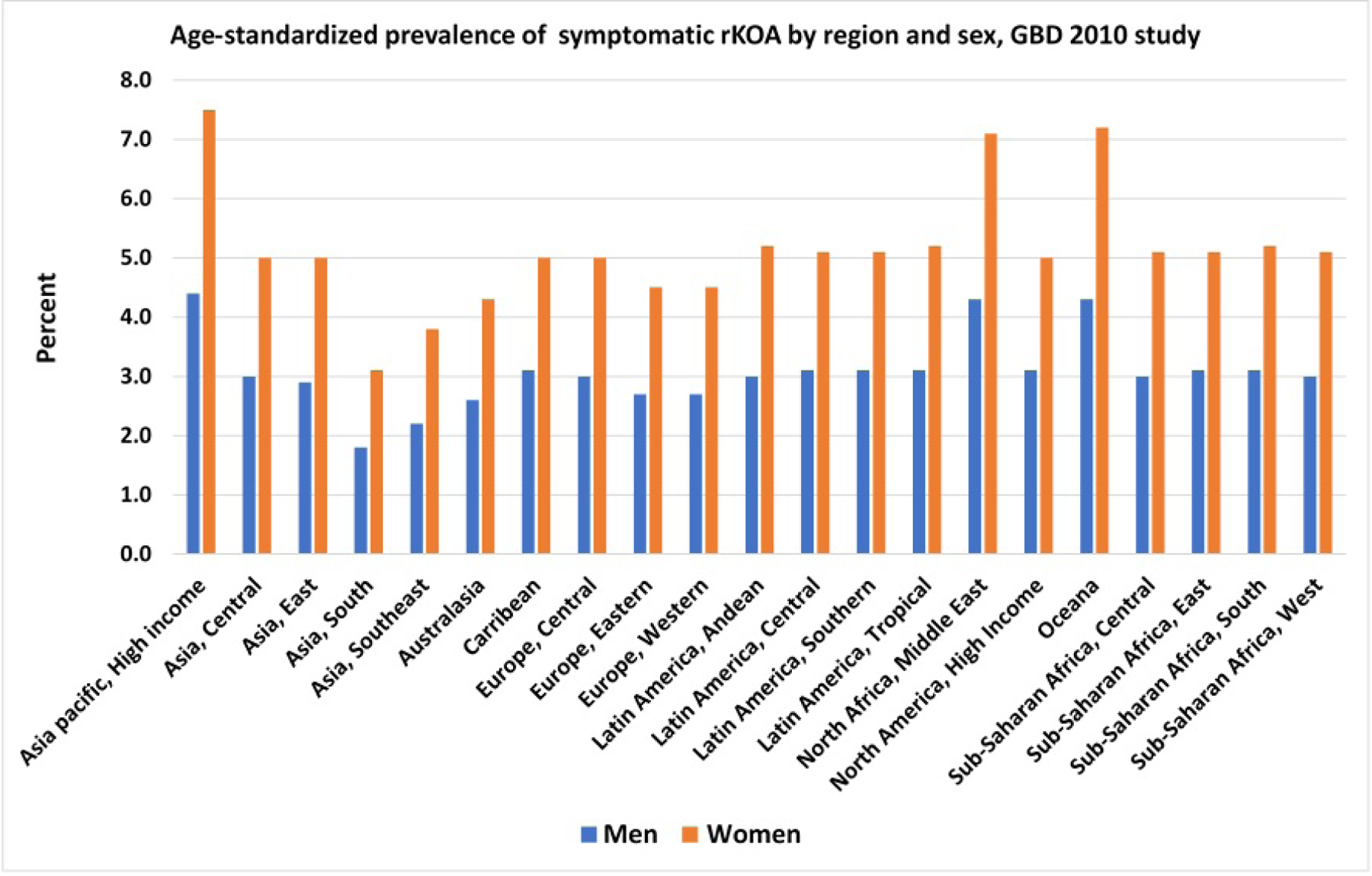
Age-standardized prevalence of symptomatic radiographically confirmed knee osteoarthritis, The Global Burden of Disease Study 2010
From Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–1330.
There is evidence that the prevalence of knee OA is higher in some Asian regions. Results from a systematic review53 point to overall prevalences of radiographic knee OA ranging from 6.5% in the Netherlands54 to 70.8% in Japan55. Prevalences of symptomatic knee OA across the globe were slightly lower, where the lowest was found in Italy (5.4%)56 and Greece (6.3%) and the highest in Korea (24.2%)57. More recently, the Fifth Korean National Health and Nutrition Examination Survey (2010–2012) found that, among people >50 years of age, the prevalences for radiographic knee OA were 44.6% for women and 20.9% for men, whereas symptomatic knee OA was 19.2% for women and 4.4% for men58. Similarly, a study in rural Wuchuan, China among people >59 years of age also reported a high prevalence of radiographic knee OA (women: 36%, men: 20%) and symptomatic knee OA (women: 27%, men: 13%)59. It has been suggested that the increased prevalence of knee OA in Asian regions may be due to high amounts of physical labor such as farming and fishing59.
The prevalence of arthritis, including OA, is known to differ between rural and urban populations. In the US, 1 in 3 adults who live in predominantly rural areas have arthritis compared to 1 in 5 in metropolitan areas60. In the Framingham OA Study which is based in a regional urban center, the prevalence of sxKOA was reported to be 7%61, while being 17% in the predominantly rural Johnston County OA project62. Compared to urban regions, rural communities generally have poorer SES (e.g., less education, lower incomes) as well as more physical inactivity and obesity, all factors linked to OA63,64. The Johnston County OA project also reported that living in areas with high community poverty (≥20%) was associated with an increase in radiographic knee OA (84%) (Table 1)45. Further, among individuals with radiographic knee OA, greater pain outcomes were associated with living in high poverty areas (≥25%)46. Living in poorer neighborhoods has also been shown to be associated with worse pain and function outcomes after total knee arthroplasty, an association that was stronger among those with lower education65.
Hip Osteoarthritis
Racial/ethnic disparities in hip OA
In Johnston County OA, AAs had lower incidence rates of radiographic and symptomatic hip OA compared with whites66. For symptomatic hip OA, incidence rates were 15/1000 person-years and 7/1000 person-years, respectively. These results confirmed previous joint-based analyses of the Johnston County OA cohort, also showing that the hazard of radiographic hip OA was lower among AAs than whites (adjusted hazard ratio: 0.44, 95% confidence interval 0.27–0.71)4.
Although some indirect comparisons indicated that black individuals living Africa and in the Caribbean have lower rates of radiographic hip OA than whites67–70, comparisons of radiographic hip OA prevalence in AAs and whites in US cohorts have not identified substantial differences71–73. However, data from the Johnston County OA cohort identified racial differences in prevalence of specific radiographic features of hip OA, which varied by gender70. Comparison of the Beijing Osteoarthritis Study with two US-based cohorts showed that hip OA was 80–90% less prevalent among Chinese individuals than whites74. Another study identified differences in hip morphology that may explain lower rates of hip OA among Chinese individuals compared with other groups75.
As described above, many studies have examined racial differences in pain and function among patients with OA in AAs and whites but not other racial or ethnic groups. A number of studies including patients with knee and/or hip OA have found worse self-reported pain and function among AAs compared to whites27. However, there has been little research on racial / ethnic differences in pain and function with a focus specifically on hip OA. Data from Johnston County OA found racial differences in patterns of hip OA progression; generally, AAs had greater progression in pain and disability, while whites had more radiographic hip OA progression76. However, in cross-sectional analyses of the Johnston County OA cohort, there were no racial differences in self-reported pain or function among participants with HOA16. In studies including patients with knee and / or hip OA, there is some evidence for BMI, overall health, and coping and other psychological factors as potential explanatory mechanisms16,36.
Socioeconomic disparities in hip OA
The annual incidence rates of hip symptoms, radiographic hip OA, severe radiographic hip OA, and symptomatic hip OA were estimated in the Johnston County OA project66. Incidence rates decreased moderately for hip symptoms and radiographic hip OA with greater levels of education (Table 2)66. When education was examined in analyses stratified by race, the trend of radiographic hip OA was also significant, but attenuated in AAs66. In terms of analyses according to household income, the annual incidence rate of 45/1000 person-years of hip symptoms for individuals with < $15,000/year (lowest level) was among the highest incidence rates observed across all of the subpopulations analyzed in the study66. Furthermore, the study from Catalonia Spain discussed in the knee OA incidence section also showed higher rates of hip OA in areas that were deemed to be the most deprived40.
Table 2.
Summary of socioeconomic differences in the incidence, prevalence and outcomes of hip OA.
| SES Measure | Study | Data Source | Country | Health Outcome | Selected Results Point estimate (95% CI) |
|---|---|---|---|---|---|
| Education | Moss et al 201666 | JoCoOA | US | IR per 1000 person-years for hip symptoms, rHOA, severe rHOA, sxHOA |
rHOA: <high school: IR = 22 (16, 30) High school: IR = 22 (18, 26) >high school: IR = 17 (13, 22) |
| Tepper et al 199371 | NHANES-I | US | Prevalence of rHOA |
rHOA: education ≤12 years vs. >12 years aOR 1.64 (0.95, 2.85) |
|
| Cleveland et al 201377 | JoCo OA | US | Prevalence of rHOA, bilateral rHOA, sxHOA, bilateral sxHOA |
Bilateral sxHOA: education ≤12 years vs. >12 years aOR=1.91 (1.08,3.39) |
|
| Grotle et al 200842 | MSK pain survey | Norway | Prevalence of self-reported hip OA |
self-reported hip OA: ≤ 9 years vs. >12 years aOR =2.85 (1.65,4.93) 9–12 years vs. >12 years aOR = 2.70 (1.62,4.49) |
|
| Jorgensen et al 201143 | Danish National Register | Denmark | Prevalence of hip OA by ICD-8 code | Highest education vs. vocational/basic school Hip OA for women: RR = 0.85 (0.80–0.90) Hip OA for men: RR = 0.65 (0.61– 0.68) |
|
| Knight et al 201178 | JoCo OA | US | WOMAC function, pain, total, HAQ-DI in rHOA and sxHOA | Edgucation ≤12 years vs. >12 years rHOA and WOMAC function: aβ=3.22(0.73,5.7) rHOA and HAQ-DI: aβ=0.15 (0.05,0.35) |
|
| Schafer et al 201080 | Dresden Hip Registry | Germany | WOMAC Response to THR |
Risk of nonresponse to THR: education 12 years vs. 8 years aOR = 0.49 (0.27, 0.89) |
|
| Greene et al 201479 | Swedish hip arthroplasty registry | Sweden | EuroQol response to THR |
Lower pain after THR: education >12 years vs. ≤ 8 years aβ =−3.3 ± 0.05 |
|
| Occupation | Cleveland et al 201377 | JoCo OA | US | Prevalence of rHOA, bilateral rHOA, sxHOA, bilateral sxHOA | For all hip OA outcomes and non-managerial vs. managerial occupations, no significant associations |
| Knight et al 201178 | JoCo OA | US | WOMAC function, pain, total, HAQ-DI in rHOA and sxHOA |
rHOA and WOMAC pain: non-managerial vs. managerial aβ =0.78 (0.09, 1.47) |
|
| Income | Moss et al 201666 | JoCo OA | US | IR per 1000 person-yrs for hip symptoms, rHOA, severe rHOA, sxHOA |
Hip symptoms: <$15,000: IR=45 (17, 24) $15–35,000: IR=34 (27,42) ≥$35,000: IR=28 (21,37) |
| Tepper et al 199371 | NHANES-I | US | Prevalence of rHOA |
rHOA: highest vs. lowest quartile of family income aOR 0.99 (0.40, 2.44) |
|
| Jorgensen et al 201143 | Danish National Register | Denmark | Prevalence of hip OA by ICD-8 code | ≥150% vs. 75–124% average household income Knee OA among women: RR = 0.97 (0.93–1.02) Knee OA among men: RR = 0.86 (0.82–0.90) |
|
| Community Poverty | Cleveland et al 201377 | JoCo OA | US | Prevalence of rHOA, bilateral rHOA, sxHOA, bilateral sxHOA |
Bilateral rHOA: high vs. low poverty aOR=1.87 (1.32,2.66) |
| Knight et al 201178 | JoCo OA | US | WOMAC function, pain, total, HAQ-DI in rHOA and sxHOA |
rHOA and HAQ-DI: high poverty vs. low poverty β=0.15 (0.01, 0.29), but not significant in models that accounted for educational attainment and income |
|
| Deprivation | Reyes et al 201540 | SIDIAP | Spain | Incidence of hip OA by ICD-10 code | Hip OA: Most vs. least deprived area age and sex-aIRR = 1.23 (1.17, 1.29) fully aIRR = 1.02 (0.97, 1.07) |
| Clement et al 201181 | Prospective cohort of THR patients | UK | Oxford hip score, dislocation, mortality | Most vs. least deprived area Hip Dislocation: aOR=5.3 (p=0.001) Mortality: OR=3.2 (p=0.02) |
Abbreviations: aβ = adjusted parameter estimate, aIRR = adjusted incidence rate ratio, aOR = adjusted odds ratio, CI= confidence interval, EuroQOL = European Quality of Life, HAQ-DI = Health Assessment Questionnaire Disability Index, ICD = International Classification of Diseases, IR= annual incidence rate, IRR = incidence rate ratio, JoCo OA = Johnston County Osteoarthritis Project, MSK = musculoskeletal, NHANES = National Health and Nutrition Examination Survey, rHOA = radiographic hip osteoarthritis, RR = rate ratio, SES = socioeconomic status, SIDIAP = System for the Development of Research in Primary Care, sxHOA = symptomatic hip osteoarthritis, THR = total hip replacement, UK = United Kingdom, US = United States, WOMAC= Western Ontario and McMaster Universities Osteoarthritis Index
As with knee OA, analyses were conducted in the early 1990s using data from NHANES-I to examine associations between education and radiographic hip OA prevalence (Table 2)71. Education > 12 years was significantly associated with radiographic OA compared to ≤ 12 years (OR = 1.69, 95% CI 1.01 – 2.81). However, in adjusted models the relationship was no longer statistically significant. Both the Danish and Norwegian studies, discussed in the knee OA section, examined associations between education and hip OA (Table 2)42,43. Increased prevalence of hip OA was significantly associated with lower levels of education in both studies. In analyses of the Danish registry, associations between lower income levels and increased hip OA were also noted43. Associations between education, occupation, and community poverty rate with radiographic and symptomatic hip OA were examined in the Johnston County OA project 77. After adjusting for all SES variables and covariates simultaneously, individuals with <12 years of education were 44% more likely to have symptomatic hip OA than those with ≥ 12 years and 90% more likely to have bilateral symptomatic hip OA (Table 2)77.
A number of studies have identified differences in pain, disability, and other health-related outcomes in hip OA (Table 2)49,78. In individuals with radiographic hip OA in the Johnston County OA project, low levels of education and living in low household poverty rate areas were both independently significantly associated with worse pain and function78. Several studies have examined associations between SES with outcomes of total hip replacement (THR)79,80. In analyses of the Dresden Hip Registry and the Swedish Hip Arthroplasty Register, poorer SES parameters were independent predictors of poorer pain, function, and quality of life outcomes after THR79,80. In analyses from the UK, patients who had the highest level of deprivation underwent THR at an earlier age, were less satisfied with their outcome, and also had an increased risk of dislocation and mortality81.
Geographic disparities in hip OA
The reported prevalence of symptomatic hip OA tends to be greater in high-income countries compared with low-income countries. Results from the Global Burden of Disease 2010 study indicate that the global age-standardized prevalence of symptomatic hip OA in adults in 2010 was 0.85% (Figure 3)52. In general, the prevalence of hip OA was higher in North America high-income regions where the age-standardized prevalence was nearly 2%, followed by southern Latin America and Asia Pacific high-income regions. Prevalence was lowest in East Asia and North Africa/Middle East, while European countries tended to fall in the middle range along with Australia, Latin America and Sub-Saharan Africa.
Figure 3:
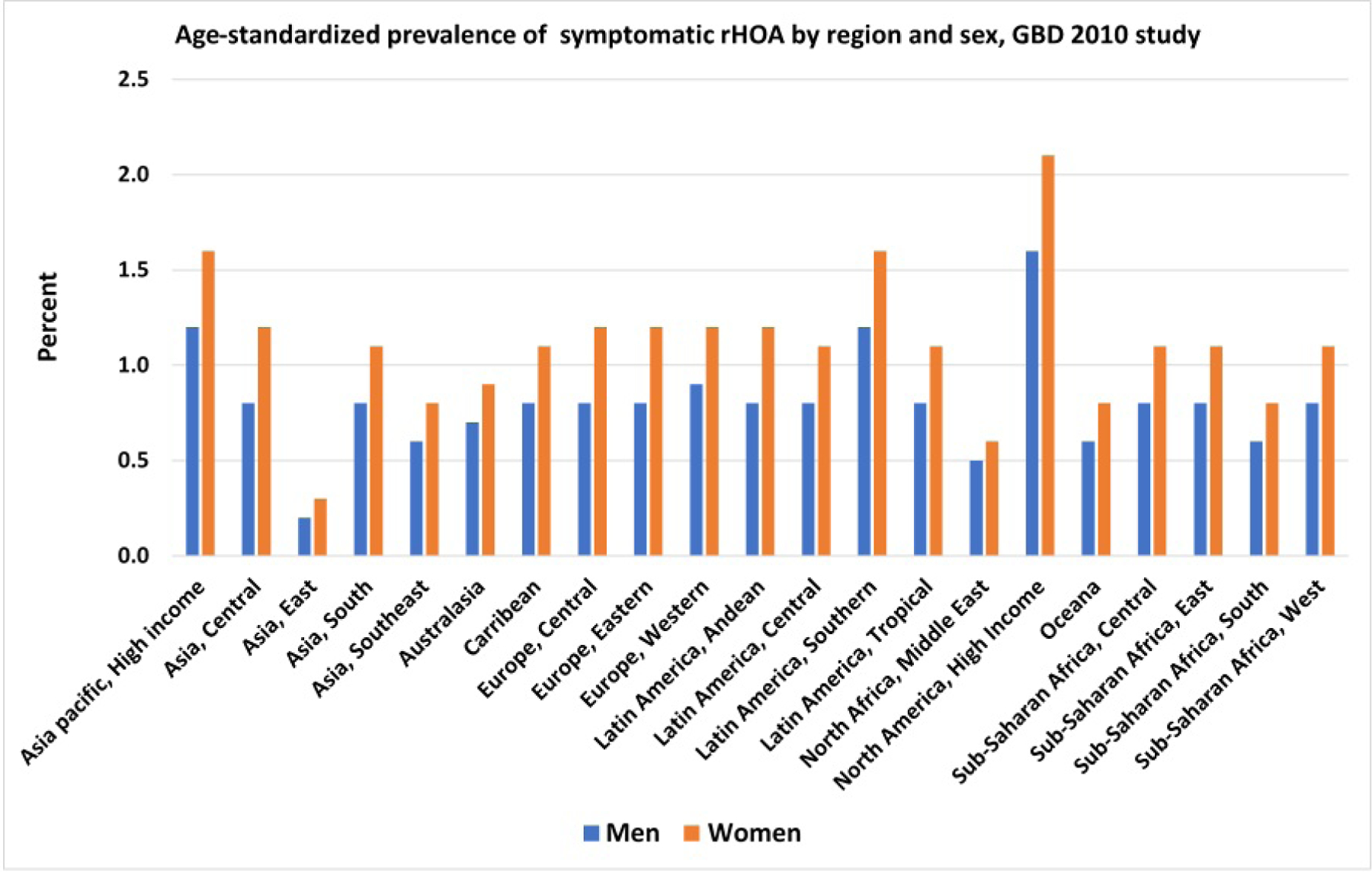
Age-standardized prevalence of symptomatic radiographically confirmed hip osteoarthritis, The Global Burden of Disease Study 2010
From Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–1330.
In the Framingham OA study of adults ≥50 years of age, the age-standardized prevalence for symptomatic hip OA was reportedly higher at 4.2%, and for radiographic hip OA it was 19.6%82, while in Korea, the prevalence of symptomatic hip OA among adults ≥50 years of age was low (0.1%–0.2%)83. A systematic review53 presented prevalence rates of radiographic hip OA that ranged from 1.0% in Japan84 and China74 to 45% in Tasmania85, and prevalence rates of symptomatic hip OA ranging from 0.9% in Greece86 to 7.4% in Spain87. While the prevalence of radiographic knee OA was reported to be fairly high in China, radiographic hip OA is very low, being less than 1%74,88. However, the prevalence in other Asian countries may differ. In a Japanese study among individuals aged 23–95 years, the crude prevalence of radiographic hip OA was reported to be 18.2% in men and 14.3% in women89. This study also reported the prevalence of sxHOA to be 0.29% in men and 0.99% in women89.
Community-level factors also play a role in hip OA. Results from the Johnston County OA project indicate that living in areas with high levels of household poverty is associated with a 50% higher risk of having radiographic hip OA overall and 87% higher risk of having bilateral radiographic hip OA77. Additionally, among individuals with radiographic hip OA, greater disability is associated with living in high household poverty areas78. Further, a large institutional registry of THR due to radiographic hip OA showed that WOMAC function and pain were higher in communities with census tract Medicaid coverage >10%, an indicator of community economic deprivation90. Further, this effect of worse WOMAC function seen in those living in areas with high Medicaid coverage was more pronounced in AAs than whites90.
Conclusions
OA is a highly prevalent painful and disabling condition which affects the population globally. Knee and hip OA and their associated outcomes vary by race/ethnicity, SES, and geographic regions. Based on current evidence, the burden of OA may be generally higher among particular subgroups, such as AAs and those with lower SES. However, there are notable gaps in our understanding of these disparities. Most research to date on knee and hip OA has been conducted among AAs and whites. Potential mechanisms underlying disparities in OA outcomes have been determined in specific populations, but knowledge is limited about which factors may be distinct in certain subgroups or common to all. Future research should focus on examining OA occurrence in other racial/ethnic groups (e.g., Hispanic/Latino, Asian American, and American Indian/Native American populations) and on identifying modifiable factors that explain OA differences by race/ethnicity, SES, and geography in order to inform public health approaches to mitigate the burden of OA.
Key points:
African Americans with knee osteoarthritis (OA) have greater prevalence, severity, progression and worse pain and function compared to whites.
There is a lower prevalence of hip OA among Chinese than US whites and a possible lower risk of hip OA among African Americans compared to whites.
Individuals with lower levels of socioeconomic status have greater incidence, greater prevalence and worse clinical outcomes of both knee and hip OA.
Synopsis:
It is estimated that 32.5 million US adults have clinical osteoarthritis (OA), with the most common sites being knee and hip. OA is associated with substantial individual and societal costs. Race/ethnicity, socioeconomic status (SES) and geographic variations in the prevalence of knee and hip OA are well established around the world. In addition, clinical outcomes associated with hip and knee OA differ according to race/ethnicity, SES, and geography. This variation is likely multifactorial and may also reflect country-specific differences in healthcare systems. The interplay between different factors, such as geography, SES and race/ethnicity is difficult to study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure statement: The authors have nothing to disclose.
Contributor Information
Leigh F. Callahan, School of Medicine, Thurston Arthritis Research Center, University of North Carolina at Chapel Hill, Chapel Hill, NC USA.
Rebecca J. Cleveland, School of Medicine, Thurston Arthritis Research Center, University of North Carolina at Chapel Hill, Chapel Hill, NC USA.
Kelli D. Allen, School of Medicine, Thurston Arthritis Research Center, University of North Carolina at Chapel Hill, Chapel Hill, NC USA; Center of Innovation to Accelerate Discovery and Practice Transformation, VA Healthcare System, Durham, NC, USA.
Yvonne M. Golightly, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC USA.
REFERENCES
- 1.Hochberg MC, Cisternas MG, Watkins-Castillo SI. Arthritis. United States Bone and Joint Initiative: The Burden of Musculoskeletal Diseases in the United States (BMUS), Fourth Edition, forthcoming. https://www.boneandjointburden.org/fourth-edition/iiib10/osteoarthritis. Accessed March 13, 2020, 2020.
- 2.Osteoarthritis (OA). 2020; https://www.cdc.gov/arthritis/basics/osteoarthritis.htm. Accessed March 13, 2020, 2020.
- 3.Loeser RF, Goldring SR, Scanzello CR, Goldring MB. Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum. 2012;64(6):1697–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kopec JA, Sayre EC, Schwartz TA, et al. Occurrence of radiographic osteoarthritis of the knee and hip among African Americans and whites: a population-based prospective cohort study. Arthritis Care Res (Hoboken). 2013;65(6):928–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy LB, Moss S, Do BT, et al. Annual Incidence of Knee Symptoms and Four Knee Osteoarthritis Outcomes in the Johnston County Osteoarthritis Project. Arthritis Care Res (Hoboken). 2016;68(1):55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991–1994. The Journal of Rheumatology. 2006. 33:2271–2279. [PubMed] [Google Scholar]
- 7.Sowers M, Lachance L, Hochberg M, Jamadar D. Radiographically defined osteoarthritis of the hand and knee in young and middle-aged African American and Caucasian women. Osteoarthritis and Cartilage. 2000;8:69–77. [DOI] [PubMed] [Google Scholar]
- 8.Jordan JM, Helmick CG, Renner JB, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. The Journal of Rheumatology. 2007;31(4):172–180. [PubMed] [Google Scholar]
- 9.Anderson JJ, Felson DT. Factors associated with osteoarthritis of the knee in the first National Health and Nutrition Examination Survey (HANES I). American Journal of Epidemiology. 1988;128(1):179–189. [DOI] [PubMed] [Google Scholar]
- 10.Braga L, Renner JB, Schwartz TA, et al. Differences in radiographic features of knee osteoarthritis in African Americans and Caucasians: The Johnston County Osteoarthritis Project. Osteoarthritis & Cartilage. 2009;17:1554–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Felson DT, Nevitt MC, Zhang Y, et al. High prevalence of lateral knee osteoarthritis in Beijing Chinese compared with Framingham Caucasian subjects. Arthritis and Rheumatism. 2002;46(5):1217–1222. [DOI] [PubMed] [Google Scholar]
- 12.Zhang Y, Xu L, Nevitt MC, et al. Comparison of the prevalence of knee osteoarthritis between the elderly Chinese population in Beijing and whites in the United States: The Beijing Osteoarthritis Study. Arthritis Rheum. 2001;44(9):2065–2071. [DOI] [PubMed] [Google Scholar]
- 13.Chang A, Hochberg M, Song J, et al. Frequency of varus and valgus thrust and factors associated with thrust presence in persons with or at higher risk for knee osteoarthritis. Arthritis & Rheumatism. 2010;March 8 Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 14.Centers for Disease Control and Prevention. Racial/ethnic differences in the prevalence and impact of doctor-diagnosed arthritis - United States, 2002. Morbidity and Mortality Weekly Report. 2005;54:119–123. [PubMed] [Google Scholar]
- 15.Sims EL, Keefe FJ, Kraus VB, Guilak F, Queen RM, Schmitt D. Racial differences in gait mechanics associated with knee ostoarthritis. Aging Clinical and Experimental Research. 2009;21(6):463–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allen KD, Helmick CG, Schwartz TA, DeVellis B, Renner JB, Jordan JM. Racial differences in self-reported pain and function among individuals with radiographic hip and knee osteoarthritis: The Johnston County Osteoarthritis Project. Osteoarthritis & Cartilage. 2009;17(9):1132–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Golightly YM, Dominick KL. Racial variations in self-reported osteoarthritis symptom severity among veterans. Aging: Clinical and Experimental Research. 2005;17:264–269. [DOI] [PubMed] [Google Scholar]
- 18.Allen KD. Racial and ethnic disparities in osteoarthritis phenotypes. Curr Opin Rheumatol. 2010;22(5):528–532. [DOI] [PubMed] [Google Scholar]
- 19.Burns R, Graney MJ, Lummus AC, Nichols LO, Martindale-Adams J. Differences in self-reported osteoarthritis disability and race. Journal of the National Medical Association. 2007;99(9):1046–1051. [PMC free article] [PubMed] [Google Scholar]
- 20.Foy CG, Pennix BW, Shumaker SA, Messier SP, Pahor M. Long-term exercise therapy resolves ethnic differences in baseline health status in older adults with knee osteoarthritis. Journal of the American Geriatrics Society. 2005;53(9):1469–1457. [DOI] [PubMed] [Google Scholar]
- 21.Groeneveld PW, Kwoh CK, Mor MK, et al. Racial differences in expectations of joint replacement surgery outcomes. Arthritis & Rheumatism. 2008;59(5):730–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Song J, Chang HJ, Tirodkar M, Chang RW, Manheim LM, Dunlop DD. Racial / ethnic differences in activities of daily living disability in older adults with arthritis: a longitudinal study. Arthritis Care and Research. 2007;57(6):1058–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shih VC, Song J, Chang RW, Dunlop DD. Racial differences in activities of daily living limitation onset in older adults with arthritis: a national cohort study. Archives of Physical Medicine & Rehabilitation. 2005;86:1521–1526. [DOI] [PubMed] [Google Scholar]
- 24.Theis KA, Murphy L, Hootman JM, Helmick CG, Yelin E. Prevalence and correlates of arthritis-attributable work limitation in the US population among persons ages 18–64: 2002 National Health Interview Survey data. Arthritis Care and Research. 2007;57(3):355–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Collins JE, Katz JN, Dervan EE, Losina E. Trajectories and risk profiles of pain in persons with radiographic, symptomatic knee osteoarthritis: data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2014;22(5):622–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Booker S, Cardoso J, Cruz-Almeida Y, et al. Movement-evoked pain, physical function, and perceived stress: An observational study of ethnic/racial differences in aging non-Hispanic Blacks and non-Hispanic Whites with knee osteoarthritis. Exp Gerontol. 2019;124:110622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vaughn IA, Terry EL, Bartley EJ, Schaefer N, Fillingim RB. Racial-Ethnic Differences in Osteoarthritis Pain and Disability: A Meta-Analysis. J Pain. 2019;20(6):629–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thompson KA, Terry EL, Sibille KT, et al. At the Intersection of Ethnicity/Race and Poverty: Knee Pain and Physical Function. J Racial Ethn Health Disparities. 2019;6(6):1131–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cruz-Almeida Y, Sibille KT, Goodin BR, et al. Racial and ethnic differences in older adults with knee osteoarthritis. Arthritis & Rheumatology. 2014;66(7):1800–1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glover TL, Goodin BR, Horgas AL, et al. Vitamin D, race, and experimental pain sensitivity in older adults with knee osteoarthritis. Arthritis Rheum. 2012;64(12):3926–3935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ahn H, Weaver M, Lyon DE, et al. Differences in Clinical Pain and Experimental Pain Sensitivity Between Asian Americans and Whites With Knee Osteoarthritis. Clin J Pain. 2017;33(2):174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bartley EJ, Hossain NI, Gravlee CC, et al. Race/Ethnicity Moderates the Association Between Psychosocial Resilience and Movement-Evoked Pain in Knee Osteoarthritis. ACR Open Rheumatol. 2019;1(1):16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vina ER, Ran D, Ashbeck EL, Kwoh CK. Natural history of pain and disability among African-Americans and Whites with or at risk for knee osteoarthritis: A longitudinal study. Osteoarthritis Cartilage. 2018;26(4):471–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Walker JL, Harrison TC, Brown A, Thorpe RJ Jr., Szanton SL. Factors associated with disability among middle-aged and older African American women with osteoarthritis. Disabil Health J. 2016;9(3):510–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Flowers PPE, Schwartz TA, Arbeeva L, et al. Racial differences in performance-based function and potential explanatory factors among individuals with knee osteoarthritis. Arthritis Care Res (Hoboken). 2019. [DOI] [PMC free article] [PubMed]
- 36.Allen KD, Oddone EZ, Coffman CJ, Keefe FJ, Lindquist JH, Bosworth HB. Racial differences in osteoarthritis pain and function: potential explanatory factors. Osteoarthritis & Cartilage. 2010;18:160–167. [DOI] [PubMed] [Google Scholar]
- 37.Allen KD, Chen JC, Callahan LF, et al. Racial differences in knee osteoarthritis pain: potential contribution of occupational and household tasks. J Rheumatol. 2012;39(2):337–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ahn H, Weaver M, Lyon D, Choi E, Fillingim RB. Depression and Pain in Asian and White Americans With Knee Osteoarthritis. J Pain. 2017;18(10):1229–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dominguez-Berjon MF, Borrell C, Cano-Serral G, et al. [Constructing a deprivation index based on census data in large Spanish cities(the MEDEA project)]. Gac Sanit. 2008;22(3):179–187. [DOI] [PubMed] [Google Scholar]
- 40.Reyes C, Garcia-Gil M, Elorza JM, et al. Socio-economic status and the risk of developing hand, hip or knee osteoarthritis: a region-wide ecological study. Osteoarthritis Cartilage. 2015;23(8):1323–1329. [DOI] [PubMed] [Google Scholar]
- 41.Hannan MT, Anderson JJ, Pincus T, Felson DT. Educational attainment and osteoarthritis: differential associations with radiographic changes and symptom reporting. J Clin Epidemiol. 1992;45(2):139–147. [DOI] [PubMed] [Google Scholar]
- 42.Grotle M, Hagen KB, Natvig B, Dahl FA, Kvien TK. Prevalence and burden of osteoarthritis: results from a population survey in Norway. J Rheumatol. 2008;35(4):677–684. [PubMed] [Google Scholar]
- 43.Jorgensen KT, Pedersen BV, Nielsen NM, Hansen AV, Jacobsen S, Frisch M. Socio-demographic factors, reproductive history and risk of osteoarthritis in a cohort of 4.6 million Danish women and men. Osteoarthritis Cartilage. 2011;19(10):1176–1182. [DOI] [PubMed] [Google Scholar]
- 44.Callahan LF, Shreffler J, Siaton BC, et al. Limited educational attainment and radiographic and symptomatic knee osteoarthritis: a cross-sectional analysis using data from the Johnston County (North Carolina) Osteoarthritis Project. Arthritis research & therapy. 2010;12(2):R46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Callahan LF, Cleveland RJ, Shreffler J, et al. Associations of educational attainment, occupation and community poverty with knee osteoarthritis in the Johnston County (North Carolina) osteoarthritis project. Arthritis research & therapy. 2011;13(5):R169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cleveland RJ, Luong ML, Knight JB, et al. Independent associations of socioeconomic factors with disability and pain in adults with knee osteoarthritis. BMC Musculoskelet Disord. 2013;14:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hawker GA, Wright JG, Glazier RH, et al. The effect of education and income on need and willingness to undergo total joint arthroplasty. Arthritis Rheum. 2002;46(12):3331–3339. [DOI] [PubMed] [Google Scholar]
- 48.Kiadaliri AA, Gerhardsson de Verdier M, Turkiewicz A, Lohmander LS, Englund M. Socioeconomic inequalities in knee pain, knee osteoarthritis, and health-related quality of life: a population-based cohort study in southern Sweden. Scand J Rheumatol. 2017;46(2):143–151. [DOI] [PubMed] [Google Scholar]
- 49.Luong ML, Cleveland RJ, Nyrop KA, Callahan LF. Social determinants and osteoarthritis outcomes. Aging health. 2012;8(4):413–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Peters TJ, Sanders C, Dieppe P, Donovan J. Factors associated with change in pain and disability over time: a community-based prospective observational study of hip and knee osteoarthritis. Br J Gen Pract. 2005;55(512):205–211. [PMC free article] [PubMed] [Google Scholar]
- 51.Reichmann WM, Katz JN, Losina E. Differences in self-reported health in the Osteoarthritis Initiative (OAI) and Third National Health and Nutrition Examination Survey (NHANES-III). PLoS One. 2011;6(2):e17345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–1330. [DOI] [PubMed] [Google Scholar]
- 53.Pereira D, Peleteiro B, Araujo J, Branco J, Santos RA, Ramos E. The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthritis Cartilage. 2011;19(11):1270–1285. [DOI] [PubMed] [Google Scholar]
- 54.Bergink AP, Uitterlinden AG, Van Leeuwen JP, et al. Vitamin D status, bone mineral density, and the development of radiographic osteoarthritis of the knee: The Rotterdam Study. J Clin Rheumatol. 2009;15(5):230–237. [DOI] [PubMed] [Google Scholar]
- 55.Oka H, Akune T, Muraki S, et al. Association of low dietary vitamin K intake with radiographic knee osteoarthritis in the Japanese elderly population: dietary survey in a population-based cohort of the ROAD study. J Orthop Sci. 2009;14(6):687–692. [DOI] [PubMed] [Google Scholar]
- 56.Salaffi F, Carotti M, Stancati A, Grassi W. Health-related quality of life in older adults with symptomatic hip and knee osteoarthritis: a comparison with matched healthy controls. Aging Clin Exp Res. 2005;17(4):255–263. [DOI] [PubMed] [Google Scholar]
- 57.Kim I, Kim HA, Seo YI, Song YW, Jeong JY, Kim DH. The prevalence of knee osteoarthritis in elderly community residents in Korea. J Korean Med Sci. 2010;25(2):293–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lee S, Kim SJ. Prevalence of knee osteoarthritis, risk factors, and quality of life: The Fifth Korean National Health And Nutrition Examination Survey. Int J Rheum Dis. 2017;20(7):809–817. [DOI] [PubMed] [Google Scholar]
- 59.Kang X, Fransen M, Zhang Y, et al. The high prevalence of knee osteoarthritis in a rural Chinese population: the Wuchuan osteoarthritis study. Arthritis Rheum. 2009;61(5):641–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Boring MA, Hootman JM, Liu Y, et al. Prevalence of Arthritis and Arthritis-Attributable Activity Limitation by Urban-Rural County Classification - United States, 2015. MMWR Morb Mortal Wkly Rep. 2017;66(20):527–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30(8):914–918. [DOI] [PubMed] [Google Scholar]
- 62.Johnson VL, Hunter DJ. The epidemiology of osteoarthritis. Best Pract Res Clin Rheumatol. 2014;28(1):5–15. [DOI] [PubMed] [Google Scholar]
- 63.Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000;133(8):635–646. [DOI] [PubMed] [Google Scholar]
- 64.Hill JL, You W, Zoellner JM. Disparities in obesity among rural and urban residents in a health disparate region. BMC Public Health. 2014;14:1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Goodman SM, Mandl LA, Mehta B, et al. Does Education Level Mitigate the Effect of Poverty on Total Knee Arthroplasty Outcomes? Arthritis Care Res (Hoboken). 2018;70(6):884–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Moss AS, Murphy LB, Helmick CG, et al. Annual incidence rates of hip symptoms and three hip OA outcomes from a U.S. population-based cohort study: the Johnston County Osteoarthritis Project. Osteoarthritis Cartilage. 2016;24(9):1518–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ali-Gombe A, Croft PR, Silman AJ. Osteoarthritis of the hip and acetabular dysplasia in Nigerian men. The Journal of Rheumatology. 1996;23(3):512–515. [PubMed] [Google Scholar]
- 68.Solomon L, Beighton P, Lawrence JS. Rheumatic disorders in the South African Negro. Part II. Osteo-arthritis. South African Medical Journal. 1975;49:1737–1740. [PubMed] [Google Scholar]
- 69.Lawrence JS, Sebo M. The geography of osteoarthritis. In: Nuki GK, ed. The Aetiopathogeneis of Osteoarthritis London: Pitman; 1980. [Google Scholar]
- 70.Nelson AE, Braga L, Renner JB, et al. Characterization of individual radiographic features of hip osteoarthritis in African American and White women and men: the Johnston County Osteoarthritis Project. Arthritis Care Res (Hoboken). 2010;62(2):190–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tepper S, Hochberg M. Factors associated with hip osteoarthritis: data from the First National Health and Nutrition Examination Survey (NHANES-I). American Journal of Epidemiology. 1993;137(10):1081–1088. [DOI] [PubMed] [Google Scholar]
- 72.Jordan JM, Helmick CG, Renner JB, et al. Prevalence of hip symptoms and radiographic and symptomatic hip osteoarthritis in African Americans and Whites: The Johnston County Osteoarthritis Project. The Journal of Rheumatology. 2009;36(4):809–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Murphy LB, Helmick CG, Schwartz TA, et al. One in four people may develop symptomatic hip osteoarthritis in his or her lifetime. Osteoarthritis & Cartilage. 2010;18(11):1372–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nevitt MC, Xu L, Zhang Y, et al. Very low prevalence of hip osteoarthritis among Chinese elderly in Beijing, China, compared with whites in the United States: the Beijing osteoarthritis study. Arthritis Rheum. 2002;46(7):1773–1779. [DOI] [PubMed] [Google Scholar]
- 75.Edwards K, Leyland KM, Sanchez-Santos MT, et al. Differences between race and sex in measures of hip morphology: a population-based comparative study. Osteoarthritis Cartilage. 2020;28(2):189–200. [DOI] [PubMed] [Google Scholar]
- 76.Foley B, Cleveland RJ, Renner JB, Jordan JM, Nelson AE. Racial differences in associations between baseline patterns of radiographic osteoarthritis and multiple definitions of progression of hip osteoarthritis: the Johnston County Osteoarthritis Project. Arthritis research & therapy. 2015;17:366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cleveland RJ, Schwartz TA, Prizer LP, et al. Associations of educational attainment, occupation, and community poverty with hip osteoarthritis. Arthritis Care Res (Hoboken). 2013;65(6):954–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Knight JB, Callahan LF, Luong ML, et al. The association of disability and pain with individual and community socioeconomic status in people with hip osteoarthritis. Open Rheumatol J. 2011;5:51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Greene ME, Rolfson O, Nemes S, Gordon M, Malchau H, Garellick G. Education attainment is associated with patient-reported outcomes: findings from the Swedish Hip Arthroplasty Register. Clin Orthop Relat Res. 2014;472(6):1868–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Schafer T, Krummenauer F, Mettelsiefen J, Kirschner S, Gunther KP. Social, educational, and occupational predictors of total hip replacement outcome. Osteoarthritis Cartilage. 2010;18(8):1036–1042. [DOI] [PubMed] [Google Scholar]
- 81.Clement ND, Muzammil A, Macdonald D, Howie CR, Biant LC. Socioeconomic status affects the early outcome of total hip replacement. J Bone Joint Surg Br. 2011;93(4):464–469. [DOI] [PubMed] [Google Scholar]
- 82.Kim C, Linsenmeyer KD, Vlad SC, et al. Prevalence of radiographic and symptomatic hip osteoarthritis in an urban United States community: the Framingham osteoarthritis study. Arthritis Rheumatol. 2014;66(11):3013–3017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Park JH, Hong JY, Han K, et al. Prevalence of symptomatic hip, knee, and spine osteoarthritis nationwide health survey analysis of an elderly Korean population. Medicine (Baltimore). 2017;96(12):e6372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yoshimura N, Campbell L, Hashimoto T, et al. Acetabular dysplasia and hip osteoarthritis in Britain and Japan. Br J Rheumatol. 1998;37(11):1193–1197. [DOI] [PubMed] [Google Scholar]
- 85.Ding C, Cicuttini F, Boon C, et al. Knee and hip radiographic osteoarthritis predict total hip bone loss in older adults: a prospective study. J Bone Miner Res. 2010;25(4):858–865. [DOI] [PubMed] [Google Scholar]
- 86.Andrianakos AA, Kontelis LK, Karamitsos DG, et al. Prevalence of symptomatic knee, hand, and hip osteoarthritis in Greece. The ESORDIG study. J Rheumatol. 2006;33(12):2507–2513. [PubMed] [Google Scholar]
- 87.Quintana JM, Arostegui I, Escobar A, Azkarate J, Goenaga JI, Lafuente I. Prevalence of knee and hip osteoarthritis and the appropriateness of joint replacement in an older population. Arch Intern Med. 2008;168(14):1576–1584. [DOI] [PubMed] [Google Scholar]
- 88.Zhang JF, Song LH, Wei JN, et al. Prevalence of and risk factors for the occurrence of symptomatic osteoarthritis in rural regions of Shanxi Province, China. Int J Rheum Dis. 2016;19(8):781–789. [DOI] [PubMed] [Google Scholar]
- 89.Iidaka T, Muraki S, Akune T, et al. Prevalence of radiographic hip osteoarthritis and its association with hip pain in Japanese men and women: the ROAD study. Osteoarthritis Cartilage. 2016;24(1):117–123. [DOI] [PubMed] [Google Scholar]
- 90.Goodman SM, Mehta B, Zhang M, et al. Disparities in Total Hip Arthroplasty Outcomes: Census Tract Data Show Interactions Between Race and Community Deprivation. J Am Acad Orthop Surg. 2018;26(21):e457–e464. [DOI] [PubMed] [Google Scholar]
- 91.Feldman CH, Dong Y, Katz JN, Donnell-Fink LA, Losina E. Association between socioeconomic status and pain, function and pain catastrophizing at presentation for total knee arthroplasty. BMC Musculoskelet Disord. 2015;16:18. [DOI] [PMC free article] [PubMed] [Google Scholar]


