Abstract
Background:
COVID-19 has had a significant impact on the economy, health care, and society as a whole. To prevent the spread of infection, local governments across the United States issued mandatory lockdowns and stay-at-home orders. In the surgical world, elective cases ceased to help “flatten the curve” and prevent the infection from spreading to hospital staff and patients. We explored the effect of the cancellation of these procedures on trainee operative experience at our high-volume, multihospital neurosurgical practice.
Methods:
Our department cancelled all elective cases starting March 16, 2020, and resumed elective surgical and endovascular procedures on May 11, 2020. We retrospectively reviewed case volumes for 54 days prelockdown and 54 days postlockdown to evaluate the extent of the decrease in surgical volume at our institution. Procedure data were collected and then divided into cranial, spine, functional, peripheral nerve, pediatrics, and endovascular categories.
Results:
Mean total cases per day in the prelockdown group were 12.26 ± 7.7, whereas in the postlockdown group, this dropped to 7.78 ± 5.5 (P = 0.01). In the spine category, mean cases per day in the prelockdown group were 3.13 ± 2.63; in the postlockdown group, this dropped to 0.96 ± 1.36 (P < 0.001). In the functional category, mean cases per day in the prelockdown group were 1.31 ± 1.51, whereas in the postlockdown group, this dropped to 0.11 ± 0.42 (P < 0.001). For cranial (P = 0.245), peripheral nerve (P = 0.16), pediatrics (P = 0.34), and endovascular (P = 0.48) cases, the volumes dropped but were not statistically significant decreases.
Conclusion:
The impact of this outbreak on operative training does appear to be significant based solely on statistics. Although the drop in case volumes during this time can be accounted for by the pandemic, it is important to understand that this is a multifactorial effect. Further studies are needed for these results to be generalizable and to fully understand the effect this pandemic has had on trainee operative experience.
Keywords: Case volumes, COVID-19 pandemic, Lockdown, Operative experience, Trainees

INTRODUCTION
COVID-19 is an extremely infectious disease that has had a detrimental effect on global health care, health care workers, and the international economy.[3,10] On March 13, 2020, the American College of Surgeons recommended complete cessation of elective cases[4] across surgical disciplines in an effort to prevent further spread of the novel coronavirus.
The American College of Surgeons’ recommendations to cancel all elective cases and office visits meant that neurosurgery case volumes significantly decreased over the course of this pandemic. In an effort to comply with these recommendations, academic neurosurgical practices rescheduled all elective cases, moved to telehealth outpatient visits, and adopted a teleconference approach to continue resident education meetings and department-wide conferences.[6-8,11] Furthermore, during this lockdown period, many training programs, including our own, decreased resident coverage in hospitals to a 1 week on and 1 week off model to prevent further spread of the virus.[4,5,8,11] This has affected the training of chief, mid-level, and junior residents, and endovascular and spine fellows within our department.
Our academic neurosurgical practice has constantly been growing in case volume over the last several years. We routinely perform cases in all areas of neurosurgery, which include cranial, spine, functional, pediatrics, peripheral nerve, and endovascular. In our region, complete “lockdown” was issued by the governor to take effect on March 22, 2020 (https://coronavirus.health.ny.gov/new-york-state-pause); however, in anticipation of an influx of coronavirus cases in our region before that date, our neurosurgery department cancelled elective procedures on March 16, 2020. After meeting the criteria of Phase I reopening, we started to schedule elective cases once again as of May 11, 2020. We explored the reduction in case volume and the associated effect on training during this lockdown period.
MATERIALS AND METHODS
After the University at Buffalo institutional review board deemed our study as “no greater than minimal risk,” we conducted a retrospective review of all neurosurgical cases (cranial, spine, functional, peripheral nerve, pediatric, and endovascular) performed from January 22, 2020, through May 8, 2020. Because elective surgeries are not routinely performed on weekends, we decided to collect data only through Friday, March 8, 2020, and not include the last weekend before elective surgeries resumed. From the day our department cancelled elective surgeries on March 16, 2020– May 8, 2020, that meant a period of 54 days without elective surgery. Given this information, we decided to compare the case numbers to the 54 days before the cancellation of elective cases and used the dates January 22, 2020–March 15, 2020, for the comparison group.
Case data that were collected were divided into cranial, spine, functional, peripheral nerve, pediatrics, and endovascular categories. Data were reported as case volumes per day and per every 6 days (normal trainee work week). Cases completed at Buffalo General Hospital, Gates Vascular Institute, and Oishei Children’s Hospital were included in our analysis because most of our residents and all of our fellows are based at these hospitals. Department staff also perform procedures at Erie County Medical Center (1 resident covers this level I trauma hospital), Roswell Park Cancer Institute (1 resident covers this hospital), Sisters of Charity Hospital (no residents cover this hospital), Millard Fillmore Suburban Hospital (no residents cover this hospital), Kenmore Mercy Hospital (no residents cover this hospital), and Mount Saint Mary’s Hospital (no resident covers this hospital), within the Western New York region. There was no cessation of cases at Erie County Medical Center or Roswell Park Cancer Institute.
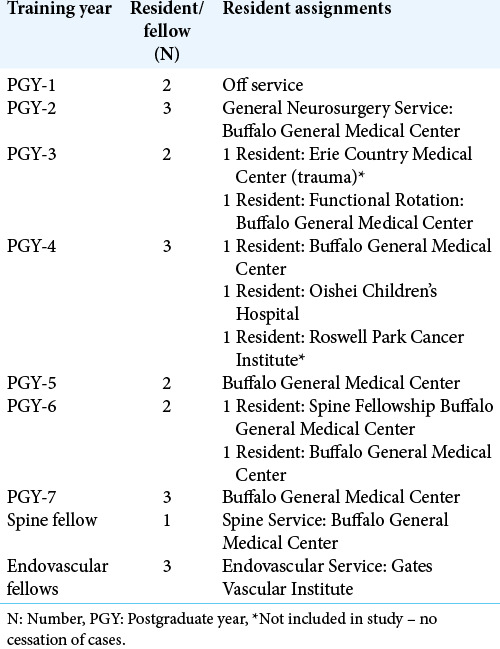
Our trainee cohort consisted of three chief residents, two postgraduate year (PGY)-6 residents (1 of whom was a completing an enfolded spine fellowship), two PGY-5 residents, three PGY-4 residents, two PGY-3 residents, three PGY-2 residents, two PGY-1 residents, three neuroendovascular fellows, and one additional spine fellow, for a total of 17 residents and four fellows. Routinely at our institution, chief residents perform high-level, complex cranial and spine cases. Our PGY-6 who was doing the enfolded spine fellowship was solely performing spine cases, and the other PGY-6 was performing miscellaneous operations along with our PGY-5s and 1 PGY-4 on service. Our PGY-4s were split between our pediatric hospital and cancer hospital (for which the data were not available), and our general service. Our PGY-3s were split between functional cases and a rotation at our trauma center. PGY-2s were on primary service, seeing consultations and managing patients in the intensive care unit on the floor. PGY-1s were off general neurosurgery service during the pandemic and were placed on various Accreditation Council for Graduate Medical Education (ACGME)-required rotations. Our endovascular fellows were performing solely endovascular procedures, and our additional spine fellow was performing only spine cases. A complete breakdown of our resident and fellow cohort and their assignments prelockdown is provided in [Table 1].
Table 1:
Resident and fellow assignments at our institution.
Statistical methods
SPSS Version 26 (IBM, Armonk, NY) was used for statistical analysis of procedural data. Continuous variables were reported as weighted mean ± standard deviation, and categorical variables were reported as a percentage. Levene’s test was used to assess for homogeneity of variance. Independent t-test or Mann–Whitney U-test was performed to compare for mean prelockdown and postlockdown caseloads. Excel version 16.30 (Microsoft, Redmond, WA) was used for graphical depiction of the data. Alpha was set at 0.05 with any value <0.05 considered statistically significant.
RESULTS
A categorical breakdown of our prelockdown and postlockdown raw numbers is provided in [Table 2].
Table 2:
Case volumes prelockdown and postlockdown.
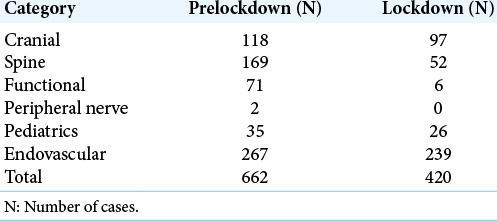
Total cases
Mean cases per day in the prelockdown group were 12.26 ± 7.7; in the postlockdown group, this dropped to 7.78 ± 5.5 (P = 0.01). When the data were analyzed per 6 days, mean case volume prelockdown was 73.56 ± 12.03 and dropped to 46.67 ± 20.31 postlockdown (P = 0.05).
Cranial cases
Mean cases per day in the prelockdown group were 2.19 ± 1.77; in the postlockdown group, this dropped to 1.80 ± 1.68 (P = 0.245). When the data were analyzed per 6 days, mean case volume prelockdown was 13.11 ± 4.18. Postlockdown, this dropped to 10.78 ± 6.24 cases (P = 0.368).
Spine cases
Mean cases per day in the prelockdown group were 3.13 ± 2.63. In the postlockdown group, this dropped to 0.96 ± 1.36 (P < 0.001). When the data were analyzed per 6 days, mean case volume prelockdown was 18.78 ± 5.74 and dropped to 5.78 ± 4.41 in the postlockdown group (P < 0.001).
Functional cases
Mean cases per day in the prelockdown group were 1.31 ± 1.51, whereas in the postlockdown group, this dropped to 0.11 ± 0.42 (P <0.001). When the data were analyzed per 6 days, mean case volume prelockdown was 7.89 ± 2.36, and this dropped to 0.6 ± 0.86 (P < 0.001) postlockdown.
Peripheral nerve cases
Mean cases per day in the prelockdown group were 0.04 ± 0.19. In the postlockdown group, this dropped to 0 (P = 0.16). When the data were analyzed per 6 days, mean case volume prelockdown was 0.22 ± 0.44; this dropped to 0 (P = 0.17).
Pediatric cases
Mean cases per day in the prelockdown group were 0.65 ± 1.03, whereas in the postlockdown group, this dropped to 0.48 ± 0.77 (P = 0.34). When the data were analyzed per 6 days, mean case volume prelockdown was 3.89 ± 2.32; this dropped to 2.89 ± 1.17 (P = 0.27) postlockdown.
Endovascular cases
Mean cases per day in the prelockdown group were 4.94 ± 3.75. In the postlockdown group, this dropped to 4.43 ± 3.88 (P = 0.48). When the data were analyzed per 6 days, mean case volume prelockdown was 29.67 ± 8.2 and dropped to 26.56 ± 14.6 (P = 0.59) postlockdown.
DISCUSSION
During the lockdown period, we saw a decrease in total case volumes in all procedure categories studied. Spine and functional cases were affected the most, demonstrating statistical significance.
Cranial
Cranial cases at our institution comprise brain tumor resections, open vascular cases, cerebrospinal fluid flow diversion, cranioplasties, and brain biopsies. As the statistics demonstrates, there has been a decrease in cranial case volume after the lockdown commenced, although this was not statistically significant. Routinely, the high-level cranial cases are performed by our chief residents and the less complex cranial cases are divided among mid-level residents. During the 54-day prelockdown period, a total of 118 cranial cases were completed; while during the lockdown, 97 cranial cases were completed, resulting in a drop of 21 cases. The effect this had on resident training can be argued based on published literature as Agarwal et al. studied the trends in cranial case volumes and concluded there to be an increase of 26.59 cases per resident, per year, between 2009 and 2017.[1] Based on those trends, our 54-day long lockdown period likely did not impact the state of resident education to a significant capacity. That being stated, the pandemic occurring toward the end of the academic year, during a time when chief residents start to gain more autonomy and become comfortable performing the critical portions of complex cranial cases under attending supervision, might have impacted their growth to some extent as they transition toward independent practice later this year.
Spine
Spine cases were markedly down postlockdown. During the 54 days prelockdown, a total of 169 spine cases were performed, which dropped dramatically to 52 cases. This is understandable because most spine cases at our institution are done on an elective basis. Routinely, the spine fellow and our resident serving an enfolded spine fellowship complete our spine cases with the assistance of a mid-level or junior resident under the supervision of an attending neurosurgeon. On a regular basis, approximately three spine cases are performed daily, and this decreased to <1 case per day. Thus, our spine fellows and neurosurgery residents lost the opportunity for 117 total cases of spine experience during the 54 days of the lockdown in our practice. Pham et al. studied the trends in spine surgery over a 10-year period between 2009 and 2018 and found that the average number of spine cases per neurosurgical resident increased 26.5% over that time period.[12] They also found that in 2018, an average of 477.5 spine cases was performed per neurosurgical resident; whereas in 2009, an average of 374.3 spine cases was performed per neurosurgical resident. Agarwal et al. reported similar numbers in spine procedures in their study, though this study was an evaluation of resident case logs between 2013 and 2017.[2] Although the 54-day lockdown reduced our spine volume significantly, based on those trends, it is unlikely to hinder our residents meeting their minimum requirement of spine cases for graduation. That being said, it can be argued that the lockdown on a perresident basis may have hindered their operative skills. Usually, junior residents (PGY1-3) learn the basics of operative technique during routine spine cases and become comfortable with positioning, opening, exposure, anatomy visualization, closing, and develop their overall surgical confidence during these cases. As our junior residents, particularly PGY-2 and PGY-3 residents, transition into their next academic year, the loss of these cases may have a negative impact on their overall surgical skills as they progress through residency.
Functional
The volume of functional cases at our institution also declined significantly during the lockdown period. On our service, a PGY-3 or PGY-6 resident rotates with the functional team for 3 months at a time. Our data show that the functional resident performed 71 cases over the course of the 54 days prelockdown. Typically, these cases include deep brain stimulation, spinal cord stimulators, baclofen pump placements, and epilepsy focused surgery. During the lockdown period, only six functional cases were performed over a course of 54 days. The resident who was on the functional rotation, which only lasts 3 months at our institution, missed out on the opportunity for valuable functional neurosurgery experience. Agarwal et al. found that between 2009 and 2017 residents were completing 6.82 times more functional cases than the minimum required standard established by the ACGME, throughout the course of their residency.[1] In terms of completing the required number of cases, once again, the pandemic will unlikely hinder that based on the previously published trends. The completion of graduation requirements may not be hindered, but it is important to consider that missed opportunities for surgical training during the transition from junior-level resident to mid-level resident can possibly hinder the surgical growth of residents because they are expected to take on more responsibility in the operating room during each transition. Typically at our institution, it is during the functional rotation where junior-level residents start to learn the nuances of intracranial neurosurgical practice.
Pediatrics
Compared to adult neurosurgery, our pediatric neurosurgical case volume is low. Based on our analysis, pediatric case numbers were not impacted by the lockdown significantly when compared to prelockdown numbers. A PGY-4 resident normally rotates with our pediatric neurosurgery team for 4–6 months. Furthermore, it is worth mentioning that our pediatric neurosurgery team performs operations 2 days a week, unlike their adult neurosurgery team counterparts who perform cases every day of the week. Prelockdown, there were 35 cases over the course of 54 days; postlockdown, this number dropped to 26 cases. These cases consist of cranial and spine procedures. Pediatric neurosurgical experience during residency is scarce when compared to adult neurosurgical experience, with only 10.5% of programs having more than 1000 cases a year and 11.8% performing <100 cases a year.[1,2,9,12] White et al. found that the average number of pediatric neurosurgical cases performed per resident between the years 2013 and 2017 was 98.8, which was less than the average numbers for operations on adult patients.[13] At our practice, the lockdown did not seem to significantly impact the number of cases for the rotating resident and is unlikely to affect the ACGME requirements of pediatric cases for graduation. The pediatric rotation here is a bridge from junior residency to senior residency and is often when our residents learn to hone their microsurgical skills operating under a microscope. This is also the time that they familiarize themselves with more complex cranial anatomy, operating on posterior fossa tumors often for the 1st time as a first assist. Honing their microsurgical skills in cranial and spinal cases prepare them well as they transition back to adult neurosurgery and are expected to have more autonomy during complex cranial cases. Although the numbers are often variable per resident and their experience at our pediatric hospital differs in terms of case types, it can be concluded that the microsurgical experience of our pediatric resident as a first assist did suffer during this lockdown.
Endovascular
Due to the emergent nature of endovascular neurosurgery at the Gates Vascular Institute comprehensive stroke center, it is no surprise that there was not a significant decline in case numbers. Three endovascular fellows (one senior and two juniors) and a resident rotate with the endovascular team. During the lockdown, the endovascular resident was pulled from the rotation to minimize exposure to staff and patients and was placed on the general neurosurgery team as 17 part of the 1 week on and 1 week off skeleton crew. Although this did not result in a significant decrease in case volume, resident training in the endovascular realm was affected. Again, Agarwal et al. demonstrated an overall increase in endovascular cases completed compared to ACGME requirements, so this should not impact training on a more global scale.[1] That being stated, our resident who lost almost 2 months of the endovascular rotation will need to satisfy the ACGME’s endovascular requirements. Furthermore, it is reasonable to point out that endovascular neurosurgery has certain nuances of medical management that are not routinely performed by nonendovascular neurosurgeons, and losing out on that aspect of the rotation for our resident is another aspect to consider.
Moving forward
At an academic institution, trainee education is a top priority in ensuring that trainees meet case requirements and are properly trained before they transition into practice. Every academic year, whether during residency or fellowship, there are opportunities to learn and gain experience in the operating room. With talks in the media of a second wave of COVID-19 coming to overwhelm our health-care system again, many states are anticipating a second lockdown as the number of cases rise. We have yet to see the effect of a second wave on neurosurgical practice. If elective cases are cancelled again for some period of time, there will certainly be further impact on trainee operative experience. Therefore, we are encouraging trainees to double scrub during cases and potentially hiring more nurse practitioners and physician assistants to ease the burden of routine hospital floor tasks on junior residents in the hope that they can operate on a more consistent basis. With an anticipated second wave and intensive care units being overloaded, neurosurgeons may be recruited for the management of critically ill COVID-19 patients. Furthermore, if a second wave does cause a shutdown, neurosurgeons and hospitals should develop a protocol for certain subgroups of elective cases to proceed. For example, each patient should be tested for COVID-19 before surgical intervention, and cases with an anticipated discharge within 3 days of surgical intervention should be allowed to continue with minimal risk to the patient and staff if appropriate caution is implemented. This will allow patients to obtain their surgical intervention and trainees to continue to hone their surgical skills.
Limitations
Our study has the inherent limitations of a single-center retrospective review design. Case volumes were collected for only 54 days prelockdown and 54 days of lockdown. These results may not be generalized to academic neurosurgical practices across the nation due to the small sample size and the inherent differences in program structures.
CONCLUSION
COVID-19 has had an impact on trainee education in many ways. To the best of our knowledge, we report the first study on its direct impact on case volume at an academic neurosurgical practice. Although the impact of this pandemic on training has been multifactorial because it has also resulted in a decrease in conferences, consults being conducted through simple chart review, and resident teaching being conducted remotely, its impact on the operating room does appear to be significant based on our case volume data. Further studies are warranted on the long-term impacts of resident education and trends of case volumes overtime and the complexity of these cases until we return to “normalcy.”
Acknowedgment
We thank Debra J. Zimmer for editorial assistance.
Footnotes
How to cite this article: Khan A, Mao JZ, Soliman MA, Rho K, Hess RM, Reynolds RM, et al. The effect of COVID-19 on trainee operative experience at a multihospital academic neurosurgical practice: A first look at case numbers. Surg Neurol Int 2021;12:271.
Contributor Information
Asham Khan, Email: akhan@ubns.com.
Jennifer Z. Mao, Email: jmao@ubns.com.
Mohamed A. R. Soliman, Email: moh.ar.sol@kasralainy.edu.eg.
Kyungduk Rho, Email: krho@ubns.com.
Ryan M. Hess, Email: rhess@ubns.com.
Renée M. Reynolds, Email: rreynolds@ubns.com.
Jonathan P. Riley, Email: jriley@ubns.com.
Jeffrey P. Mullin, Email: jmullin@ubns.com.
Adnan H. Siddiqui, Email: asiddiqui@ubns.com.
Elad I. Levy, Email: elevy@ubns.com.
John Pollina, Email: jpollina@ubns.com.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
The authors report the following relationships, although not directly related to this submission: Dr. Pollina: Surgical training: Medtronic; Consultant and royalties: ATEC Spine. Dr. Mullin: Clinical research: Cerapedics; Research funding: AOSpine North America (AOSNA) and the Research Committee Award #87639; Medtronic: External Research Program Health Professionals, ERP ID#2020-12271 Dr. Levy: Shareholder/Ownership interests: NeXtGen Biologics, RAPID Medical, Claret Medical, Cognition Medical, Imperative Care (formerly the Stroke Project), Rebound Therapeutics, StimMed, Three Rivers Medical; National Principal Investigator/Steering Committees: Medtronic (merged with Covidien Neurovascular) SWIFT Prime and SWIFT Direct Trials; Honoraria: Medtronic (training and lectures); Consultant: Claret Medical, GLG Consulting, Guidepoint Global, Imperative Care, Medtronic, Rebound, StimMed; Advisory Board: Stryker (AIS Clinical Advisory Board), NeXtGen Biologics, MEDX, Cognition Medical, Endostream Medical; Site Principal Investigator: CONFIDENCE study (MicroVention), STRATIS Studyu2014Sub I (Medtronic). Dr. Siddiqui: Financial interest/investor/stock options/ ownership: Adona Medical, Inc., Amnis Therapeutics (Purchased by Boston Scientific October 2017), Blink TBI Inc., Buffalo Technology Partners Inc., Cerebrotech Medical Systems, Inc., Cognition Medical, Endostream Medical Ltd., Imperative Care, International Medical Distribution Partners, Neurovascular Diagnostics Inc., Qu2019Apel Medical Inc., Rebound Therapeutics Corp. (Purchased 2019 by Integra Lifesciences, Corp.), Rist Neurovascular Inc., Sense Diagnostics, Inc., Serenity Medical Inc., Silk Road Medical, Spinnaker Medical, Inc., StimMed, Synchron, Three Rivers Medical Inc., Vastrax, LLC, VICIS, Inc., Viseon, Inc.; Consultant/advisory board: Amnis Therapeutics, Boston Scientific, Canon Medical Systems USA Inc., Cerebrotech Medical Systems Inc., Cerenovus, Corindus Inc., Endostream Medical Ltd., Imperative Care, Inc., Integra LifeSciences Corp., Medtronic, MicroVention, Minnetronix Neuro, Inc., Northwest Universityu2013DSMB Chair for HEAT Trial, Penumbra, Qu2019Apel Medical Inc., Rapid Medical, Rebound Therapeutics Corp.(Purchased by Integra LifeSciences Corp.), Serenity Medical Inc., Silk Road Medical, StimMed, Stryker, Three Rivers Medical, Inc., VasSol, W.L. Gore and Associates; Principal investigator/steering committee of the following trials: Cerenovus NAPA and ARISE II; Medtronic SWIFT PRIME and SWIFT DIRECT; MicroVention FRED and CONFIDENCE; MUSC POSITIVE; and Penumbra 3D Separator, COMPASS, INVEST, TIGER. Dr. Riley: Consultant: Voyager Therapeutics (refinement of intracranial gene therapy delivery approaches). Ms. Mao receives research funding from AOSpine North America (AOSNA) for works to advance 3D printing. Dr. Khan received a research grant from the Scoliosis Research Society to study scoliosis in Chiari patients. Remaining authors: None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Agarwal N, White MD, Cohen J, Lunsford LD, Hamilton DK. Longitudinal survey of cranial case log entries during neurological surgery residency training. J Neurosurg. 2018;2018:1–7. doi: 10.3171/2018.2.JNS172734. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal N, White MD, Hamilton DK. A longitudinal survey of adult spine and peripheral nerve case entries during neurosurgery residency training. J Neurosurg Spine. 2018;29:442–7. doi: 10.3171/2018.3.SPINE171370. [DOI] [PubMed] [Google Scholar]
- 3.Alradhawi M, Shubber N, Sheppard J, Ali Y. Effects of the COVID-19 pandemic on mental well-being amongst individuals in society a letter to the editor on the socioeconomic implications of the coronavirus and COVID-19 pandemic: A review. Int J Surg. 2020;78:147–8. doi: 10.1016/j.ijsu.2020.04.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bambakidis NC, Tomei KL. Editorial, Impact of COVID-19 on neurosurgery resident training and education. J Neurosurg. 2020;2020:1–2. doi: 10.3171/2020.3.JNS20965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carter BS, Chiocca EA. Editorial, COVID-19 and academic neurosurgery. J Neurosurg. 2020;2020:1–2. doi: 10.3171/2020.4.JNS201013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eichberg DG, Shah AH, Luther EM, Menendez I, Jimenez A, Perez-Dickens M, et al. Letter: Academic neurosurgery department response to COVID-19 pandemic: The university of Miami/Jackson memorial hospital model. Neurosurgery. 2020;87:E63–5. doi: 10.1093/neuros/nyaa118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Ghandour NM, Elsebaie EH, Salem AA, Alkhamees AF, Zaazoue MA, Fouda MA, et al. Letter: The impact of the coronavirus (COVID-19) pandemic on neurosurgeons worldwide. Neurosurgery. 2020;87:E250–7. doi: 10.1093/neuros/nyaa212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hess R, Mao JZ, Rho K, Khan A, Levy E, Pollina J, et al. Letter to the editor: Embracing disruptive change during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic. World Neurosurg. 2020;139:726–7. doi: 10.1016/j.wneu.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Limoges N, D’Agostino E, Gelinne A, Maher CO, Scott RM, Grant G, et al. Pediatric neurosurgery training during residency in the United States: A program director survey. J Neurosurg Pediatr. 2020;2020:1–7. doi: 10.3171/2020.1.PEDS19662. [DOI] [PubMed] [Google Scholar]
- 10.Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg. 2020;78:185–93. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pennington Z, Lubelski D, Khalafallah AM, Ehresman J, Sciubba DM, Witham TF, et al. Letter to the editor changes to neurosurgery resident education since onset of the COVID-19 pandemic. World Neurosurg. 2020;139:734–40. doi: 10.1016/j.wneu.2020.05.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pham MH, Jakoi AM, Wali AR, Lenke LG. Trends in spine surgery training during neurological and orthopaedic surgery residency: A 10-year analysis of ACGME case log data. J Bone Joint Surg Am. 2019;101:e122. doi: 10.2106/JBJS.19.00466. [DOI] [PubMed] [Google Scholar]
- 13.White MD, Zollman J, McDowell MM, Agarwal N, Abel TJ, Hamilton DK. Neurosurgical resident exposure to pediatric neurosurgery: An analysis of resident case logs. Pediatr Neurosurg. 2019;54:181–7. doi: 10.1159/000500299. [DOI] [PubMed] [Google Scholar]


