Abstract
Japanese encephalitis (JE) is the major cause of viral encephalitis (VE) in most Asian-Pacific countries. In Vietnam, there is no nationwide surveillance system for JE due to lack of medical facilities and diagnoses. Culex tritaeniorhynchus, Culex vishnui, and Culex quinquefasciatus have been identified as the major JE vectors in Vietnam. The main objective of this study was to forecast a risk map of Culex mosquitoes in Hanoi, which is one of the most densely populated cities in Vietnam. A total of 10,775 female adult Culex mosquitoes were collected from 513 trapping locations. We collected temperature and precipitation information during the study period and its preceding month. In addition, the other predictor variables (e.g., normalized difference vegetation index [NDVI], land use/land cover and human population density), were collected for our analysis. The final model selected for estimating the Culex mosquito abundance included centered rainfall, quadratic term rainfall, rice cover ratio, forest cover ratio, and human population density variables. The estimated spatial distribution of Culex mosquito abundance ranged from 0 to more than 150 mosquitoes per 900m2. Our model estimated that 87% of the Hanoi area had an abundance of mosquitoes from 0 to 50, whereas approximately 1.2% of the area showed more than 100 mosquitoes, which was mostly in the rural/peri-urban districts. Our findings provide better insight into understanding the spatial distribution of Culex mosquitoes and its associated environmental risk factors. Such information can assist local clinicians and public health policymakers to identify potential areas of risk for JE virus. Risk maps can be an efficient way of raising public awareness about the virus and further preventive measures need to be considered in order to prevent outbreaks and onwards transmission of JE virus.
Author summary
Our study was to estimate the spatial distribution of Culex mosquitoes in Hanoi, which is one of the most densely populated cities in Vietnam. Our findings may provide better insight into understanding the spatial distribution of Culex mosquitoes and its associated environmental risk factors. Such information can assist local clinicians and public health policymakers to identify the potential areas of risk for JE virus.
Introduction
Japanese encephalitis (JE) is the major cause of viral encephalitis (VE) in most Asian-Pacific countries. It is a vector-borne flavivirus, in the same viral family, Flaviviridae, as dengue, yellow fever and West Nile virus [1–3]. About 3.1 billion people live in endemic areas with an estimated number of 50,000–68,000 clinical cases and 10,000–15,000 deaths annually [4,5]. Most human infections are asymptomatic, or very mild febrile disease, but when clinical encephalitis occurs, the death rate could reach 30%, and another 30–50% of patients suffer from permanent neurologic or psychiatric sequelae [4,6].
In Vietnam, the JE virus was first reported in 1951 and became a serious public health issue across the country, particularly in the northern part [7]. Currently, there is no nationwide surveillance system for JE due to lack of medical facilities and diagnoses, but there is national surveillance data available for viral encephalitis (VE) [8]. Some studies found that JE cases accounted for 12–72% of total VE cases, therefore VE cases can be considered to be a proxy for JE cases [8–10]. Before the vaccination was scaled out, the Red River Delta region (including Hanoi) had the highest JE incidence rate with an estimated 22 cases /100,000 people [8]. Culex tritaeniorhynchus, Culex vishnui, and Culex quinquefasciatus have been identified as the major JE vectors in Vietnam, of which the two first were mosquitoes associated with rice production, pig farms and wastewater [11–13]. In Hanoi, a study between 2006 and 2008 found the most Culex mosquitoes in rural districts of the city, and also isolated three JE virus strains from mosquitoes in the southern and western parts of Hanoi [14]. Pigs are a major amplifying host for the JE virus, and since they are commonly raised in the backyard farms, the transmission of the virus to humans is facilitated [5,15]. A study conducted in Hanoi showed that approximately 60% of pig samples from slaughterhouses were seropositive [16].
Remote sensing, with recent advances in sensor capability and open-access data policies, can provide great opportunities for public health researchers and scientists to predict and map the abundance of mosquitoes or disease risks [17–19]. By linking data from the known mosquito abundance locations with their associated environmental and socio-economic information, researchers can estimate the mosquito species distribution in other less well known locations [20]. Several studies have been conducted to map the abundance of different Culex species and potential JE transmission risk areas worldwide [21–23]. Studies suggest that the Asia, including the Southeast Asia region have the highest risk of Culex mosquitoes whereas approximately 1.7 billion people are estimated to live in areas with a high risk of encephalitis [24–26].
Previous studies have been designed to estimate the mosquito distribution at the regional and global level, which may not be suitable for the local context. In Vietnam, some studies have sought to understand the ecology of JE vectors and Culex mosquitoes [12,27,28]. However, to our knowledge, no studies have been conducted to estimate the spatial distribution of Culex mosquito abundance in Vietnam using remote sensing data. Therefore, the main objective of this study was to estimate the spatial distribution of Culex mosquitoes in Hanoi, which is one of the most densely populated cities in Vietnam. This information can be helpful for local health authorities and clinicians to implement better JE control programs by identifying the potential hotspot areas for the virus.
Materials and methods
Ethics statement
This study was approved by the Institutional Review Board for Biomedical Research of Hanoi University of Public Health No. 406/2018 YTCC-HD3.
Study area and mosquito data
The study location was Hanoi, the capital of Vietnam, which has an area of 3.359km2, consists of 30 districts and is home to approximately 8 million people (Fig 1).
Fig 1. The study area with mosquito sampling locations in Hanoi (source of shapefile: https://www.diva-gis.org/gdata).
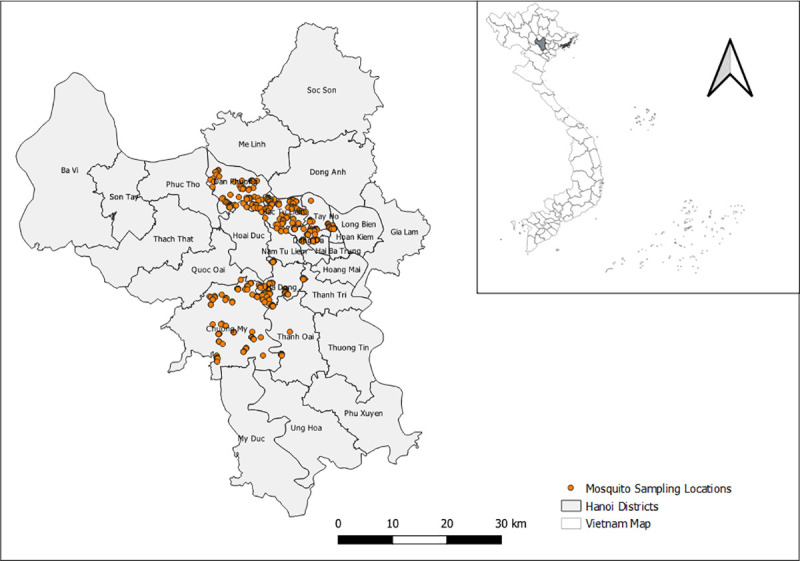
The city’s landscapes are mainly characterized by cropland and built-up infrastructure with most of the land below 20m above sea level [29]. Although the study area has experienced rapid expansion of urbanization, the majority of the land is occupied by agriculture farms (~40%), especially rice fields [30]. The rainfall and temperature vary significantly between months with monthly mean ranges of 16-330mm and 17–29°C, respectively, with a peak between June and August. The subtropical climate along with extensive rice production ecosystems can create favorable conditions for mosquito breeding [12,31].
Mosquito samples were collected in urban and peri-urban/rural areas of Hanoi from September to October 2018. A total of 513 locations were randomly selected for mosquito trapping in six districts, and the nearest consenting household with livestock and without livestock was included. At each household, CDC light and BG sentinel traps were used to collect mosquitoes both in houses and outside/gardens. Traps in the garden were installed within a radius of 20-30m from the house by investigators. Households with no insecticides or mosquito sprays were selected to avoid sampling biases.
The collected mosquito samples were transported to the Vietnam National Institute of Hygiene and Epidemiology in cool containers and identified/grouped into species using taxonomic keys [11]. The number of Culex mosquitoes was counted by experts at each sampling location. Since all sampling locations were randomly selected, some traps were installed very close to each other. In this case, the total number of counted mosquitoes was aggregated as one point if more than two traps were located within the same pixel (30m). The analyses considered only female mosquitoes identified as Cx. tritaeniorhynchus, Cx. quinquefasciatus, and Cx. vishnui since these are the primary vectors for JE virus transmission [32].
Environmental and socio-economic predictor variables
The survival and distribution of mosquitoes species can be significantly influenced by climate and socio-economic conditions [33,34]. For meteorological data, we collected temperature and precipitation information during the study period and its preceding month. In addition, the other predictor variables (e.g., normalized difference vegetation index [NDVI], land use/land cover and human population density), were collected for our analysis. The NDVI represents vegetation health and its value ranges from -1 to +1, a higher NDVI value means denser and healthier vegetation and vice versa [35]. All the collected data was pre-processed with the same study extent, resampled to the same spatial resolution of Landsat 8 (30m pixel size), and then converted to UTM zone 48N.
Specifically, we used eight-day average MODIS land surface temperature data from NASA’s Land Processes Distributed Active Archive Center (https://lpdaac.usgs.gov/), and precipitation data from the Climate Hazards Center (https://chc.ucsb.edu/data/chirps). Data included mean temperature (September and October), previous-month temperature (August), mean total rainfall (September and October), and previous-month rainfall (August). The 30m land cover/land-use layer with five classes (rice, urban/built-up, water body, forest and other agricultural land) was obtained from a previous study [36]. In addition, the human population density layer for 2015 was downloaded from the NASA SEDAC at the Center for International Earth Science Information Network while the mean NDVI was calculated from Landsat 8 (red and near-infrared bands) data (https://earthexplorer.usgs.gov/) during the study period.
Previous research suggested that mosquitoes are active within hundreds of meters (e.g. 200-300m) from their nearest breeding sites [37,38]. Also, most mosquito-borne diseases were observed among people living near mosquito breeding habitats [39]. Thus, we computed the cover ratios for rice, forest, and water at 250m buffer radius for every pixel whereas meteorological, human population and NDVI layers were taken as an average. Therefore, a total of 9 potential risk factors were used for developing a model.
Data analysis
A Poisson regression model has been commonly used for countable data, which assumes the equality between the sample mean and variance [40,41]. However, our mosquito count data showed evidence of overdispersion (variance is greater than the mean). An alternative approach for over-dispersed count data is negative binomial regression (NBR) because it has an extra parameter (alpha [α]) to account for the over-dispersion [42, 43].
Given Y is the response variable (Y∈{0,1,2,3,4…}), representing the number of mosquitoes at a certain location, having x1, x2, x3, …., xi with predictor variables (e.g. environmental and socio-economic variables). The NBR distribution can be expressed as follow [44, 45]:
Model mean and variance are and , respectively, and α (α ≥ 0) is the dispersion parameter. To minimize the overfitting problem, our data was randomly split into two parts, training (80%) and testing (20%).
A shapefile is a digital vector storage format for storing geometric location and associated attribute information. We used the point vector shapefile (https://www.diva-gis.org/gdata) with mosquito count data in order to extract environmental and socio-economic values from associated raster layers using raster package in R [46]. We used “glmmTMB” package in R to evaluate the association between mosquito abundance and environmental predictor variables. The glmmTMB package is used to fit generalized linear mixed models with various extensions for random effects and non-normal data such as negative binomial regression as described by Magnusson et al [47]. For variable screening, all predictor variables were examined for their collinearity using Pearson’s correlation test and any variables with a Pearson’s coefficient <0.7 were considered in the models. If two or more variables were strongly correlated, we considered their biological relevance with mosquitoes. In addition, the effects of linearity between potential predictor variables and mosquito abundance were explored using loess smoothed curves. If any nonlinearity was observed, a quadratic function of the predictor variable was explored and retained if p-value <0.05.
Because of nonlinearity between mosquito abundance and total mean rainfall, we created two new variables (1. centered variable, 2. quadratic term variable) from the current month rainfall (September-October). The centered variable was computed by subtracting the rainfall mean across mosquito sampling locations while the quadratic term variable was the square of the centered variable. In addition, a random effect for sampling locations (rural/peri-urban and urban) was included to take into account the variability among trapping locations. Variables with p-value < 0.05 were considered in the final model. The incidence rate ratio (IRR) was calculated for the final NBR model.
The performance of the final fitted model was assessed using root mean square error (RMSE) and mean absolute error (MAE). The RMSE is the square root of the average of squared differences between predicted values and observed values while the MAE is the average of absolute differences between predicted values and observed values [48,49]. Finally, three additional raster layers (centered, quadratic term and random effect layers) were created and stacked with other relevant layers, and then the abundance of mosquitoes was estimated with stacked layers from the final model. All data analysis was conducted in R version 4.0.1 while risk maps were created through QGIS version 3.16.
Results
Mosquito descriptive statistics
A total of 10,775 female adult Culex mosquitoes were collected from 513 trapping locations. The most dominant Culex mosquitoes were Cx. tritaeniorhynchus (80%), followed by Cx. quinquefasciatus (10.39%) and Cx. vishnui (9.61%). Also, our mosquito data showed that nearly 97% of the samples had less than 150 cumulative counts per location during the study period whereas approximately 2% of trapping locations had a cumulative count of more than 200 mosquitoes (Fig 2, left).
Fig 2. Distribution and mosquito sampling count from six districts in Hanoi.
A total of 6,361 mosquitoes were obtained in Ha Dong suburb district, accounting for 59% of the total while Ba Dinh (urbanized district) generated 44 collected mosquitoes (0.4%) (Fig 2, right). Overall, the rural/ peri-urban districts had a much higher number of mosquitoes than densely urban areas.
Final NBR models and estimated spatial distribution of Culex abundance
Overall, the NDVI value and temperature (lag1) had a strong correlation with bi-monthly temperature whereas other remaining variables were less correlated (Table 1). The final model selected for estimating the Culex mosquito abundance included centered rainfall, quadratic term rainfall, rice cover ratio, forest cover ratio, and human population density variables. The NBR model showed that there was an increase in the mosquito abundance as total monthly rainfall rose to its mean value (220mm), but it dropped gradually as the precipitation increased beyond its mean value (Table 2). In addition, a percentage increase in rice cover ratio corresponded to an increase in the mosquito abundance by 3.78 times. In contrast, a 1% increase in forest cover ratio corresponded to a reduction in the mosquito abundance by 97.5%. Similarly, a unit increase in human population density (per km2) had resulted in 1.1% reduction of the mosquito population. Our final model showed that the RMSE and MAE were 24.15 and 16.83, respectively.
Table 1. Pearson’s correlation coefficient (r) among predictor variables.
| Variables | Forest cover ratio (%) | Rice cover ratio (%) | Water cover ratio (%) | Temperature (lag1, oC) | Bi-monthly temperature (oC) | Rainfall (lag1, mm) | Bi-monthly rainfall (mm) | NDVI | Human population density (per km2) |
|---|---|---|---|---|---|---|---|---|---|
| Forest cover ratio | 1 | ||||||||
| Rice cover ratio | 0.24 | 1 | |||||||
| Water cover ratio | -0.13 | 0.10 | 1 | ||||||
| Temperature | -0.23 | -0.51 | -0.14 | 1 | |||||
| Bi-monthly temperature | -0.29 | -0.38 | -0.16 | 0.84 | 1 | ||||
| Rainfall | 0.07 | 0.24 | -0.03 | -0.25 | -0.14 | 1 | |||
| Bi-monthly rainfall | -0.18 | 0.01 | -0.23 | 0.30 | 0.57 | 0.14 | 1 | ||
| NDVI | 0.27 | 0.47 | -0.03 | -0.7 | -0.48 | 0.37 | -0.05 | 1 | |
| Human population density | -0.21 | -0.46 | -0.06 | 0.62 | 0.35 | -0.52 | -0.06 | -0.56 | 1 |
Lag1 = preceding month; bi-monthly = during study period
Table 2. Final NBR model with accuracy and associated risk factors of Culex mosquito abundance in Hanoi.
| Variables | Adjusted IRRs | 95% CI | P-value | RMSE | MAE |
|---|---|---|---|---|---|
| Bi-monthly total mean rainfall (mm, centering variable) | 1.0492 | 1.021–1.077 | <0.0004 | ||
| Bi-monthly total mean rainfall (mm, quadratic term) | 1.001 | 1.000–1.002 | 0.0475 | ||
| Rice cover ratio (%) | 3.778 | 1.549–9.204 | 0.0034 | ||
| Forest cover ratio (%) | 0.0249 | 0.003–0.105 | <0.0001 | ||
| Human population density (person per km2) | 0.989 | 0.986–0.991 | <0.0001 | ||
| Accuracy | 24.15 | 16.83 |
CI = confidence interval; IRR = incidence rate ratio; NBR = negative binomial regression; Bi-monthly = study period (Sep-Oct)
The estimated spatial distribution of Culex mosquito abundance ranged from 0 to 150, and the colors ranged from purple-blue for areas with low to orange-red berry for areas with high abundance of the mosquitoes (Fig 3).
Fig 3. Estimated map of the Culex mosquito abundance in Hanoi (source of shapefile: https://www.diva-gis.org/gdata).
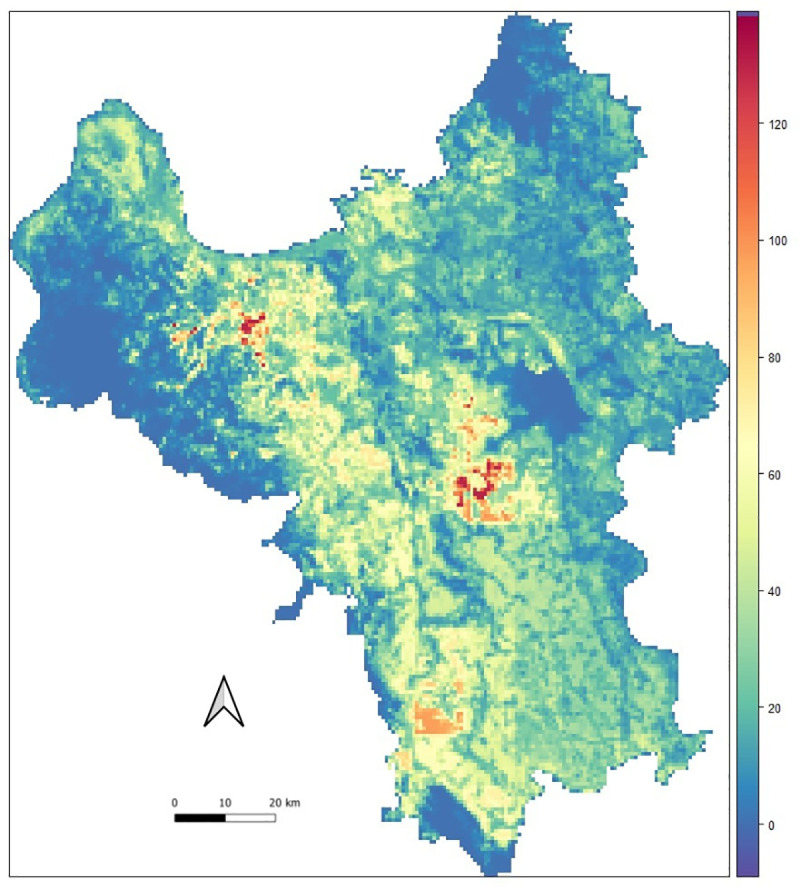
The abundance of Culex species was mainly observed in rural and agriculture areas, whereas the central districts of Hanoi and forest areas showed the lowest abundance. Noticeably, some areas in the northwest region had the highest mosquito abundance. Our model estimated that 87% of the Hanoi area had an abundance of mosquitoes from 0 to 50, whereas approximately 1.2% of the area showed more than 100 mosquitoes, which was mostly in the rural/peri-urban districts.
Discussion
This study was the first evaluation of the spatial abundance of Culex mosquitoes using remote sensing data in Hanoi, Vietnam. We found that the rice paddy cover was positively associated with the spatial distribution of mosquito abundance, which was similar to findings from previous studies, suggesting that the rice crop ecosystem is the most important breeding habitat for the Culex mosquitoes, and expanding rice cultivation is positively associated with JE virus. [12,13,50]. These results are similar to those of an earlier study that observed Culex mosquitoes in the rice fields and stagnant water habitats in northern Vietnam [12]. In addition, rainfall was identified as the main driver of Culex mosquito abundance in areas with rainfall level below 220mm, then gradually decreased at rainfall level higher than 220mm annually. A Chinese study found that a precipitation between 80mm and 120mm was suitable for mosquito growing and breeding. Other studies have suggested that locations with higher precipitation were more suitable for mosquitoes with JE virus, but excessive rainfall such as typhoons could wash away mosquitos’ habitats and larvae [51,52].
However, this study found that high forest cover had a negative association with mosquito abundance. One study, in Thailand, suggested that mosquitoes were least likely to survive in dense forests because of unfavorable environmental conditions (e.g. low temperature) [53]. Similarly, other studies found that a forest with bushy vegetation was likely to block the sunshine which reduced the temperature of small water bodies, thereby preventing larval growth [54,55]. Our study also exhibited that mosquito abundance decreased as human population density increased which was consistent with previous studies [56,57]. These studies indicated that the reduction of mosquitoes in more densely populated areas was due to regular mosquito control programs, improved urban planning, and better sanitation.
The estimated map of Culex mosquitoes demonstrated the higher risks associated with the rice ecosystems and rural areas that were observed in some rice growing areas of My Duc, Phuc Tho and Ha Dong districts (in strong red color areas in Fig 3). For rural areas, it is likely that poor environmental sanitation facilitates the mosquitoes’ breeding habitats whereas people in urban areas are more aware of JE virus and other vector-borne diseases. For instance, one study in Pakistan showed that 65% of urban households implemented mosquito control measures, while only 39% of rural households did it [58]. However, previous studies in the Hanoi Province have had mixed findings. Jakobsen et al suggested that peri-urban households in Hanoi had better mosquito control knowledge and practices compared to households in more central districts [59]. Other studies have suggested that regular indoor spraying and removing water containers close to the house could contribute to a reduction of mosquitoes and vector-borne diseases [60,61].
Over the past two decades, remote sensing has increasingly involved in mapping mosquito-borne risks and species distribution. Michael et al highlighted that increasingly available earth observation data play a crucial role in the control of vector-borne diseases [62]. In addition, Anna et al indicated that remote sensing-based variables were likely to reduce the over-fitting problems in ecological statistical models [63]. Several global and regional mappings of mosquito-borne diseases and species distribution took advantage of this unique data nature and provided useful information [34,64,65]. Such data visualization would be very important to clinicians to target vulnerable areas and early intervention programs are timely undertaken for those areas.
Although coarse spatial resolution data has been frequently used in geospatial public health, it is less likely to take into consideration local variations or micro-habitats because of large pixel size [24–26]. For example, an earlier Asian JE and Culex mosquito risk map showed the spatial patterns of mosquitoes and vector-borne diseases but it did not identify the accurate locations where mosquito-borne diseases occur (e.g. at village level) [26]. This limitation was improved in our study by constructing 30 x30m pixel size raster layer and computing variations among local pixels (e.g. using a 250m buffer) as this better resolution can reflect local variations and consequently increase the accuracy of mosquito risk maps [66].
Our study was not able to identify the geographic association between JE reported cases and Culex mosquitoes because JE data was unavailable. However, several studies showed that Culex mosquito abundance was geographically associated with JE, and West Nile viruses [25,26,67]. In Vietnam, Culex mosquitoes are the primary vector for JE virus across the country [14,28]. From a public health point of view, risk maps can be useful to increase the public awareness in areas with high-risk of Culex mosquitoes. This early warning information can alert people to take precautions such as wearing long-sleeved shirts, trousers, and hats when engaged in outdoor activities or travelling to hotspots. Culex mosquitoes lay their eggs in standing water, such as is found in rice fields and septic tanks, but can also breed in smaller water bodies. Our risk map identified some high-risk areas with more than 130 mosquitoes/ 900m2 in the rice fields and rural areas where further preventive control measures need to be considered (e.g. use of insecticides and proper sanitation).
This study had several limitations. First, the mosquito sampling was conducted in six out of 30 districts for a limited time, so our samples may not be representative across the entire year and/or seasons. However, our study was more robust than other similar studies in Egypt, Italy, and the United States that employed one-period sampling of mosquitoes, in terms of large mosquito sampling points collected and/or higher spatial resolution [68–71]. In addition, we may have overestimated the mosquito population in this study because samples were collected during the wet season (May–October), not the dry season (November–April). One study suggested that Culex mosquitoes were more predominant (43%) during the rainy season than the dry season in Hanoi [12]. We assumed that more mosquitoes have a higher chance of being infected with JE virus. However, we did not know the proportion of mosquitoes with JE virus as laboratory confirmation was not conducted. Furthermore, livestock are commonly raised in many rural/peri-urban districts of Hanoi, but this raster layer was not available for our study. Previous research suggested that livestock production was associated with the mosquito abundance and JE virus [72,73]. Animal waste and nearby ponds can provide favorable mosquito-breeding areas if the livestock and their barns were not regularly washed and cleaned [74,75]. Lastly, the human population density used in this study was from 2015, which was assumed to be constant for 2018, but it was unlikely to be accurate because of rapid urbanization in Hanoi.
Our findings may provide better insight into understanding the spatial distribution of Culex mosquitoes and its associated environmental risk factors. Such information can assist local clinicians and public health policymakers to identify the potential areas of risk for JE virus. Risk maps can be an efficient way of raising public awareness about the virus and further preventive measures need to be considered in order to prevent outbreaks and onwards transmission of the JE virus.
Acknowledgments
We also would like to give special thanks to Paul Karaimu for English editing.
Data Availability
The data is available at https://github.com/tuyenhavan/Mosquito_ILRI.
Funding Statement
This study was supported by the Southeast Asia One Health University Network (SEAOHUN); and the United States Agency for International Development (USAID). In addition, this study was also supported by the CGIAR Research Program on Agriculture for Nutrition and Health (A4NH), which is led by the International Food Policy Research Institute (IFPRI); and the “Metropolitan Mosquitoes Project,” which is funded by the Swedish Research Council for Environment, Agricultural Sciences and Spatial Planning (Formas, grant number 2016-00364). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Solomon T. Control of Japanese encephalitis—within our grasp? New England Journal of Medicine. 2006;355(9):869–71. doi: 10.1056/NEJMp058263 [DOI] [PubMed] [Google Scholar]
- 2.Japanese encephalitis [Internet]. WHO. 2019 [cited 15/12/2020].
- 3.Heinz F, Stiasny K. Flaviviruses and their antigenic structure. Journal of Clinical Virology. 2012;55(4):289–95. doi: 10.1016/j.jcv.2012.08.024 [DOI] [PubMed] [Google Scholar]
- 4.Campbell GL, Hills SL, Fischer M, Jacobson JA, Hoke CH, Hombach JM, et al. Estimated global incidence of Japanese encephalitis: a systematic review. Bulletin of the World Health Organization. 2011;89:766–74. doi: 10.2471/BLT.10.085233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erlanger TE, Weiss S, Keiser J, Utzinger J, Wiedenmayer K. Past, present, and future of Japanese encephalitis. Emerging infectious diseases. 2009;15(1):1. doi: 10.3201/eid1501.080311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Japanese encephalitis [Internet]. 2019 [cited 10/12/2020]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/japanese-encephalitis.
- 7.Okuno T. An epidemiological review of Japanese encephalitis. World health statistics quarterly Rapport trimestriel de statistiques sanitaires mondiales. 1978;31(2):120–33. [PubMed] [Google Scholar]
- 8.Yen NT, Duffy MR, Hong NM, Hien NT, Fischer M, Hills SL. Surveillance for Japanese encephalitis in Vietnam, 1998–2007. The American journal of tropical medicine and hygiene. 2010;83(4):816–9. doi: 10.4269/ajtmh.2010.10-0262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Solomon T, Dung NM, Kneen R, Thao LTT, Gainsborough M, Nisalak A, et al. Seizures and raised intracranial pressure in Vietnamese patients with Japanese encephalitis. Brain. 2002;125(5):1084–93. doi: 10.1093/brain/awf116 [DOI] [PubMed] [Google Scholar]
- 10.Tan LV, Thai LH, Phu NH, Nghia HDT, Chuong LV, Sinh DX, et al. Viral aetiology of central nervous system infections in adults admitted to a tertiary referral hospital in southern Vietnam over 12 years. PLoS neglected tropical diseases. 2014;8(8):e3127. doi: 10.1371/journal.pntd.0003127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reuben R, Tewari S, Hiriyan J, Akiyama J. Illustrated keys to species of Culex (Culex) associated with Japanese encephalitis in Southeast Asia (Diptera: Culicidae). Mosquito systematics. 1994;26(2):75–96. [Google Scholar]
- 12.Ohba S-y, Van Soai N, Van Anh DT, Nguyen YT, Takagi M. Study of mosquito fauna in rice ecosystems around Hanoi, Northern Vietnam. Acta tropica. 2015;142:89–95. doi: 10.1016/j.actatropica.2014.11.002 [DOI] [PubMed] [Google Scholar]
- 13.Keiser J, Maltese MF, Erlanger TE, Bos R, Tanner M, Singer BH, et al. Effect of irrigated rice agriculture on Japanese encephalitis, including challenges and opportunities for integrated vector management. Acta tropica. 2005;95(1):40–57. doi: 10.1016/j.actatropica.2005.04.012 [DOI] [PubMed] [Google Scholar]
- 14.Kuwata R, Nga PT, Yen NT, Hoshino K, Isawa H, Higa Y, et al. Surveillance of Japanese encephalitis virus infection in mosquitoes in Vietnam from 2006 to 2008. The American journal of tropical medicine and hygiene. 2013;88(4):681–8. doi: 10.4269/ajtmh.12-0407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mackenzie J, Barrett AD, Deubel V. Japanese encephalitis and West Nile viruses: Springer Science & Business Media; 2012. [Google Scholar]
- 16.Ruget AS, Beck C, Gabassi A, Trévennec K, Lecollinet S, Chevalier V, et al. Japanese encephalitis circulation pattern in swine of northern Vietnam and consequences for swine’s vaccination recommendations. Transboundary and emerging diseases. 2018;65(6):1485–92. doi: 10.1111/tbed.12885 [DOI] [PubMed] [Google Scholar]
- 17.Kalluri S, Gilruth P, Rogers D, Szczur M. Surveillance of arthropod vector-borne infectious diseases using remote sensing techniques: a review. PLoS Pathog. 2007;3(10):e116. doi: 10.1371/journal.ppat.0030116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palaniyandi M. The role of Remote Sensing and GIS for spatial prediction of vector-borne diseases transmission: A systematic review. Journal of vector borne diseases. 2012;49(4):197. [PubMed] [Google Scholar]
- 19.Yang G-J, Vounatsou P, Xiao-Nong Z, Utzinger J, Tanner M. A review of geographic information system and remote sensing with applications to the epidemiology and control of schistosomiasis in China. Acta tropica. 2005;96(2–3):117–29. doi: 10.1016/j.actatropica.2005.07.006 [DOI] [PubMed] [Google Scholar]
- 20.Elith J, Leathwick JR. Species distribution models: ecological explanation and prediction across space and time. Annual review of ecology, evolution, and systematics. 2009;40:677–97. [Google Scholar]
- 21.Dale P, Morris C. Culex annulirostris breeding sites in urban areas: using remote sensing and digital image analysis to develop a rapid predictor of potential breeding areas. Journal of the American Mosquito Control Association. 1996;12(2 Pt 1):316–20. [PubMed] [Google Scholar]
- 22.Zou L, Miller SN, Schmidtmann ET. Mosquito larval habitat mapping using remote sensing and GIS: implications of coalbed methane development and West Nile virus. Journal of medical entomology. 2006;43(5):1034–41. doi: 10.1603/0022-2585(2006)43[1034:mlhmur]2.0.co;2 [DOI] [PubMed] [Google Scholar]
- 23.Jacob BG, Gu W, Caamano EX, Novak RJ. Developing operational algorithms using linear and non-linear squares estimation in Python® for the identification of Culex pipiens and Culex restuans in a mosquito abatement district (Cook County, Illinois, USA). Geospatial Health. 2009;3(2):157–76. doi: 10.4081/gh.2009.218 [DOI] [PubMed] [Google Scholar]
- 24.Alaniz AJ, Carvajal MA, Bacigalupo A, Cattan PE. Global spatial assessment of Aedes aegypti and Culex quinquefasciatus: a scenario of Zika virus exposure. Epidemiology & Infection. 2019;147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Samy AM, Elaagip AH, Kenawy MA, Ayres CF, Peterson AT, Soliman DE. Climate change influences on the global potential distribution of the mosquito Culex quinquefasciatus, vector of West Nile virus and lymphatic filariasis. PloS one. 2016;11(10):e0163863. doi: 10.1371/journal.pone.0163863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Longbottom J, Browne AJ, Pigott DM, Sinka ME, Golding N, Hay SI, et al. Mapping the spatial distribution of the Japanese encephalitis vector, Culex tritaeniorhynchus Giles, 1901 (Diptera: Culicidae) within areas of Japanese encephalitis risk. Parasites & vectors. 2017;10(1):1–12. doi: 10.1186/s13071-017-2086-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lowry PW, Truong DH, Hinh LD, Ladinsky JL, Karabatsos N, Cropp CB, et al. Japanese encephalitis among hospitalized pediatric and adult patients with acute encephalitis syndrome in Hanoi, Vietnam 1995. The American journal of tropical medicine and hygiene. 1998;58(3):324–9. doi: 10.4269/ajtmh.1998.58.324 [DOI] [PubMed] [Google Scholar]
- 28.Lindahl JF, Ståhl K, Chirico J, Boqvist S, Thu HTV, Magnusson U. Circulation of Japanese encephalitis virus in pigs and mosquito vectors within Can Tho city, Vietnam. PLoS Negl Trop Dis. 2013;7(4):e2153. doi: 10.1371/journal.pntd.0002153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pham VC, Pham T-T-H, Tong THA, Nguyen TTH, Pham NH. The conversion of agricultural land in the peri-urban areas of Hanoi (Vietnam): patterns in space and time. Journal of Land Use Science. 2015;10(2):224–42. [Google Scholar]
- 30.Statistical Yearbook 2018 [Internet]. 2018 [cited 05/10/2020]. Available from: https://www.gso.gov.vn/.
- 31.Victor TJ, Reuben R. Population dynamics of mosquito immatures and the succession in abundance of aquatic insects in rice fields in Madurai, South India. Indian journal of malariology. 1999;36(1–2):19–32. [PubMed] [Google Scholar]
- 32.Mackenzie JS, Gubler DJ, Petersen LR. Emerging flaviviruses: the spread and resurgence of Japanese encephalitis, West Nile and dengue viruses. Nature medicine. 2004;10(12):S98–S109. doi: 10.1038/nm1144 [DOI] [PubMed] [Google Scholar]
- 33.Afrane YA, Githeko AK, Yan G. The ecology of Anopheles mosquitoes under climate change: Case studies from the effects of environmental changes in east Africa highlands. Annals of the New York Academy of Sciences. 2012;1249:204. doi: 10.1111/j.1749-6632.2011.06432.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zheng X, Zhong D, He Y, Zhou G. Seasonality modeling of the distribution of Aedes albopictus in China based on climatic and environmental suitability. Infectious diseases of poverty. 2019;8(1):1–9. doi: 10.1186/s40249-018-0513-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hashim H, Abd Latif Z, Adnan NA. Urban vegetation classification with NDVI thresold value method with very high resolution (VHR) PLEIADES Imagery. Int Arch Photogramm Remote Sens Spat Inf Sci. 2019:237–40. [Google Scholar]
- 36.Huy Van Nguyen. A Comparison of Advanced Classification Methods for Land Use/Land Cover Changes Investigation in Hanoi, Vietnam [Thesis]: Stuttgart University of Applied Sciences; 2019.
- 37.Thomas CJ, Cross DE, Bøgh C. Landscape movements of Anopheles gambiae malaria vector mosquitoes in rural Gambia. PloS one. 2013;8(7):e68679. doi: 10.1371/journal.pone.0068679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Medeiros MC, Boothe EC, Roark EB, Hamer GL. Dispersal of male and female Culex quinquefasciatus and Aedes albopictus mosquitoes using stable isotope enrichment. PLoS neglected tropical diseases. 2017;11(1):e0005347. doi: 10.1371/journal.pntd.0005347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jardine A, Neville PJ, Lindsay MD. Proximity to mosquito breeding habitat and Ross River virus risk in the Peel region of Western Australia. Vector-Borne and Zoonotic Diseases. 2015;15(2):141–6. doi: 10.1089/vbz.2014.1693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee HS, Nguyen-Viet H, Lee M, Duc PP, Grace D. Seasonality of viral encephalitis and associated environmental risk factors in son La and Thai Binh provinces in Vietnam from 2004 to 2013. The American journal of tropical medicine and hygiene. 2017;96(1):110–7. doi: 10.4269/ajtmh.16-0471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mouatassim Y, Ezzahid EH. Poisson regression and Zero-inflated Poisson regression: application to private health insurance data. European actuarial journal. 2012;2(2):187–204. [Google Scholar]
- 42.Lindén A, Mäntyniemi S. Using the negative binomial distribution to model overdispersion in ecological count data. Ecology. 2011;92(7):1414–21. doi: 10.1890/10-1831.1 [DOI] [PubMed] [Google Scholar]
- 43.Gardner W, Mulvey EP, Shaw EC. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychological bulletin. 1995;118(3):392. doi: 10.1037/0033-2909.118.3.392 [DOI] [PubMed] [Google Scholar]
- 44.McCulloch CE, Neuhaus JM. Generalized linear mixed models. Wiley StatsRef: Statistics Reference Online. 2014. [Google Scholar]
- 45.Myers RH, Montgomery DC, Vining GG, Robinson TJ. Generalized linear models: with applications in engineering and the sciences: John Wiley & Sons; 2012. [Google Scholar]
- 46.Hijmans RJ, Van Etten J, Cheng J, Mattiuzzi M, Sumner M, Greenberg JA, et al. Package ‘raster’. R package. 2015;734. [Google Scholar]
- 47.Magnusson A, Skaug H, Nielsen A, Berg C, Kristensen K, Maechler M, et al. Package ‘glmmTMB’. R Package Version 02 0. 2017. [Google Scholar]
- 48.Wang W, Lu Y, editors. Analysis of the mean absolute error (MAE) and the root mean square error (RMSE) in assessing rounding model. IOP Conference Series: Materials Science and Engineering; 2018.
- 49.Chai T, Draxler RR. Root mean square error (RMSE) or mean absolute error (MAE)? GMDD. 2014;7(1):1525–34. [Google Scholar]
- 50.Phukan A, Borah P, Mahanta J. Japanese encephalitis in Assam, northeast India. Southeast Asian journal of tropical medicine and public health. 2004;35:618–22. [PubMed] [Google Scholar]
- 51.Wang L, Hu W, Magalhaes RJS, Bi P, Ding F, Sun H, et al. The role of environmental factors in the spatial distribution of Japanese encephalitis in mainland China. Environment international. 2014;73:1–9. doi: 10.1016/j.envint.2014.07.004 [DOI] [PubMed] [Google Scholar]
- 52.Gubler DJ, Reiter P, Ebi KL, Yap W, Nasci R, Patz JA. Climate variability and change in the United States: potential impacts on vector-and rodent-borne diseases. Environmental health perspectives. 2001;109(suppl 2):223–33. doi: 10.1289/ehp.109-1240669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thongsripong P, Green A, Kittayapong P, Kapan D, Wilcox B, Bennett S. Mosquito vector diversity across habitats in central Thailand endemic for dengue and other arthropod-borne diseases. PLoS Negl Trop Dis. 2013;7(10):e2507. doi: 10.1371/journal.pntd.0002507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jacob BG, Muturi EJ, Mwangangi JM, Funes J, Caamano EX, Muriu S, et al. Remote and field level quantification of vegetation covariates for malaria mapping in three rice agro-village complexes in Central Kenya. International Journal of Health Geographics. 2007;6(1):21. doi: 10.1186/1476-072X-6-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sunish I, Reuben R. Factors influencing the abundance of Japanese encephalitis vectors in ricefields in India–I. Abiotic. Medical and veterinary entomology. 2001;15(4):381–92. doi: 10.1046/j.0269-283x.2001.00324.x [DOI] [PubMed] [Google Scholar]
- 56.Lindsay SW, Wilson A, Golding N, Scott TW, Takken W. Improving the built environment in urban areas to control Aedes aegypti-borne diseases. Bulletin of the world health organization. 2017;95(8):607. doi: 10.2471/BLT.16.189688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ferraguti M, Martínez-de La Puente J, Roiz D, Ruiz S, Soriguer R, Figuerola J. Effects of landscape anthropization on mosquito community composition and abundance. Scientific reports. 2016;6(1):1–9. doi: 10.1038/s41598-016-0001-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hafeez F, Akram W, Suhail A, Arshad M. Knowledge and attitude of the public towards dengue control in urban and rural areas of Punjab. Pakistan Journal of Zoology. 2012;44(1). [Google Scholar]
- 59.Jakobsen F, Nguyen-Tien T, Pham-Thanh L, Bui VN, Nguyen-Viet H, Tran-Hai S, et al. Urban livestock-keeping and dengue in urban and peri-urban Hanoi, Vietnam. PLoS neglected tropical diseases. 2019;13(11):e0007774. doi: 10.1371/journal.pntd.0007774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mani T, Arunachalam N, Rajendran R, Satyanarayana K, Dash A. Efficacy of thermal fog application of deltacide, a synergized mixture of pyrethroids, against Aedes aegypti, the vector of dengue. Tropical Medicine & International Health. 2005;10(12):1298–304. doi: 10.1111/j.1365-3156.2005.01522.x [DOI] [PubMed] [Google Scholar]
- 61.Perich MJ, Rocha N, Castro A, Alfaro A, Platt K, Solano T, et al. Evaluation of the efficacy of lambda-cyhalothrin applied by three spray application methods for emergency control of Aedes aegypti in Costa Rica. Journal of the American Mosquito Control Association. 2003;19(1):58–62. [PubMed] [Google Scholar]
- 62.Wimberly MC, de Beurs KM, Loboda TV, Pan WK. Satellite Observations and Malaria: New Opportunities for Research and Applications. Trends in parasitology. 2021. doi: 10.1016/j.pt.2021.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cord AF, Klein D, Gernandt DS, de la Rosa JAP, Dech S. Remote sensing data can improve predictions of species richness by stacked species distribution models: a case study for Mexican pines. Journal of Biogeography. 2014;41(4):736–48. [Google Scholar]
- 64.Messina JP, Brady OJ, Golding N, Kraemer MU, Wint GW, Ray SE, et al. The current and future global distribution and population at risk of dengue. Nature microbiology. 2019;4(9):1508–15. doi: 10.1038/s41564-019-0476-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rogers D, Wilson A, Hay S, Graham A. The global distribution of yellow fever and dengue. Advances in parasitology. 2006;62:181–220. doi: 10.1016/S0065-308X(05)62006-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bøgh C, Lindsay SW, Clarke SE, Dean A, Jawara M, Pinder M, et al. High spatial resolution mapping of malaria transmission risk in the Gambia, west Africa, using LANDSAT TM satellite imagery. The American journal of tropical medicine and hygiene. 2007;76(5):875–81. [PubMed] [Google Scholar]
- 67.Liu B, Gao X, Ma J, Jiao Z, Xiao J, Wang H. Influence of host and environmental factors on the distribution of the Japanese Encephalitis vector Culex tritaeniorhynchus in China. International journal of environmental research and public health. 2018;15(9):1848. doi: 10.3390/ijerph15091848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Baldacchino F, Marcantonio M, Manica M, Marini G, Zorer R, Delucchi L, et al. Mapping of Aedes albopictus abundance at a local scale in Italy. Remote Sensing. 2017;9(7):749. [Google Scholar]
- 69.El-Zeiny A, El-Hefni A, Sowilem M. Geospatial techniques for environmental modeling of mosquito breeding habitats at Suez Canal Zone, Egypt. The Egyptian Journal of Remote Sensing and Space Science. 2017;20(2):283–93. [Google Scholar]
- 70.Cleckner HL, Allen TR, Bellows AS. Remote sensing and modeling of mosquito abundance and habitats in Coastal Virginia, USA. Remote Sensing. 2011;3(12):2663–81. [Google Scholar]
- 71.El-Hefni AM, El-Zeiny AM, Effat HA, editors. Environmental sensitivity to mosquito transmitted diseases in El-Fayoum using spatial analyses. E3S Web of Conferences; 2020: EDP Sciences. [Google Scholar]
- 72.Lee HS, Bui VN, Nguyen HX, Bui AN, Hoang TD, Nguyen-Viet H, et al. Seroprevalences of multi-pathogen and description of farm movement in pigs in two provinces in Vietnam. BMC veterinary research. 2020;16(1):15. doi: 10.1186/s12917-020-2236-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nguyen TT, Pham LT, Nguyen-Viet H, Lundkvist A, Lindahl JF. The association between livestock keeping and mosquito-borne diseases in urban areas in Hanoi city, Vietnam. 2018. [Google Scholar]
- 74.Solomon T, Dung NM, Kneen R, Gainsborough M, Vaughn DW, Khanh VT. Japanese encephalitis. Journal of Neurology, Neurosurgery & Psychiatry. 2000;68(4):405–15. doi: 10.1136/jnnp.68.4.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lawler S. Managing mosquitoes on the farm: UCANR Publications; 2005. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data is available at https://github.com/tuyenhavan/Mosquito_ILRI.



