Abstract
Introduction
Housing affects an individual’s physical and mental health, particularly among people who use substances. Understanding the association between individual characteristics and housing status can inform housing policy and help optimize the care of people who use drugs. The objective of this study was to explore the factors associated with unstable housing among people who use drugs in Ottawa.
Methods
This is a cross-sectional analysis of data from 782 participants in the Participatory Research in Ottawa: Understanding Drugs (PROUD) Study. PROUD is a prospective cohort study of people who use drugs in Ottawa. Between March and December 2013, participants were recruited through peer-based recruitment on the streets and in social services settings and completed a peer-administered questionnaire that explored socio-demographic information, drug use patterns, community integration, experiences with police and incarceration, and access to health care and harm reduction services. Eligibility criteria included age of 16 years or older, self-reported illicit drug use within the past 12 months and having lived in Ottawa for at least 3 months. Housing status was determined by self-report. “Stable housing” was defined as residence in a house or apartment and “unstable housing” was defined as all other residence types. Exploratory multivariable logistic regression analyses of the association between characteristics of people who use drugs and their housing status were conducted.
Results
Factors that were associated with unstable housing included: recent incarceration; not having a regular doctor; not having received support from a peer worker; low monthly income; income source other than public disability support payments; and younger age. Gender, language, ethnicity, education level, opioid use and injection drug use were not independently associated with housing status.
Conclusions
People who use drugs face significant barriers to stable housing. These results highlight key areas to address in order to improve housing stability among this community.
Introduction
Housing instability is associated with an increased risk of homelessness [1] and is itself known to have both a direct and indirect impact on physical and mental health [2]. Unstable housing is associated with increased use of health and social services, poorer health outcomes, and increased mortality, making it a significant public health issue [3–6]. Given the importance of housing status as a determinant of health, studies have identified predictors of unstable housing among the general population, including male gender [5], younger age [4], mental illness (depression and psychiatric hospitalization), having a lower income [6,7], having less than a high school education [6], and being unemployed [4,8]. Recent incarceration has been associated with loss of housing and greater length of time unstably housed [4,9]. A rating of “severe” on the Drug Abuse Screening Test has been associated with a higher risk of housing instability [5] and greater difficulty in obtaining stable housing [10]. Among people who use drugs, unstable housing has also been associated with higher risk drug use [11–16]. It is thus unsurprising that unstable housing has been found to increase hospitalization and health care costs among people who use drugs [17].
While the impacts of housing status on drug use and vice-versa have been studied, there is a significant gap in our knowledge of factors associated with unstable housing specifically among people who use drugs. Identifying such factors is essential to effectively target housing interventions and resources for this population. In order to better understand these issues, we studied the factors associated with unstable housing among marginalized people actively using illicit drugs in Ottawa, Ontario, Canada. Using a community-led approach, we used data from the Participatory Research in Ottawa: Understanding Drugs (PROUD) Study [18], a community-based cohort of people who use drugs in Ottawa, to examine demographic, economic and social variables impacting the lives of participants.
Methods
Study setting
Ottawa, Ontario is a city with approximately one million residents, and is the capital of Canada. Ontario has a single payer publicly funded health system with universal access for necessary physician services.
Study design
The PROUD Study is a cross-sectional cohort study examining HIV risk among people who use drugs in Ottawa, Ontario and has been described in detail elsewhere [18]. PROUD incorporates community-based participatory research principles of community engagement, trust and ownership by actively engaging a Community Advisory Committee (CAC) consisting of people with drug use experience and their allies [19–21]. The survey was created by the CAC to be relevant for the local community of marginalized people who use drugs. It includes questions in eight broad sections chosen by the CAC to describe the HIV risk environment in their community. These sections include: characteristics of drug users in Ottawa; drug use patterns; access to harm reduction services; health status and health care access; sexual activities and history; connections to community; housing and homelessness; and the influence of law enforcement. Between March and December 2013, participants were recruited through peer-based recruitment on the streets and in social services settings frequented by people who use drugs in Ottawa. Eligibility criteria included age 16 years or older, self-reported drug use within the past 12 months (not including exclusive marijuana use) and having lived in Ottawa for at least 3 months. Participants completed a one-time peer or medical student administered quantitative survey and received a cash honorarium of $20.
This study received approval from the Ottawa Health Sciences Network Research Ethics Board (OHSN-REB #20120566-01H) and the Ottawa Public Health Research Ethics Board. Consent to publish was obtained as part of informed consent. Written consent for this study was obtained prior to completion of the survey.
Outcome
Our main outcome variable, unstable housing, was based on self-reported type of residence in response to the question “where are you living right now?” Participants were asked to select from the following list: Own apartment/house, rooming house, shelter, supportive housing, recovery house/detox, friends/relatives house/place, street/homeless, hotel/motel room, other. In consultation with the CAC, we defined “stable housing” as residence in “own apartment/house” and “unstable housing” as all other residence types. This definition was chosen by the community to capture a measure of permanent housing that supports autonomy and is consistent with that used in previous Canadian studies [22].
Variables of interest
To identify factors associated with unstable housing, we considered a number of explanatory variables including self-reported sociodemographic factors: gender (male vs. female vs. other), age (<25 years, 25–34 years, 35–44 years or 45+ years), and ethnicity (Aboriginal vs. Caucasian vs. neither). Gender was identified as male, female, or "other" if the participant reported trans male, trans female, Two-Spirited, other, or no answer. Given their demographic importance, we excluded any participants with missing responses for age and gender.
Drug use variables included opioid use in the last 12 months (yes vs. no) and injection drug use in the last 12 months (yes vs. no). Opioid use was categorized as "yes" if the participant reported using any of the following when asked about each drug in turn: heroin, oxycodone, morphine, percocet, fentanyl, or hydromorphone.
Socioeconomic variables included self-reported education level (less than high school vs. high school graduate vs. some college/university vs. college/university graduate), estimated monthly income (<$499 vs. $500–999 vs. $1000–1999 vs. >$2000), and source of income (disability payments (Ontario Disability Support Program [ODSP]) vs. income assistance (Ontario Works) vs. neither).
The following variables were dichotomized as “yes” if the participant responded in the affirmative and “other” if the participant responded “no”, “no answer”, “don’t know”: spent overnight or longer in jail in the last 12 months; currently on methadone; has a regular doctor; ever received support from a peer worker. A peer worker is a non-professional worker who has lived experience with drug use and plays a supportive or navigator role in accessing health or social services. If responses were missing due to the skip pattern in the survey, these were recoded as “no”. Complete case analysis for the model was performed by removing all responses other than “yes” and “no” from dichotomous variables and the results were unchanged. Results with low cell counts are reported as a range in order to preserve the confidentiality of the participants.
Analyses
We used descriptive statistics to describe the study population and to compare those who had stable and unstable housing. We used logistic regression to examine which participant characteristics were associated with unstable housing. We explored covariates that were chosen a priori by the research team, including the CAC, because they were felt to be potential independent predictors or confounders of housing status. The relationship between the following variables was examined for the presence of collinearity by examining both the variance inflation factor and the correlation coefficient: income; income source; education; access to a regular doctor; methadone treatment. None of these variables displayed a high degree of collinearity (defined as a variance inflation factor >10 or a correlation coefficient of >0.7) and therefore all were included in the model. We report associations as odds ratios from univariable and multivariable analyses with 95% confidence intervals. We determined a priori that statistically significant proportional differences would be at the p< = 0.05 level. All analyses were conducted using SPSS version 24.
Results
There were 858 responses to the PROUD survey between March and December 2013. For this analysis, 28 survey responses were eliminated before univariable analysis was conducted: 14 as duplicates and 14 because the participant had not responded to key questions required for analysis of housing status. We also excluded 48 participants who had missing age responses, leaving 782 participants for analysis (see Fig 1). Of the remaining 782 participants, 503 (60.6%) reported unstable housing (Table 1). Participants were predominantly male (n = 618; 74.5%), the mean age was 41.8 years, 586 (70.6%) self-identified as Caucasian, 393 (47.3%) reported injecting drugs within the last 12 months, and 528 (63.6%) reported using opioids within the past 12 months.
Fig 1. STROBE diagram.
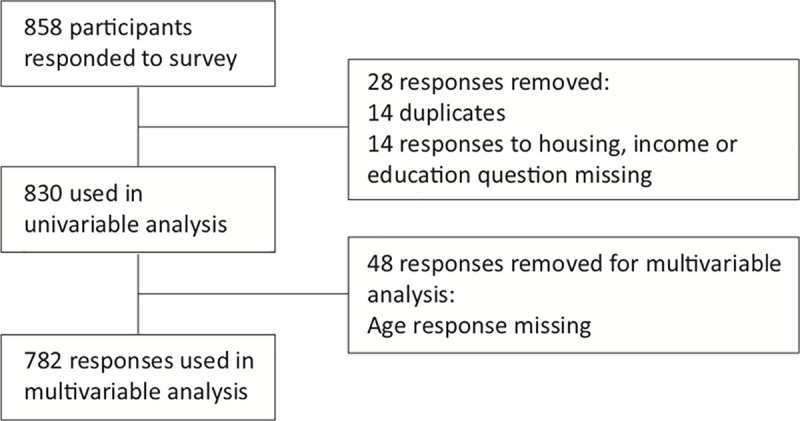
Table 1. Characteristics of participants stratified by housing status (n = 830).
| Total % (n) | Housing status | ||||
|---|---|---|---|---|---|
| Stable (n = 327) % (n) | Unstable (n = 503) % (n) | p-value | |||
| Age (years) | <25 | 6.9 (57) | 4.9 (16) | 8.2 (41) | |
| 25–34 | 18.8 (156) | 12.2 (40) | 23.1 (116) | ||
| 35–44 | 25.5 (212) | 25.1 (82) | 25.8 (130) | ||
| 45+ | 43.0 (357) | 51.4 (168) | 37.6 (189) | <0.001 | |
| Missing | 5.8(48) | 6.4 (21) | 5.4 (27) | ||
| Gender | Male | 74.5 (618) | 70.6 (231) | 76.9 (387) | 0.103 |
| Female | 20–30 (166–249) | 25–30 (82–98) | 20–25 (101–126) | ||
| Other | 0–5 (0–42) | 0–5 (0–16) | 0–5 (0–25) | ||
| First Language | English | 75.8 (629) | 78.6 (257) | 74.0 (372) | 0.299 |
| French | 16.3 (135) | 14.7 (48) | 17.3 (87) | ||
| Other | 8.0 (66) | 6.7 (22) | 8.7 (44) | ||
| Ethnicity | Aboriginal | 18.2 (151) | 18.7 (61) | 17.9 (90) | 0.327 |
| Caucasian | 70.6 (586) | 72.2 (236) | 69.6 (350) | ||
| Other | 11.2 (93) | 9.2 (30) | 12.5 (63) | ||
| Injected drugs in the last 12 months | Yes | 47.3 (393) | 51.1 (167) | 44.9 (226) | 0.083 |
| Other | 52.7 (437) | 48.9 (160) | 55.1 (277) | ||
| Opioid use in the last 12 months | Yes | 63.6 (528) | 65.7 (215) | 62.2 (313) | 0.303 |
| Other | 36.4 (302) | 34.3 (112) | 37.8 (190) | ||
| Education level | College/university graduate | 10.1 (84) | 11.0 (36) | 9.5 (48) | |
| Some college/university | 14.1 (117) | 16.2 (53) | 12.7 (64) | ||
| High school graduate | 28.2 (234) | 31.2 (102) | 26.2 (132) | ||
| Some high school or less | 47.6 (395) | 41.6 (136) | 51.5 (259) | 0.047 | |
| Monthly income | >$2000 | 13.7 (114) | 16.2 (53) | 12.1 (61) | |
| $1000–1999 | 33.0 (274) | 39.4 (129) | 28.8 (145) | ||
| $500–999 | 36.7 (305) | 36.1 (118) | 37.2 (187) | ||
| Less than $499 | 16.5 (137) | 8.3 (27) | 21.9 (110) | <0.001 | |
| Income source | ODSP | 39.2 (325) | 52.0 (170) | 30.8 (155) | <0.001 |
| Ontario Works | 37.7 (313) | 27.5 (90) | 44.3 (223) | ||
| Neither | 23.1 (192) | 20.5 (67) | 24.9 (125) | ||
| In jail in the last 12 months | Yes | 37.0 (307) | 26.6 (87) | 43.7 (220) | <0.001 |
| Other | 63.0 (523) | 73.4 (240) | 56.3 (283) | ||
| Currently on Methadone | Yes | 23.3 (193) | 30.0 (98) | 18.9 (95) | <0.001 |
| Other | 76.7 (637) | 70.0 (229) | 81.1 (408) | ||
| Has regular doctor | Yes | 55.2 (458) | 66.1 (216) | 48.1 (242) | <0.001 |
| Other | 44.8 (372) | 33.9 (111) | 51.9 (261) | ||
| Ever received support from a peer worker | Yes | 39.9 (331) | 45.0 (147) | 36.6 (184) | 0.016 |
| Other | 60.1 (499) | 55.0 (180) | 63.4 (319) | ||
The characteristics of the study sample stratified by housing status are presented in Table 1. Age differed among those with stable versus unstable housing, with more participants with unstable housing falling into younger age groups. For instance, 24.4% of individuals with unstable housing were 25–34 years old, while only 13.1% of those with stable housing fell into this age category. Unsurprisingly, a larger proportion of participants with unstable housing reported less than a high school education, an income of less than $499 per month from all sources, and income assistance among their sources of income. Among participants with unstable housing, the proportion reporting incarceration within the last 12 months was also higher than among those with stable housing. While the majority of participants overall did not report currently taking methadone, among those with unstable housing fewer reported current methadone use than among those with stable housing. More participants with unstable housing also reported not having a regular doctor.
The results of the univariable and multivariable analyses are shown in Table 2. In univariable analyses, unstable housing status was associated with younger age, monthly income below $499, not receiving disability payments, incarceration within the last 12 months, no current methadone use, not having a regular doctor, and not receiving support from a peer worker. In multivariable analyses, unstable housing remained associated with all of these variables except for no current methadone use.
Table 2. Unadjusted and adjusted analysis of characteristics associated with unstable housing, adjusted for listed characteristics (n = 782).
| Univariable analysis | Multivariable analysis | ||||
|---|---|---|---|---|---|
| Unadjusted odds ratio | p-value | Adjusted odds ratio | p-value | ||
| Age | <25 | 2.28 (1.23–4.21) | 0.009 | 1.78 (0.90–3.52) | 0.095 |
| 25–34 | 2.58 (1.70–3.90) | <0.001 | 2.21 (1.38–3.52) | 0.001 | |
| 35–44 | 1.41 (1.00–1.99) | 0.052 | 1.30 (0.88–1.90) | 0.184 | |
| 45+ | ref | ref | |||
| Gender | Male | ref | ref | ||
| Female | 0.74 (0.53–1.01) | 0.060 | 0.79 (0.54–1.15) | 0.215 | |
| Other | 0.48 (0.13–1.80) | 0.274 | 0.24 (0.05–1.16) | 0.075 | |
| First Language | English | ref | ref | ||
| French | 1.25 (0.85–1.84) | 0.254 | 1.30 (0.84–2.01) | 0.244 | |
| Other | 1.38 (0.81–2.36) | 0.237 | 1.04 (0.52–1.95) | 0.991 | |
| Ethnicity | Aboriginal | ref | ref | ||
| Caucasian | 1.01 (0.70–1.45) | 0.978 | 1.28 (0.83–1.97) | 0.272 | |
| Other | 1.42 (0.83–2.45) | 0.202 | 1.40 (0.74–2.64) | 0.302 | |
| Injected drugs in the last 12 months | Other | ref | ref | ||
| Yes | 0.78 (0.59–1.03) | 0.084 | 0.92 (0.62–1.37) | 0.692 | |
| Opioid use in the last 12 months | Other | ref | ref | ||
| Yes | 0.86 (0.64–1.15) | 0.303 | 0.93 (0.62–1.38) | 0.709 | |
| Education level | College/university graduate | ref | ref | ||
| Some college/university High school graduate | 0.91 (0.52–1.59) | 0.731 | 1.01 (0.53–1.94) | 0.977 | |
| 0.97 (0.59–1.61) | 0.907 | 0.86 (0.48–1.55) | 0.620 | ||
| Some high school or less | 1.43 (0.88–2.31) | 0.145 | 1.29 (0.73–2.26) | 0.380 | |
| Monthly income | >2000 | ref | ref | ||
| $1000–1999 | 0.98 (0.63–1.51) | 0.916 | 1.64 (0.98–2.74) | 0.060 | |
| $500–999 | 1.38 (0.89–2.13) | 0.149 | 2.04 (1.23–3.39) | 0.006 | |
| $Less than 499 | 3.54 (2.02–6.19) | <0.001 | 4.90 (2.56–9.39) | <0.001 | |
| Income source | ODSP | ref | ref | 0.043 | |
| Ontario Works (no ODSP) | 2.72 (1.96–3.77) | <0.001 | 1.53 (1.02–2.28) | 0.038 | |
| Neither | 2.05 (1.42–2.96) | <0.001 | 1.59 (1.04–2.41) | 0.031 | |
| In jail in the last 12 months | Other | ref | ref | ||
| Yes | 2.15 (1.59–2.90) | <0.001 | 2.22 (1.57–3.15) | <0.001 | |
| Currently on Methadone | Yes | ref | ref | ||
| Other | 1.84 (1.33–2.55) | <0.001 | 1.49 (1.00–2.24) | 0.053 | |
| Has regular doctor | Yes | ref | ref | ||
| Other | 2.10 (1.57–2.80) | <0.001 | 1.67 (1.20–2.34) | 0.003 | |
| Ever received support from a peer worker | Yes | ref | ref | ||
| Other | 1.42 (1.07–1.88) | 0.016 | 1.40 (1.01–1.94) | 0.041 | |
After adjustment, individuals aged 25–34 years had higher odds of reporting unstable housing compared with those 45 years and older (adjusted odds ratio [AOR] 2.21, 95% confidence interval [95%CI]: 1.38–3.52). Income showed a strong association with housing stability: Lower monthly income was associated with unstable housing (<$499: AOR 4.90, 95%CI 2.56–9.39; $500–999: AOR 2.04, 95%CI 1.23–3.39) when compared to an income of >$2000. Source of income was also associated with unstable housing, with increased odds of unstable housing among those receiving no financial support or receiving only income assistance relative to those receiving disability payments (no financial support: AOR 1.59, 95%CI 1.04–2.41; income assistance AOR 1.53, 95%CI 1.02–2.28). Other factors that remained associated with increased odds of unstable housing include incarceration within the last 12 months (AOR 2.22, 95%CI 1.57–3.15), not having a regular doctor (AOR 1.67, 95%CI 1.20–2.34), and not having received support from a peer worker (AOR 1.40, 95%CI 1.01–1.94).
Discussion
We conducted a study exploring factors associated with housing stability among people who use drugs in Ottawa. In our study, 61% of participants reported unstable housing. We found that lower age, lower income, not receiving disability support payments, recent incarceration, no access to a regular doctor, and not receiving services from a peer worker were all independently associated with unstable housing status.
Our findings on the association between having a doctor or peer worker support and housing stability suggest the importance of care models [23,24] that emphasize improved coordination and integration of medical, mental health, and substance use care for people who use drugs [25,26]. Although we did not find a significant association between current methadone use and housing stability, access to addictions treatment has been associated with stable housing in previous studies [27,28]. Within an integrated, team-based model of care, peer workers are increasingly included as part of health and social services delivery. Peer workers are thought to meet the needs of marginalized groups through shared lived-experience and strengths-focused social and practical support [29,30]. However, there is limited high quality research examining the impact of peer workers on housing stability among people who use drugs [31]. The association between peer support and housing is a novel and potentially important finding that should be further explored through longitudinal studies in order to understand the impact of including peer workers within health and social services programs, including housing services.
It is well established that drug use is prevalent among people with unstable housing [11,12] and that high intensity drug use is associated with unstable housing [5,10]. It was therefore surprising that, in our study, injection drug use and use of opioids were not associated with unstable housing. Polysubstance use is complex and it is possible that, among this cohort of marginalized people who actively use drugs, type of drug use may not be as salient a distinction as it is among a broader population of people at risk of unstable housing. While input from community members with lived experience of drug use was sought to assist in identifying the most relevant variables to include, it is possible that our data regarding type and route of drug use was insufficient to fully capture associations between overall patterns of drug use and housing status.
We also found a clear association between lower self-reported income and increasing odds of unstable housing among people who use drugs, which is consistent with the literature [6,7]. In our study each lower income category had a higher odds of unstable housing, with almost 5 times the odds among those reporting less than $499 per month. Source of income was also found to be independently associated with unstable housing. Compared to disability payments, both income assistance and other forms of reported income were associated with unstable housing. Income assistance benefits are lower and less stable than disability payments in Ontario, which could contribute to housing instability through decreased overall income [32]. These findings could inform programs aiming to address poverty and highlight the fact that people who use drugs may be a priority population for such programs.
Incarceration within the previous year more than doubled the odds of unstable housing in our study population. This is consistent with previous literature showing incarceration to be associated with loss of stable housing and greater difficulty establishing stable housing [4,9,33]. A recent study among people who use drugs and who were incarcerated also showed that certain types of housing are associated with a greater chance of resuming substance use following incarceration [34]. Previous studies using data from the PROUD cohort have also found incarceration to be associated with increased emergency department visits [35]. This speaks to the wide-reaching impact of interactions with the criminal justice system on the lives of people who use drugs. Our findings indicate that individuals who have recently been incarcerated may represent a sub-population that is particularly vulnerable to housing instability and could benefit from additional supports to mitigate some of the unintended consequences of incarceration that perpetuate cycles of marginalization.
Strengths and limitations
The strengths of this study include the community-based participatory design that engaged community members with lived drug use experience in decision-making at every step of the research process. This drew on a “Nothing about us without us” approach, anchored in the Greater Meaningful Involvement of People with HIV (GIPA-MIPA) principles [20]. This approach allowed for the collection of rich survey data on a typically hard to reach, marginalized population. It was the largest study of its kind in Ottawa at the time and one of the largest cohorts of people who use drugs nationally [18].
Our study also has several limitations. First, our street-based sampling methods recruited a non-random sample of a highly disadvantaged population. Therefore, the findings may not be generalizable to the entire population of people who use drugs. Second, the face-to-face interviews used to elicit self-reported information on stigmatized and illegal activities could have contributed to social desirability bias as well as recall bias. However, this was mitigated by the use of trained peer researchers to conduct the interviews. Third, our results could be impacted by unmeasured confounding effects, especially given the complex nature of the risk environment for people who use drugs [36].
Finally, based on community input we used a specific definition of housing stability that emphasized permanent housing and autonomy, which may not reflect other definitions, including for different jurisdictions or populations. Those types of housing that are included in our definition of unstable housing due to their temporary nature, such as supportive housing and recovery housing make up a very small portion of those who reported “unstable housing” and are therefore unlikely to influence our results. Although the CAC considered that the housing we categorized as “stable” was more likely to be permanent, our definition was based on the self-reported place of residence at a single moment in time in our study. While this definition has been used in other studies [22], it may not fully reflect the fluidity of housing situations for people who use drugs [4]. As such, our findings should be interpreted carefully in the context of our community-based definition of housing stability and data limitations.
While our results add to the body of knowledge on housing and drug use, given the cross-sectional nature of this study, we can only identify factors associated with unstable housing and cannot establish causality. Longitudinal studies in this area are needed to explore the temporal relationship between the variables that we identified and housing stability.
Conclusions
Unstable housing has a significant impact on health. While factors associated with unstable housing have been well established, few studies have examined characteristics specific to people who use drugs. Our study identifies variables associated with risk of unstable housing among a marginalized group of people who use drugs in Ottawa. The findings suggest that existing income support programs are insufficient to address pervasive precarious housing among people who use drugs, as are post-incarceration support programs. Access to a regular physician and support from a peer worker may also play a role in housing stability, which speaks to the value of integrated services targeting the health needs of this community [37,38].
Acknowledgments
We thank the PROUD Community Advisory Committee for their essential contributions in the survey design and data collection and for providing valuable insight into the interpretation of the data. We also thank all the PROUD participants.
Data Availability
The datasets used and/or analysed during the current study are available on reasonable request. We cannot make our data available for upload because it is considered to be co-owned by the community (as represented by our CAC). Please direct requests to the research ethics committee through the chair of the Ottawa Health Research Institute, Raphael Saginur, at REBAdministration@ohri.ca.
Funding Statement
This project was supported by grants from the Canadian Institutes of Health Research (https://cihr-irsc.gc.ca/e/193.html) and the Ontario HIV Treatment Network (https://www.ohtn.on.ca/). None of the funding bodies were involved in designing the study, data collection, analysis, interpretation of data, or writing the manuscript.
References
- 1.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71–7. doi: 10.1111/j.1525-1497.2005.00278.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turnbull J, Muckle W, Masters C. Homelessness and health. CMAJ. 2007. Oct;177(9):1065–6. doi: 10.1503/cmaj.071294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Culhane DP, Metraux S, Hadley T. Public service reductions associated with placement of homeless persons with severe mental illness in supportive housing. Hous Policy Debate. 2002. Jan;13(1):107–63. [Google Scholar]
- 4.Cheng T, Wood E, Feng C, Mathias S, Montaner J, Kerr T, et al. Transitions into and out of homelessness among street-involved youth in a Canadian setting. Heal Place. 2013;23:122–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.To MJ, Palepu A, Aubry T, Nisenbaum R, Gogosis E, Gadermann A, et al. Predictors of homelessness among vulnerably housed adults in 3 Canadian cities: a prospective cohort study. BMC Public Health. 2016. Dec;16(1):1041. doi: 10.1186/s12889-016-3711-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caton CL, Hasin D, Shrout PE, Opler LA, Hirshfield S, Dominguez B, et al. Risk factors for homelessness among indigent urban adults with no history of psychotic illness: a case-control study. Am J Public Health. 2000. Feb;90(2):258–63. doi: 10.2105/ajph.90.2.258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shelton KH, Taylor PJ, Bonner A, van den Bree M. Risk Factors for Homelessness: Evidence From a Population-Based Study. Psychiatr Serv. 2009. Apr;60(4):465–72. doi: 10.1176/appi.ps.60.4.465 [DOI] [PubMed] [Google Scholar]
- 8.Washington DL, Yano EM, McGuire J, Hines V, Lee M, Gelberg L. Risk Factors for Homelessness among Women Veterans. J Health Care Poor Underserved [Internet]. 2010;21(1):82–91. Available from: http://muse.jhu.edu/content/crossref/journals/journal_of_health_care_for_the_poor_and_underserved/v021/21.1.washington.html. doi: 10.1353/hpu.0.0237 [DOI] [PubMed] [Google Scholar]
- 9.Caton CLM, Dominguez B, Schanzer B, Hasin DS, Shrout PE, Felix A, et al. Risk factors for long-term homelessness: findings from a longitudinal study of first-time homeless single adults. Am J Public Health. 2005. Oct;95(10):1753–9. doi: 10.2105/AJPH.2005.063321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aubry T, Klodawsky F, Coulombe D. Comparing the Housing Trajectories of Different Classes Within a Diverse Homeless Population. Am J Community Psychol. 2012. Mar;49(1–2):142–55. doi: 10.1007/s10464-011-9444-z [DOI] [PubMed] [Google Scholar]
- 11.Feng C, DeBeck K, Kerr T, Mathias S, Montaner J, Wood E. Homelessness independently predicts injection drug use initiation among street-involved youth in a Canadian setting. J Adolesc Health. 2013. Apr;52(4):499–501. doi: 10.1016/j.jadohealth.2012.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roy É, Robert M, Fournier L, Laverdière É, Berbiche D, Boivin J-F. Predictors of residential stability among homeless young adults: a cohort study. BMC Public Health. 2015. Dec;16(1):131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salazar LF, Crosby RA, Holtgrave DR, Head S, Hadsock B, Todd J, et al. Homelessness and HIV-Associated Risk Behavior Among African American Men Who Inject Drugs and Reside in the Urban South of the United States. AIDS Behav. 2007. Nov;11(S2):70–7. doi: 10.1007/s10461-007-9239-2 [DOI] [PubMed] [Google Scholar]
- 14.Aidala A, Cross JE, Stall R, Harre D, Sumartojo E. Housing Status and HIV Risk Behaviors: Implications for Prevention and Policy. AIDS Behav. 2005. Sep;9(3):251–65. doi: 10.1007/s10461-005-9000-7 [DOI] [PubMed] [Google Scholar]
- 15.Lum PJ, Sears C, Guydish J. Injection Risk Behavior among Women Syringe Exchangers in San Francisco. Subst Use Misuse. 2005. Jan;40(11):1681–96. doi: 10.1080/10826080500222834 [DOI] [PubMed] [Google Scholar]
- 16.Corneil TA, Kuyper LM, Shoveller J., Hogg R. S., Li K., Spittal P. M., et al. Unstable Housing, Associated Risk Behaviour, and Increased Risk for hiv Infection among Injection Drug Users. Health Place. 2006;12(1):79–85. doi: 10.1016/j.healthplace.2004.10.004 [DOI] [PubMed] [Google Scholar]
- 17.Palepu A, Tyndall MW, Leon H, Muller J, O’Shaughnessy M V, Schechter MT, et al. Hospital utilization and costs in a cohort of injection drug users. CMAJ. 2001. Aug;165(4):415–20. [PMC free article] [PubMed] [Google Scholar]
- 18.Lazarus L, Shaw A, LeBlanc S, Martin A, Marshall Z, Weersink K, et al. Establishing a community-based participatory research partnership among people who use drugs in Ottawa: the PROUD cohort study. Harm Reduct J. 2014;11(26):1–8. doi: 10.1186/1477-7517-11-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Minkler M. Community-Based Research Partnerships: Challenges and Opportunities. J Urban Heal Bull New York Acad Med [Internet]. 2005. Jun 1;82(2_suppl_2):ii3–12. Available from: http://link.springer.com/10.1093/jurban/jti034. doi: 10.1093/jurban/jti034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Canadian HIV/AIDS Legal Network. Nothing About Us Without Us”. Greater Meaningful Involvement of People Who Use Illegal Drugs: A Public Health, Ethical and Human Rights Imperative. 2005; Available from: http://www.hivlegalnetwork.ca/site/wp-content/uploads/2013/04/Greater+Involvement+-+Rpt+-+Drug+Policy+-+ENG.pdf.
- 21.Wallwork E. Ethical Analysis of Research Partnerships with Communities. Kennedy Inst Ethics J [Internet]. 2008;18(1):57–85. Available from: http://muse.jhu.edu/content/crossref/journals/kennedy_institute_of_ethics_journal/v018/18.1.wallwork.html. doi: 10.1353/ken.0.0000 [DOI] [PubMed] [Google Scholar]
- 22.Palepu A, Marshall BDL, Lai C, Wood E, Kerr T. Addiction Treatment and Stable Housing among a Cohort of Injection Drug Users. Miles J, editor. PLoS One. 2010. Jul;5(7):e11697. doi: 10.1371/journal.pone.0011697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rush B, Fogg B, Nadeau L, Furlong A. On the Integration of Mental Health and Substance Use Services and Systems: Main Report. Summ report Can Exec Counc Addict [Internet]. 2008;128. Available from: https://ceca-cect.ca/pdf/Summary-reportFINAL-Dec18-08.pdf. [Google Scholar]
- 24.Korthuis PT, McCarty D, Weimer M, Bougatsos C, Blazina I, Zakher B, et al. Primary Care–Based Models for the Treatment of Opioid Use Disorder. Ann Intern Med. 2017. Feb;166(4):268. doi: 10.7326/M16-2149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Islam MM, Topp L, Day CA, Dawson A, Conigrave KM. The accessibility, acceptability, health impact and cost implications of primary healthcare outlets that target injecting drug users: A narrative synthesis of literature. International Journal of Drug Policy. 2012. p. 94–102. doi: 10.1016/j.drugpo.2011.08.005 [DOI] [PubMed] [Google Scholar]
- 26.Wilson T, Brar R, Sutherland C, Nolan S. Use of a primary care and pharmacy-based model for the delivery of injectable opioid agonist treatment for severe opioid use disorder: a case report. Can Med Assoc J. 2020. Feb;192(5):E115–7. doi: 10.1503/cmaj.190732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Royse D, Leukefeld C, Logan TK, Dennis M, Wechsberg W, Hoffman J, et al. Homelessness and Gender in Out-of-Treatment Drug Users. Am J Drug Alcohol Abuse. 2000. Jan;26(2):283–96. doi: 10.1081/ada-100100605 [DOI] [PubMed] [Google Scholar]
- 28.Appel PW, Tsemberis S, Joseph H, Stefancic A, Lambert-Wacey D. Housing First for Severely Mentally Ill Homeless Methadone Patients. J Addict Dis. 2012. Jul;31(3):270–7. doi: 10.1080/10550887.2012.694602 [DOI] [PubMed] [Google Scholar]
- 29.Watson E. The mechanisms underpinning peer support: a literature review. J Ment Heal. 2017. Dec;1–12. doi: 10.1080/09638237.2017.1417559 [DOI] [PubMed] [Google Scholar]
- 30.Treloar C, Rance J, Bath N, Everingham H, Micallef M, Day C, et al. Evaluation of two community-controlled peer support services for assessment and treatment of hepatitis C virus infection in opioid substitution treatment clinics: The ETHOS study, Australia. Int J Drug Policy. 2015. Oct;26(10):992–8. doi: 10.1016/j.drugpo.2015.01.005 [DOI] [PubMed] [Google Scholar]
- 31.Barker SL, Maguire N. Experts by Experience: Peer Support and its Use with the Homeless. Community Ment Health J. 2017;53(5):598–612. doi: 10.1007/s10597-017-0102-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Income Security Advocacy Centre. OW and ODSP Rates and the OCB 2017. Toronto, ON; 2017.
- 33.To MJ, Palepu A, Matheson FI, Ecker J, Farrell S, Hwang SW, et al. The effect of incarceration on housing stability among homeless and vulnerably housed individuals in three Canadian cities: A prospective cohort study. Can J Public Heal [Internet]. 2016. Nov 1;107(6):e550–5. Available from: http://link.springer.com/10.17269/CJPH.107.5607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chamberlain A, Nyamu S, Aminawung J, Wang EA, Shavit S, Fox AD. Illicit substance use after release from prison among formerly incarcerated primary care patients: a cross-sectional study. Addict Sci Clin Pract [Internet]. 2019. Dec 19;14(1):7. Available from: https://ascpjournal.biomedcentral.com/articles/10.1186/s13722-019-0136-6. doi: 10.1186/s13722-019-0136-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kendall C, Boucher L, Mark A, Martin A, Marshall Z, Boyd R, et al. A Cohort Study Examining Emergency Department Visits and Hospital Admissions Among People Who Use Drugs in Ottawa, Canada. Harm Reduct J. 2017;14(16):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rhodes T. Risk environments and drug harms- a social science for harm reduction approach. Int J Drug Policy. 2009;20:193–201. doi: 10.1016/j.drugpo.2008.10.003 [DOI] [PubMed] [Google Scholar]
- 37.Samet JH, Friedmann P, Saitz R. Benefits of Linking Primary Medical Care and Substance Abuse Services. Arch Intern Med. 2001. Jan;161(1):85. doi: 10.1001/archinte.161.1.85 [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. Integrated Prevention Services for HIV Infection, Viral Hepatitis, Sexually Transmitted Diseases, and Tuberculosis for Persons Who Use Drugs Illicitly: Summary Guidance from CDC and the U.S. Department of Health and Human Services Morbidity and Mortality. 2012;61(5). [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available on reasonable request. We cannot make our data available for upload because it is considered to be co-owned by the community (as represented by our CAC). Please direct requests to the research ethics committee through the chair of the Ottawa Health Research Institute, Raphael Saginur, at REBAdministration@ohri.ca.


