Abstract
Background
Treatment seeking delay is defined as the time interval between the onset of the major symptoms of tuberculosis (TB) and the first visit to the formal health care facility. The patient was said to be delayed if the patient visited the health-facility after 3 weeks onset of major symptoms. However, in low-income countries like Ethiopia, the delay in treatment-seeking among tuberculosis patients contributes to a widespread transmission and high prevalence of tuberculosis.
Methods
Studies were retrieved from PubMed, Cochrane Database, Cinahl, Scopus, Mednar, and Google Scholar by employing a combination of search terms with Boolean operators. Heterogeneity across studies was assessed using the Cochrane Q test. A funnel plot was used for visual assessment of publication bias. Subgroup analyses were performed to explore the possible causes of heterogeneity. Egger’s weighted regression test at a p-value < 0.05 was used to assess the presence of publication bias. Sensitivity analysis was performed to judge whether the pooled effect size was influenced by individual study. STATA software version 14 was used for all statistical analyses.
Result
A total of 12 studies with 5122 total sample size were included. The national pooled prevalence of treatment seeking delay was 44.29% (95% CI: 39.805, 48.771). The visual inspection of the funnel plot showed the asymmetrical distribution, and the Egger test showed insignificant (P = 0.348). Patients who did not seek formal health care providers on a first contact had about 7 times more likely to delay than patients who sought formal health care provider on a first contact (OR: 7.192 ((95% CI 5.587–9.257), P = 0.001, I2: 85%). The others independent predictors of delay were rural residence (OR: 3.459 ((95% CI 1.469–8.148), P ≤ 0.001), extra pulmonary TB (OR: 2.520 ((95% CI 1.761–3.605), 0.180), lower educational level (OR 11.720 ((95% CI 1.006–2.938), P <0.001), and distance more than 10km from health facility (OR: 1.631 ((95% CI (10.858–3.101), P = 0.001).
Conclusion
In this review, we identified a substantial treatment seeking delay among TB patients in Ethiopia. And, the independent predictors of delay were treatment sought before formal health care provider, residence of the patient, type of TB, educational level, and distance from a health facility. Thus, we recommend health extension workers, health professionals and other stakeholders to focus on patient education, and to continuously mobilize the whole communities on early treatment seeking with a special emphasis given to where treatment sought before formal health care provider, rural resident, extra pulmonary TB, and a patient living farther than 10km distance from health facility.
Background
Tuberculosis (TB) is a communicable disease that can be mainly caused Mycobacterium tuberculosis. It can also be rarely caused by Mycobacterium bovis and Mycobacterium africanum [1]. TB infected a third of the world’s population each year [2,3]. Globally, 10.4 million incident cases, of whom 6.1million notified and 1.4 million deaths were estimated to occur in 2015 [4]. Thus, the latest strategy, “End TB” has been designed in line with the sustainable development goals (SDG). The strategy aimed at reaching 90% case detection and treatment success by 2025 [5]. According to the 2020 globally milestones of the ‘End TB Strategy’, the annual reduction of TB prevalence should be by a rate of 4–5% [6,7]. However, Ethiopia is still one among the 30 high burdens TB countries and The TB case detection rate is very low compared to the World Health Organization (WHO) target of detecting all infectious TB cases [8]. A recent study conducted in Ethiopia showed that more than half of TB patients reported to have a treatment seeking delay [9].
There is no standard definition of treatment seeking delay. Different studies used different definitions of delay. Almost all studies defined “treatment seeking delay” contextually as the time interval between the onset of the major symptoms of TB to the first visit to formal health care facility [10–12]. TB transmissions occur between onset of symptoms and initiation of treatment. Hence, early case detection and timely initiation of the treatment are the basis to reverse the incidence of the disease [13,14].
Although most patients can be cured with a timely diagnosis and early treatment initiation, the delay in treatment seeking is a major concern in most low-income countries [15,16]. The main barrier is the detection of sputum smear-positive TB cases which depends on passive case findings and self-reports to the health facilities. This is highly dependent on patient inspiration, financial capability, degree of suspiciousness of health workers, and the accuracy and effectiveness of diagnostic services [15]. Similarly, a study found that more than half of the patients perceived as symptoms would disappear without treatment while more than quarter of them seek traditional treatment [15,17].
In Ethiopia, almost 50% of all suspected pulmonary tuberculosis patients had a history of treatment seeking delay [18]. Hence, the remaining half will continue to transmit TB infection in the community until detected and treated by another health care provider [19,20]. Furthermore, a single untreated case of smear positive tuberculosis can infect up to 15 individuals annually and over 20 during the natural course of disease [21].
The goal of TB control programs is to reduce transmission within the community. Achieving this goal requires a considerable time because most persons in endemic areas are already infected, constituting a pool that continuously contributes to the source of infectious cases. Delay in treatment seeking is significant not only due to disease prognosis at the individual level, but also due to transmission within the community and the reproductive rate of the TB epidemic [22].
Although Ethiopia adopted the Direct Observed Therapy (DOT) program, the disease has still become a major public health problem. On the other hand, the TB case detection rate in Ethiopia was 67.3%, which was lower than the target set by the ministry of health and WHO. Furthermore, this detection rate also highly variable across the region and the district [20].
At the beginning of Millennium Development Goal, our country aimed to reduce TB related mortality by more than 50%. In addition, in 2004, Ethiopia launched Health Extension Workers (HEWs) program with the aim of delivering health information to the community. But, the burden of the disease and poor treatment seeking behavior among TB patient is still now high. This directly affects effective TB control program in the country. There have been also conflicting findings on the prevalence and risk factors of treatment seeking delay. Hence, this review was aimed to solve these conflicting issues by generating the national pooled prevalence of treatment seeking delay and factors affecting delay among tuberculosis patients in Ethiopia.
Method
The Eligibility criteria based on the Condition, Context and Population (COCOPO) principle adapted from JBI 2017 guideline of prevalence review.
Types of population: Tuberculosis patients who reported to have a treatment seeking delay, and/or patient delay.
Context: This review considered only studies conducted in Ethiopia.
Condition: This review considered studies that measured the outcome of interest based prevalence and risk factors of treatment delay.
Inclusion criteria
All observational studies conducted on patient delay, and/or treatment seeking delays at health facilities in Ethiopia were considered. This systematic review and meta analysis included studies which measured the outcome of interest on prevalence and risk factors of patient delay, and/or treatment seeking delay. Furthermore, studies that explained a two by two table of frequency of independent variable with a dependent variable to determine factors affecting treatment seeking delay were included. In addition, the studies that used 3 weeks or 21days as a cutoff point to determine presence or absence of treatment seeking delay were included. Published and unpublished studies written in English language from January 01, 2000 to October 24, 2020 were also considered.
Exclusion criteria
Studies that used median to determine treatment seeking delay, and associated factors were excluded. On the other hand, studies that used 15 days and 30 days as a cutoff point to determine treatment seeking delay were excluded. Studies that did not explain a two by two table of frequency of independent variable with a dependent variable to determine factors affecting treatment seeking delay, studies that were not fully accessed, studies that were not conducted on human, studies that did not conduct in English language, studies that conducted before January 01, 2000 and after October 24, 2020, studies that conducted only on health systems delay or studies that did not report patient delay, and/or treatment seeking delay, study with data inconsistence whose author failed to respond after multiple request were excluded. Final exclusion was done after careful critical appraisals. The 2017 Joanna Briggs Institute (JBI) Critical Appraisal instruments for prevalence studies were used to evaluate the methodological quality of each article [23]. The used criteria include: appropriateness of sampling frame to address the target population, adequacy of sample size, detail description of the study subjects and the setting, conduction of data analysis with sufficient coverage of the identified sample, selection of participants in appropriate ways, methods used for the identification of the condition, measurement of the condition in a standard, reliable way for all participants, appropriateness of statistical analysis used, and adequacy of the response rate, and if not, how appropriately the low response rate managed. After evaluation of each study against these criteria, studies with a score of below 7 out of 9 criteria of Critical Appraisal instruments for prevalence studies were excluded. On the other hand, studies with a minimum score of 7 or above were included.
Study design and search strategy
A search beyond published literature was performed to reduce the risk of publication bias. The search was also restricted to studies published in the English language from January 01, 2000 to October 24, 2020. An initial limited search of PubMed, Cochrane Database, Cinahl, Scopus, Mednar and Google scholar were undertaken for published articles. Unpublished studies were searched from the Addis Ababa University electronic thesis and dissertation, and Jimma University open access institutional repository. These followed by analysis of the text words contained in the title and abstract, and of the index terms used to describe article. A second search using all identified keywords and index terms was then undertaken across all included databases. Thirdly, the reference list of all identified reports and articles were searched for additional studies. We performed the literature search using the medical subject headings (MeSH) and text words related. The following search key terms were used to include studies from above mentioned data base: “Tuberculosis”, “patient delay”, “treatment seeking delay”, "Time-to-Treatment", and “Ethiopia”. The Boolean operators (AND and OR) combination were used to search databases. The PubMed search terms with their Boolean operators of this review was attached as an additional file (S1 File. Search details).
Reporting
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for literature search strategy, selection of studies, data extraction, and result reporting [23] (S2 File. Prisma 2017 Checklist). The protocol was not registered in the Prospero database.
The outcome of the study
The outcomes of this review were treatment seeking delay and associated factors.
Operational definition
Treatment seeking delay
The time period from onset of TB symptoms till first presentation to a formal health care facility. The patient was said to be delayed if the patient visited a health-facility after 3 weeks or twenty one days of onset of major TB symptoms.
Onset of symptom
It is the day when the patient first becomes aware of the symptom or symptoms.
Formal-health care facility
Modern health care facility such as health posts, clinics, health centers and hospitals owned by the government or the private sector.
Studies with good methodological quality
Studies with a minimum score of 7 or above upon evaluation against Critical Appraisal instruments for prevalence studies.
Studies with poor methodological quality
Studies with a score of below 7 out of 9 criteria upon evaluation against Critical Appraisal instruments for prevalence studies.
Non-formal health care facility
It included traditional health care providers and drug retail outlets.
Pulmonary tuberculosis
It is a type of tuberculosis that exclusively affects the lung parenchyma.
Extra pulmonary tuberculosis
It is a type of tuberculosis that exclusively affects other organ rather lung parenchyma. It includes tuberculosis meningitis, abdominal tuberculosis, skeletal tuberculosis, Pott’s disease (spine TB), scrofula TB (lymphadenitis), and genitourinary (renal) tuberculosis.
Data quality control measures
Joanna Briggs Institute (JBI’s) critical appraisal checklist for prevalence studies was used to assess quality of the included studies [24]. Studies with a score of 7 or more were included. The quality of each study was evaluated independently by two authors (M. S, and T. D) (S4 File. JBI Critical Appraisal). Discrepancies were solved by discussion with third independent reviewer (NG).
Data extraction
The standardized data extraction tool of JBI MAStARI was used to extract data on Microsoft Excel 2016 spreadsheet. The name of the first author, publication year, region, sample size, frequency of delay and risk factors were extracted (Table 1). Two independent reviewers (MS and TD) extracted the data and cross-checked their consistency. We tried to contact the corresponding author(s) for further information, but we could not obtain a response from the corresponding author.
Table 1. Characteristics of the included studies on treatment seeking delay in Ethiopia, 2020.
| S.No | Author | Year | Region | Study design | Sample size | Frequency |
|---|---|---|---|---|---|---|
| 1. | Terefe G [17] | 2018 | SNNPR | cross sectional | 398 | 230 |
| 2. | Melashu B [25] | 2019 | Amhara | cross sectional | 170 | 102 |
| 3. | Tirusew M [18] | 2019 | Oromia | cross sectional | 598 | 275 |
| 4. | Abdurahman S [26] | 2018 | Amhara | cross sectional | 382 | 157 |
| 5. | Hailesillase [27] | 2019 | Tigray | cross sectional | 422 | 132 |
| 6. | Mihret A [28] | 2017 | Amhara | cross sectional | 605 | 240 |
| 7. | Kiros T [29] | 2020 | Tigray | cross sectional | 875 | 392 |
| 8. | Tatek W [30] | 2007 | Oromia | cross sectional | 198 | 73 |
| 9. | Yibeltal E [31] | 2020 | Amhara | cross sectional | 300 | 126 |
| 10. | Getinet S [32] | 2017 | Addis Ababa | cross sectional | 425 | 179 |
| 11. | Abdulbasit H [33] | 2015 | Oromia | cross sectional | 362 | 133 |
| 12. | Mohammed Abdu [14] | 2020 | Oromia | cross sectional | 387 | 211 |
Statistical analysis
Statistical analyses were done by using Stata version 14.0 (Stata Corp. LP, College Station, United States of America). The heterogeneity test was conducted by using I-Squared (I2) statistics. The value of I2 statistics ranges from 0 to 100% and the 25, 50, and 75%, which represent low, medium, and high heterogeneity across the included studies, respectively [21]. The pooled prevalence of treatment seeking delay among TB patients was carried out using a random-effects (DerSimonian and Laird) method. To reduce the potential random variations between studies; the sources of heterogeneity were analyzed using the subgroup analysis, and meta-regression. Publication bias was checked subjectively by the funnel plots. Asymmetry of funnel plot was used as an indication of publication bias [34]. Egger’s weighted regression test at a p-value < 0.05 was used to objectively assess the presence of publication bias [35]. A leave-out-one sensitivity analysis was conducted by excluding each study at a time to identify the impact of each study on the overall estimate.
Study selection
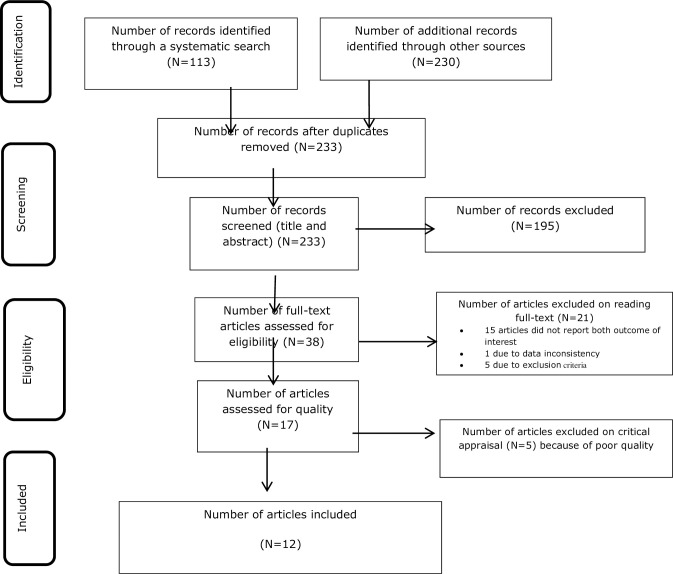
In this systematic review and meta-analysis, out of total 343 articles retrieved, 113 articles were retrieved through electronic online and 230 articles were retrieved through manual searching. Among them, 110 duplicated records were removed and 195 articles were excluded through screening the title and abstracts. Then, the remaining 38 full articles were assessed for eligibility; among them, 15 articles did not report the outcome of interest, 1 article had data inconsistency, and 5 articles had not fulfilled other eligibility criteria. As a result, 21 articles were excluded through reading full texts based on a predefined inclusion, and/or exclusion criteria. After that, a total of 17 full-texts were assessed for a critical appraisal. Five studies failed to meet the inclusion criteria; hence, excluded due to poor methodological quality. Finally, only 12 published studies met the inclusion criteria, and thereby contributed to our systematic review and meta-analysis (Fig 1).
Fig 1. PRISMA flow diagram of treatment seeking delay among TB patients in Ethiopia, 2020.
Result
Characteristics of the included studies
A total of 12 studies with 5122 patients were included in this meta analysis and systematic review. The total number of patients who delayed in seeking health care was 2250. All of the included studies were cross-sectional studies. The sample size ranged from 1700 [25] to 875 [29]. The studies were conducted between 2013 and 2020 across the country. Of these studies, 4 were from the Amhara region, 4 studies were from the Oromia region, and 2 studies were from the Tigray region, and 1 study from SNNPR (Southern Nations, Nationalities, and Peoples Region) and Addis Ababa city administration (Table 1).
Prevalence of treatment seeking delay
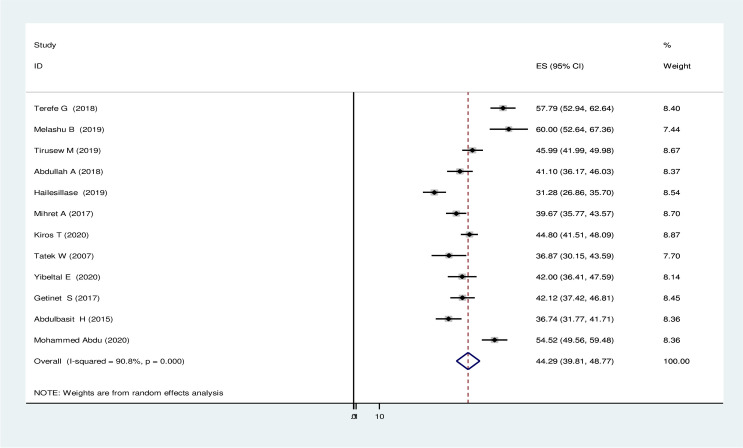
The patient was delayed if it took more than twenty one days from presentation of major TB clinical symptoms to arrival of formal health care institution. The pooled effect size of treatment seeking delay using the fixed effect model showed significant heterogeneity across the studies with (I2) of 90.8% (P ≤ 0.001). Therefore, we performed the analysis with a random-effect model with 95% CI to regulate for the observed variability. Accordingly, the national pooled prevalence of treatment seeking delay was 44.29% (95% CI: 39.805, 48.771) (Fig 2).
Fig 2. Pooled prevalence of treatment seeking delay in seeking health service delivery among tuberculosis patients in Ethiopia, 2020.
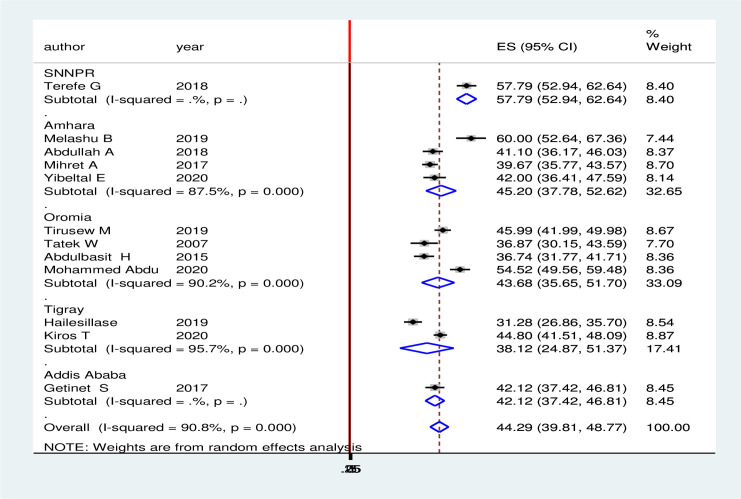
Subgroup analysis
To adjust and minimize the reported heterogeneity of this study, we performed a subgroup analysis based on the region in Ethiopia. Accordingly, the highest rate of treatment seeking delay was observed in Oromia region 57.789% (95% CI: 52.937, 62.641) followed by Amhara region 45.20% (95% CI: 37.784, 52.620) and Oromia region 43.677% (95% CI: 35.653, 51.701). On the other hand, the lowest pooled prevalence of delay in health seeking was in Tigray region 38.124% (95% CI: -24.875, 51.372, and Addis Ababa city administration 42.118% (95% CI: 37.423, 46.812 (Fig 3).
Fig 3. Subgroup analyses by region among TB patient in Ethiopia, 2020.
Heterogeneity and publication bias
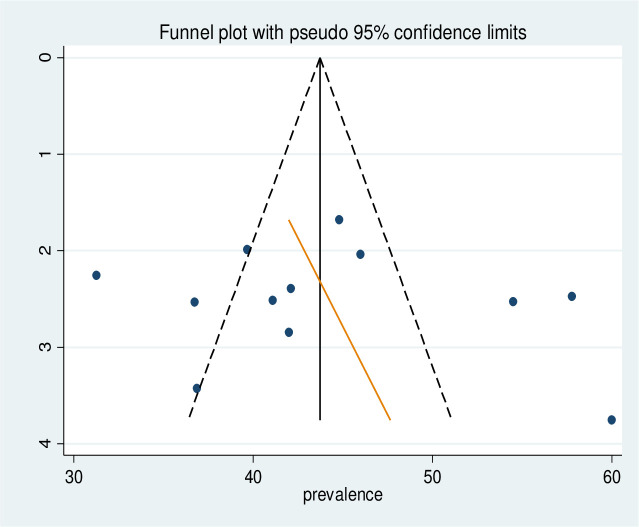
Meta-regression was also conducted to identify the source of heterogeneity using sample size and year of publication as a covariate. It was indicated that there was no effect of sample size and year of publication on heterogeneity between studies (Table 2). The presence of publication bias was tested by Egger’s test and graphically by a funnel plot. Visual inspection of the funnel plot showed asymmetrical distribution, and the Egger test showed insignificant (P = 0.348) (Fig 4).
Table 2. Meta-regression analysis of factors affecting between-study heterogeneity.
| Type of outcome | Heterogeneity source | Coefficients | Std. Err. | P>t |
|---|---|---|---|---|
| Delay to seek health care | Publication year | -.0143786 | .0145204 | 0.348 |
| Sample size | 1.239396 | .7957167 | 0.154 |
Fig 4. Funnel plot to test publication bias in 14 studies with 95% confidence limit.
Sensitivity analysis
We also executed sensitivity analysis by removing studies step by step to evaluate the effect of a single study on the overall effect estimate. The results indicated that removing a single study did not have a significant influence on pooled effects (Table 3).
Table 3. Sensitivity analysis of pooled prevalence for each study being removed one at a time.
| Study omitted | Estimate | [95% Conf. Interval] | |
|---|---|---|---|
| Terefe G (2018) [17] | 43.015514 | 38.887733 | 47.143299 |
| Melashu B (2019) [25] | 43.028976 | 38.666386 | 47.391567 |
| Tirusew M (2019) [18] | 44.140415 | 39.171921 | 49.10891 |
| Abdullah A (2018) | 44.588055 | 39.719296 | 49.45681 |
| Hailesillase (2019) [27] | 45.48138 | 41.283703 | 49.679058 |
| Mihret A (2017) [28] | 44.736866 | 39.824715 | 49.649021 |
| Kiros T (2020) [29] | 44.257614 | 39.142715 | 49.372517 |
| Tatek W (2007) [30] | 44.909893 | 40.205029 | 49.614761 |
| Yibeltal E (2020) [31] | 44.498741 | 39.661049 | 49.33643 |
| Getinet S (2017) [32] | 44.498489 | 39.594158 | 49.402821 |
| Abdulbasit H (2015) [33] | 44.978291 | 40.257931 | 49.698647 |
| Mohammed Abdu (2020) [14] | 43.343212 | 38.868977 | 47.817444 |
| Combined | 44.288032 | 39.805081 | 48.770983 |
Factors associated with treatment seeking delay in seeking health care
12 variables were extracted to identify factors associated with delay in seeking health care. Of these, 8 variables (age, Information about TB, residence, distance, social stigma, occupational status, marital status and educational status) had a strong significant association with delay in treatment seeking at P-value of less than 0.001(Table 4).
Table 4. Factors associated with delay in seeking health care among tuberculosis patients visited health facilities in Ethiopia.
| Determinants (References) | Comparison | Number of Studies | Sample Size | OR (95% CI) | P value | I2 (%) | Heterogeneity test (P value) | Egger test (P value) |
|---|---|---|---|---|---|---|---|---|
| Information about TB [14,17,18,25,27,32] | Good Vs poor | 6 | 2379 | 0.975(0.6391.48) | < 0.001 | 83.6 | 0.907 | 0.767 |
| Residence [14,17,28,29,36] | Rural Vs Urban | 5 | 2715 | 3.459(1.469–8.148) | < 0.001 | 95.8 | 0.005 | 0.939 |
| Sex [17,28,29,36] | Male Vs Female | 4 | 2370 | 0.972 (0.893–1.059) | 0.015 | 71.4 | 0.517 | 0.482 |
| Marital status [28,32,36] | Married Vs Others | 3 | 1392 | 0.979 (0.454–2.112) | < 0.001 | 90.4 | 0.286 | 0.661 |
| Distance [14,18,29] | ≥10km Vs <10km | 3 | 1858 | 1.631(0.858–3.101) | < 0.001 | 90.2 | 0.136 | 0.952 |
| Social stigma [27,32] | High Vs low | 2 | 847 | 1.187(0.293–4.798) | < 0.001 | 95.5 | 0.810 | - |
| Age [17,27,28] | ≥ 45 Vs <45 | 3 | 1422 | 0.363(0.082–1.598) | < 0.001 | 96.2 | 0.180 | 0.433 |
| Occupation [17,27,28,32,36] | Employed Vs Others | 5 | 2944 | 0.670(0.608–0.739) | < 0.001 | 93.6 | 0.001 | 0.586 |
| HIV Sero status [36,37] | Positive Vs Negative | 2 | 1237 | 0.502(0.257–0.981) | 0.160 | 49 | < 0.001 | - |
| Other treatment sought [14,18,29] | Not Sought Vs sought | 3 | 2212 | 7.192(5.587–9.257) | 0.001 | 85 | < 0.001 | 0.044 |
| TB can be cured [17,18,25] | Yes Vs No | 3 | 1155 | 0.586(0.321–1.070) | 0.024 | 73.1 | 0.082 | 0.975 |
| Type of TB [14,25,33] | ETPTB Vs PTB | 3 | 911 | 2.520(1.761–3.605) | 0.180 | 95.3 | 0.001 | 0.882 |
| Educational level [14,17,28,38,39] | ≤primary school Vs > primary school | 5 | 2164 | 11.720(1.006–2.938) | <0.001 | 85.0 | 0.047 | 0.923 |
NB: Vs means versus.
Patients who had good information about tuberculosis were 2.5% less likely to delay in treatment seeking than the patients who had poor knowledge about tuberculosis (OR: 0.975 (95% CI 0.639–1.487), P <0.001, I2: 83.6%; the heterogeneity test (P = 0.907) showed significant evidence of variation across studies, and Egger’s test showed no evidence of publication bias (p = 0.767)).
Additionally, patients who had a perception of tuberculosis as a curable disease were about 41.4% less likely to delay than who were not(OR: 0.586 ((95% CI 0.321–1.070), P = 0.024, I2: 66.8%), the heterogeneity test (p = 0.082) showed significant variation across studies, and Egger’s test showed no evidence of publication bias (P = 0.975)).
Patients who did not seek health care providers on a first contact had about 7 times more likely to delay in treatment seeking than patients who sought formal health care provider on a first contact (OR: 7.192 ((95% CI 5.587–9.257), p = 0.001, I2: 85%), the heterogeneity test (P < 0.001) showed no significant variation across studies, and Egger’s test showed there is evidence of publication bias (P = 0.044)).
Furthermore, patients from rural areas had about four times more likely to have a treatment seeking delay than the patients who visited health facility from urban (OR: 3.459((95% CI 1.469–8.148), p < 0.001, I2: 89%), the heterogeneity test (P = 0.005) showed no significant variation across studies, and the result of Egger’s test showed no evidence of publication bias (P = 0.939)). Those who travelled more than 10km to reach health facility were almost two times more likely to delay seeking health care than who travelled less than 10km (OR: 1.631((95% CI (10.858–3.101), P = 0.001, I2: 90.2%). The heterogeneity test (P = 0.136) showed significant variation across studies, and Egger’s test showed no evidence of publication bias (P = 0.952)).The others independent predictors of delay was extra pulmonary TB (OR: 2.520 ((95% CI 1.761–3.605), 0.180), and lower educational level (OR 11.720 ((95% CI 1.006–2.938), P <0.001).
Discussion
This review revealed a substantial delay in treatment seeking behaviors among TB patients in Ethiopia. It was found that the national pooled prevalence of treatment seeking delay was 44.29%. This high prevalence greatly affects tuberculosis control and prevention program. On the other hand, the prevalence of treatment seeking delay was shorter than previous studies in Ethiopia [17,28,31] and higher than other reports from Ethiopia [30,40,41]. This might be partly due to lack of awareness and traditional medicinal practices across different region of Ethiopia [28].
According to the findings of this review, patients who did not visit formal health care provider on a first contact were a significant risk factor of treatment seeking delay which is consistent with the findings of other similar studies [15,42,43]. Another study also found that the use of informal treatment provider was a strong predictor of treatment seeking delay [41]. This study also in line with other previous studies in Ethiopia [14,15], and Nigeria [44]. This might be due to low confidence in treatment in a health facility and high cultural beliefs of patients for treatment of TB. Besides, the use of some home remedies or antibiotics might reduce or mask the symptoms of the illness which might hinder the timely presentation of the patient to the health care facility [29].
This meta analysis showed that patients from rural areas was a risk factor of treatment seeking delay which agrees with other similar studies [45,46]. In contrary to the current review, another study found that the remoteness of their residence was not found to be associated with delay [17]. In line with current review, other studies conducted in Ethiopia found that rural residents had higher odds of delay compared to the urban residents [26,47]. This might be related to the poor access of rural residents to health information and health facility compared to the urban residents. In addition, the low delay among urban residents could also be as a result of regular and intensive health education offered by health care providers about the disease and easy accessibly to health care institutions.
This review found that long walking distance between health facilities and patient home was a risk factor of delay. A patient who travelled farther than 10 kilometers from health facilities, have a higher delay as compared to those who travelled less than 10 kilometers. The result of this study is in line with other studies conducted in Oromia Special Zone and North Wollo [14,18]. This might be due to rural residency makes it difficult to travel to health facility due to lack of road or distance [48]. Unlike this study, the distance to health facility had not found to affect the treatment seeking delay [11,49,50]. This difference might be due to the fact that the majority of the respondents of those studies live in a distance of less than 2 hours travel. In contrast to the current review, the other studies conducted in Tanzania and Chad also showed shorter time delay by rural patient. This differences could be related with accessibility to the health facility as about 87.5% and 89% of the study participants in Tanzania and Chad had lived with less than 10km from the health facility respectively [12,51].
According to the finding of this review, patients with extra pulmonary TB patients had a higher risk of treatment seeking delay than its counterparts which agrees with other similar study [14]. Similarly, another study also found that extra pulmonary Tuberculosis is significantly associated with delay [36,40]. This could be due to the fact that patient who had extra pulmonary tuberculosis is less likely to produce the cough and expectorate sputum that helped the patients to seek health facility.
The present review showed that treatment seeking delay has been associated with various Sociodemographic factors which agrees with other multiple studies conducted in Ethiopia and elsewhere [30,52–54]. In this review, unemployed patients took relatively long time to go to health care facility compared to employed patients. Similarly, another study found that unemployed patients were independent predictors of treatment seeking delay [55]. This finding is in agreement with study findings done in Uganda, where farmers were experiencing unacceptable patient delay compared to the rest of the respondents [56]. This could be due to lack of awareness on tuberculosis among farmers or unemployed patients, which eventually affects health care seeking behavior.
The present study revealed that age was strongly associated with treatment seeking delay. In contrast to this study, another study found that age was not statistically significant with treatment seeking delay [54]. However, a study conducted in Hadiya Zone, southern Ethiopia showed younger patients aged less than 19 years and elderly patients aged more than 45 years took a longer time to go to the health facility in seeking treatment for their symptoms [55]. This may be due to younger and elderly patients are economically dependent on others in Ethiopia.
The findings of this study also revealed that level of information about tuberculosis and educational status were strongly associated with treatment seeking delay. Other studies conducted in Ethiopia reported lower educational level as an independent predictor of treatment seeking delay [29,47]. Patients who had poor information about TB were more likely to have longer patients delay than those who had good information about TB [57]. In addition, the absence of formal education was strongly associated with treatment seeking delay [47]. This might be due the fact that patient’s who attended higher education levels might have better information about TB to early seek treatment [58].
According to the finding of this review, patient perception on TB was significantly associated with a treatment seeking delay which is consistent with a study conducted on an analysis of symptom duration among Ethiopian pulmonary tuberculosis patients [59]. Similarly, another study done in southern Ethiopia showed that patients who thought TB can be cured was more likely to delay than its counterpart. In this case, the majority of patients believed that their illness will disappear by itself; hence, patients may not visit health facilities [60]. In contrast to our study, the finding of another study done in Uganda revealed that patients who thought TB as a curable disease were more likely to delay seeking treatment than its counterpart [61]. This may be because of their awareness that makes them reluctant.
Being HIV Sero positive patients and being affected with high social stigma are other factors associated with treatment seeking delay which agrees with another study [39]. Similarly, a study conducted on health care seeking delay among pulmonary tuberculosis patients in the North West zone of Tigrai region, North Ethiopia showed that the presence of stigma was independent predictors of treatment seeking delay [27]. The linking of TB with HIV progressively created attitudes and perceptions that have become a source of stigma associated with TB as well as fears of being infected with HIV, and has been cited in several studies as one of the reasons for delays in treatment seeking [62,63].
The limitations of this review were some studies did not contain sufficient predictor variables. Besides, other studies categories predictor variables like patients’ income differently. As a result, we excluded predictor variables like patients’ income from the data analysis.
Conclusion
In this meta analysis and systematic review, we identified a substantial treatment seeking delay among TB patients in Ethiopia. However, the treatment seeking delay varies among different studies and regions of the country. Furthermore, delay was affected by age, information about TB, residence, distance, social stigma, occupational status, marital status and educational status. And, the independent predictors of delay were treatment sought before formal health care provider, residence of the patient, type of TB, educational level, and distance from a health facility. Thus, we recommend health extension workers, health professionals and other stakeholders to focus on patient education, and to continuously mobilize the whole communities on early treatment seeking with a special emphasis given to where treatment sought before formal health care provider, rural resident, extra pulmonary TB, and a patient living farther than 10km distance from health facility.
Supporting information
(DOCX)
(DOC)
(XLSX)
This is the JBI Critical Appraisal of treatment seeking delay.
(DOCX)
Acknowledgments
We would like to thank all authors of studies included in this systematic review and meta-analysis.
Abbreviations
- CI
Confidence Interval
- ETPTB
Extra Pulmonary Tuberculosis
- HCP
Health Care Provider
- OR
Odds Ratio
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PTB
Pulmonary Tuberculosis
- Vs
Versus
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Gebreegziabher SB, Yimer SA, Bjune GA (2016) Tuberculosis case notification and treatment outcomes in West Gojjam Zone, Northwest Ethiopia: a five-year retrospective study. Journal of Tuberculosis Research 4: 23–33. [Google Scholar]
- 2.Girum T, Tariku Y, Dessu S (2017) Survival status and treatment outcome of multidrug resistant tuberculosis (MDR-TB) among patients treated in treatment initiation centers (TIC) in South Ethiopia: a retrospective cohort study. Annals of Medical and Health Sciences Research 7. [Google Scholar]
- 3.Jagger A, Reiter-Karam S, Hamada Y, Getahun H (2018) National policies on the management of latent tuberculosis infection: review of 98 countries. Bulletin of the World Health Organization 96: 173. doi: 10.2471/BLT.17.199414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Organization WH (2016) World malaria report 2015: World Health Organization.
- 5.Raviglione M, Director G (2013) Global strategy and targets for tuberculosis prevention, care and control after 2015. World Health Organization, Geneva.
- 6.Jacobs MG, Pinto Junior VL (2020) Characterization of drug-resistant tuberculosis in Brazil, 2014. Epidemiologia e Serviços de Saúde 28: e2018294. doi: 10.5123/S1679-49742019000300014 [DOI] [PubMed] [Google Scholar]
- 7.Petersen E, Blumberg L, Wilson ME, Zumla A (2017) Ending the Global Tuberculosis Epidemic by 2030—The Moscow declaration and achieving a major translational change in delivery of TB healthcare. International Journal of Infectious Diseases 65: 156–158. doi: 10.1016/j.ijid.2017.11.029 [DOI] [PubMed] [Google Scholar]
- 8.Grobusch MP, Kapata N (2018) Global burden of tuberculosis: where we are and what to do. The Lancet Infectious Diseases 18: 1291–1293. doi: 10.1016/S1473-3099(18)30654-6 [DOI] [PubMed] [Google Scholar]
- 9.Shiferaw MB, Zegeye AM (2019) Delay in tuberculosis diagnosis and treatment in Amhara state, Ethiopia. BMC health services research 19: 1–8. doi: 10.1186/s12913-018-3827-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gebeyehu E, Azage M, Abeje G (2014) Factors associated with patient’s delay in tuberculosis treatment in Bahir Dar City administration, Northwest Ethiopia. BioMed Research International 2014. doi: 10.1155/2014/701429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hussen A, Biadgilign S, Tessema F, Mohammed S, Deribe K, et al. (2012) Treatment delay among pulmonary tuberculosis patients in pastoralist communities in Bale Zone, Southeast Ethiopia. BMC research notes 5: 320. doi: 10.1186/1756-0500-5-320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ngangro NN, Ngarhounoum D, Ngangro MN, Rangar N, Siriwardana MG, et al. (2012) Pulmonary tuberculosis diagnostic delays in Chad: a multicenter, hospital-based survey in Ndjamena and Moundou. BMC public health 12: 513. doi: 10.1186/1471-2458-12-513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ocampo JA (2006) The Millennium Development Goals Report 2005. United Nations, New York.
- 14.Abdu M, Balchut A, Girma E, Mebratu W (2020) Patient Delay in Initiating Tuberculosis Treatment and Associated Factors in Oromia Special Zone, Amhara Region. Pulmonary Medicine 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mesfin MM, Newell JN, Walley JD, Gessessew A, Madeley RJ (2009) Delayed consultation among pulmonary tuberculosis patients: a cross sectional study of 10 DOTS districts of Ethiopia. BMC Public Health 9: 53. doi: 10.1186/1471-2458-9-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Organization WH (2011) World Health Organization global tuberculosis control report 2009. Global tuberculosis control.
- 17.Fuge TG, Bawore SG, Solomon DW, Hegana TY (2018) Patient delay in seeking tuberculosis diagnosis and associated factors in Hadiya Zone, Southern Ethiopia. BMC research notes 11: 115. doi: 10.1186/s13104-018-3215-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wondawek TM, Ali MM (2019) Delay in treatment seeking and associated factors among suspected pulmonary tuberculosis patients in public health facilities of Adama town, eastern Ethiopia. BMC public health 19: 1527. doi: 10.1186/s12889-019-7886-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Takarinda KC, Harries AD, Nyathi B, Ngwenya M, Mutasa-Apollo T, et al. (2015) Tuberculosis treatment delays and associated factors within the Zimbabwe national tuberculosis programme. BMC public health 15: 29. doi: 10.1186/s12889-015-1437-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Health FDRoEMo (2015) Health Sector Development Programme IV Annual Performance Report, EFY 2007 (2014/15). Federal Ministry of Health Addis Ababa, Ethiopia.
- 21.Migliori GB, Nardell E, Yedilbayev A, D’Ambrosio L, Centis R, et al. (2019) Reducing tuberculosis transmission: a consensus document from the World Health Organization Regional Office for Europe. European Respiratory Journal 53: 1900391. doi: 10.1183/13993003.00391-2019 [DOI] [PubMed] [Google Scholar]
- 22.Bjune G (2005) Tuberculosis in the 21st century: an emerging pandemic? Norsk epidemiologi 15. [Google Scholar]
- 23.Buccheri RK, Sharifi C (2017) Critical appraisal tools and reporting guidelines for evidence-based practice. Worldviews on Evidence-Based Nursing 14: 463–472. doi: 10.1111/wvn.12258 [DOI] [PubMed] [Google Scholar]
- 24.Munn Z, Moola S, Riitano D, Lisy K (2014) The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. International journal of health policy and management 3: 123. doi: 10.15171/ijhpm.2014.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shiferaw MB, Zegeye AM (2019) Delay in tuberculosis diagnosis and treatment in Amhara state, Ethiopia. BMC health services research 19: 232. doi: 10.1186/s12913-019-4056-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seid A, Metaferia Y (2018) Factors associated with treatment delay among newly diagnosed tuberculosis patients in Dessie city and surroundings, Northern Central Ethiopia: a cross-sectional study. BMC Public Health 18: 931. doi: 10.1186/s12889-018-5823-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Trull T (2012) Clinical Psychology. Kindle.
- 28.Asres M, Gedefaw M, Kahsay A, Weldu Y (2017) Patients’ delay in seeking health care for tuberculosis diagnosis in East Gojjam zone, Northwest Ethiopia. The American journal of tropical medicine and hygiene 96: 1071–1075. doi: 10.4269/ajtmh.16-0892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tedla K, Medhin G, Berhe G, Mulugeta A, Berhe N (2020) Factors associated with treatment initiation delay among new adult pulmonary tuberculosis patients in Tigray, Northern Ethiopia. PloS one 15: e0235411. doi: 10.1371/journal.pone.0235411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wondimu T, Kassahun W, Getachew S (2007) Delay in initiating tuberculosis treatment and factors associated among pulmonary tuberculosis patients in East Wollega, Western Ethiopia. Ethiopian Journal of Health Development 21: 148–156. [Google Scholar]
- 31.Ayalew YE, Yehualashet FA, Bogale WA, Gobeza MB (2020) Delay for Tuberculosis Treatment and Its Predictors among Adult Tuberculosis Patients at Debremarkos Town Public Health Facilities, North West Ethiopia. Tuberculosis Research and Treatment 2020. doi: 10.1155/2020/1901890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wolfe J (2007) Curing Mental Illness: Beyond Magic Bullets. In: Wolfe J, editor. Introduction To Psychology: MIT Open Courseware. [Google Scholar]
- 33.Abdulbasit H, Meaza D, Sisay G, Getu T (2015) Delay in Tuberculosis Diagnosis among Tuberculosis Patients at the Three Hospitals: Asella, Robe and Abomsa of Arsi Zone, Oromia Regional State, March, 2015. Open Access Library Journal 2: 1–13. [Google Scholar]
- 34.Egger M, Smith GD, Phillips AN (1997) Meta-analysis: principles and procedures. Bmj 315: 1533–1537. doi: 10.1136/bmj.315.7121.1533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tura G, Fantahun M, Worku A (2013) The effect of health facility delivery on neonatal mortality: systematic review and meta-analysis. BMC pregnancy and childbirth 13: 1–9. doi: 10.1186/1471-2393-13-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hamza A, Ababa A (2015) Delay in tuberculosis diagnosis among tuberculosis patients at the three hospitals: asella, robe and abomsa of arsi zone, oromia regional state, March, 2015. Open Access Library Journal 2: 1. [Google Scholar]
- 37.Steinberg L (2012) Big Think. Youtube.
- 38.Bieschke KJ, Abels A, Adams E, Miville M, Schreier B, et al. (2009) Counseling Psychology Model Training Values Statement Addressing Diversity. Counseling Psychologist 37: 641–643. [Google Scholar]
- 39.Adenager GS, Alemseged F, Asefa H, Gebremedhin AT (2017) Factors associated with treatment delay among pulmonary tuberculosis patients in public and private health facilities in Addis Ababa, Ethiopia. Tuberculosis research and treatment 2017. doi: 10.1155/2017/5120841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Asres A, Jerene D, Deressa W (2018) Delays to treatment initiation is associated with tuberculosis treatment outcomes among patients on directly observed treatment short course in Southwest Ethiopia: a follow-up study. BMC pulmonary medicine 18: 64. doi: 10.1186/s12890-018-0628-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Alema HB, Hailemariam SA, Misgina KH, Weldu MG, Gebregergis YS, et al. (2019) Health care seeking delay among pulmonary tuberculosis patients in North West zone of Tigrai region, North Ethiopia. BMC infectious diseases 19: 309. doi: 10.1186/s12879-019-3893-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Belay M, Bjune G, Ameni G, Abebe F (2012) Diagnostic and treatment delay among Tuberculosis patients in Afar Region, Ethiopia: a cross-sectional study. BMC public health 12: 369. doi: 10.1186/1471-2458-12-369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Saifodine A, Gudo PS, Sidat M, Black J (2013) Patient and health system delay among patients with pulmonary tuberculosis in Beira city, Mozambique. BMC public health 13: 559. doi: 10.1186/1471-2458-13-559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Babatunde OI, Bismark EC, Amaechi NE, Gabriel EI, Olanike A-UR (2015) Determinants of treatment delays among pulmonary tuberculosis patients in Enugu Metropolis, South-East, Nigeria. Health 7: 1506. [Google Scholar]
- 45.Fatiregun A, Ejeckam C (2010) Determinants of patient delay in seeking treatment among pulmonary tuberculosis cases in a government specialist hospital in Ibadan, Nigeria. Tanzania journal of health research 12: 113–120. [Google Scholar]
- 46.Li Y, Ehiri J, Tang S, Li D, Bian Y, et al. (2013) Factors associated with patient, and diagnostic delays in Chinese TB patients: a systematic review and meta-analysis. BMC medicine 11: 156. doi: 10.1186/1741-7015-11-156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Awoke N, Dulo B, Wudneh F (2019) Total delay in treatment of tuberculosis and associated factors among new pulmonary TB patients in selected health facilities of Gedeo zone, southern Ethiopia, 2017/18. Interdisciplinary perspectives on infectious diseases 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mondal M, Nazrul HM, Chowdhury M, Howard J (2014) Socio-demographic factors affecting knowledge level of Tuberculosis patients in Rajshahi City, Bangladesh. African health sciences 14: 855–865. doi: 10.4314/ahs.v14i4.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Demissie M, Lindtjorn B, Berhane Y (2002) Patient and health service delay in the diagnosis of pulmonary tuberculosis in Ethiopia. BMC public health 2: 23. doi: 10.1186/1471-2458-2-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Huong NT, Vree M, Duong BD, Khanh VT, Loan VT, et al. (2007) Delays in the diagnosis and treatment of tuberculosis patients in Vietnam: a cross-sectional study. BMC public health 7: 110. doi: 10.1186/1471-2458-7-110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wandwalo E, Mørkve O (2000) Delay in tuberculosis case-finding and treatment in Mwanza, Tanzania. The International Journal of Tuberculosis and Lung Disease 4: 133–138. [PubMed] [Google Scholar]
- 52.Odusanya OO, Babafemi JO (2004) Patterns of delays amongst pulmonary tuberculosis patients in Lagos, Nigeria. BMC public health 4: 1–5. doi: 10.1186/1471-2458-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ngadaya ES, Mfinanga GS, Wandwalo ER, Morkve O (2009) Delay in tuberculosis case detection in Pwani region, Tanzania. A cross sectional study. BMC health services research 9: 1–8. doi: 10.1186/1472-6963-9-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Demissie M, Lindtjorn B, Berhane Y (2002) Patient and health service delay in the diagnosis of pulmonary tuberculosis in Ethiopia. BMC public health 2: 1–7. doi: 10.1186/1471-2458-2-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fuge TG, Bawore SG, Solomon DW, Hegana TY (2018) Patient delay in seeking tuberculosis diagnosis and associated factors in Hadiya Zone, Southern Ethiopia. BMC research notes 11: 1–6. doi: 10.1186/s13104-017-3088-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kiwuwa MS, Charles K, Harriet MK (2005) Patient and health service delay in pulmonary tuberculosis patients attending a referral hospital: a cross-sectional study. BMC Public Health 5: 1–7. doi: 10.1186/1471-2458-5-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mesfin MM, Newell JN, Walley JD, Gessessew A, Madeley RJ (2009) Delayed consultation among pulmonary tuberculosis patients: a cross sectional study of 10 DOTS districts of Ethiopia. BMC Public Health 9: 1–10. doi: 10.1186/1471-2458-9-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chanie T, Meaza D (2011) Knowledge and practices of tuberculosis infection control among health professionals in Northwest Ethiopia. BMC health ser res 14: 593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Madebo T, Lindtjorn B (1999) Delay in treatment of pulmonary tuberculosis: an analysis of symptom duration among Ethiopian patients. MedGenMed: Medscape general medicine: E6–E6. [PubMed] [Google Scholar]
- 60.Wondawek TM, Ali MM (2019) Delay in treatment seeking and associated factors among suspected pulmonary tuberculosis patients in public health facilities of Adama town, eastern Ethiopia. BMC public health 19: 1–7. doi: 10.1186/s12889-018-6343-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sendagire I, Van der Loeff MS, Mubiru M, Konde-Lule J, Cobelens F (2010) Long delays and missed opportunities in diagnosing smear-positive pulmonary tuberculosis in Kampala, Uganda: a cross-sectional study. PLOS one 5: e14459. doi: 10.1371/journal.pone.0014459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Deribew A, HaileMichael Y, Tesfaye M, Desalegn D, Wogi A, et al. (2010) The synergy between TB and HIV co-infection on perceived stigma in Ethiopia. BMC research notes 3: 249. doi: 10.1186/1756-0500-3-249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Møller V, Erstad I (2007) Stigma associated with tuberculosis in a time of HIV/AIDS: narratives from the Eastern Cape, South Africa. South African Review of Sociology 38: 103–119. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOC)
(XLSX)
This is the JBI Critical Appraisal of treatment seeking delay.
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.