Abstract
Insomnia and depression are distinct clinical phenomena, yet they are highly comorbid. One potential explanation for the high comorbidity rates is the overlap in risk factors. Atypical responses to stress, for example, place individuals at greater risk for both insomnia and depression. The goal of the present study was to simultaneously assess vulnerability to stress-related sleep disturbance (sleep reactivity) and the tendency to make negative attributions about stressful events (negative cognitive style), and how they relate to insomnia and depression. Study participants included 224 undergraduate students recruited from a large, public university in the United States. Sleep reactivity and negative cognitive style were assessed using the Ford Insomnia Response to Stress Test (FIRST) and the Cognitive Style Questionnaire (CSQ), respectively. Insomnia symptoms were assessed using the Insomnia Severity Index (ISI), and depressive symptoms were measured using the Center for Epidemiologic Studies Depression Scale (CES-D). Sleep reactivity was independently associated with greater insomnia and depression symptoms. Additionally, a negative cognitive style was related to greater depressive symptoms, and this effect was partially mediated by sleep reactivity. The current findings suggest that sleep reactivity may contribute to the development of disorders beyond insomnia. These findings further support the use of an interdisciplinary approach to investigating etiological models, and more specifically, the further exploration of how multiple stress responses (in terms of cognitions, sleep, etc.) place individuals at greater risk for developing psychopathology.
1. Introduction
Insomnia and depression are highly comorbid conditions (Khurshid, 2018; Staner, 2010; Taylor et al., 2005). Traditionally, research in this area has assumed that insomnia was simply a symptom of depression. More recent work and changes to the latest diagnostic classification system, however, support that they are distinct phenomena (American Psychiatric Association, 2013; Lichstein, 2006). More, studies show that insomnia often precedes and predicts the onset of a depressive episode (Baglioni et al., 2011; Johnson et al., 2006; Li et al., 2016). Despite scientific progress highlighting that insomnia and depression are unique disorders, there continue to be few explanations that can adequately describe the reasons for the high rates of co-occurrence. Such explanations would be able to provide important insights into whether insomnia and depression actually represent the same or different disease processes. For example, they may be associated because they are triggered by shared risk factors. One precipitating factor common to both disorders is stressful life events (Monroe and Harkness, 2005; Perlis et al., 2011). While some sleeplessness and changes in affect following stress can be considered adaptive, more extreme responses to stress may be indicative of or increase risk for clinical insomnia or depression (Drake et al., 2014; Kalmbach et al., 2018). For some individuals, the threshold for a stress response may be lower and/or the magnitude of that response may be greater. In the depression literature, these individual differences in stress reactivity have been discussed in terms of a “cognitive vulnerability” (i.e., how we think about the stressor; Abramson et al., 1989). In the insomnia literature, these individual differences have been discussed in terms of sleep reactivity (i.e., how we sleep in response to the stressor; Drake et al., 2004). To date, these lines of work have yet to be integrated. It may be that these constructs are related and partially explain the insomnia-depression connection.
1.1. Cognitive reactivity to stress
According to the hopelessness theory of depression, individual differences in attributions about life stress make some people more vulnerable to developing depression (Abramson et al., 1989). Some individuals have a “negative cognitive style” in which they have a greater tendency to make negative attributions about stressful life events (Haeffel et al., 2017). These negative attributions tend to focus on (1) the stability and globality of the perceived cause of the event, (2) the likelihood that this will lead to other negative consequences in the future, and (3) the implications that the event has on one’s own self-worth. Research supports that possessing this negative cognitive style makes one more vulnerable, in the face of stress, to depressive symptomatology or even a full-blown depressive disorder (Abramson et al., 1999; Alloy et al., 2006; Gibb et al., 2006; Haeffel and Grigorenko, 2007; Mac Giollabhui et al., 2018).
1.2. Sleep reactivity to stress
A separate but parallel line of research investigates the factors that contribute to whether or not a person experiences sleep disturbance in response to various challenges or stressors (Drake et al., 2004). This concept is referred to as sleep reactivity or the degree to which individuals are vulnerable to stress-related sleep disturbance (i.e., difficulty falling and/or staying asleep). Prior research supports that sleep reactivity is a predisposing factor to insomnia disorder (Drake et al., 2014; Jarrin et al., 2013; Nakajima et al., 2014). These studies suggest that, prior to the onset of insomnia disorder, individuals who are highly sleep reactive have a greater tendency to experience sleep disturbance following a stressful life event. Although the consequences of greater sleep reactivity have been examined in the context of insomnia disorder, sleep reactivity is a propensity for sleep disturbance in response to stress, and thus not inherently insomnia disorder specific. That is, risk for the future development of insomnia is a consequence of sleep reactivity and not the cause. Some studies, for example, have shown that sleep reactivity is also related to larger depression scores (Drake et al., 2014; Vargas et al., 2015). Much like hopelessness theory’s negative cognitive style, the underlying vulnerability factor here is related to how people respond to stress, and it is these individual differences that place some at greater risk for future psychopathology.
1.3. Integrated theory of cognitive and sleep reactivity
Both negative cognitive style and sleep reactivity tap into a person’s tendency to think about how they will respond to a life event or situation (in terms of their cognitions or sleep, respectively). It is possible, if not likely, that these two constructs are highly related (e.g., someone who has overly negative thoughts following a stressor, may also have trouble sleeping in response to stress). Also, they may be related in a mechanistic way that could potentially explain at least one pathway by which these vulnerability factors predispose individuals to both insomnia and depression. As originally proposed in the hopelessness theory, a negative cognitive style results in greater negative cognitions following a stressor. It is these negative cognitions that are thought to ultimately lead to greater depressive symptoms. An increased number of negative cognitions, however, may lead to an intermediate step of difficulty with falling or staying asleep. Our hypothesis is that individuals who exhibit a greater negative cognitive style will also have greater sleep reactivity, and in turn, greater sleep reactivity will be associated with greater insomnia and depression symptoms. Put differently, sleep reactivity will mediate the association between cognitive vulnerability and depression.
2. Methods
2.1. Participants and procedure
Study participants included 224 undergraduate students (160 female, Mage = 19.4 years, SDage = 1.9, Rangeage = 18–31 years) recruited from a large, public university in the southern United States. The sample’s self-reported race and ethnicity consisted of 82.6% Caucasian/White, 5.8% Latino or Latina, 4.5% Black, African American, African, 2.2% Asian or Asian American, 1.8% American Indian, Native American, Alaska Native, 0.4% Middle Eastern, and 2.7% Multiracial. Students were recruited from the General Psychology Research Participation Pool via Sona Systems (http://www.sona-systems.com/) to participate in a study on “Sleep and Thinking”. Sona Systems is a departmentally administered web-based research management software package. Interested participants were invited to sign up for the study via Sona. Participants were included in the present study if they were at least 18 years old, had a stable internet connection, corrected-to-normal vision, and were able to read and write in English. The study consisted of a single, online survey administered via Qualtrics XM (a secure, widely used online survey hosting site). The Institutional Review Board at the University of Arkansas approved the study, and participants completed an informed consent form prior to being instructed to answer questions about their sleep, cognitive styles, and mood. Participants were compensated 1 research credit hour for completing the survey.
2.2. Measures
2.2.1. Negative cognitive style
The Cognitive Style Questionnaire (CSQ; Abramson and Metalsky, 1989; Haeffel et al., 2008) was used to assess participants’ negative cognitive style. The CSQ is a modified version of the Attributional Style Questionnaire, which was originally developed by Peterson and colleagues (1982). The CSQ includes both negative and positive, hypothetical events. For each hypothetical event, participants are instructed to vividly imagine themselves in that situation (example event: “You take an exam and receive a low grade on it.”). Next, they were instructed to write down what they believe to be the one major cause of the event (e.g., “I did not study”). Participants then used a 7-point Likert scale to rate the cause that they have specified on dimensions of (1) stability and (2) globality and on the (3) consequences and (4) self-worth implications of the hypothetical event. The CSQ quantifies two factors, a negative cognitive style and a positive or enhancing cognitive style. The negative cognitive style factor estimates a person’s tendency to make negative attributions about a negative life event. In contrast, the enhancing cognitive style factor estimates a person’s tendency to make positive attributions about a positive life event and has been shown to be related to greater resiliency to depression (Needles and Abramson, 1990). While both factors were assessed, only negative cognitive style was included in the following analyses. An individual’s negative cognitive style is their average rating across the four scales for the 12 hypothetical negative events. Composite scores can range from 1 to 7, with higher scores reflecting a greater negative cognitive style. The CSQ has good internal consistency, reliability, and validity (Haeffel et al., 2008). In the present study, the full-scale composite score for negative cognitive style demonstrated good internal consistency (α = 0.84).
2.2.2. Sleep reactivity
The Ford Insomnia Response to Stress Test (FIRST; Drake et al., 2004) is a 9-item questionnaire used to assess vulnerability to stress- related sleep disturbance (i.e., sleep reactivity). The FIRST measures the probability that a person would have difficulty sleeping following (or in anticipation of) a stressful situation. It asks how likely (1 = “not likely”; 2 = “somewhat likely”; 3 = “moderately likely”; 4 = “very likely”) the participant would have difficulty sleeping under nine stressful situations (e.g., before an important meeting the next day, after getting bad news during the day, after an argument, and before having to speak in public). Participants were asked to rate the likelihood even if they had not experienced the situation recently. The FIRST has been widely used in previous sleep research (Altena et al., 2017; Drake et al., 2008; Fernández-Mendoza et al., 2010; Vargas et al., 2015; Yang et al., 2011), and has demonstrated good psychometric properties. The total score was equal to the sum of the nine items, with higher scores suggesting greater sleep reactivity. The FIRST also demonstrated good internal consistency (α = 0.82) in the current sample.
2.2.3. Insomnia symptoms
Participants completed the Insomnia Severity Index (ISI; Morin, 1993) to assess self-reported perception of insomnia symptom severity and the degree to which they experienced distress caused by those symptoms. Total scores on the full 7-item scale range from 0 to 28, with higher scores indicating higher insomnia symptom severity. High internal consistency (α = 0.77) and test-retest reliability (r = 0.83, r = 0.77, r = 0.73) after 1, 2, and 3 months have been previously reported for the ISI (Bastien et al., 2001). The ISI demonstrated good internal consistency (α = 0.87) in this study.
2.2.4. Depression symptoms
The Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977) was used to assess current self-reported depression symptoms. The CES-D consists of 20 four-point scale items assessing various symptoms commonly reported in depression. Total scores on the full 20-item scale range from 0 to 60. Good internal consistency (α = 0.85) and test retest reliability (r = 0.61) have been previously reported for the CES-D (Devins et al., 1988; Radloff, 1977). In the current study, analyses were conducted with and without the “restless sleep” item in order to account for the overlap between the CES-D and insomnia items. The full-scale CES-D demonstrated excellent internal consistency (α = 0.91).
3. Statistical analysis
Pearson correlations and descriptive statistics were first computed. This was followed up by a series of linear and hierarchical regressions (via IBM SPSS Statistics 26), which were used to estimate the associations between negative cognitive style, sleep reactivity, insomnia symptoms, and depression symptoms. All variables were continuous and normally distributed, and as a result, analyzed in their uncorrected forms. Gender and age were entered as covariates in all the adjusted models. To determine the independent effect of negative cognitive styles on each variable (i.e., sleep reactivity, insomnia symptoms, and depression symptoms), a series of unadjusted linear regressions were conducted where CSQ was entered as the independent variable. Similarly, the independent effect of sleep reactivity on insomnia and depression symptoms was assessed. Next, hierarchical regressions were used to estimate the proportion of the variance accounted for by each variable, when all the variables are entered into the model. When examining whether FIRST scores predict depression symptoms, for example, CSQ, ISI, and gender were entered in Step 1 of the model and FIRST was entered in Step 2. The R2 change was used to quantify the proportion of variance in depression symptoms uniquely predicted by differences in FIRST scores. Analyses were conducted with and without the sleep item included in the CES-D. No significant differences were observed, and therefore, only the models with the full-scale CES-D (sleep item included) were reported below. Finally, a Sobel test (Sobel, 1982) was used to calculate whether sleep reactivity mediated that association between negative cognitive style and depression symptoms. This test was repeated with insomnia symptoms as the dependent variable. Unstandardized regression coefficients and standard errors were used to conduct these mediation tests.
4. Results
4.1. Descriptive statistics
Table 1 provides the Pearson correlations for all four measures. Consistent with previous studies in college students (e.g., Haeffel, 2017; Hankin et al., 2004), negative cognitive style scores (i.e., CSQ) ranged from 2.3 to 7.0 (Mean = 4.4; SD = 0.7). Sleep reactivity scores (i.e., FIRST) ranged from 9 to 36 (Mean = 21.4; SD = 6.0). Depression symptom scores (i.e., CES-D) ranged from 0 to 51 (Mean = 17.3; SD = 11.0). Insomnia symptom scores (i.e., ISI) ranged from 0 to 25 (Mean = 8.3; SD = 5.4). Not surprisingly, the CSQ and FIRST were each correlated with depression (CSQ, r = 0.24, p < 0.001; FIRST, r = 0.39, p < 0.001) and insomnia symptoms (CSQ, r = 0.21, p < 0.001; FIRST, r = 0.44, p < 0.001). Depression and insomnia symptoms were also significantly correlated, r = 0.60, p < 0.001, as were the CSQ and FIRST, r = 0.20, p < 0.01. Mean comparisons by gender revealed that females reported, in general, greater scores on all measures, yet only mean differences in the FIRST were statistically significant (Table 2). This finding suggests that women reported being more vulnerable to stress-related sleep disturbance relative to men.
Table 1.
Pearson correlation (r) for all study variables.
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| (1) Negative Cognitive Style (CSQ) | – | |||
| (1) Sleep Reactivity (FIRST) | 0.197* | – | ||
| (1) Insomnia Symptoms (ISI) | 0.213* | 0.441** | – | |
| (1) Depression Symptoms (CES-D) | 0.238** | 0.390** | 0.605** | – |
p < 0.05
p < 0.01
p < 0.001
Table 2.
Means and standard deviations for study variables.
| Total (n = 224) | Male (n = 64) | Female (n = 160) | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | t-test | |
| Age (in years) | 19.4 | 1.9 | 19.8 | 2.0 | 19.3 | 1.8 | 1.79 |
| Negative Cognitive Style (CSQ) | 4.4 | 0.7 | 4.4 | 0.6 | 4.4 | 0.8 | 0.41 |
| Sleep Reactivity (FIRST) | 21.4 | 6.0 | 17.9 | 4.7 | 22.8 | 5.9 | 5.91** |
| Insomnia Symptoms (ISI) | 8.3 | 5.4 | 7.4 | 5.3 | 8.6 | 5.5 | 1.58 |
| Depression Symptoms (CES-D) | 17.3 | 11.0 | 15.5 | 10.3 | 18.0 | 11.2 | 1.50 |
p < 0.05
p < 0.01
p < 0.001
4.2. Unadjusted and adjusted regressions
A series of unadjusted and adjusted regression models were performed in order to estimate the independent association between each of the relevant variables (i.e., main effects). According to the unadjusted models (i.e., no covariates entered into the model), CSQ was positively and significantly associated with both insomnia and depression symptoms (Table 3). The proportion of the variance explained by CSQ scores was, however, relatively small (R2 < 0.06). FIRST scores were also associated with greater CES-D, R2 = 0.15, p < 0.001, and ISI scores, R2 = 0.20, p < 0.001. The independent association between CSQ and FIRST was also significant, R2 = 0.03, p < 0.01. While controlling for the other variables in the model (see adjusted models in Table 3), CSQ was not significantly associated with CES-D, R2 change = 0.007, p = 0.12, ISI, R2 change = 0.003, p = 0.27 or FIRST, R2 change = 0.007, p = 0.13. In contrast, greater FIRST scores continued to be positively related to greater scores on the CES-D, R2 change = 0.014, p = 0.02, and ISI, R2 = 0.044 change, p < 0.001, even while controlling for the other measures.
Table 3.
Results from unadjusted and adjusted regression analyses: proportion of variance (R2) explained by each bivariate association. ΔR2 is the proportion of variance specific to each bivariate association while controlling for age, gender, and the other three study variables. In the adjusted model, variables were entered hierarchically, with all covariates entered in Step 1 and the variable of interest entered in Step 2.
| Unadjusted Models | Adjusted Models | |||
|---|---|---|---|---|
| R2 | p-value | ΔR2 | p-value | |
| CSQ – CES-D | 0.057 | < 0.001 | 0.007 | 0.12 |
| CSQ – ISI | 0.045 | < 0.01 | 0.003 | 0.27 |
| CSQ – FIRST | 0.039 | < 0.01 | 0.007 | 0.13 |
| FIRST – CES-D | 0.152 | < 0.001 | 0.014 | 0.02 |
| FIRST – ISI | 0.195 | < 0.001 | 0.044 | < 0.001 |
| ISI – CES-D | 0.366 | < 0.001 | 0.218 | < 0.001 |
CSQ = Cognitive Style Questionnaire, FIRST = Ford Insomnia Response to Stress Test, ISI = Insomnia Severity Index, CES-D = Center for Epidemiologic Studies Depression Scale.
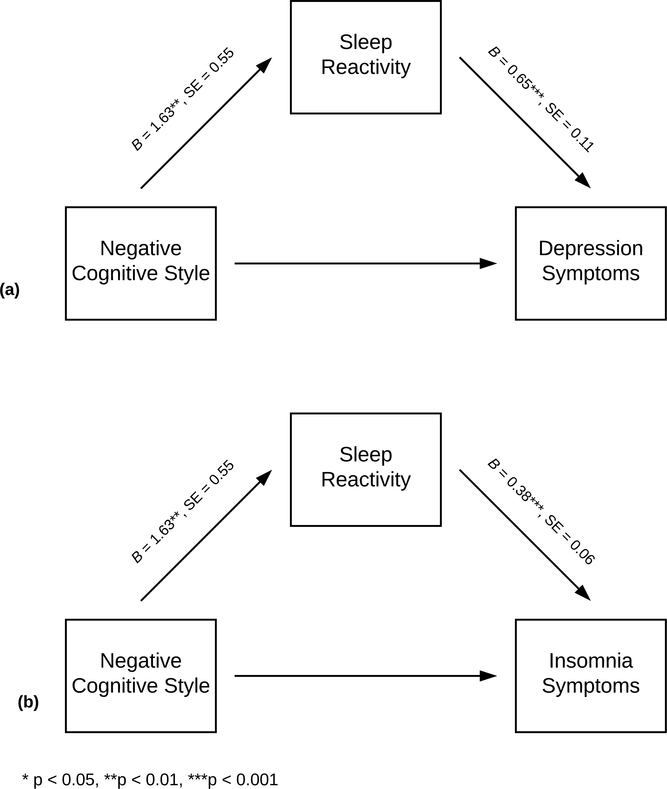
4.3. Mediation analyses
Finally, a Sobel Test was used to estimate whether sleep reactivity partially mediated the association between negative cognitive style and depressive symptomology. The impact of sleep reactivity on depression symptoms, while controlling for the effect of negative cognitive style was computed first. Consistent with the analyses presented above, this model revealed that both greater sleep reactivity, B = 0.652, t(221) = 5.718, p < 0.001, and negative cognitive style, B = 2.547, t(221) = 2.69, p < 0.01, predicted greater depressive symptoms (Fig. 1a). Furthermore, results from the mediation analysis suggested that sleep reactivity partially mediated the effect of negative cognitive style on depression symptoms, Sobel’s test = 2.65 (SE = 0.40), p < 0.01. A second mediation analyses was computed with insomnia scores entered as the dependent variable (Fig. 1b). According to this model, greater sleep reactivity, B = 0.379, t(223) = 6.824, p < 0.001, and negative cognitive style, B = 0.991, t(223) = 2.152, p = 0.03, predicted greater insomnia scores. This model also supported that sleep reactivity mediated the association between negative cognitive style and depression symptoms, Sobel’s test = 2.73 (SE = 0.23), p < 0.01.
Figure 1.
Results from the mediation models. Unstandardized regression coefficients quantify the association between negative cognitive style and the mediator (sleep reactivity), and the association between the mediator and (a) depression or (b) insomnia symptoms, while negative cognitive style was simultaneously entered into the model.
5. Discussion
Results from the present study support the following two conclusions: (1) cognitive vulnerability (i.e., the likelihood to make negative attributions in response to stress) and sleep reactivity (i.e., the likelihood to have trouble sleeping in response to stress) are related constructs, and (2) there is an indirect effect of cognitive vulnerability on depression and insomnia symptoms that is, in part, explained by differences in sleep reactivity (i.e., mediation effect). With regard to the first conclusion, the data suggest that there is a small, but significant, proportion of shared variance between the CSQ and the FIRST. It is possible that whatever biobehavioral processes are responsible for the increased probability of making negative attributions about a stressful life event, are also responsible for the increased probability of having trouble sleeping in response to stress. It is worth noting here that the FIRST is not actually a measure of sleep per se, but rather a measure of how a person thinks about the likelihood that they will have trouble sleeping when confronted with a stressor. That said, greater FIRST scores reliably predict the future onset of insomnia disorder (Drake et al., 2014; Kalmbach et al., 2018). With regard to the second conclusion, part of the variance in depression (and insomnia) symptoms explained by the cognitive vulnerability factor is through its relationship with sleep reactivity. These findings are consistent with other research showing that sleep reactivity is related to greater stress-related cognitive intrusion/rumination, and its prospective effect on insomnia (Drake et al., 2014). Additionally, they are in line with prior research suggesting that a negative cognitive style predicts depression (Alloy et al., 2006; Gibb et al., 2006), however, this is the first study to show that sleep disturbance (or at least the perceived likelihood of sleep disturbance) partially explains this association. That is, someone with a negative cognitive style, when confronted with a stressful situation(s), will likely make negative attributions about these situations. These negative cognitions may, in turn, lead to difficulty falling or staying asleep and ultimately depression. As with prior literature (Fava and Tossani, 2007; Perlis et al., 1997), these findings support that sleep disturbance may be an early sign of vulnerability to depression.
The current findings also add to the growing list of studies that have demonstrated an independent association between sleep reactivity and depression (Drake et al., 2014; Vargas et al., 2015). In fact, it is worth noting that in the current sample the FIRST was more highly correlated with depression symptoms than even the CSQ. This is important because, as is implied in the title of the questionnaire used to assess it, sleep reactivity was originally conceived of as a vulnerability factor for insomnia disorder. It is becoming increasingly clear that sleep reactivity may be a vulnerability factor for other disorders with a diathesis-stress- based etiology. Under stressful conditions, sleep may be the “first thing to go”, and therefore, predictive of more severe psychopathology. More work is still needed to demonstrate that sleep reactivity is prospectively related to the future-onset of a depressive episode, but present and past findings are promising.
There were also significant gender differences in sleep reactivity. On average, women reported being more likely to experience stress-related sleep disturbance. The present sample was young and relatively healthy, which may explain why gender differences in sleep reactivity, and not insomnia or depression symptoms, were observed. Approximately 15% and 35% of the entire sample reported insomnia (ISI ≥ 15) and depression symptoms (CES-D ≥ 20; Vilagut et al., 2016), respectively, in the clinically significant range. While these prevalence rates are consistent with other reports (Kessler et al., 2003; Morin and Jarrin, 2013; Ohayon, 1997), individual differences in symptom severity may be attenuated in younger samples.
There are a number of strengths and limitations worth highlighting here. As summarized above, this study is the first to incorporate two separate, but related fields of research. Such efforts may help fill in some of the gaps in knowledge and provide a more comprehensive model for understanding the factors that predispose individuals to insomnia, depression, or both. A major limitation of the findings has to do with the descriptive and cross-sectional nature of the research. While we are not able to say with certainty whether cognitive vulnerability and sleep reactivity are influencing insomnia and depression symptoms (or vice versa), these data are consistent with previous prospective findings (Drake et al., 2014). It’s possible that greater insomnia and/or depression symptoms impact people’s reporting behaviors (i.e., higher chance that they will report greater tendencies toward negative attributions and sleep disturbance because they are depressed or already experiencing some insomnia). Moreover, due to the cross-sectional nature of the study, the present data cannot address whether the cognitive vulnerability and sleep reactivity factors precede and predict the onset of insomnia and depression symptoms (and therefore suggest they are predisposing factors), as compared to reinforcing or exacerbating symptoms once they develop (i.e., perpetuating factors). Prior prospective data (e.g., (Alloy et al., 2006; Drake et al., 2014)) and theory suggests that these are both vulnerability or predisposing factors. That is, these individual tendencies interact with stress (precipitating factor) to increase risk for developing insomnia and/or depression symptoms. This said, follow-up studies are needed in order to examine these associations prospectively. For example, does a negative cognitive style predict the future onset of more persistent insomnia symptoms (and subsequently depression), and is this association explained via its effect on sleep reactivity. As mentioned previously, the study sample consisted of predominately young, white women, many of which reported minimal to no symptoms of insomnia and depression. The nature of the sample certainly limits the generalizability of these findings, and therefore an important next step will be to replicate these findings in an older and more diverse sample. Future research can also examine the relationship between these variables longitudinally in an asymptomatic, but at-risk group (e.g., familial risk and/or previous history of depression or insomnia).
6. Conclusion
The primary aim of this research was to explore the association between negative cognitive style (a vulnerability factor for depression) and sleep reactivity (a vulnerability factor for insomnia), and whether they predict, alone or in combination, insomnia or depression symptoms. This was done by assessing self-reported differences on these measures among a sample of undergraduate students. According to the results, negative cognitive style and sleep reactivity are related constructs, and sleep reactivity may mediate the association between negative cognitive style and insomnia/depression symptoms. In general, these findings support the use of an interdisciplinary approach to investigating etiological models, and more specifically, the further exploration of how multiple stress responses (in terms of cognitions, sleep, etc.) place individuals at greater risk for developing psychopathology.
Acknowledgements
We would like to acknowledge the participants that volunteered their time to complete this research.
Role of Funding Source
The authors have no funding sources to report.
Footnotes
Declarations of Competing Interest
None.
References
- Abramson LY, Alloy LB, Hogan ME, Whitehouse WG, Donovan P, Rose DT, … Raniere D, 1999. Cognitive vulnerability to depression: theory and evidence. Journal of Cognitive Psychotherapy 13 (1), 5–20. Retrieved from http://www.ingentaconnect.com/content/springer/jcogp/1999/00000013/00000001/art00002. [Google Scholar]
- Abramson LY, & Metalsky GI (1989). The cognitive style questionnaire: measurement of negative cognitive styles about self and consequences. Unpublished Work.
- Abramson LY, Metalsky GI, Alloy LB, 1989. Hopelessness depression: a theory-based subtype of depression. Psychol. Rev. 96 (2), 358–372. doi: 10.1037/0033-295X.96.2.358. [DOI] [Google Scholar]
- Alloy LB, Abramson LY, Whitehouse WG, Hogan ME, Panzarella C, Rose DT, 2006. Prospective incidence of first onsets and recurrences of depression in individuals at high and low cognitive risk for depression. J. Abnorm. Psychol. 115 (1), 145–156. doi: 10.1016/j.jad.2006.02.012. [DOI] [PubMed] [Google Scholar]
- Altena E, Chen IY, Daviaux Y, Ivers H, Philip P, Morin CM, 2017. How hyperarousal and sleep reactivity are represented in different adult age groups: Results from a large cohort study on insomnia. Brain Sci. 7 (4). doi: 10.3390/brainsci7040041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association, 2013. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®), fifth ed. Retrieved from https://books.google.com/books?hl=en&lr=&id=-JivBAAAQBAJ&oi=fnd&pg=PT18&dq=diagnostic+and+statistical+manual+&ots=cdWQ04LKx7&sig=wBBV2FDDB-n4dI3pwQFUyYTyW2A. [Google Scholar]
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, … Riemann D, 2011. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. Journal of Affective Disorders 135 (1–3), 10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Bastien CH, Vallieres A, Morin CM, 2001. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2 (4), 297–307. doi: 10.1016/S1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Devins G, Orme C, Costello C, 1988. Measuring depressive symptoms in illness populations: psychometric properties of the Center for Epidemiologic Studies Depression (CES-D) scale. Psychol. Health. Retrieved from 10.1080/08870448808400349. [DOI] [Google Scholar]
- Drake CL, Pillai V, Roth T, 2014. Stress and sleep reactivity: a prospective investigation of the stress-diathesis model of insomnia. Sleep 37 (8), 1295–1304. doi: 10.5665/sleep.3916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake CL, Richardson G, Roehrs T, Scofield H, Roth T, 2004. Vulnerability to stress- related sleep disturbance and hyperarousal. Sleep 27 (2), 285–291. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15124724. [DOI] [PubMed] [Google Scholar]
- Drake CL, Scofield H, Roth T, 2008. Vulnerability to insomnia: the role of familial aggregation. Sleep Med. 9 (3), 297–302. doi: 10.1016/j.sleep.2007.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fava GA, Tossani E, 2007. Prodromal stage of major depression. Early Interv. Psychiatry 1, 9–18. doi: 10.1111/j.1751-7893.2007.00005.x. [DOI] [PubMed] [Google Scholar]
- Fernández-Mendoza J, Vela-Bueno A, Vgontzas AN, Ramos-Platón MJ, Olavarrieta-Bernardino S, Bixler EO, De la Cruz-Troca JJ, 2010. Cognitive-emotional hyperarousal as a premorbid characteristic of individuals vulnerable to insomnia. Psychosom. Med. 72 (4), 397–403. doi: 10.1097/PSY.0b013e3181d75319. [DOI] [PubMed] [Google Scholar]
- Gibb BE, Beevers CG, Andover MS, Holleran K, 2006. The hopelessness theory of depression: a prospective multi-wave test of the vulnerability-stress hypothesis. Cognit. Ther. Res. 30 (6), 763–772. doi: 10.1007/s10608-006-9082-1. [DOI] [Google Scholar]
- Haeffel G, Hershenberg RE, Goodson JT, Hein S, Square A, Grigorenko EL, Chapman J, 2017. The hopelessness theory of depression: clinical utility and generalizability. Cognit. Ther. Res. 41, 543–555. [Google Scholar]
- Haeffel GJ, 2017. Don’t sleep on it: less sleep reduces risk for depressive symptoms in cognitively vulnerable undergraduates. J. Pers. Soc. Psychol. 113 (6), 925–938. doi: 10.1037/pspp0000119. [DOI] [PubMed] [Google Scholar]
- Haeffel GJ, Gibb BE, Metalsky GI, Alloy LB, Abramson LY, Hankin BL, … Swendsen JD, 2008. Measuring cognitive vulnerability to depression: development and validation of the cognitive style questionnaire. Clinical Psychology Review 28 (5), 824–836. doi: 10.1016/j.cpr.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haeffel GJ, Grigorenko EL, 2007. Cognitive vulnerability to depression: exploring risk and resilience. Child Adolesc. Psychiatr. Clin. N. Am. 16 (2), 435–448. doi: 10.1016/j.chc.2006.11.005. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Miller N, Haeffel GJ, 2004. Cognitive vulnerability-stress theories of depression: Examining affective specificity in the prediction of depression versus anxiety in three prospective studies. Cognit. Ther. Res. 28 (3), 309–345. doi: 10.1023/B:COTR.0000031805.60529.0d. [DOI] [Google Scholar]
- Jarrin D, Chen I, Ivers H, Morin C, 2013. Does vulnerability to stress- related insomnia predict future incident and persistent insomnia among good sleepers? Sleep Med.. Retrieved from http://www.sciencedirect.com/science/article/pii/S1389945713015839. [Google Scholar]
- Johnson EO, Roth T, Breslau N, 2006. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J. Psychiatr. Res. 40 (8), 700–708. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- Kalmbach DA, Anderson JR, Drake CL, 2018. The impact of stress on sleep: pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J. Sleep Res. 27, e12710. doi: 10.1111/jsr.12710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Berglund P, Demler O, Jin R, Koretz D, Merikangas K, … Wang, 2003. The epidemiology of major depressive disorder. Journal of the American Medical Association 2003 (289), 186–187. [DOI] [PubMed] [Google Scholar]
- Khurshid KA, 2018. Comorbid insomnia and psychiatric disorders: an update. Innov. Clin. Neurosci. 15, 28–32 Matrix Medical Communications. [PMC free article] [PubMed] [Google Scholar]
- Li L, Wu C, Gan Y, Qu X, Lu Z, 2016. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry 16 (1). doi: 10.1186/s12888-016-1075-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichstein KL, 2006. Secondary insomnia: a myth dismissed. Sleep Med. Rev. 10 (1), 3–5. doi: 10.1016/j.smrv.2005.10.001. [DOI] [PubMed] [Google Scholar]
- Giollabhui, Mac N, Hamilton L,J, Nielsen J, Connolly SL, Stange JP, Varga S, … Alloy LB, 2018. Negative cognitive style interacts with negative life events to predict first onset of a major depressive episode in adolescence via hopelessness. Journal of Abnormal Psychology 127 (1), 1–11. doi: 10.1037/abn0000301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM, Harkness KL, 2005. Life stress, the “kindling” hypothesis, and the recurrence of depression: considerations from a life stress perspective. Psychol. Rev. 112 (2), 417–445. doi: 10.1037/0033-295X.112.2.417. [DOI] [PubMed] [Google Scholar]
- Morin CM, 1993. Insomnia: Psychological Assessment and Management Retrieved from http://www.guilford.com/books/Insomnia/Charles-Morin/9781572301207/reviews.
- Morin CM, Jarrin DC, 2013. Epidemiology of insomnia. Sleep Med. Clin. 8 (3), 281–297. doi: 10.1016/j.jsmc.2013.05.002. [DOI] [PubMed] [Google Scholar]
- Nakajima S, Okajima I, Sasai T, Kobayashi M, Furudate N, Drake CL, … Inoue Y, 2014. Validation of the Japanese version of the Ford insomnia response to stress test and the association of sleep reactivity with trait anxiety and insomnia. Sleep Medicine 15 (2), 196–202. doi: 10.1016/j.sleep.2013.09.022. [DOI] [PubMed] [Google Scholar]
- Needles DJ, Abramson LY, 1990. Positive life events, attributional style, and hopefulness: testing a model of recovery from depression. J. Abnorm. Psychol. 99 (2), 156–165. doi: 10.1037/0021-843x.99.2.156. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, 1997. Prevalence of DSM-IV diagnostic criteria of insomnia: distinguishing insomnia related to mental disorders from sleep disorders. J. Psychiatr. Res. 31 (3), 333–346. doi: 10.1016/S0022-3956(97)00002-2. [DOI] [PubMed] [Google Scholar]
- Perlis ML, Giles DE, Buysse DJ, Tu X, Kupfer DJ, 1997. Self-reported sleep disturbance as a prodromal symptom in recurrent depression – google scholar. J. Affect. Disord. 42 (2–3), 209–212. Retrieved from http://psycnet.apa.org/record/1997-06526-013. [DOI] [PubMed] [Google Scholar]
- Perlis ML, Shaw PJ, Cano G, Espie CA, 2011. Models of insomnia. In: Kryger MH, Roth T, Dement WC (Eds.), Principles and Practice of Sleep Medicine, pp. 850–865. doi: 10.1016/B0-7216-0797-7/X5001-0. [DOI] [Google Scholar]
- Peterson C, Semmel A, von Baeyer C, Abramson LY, Metalsky GI, Seligman MEP, 1982. The attributional style questionnaire. Cognit. Ther. Res. 6 (3), 287–299. doi: 10.1007/BF01173577. [DOI] [Google Scholar]
- Radloff LS, 1977. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1 (3), 385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Sobel M, 1982. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol. Methodol. 13, 290–312, [Google Scholar]
- Staner L, 2010. Comorbidity of insomnia and depression. Sleep Med. Rev. 14 (1), 35–46. doi: 10.1016/j.smrv.2009.09.003. [DOI] [PubMed] [Google Scholar]
- Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ, 2005. Epidemiology of insomnia, depression, and anxiety. Sleep 28 (11), 1457–1464. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- Vargas I, Friedman NP, Drake CL, 2015. Vulnerability to stress-related sleep disturbance and insomnia: investigating the link with comorbid depressive symptoms. Transl. Issues Psychol. Sci. 1 (1), 57–66. doi: 10.1016/j.biotechadv.2011.08.021.Secreted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilagut G, Forero CG, Barbaglia G, Alonso J, 2016. Screening for depression in the general population with the center for epidemiologic studies depression (CES-D): a systematic review with meta-analysis. PLoS One 11 (5), 1–17. doi: 10.1371/journal.pone.0155431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C-M, Chou CP-W, Hsiao F-C, 2011. The association of dysfunctional beliefs about sleep with vulnerability to stress-related sleep disturbance in young adults. Behav. Sleep Med. 9 (2), 86–91. doi: 10.1080/15402002.2011.557990. [DOI] [PubMed] [Google Scholar]