Abstract
Previously incarcerated persons with substance use disorder (SUD) need recovery supports, given the overrepresentation of this population in prison and community supervision. Peer support programs have the potential to fill gaps in postrelease support for persons with SUD. To assess the effectiveness of peer support approaches, this pilot study randomized access to peer recovery coaches within a well-established community reentry program. We examined several proximal outcomes to determine potential mechanisms of action, along with several exploratory outcomes. While attrition due to re-incarceration, death, and program disengagement was high, our findings suggest that those who received peer recovery coach support in the reentry program had recovery-based improvements, including improved self-reported mental and physical health and reductions in substance use behaviors. The treatment group also saw improvements in measures of treatment motivation and self-efficacy. Both groups saw similar positive trends in some outcomes, likely due to the relative success of the well-established reentry program regardless of the inclusion of peer support coaches. This study contributes lessons learned and potential mechanisms of action to limited research on the effectiveness of peer recovery supports for reentry populations with SUD.
Keywords: Peer recovery coach, Reentry, Substance use treatment
1. Introduction
The U.S. prison incarceration rate is the highest in the world (World Prison Brief et al., 2018), and the process of community reintegration impacts more than 600,000 adults who are released from prison per year, many of whom are surveilled by community supervision agents (probation or parole) for an extended period of time (U.S. Department of Health and Human Services, 2015). Among this population, persons with substance use disorder (SUD) are extremely overrepresented, as misconduct related to an SUD (i.e., relapse) is one of the primary reasons for re-incarceration (Binswanger et al., 2007; Chandler et al., 2009; The Council of State Governments, 2019). Prisons are not equipped to address the reentry needs of detainees with SUD (Binswanger, 2013; Bronson et al., 2017; Bronson & Berzofsky, 2017; Centers for Disease Control & Prevention, 2015; Maruschak & Berzofsky, 2016; Maruschak & Bronson, 2017; Pizzicato et al., 2018; Ranapurwala et al., 2018). As a result, this population has a high mortality rate in the period immediately following release (Binswanger, 2013; Pizzicato et al., 2018; Ranapurwala et al., 2018).
Ongoing recovery support is necessary for reentry populations with SUD, and peer recovery supports have potential to fill this gap. The peer support workforce consists of current or former clients of behavioral health services who often go by titles such as peer provider, peer support specialist, or peer recovery coach (PRC) and typically engage with individuals with SUD and/or mental illness who face personal recovery barriers. Peer services have been expanding within the U.S. SUD treatment field for the past 20 years (Gagne et al., 2018; Kelly et al., 2019). This expansion coincides with a broader shift from an acute SUD care to a recovery-oriented approach based on the chronic disease model that focuses on long-term services and supports in the community that are consistent with client goals (Humphreys & Tucker, 2002; Institute of Medicine, 2006; Laudet & Humphreys, 2013; White et al., 2003; White, 2009). Many states have developed a PRC certification process to better integrate this workforce into behavioral health systems to bridge clinical and community services (White, 2009) and to engage clients in care (Pfeiffer et al., 2012).
Peer services are a promising approach, as research suggests increased adherence to SUD treatment and reduced hospitalizations for those who receive peer supports (Boisvert et al., 2008; Cos et al., 2019; Min et al., 2007; O’Connell et al., 2017; Reingle Gonzalez, 2019; Rowe et al., 2007; Tracy et al., 2011). However, systematic reviews have pointed to a lack of rigorous designs in peer-intervention studies (Bassuk et al., 2016; Eddie et al., 2019; Reif et al., 2014), with much of the prior research being focused on clients with SUD or serious mental illness already living in the community (Armitage et al., 2010; Ashford et al., 2018; Cabassa et al., 2017; Miler et al., 2020; Stubbs et al., 2016; Waye et al., 2019), rather than those returning from incarceration. Returning citizens face a number of additional obstacles, including employment, housing, unmet medical needs, weak social ties (Carson & Sabol, 2012; Khan & Epperson, 2012; Travis et al., 2003; Visher et al., 2004), as well as discrimination and anticipated stigma (LeBel, 2008, 2012; LeBel et al., 2014; Pager, 2003; Winnick & Bodkin, 2008), that contribute to poor treatment retention (Mallik-Kane & Visher, 2008; Morenoff & Harding, 2014). While several jurisdictions have started to utilize peers with those formerly incarcerated as part of reentry planning (Curtis et al., 2018; The Federal Interagency Reentry Council, 2016), the program designs vary dramatically—often without a specific population focus (i.e., SUD or SMI)—and often lack methodological rigor necessary to determine efficacy (Marlow et al., 2015; Randall & Ligon, 2014; Reingle Gonzalez, 2019; Reingle Gonzalez et al., 2019; Salem et al., 2017).
The pilot study described in this paper was for an intervention called Substance Use Programming for Person-Oriented Recovery and Treatment (SUPPORT), which is a peer service model developed to address the need for ongoing recovery support for persons with an SUD who are reintegrating into the community following release from jail or prison. SUPPORT provides client-focused, strength-based addiction care through a network of comprehensive treatment and recovery supports (Halvorson et al., 2009; Laudet, 2008). The model consists of state-certified peer recovery coaches (PRCs) who provide nonclinical services (e.g., mentoring, support groups, employment assistance, and/or housing services) and recovery-oriented treatment planning to align services with client goals; SUPPORT also provides vouchers to fund services and supports that are aligned with client recovery goals (see Watson et al., 2017). Limited research on the efficacy of PRCs has been conducted with reentry populations with SUD; partially because of the difficulties of longitudinal clinical research designs with this hard-to-reach population. Therefore, one of the goals of SUPPORT’s early-stage work was to successfully complete a pilot randomized controlled trial (RCT) of the intervention: here we examine the proximal outcomes of the intervention (i.e., potential mechanisms of action, such as increased self-determination, motivation, and self-efficacy) as well as the primary outcomes related to substance use and quality of life.
2. Methods
2.1. Participants and randomization procedures
Research staff recruited clients into the study upon clients’ enrollement in services at Public Advocates in Community Re-Entry (PACE)—a nonprofit organization that provides community-based services to previously incarcerated individuals in Marion County, Indiana, the largest county in the state and home to Indianapolis, the state capital. Persons with at least one felony or five misdemeanors are eligible to receive PACE services. From October 2017 through December 2018, clients over the age of 18 who had an SUD and had been released from jail or prison within the three months prior were eligible for study participation and recruited from orientation meetings (clients who were on parole, probation, or home detention were still eligible for study participation). Research assistants confirmed eligibility and informed clients about the SUPPORT program services, then, for those who agreed to participate, obtained informed consent and notified them of arm assignment. The project manager (LRT) predetermined randomization with oversight from one of the lead investigators (DPW), using a computer-generated simple randomization schedule that assigned predetermined sequential participant identification numbers to one of the two study arms (Haahr, 2020). A card containing arm assignment details remained inside a sealed envelope stored within the packet and remained unopened until consent was completed. Finally, to help locate participants for follow-up data collection, researchers collected an address, email address, and phone number for each participant as well as contact information for two close family members or friends.
The study conducted interviews with participants at baseline (i.e., the day participants first enrolled in servies at PACE, which could have been at any point from one day to three months after release), and again at 6 and 12 months following baseline. Researchers began contacting participants one month prior to their follow-up date. All 6-month data collection occurred between May 2018 and May 2019, and all 12-month data collection occurred between September 2018 and November 2019. Study staff contacted participants (or their friends/family members) up to five times at each follow-up time point, through either phone or email, before determining them to be unreachable. The study collected all data through structured, 60–90-minute computer-assisted personal interviews (CAPI) (Gravlee, 2002; Webb et al., 1999) in the Research Electronic Data Capture (REDCap) system (Harris et al., 2009). Participants received $60 for each completed interview; the study also entered them into a drawing for one of two $100 gift cards at each data collection point. Researchers were also able to collect administrative data not collected in the CAPI from PACE and local publicly available administrative criminal records databases. An academic university Institutional Review Board approved all study procedures (Protocol Number: 1511731907), and we preregistered the study with ClinicalTrials.gov (Clinical Trials ID: NCT03132753 and Protocol Number: 1511731907).
2.2. Intervention
The study offered participants assigned to the experimental arm 12 months of SUPPORT services with a trained PRC to offer guidance, support, and coordination of treatment services, as well as $700 in vouchers to cover the cost of the additional flexible recovery support services that could not be covered by other funding sources (e.g., housing [permanent and transitional], employment services [training, placement, and readiness], substance use treatment, transportation, childcare, educational or vocational services, and aftercare planning). The PRC was responsible for tracking voucher spending as they assisted clients in choosing appropriate services and monitoring service completion over the 12 months of the intervention. The frequency and length of meetings with the PRC were individualized, based on individual client needs and preferences. The treatment as usual (TAU) arm did not receive PRC services or vouchers; however, participants in both arms could access PACE’s standard substance use counseling and case management services. This study hypothesized SUPPORT intervention to increase choice and options available to clients through its expanded infrastructure and flexible services, thereby improving agency in recovery and motivation to participate in treatment and supportive services (i.e., recovery capital), which should reduce relapse (Watson et al., 2017).
2.3. Measures
Given the pilot nature of the study, we examined several proximal outcomes as likely potential mechanisms of action, along with several exploratory outcomes. We assessed agency using the Self-Determination Scale (Sheldon, 1995) subscale on perceived choice, which presents participants with opposing statements labeled A and B (e.g., “I always feel like I choose the things I do” and “I sometimes feel that it’s not really me choosing the things I do”) and asked them to rate each on a Likert scale ranging from 1 (only “A” feels true) to 5 (only “B” feels true). Treatment Motivation Questionnaire (Ryan et al., 1995) is a 26-item instrument with three subscales (external, internal, and help seeking) that measures attitudes about treatment and reasons for entering the treatment by asking the respondent to indicate how true each statement is (1 = not at all true to 7 = very true). General Self-Efficacy Adult Protocol (Schwarzer & Jersusalem, 1995) measures perceptions about overcoming challenges and accomplishing life goals with items measured on a 4-point scale (1 = not at all true to 4 = exactly true) and summed for a composite score.
We explored several outcomes that might be associated with peer supports among returning citizens with SUD. Our primary outcome was self-reported substance use and abstinence, which the study measured using 12 items from the National Survey on Drug Use and Health (Substance Abuse and Mental Health Services Administration, 2014) on the frequency of use for tobacco, alcohol, sedative, tranquilizers, painkillers, stimulants, marijuana, cocaine, crack, hallucinogens, inhalants, heroin, and prescription medications. We were interested both in measuring progress toward recovery as well as a global indicator of quality of life as secondary outcomes. The study assessed recovery progress with the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) (Burrow-Sanchez & Lundberg, 2007; Miller & Tonigan, 1996; Mitchell & Angelone, 2006), a 19-item instrument that assesses readiness to change behaviors in relation to substance use by asking the respondent to indicate level of agreement from 1 (No! strongly disagree) to 5 (Yes! strongly agree). We used the Quality of life scale, a 4-item measure developed by the CDC, to measure perceived health-related (both mental and physical) quality of life in the past 30 days (Centers for Disease Control and Prevention, 2000).
2.4. Statistical analysis
We first compared participant characteristics at baseline, where we summarized categorical variables, using frequencies and proportions, and we summarized continuous variables using median and interquartile range (IQR) or mean and standard deviation (SD). Next we examined the attrition rates and assessed whether the SUPPORT arm had a different attrition rate than the TAU arm. The study compared the proportions of particpants missing their 6-month interview between intervention arms, and the study examined baseline characteristics associated with attrition using univariable logistic regression with stepwise variable selection. We focused on the attrition at 6 months because fewer participants completed their 12-month interview, making it difficult to investigate the difference in participant characteristics for those with and without complete 12-month data.
For both proximal outcomes and study outcomes, we examined changes from baseline to 6 months and from baseline to 12 months. For continuous outcomes, we summarized changes within each intervention arm using mean (SD) or interquartile rate (IQR) and evaluated them using the paired-t test or Wilcoxon signed rank test. The study performed between-arm comparisons of the changes using the two-sample t-test or Wilcoxon rank sum test. Prior to the study, the intervention effect size was estimated using the Cohen’s d to determine that 80 participants would suffice to detect meaningful differences in susbtance use; we based this dertermination on an assumption that the standard deviation of days of illict drug use was nine, which was derived from SUPPORT’s predecessor study (Ray et al., 2017). These analyses excluded participants with incomplete follow-up visits and hence produced valid inference when data were missing completely at random. As a sensitivity analysis, we used the constrained longitudinal data analysis (cLDA) to analyze the changes in these outcomes within and between intervention arms. The study used the cLDA because of its flexibility and efficiency in handling repeated measures and missing data with valid inference when data were missing at random. For binary outcomes, the study evaluated changes over time within an intervention arm and comparison of the changes between the two intervention arms using the exact conditional logistic regression due to the small sample size. The study examined appropriate functional forms of continuous variables using the locally estimated scatter plot smoothing (LOESS) method where appropriate. All statistical tests were two-sided and the study considered p-values < .05 statistically significant. Study staff performed analyses using SAS software (version 9.4, The SAS Institute, Cary, NC).
3. Results
3.1. Sample characteristics and attrition
Between October 2017 and December 2018, the study screened a total of 762 participants, of whom 110 were eligible and 100 agreed to participate in the study. The study randomized forty-six participants to the SUPPORT arm and 54 to the TAU arm (see Figure 1 CONSORT Flow Diagram for transparent reporting of randomized control trials) (CONSORT, n.d.). Table 1 displays sample characteristics at baseline. Among the SUPPORT arm, 41% (n=19) completed 6-month follow-up and 28% (n=13) completed 12-month follow-up. These rates were statistically similar to the TAU group, with 41% (n=22) completing the 6-month follow-up and 37% (n=20) completing the 12-month follow-up.
Figure 1:
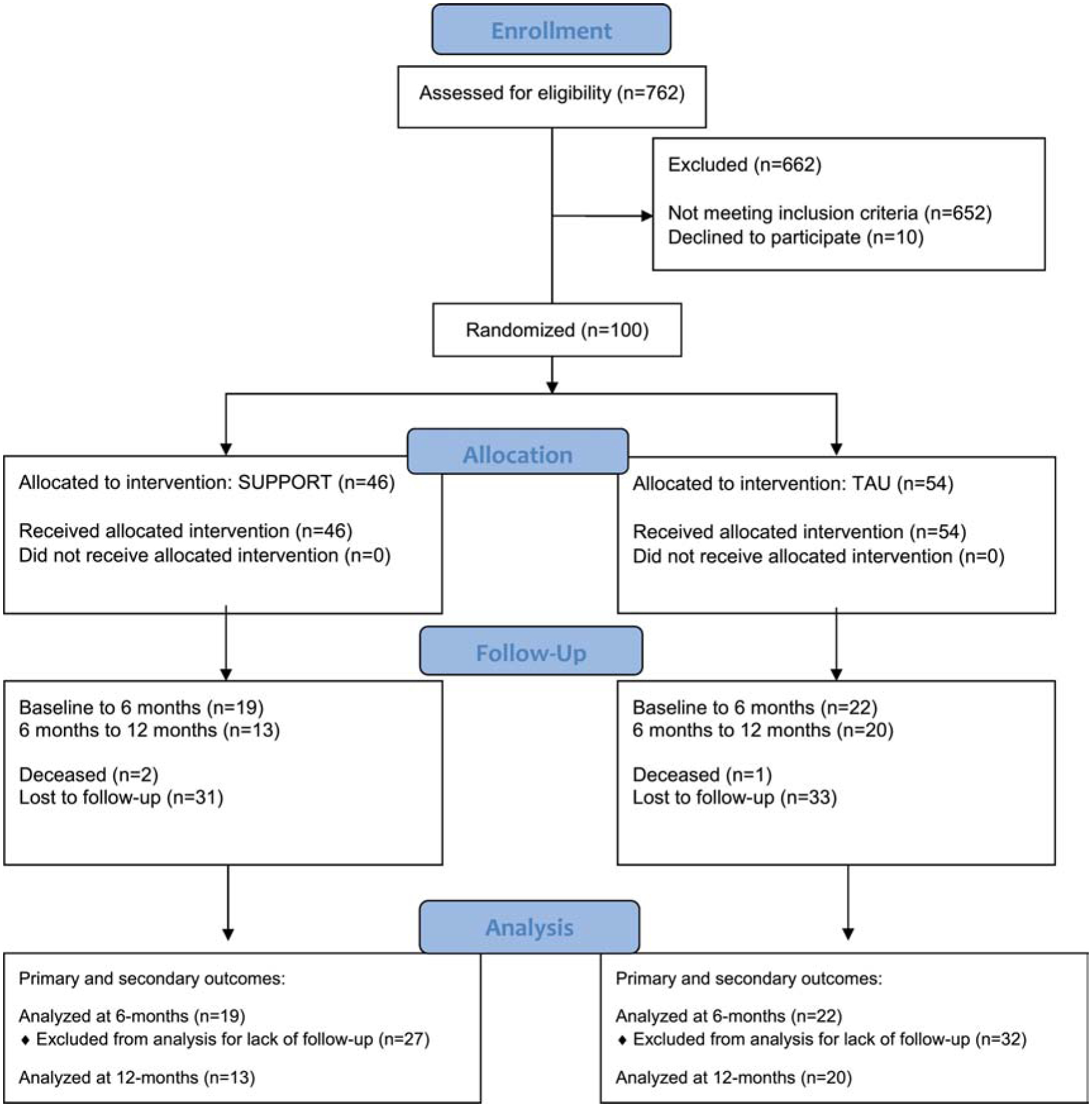
CONSORT 2010 Flow Diagram
Table 1.
SUPPORT baseline characteristics
| Total (n = 100) | Support (n = 46) | TAU (n = 54) | |
|---|---|---|---|
| Age in years, mean (sd) | 38.5 (10.4) | 39.0 (8.9) | 38.1 (11.6) |
| Female gender | 42% | 44% | 41% |
| Hispanic ethnicity | 3% | 4% | 2% |
| Race | |||
| White | 60% | 65% | 56% |
| Black or African American | 36% | 26% | 44% |
| Multiracial | 4% | 9% | |
| Sexual orientation | |||
| Straight | 92% | 89% | 94% |
| Gay/Lesbian | 4% | 7% | 2% |
| Bisexual | 3% | 2% | 4% |
| Don’t know/Not sure | 1% | 2% | 0% |
| Served in military | 4% | 2% | 6% |
| Living | |||
| Shelter | 16% | 17% | 15% |
| Street/Outdoors | 3% | 4% | 2% |
| Institution | 10% | 9% | 11% |
| Housed: own | 12% | 11% | 13% |
| Housed: someone else’s | 23% | 20% | 26% |
| Housed: halfway house | 14% | 20% | 9% |
| Housed: residential treatment | 18% | 13% | 22% |
| Housed: other | 4% | 7% | 2% |
| Satisfaction with living condition | |||
| Very dissatisfied | 2% | 26% | 22% |
| Dissatisfied | 18% | 24% | 13% |
| Neither satisfied nor dissatisfied | 18% | 13% | 2% |
| Satisfied | 24% | 22% | 26% |
| Very satisfied | 16% | 15% | 17% |
| Has children | 70% | 70% | 70% |
| Number of children, median (IQR) | 2.0 (0.0 – 3.0) | 2.0 (0.0 – 3.0) | 1.0 (0.0 – 3.0) |
| Education level | |||
| Lower than high school | 20% | 20% | 20% |
| High school/GED | 4% | 46% | 44% |
| College or above | 35% | 35% | 35% |
| Employed currently | 12% | 13% | 11% |
| Received income in past 30 days | 17% | 13% | 20% |
| Enough money to meet needs | |||
| Not at all | 66% | 70% | 63% |
| A little | 18% | 13% | 22% |
| Moderately | 6% | 7% | 6% |
| Mostly | 8% | 9% | 7% |
| Completely | 2% | 2% | 2% |
| Arrested in past 30 days | 13% | 20% | 7% |
| Drug-related arrest in past 30 days | 6% | 9% | 4% |
| Days of experiencing serious depression in past 30 days not due to use of alcohol or drug | |||
| 0 days | 34% | 27% | 41% |
| 1+ days | 66% | 73% | 59% |
| Days of experiencing anxiety or tension in past 30 days not due to use of alcohol or drug | |||
| 0 days | 29% | 24% | 34% |
| 1+ days | 71% | 76% | 66% |
Although there was no difference in the 6- or 12-month attrition rates between the arms, univariable logistic regression predicting 6-month follow-up suggests participants with greater confidence in treatment motivation were more likely to remain in the study, with a 35% lower odds of attrition for each unit increase in the TMQ-confidence subscale score (OR=0.65; 95% CI = 0.45–0.96, p=0.031; Table 2). Participants with more recent release from the criminal justice system were less likely to remain in the study, with a 5% lower odds of missing the 6-month assessment for every additional day between release and study enrollment (OR=0.949; 95% CI=0.905–0.996, p=0.035), which leveled off when participants were enrolled more than 30 days after the most recent release.
Table 2.
Association between baseline sample characteristics and follow-up attrition
| Variable | Missing 6-month follow-up visit | Univariable association | Multivariable association | |||
|---|---|---|---|---|---|---|
| Yes (n = 59) | No (n = 41) | OR (95% CI) | P value | OR (95% CI) | P value | |
| Intervention | ||||||
| TAU | 32 (54.2%) | 22 (53.7%) | 1 | |||
| SUPPORT | 27 (45.8%) | 19 (46.3%) | 0.98 (0.44, 2.17) | 0.95 | ||
| Age, mean (sd) | 37.0 (9.8) | 40.6 (11.0) | 0.967 (0.929, 1.006) | 0.092 | ||
| Days from release to enrollment, median (IQR) | 18.0 (13.0 – 34.0) | 29.0 (17.0 – 46.0) | 0.955 (0.912, 1.000) | 0.051 | 0.949 (0.905, 0.996) | 0.035 |
| Gender | ||||||
| Male | 34 (57.6%) | 24 (58.5%) | 0.96 (0.43, 2.16) | 0.93 | ||
| Female | 25 (42.4%) | 17 (41.5%) | 1 | |||
| Race | ||||||
| White | 36 (61.0%) | 24 (58.5%) | 1 | |||
| Black or African American | 20 (33.9%) | 16 (39.0%) | 0.83 (0.36, 1.92) | 0.67 | ||
| Multiracial | 3 (5.1%) | 1 (2.4%) | 1.57 (0.17, 14.14) | 0.69 | ||
| Any alcohol | ||||||
| No | 47 (79.7%) | 36 (87.8%) | 1 | |||
| Yes | 12 (20.3%) | 5 (12.2%) | 1.84 (0.59, 5.69) | 0.29 | ||
| Any opiates | ||||||
| No | 52 (88.1%) | 38 (92.7%) | 1 | |||
| Yes | 7 (11.9%) | 3 (7.3%) | 1.70 (0.41, 7.02) | 0.46 | ||
| Any illegal drug | ||||||
| No | 44 (74.6%) | 34 (82.9%) | 1 | |||
| Yes | 15 (25.4%) | 7 (17.1%) | 1.66 (0.61, 4.51) | 0.32 | ||
| Living satisfaction | ||||||
| Very dissatisfied | 15 (25.4%) | 9 (22.0%) | 1 | |||
| Dissatisfied | 9 (15.3%) | 9 (22.0%) | 0.60 (0.17, 2.07) | 0.42 | ||
| Neither Satisfied or Dissatisfied | 11 (18.6%) | 7 (17.1%) | 0.94 (0.27, 3.32) | 0.93 | ||
| Satisfied | 12 (20.3%) | 12 (29.3%) | 0.60 (0.19, 1.90) | 0.38 | ||
| Very Satisfied | 12 (20.3%) | 4 (9.8%) | 1.80 (0.44, 7.31) | 0.41 | ||
| Any children | ||||||
| No | 19 (32.2%) | 11 (26.8%) | 1 | |||
| Yes | 40 (67.8%) | 30 (73.2%) | 0.77 (0.32, 1.86) | 0.56 | ||
| Number of children, median (IQR) | 2.0 (0.0 – 3.0) | 1.0 (0.0 – 4.0) | 0.95 (0.76, 1.18) | 0.63 | ||
| Education | ||||||
| Less than high school | 14 (23.7%) | 6 (14.6%) | 1 | |||
| College or above | 21 (35.6%) | 14 (34.1%) | 0.64 (0.20, 2.07) | 0.46 | ||
| High school/GED | 24 (40.7%) | 21 (51.2%) | 0.49 (0.16, 1.50) | 0.21 | ||
| Employment | ||||||
| No | 52 (88.1%) | 36 (87.8%) | 1 | |||
| Yes | 7 (11.9%) | 5 (12.2%) | 0.97 (0.29, 3.30) | 0.96 | ||
| Any income | ||||||
| No | 49 (83.1%) | 34 (82.9%) | 1 | |||
| Yes | 10 (16.9%) | 7 (17.1%) | 0.99 (0.34, 2.86) | 0.99 | ||
| Any arrested | ||||||
| No | 50 (84.7%) | 37 (90.2%) | 1 | |||
| Yes | 9 (15.3%) | 4 (9.8%) | 1.66 (0.48, 5.82) | 0.42 | ||
| Tested HIV | ||||||
| No | 5 (8.5%) | 4 (9.8%) | 1 | |||
| Yes | 54 (91.5%) | 37 (90.2%) | 1.17 (0.29, 4.64) | 0.83 | ||
| Any depression | ||||||
| No | 18 (30.5%) | 16 (40.0%) | 1 | |||
| Yes | 41 (69.5%) | 24 (60.0%) | 1.52 (0.65, 3.52) | 0.33 | ||
| Any anxiety | ||||||
| No | 16 (27.6%) | 13 (31.7%) | 1 | |||
| Yes | 42 (72.4%) | 28 (68.3%) | 1.22 (0.51, 2.92) | 0.66 | ||
| Self-determination scale-perceived choice, median (IQR) | 3.8 (3.2 – 4.2) | 3.6 (2.8 – 4.4) | 1.10 (0.74, 1.64) | 0.65 | ||
| Treatment motivation, median (IQR) | ||||||
| External reasons | 2.5 (1.0 – 4.3) | 2.3 (1.3 – 3.3) | 1.15 (0.90, 1.47) | 0.26 | ||
| Internalized reasons | 6.3 (5.3 – 6.7) | 6.3 (5.5 – 7.0) | 0.84 (0.56, 1.27) | 0.41 | ||
| Help seeking | 6.0 (4.7 – 7.0) | 6.0 (5.0 – 7.0) | 0.96 (0.71, 1.31) | 0.81 | ||
| Confidence | 6.4 (4.6 – 7.0) | 6.8 (5.8 – 7.0) | 0.68 (0.47, 0.99) | 0.044 | 0.654 (0.445, 0.961) | 0.031 |
| General self-efficacy - sum, median (IQR) | 32.0 (29.0 – 36.0) | 32.0 (29.0 – 34.0) | 1.04 (0.96, 1.12) | 0.37 | ||
3.2. Potential mechanisms (proximal outcomes) from SUPPORT
We explored changes in self-determination, treatment motivation, and self-efficacy between baseline and follow-up to assess whether the intervention may have affected these potential mechanims. At 6-month follow-up the external motivation scores were significantly improved for the SUPPORT arm (mean=0.76; 95% CI=0.002–1.52; p=0.049), but not for the TAU arm. Although the between-group comparison did not show statistical significance (p=0.11), the effect size of 0.52 using Cohen’s d revealed a moderate difference between the two arms. At 12 months, the perceived choice scores in self-determination scale increased among the TAU arm (mean=0.36; 95% CI=0.01–0.71; p=0.044). During that same period, the SUPPORT arm had significant within-group increases in general self-efficacy scores (mean=5; 95% CI=0.55–9.45; p=0.031). For TAU, general self-efficacy scores trended toward a significant increase from baseline to the 12-month follow-up (mean=1.85; 95% CI= −0.03–3.73; p=0.053). Results also showed no significant within-group changes in other proximal outcomes, nor were there any between-group differences. The cLDA showed similar results with no significant difference between intervention arms.
3.3. SUPPORT outcomes
The use of alcohol or illegal drugs decreased from 30% at baseline to 16% at 6 months for SUPPORT arm participants, whereas in the TAU arm, the percentages were 26% at baseline and 41% at 6 months (Table 4). These changes were not statistically significant, nor was the comparison of temporal trend between arms. There was a slight increase in the use of alcohol or illegal drugs at 12 months compared to 6 months in both treatment arms (16% to 23% for the SUPPORT and 41% to 42% for the TAU).
Table 4.
Changes in primary outcome (presence of alcohol and illegal drug use in past 30 days) between baseline, 6 months and 12 months
| Use of Alcohol | Use of Illegal drug | Use of Alcohol or drugs | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | 0 days | 1 to 30 days | P Value for change relative to baseline | 0 days | 1 to 30 days | P Value for change relative to baseline | 0 days | 1 to 30 days | P Value for change relative to baseline | ||
| SUPPORT | Baseline | 46 | 38 (82.6%) | 8 (17.4%) | - | 35 (76.1%) | 11 (23.9%) | - | 32 (69.6%) | 14 (30.4%) | - |
| 6 months | 19 | 18 (94.7%) | 1 (5.3%) | 1 | 17 (89.5%) | 2 (10.5%) | 1 | 16 (84.2%) | 3 (15.8%) | 1 | |
| 12 months | 13 | 13 (100%) | 0 (0%) | 0.75 | 10 (76.9%) | 3 (23.1%) | 1 | 10 (76.9%) | 3 (23.1%) | 1 | |
| TAU | Baseline | 54 | 45 (83.3%) | 9 (16.7%) | - | 43 (79.6%) | 11 (20.4%) | - | 40 (74.1%) | 14 (25.9%) | - |
| 6 months | 22 | 14 (63.6%) | 8 (36.4%) | 0.11 | 21 (95.5%) | 1 (4.5%) | 0.13 | 13 (59.1%) | 9 (40.9%) | 0.32 | |
| 12 months | 19 | 11 (57.9%) | 8 (42.1%) | 0.11 | 17 (89.5%) | 2 (10.5%) | 0.63 | 11 (57.9%) | 8 (42.1%) | 0.32 | |
The SOCRATES readiness for change scores within the SUPPORT arm had a significant (p = 0.03) decrease in their recognition scores from baseline to the 6-month follow-up (mean= −1.9; 95% CI= −3.7 to −0.1; p=0.044) (Table 5). At 12 months, those in the SUPPORT arm had a significantly lower recognition score (mean change= −5.8, 95% CI= −10.1 to −1.6; p=0.013) and a lower ambivalence score (mean change= −4.9; 95% CI= −7.4 to −2.4; p=0.001). However, between-group differences did not occur in these outcomes. The study found similar results based on the cLDA, which showed no significant difference between intervention arms.
Table 5.
Changes in secondary outcomes (readiness to change behaviors in relation to substance use and quality of life) between baseline, 6 months and 12 months
| SUPPORT | USUAL | Difference between Intervention Arms | |||||
|---|---|---|---|---|---|---|---|
| Change since baseline, mean (sd) or median (IQR) | P Value | Change since baseline, mean (sd) or median (IQR) | P Value | Estimate (95% CI) | P Value | Cohen’s d | |
| Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) - Recognition | |||||||
| 6 months | −1.9 (3.8) | 0.044 | −1.4 (9.3) | 0.48 | −0.47 (−4.89, 3.95) | 0.83 | −0.06 |
| 12 months | −5.8 (6.4) | 0.013 | −5.3 (11.5) | 0.055 | −0.56 (−8.27, 7.15) | 0.88 | −0.06 |
| Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) - Ambivalence | |||||||
| 6 months | −1.5 (3.6) | 0.093 | −0.2 (4.8) | 0.85 | −1.28 (−4.00, 1.45) | 0.35 | −0.30 |
| 12 months | −4.9 (3.7) | 0.001 | −2.1 (6.1) | 0.14 | −2.81 (−6.93, 1.31) | 0.17 | −0.52 |
| Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) - Taking steps | |||||||
| 6 months | 0.3 (3.9) | 0.73 | −2.2 (6.6) | 0.13 | 2.54 (−0.86, 5.94) | 0.14 | 0.46 |
| 12 months | 0.3 (7.2) | 0.9 | −2.7 (5.8) | 0.053 | 2.94 (−1.91, 7.78) | 0.23 | 0.47 |
| Quality of life - General health | |||||||
| 6 months | 0.0 (0.0 – 10) | 1 | 0.0 (−1.0 – 0.0) | 1 | 0.05 (−0.45, 0.55) | 0.83 | 0.07 |
| 12 months | 0.0 (−1.0 – 0.0) | 1 | 0.0 (−1.0 – 0.0) | 0.18 | 0.32 (−0.34, 0.97) | 0.33 | 0.37 |
| Quality of life - Number of physically/mentally unhealthy days | |||||||
| 6 months | −1.0 (−10.0 – 9.0) | 0.57 | 0.0 (−15.0 – 0.0) | 0.024 | 4.23 (−4.35, 12.81) | 0.32 | 0.31 |
| 12 months | −2.0 (−30.0 – 4.0) | 0.22 | −2.0 (−16.0 – 4.0) | 0.11 | −4.11 (−17.03, 8.81) | 0.52 | −0.25 |
| Quality of life - Number of days that usual activities are prevented due to poor physical or mental health | |||||||
| 6 months | −2.5 (−7.0 – 2.0) | 0.11 | 0.0 (−13.0 – 0.0) | 0.002 | 3.04 (−3.53, 9.60) | 0.36 | 0.30 |
| 12 months | −4.0 (−7.0 – 0.0) | 0.055 | 0.0 (−20.0 – 0.0) | 0.023 | 3.78 (−3.21, 10.77) | 0.28 | 0.35 |
The ranges of SOCRATES scores are 7–35 for the Recognition subscale, 4–20 for the Ambivalence subscale, and 8–40 for the Taking Steps subscale. Higher values indicate greater recognition of problems, more openness to reflection, and greater readiness to change.
4. Discussion
The SUPPORT study implemented and conducted a pilot RCT of a community-based PRC model for persons returning from prison. While only a pilot, such methodological rigor has been largely absent in much of the PRC literature, particularly with justice-involved populations, and the lessons learned from this study can inform future work in this area. In particular, the pilot struggled with retention, as only one-third of participants completed a 12-month follow-up interview despite multiple follow-up attempts and incentives. However, while our attrition analysis is limited to measures available in the study, results do not suggest bias between treatment and TAU arms and are consistent with the earlier studies showing that those seeking behavioral health services with criminal records are less likely to be retained in studies (Claus et al., 2002; Coen et al., 1996; Crisanti et al., 2014; Western et al., 2016).
Study retention among those with behavioral health problems in community-based intervention settings is a persistent problem (Barry, 2005; Bucholz et al., 1996; Furimsky et al., 2008; Kanuch et al., 2016; Leonard et al., 2003; Sullivan et al., 1996). Participants are overwhelmed with meeting the basic requirements of daily life after returning from incarceration, including navigating compliance with criminal-legal and community-supervision systems to maintain freedom (Ortiz & Wrigley, 2020; The Council of State Governments, 2019; Visher et al., 2004). Retention can be especially difficult when participants are engaged in illegal activities or substance misuse, as relapse can result in suspicion or fear of researchers (Bucholz et al., 1996; Cottler et al., 1996; Lankenau et al., 2010; J. E. Ryan et al., 2019; Vaughn et al., 2002; Ziek et al., 1996).
The SUPPORT arm had recovery-based improvements that are consistent with other peer support studies with justice-involved populations (Bassuk et al., 2016; Prendergast et al., 2017; Reif et al., 2014). Specifically, the SUPPORT arm had improvements in treatment motivation external reasons (Cohen’s d=0.52 at 6 months) and general self-efficacy (Cohen’s d=0.62 at 12 months), which are mediating variables in the model underlying SUPPORT’s theorized mechanisms of change (Watson et al., 2017). As such, given the difficulties members of a reentry population face, a longer exposure to the intervention may result in a greater improvement in more distal outcomes like drug use and criminal behavior for the SUPPORT arm. Results regarding readiness to change were in the opposite direction of what we expected. Most noticeable was the significant decrease in recognition scores for the SUPPORT arm, which may be the result of limitations in using the SOCRATES instrument to measure changes over time (Miller & Tonigan, 1996). Furthermore, interpreting observed changes in SOCRATES scores is difficult considering a reduction in one domain can be interpreted as either positive or negative, depending on changes observed in the other domains (e.g., reduced recognition scores might not be undesirable if taking step scores improve). Thus, the positive changes in treatment motivation and self-efficacy are likely better proxies for understanding how SUPPORT participants’ readiness might have changed due to the intervention.
One reason for similar improvements in study arms could be a ceiling effect in the TAU experience. Prior research on returning inmates with SUD in this jurisdiction found clients in the study setting (PACE) had a considerably low recidivism rate (Ray et al., 2017). Those in the TAU arm received the standard services at an agency with seasoned professionals who had long standing relationships with local criminal-legal stakeholders. Indeed, TAU participants received access to myriad recovery-based social services within PACE, such as recovery support groups, high school equivalency courses, mental health coaching, therapy, employment coaching, and coordinated case manager. Thus, PRCs and vouchers might not add to an already rich service environment.
This ceiling effect speaks to the variation in the quality of care that is likely to impact peer engagement efforts, as peers working with providers or in communities with better services might have more success with client engagement. Rigourous methodologies, like the randomization protocols used in this study, should examine these outcomes. This intervention studied PRCs for those with SUD returing from prison. Some recent PRC support models have focused specifically on jail populations (Bellamy et al., 2019; Morrison, 2016) and others have focused on developing rapport prior to release through in-reach efforts (Randall & Ligon, 2014; Reingle Gonzalez, 2019). Peers can engage with the justice-involved population in a number of ways, and at various points in the criminal-legal process, as evident by efforts to incorporate peers into law enforcement practices (Krider et al., 2020). Regardless of the approach, researchers should detail the specifics of the peer support model and conduct rigorous research to understand the effectiveness of these approaches.
5. Limitations
While this study demonstrates promising evidence of positive outcomes associated with SUPPORT, there are notable limitations. First, the findings are not generalizable given the limited sample size, setting, and specific justice-involved population. Further, the use of self-reported data collection may create bias in reporting results. One notable strength is that the study recruited one hundred clients for participation in this pilot, which is slightly above the high end of the range recommended for a minimally acceptable pilot sample (Lancaster et al., 2004; Sim & Lewis, 2012; Whitehead et al., 2016). Because this was a pilot study, its goal was to understand the feasibility of the intervention and the potential magnitude of the intervention’s effect on participant outcomes. However, the attrition rate on follow-up assessments suggests that we would not have been powered to detect longer-term outcomes. Based on results related to the primary outcomes, we project the sample size for the larger definitive trial would be 152 per intervention arm to achieve 80% power at the 5% significance level based on the two-sample z-test for the comparison of proportions in two independent samples, assuming the rate of alcohol or illegal drug use is 25% in the SUPPORT arm and 40% in the TAU arm. More frequent, ongoing contact and shorter follow-up windows have demonstrated success (Scott, 2004), but future studies may find it benefitial to have peer research assistants administer participant surveys in an attempt to improve rapport, empathy, and retention (Visher et al., 2004; Victor et al. 2020) Researchers should employ rigorous techniques to ensure adequate follow-up but also access to administrative-level data to adequately track re-incarceration systematicially.
6. Conclusion
Peer support services for those returning from incarceration with an SUD offers a promising community-based approach to improve treatment adherence and reduce harms associated with substance use. However, limited research has been conducted with and few have used longitudinal clinical research designs because the population is hard to reach. In this study of SUPPORT, we illustrate a feasible method of conducting an RCT for PRC services and in doing so highlight some of the lessons learned. Future research that continues to assess the effectiveness of peer supports with justice-involved populations should accurately detail in the literature the models used and evaluate peer supports using rigorous research methodologies.
Table 3.
Changes in possible mechanisms (proximal outcomes) between baseline, 6 months and 12 months
| SUPPORT | TAU | Difference between Intervention Arms | |||||
|---|---|---|---|---|---|---|---|
| Mean change since baseline (sd) | P Value | Mean change since baseline (sd) | P Value | Estimate (95% CI) | P Value | Cohen’s d | |
| Self Determination Scale-Perceived Choice | |||||||
| 6 months | 0.13 (1.13) | 0.63 | 0.30 (0.84) | 0.11 | −0.18 (−0.80, 0.45) | 0.57 | −0.18 |
| 12 months | 0.41 (1.31) | 0.30 | 0.36 (0.74) | 0.04 | 0.05 (−0.83, 0.93) | 0.90 | 0.05 |
| Treatment Motivation - External Reasons | |||||||
| 6 months | 0.76 (1.58) | 0.05 | 0.03 (1.23) | 0.90 | 0.73 (−0.16, 1.62) | 0.11 | 0.52 |
| 12 months | 0.14 (1.60) | 0.78 | −0.04 (1.90) | 0.93 | 0.17 (−1.21, 1.55) | 0.80 | 0.10 |
| Treatment Motivation - Internal Reasons | |||||||
| 6 months | −0.18 (0.76) | 0.33 | −0.26 (0.68) | 0.08 | 0.09 (−0.37, 0.54) | 0.69 | 0.25 |
| 12 months | −0.66 (1.34) | 0.11 | −0.40 (1.27) | 0.17 | −0.26 (−1.22, 0.70) | 0.59 | −0.20 |
| Treatment Motivation - Help Seeking | |||||||
| 6 months | 0.04 (0.64) | 0.81 | −0.19 (1.08) | 0.42 | 0.23 (−0.33, 0.78) | 0.41 | 0.12 |
| 12 months | −0.27 (1.21) | 0.47 | −0.06 (1.44) | 0.86 | −0.21 (−1.26, 0.83) | 0.68 | −0.16 |
| Treatment Motivation - Confidence | |||||||
| 6 months | −0.47 (1.36) | 0.15 | −0.25 (1.20) | 0.35 | −0.23 (−1.03, 0.58) | 0.58 | −0.18 |
| 12 months | −0.35 (1.39) | 0.43 | −0.72 (1.68) | 0.07 | 0.37 (−0.84, 1.59) | 0.53 | 0.24 |
| General Self-Efficacy - Sum | |||||||
| 6 months | 1.79 (4.94) | 0.13 | 1.50 (4.19) | 0.11 | 0.29 (−2.60, 3.17) | 0.84 | 0.06 |
| 12 months | 5.00 (6.62) | 0.03 | 1.85 (4.02) | 0.05 | 3.15 (−1.54, 7.84) | 0.17 | 0.62 |
Self-determination scale perceived choice scores range from 1 to 5, with higher values indicating greater levels of self-determination.
Treatment motivation scores range from 1 to 7, with higher values indicating greater treatment motivation.
General self-efficacy scale scores range from 10 to 40, with higher values indicating greater self-efficacy.
Highlights.
Studies of recovery coaching in the reentry settings have lacked methodological rigor
Researchers piloted an RCT of peer recovery coaching for recently incarcerated persons
Results show reduced drug use and increased self-efficacy and treatment motivation
This pilot study contributes to lessons learned for evaluating re-entry recovery coaching
Acknowledgements
This project was conducted in collaboration with the Central Indiana Recovery Services Coalition (CIRSC), which includes the member organizations Public Advocates in Community Re-Entry and Drug Free Marion County. This project would not be possible without the support of Indiana’s Division of Mental Health and Addiction, which provided initial funding for CIRSC’s work. The study was supported by the National Institute on Drug Abuse (R34DA041640). The content of this article is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Interest
None
References
- Armitage EV, Lyons H, & M. TL PHD (2010). Recovery Association Project (RAP), Portland, Oregon. Alcoholism Treatment Quarterly, 28(3), 339–357. 10.1080/07347324.2010.488539 [DOI] [Google Scholar]
- Ashford RD, Curtis B, & Brown AM (2018). Peer-delivered harm reduction and recovery support services: Initial evaluation from a hybrid recovery community drop-in center and syringe exchange program. Harm Reduction Journal, 15(1), 52. 10.1186/s12954-018-0258-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry AE (2005). How Attrition Impacts the Internal and External Validity of Longitudinal Research. Journal of School Health, 75(7), 267–270. 10.1111/j.1746-1561.2005.00035.x [DOI] [PubMed] [Google Scholar]
- Bassuk EL, Hanson J, Greene RN, Richard M, & Laudet A (2016). Peer-Delivered Recovery Support Services for Addictions in the United States: A Systematic Review. Journal of Substance Abuse Treatment, 63, 1–9. 10.1016/j.jsat.2016.01.003 [DOI] [PubMed] [Google Scholar]
- Bellamy C, Kimmel J, Costa MN, Tsai J, Nulton L, Nulton E, Kimmel A, Aguilar NJ, Clayton A, & O’Connell M (2019). Peer support on the “inside and outside”: Building lives and reducing recidivism for people with mental illness returning from jail. Journal of Public Mental Health, 18(3), 188–198. 10.1108/JPMH-02-2019-0028 [DOI] [Google Scholar]
- Binswanger IA (2013). Mortality After Prison Release: Opioid Overdose and Other Causes of Death, Risk Factors, and Time Trends From 1999 to 2009. Annals of Internal Medicine, 159(9), 592. 10.7326/0003-4819-159-9-201311050-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, & Koepsell TD (2007). Release from Prison—A High Risk of Death for Former Inmates. New England Journal of Medicine, 356(2), 157–165. 10.1056/NEJMsa064115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boisvert RA, Martin LM, Grosek M, & Clarie AJ (2008). Effectiveness of a peer-support community in addiction recovery: Participation as intervention. Occupational Therapy International, 15(4), 205–220. 10.1002/oti.257 [DOI] [PubMed] [Google Scholar]
- Bronson J, & Berzofsky M (2017). Indicators of Mental Health Problems Reported by Prisoners and Jail Inmates, 2011–12 (p. 17). US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics. [Google Scholar]
- Bronson J, Stroop J, Zimmer S, & Berzofsky M (2017). Drug Use, Dependence, and Abuse Among State Prisoners and Jail Inmates, 2007–2009 (p. 27). US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics. https://www.bjs.gov/content/pub/pdf/dudaspji0709.pdf [Google Scholar]
- Bucholz KK, Shayka JJ, Marion SL, Lewis CE, Pribor EF, & Rubio DM (1996). Is a history of alcohol problems or of psychiatric disorder associated with attrition at 11-year follow-up? Annals of Epidemiology, 6(3), 228–234. 10.1016/1047-2797(96)00002-6 [DOI] [PubMed] [Google Scholar]
- Burrow-Sanchez JJ, & Lundberg KJ (2007). Readiness to change in adults waiting for publicly funded substance abuse treatment. Addictive Behaviors, 32(1), 199–204. 10.1016/j.addbeh.2006.03.039 [DOI] [PubMed] [Google Scholar]
- Cabassa LJ, Camacho D, Vélez-Grau CM, & Stefancic A (2017). Peer-based health interventions for people with serious mental illness: A systematic literature review. Journal of Psychiatric Research, 84, 80–89. 10.1016/j.jpsychires.2016.09.021 [DOI] [PubMed] [Google Scholar]
- Carson EA, & Sabol W (2012). Prisoners in 2011. Bureau of Justice Statistics. https://www.bjs.gov/index.cfm?ty=pbdetail&iid=4559
- Centers for Disease Control & Prevention. (2015). Viral Hepatitis Surveillance—United States, 2015 (p. 73). https://www.cdc.gov/hepatitis/statistics/2015surveillance/pdfs/2015HepSurveillanceRpt.pdf
- Centers for Disease Control and Prevention. (2000). Measuring Healthy Days: Population Assessment of Health-Related Quality of Life (p. 44). US Department of Health and Human Services: National Center for Chronic Disease Prevention and Health Promotion-Division of Adult and Community Health. https://www.cdc.gov/hrqol/pdfs/mhd.pdf [Google Scholar]
- Chandler RK, Fletcher BW, & Volkow ND (2009). Treating Drug Abuse and Addiction in the Criminal Justice System: Improving Public Health and Safety. JAMA, 301(2), 183. 10.1001/jama.2008.976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claus RE, Kindleberger LR, & Dugan MC (2002). Predictors of Attrition in a Longitudinal Study of Substance Abusers. Journal of Psychoactive Drugs, 34(1), 69–74. 10.1080/02791072.2002.10399938 [DOI] [PubMed] [Google Scholar]
- Coen AS, Patrick DC, & Shern DL (1996). Minimizing attrition in longitudinal studies of special populations: An integrated management approach. Evaluation and Program Planning, 19(4), 309–319. 10.1016/S0149-7189(96)00024-9 [DOI] [Google Scholar]
- CONSORT. (n.d.). Retrieved September 21, 2020, from http://www.consort-statement.org/
- Cos TA, LaPollo AB, Aussendorf M, Williams JM, Malayter K, & Festinger DS (2019). Do Peer Recovery Specialists Improve Outcomes for Individuals with Substance Use Disorder in an Integrative Primary Care Setting? A Program Evaluation. Journal of Clinical Psychology in Medical Settings 10.1007/s10880-019-09661-z [DOI] [PubMed] [Google Scholar]
- Cottler LB, Compton WM, Ben-Abdallah A, Horne M, & Claverie D (1996). Achieving a 96.6 percent follow-up rate in a longitudinal study of drug abusers. Drug and Alcohol Dependence, 41(3), 209–217. 10.1016/0376-8716(96)01254-9 [DOI] [PubMed] [Google Scholar]
- Crisanti AS, Case BF, Isakson BL, & Steadman HJ (2014). Understanding Study Attrition in the Evaluation of Jail Diversion Programs for Persons With Serious Mental Illness or Co-Occurring Substance Use Disorders. Criminal Justice and Behavior, 41(6), 772–790. 10.1177/0093854813514580 [DOI] [Google Scholar]
- Curtis K, Forkey K, & Reynolds W (2018). Reentry: New Jersey Opioid Addiction Report: A Modern Plague. New Jersey Reentry Corporation. https://www.njreentry.org/application/files/4815/5924/0678/Published_9_24.pdf [Google Scholar]
- Eddie D, Hoffman L, Vilsaint C, Abry A, Bergman B, Hoeppner B, Weinstein C, & Kelly JF (2019). Lived Experience in New Models of Care for Substance Use Disorder: A Systematic Review of Peer Recovery Support Services and Recovery Coaching. Frontiers in Psychology, 10. 10.3389/fpsyg.2019.01052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furimsky I, Cheung AH, Dewa CS, & Zipursky RB (2008). Strategies to enhance patient recruitment and retention in research involving patients with a first episode of mental illness. Contemporary Clinical Trials, 29(6), 862–866. 10.1016/j.cct.2008.07.005 [DOI] [PubMed] [Google Scholar]
- Gagne CA, Finch WL, Myrick KJ, & Davis LM (2018). Peer Workers in the Behavioral and Integrated Health Workforce: Opportunities and Future Directions. American Journal of Preventive Medicine, 54(6, Supplement 3), S258–S266. 10.1016/j.amepre.2018.03.010 [DOI] [PubMed] [Google Scholar]
- Gravlee CC (2002). Mobile Computer-Assisted Personal Interviewing with Handheld Computers: The Entryware System 3.0. 14(3), 322–336. [Google Scholar]
- Halvorson A, Whitter M, & Taitt SB (2009). Approaches to recovery-oriented systems of care at the state and local levels: Three case studies. Substance Abuse and Mental Health Services Administration. http://www.williamwhitepapers.com/pr/ROSC%20Case%20Studies%202009.pdf [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K, & Tucker JA (2002). Toward more responsive and effective intervention systems for alcohol-related problems. Addiction, 97(2), 126–132. 10.1046/j.1360-0443.2002.00004.x [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2006). Improving the quality of health care for mental and substance use conditions. National Academy Press. [PubMed] [Google Scholar]
- Kanuch SW, Cassidy KA, Dawson NV, Athey M, Fuentes-Casiano E, & Sajatovic M (2016). Recruiting and Retaining Individuals with Serious Mental Illness and Diabetes in Clinical Research: Lessons Learned from a Randomized, Controlled Trial. Journal of Health Disparities Research and Practice, 9(3), 115–126. [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Abry AW, & Fallah-Sohy N (2019). Mutual Help and Peer Support Models for Opioid Use Disorder Recovery. In Kelly JF & Wakeman SE (Eds.), Treating Opioid Addiction (pp. 139–167). Springer International Publishing. 10.1007/978-3-030-16257-3_7 [DOI] [Google Scholar]
- Khan M, & Epperson M (2012). Disconnected. Incarceration cuts you off from your social network—And HIV thrives on that. Positively Aware: The Monthly Journal of the Test Positive Aware Network, 24(3), 36–37. [PubMed] [Google Scholar]
- Krider A, Huerter R, Gaherty K, & Moore A (2020). Responding to Individuals in Behavioral Health Crisis via Co-Responder Models: The Roles of Cities, Counties, Law Enforcement, and Providers (p. 13). National League of Cities. https://www.theiacp.org/sites/default/files/SJCResponding%20to%20Individuals.pdf [Google Scholar]
- Lancaster GA, Dodd S, & Williamson PR (2004). Design and analysis of pilot studies: Recommendations for good practice. Journal of Evaluation in Clinical Practice, 10(2), 307–312. 10.1111/j..2002.384.doc.x [DOI] [PubMed] [Google Scholar]
- Lankenau SE, Sanders B, Hathazi D, & Bloom JJ (2010). Recruiting and Retaining Mobile Young Injection Drug Users in a Longitudinal Study. Substance Use & Misuse, 45(5), 684–699. 10.3109/10826081003594914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB (2008). The road to recovery: Where are we going and how do we get there? Empirically driven conclusions and future directions for service development and research. Substance Use & Misuse, 43(12–13), 2001–2020. 10.1080/10826080802293459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, & Humphreys K (2013). Promoting recovery in an evolving policy context: What do we know and what do we need to know about recovery support services? Journal of Substance Abuse Treatment, 45(1), 126–133. 10.1016/j.jsat.2013.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBel TP (2008). Perceptions of and Responses to Stigma. Sociology Compass, 2(2), 409–432. 10.1111/j.1751-9020.2007.00081.x [DOI] [Google Scholar]
- LeBel TP (2012). Invisible Stripes? Formerly Incarcerated Persons’ Perceptions of Stigma. Deviant Behavior, 33(2), 89–107. 10.1080/01639625.2010.538365 [DOI] [Google Scholar]
- LeBel TP, Richie M, & Maruna S (2014). Helping Others as a Response to Reconcile a Criminal Past: The Role of the Wounded Healer in Prisoner Reentry Programs. Criminal Justice and Behavior. 10.1177/0093854814550029 [DOI] [Google Scholar]
- Leonard NR, Lester P, Rotheram-Borus MJ, Mattes K, Gwadz M, & Ferns B (2003). Successful Recruitment and Retention of Participants in Longitudinal Behavioral Research. AIDS Education and Prevention, 15(3), 269–281. 10.1521/aeap.15.4.269.23827 [DOI] [PubMed] [Google Scholar]
- Mallik-Kane K, & Visher C (2008). Health and Prisoner Reentry: How Physical, Mental, and Substance Abuse Conditions Shape the Process of Reintegration. Urban Institute Justice Policy Center. https://www.urban.org/research/publication/health-and-prisoner-reentry
- Marlow E, Grajeda W, Lee Y, Young E, Williams M, & Hill K (2015). Peer Mentoring for Male Parolees: A CBPR Pilot Study. Progress in Community Health Partnerships: Research, Education, and Action, 9(1), 91–100. 10.1353/cpr.2015.0013 [DOI] [PubMed] [Google Scholar]
- Maruschak LM, & Berzofsky M (2016). Medical Problems of State and Federal Prisoners and Jail Inmates, 2011–12 (p. 23). US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics. https://www.bjs.gov/content/pub/pdf/mpsfpji1112.pdf [Google Scholar]
- Maruschak LM, & Bronson J (2017). HIV in Prisons, 2015—Statistical Tables (p. 18). US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics. https://www.bjs.gov/content/pub/pdf/hivp15st.pdf [Google Scholar]
- Miler JA, Carver H, Foster R, & Parkes T (2020). Provision of peer support at the intersection of homelessness and problem substance use services: A systematic ‘state of the art’ review. BMC Public Health, 20(1), 641. 10.1186/s12889-020-8407-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, & Tonigan JS (1996). Assessing drinkers’ motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES). Psychology of Addictive Behaviors, 10(2), 81–89. 10.1037/0893-164X.10.2.81 [DOI] [Google Scholar]
- Min S-Y, Whitecraft J, Rothbard AB, & Salzer MS (2007). Peer Support for Persons with Co-Occurring Disorders and Community Tenure: A Survival Analysis. Psychiatric Rehabilitation Journal, 30(3), 207–213. 10.2975/30.3.2007.207.213 [DOI] [PubMed] [Google Scholar]
- Mitchell D, & Angelone DJ (2006). Assessing the validity of the Stages of Change Readiness and Treatment Eagerness Scale with treatment-seeking military service members. Military Medicine, 171(9), 900–904. 10.7205/milmed.171.9.900 [DOI] [PubMed] [Google Scholar]
- Morenoff JD, & Harding DJ (2014). Incarceration, Prisoner Reentry, and Communities. Annual Review of Sociology, 40(1), 411–429. 10.1146/annurev-soc-071811-145511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison S (2016). Recovery Coaches: Playing an Important Role in Marin County Collaborative Courts. Berkeley Mack Center, 8. [Google Scholar]
- O’Connell MJ, Flanagan EH, Delphin-Rittmon ME, & Davidson L (2017). Enhancing outcomes for persons with co-occurring disorders through skills training and peer recovery support. Journal of Mental Health, 0(0), 1–6. 10.1080/09638237.2017.1294733 [DOI] [PubMed] [Google Scholar]
- Ortiz JM, & Wrigley K (2020). The Invisible Enclosure: How Community Supervision Inhibits Successful Reentry. Corrections, 0(0), 1–16. 10.1080/23774657.2020.1768967 [DOI] [Google Scholar]
- Pager D (2003). The Mark of a Criminal Record. American Journal of Sociology, 108(5), 937–975. [Google Scholar]
- Pfeiffer PN, Blow AJ, Miller E, Forman J, Dalack GW, & Valenstein M (2012). Peers and Peer-Based Interventions in Supporting Reintegration and Mental Health Among National Guard Soldiers: A Qualitative Study. Military Medicine, 177(12), 1471–1476. 10.7205/MILMED-D-12-00115 [DOI] [PubMed] [Google Scholar]
- Pizzicato LN, Drake R, Domer-Shank R, Johnson CC, & Viner KM (2018). Beyond the walls: Risk factors for overdose mortality following release from the Philadelphia Department of Prisons. Drug and Alcohol Dependence, 189, 108–115. 10.1016/j.drugalcdep.2018.04.034 [DOI] [PubMed] [Google Scholar]
- Prendergast ML, McCollister K, & Warda U (2017). A randomized study of the use of screening, brief intervention, and referral to treatment (SBIRT) for drug and alcohol use with jail inmates. Journal of Substance Abuse Treatment, 74, 54–64. 10.1016/j.jsat.2016.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranapurwala SI, Shanahan ME, Alexandridis AA, Proescholdbell SK, Naumann RB, Edwards D, & Marshall SW (2018). Opioid Overdose Mortality Among Former North Carolina Inmates: 2000–2015. American Journal of Public Health, 108(9), 1207–1213. 10.2105/AJPH.2018.304514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall M, & Ligon K (2014). From Recidivism to Recovery: The Case for Peer Support in Texas Correctional Facilities. National Institute of Corrections. https://nicic.gov/recidivism-recovery-case-peer-support-texas-correctional-facilities [Google Scholar]
- Ray B, Grommon E, Buchanan V, Brown B, & Watson DP (2017). Access to Recovery and Recidivism Among Former Prison Inmates. International Journal of Offender Therapy and Comparative Criminology, 61(8), 874–893. 10.1177/0306624X15606688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reif S, Braude L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, Salim O, & Delphin-Rittmon ME (2014). Peer recovery support for individuals with substance use disorders: Assessing the evidence. Psychiatric Services (Washington, D.C.), 65(7), 853–861. 10.1176/appi.ps.201400047 [DOI] [PubMed] [Google Scholar]
- Reingle Gonzalez J (2019). Hogg Foundation for Mental Health Grant Program: Project CRE-001 Evaluation of DSHS Re-entry Project. University of Texas School of Public Health. https://hogg.utexas.edu/wp-content/uploads/2019/02/Re-Entry-Peer-Support-Final-Report-Jan-10-2019.pdf
- Reingle Gonzalez J, Rana RE, Jetelina KK, & Roberts MH (2019). The Value of Lived Experience With the Criminal Justice System: A Qualitative Study of Peer Re-entry Specialists. International Journal of Offender Therapy and Comparative Criminology, 63(10), 1861–1875. 10.1177/0306624X19830596 [DOI] [PubMed] [Google Scholar]
- Rowe M, Bellamy C, Baranoski M, Wieland M, O’Connell MJ, Benedict P, Davidson L, Buchanan J, & Sells D (2007). A Peer-Support, Group Intervention to Reduce Substance Use and Criminality Among Persons With Severe Mental Illness. Psychiatric Services, 58(7), 955–961. 10.1176/ps.2007.58.7.955 [DOI] [PubMed] [Google Scholar]
- Ryan JE, Smeltzer SC, & Sharts-Hopko NC (2019). Challenges to Studying Illicit Drug Users. Journal of Nursing Scholarship : An Official Publication of Sigma Theta Tau International Honor Society of Nursing, 51(4), 480–488. 10.1111/jnu.12486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan RM, Plant RW, & O’Malley S (1995). Initial motivations for alcohol treatment: Relations with patient characteristics, treatment involvement, and dropout. Addictive Behaviors, 20(3), 279–297. 10.1016/0306-4603(94)00072-7 [DOI] [PubMed] [Google Scholar]
- Salem L, Reichert E, Siegfriedt J, Hall T, & Hartwell SW (2017). Boston Offender Needs Delivery Project International Journal of Offender Therapy and Comparative Criminology. 10.1177/0306624X17741807 [DOI] [PubMed] [Google Scholar]
- Schwarzer R, & Jersusalem M (1995). Generalized Self-efficacy Scale. Causal and Control Beliefs, 1(1), 35–37. [Google Scholar]
- Scott CK (2004). A replicable model for achieving over 90% follow-up rates in longitudinal studies of substance abusers. Drug and Alcohol Dependence, 74(1), 21–36. 10.1016/j.drugalcdep.2003.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheldon K (1995). Creativity and Self-Determination in Personality. Creativity Research Journal, 8(1), 25–36. [Google Scholar]
- Sim J, & Lewis M (2012). The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. Journal of Clinical Epidemiology, 65(3), 301–308. 10.1016/j.jclinepi.2011.07.011 [DOI] [PubMed] [Google Scholar]
- Stubbs B, Williams J, Shannon J, Gaughran F, & Craig T (2016). Peer support interventions seeking to improve physical health and lifestyle behaviours among people with serious mental illness: A systematic review. International Journal of Mental Health Nursing, 25(6), 484–495. 10.1111/inm.12256 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2014). Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. US Department of Health and Human Services. https://store.samhsa.gov/product/Results-from-the-2013-National-Survey-on-Drug-Use-and-Health-Summary-of-National-Findings/sma14-4863 [Google Scholar]
- Sullivan CM, Rumptz MH, Campbell R, Eby KK, & Davidson WS II (1996). Retaining participants in longitudinal community research: A comprehensive protocol. Journal of Applied Behavioral Science, 32(3), 262–276. 10.1177/0021886396323002 [DOI] [Google Scholar]
- The Council of State Governments. (2019). Confined and Costly. CSG Justice Center. https://csgjusticecenter.org/publications/confined-costly/ [Google Scholar]
- The Federal Interagency Reentry Council. (2016). The Federal Interagency Reentry Council: A Record of Progress and a Roadmap for the Future. The White House; US Department of Justice. https://berkslancasterlebanonlink.files.wordpress.com/2017/05/firc-reentry-report.pdf [Google Scholar]
- The Temple University Collaborative on Community Inclusion. (2016). Reentry and Renewal: A review of Peer-run Organizations that Serve Individuals with Behavioral Health Conditions and Criminal Justice Involvement. http://tucollaborative.org/wp-content/uploads/2017/03/Reentry-and-Renewel.pdf
- Tracy K, Burton M, Nich C, & Rounsaville B (2011). Utilizing peer mentorship to engage high recidivism substance-abusing patients in treatment. The American Journal of Drug and Alcohol Abuse, 37(6), 525–531. 10.3109/00952990.2011.600385 [DOI] [PubMed] [Google Scholar]
- Travis J, Keegan S, Cadora E, Solomon A, & Swartz C (2003). A Portrait of Prisoner Reentry in New Jersey. Urban Institute Justice Policy Center. https://www.urban.org/sites/default/files/publication/59491/410899-A-Portrait-of-Prisoner-Reentry-in-New-Jersey.PDF
- US Department of Health and Human Services. (2015, November 23). Incarceration & Reentry. Office of the Assistant Secretary for Planning and Evaluation. https://aspe.hhs.gov/incarceration-reentry [Google Scholar]
- Vaughn T, Sarrazin MV, Saleh SS, Huber DL, & Hall JA (2002). Participation and retention in drug abuse treatment services research. Journal of Substance Abuse Treatment, 23(4), 387–397. 10.1016/S0740-5472(02)00299-4 [DOI] [PubMed] [Google Scholar]
- Visher C, LaVigne N, & Travis J (2004). Returning Home: Understanding the Challenges of Prisoner Reentry-Maryland Pilot Study: Findings from Baltimore. Urban Institute Justice Policy Center. https://www.urban.org/sites/default/files/publication/42841/410974-Returning-Home-Understanding-the-Challenges-of-Prisoner-Reentry.PDF
- Watson DP, Ray B, Robison L, Xu H, Edwards R, Salyers MP, Hill J, & Shue S (2017). Developing Substance Use Programming for Person-Oriented Recovery and Treatment (SUPPORT): Protocol for a pilot randomized controlled trial. Pilot and Feasibility Studies, 3(1). 10.1186/s40814-017-0212-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waye KM, Goyer J, Dettor D, Mahoney L, Samuels EA, Yedinak JL, & Marshall BDL (2019). Implementing peer recovery services for overdose prevention in Rhode Island: An examination of two outreach-based approaches. Addictive Behaviors, 89, 85–91. 10.1016/j.addbeh.2018.09.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb P, Zimet G, Fortenberry J, & Blythe M (1999). Comparability of a computer-assisted versus written method for collecting health behavior information from adolescent patients. The Journal of Adolescent Health : Official Publication of the Society for Adolescent Medicine, 24(6), 383–388. 10.1016/s1054-139x(99)00005-1 [DOI] [PubMed] [Google Scholar]
- Western B, Braga A, Hureau D, & Sirois C (2016). Study retention as bias reduction in a hard-to-reach population. Proceedings of the National Academy of Sciences of the United States of America, 113(20), 5477–5485. 10.1073/pnas.1604138113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White W, Boyle M, Loveland D, & Corrigan P (2003). What is behavioral health recovery management? A brief primer.
- White WL (2009). Peer-Based Addiction Recovery Support: History, Theory, Practice, and Scientific Evaluation Executive Summary (Vol. 10). Great Lakes Addiction Technology. [Google Scholar]
- Whitehead AL, Julious SA, Cooper CL, & Campbell MJ (2016). Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Statistical Methods in Medical Research, 25(3), 1057–1073. 10.1177/0962280215588241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winnick TA, & Bodkin M (2008). Anticipated Stigma and Stigma Management Among Those to be Labeled “Ex-con.” Deviant Behavior, 29(4), 295–333. 10.1080/01639620701588081 [DOI] [Google Scholar]
- World Prison Brief, Institute for Crime and Justice Policy Research, & Birkbeck University of London. (2018). Highest to Lowest—Prison Population Rate. https://www.prisonstudies.org/highest-to-lowest/prison_population_rate?field_region_taxonomy_tid=All
- Ziek K, Beardsley M, Deren S, & Tortu S (1996). Predictors of follow-up in a sample of urban crack users. Evaluation and Program Planning, 19(3), 219–224. 10.1016/0149-7189(96)00014-6 [DOI] [Google Scholar]


