INTRODUCTION
The COVID-19 pandemic has prompted a reassessment of the traditional pathways and processes involved in the delivery of health care. This is especially true for diagnostic services, which have been profoundly affected during the pandemic as a result of an increase in demand and the reduction in workforce availability that followed staff illness, isolation, and redeployment. This has led to a dramatic increase in the number of patients waiting for key investigations; this is a problem felt acutely by echocardiography services across the UK. The effects of the pandemic have also exacerbated pre-existing tensions for echocardiography services, where an increasing incidence of cardiovascular pathology has not been matched by the number of sonographers trained to perform the scans.1 This presents clinicians and healthcare providers with the potential for significant risk as large numbers of patients wait for a test with no meaningful framework available to easily determine which of them are in greatest need.
DECIDING WHEN ECHOCARDIOGRAPHY IS OF BENEFIT
These concerns prompted the British Society of Echocardiography (BSE) along with NHS England to produce expert consensus guidance on when echocardiography is indicated and in which clinical situations it is unlikely to add benefit to a patient’s clinical journey.2 These recommendations were developed by expert review of the available literature for indications for an echocardiogram in specific clinical scenarios. This evidence base was applied pragmatically to develop consensus on when an echocardiogram is likely or unlikely to be of benefit to patients.
It was felt by the guideline development committee that it is often more helpful for non-specialist clinicians to understand when a particular test is not needed, and this is often not covered in usual guidelines and recommendation documents. As many requests for echocardiography originate from primary care, specific guidance to support primary care clinicians in situations where balanced clinical reasoning favours avoiding further investigation has now been published (Figure 1). However, it is important to acknowledge that this guidance is not intended to replace individual clinical judgement.
Figure 1.
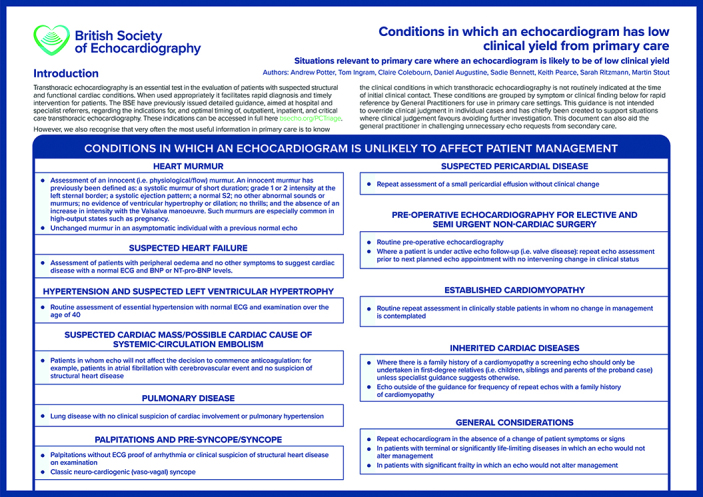
British Society of Echocardiography primary care triage poster.
© Copyright British Society of Echocardiography. Reproduced with permission.
An overreaching principle of medicine is that the result of any investigation should have a significant impact on a patient’s management. It is often more challenging to decide when an echocardiogram is not needed, and this decision can be especially difficult to reach in a patient with a life-limiting condition. In this situation, the inevitable deterioration in symptoms may often provoke the clinician to look for a cause, but it must be clear that identification of this will meaningfully affect subsequent patient care. Careful discussion of the reasons for inaction is necessary but often it can be comforting for patients that another test is not needed.
Heart failure
Assessment for possible heart failure is an extremely common reason to request an echocardiogram, especially if cardiomegaly is reported on a chest X-ray. However, in the absence of a significant cardiac history, and with a normal physical examination and 12-lead electrocardiogram (ECG), then the presence of simple cardiomegaly (without pulmonary congestion or other findings suggestive of cardiac disease) on a chest X-ray does not warrant an echocardiogram as the likely yield of identifying significant cardiac pathology is low.3
Hypertension
Hypertension in a young patient (that is, aged <40 years) can prompt a search for a secondary cause and an echocardiogram is an important part of the work-up to look for an underlying cardiovascular aetiology (for example, coarctation of the aorta) and end organ damage.4 However, an echocardiogram is not indicated routinely to evaluate patients with hypertension, particularly when a normal 12-lead ECG and physical examination is present. Inherited cardiac diseases can present in a wide age range and echocardiogram surveillance is mandated in patients who are primary-degree relatives of an affected individual. These patients should be under regular echocardiogram follow-up guided by a specialist clinic. However, unless symptoms change, an echocardiogram outside the international guidance is not indicated.5
CONCLUSION
Echocardiography is an incredibly versatile diagnostic tool and when used appropriately is vital in the prompt diagnosis and management in patients presenting with potential cardiac disease. However, its timely utility is predicated on the most appropriate use of this imaging modality. In general practice often the most challenging decision is whether or not to refer or test. This guidance produced by the BSE is hoped to prompt reflection on the necessity of testing by the clinician, and support rational and evidence-based referral to echocardiography services.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.The King’s Fund NHS workforce: our position. 2021. https://www.kingsfund.org.uk/projects/positions/nhs-workforce (accessed 2 Jun 2021).
- 2.British Society of Echocardiography Clinical indications and triage of echocardiography posters. https://www.bsecho.org/Public/News/Articles/2021/2021-01/202101-triaging-posters.aspx (accessed 27 May 2021).
- 3.Wingate-Saul L, Javaid Y, Chambers J. Echocardiography is not indicated for an enlarged cardiothoracic ratio. Br J Cardiol. 2013;20:149–150. [Google Scholar]
- 4.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH) Eur Heart J. 2018;39(33):3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 5.Elliott PM, Anastasakis A, Borger MA, et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC) Eur Heart J. 2014;35(39):2733–2779. doi: 10.1093/eurheartj/ehu284. [DOI] [PubMed] [Google Scholar]


