Abstract
Objective:
To test sleep quality as one mechanistic pathway through which repeated concussion increases risk of depression later in life among former contact sport athletes.
Setting:
Multicenter study enrolled former American collegiate football players from 16 different NCAA member institutions.
Participants:
Fifty-eight former American collegiate football players approximately 15-years following sport discontinuation.
Design:
Participants completed in-person evaluations including comprehensive semi-structured interviews with detailed concussion history and sport history, as well as self-reported measures of depression symptom severity (Beck Depression Inventory-II) and sleep quality (Pittsburgh Sleep Quality Index). Years of football participation was included as a covariate. Mediation modeling examined the degree to which sleep quality accounted for the association between repeated concussion and depression symptoms.
Results:
Within the mediation model, concussion history significantly predicted sleep quality (B=1.03, 95%CI=.37,1.65, p=.002) and sleep quality significantly predicted depressive symptom severity (controlling for the effects of concussion history; B=.15, 95%CI=.06, .24, p=.001). With inclusion of the indirect effects, concussion history did not predict depressive symptom severity (direct effect, p=.249, B=.14, 95%CI= −.09, .41; indirect effect=.15, 95%CI=.03, .29 p=.016).
Conclusions:
Current findings raise the possibility that the greater risk of depression reported in those with a history of mTBI/concussion is mediated by sleep quality, a common sequelae of mTBI. These findings highlight potential opportunities for prophylactic sleep-related intervention among individuals with multiple prior concussions to mitigate the risk of depression.
Keywords: Concussion, sleep, depression, mediation, contact sport, TBI
INTRODUCTION
Repeated concussion is a risk factor for depression among former contact sport athletes independent of physical health.1 The mechanisms linking cumulative concussion earlier in life and the subsequent onset of depression years following discontinuation from sports remains unclear. Sleep quality may constitute one mechanistic pathway given the close association between depression and sleep.2,3 While depression may give rise to insomnia, it is also clear that sleep abnormalities may predispose individuals to clinical depression. A longitudinal study showed that over a 6-year period, symptoms of persistent insomnia were significantly associated with an increased risk of depression among community dwelling adults (non-TBI) without a history of depression.2 This is consistent with meta-analyses showing that sleep disturbance is a precursor of depression in adolescence and young-adulthood.3 Importantly, changes in sleep is common following mild traumatic brain injury (mTBI), with evidence suggesting mTBI, and repetitive mTBI in particular, can lead to chronic disturbances in sleep quality.4 The aim of the current study was to examine whether sleep quality mediates the relationship between prior concussion and the severity of self-reported depressive symptoms in a sample of former, collegiate American football players.
MATERIALS AND METHODS
This study was approved by an Institutional Review Board (IRB) and all participants provided written informed consent prior to any study activities. Participants were recruited from 16 different National Collegiate Athletic Association (NCAA) member institutions who had participated in an online health survey prior to the current study. Inclusion criteria included at least one year of collegiate American football participation and completion of Part I of the study (i.e., online Health Survey). Of those who reported a history of concussion, the most recently sustained concussion was approximately 13-years prior. Exclusion criteria included a history of psychotic disorder with active symptoms and contraindication to parent study (NCAA 15-Year Follow-up Study) procedures, such as inability to travel to the in-person evaluation.
Measures
Demographic and medical health histories were provided by participants. Participants were asked to recall any injuries to their head as defined by “an injury occurring typically, but not necessarily, from a blow to the head, followed by a variety of symptoms that may include any of the following: headache, dizziness, loss of balance, blurred vision, ‘seeing stars,’ feeling in a fog or slowed down, memory problems, poor concentration, nausea, throwing up, and loss of consciousness. Depression symptom severity was measured using the Beck Depression Inventory-II (BDI) and sleep quality with the Pittsburgh Sleep Quality Index (PSQI) global score.
Statistical analysis
Statistical analyses were performed with Mplus (version 8.3),5 which tested whether the relationship between concussion history and depressive symptom severity was mediated by sleep quality using maximum likelihood estimation. Given that BDI scores are count data with a higher distribution of responses around zero, negative binomial parameterization was used. The proposed model was assessed by estimating the direct effect of concussion history on depressive symptom severity, the indirect effect (i.e., mediating effect of sleep between concussion history and depressive symptoms), and the total effect (direct plus indirect effects). CI and standard errors of model effects were generated using the percentile bootstrapping method (i.e., 10,000 sample).
Years of American football participation was included as an a priori covariate within mediation models. Concussion history was binned as an ordinal classification consisting of 4 groups; 0–1, 2–4, 5–7, 8+. An important assumption when testing mediation includes sequential ignorability, or that there is no unmeasured confounding of the mediator-outcome relationship. If variables that affect both the mediator and the outcome are omitted from the model (ie, confounds), this can result in biased parameter estimates or even faulty inferences. Sensitivity analyses, as proposed by Imai et al.,6 were performed in order to test the robustness of the tested mediation model and indirect effect across the range of ρ values (−.9 to .9) with depression treated as a continuous variable. Additional sensitivity analyses including a two-tail winsorization (90%), log transformation, and trimming of concussion history were also performed to ensure that results did not vary as a result of method of transformation. Statistical significance was evaluated at alpha = 0.05 (two-tailed). The data utilized as part of this study that support the reported findings are available from the corresponding author (BLB), upon reasonable request.
RESULTS
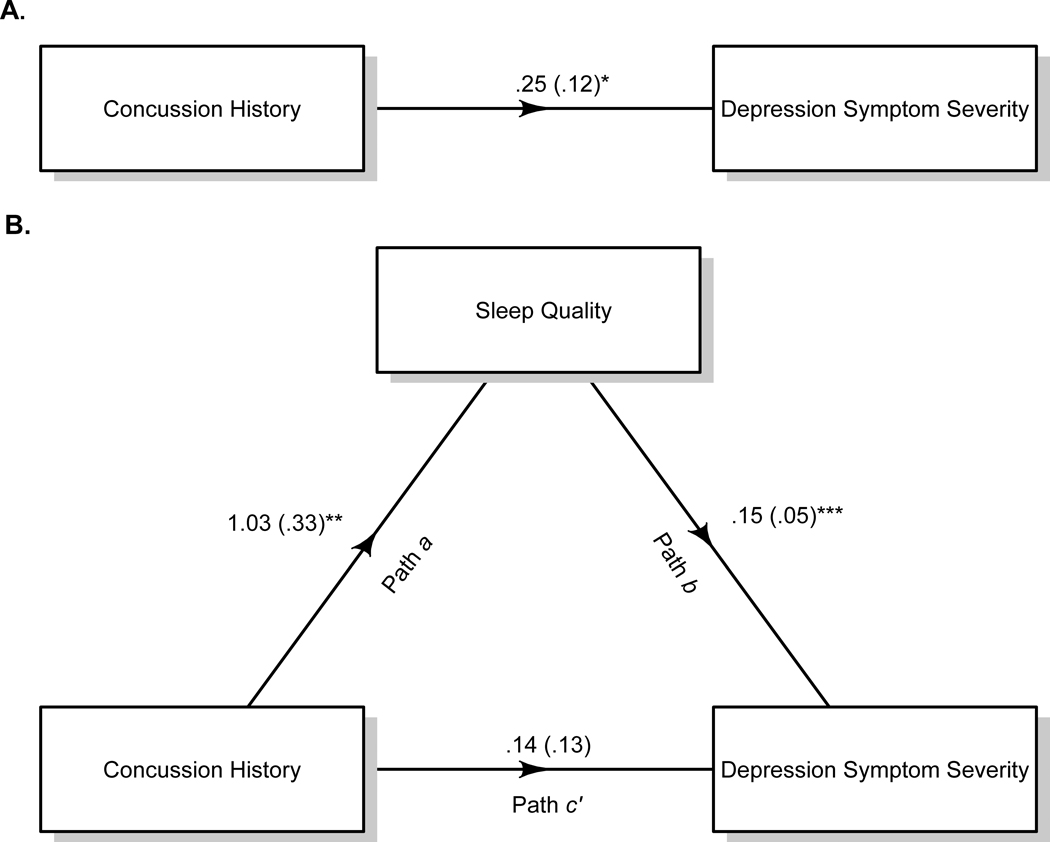
A total of 58 participants met the study criteria highlighted above (Table 1). Notable medical history, including sleep apnea, did not significantly differ between concussion history groups, ps >.05 (Table 2). A greater concussion history was significantly associated with increased depressive symptom severity (B=.25, SE=.12, 95%CI=.03, .50, p=.037,). Within the mediation model (Figure 1), concussion history was significantly predictive of sleep quality, (path a; B=1.03, SE=.33, 95%CI=.37, 1.65, p=.002,) and sleep quality (controlling for concussion history) was significantly predictive of depressive symptom severity (path b; B=.15, SE=.05, 95%CI=.06, .24, p =.001). With inclusion of the indirect effects, concussion history was not significantly predictive of depressive symptom severity (direct effect path c’; B=.14, SE=.13, 95%CI= −.09, .41, p=.249,), indicating complete mediation. Bootstrap confidence interval of the indirect effect (i.e., mediated effect of sleep on the relationship between concussion history and depressive symptom severity) was statistically different from zero (indirect effect=.15, SE=.06, 95%CI=.03, .29, p=.016). The total effect (i.e., direct and indirect) of concussion history on depression was significant (B=.30, SE=.12, 95%CI=.08, .53, p=.010). The above results were comparable when sleep apnea was included as a covariate within the model (e.g., indirect effect=.15, SE=.07 p=.023 versus reported results of indirect effect=.15, SE=.06, p=.016).
Table 1.
Demographics and Sample Characteristics
| Demographic | M(SD) or N Range |
|---|---|
| N | 58 |
| Age | 37.92(1.47) 35 to 41 |
| Race (N) | |
| White | 48 |
| Black | 7 |
| Other | 3 |
| Years of American Football Participation | 12.10(3.18) 6 to 19 |
| Number of Concussions | |
| 0 to 1 | 23 |
| 2 to 4 | 10 |
| 5–7 | 12 |
| 8+ | 13 |
| Measures | M(SD); Median (IQR) Range |
| Pittsburgh Sleep Quality Index | 5.67(3.05);* 5 (4–7.25); 1 to 14 |
| Beck Depression Inventory | 7.29(7.26); 5 (1–11); 0 to 34 |
M=Mean; SD=Standard deviation; IQR= Interquartile range
31 participants met criteria for “poor sleep quality” according to an established cut score of 5 on the PSQI
Table 2.
Medical History and Prior Concussion
| Medical History | N(%) | FET | p-value |
|---|---|---|---|
| Hypertension | 8 (13.8.2%) | .54 | 1.0 |
| Asthma | 8 (13.8%) | 1.35 | .76 |
| Osteoarthritis | 7 (12.1%) | .584 | 1.0 |
| Sleep Apnea | 6 (10.3%) | 2.88 | .37 |
| Migraines | 3 (5.2%) | 1.41 | 1.0 |
| Attention-Deficit Hyperactivity Disorder | 3 (5.2%) | 1.41 | 1.0 |
| Chronic Obstructive Pulmonary Disease; Coronary Artery Disease; Diabetes Mellitus-II; Emphysema; Myocardial Infarction; Kidney Disease; Liver Disease; Stroke/Cerebrovascular Accident; Inflammatory Bowel Disease | 0 (0%) | ____ | ____ |
The above analyses display differences in medical history across concussion history groups; FET=Fisher’s Exact Test
Figure 1: Proposed Mediation Model of Concussion History, Sleep, and Depression.
The effect of concussion history on depressive symptom severity when controlling for years of American football participation, p = .037, β = .25, SE=.12, CI = .03 – .50; b) The proposed mediation model involving the association of concussion history and depressive symptom severity through the effect of sleep quality. Concussion history was significantly predictive of sleep quality, (path a; p=.002, β = β = 1.03, SE=.33) and sleep quality (controlling for concussion history) was significantly predictive of depressive symptom severity (path b; p = .001, β = .15, SE=.05). Concussion history was not significantly predictive of depressive symptom severity (direct effect, path c’; p=.249, β = .14, SE-.13) with inclusion of the indirect effect, which was significant, demonstrating complete mediation (p=.016, indirect effect= .15, SE= .04). ** p<.01; *** p<.001
Given BDI contains a sleep-related item, sensitivity analyses were performed without the sleep-related item in the model, and yielded comparable results to those described above (indirect effect=.15, SE=.07, 95%CI =.03, .29, p=.019). An alternative model that included concussion history as the predictor, sleep quality as the outcome, and depressive symptom severity as the mediator was fit given the relationship between sleep and depression is likely bidirectional. A significant indirect effect was not observed within this mediation model, (indirect effect =.05, SE=.03, 95%CI= .00, .10, p=.054), and depression did not completely mediate the relationship between concussion history and sleep quality, as the direct effect between concussion history and sleep quality remained significant in the full mediation model (path c’; B = .13, SE=.05, 95%CI= −.03, .23, p=.011). Finally, sensitivity analyses demonstrated that the CI of the indirect effect included zero when ρ ≥ 0.30, suggesting that results would be sensitive to violation of the sequential ignorability assumption (ie, failure to include confounding unmeasured covariates that affect both sleep quality and depression).
DISCUSSION
These findings raise the possibility that the greater risk of depression reported in those with a history of repeated mTBI/concussion is mediated by sleep quality, a common sequelae of mTBI. The proposed mediation model suggested a complete mediation effect of sleep on the relationship between concussion history and depressive symptom severity. This finding is clinically relevant given that insomnia can be successfully treated, thus providing an opportunity for early intervention to reduce the risk of depressive episodes and their associated morbidity after mTBI. Further early interventions to improve sleep hygiene and quality could be considered in younger athletes that may be at increased risk for depression later in life due to multiple concussions occurring during sport participation.1,7
The biological mechanism underlying the depressogenic effect of sleep quality differences in the context of mTBI is unknown and requires further investigation. Specifically, it is unclear if cumulative head injury could have a distinct effect on sleep quality differences via changes in hormonal or neurotransmitter disturbance (e.g., melatonin or GABA), which over time increase the likelihood of depression.8 Alternatively, strong evidence exists for the role of inflammation across all three factors, suggesting that the mediating effect of sleep on concussion history and depression may occur through this or related processes.9–11
We note that the study is cross-sectional and thus causal conclusions cannot be definitively drawn. Longitudinal studies with larger samples are required to confirm the observed mediating effect of sleep on concussion history and depressive symptom severity, particularly sleep quality changes as a chronic phenomenon, as the PSQI assesses only current sleep quality. However, it is worth nothing that the evidence for head injury temporally preceding sleep changes and sleep disturbance as a risk factor for depression is robust across multiple longitudinal studies.2,3,12 In addition, the current sample size did not permit a causal mediation approach in order to rule out other potentially unmeasured confounds or performing analyses from a counterfactual framework. This will be essential, as the sensitivity analyses showed that the mediating effect of sleep could diminish if there are unaccounted for variables that affect both sleep quality and depression in the same manner. Sleep quality was self-reported. Nevertheless, the PSQI shows a high sensitivity (99%) and specificity (84%) in identifying insomnia in addition to significant correlations with sleep diaries and polysomnography.13 Additionally, assessment of sleep problems in clinical practice primarily relies on patients’ subjective evaluation. Medical and concussion histories were self-reported and not able to be verified via medical record. The reliability of self-reported concussion history has been shown to be dependent on the sample queried, with those who are younger and at lower levels of play (i.e., high school versus professional) showing higher consistency in reporting.14,15 The current sample is in the mid-range for both factors. In spite of these limitations, the current findings highlight potential opportunities for prophylactic sleep-related intervention to mitigate the risk of depression in individuals with a history of multiple concussions.
ACKNOWLEDGEMENT
The authors would like to thank Amy Nader (Department of Neurosurgery at the Medical College of Wisconsin), Robyn Furger (Department of Neurosurgery at the Medical College of Wisconsin), Candice Goerger (Center for the Study of Retired Athletes at the University of North Carolina at Chapel Hill), Leah Thomas (Center for the Study of Retired Athletes at the University of North Carolina at Chapel Hill), for study coordination and management; We are grateful for the participation of the athletes, without whom this research would not be possible.
Disclosures: The authors have no individual conflicts of interest to report. This research was supported through funding from the National Collegiate Athletic Association, and institutional support from the University of North Carolina at Chapel Hill and Medical College of Wisconsin. The REDCap electronic database used for this project were supported by the National Center for Advancing Translational Sciences, National Institutes of Health, Award Number UL1TR001436. BLB acknowledges support from the National Institute of Neurological Disorders and Stroke under the National Institutes of Health under the award L30 NS113158-01. TM acknowledges the support of the National Institute Of Neurological Disorders And Stroke of the National Institutes of Health (R01NS102225; R21NS099789). JS acknowledges the support of the National Institute of General Medical Sciences (P20GM121312) and the National Institute of Mental Health (R21MH113871).
References
- 1.Kerr ZY, Marshall SW, Harding HP, Guskiewicz KM. Nine-year risk of depression diagnosis increases with increasing self-reported concussions in retired professional football players. Am J Sports Med. 2012;40(10):2206–2212. [DOI] [PubMed] [Google Scholar]
- 2.Jaussent I, Bouyer J, Ancelin ML, et al. Insomnia and daytime sleepiness are risk factors for depressive symptoms in the elderly. Sleep. 2011;34(8):1103–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lovato N, Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med Rev. 2014;18(6):521–529. [DOI] [PubMed] [Google Scholar]
- 4.Chaput G, Giguere JF, Chauny JM, Denis R, Lavigne G. Relationship among subjective sleep complaints, headaches, and mood alterations following a mild traumatic brain injury. Sleep Med. 2009;10(7):713–716. [DOI] [PubMed] [Google Scholar]
- 5.Muthén LK, Muthén BO. Mplus User’s Guide 7th ed. ed. Los Angeles, CA: Muthén & Muthén; 1998–2015. [Google Scholar]
- 6.Imai K, Keele L, Yamamoto T. Identification, Inference and Sensitivity Analysis for Causal Mediation Effects. Statistical Science. 2010;25(1):51–71. [Google Scholar]
- 7.Christensen H, Batterham PJ, Gosling JA, et al. Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight Study): a randomised controlled trial. Lancet Psychiatry. 2016;3(4):333–341. [DOI] [PubMed] [Google Scholar]
- 8.Siegel JM. The neurotransmitters of sleep. J Clin Psychiatry. 2004;65 Suppl 16:4–7. [PMC free article] [PubMed] [Google Scholar]
- 9.Irwin MR, Olmstead R, Carroll JE. Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation. Biol Psychiatry. 2016;80(1):40–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nitta ME, Savitz J, Nelson LD, et al. Acute elevation of serum inflammatory markers predicts symptom recovery after concussion. Neurology. 2019;93(5):e497–e507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reus GZ, Fries GR, Stertz L, et al. The role of inflammation and microglial activation in the pathophysiology of psychiatric disorders. Neuroscience. 2015;300:141–154. [DOI] [PubMed] [Google Scholar]
- 12.Theadom A, Cropley M, Parmar P, et al. Sleep difficulties one year following mild traumatic brain injury in a population-based study. Sleep Med. 2015;16(8):926–932. [DOI] [PubMed] [Google Scholar]
- 13.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53(3):737–740. [DOI] [PubMed] [Google Scholar]
- 14.Wojtowicz M, Iverson GL, Silverberg ND, et al. Consistency of Self-Reported Concussion History in Adolescent Athletes. J Neurotrauma. 2017;34(2):322–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kerr ZY, Marshall SW, Guskiewicz KM. Reliability of concussion history in former professional football players. Med Sci Sports Exerc. 2012;44(3):377–382. [DOI] [PubMed] [Google Scholar]