Abstract
We described a strategy for preventing virus transmission within hospitals through screening and advanced isolation during the coronavirus pandemic. Patients were screened and admitted to the adult advanced isolation unit from February to April 2020. Our process minimized exposure without delaying proper treatment and prevented virus transmission within the hospital.
Keywords: Covid-19, Cross infection, Patient isolation, Severe acute respiratory syndrome coronavirus 2
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has infected approximately 25 million people and caused 850,000 deaths globally as of September 2, 2020.1 Since the virus is not associated with specific symptoms or radiological findings, early detection and isolation are essential for any coronavirus disease (COVID-19) quarantine process.2 Therefore, advanced isolation and testing of patients with suspicious symptoms or community-acquired pneumonia of an unknown origin are of prime importance in the current pandemic.
Healthcare facilities have implemented strategies to minimize the nosocomial transmission of COVID-19 and protect inpatients and healthcare workers (HCWs).3 In this study, we present our institution's policy for the screening and advanced isolation of high-risk patients during the COVID-19 pandemic in South Korea.
Methods
Preparation of the advanced isolation unit
The advanced isolation unit (AIU) was created using negative-pressure rooms in the general ward (GW) that had been used for patients with infectious diseases. Previously hospitalized patients in these wards were sequentially moved or discharged to other facilities. On February 19, once the transfer of these patients was complete, we began using the rooms as a transition zone for patients with suspected COVID-19.
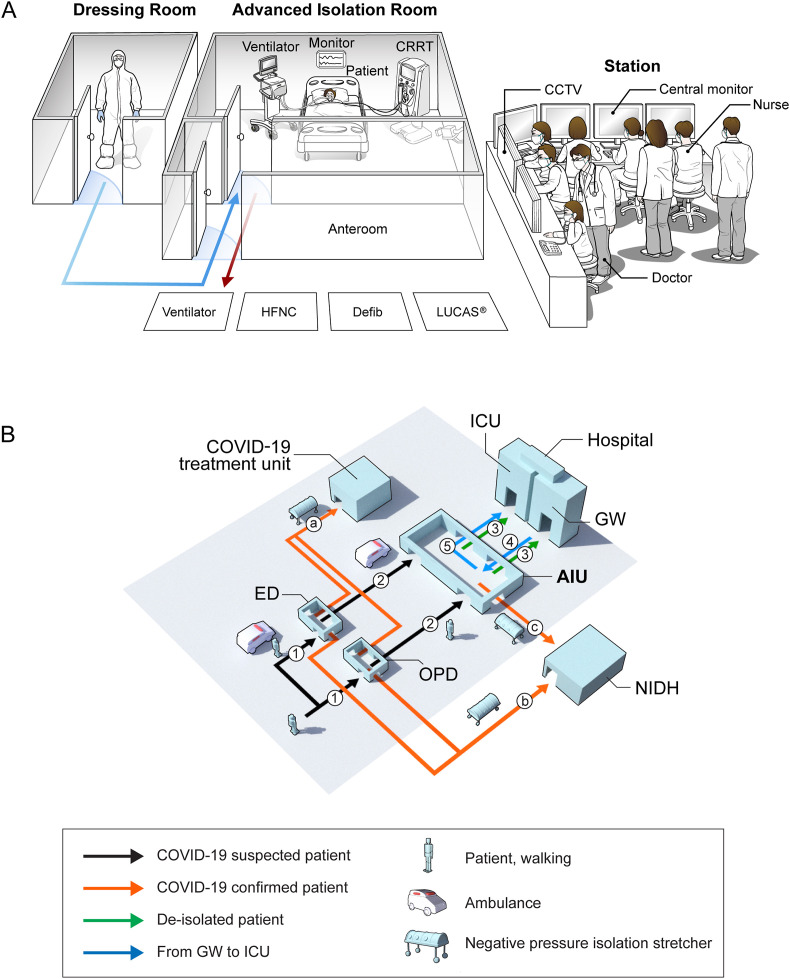
The AIU consists of patient rooms with anterooms, a dressing room, a nursing station with a central monitoring system, and a doctor station (Fig. 1 A). High-efficiency particulate air filters were added to the ventilation systems in the patient rooms and anterooms. The unit contains 11 isolation beds, including six intensive care unit (ICU) beds and five GW beds. We equipped the rooms with multiple critical-care resources, including three mechanical ventilators, six high-flow nasal cannulas, two continuous renal replacement therapy machines, a portable hemodialysis machine, and a LUCAS® (Stryker Medical, Portage, MI, USA) chest compression system. One critical care staff member, one pulmonology fellow, and one internal medicine resident remained in the unit during the day, and on-call doctors were responsible for the night shift. A 1:1 nurse-to-patient ratio was maintained.
Figure 1.
Structure of the advanced isolation unit and flow of the advanced isolation system. (A) Structure of the advanced isolation unit. The staff members entered the advanced isolation room after donning personal protective equipment in the dressing room and exited through the decontamination area of an anteroom, where the protective equipment was removed. Abbreviations: HFNC, high-flow nasal cannula; CRRT, continuous renal replacement therapy; CCTV, closed-circuit television; Defib, defibrillator (B) Flow of the advanced isolation system to screen for COVID-19. 1) Patients visited the screening clinics. 2) Patients were tested for SARS-CoV-2 and required admission to the adult AIU. 3) Patients were transferred from the AIU to the GW or ICU after de-isolation. 4) GW patients who required ICU admission went through the AIU. 5) GW patients were transferred to the ICU after de-isolation. a) Patients with confirmed COVID-19 were transferred to the COVID-19 treatment unit of our institution. b) Patients with confirmed COVID-19 were transferred to NIDHs. c) Patients with confirmed COVID-19 at the AIU were transferred to NIDHs. Abbreviations: AIU, advanced isolation unit; COVID-19, coronavirus disease; ED, emergency department; GW, general ward; ICU, intensive care unit; NIDH, national infectious disease hospital; OPD, outpatient department; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Screening and advanced isolation
We defined patients with suspected COVID-19 according to the definitions of Korea's Response to COVID-19 guidelines issued by the Central Disaster Management Headquarters and Central Disease Control Headquarters.4 The following patients were suspected to have COVID-19: 1) patients with fever (temperature ≥ 37.5 °C) or any newly developed or aggravated respiratory symptoms within 14 days of contact with a confirmed COVID-19 case; 2) patients with pneumonia of unknown etiology and symptoms; and 3) patients exhibiting fever (≥37.5 °C) or any newly developed or aggravated respiratory symptoms with a history of overseas travel or an epidemiological link to a domestic COVID-19 cluster.
Fig. 1B shows the advanced isolation system for the screening of patients with suspected COVID-19. The HCWs in the emergency departments (ED) and outpatient departments (OPD) screening clinics properly donned personal protective equipment (PPE). The body temperatures of all patients were taken at the hospital entrance using non-contact thermometers, and the patients completed a questionnaire on any respiratory symptoms and history of visiting a high-risk area. Anyone who met the criteria for suspected COVID-19 was sent to the screening clinics in the ED or OPD and tested for SARS-CoV-2. A chest radiograph was taken based on clinical indications. Those who did not require hospitalization were discharged with prescriptions; those requiring hospitalization were admitted to the AIU to prevent nosocomial transmission.
Patients with confirmed COVID-19 were transferred to national infectious disease hospitals or the COVID-19 treatment unit of our institution based on the government policy, disease severity, and capacity of the national infectious disease hospitals.
Strict admission criteria were applied to enter the ICU. For those who had been admitted to the GW within the past 72 h and had community-acquired pneumonia, two consecutive negative results for SARS-CoV-2 were required from specimens collected 24 h apart. For those who had been in the GW for more than 72 h, a negative result for SARS-CoV-2 within the past 72 h was required, since transmission through caregivers is a risk factor for nosocomial transmission.5
Infection prevention and control
The AIU is located in a building separate from the ED and OPD screening clinics; therefore, we transported suspected patients by ambulance via an external route rather than through an internal pathway. A doctor seated by an intubated patient with or without a mobile ventilator in the ambulance wore full PPE with powered air-purifying respirators. We also placed high-efficiency particulate air filters between the endotracheal tube and bag valve mask or ventilator.
We used different levels of PPE according to the patient's risk. Level D protection with powered air-purifying respirators was strictly required during any aerosol-generating procedures, such as intubation, cardiopulmonary resuscitation, bag-valve-mask ventilation, and nebulizer treatment. In all other situations, HCWs were required to wear well-fitting N95 respirators or equivocal masks, facial shields or goggles, gloves, gowns, and caps. PPE was removed in the decontamination area of the anteroom and monitored by other medical personnel.
Most experienced doctors on rapid response teams intubated patients using a video-laryngoscope whenever possible. A helmet-based non-invasive ventilator was used to reduce the risk of aerosolization.6 In case of a cardiac arrest, we used a LUCAS® chest compression system to minimize potential virus exposure.
Ethics statement
The study protocol was reviewed and approved by the Institutional Review Board of Severance Hospital (IRB No. 4-2020-0374), and the need for informed consent was waived by the committee.
Results
A total of 10,364 patients visited the ED and OPD screening clinics from February 19 to April 18, 2020; 5969 individuals were classified as patients with suspected COVID-19 and underwent SARS-CoV-2 testing. Admission was needed for 490 (8.2%) patients: 164 children and 326 adults. Twelve patients from the GW also required critical care. In total, 338 patients were admitted to the adult AIU during the study period.
Ten cases of confirmed COVID-19 were filtered through this system: three from the OPD screening clinic and seven from the ED clinic. One of these patients was diagnosed during admission to the AIU. No HCWs or inpatients were infected, and no hospital facilities were closed owing to the confirmed cases.
Baseline characteristics and outcomes of the patients admitted to the AIU are shown in Table 1 . The median age was 72.5 years, and 225 (66.6%) were men. Mechanical ventilation and continuous renal replacement therapy were applied in 20.4% and 7.4% of the patients, respectively. One patient received a positive result for SARS-CoV-2 and was transferred to a national infectious disease hospital.
Table 1.
Characteristics and outcomes of patients admitted to the advanced isolation unit.
| Total (n = 338) | |
|---|---|
| Baseline characteristics | |
| Age, years | 72.5 (60.8–81.0) |
| Sex, male | 225 (66.6) |
| BMI, kg/m2 | 22.8 (19.4–25.4) |
| CCI | 3.0 (2.0–5.0) |
| EDLIPS | 5.0 (2.5–7.5) |
| Route of admission | |
| OPD screening clinic | 15 (4.4) |
| ED screening clinic | 311 (92.0) |
| General ward | 12 (3.6) |
| Reason for admission | |
| Respiratory | 265 (78.4) |
| Sepsis/septic shock | 21 (6.2) |
| Cardiovascular | 20 (5.9) |
| Post-ROSC | 12 (3.6) |
| Gastrointestinal | 11 (3.3) |
| Neurological | 6 (1.8) |
| Othera | 3 (0.9) |
| Outcomes | |
| During isolation | |
| Non-invasive ventilation | 3 (0.9) |
| High-flow nasal cannula | 33 (9.8) |
| Mechanical ventilation | 69 (20.4) |
| Portable hemodialysis | 9 (2.7) |
| CRRT | 25 (7.4) |
| CPR | 9 (2.7) |
| SARS-CoV-2 result | |
| Positive | 1 (0.3) |
| Negative | 337 (99.7) |
| After de-isolation | |
| Transferred to the GW | 246 (72.8) |
| Transferred to the ICU | 77 (22.8) |
| Transferred to another hospital | 1 (0.3) |
| Discharged | 7 (2.1) |
| Death | 7 (2.1) |
| 7-day mortality | 33 (9.8) |
Note: Data are presented as numbers (%) or medians (interquartile ranges).
Abbreviations: BMI, body mass index; CCI, Charlson comorbidity index; EDLIPS, emergency department lung injury prediction score; OPD, outpatient department; ED, emergency department; ROSC, recovery of spontaneous circulation; CRRT, continuous renal replacement therapy; CPR, cardiopulmonary resuscitation; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; GW, general ward; ICU, intensive care unit.
Femur neck fracture, tonsillectomy site bleeding, or scheduled brain surgery.
Discussion
We reported the successful screening of suspected COVID-19 patients and described the operation of an advanced isolation system enabling the timely management of patients requiring admission during the COVID-19 pandemic. This approach could serve as a basis for other healthcare facilities to develop screening and triage strategies for patients with suspected COVID-19 and to develop policies for preventing virus transmission within hospitals and among inpatients or HCWs.
Ten cases of COVID-19 were confirmed through this screening system; one of these patients required admission. The positivity rate was low among patients screened based on symptoms (0.17%), which may be due to the pandemic situation in South Korea during the study period. The outbreak in Korea began in late February, with Daegu city and Gyeongbuk province, which are 300 km apart, being the most affected regions.7 However, considering the high transmissibility of SARS-CoV-2 and the immunocompromised state of most inpatients, even one non-filtered case of COVID-19 could provoke a catastrophe not only for our institution but also for the entire country.8 , 9 No inpatients or medical facilities at this institution were affected by the confirmed cases. Although cost-effectiveness analyses should be conducted in the future, we believe that our advanced isolation strategy helped protect the hospital's patients and HCWs and mitigated the transmission of COVID-19 during the pandemic. We believe it is more important to prioritize specificity over sensitivity to prevent the nosocomial spread of COVID-19.
The importance of limiting the number of HCWs working within the AIU should also be highlighted.10 We assigned a critical-care staff member, a pulmonology fellow, and an internal medicine resident to the AIU. Patient management within the unit was limited to these members to minimize possible viral exposure. Simultaneously, a continual discussion regarding the AIU patients was facilitated among cardiologists, nephrologists, intensivists, hospitalists, neurosurgeons, laboratory physicians, and emergency physicians using a social networking service. We found interdisciplinary teamwork to be essential for critical care in the AIU.
We emptied another GW to accommodate the de-isolated patients without delay, which allowed for synergism with the advanced isolation system. Bed assignments are managed by a centralized administration office in our hospital; therefore, active communication between departments was ensured by assigning the chief of this office as one of the unit members.
Prevention of virus transmission to inpatients and HCWs is a major concern for hospitals during the COVID-19 pandemic. The approach described herein—involving screening and advanced isolation—may minimize viral exposure without delaying proper treatment in medically ill patients requiring admission.
Acknowledgments
The authors thank Medical Illustration & Design, part of the Medical Research Support Services of Yonsei University College of Medicine, for artistic support related to this work.
References
- 1.Medicine JHUa. COVID-19 map. Available at: https://coronavirus.jhu.edu/map.html. [Accessed 2 September 2020].
- 2.Guan W.-j., Ni Z.-y., Hu Y., Liang W.-h., Ou C.-q., He J.-x. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Howitt R., de Jesus G.A., Araujo F., Francis J., Marr I., McVean M. Screening and triage at health-care facilities in Timor-Leste during the COVID-19 pandemic. Lancet Respir Med. 2020;8:e43. doi: 10.1016/S2213-2600(20)30183-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Headquarters CDM. Central disease Control Headquarters. Korea's responses to COVID-19. 7th ed. Released March 2, 2020.
- 5.Hui D.S., Azhar E.I., Kim Y.-J., Memish Z.A., Oh M.-d., Zumla A. Middle East respiratory syndrome coronavirus: risk factors and determinants of primary, household, and nosocomial transmission. Lancet Infect Dis. 2018;18:e217–e227. doi: 10.1016/S1473-3099(18)30127-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cabrini L., Landoni G., Zangrillo A. Minimise nosocomial spread of 2019-nCoV when treating acute respiratory failure. Lancet. 2020;395:685. doi: 10.1016/S0140-6736(20)30359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Korea GotRo . The Government of the Republic of Korea; 2020. Flattening the curve on COVID-19: how Korea responded to a pandemic using ICT. [Google Scholar]
- 8.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [PMID: 31995857] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park S.Y., Kim Y.-M., Yi S., Lee S., Na B.-J., Kim C.B. Coronavirus disease outbreak in call center, South Korea. Emerg Infect Dis. 2020;26:1666. doi: 10.3201/eid2608.201274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Griffin K.M., Karas M.G., Ivascu N.S., Lief L. Hospital preparedness for COVID-19: a practical guide from a critical care perspective. Am J Respir Crit Care Med. 2020;201:1337–1344. doi: 10.1164/rccm.202004-1037CP. [DOI] [PMC free article] [PubMed] [Google Scholar]