Abstract
BACKGROUND:
Continuous pertinent trainings for infection prevention and control (IPC) measures are essential to ensure quality health-care services along with the safety of the health personnel. Amid the COVID-19 pandemic, the current study focusses on the utilization of explicated video modules training of all health-care personnel of the institute and assessment of the effectiveness of video training for IPC practices during COVID-19 pandemic.
MATERIALS AND METHODS:
A quasi-experimental study, one group pre- and posttest design, using Google Questionnaire forms was conducted at a tertiary care center. The training was assisted by trained tutors, and three in-house videos were demonstrated to the participants regarding specific IPC measures; “Do's and Don’ts;” “Hand hygiene and personal protective equipment's (PPE)” and “Environmental cleaning and disinfection.” SPSS software version 23 (IBM Corp., N. Y., USA) was used for the analysis using the descriptive statistics, Chi-square test, Fisher's t-test, ANOVA, and post hoc Tukey's test.
RESULTS:
The level of knowledge increased significantly by 16% in the posttest. Statistically significant association between the levels of knowledge in pretest as well as posttest scores and age (P < 0.001), designation (P < 0.001), and years of experience (P < 0.001) was identified. The participants were satisfied with the video-assisted trainings and willing to use videos for revision.
CONCLUSIONS:
Video-assisted training modules similar to this study may be utilized to enhance the knowledge of various cadres of health-care staff regarding IPC practices.
Keywords: COVID-19, infection control, training, video modules
Introduction
The coronavirus disease-19 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS CoV-2), a highly transmissible virus, has placed unprecedented strain on health-care services worldwide and surpassed the other recent pandemics caused by SARS and Middle East Respiratory Syndrome (MERS) CoV.[1,2] The rapid spread and a large number of fatalities have caused anxiety and exposed the lack of human preparedness for such a medical catastrophe.[2,3,4] Experiences, like Ebola in 2014, MERS-CoV in 2012 and SARS-CoV in 2003 have demonstrated patient to patient and patient to health-care professional (HCP) transmission in health-care settings; and the critical role of infection prevention and control (IPC) programs to deal with such infections. In the currently ongoing COVID-19 pandemic, infection rates in HCPs vary between countries. In the UK, 14% of HCPs tested positive on screening, whereas in the United States, over 9000 cases were reported in health-care workers, of whom 55% had a history of contact only in a health-care setting.[5,6]
IPC continues to be scrutinized as our health-care facilities face an unforeseen public health crisis. The COVID-19 pandemic has changed the perspective of health-care organizations regarding infection control to protect patients and staff from the potential exposure within their facilities and has also prompted leaders to consider how they can strengthen IPC processes and train their staff to prevent further spread in health-care facilities and prepare all HCPs for COVID-19 and such pandemics.[7,8,9]
The health care workforce is integral to an effective pandemic response and therefore needs to be trained and competent in their response roles.[10] Among the various methods of available educational interventions for health education and health promotion programs, video technology conveys the information or knowledge in a more interesting way and allows the portrayal of complicated content.
Considering the need for training umpteen HCPs, patients and their attendants, with limitation of safe space for training and maintaining social-distancing norms, etc., video modules were developed for the same within the institute. Video-assisted trainings have been used previously for health education but the use of video modules as a part of structured IPC program under constraints of limited but trained workforce against numerous trainees in the current pandemic has yet not been addressed. We conducted IPC trainings with an emphasis over COVID-19 using the video modules, and this study was done to evaluate the effect of video modules as training tools for infection control. This study may help us improving training programs and understanding training needs of the HCPs during current COVID-19 pandemic.
Materials and Methods
A quasi experimental, one group pre- and posttest research was conducted to assess the effect of video-assisted teaching on knowledge of HCP's and to educate regarding IPC measures with special focus on COVID-19 at tertiary care institute in the northern part of India from April to May 2020. Using the convenience sampling method, 478 study participants, including HCPs (faculty members, senior and junior residents, MBBS students/interns, and nursing officers), were selected. A semi-structured questionnaire was used to collect the data. The participants who either walked out in the middle of the training session or did not attempt either pre- or posttest or did not give consent were excluded from the study. Informed consent from each of the participants was obtained for participation in the study. The study was approved by the Institutional Ethics Committee (letter no. 209/IEC/IM/NF/2020). Confidentiality of information and anonymity of the participants were maintained.
Description of the tool and scoring procedure
Google form-based questionnaire was used as a tool for assessment and consisted of five sections:
Section 1: The section of questionnaire included the demographic characteristics of participants such as age, gender, consent, designation, department, and previous training status
Section 2, 3, and 4: Structured questionnaire was used in pre- and posttest to assess the effect of video-assisted training which consisted of following statements for “Do's and Don’ts;” “Hand hygiene and PPE,” and “Environmental cleaning and disinfection”
Section 5: Structured feedback questionnaire consisting of 11 questions to assess the effectiveness of video-assisted training modules. There were different types of responses for these questions such as “Yes, No, or Maybe;” 3 points Likert scale including - “Agree, Neutral, and Disagree.”
Description of the intervention
Video-assisted trainings were conducted using in house videos prepared in the local language (Hindi). The content of videos was per institute's IPC policy and procedures which were formulated based on the guidelines of World Health Organization (WHO), Center for Disease Control, Ministry of Health and Family Welfare-Government of India, Indian Council of Medical Research, and scientific literature and available logistics of the institute.[7,11,12,13,14] The content of video modules was finalized and assessed by various experts from the field of medicine, nursing, and the Advance Center for Continuous Professional Development of the Institute [Supplementary Table 1].
Supplementary Table 1.
Youtube link of video modules used for training
| Video content | Link |
|---|---|
| Do’s and Don’ts, hand hygiene | https://www.youtube.com/watch?v=xb_YP5P05es&feature=youtu.be |
| Donning and doffing of PPE | https://www.youtube.com/watch?v=DLuLzQ9JDoQ&feature=youtu.be |
| Cleaning and disinfection | https://www.youtube.com/watch?v=isAOyzGk8ak&feature=youtu.be |
Each training was of 2 h and consisted of various sessions, as shown in Supplementary Table 2; the content of videos was organized as an introduction, detailed procedure, and conclusion. The approximate duration for each video was about 7–9 min. The training was conducted in assistance of well-trained trainers.
Supplementary Table 2.
Training schedule for each session
| Schedule of video assisted training program | |
|---|---|
| Activity | Time (min) |
| Arrival/sign-in with expectations form | 5 |
| Pretest | 15 |
| Introduction to Infection Control Programme by infection control officer or a trained tutor/resident/infection control nurse | 10 |
| Video module 1 - Do’s and Don’ts | 15 |
| Video module 2 - Hand hygiene | 15 |
| Video module 3 - Donning and doffing of personal protective equipment | 15 |
| Video module 4 - Cleaning and disinfection | 15 |
| Sample collection and transport | 15 |
| Discussion | 10 |
| Posttest and feedback form | 5 |
The self-administered pretest questionnaire was distributed to the participants before the video session. The video session was conducted for the group of 15–20 HCPs at a time, and each session was concluded in about 90–120 min including the discussion with the trainer for clarifying further doubts regarding the topics at the end of the session. After the completion of video-assisted training, a posttest was conducted among the same group of HCPs using the same structured questionnaire along with a feedback form to assess the effectiveness of the video-assisted training [Supplementary Table 2].
Data analysis
Data were entered using the data validation feature of MS Excel 2013 to maintain the data quality from Google sheets and exported to IBM SPSS Statistics for Windows, version 23 (IBM Corp., Armonk, N. Y., USA) for the analysis. Shapiro–Wilk test was used to check the normality of data. The data were analyzed in terms of descriptive frequencies and percentages of different domains to describe the pre- and posttest knowledge. Level of knowledge was based on score in pre-test and post-test as mentioned in [Table 1]. Mean and standard deviations were calculated. Paired-sample t-test was used to compare pre- and posttest scores. One-way analysis of variance (F-test) and student independent t-test were used to find out the association between demographic variables and mean pre- and posttest scores. To analyze the association within the groups with demographic variables, post hoc test was used. Chi-square test was used to check the association between knowledge level and participants’ demographic variables.
Table 1.
Level of knowledge
| Scoring knowledge score | Score | ||
|---|---|---|---|
| Level of knowledge | Sub-variable | Percentage | |
| Inadequate | Very poor | <20 | <3 |
| Poor | 20-40 | 3-7 | |
| Moderate | Average | 41-60 | 8-10 |
| Good | 61-80 | 11-15 | |
| Adequate | Very good | 81-90 | 16-17 |
| Excellent | >91 | >17 | |
Individual actual gains (Gi) were tabulated to calculate percent average actual gain (Gi = posttest score - pretest score) and percent relative gain (percent relative gain = average Gi /pretest score) for the class.[15] This was intended to minimize dependence on the different levels of participants’ understanding at the time of the precourse test. All the statistical tests were evaluated at the P < 0.05 level of significance.
Results
Response rate
In total, 478 participants attended the training, of whom 457 filled pretest and 435 filled posttest forms; however, 407 (85.1%) responses were included as 71 participants did not attend either pre- or posttest or were unable to attend the complete video training session.
Demographic characteristics of participants
The mean age of the participants was 27.65 ± 3.73 years, with 45.5% being between 26 and 30 years of age. Only 10 (2.4%) participants were above 35 years of age. The majority of the participants, 203 (49.8%) were nursing officers [Table 2].
Table 2.
Demographic variables of participants and their association with “pre- and post-test score” of health-care professionals (n=407)
| Demographic variables | n (%) | Pretest Mean±SD | One-way ANOVA test (F) or t-test Significant (pretest) | Posttest Mean±SD | One-way ANOVA test (F) or t-test Significant (posttest) |
|---|---|---|---|---|---|
| Age† (years) | |||||
| 21-25 | 130 (31.9) | 10.8±2.4 | <0.001* | 13.9±2.4 | <0.001* |
| 26-30 | 187 (45.9) | 9.4±2.6 | 12.4±2.9 | ||
| 31-35 | 80 (19.6) | 9.4±2.5 | 12.2±2.9 | ||
| >35 | 10 (2.4) | 7.5±2.3 | 10.9±1.8 | ||
| Gender‡ | |||||
| Male | 229 (56.3) | 9.7±2.7 | 0.340 | 12.8±2.9 | 0.793 |
| Female | 178 (43.7) | 9.9±2.5 | 12.8±2.9 | ||
| Designation† | |||||
| Faculty | 12 (2.9) | 8.6±1.8 | <0.001* | 11.6±1.6 | <0.001* |
| Residents | 110 (27.1) | 9.8±2.4 | 12.8±2.5 | ||
| MBBS | 77 (18.9) | 11.4±2.4 | 14.6±2.3 | ||
| Nursing officers | 203 (49.8) | 9.3±2.6 | 12.3±3.0 | ||
| Technicians | 5 (1.2) | 7.2±2.5 | 8.8±2.8 | ||
| Years of experience† | |||||
| <1 | 91 (22.3) | 10.9±2.4 | <0.001* | 13.7±2.5 | 0.005* |
| 1-5 | 242 (59.4) | 9.5±2.6 | 12.5±2.9 | ||
| 5-10 | 52 (12.7) | 9.9±2.1 | 12.8±3.1 | ||
| >10 | 22 (5.4) | 9.3±3.3 | 12.2±2.5 | ||
| Previous training† | |||||
| Yes | 151 (37.1) | 9.6±2.8 | 0.019* | - | - |
| No | 189 (46.4) | 9.7±2.4 | - | ||
| May be | 67 (16.5) | 10.6±2.5 | - |
*Significant (<0.05), †One way ANOVA, ‡t-test. SD=Standard deviation
Baseline knowledge
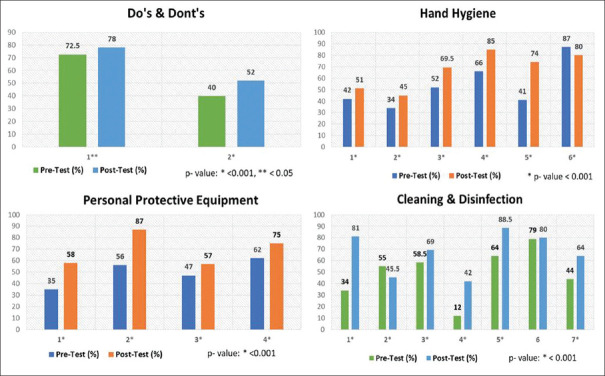
Figure 1 shows that the majority (80%) of participants had a moderate level of knowledge before training, with scores in the range of 41%–80%. The level of knowledge increased by 16% in the posttest and hence considered adequate.
Figure 1.
Level of knowledge in pretest and posttest among the health-care professionals (n = 407)
Statistically significant association between the level of knowledge in pretest and age (P < 0.001), designation (P < 0.001), and years of experience (P < 0.001) among HCPs was identified, as illustrated in [Supplementary Table 3]. There was no significant relation found between the level of knowledge in pretest among participants and previous training (P = 0.277).
Supplementary Table 3.
Association of level of knowledge in pretest and demographic variables among health-care professionals (n=407)
| Demographic variables | Pretest level of knowledge score, n (%) | Total (n) | Chi-square test (P) | ||
|---|---|---|---|---|---|
| Inadequate | Moderate | Adequate | |||
| Age in years | |||||
| 21-25 | 6 (4.6) | 120 (92.3) | 4 (3.1) | 130 | 31.01 (0.000)* |
| 26-30 | 48 (25.7) | 136 (72.7) | 3 (1.6) | 187 | |
| 31-35 | 14 (17.5) | 65 (81.3) | 1 (1.3) | 80 | |
| >35 | 5 (50) | 5 (50) | 0 | 10 | |
| Gender | |||||
| Male | 49 (21.4) | 175 (76.4) | 5 (2.2) | 229 | 4.509 (0.105) |
| Female | 24 (13.5) | 151 (84.8) | 3 (1.7) | 178 | |
| Designation | |||||
| Faculty | 3 (25) | 9 (75) | 0 | 12 | 28.72 (0.000)* |
| Residents | 15 (13.6) | 94 (85.5) | 1 (0.9) | 110 | |
| MBBS | 3 (3.9) | 69 (89.6) | 5 (6.5) | 77 | |
| Nursing officers | 50 (24.6) | 151 (74.4) | 2 (1) | 203 | |
| Technicians | 2 (40) | 3 (60) | 0 | 5 | |
| Years of experience | |||||
| <1 | 5 (5.5) | 82 (90.1) | 4 (4.4) | 91 | 23.805 (0.001)* |
| 1-5 | 54 (22.3) | 186 (76.9) | 2 (0.8) | 242 | |
| 5-10 | 6 (11.5) | 45 (86.5) | 1 (1.8) | 52 | |
| >10 | 8 (36.4) | 13 (59.1) | 1 (4.5) | 22 | |
| Previous training | |||||
| Yes | 31 (20.5) | 117 (77.5) | 3 (2) | 151 | 5.1 (0.277) |
| No | 34 (18) | 153 (81) | 2 (1.1) | 189 | |
| May be | 8 (11.9) | 56 (83.6) | 3 (4.5) | 67 | |
*P is significant i.e., <0.05
Association of demographic variables with pretraining knowledge of participants
There was a significant difference found among the mean scores of pretest in relation to age, designation, and the years of their experience of HCPs, as shown in Table 3. Further, in post hoc analysis, Tukey's test was applied to determine the differences within the groups. Younger HCPs were found to have statistically significant higher mean score in both pre- and posttest. In addition, as per designation, MBBS students followed by residents had a higher mean score in pretest than nursing officers and faculties/senior doctors. Furthermore, HCPs with experience of <1 year had a higher mean score in pretest when compared to those having experience of more than 1 year, i.e.,1–5 years and >10 years.
Table 3.
Comparison of mean pre- and post-test knowledge scores for different domains among health-care professionals (n=407)
| Domains | Maximum score | Mean±SD | Estimation of 95% CI | Student’s paired t-test (t) | Paired sample t-test P (two-tailed) | |
|---|---|---|---|---|---|---|
| Pretest score | Posttest score | |||||
| Do and don’t | 2 | 1.1±0.67 | 1.3±0.67 | 0.11-0.24 | 5.5* | 0.001* |
| Hand hygiene | 6 | 3.2±1.40 | 4.1±1.35 | 0.7-0.95 | 12.9* | 0.001* |
| PPE | 4 | 2.0±1.08 | 2.8±1.00 | 0.65-0.88 | 12.9* | 0.001* |
| Cleaning and disinfection | 7 | 3.5±1.19 | 4.7±1.23 | 1.06-1.35 | 16.5* | 0.001* |
| Total | 19 | 9.8±2.62 | 12.8±2.9 | 2.71-3.24 | 22.11* | 0.001* |
*P is significant i.e., <0.05; CI=Confidence interval, SD=Standard deviation, PPE=Personal protective equipment
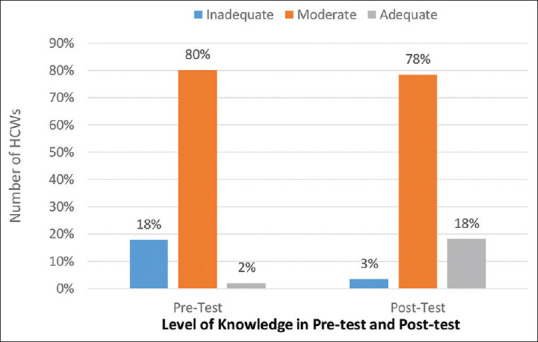
Effect on participant's knowledge of standard and additional precautions covered in video modules
As shown in Table 2, the younger age group (21–25) had higher posttest scores than the other age groups (P < 0.01), with a decrease in posttest scores with the increase in age. Post-training, there was a statistically significant (P < 0.05) increase in knowledge scores in all domains, as illustrated in Table 2. The comparison of pretest and posttest scores of individual questions in different domains among HCPs showed the percentages of correct responses in Figure 2. The percentage of scores obtained in different domains was higher in posttest as compared to the pretest, as shown in Figures 2 and 3. Overall maximum gain in knowledge was observed in the domain of PPE followed by cleaning and disinfection, as shown in Figure 3.
Figure 2.
Comparison of pretest and posttest scores of individual questions in the four domains among health-care professionals (n = 407)
Figure 3.
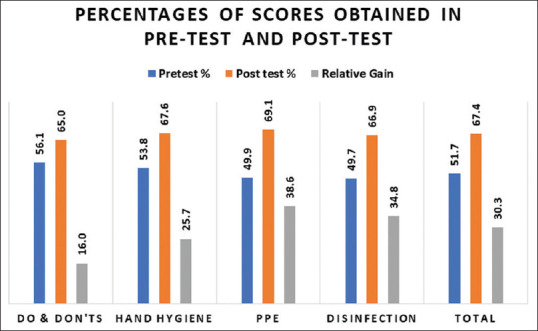
Percentages of scores obtained in pretest and posttest among different domains with relative gain of scores after video training among health-care professionals (n = 407)
Feedback of video-assisted training
All 407 HCPs responded to feedback for the effectiveness of video-assisted training sessions during the posttest, which is illustrated in Figures 4 and 5, in terms of number and percentages of each Likert scale. For the purpose of video training sessions, 17.9%, 38.1%, 37.1%, and 6.9% HCPs responded as for reinforcement, clarification, practice, and review, respectively. Although 96.3% of the participants felt that they had a better understanding of various IPC measures and 96.8% were satisfied with the video modules used for training, yet only 60.9% were willing to recommend these videos to others for learning purposes.
Figure 4.
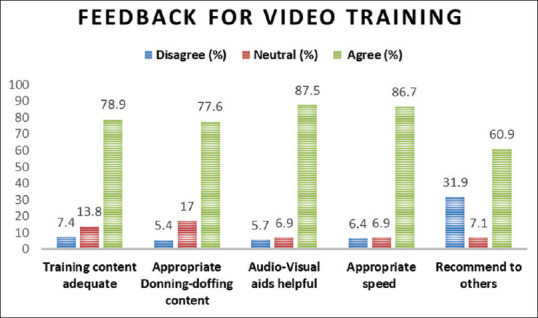
Distribution of feedback questions with each Likert scale of disagree, neutral, and agree in the number and percentage among health-care professionals (n = 407)
Figure 5.

Distribution of feedback questions with each Likert scale of yes, no, and maybe in number and percentage among health-care professionals (n = 407)
Discussion
In the past few months, COVID-19 has become a global health crisis posing a great threat to mankind and challenges to the community as well as to health-care systems. In response to the prodigious spread of COVID-19, intense IPC measures are needed to be reinforced to contain and mitigate the risk of the spread of COVID-19. During the initial phase of the current pandemic, plan for video-assisted training sessions was formulated by the institute's HICT in a short duration along with maintaining caveats of social distancing at the same time to enhance and update the knowledge of HCPs regarding IPC measures.
The training model and related tools, including the video links developed in this study, were published on the institutional website and on all desktops available in the institute such that all HCPs may have access for the videos for reinforcement, similar to studies by Zhou et al. and Lin and Chen.[16,17] Each video training module used in this study was of 7–9 min duration. The technical aspect of video duration was in agreement with the literature, which recommends that videos should not be longer than 15 min.[18]
In this study, before training, 80% of the participants had an overall moderate level of knowledge, whereas only 18% of the participants had an inadequate level of knowledge [Table 1 and Figure 1] in the various domains of training which reflected that most of the HCP's were aware of the IPC measures, which could be the result of previous preservice or in-service IPC training. Similar to our findings, various other studies and experts have reported HCP's have good baseline knowledge regarding IPC practices.[19,20,21]
In our study, the range of pre- and posttest scores of participants was large which reflects varying knowledge of the participants [Table 2 and Supplementary Table 3]. The baseline knowledge among the participants was the highest for MBBS students followed by residents, nursing staff, and faculty. Surprisingly, in our findings, even the gain in knowledge was better in the younger age group with less work experience like MBBS students and residents than those who were more than 35 years or with more work experience or at higher designation like senior doctors. The authors suggest that this may be due to poor attitude toward learning among senior doctors, which may either be due to the lack of acceptance of video modules as a training tool or reluctance to update knowledge through this training session.
In this study, an overall posttest score for hand hygiene was 65%, with a relative gain of 25.7% [Figure 3]. Since average baseline knowledge scores were more than 50% before training, apparently high knowledge gain was not observed. Other studies have also demonstrated medical students and nursing officers having the varying level of knowledge regarding hand hygiene.[22,23] Although a lot of participants scored well, few were still confused regarding moments of hand hygiene (49%) and type of solution to be used at different opportunities (45%). Despite abundant availability of alcohol-based hand rubs and ongoing training activities, participants thought soap and water to be better than alcohol rub in unsoiled hands [Figure 2].
There was 38.6% relative gain in scores of PPE domain, with an average 69.1% postscore [Figure 3], similar to Calabro et al., who reported senior students having 67.7% mean knowledge score about the use of PPE.[24] This is a significant result as donning and doffing of PPE is a critical step to prevent the HCP's from COVID-19 and other transmissible infections. The in-house video for donning and doffing was prepared according to the available logistics in the institute such that any level of staff including housekeeping and security guards may also apprehend the steps easily. Pilieci et al. in their study also showed that demonstration of instructional videos featuring medical skills such as hand disinfection, donning sterile gloves through videos before surgery may contribute significantly in reducing postsurgical infections and increasing patient safety.[25]
In this study, there was a significant gain of 34.8% in the cleaning and disinfection domain [Figure 3], the knowledge of which is of utmost importance to prevent from the transmission of deadly pathogens and prevent healthcare-associated infections. Emphasis on the cleaning schedules of various surfaces and job responsibility was also given to fill in the gaps of knowledge and practice of routine cleaning and disinfection of hospital surfaces, as reported earlier in other studies.[26,27,28] Considering the fact that watching video modules may be a passive experience similar to reading, so to make the most of the training sessions, trainers interacted with the participants before and after each video and cleared their doubts. We took advantage of the mixed method of our training, taking into account findings of this study, and in subsequent trainings, the trainers emphasized more on the points which were not correctly answered in our study along with the repeat demonstration of video modules on request during the class.
The results of the feedback survey revealed the perception of participants about the modules. Apparently, the relative gain in learning outcomes posttraining was around 30%, yet the participants appreciated the videos for covering all necessary infection control-related topics and said that they would refer to videos for revision [Figures 4, 5]. The positive feedback from the participants was a reflection of successful training and suggests that similar training programs may be adapted by other institutes. Similar feedback reports have also been utilized by authors to further improve their trainings.[29]
The video-assisted training was found to be useful in our study and such strategy may be implemented by other hospitals as well as to upgrade their existing training programs in this new normal era of social distancing. Zhou et al. also asserted that the video modules represent an important opportunity for the students to increase and support learning, thus contributing to a better performance of the respective technique.[16] Although the video cannot completely replace face-to-face lessons, it widely contributes to and complements education, as also suggested by Mouneghi et al.[30]
Training targets should include all HCPs including new hospital/medical institution staff as well as outsourced workers. Each video module was prepared as a training tool. Most items in the training model (e.g., guidelines, training CD, training program, and evaluation form) may also be used independently for a variety of purposes. This training model has an extra advantage of enhancement of knowledge with reduced human resources and implementation timing of trainings. In our study, we could not assess the retention of knowledge of the participants and their actual practices at workplaces, which is equally important. Furthermore, due to lack of time, we could not validate the questionnaire before training though they were made and checked by experienced team members of HICT. Future studies may be planned to assess knowledge gain and its retention by video-assisted training in comparison to traditional live training.
Conclusions
In the current new normal of social distancing, the use of video modules for trainings in small batches may be considered. We assert that the utilization of video modules prepared using predefined content may have an advantage over traditional live interactive classes as all the participants receive same training reducing bias of training from different trainers or content of classes. As an additional advantage over live training, video modules may be used for the purpose of revision. This study may be useful for administration board, infection control team, and HCPs working in varied health-care settings, who are facing or may encounter COVID-19 and other such transmissible infections.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank the members of Hospital Infection Control Team of the institute (especially Infection Control Nursing Officers), hospital administration, advanced center for continuous professional development, all study participants and trainers for their helpful participation in this study.
References
- 1.Gilbert GL. Commentary: SARS, MERS and COVID-19-new threats; old lessons. Int J Epidemiol. 2020;49:726–8. doi: 10.1093/ije/dyaa061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–7. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hunter E, Price DA, Murphy E, van der Loeff IS, Baker KF, Lendrem D, et al. First experience of COVID-19 screening of health-care workers in England. Lancet. 2020;395:e77–e78. doi: 10.1016/S0140-6736(20)30970-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burrer SL, de Perio MA, Hughes MM, Kuhar DT, Luckhaupt SE, McDaniel CJ, Porter RM, Silk B, Stuckey MJ, Walters M. Characteristics of health care personnel with COVID-19—United States, February 12–April 9. 2020 doi: 10.15585/mmwr.mm6915e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Geneva: World Health Organization; 2020. [Last accessed on 2020 Mar 17]. World Health Organization. Novel Coronavirus (2019-nCoV): Strategic Preparedness and Response Plan. [Google Scholar]
- 8.World Health Organization; 2020. World Health Organization. Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions: Scientific Brief. [Google Scholar]
- 9.World Health Organization; 2020. World Health Organization. Considerations in Adjusting Public Health and Social Measures in the Context of COVID-19: Interim Guidance; pp. 1–4. [Google Scholar]
- 10.Gupta P, Goyal K, Kanta P, Ghosh A, Singh MP. Novel 2019-coronavirus on new year's Eve. Indian J Med Microbiol. 2019;37:459–77. doi: 10.4103/ijmm.IJMM_20_54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Practical Guidelines for Infection Control in Health Care Facilities, SEARO Regional Publication No. 41, WPRO Regional Publication. 2004:41. 1-103. [Google Scholar]
- 12.MOHFW, National Guidelines for Infection Prevention and Control in Healthcare Facilities. 2020. [Last accessed on 2020 May 20]. Available from: https://www.mohfw.gov.in/pdf/National%20Guidelines%20for%20IPC%20in%20HCF%20-%20final%281%29.pdf .
- 13.Water, Sanitation, Hygiene and Waste Management for COVID-19. [Last accessed on 2020 Mar 05]. Available from: https://www.who.int/publications-detail/water-sanitation-hygiene-and-waste-management-for-covid-19 .
- 14.CPCB, Revision 1: Guidelines for Handling, Treatment and Disposal of Waste Generated during Treatment/Diagnosis/Quarantine of COVID-19 Patients. [Last accessed on 2020 May 28]. Available from : https://www.cpcb.nic.in/uploads/Projects/Bio-Medical-Waste/BMW-GUIDELINES-COVID_1.pdf .
- 15.Hake RR. Interactive-engagement versus traditional methods: A six-thousand-student survey of mechanics test data for introductory physics courses. Am J Phys. 1998;66:64–74. [Google Scholar]
- 16.Zhou T, Huang S, Cheng J, Xiao Y. The distance teaching practice of combined mode of massive open online course micro-video for interns in emergency department during the COVID-19 epidemic period. Telemed J E Health. 2020;26:584–8. doi: 10.1089/tmj.2020.0079. [DOI] [PubMed] [Google Scholar]
- 17.Lin JY, Chen HF. Effects of using multimedia situational teaching in establish nurse-patient relationship for new nurses. Stud Health Technol Inform. 2016;225:615–6. [PubMed] [Google Scholar]
- 18.Hartsell T, Yuen SC. Video streaming in online learning. AACE J. 2006;14:31–43. [Google Scholar]
- 19.Koenig S, Chu J. Senior medical students’ knowledge of universal precautions. Acad Med. 1993;68:372–4. doi: 10.1097/00001888-199305000-00021. [DOI] [PubMed] [Google Scholar]
- 20.Gulilat K, Tiruneh G. Assessment of knowledge, attitude and practice of health care workers on infection prevention in health institution Bahir Dar city administration. Sci J Public Health. 2014;2:384–93. [Google Scholar]
- 21.Ayub A, Goyal A, Kotwal A, Kulkarni A, Kotwal A, Mahen A. Infection control practices in health care: Teaching and learning requirements of medical undergraduates. Med J Armed Forces India. 2013;69:107–12. doi: 10.1016/j.mjafi.2012.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nair SS, Hanumantappa R, Hiremath SG, Siraj MA, Raghunath P. Knowledge, attitude, and practice of hand hygiene among medical and nursing students at a tertiary health care centre in Raichur, India. ISRN Prev Med 2014. 2014 doi: 10.1155/2014/608927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feather A, Stone SP, Wessier A, Boursicot KA, Pratt C. Now please wash your hands’: The handwashing behaviour of final MBBS candidates. J Hosp Infect. 2000;45:62–4. doi: 10.1053/jhin.1999.0705. [DOI] [PubMed] [Google Scholar]
- 24.Calabro K, Weltge A, Parnell S, Kouzekanani K, Ramirez E. Intervention for medical students: Effective infection control. Am J Infect Control. 1998;26:431–6. doi: 10.1016/s0196-6553(98)70041-0. [DOI] [PubMed] [Google Scholar]
- 25.Pilieci SN, Salim SY, Heffernan DS, Itani KMF, Khadaroo RG. A randomized controlled trial of video education versus skill demonstration: Which is more effective in teaching sterile surgical technique? Surg Infect (Larchmt) 2018;19:303–12. doi: 10.1089/sur.2017.231. [DOI] [PubMed] [Google Scholar]
- 26.Kenters N, Gottlieb T, Hopman J, Mehtar S, Schweizer ML, Tartari E, et al. An international survey of cleaning and disinfection practices in the healthcare environment. J Hosp Infect. 2018;100:236–41. doi: 10.1016/j.jhin.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 27.Keah KC, Jegathesan M, Tan SC, Chan SH, Chee OM, Cheong YM, et al. Disinfection: Gaps between recommended and actual practice. Southeast Asian J Trop Med Public Health. 1995;26:795–8. [PubMed] [Google Scholar]
- 28.Allen M, Hall L, Halton K, Graves N. Improving hospital environmental hygiene with the use of a targeted multi-modal bundle strategy. Infect Dis Health. 2018;23:107–13. doi: 10.1016/j.idh.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 29.Keithly M, Brame C, Woelfle M, Friedman K. Abstracts of Papers of the American Chemical Society. Vol. 250. Washington, DC 20036 USA: 1155 16th ST, NW, Amer Chemical Soc. 2015. Blending it up: Active learning in a STEM classroom through the use of on-line materials. [Google Scholar]
- 30.Mouneghi HK, Derakhshan A, Valai N, Mortazavi F. The effectiveness of video-based education on gaining practical learning skills in comparison with demonstrating method's effectiveness among university students. J Med Educ. 2003:4. [Google Scholar]