Abstract
BACKGROUND:
Breast cancer is the most common type of cancer among women and it is the second leading cause of mortality among cancers in women and a major health issue in developed countries. Although there are simple and effective screening methods, just minority of women use them. Given the high prevalence of breast cancer in Isfahan women and the low prevalence of screening behavior, the present study aimed to determine the impact of theory-based educational intervention on breast self-examination (BSE) behavior and mammography.
MATERIALS AND METHODS:
The present experimental study was conducted on 93 women referred to comprehensive health centers in Isfahan through convenience sampling, and by this way 46 women were included in the control group and 47 in the intervention group. Data collection was done by a valid and reliable questionnaire. Furthermore, educational interventions were performed for the intervention group in three sessions. Furthermore, the data were completed in the intervention group before, immediately after, and 3 months after intervention and before and 3 months after intervention in the control group. The data were analyzed by SPSS (16); and paired t-test and repeated measure test were used for analysis in the intervention group and also independent t-test and paired t-test were employed to analyze data of the control group.
RESULTS:
The results showed significant changes in perceived benefit constructs (P = 0.023), knowledge (P < 0.001), self-efficacy (P < 0.001), and behavioral intention regarding BSE (P = 0.035) in the intervention group over time, but changes were not significant in both perceived susceptibility and severity in the intervention group. As far as mammography behavior is concerned, only the perceived benefit construct in the intervention group had significant changes. In terms of the screening behavior, only BSE behavior significantly changed before and after intervention.
CONCLUSION:
The study showed that theory-based education by applying of constructs such as perceived benefits and self-efficacy and intention for BSE model could promote breast cancer screening behavior such as BSE. Therefore, it is suggested that health educators utilize educational texts based on these constructs to increase their influence on individuals via screening behavior for breast cancer.
Keywords: Breast cancer, breast self-examination, cancer screening, education, mammography
Introduction
Breast cancer is a common cancer in developed and developing countries.[1] It is most prevalent in women aged 40–60 years, the second most common cancer in women aged 30–40 years, and the second leading cause of death in women around the world.[2,3] In Iran, there is an increase in the number of newly diagnosed breast cancer patients.[4] The standardized mortality rate is 14.2/100,000 women with an average age of 49.84 years.[5] Breast cancer is diagnosed at advanced stages in Iran.[6] Survival rates decrease if the disease is diagnosed and treated late.[7,8] On the other hand, if breast cancer is diagnosed at an early stage, the survival rates reach above 95%.[6]
There are different diagnostic approaches to an early diagnosis including breast self-examination (BSE), clinical breast examination, and mammography.[9,10] These methods are able to reduce breast cancer mortality up to 50%.[11] Accordingly, women participation is very important; however, they are unaware of such programs due to various reasons related to social and cultural factors, lack of awareness, misconceptions and inadequate understanding of breast cancer risk, unfamiliarity with the concept of screening, lack of education on self-examination, absence of a continuous health information system, economic issues, negative attitude about BSE, lack of individual will as a self-efficacy factor, fear of cancer diagnosis, and embarrassment about breast examination.[12,13,14,15,16,17,18] Studies have shown that the rate of BSE is very low among the Iranian women. A study in Tabriz reported that only 18.8% of women performed BSE.[19] Moreover, a study on health workers in Isfahan also presented that only 39.5% performed BSE.[20] Another study in Ardabil also revealed low BSE.[21] and Mammography rates were low in Iran.[19,21,22,23,24,25,26]
Considering the impact of different factors on such behavior, interventions should be used to affect these factors. The health belief model is a widely used health education model for encouraging people to use screening programs. This model seeks to change individual behaviors by use of five constructs, namely perceived susceptibility, perceived severity, perceived barriers and benefits, and self-efficacy.
As mentioned above, there are various factors affecting these methods usage, including subjective norms, perceived behavioral control, and behavioral intentions that cannot be changed only through the health belief model. Therefore, more effective interventions could be obtained through combining the theory of planned behavior and its constructs with the health belief model.
Several studies have been conducted by employing the health belief model in the field of screening methods.[21,24,27] Moodi et al. found that education based on the health belief model improved awareness and level of BSE in a group of students.[28,29] In another study by Moodi on women over 40 years of age in Isfahan, it was found that education based on the health belief model was also observed to affect mammography behavior.[20] Research has further used the theory of planned behavior indicating the effectiveness of such models in the behavioral change. For instance, Sargazi et al. and Hatefnia et al. reported that education based on such model could promote screening behavior.[30,31] Taymoori and Farhadifar combined two models of health belief and theory of planned behavior for intervention. In this way, Taymoori et al. used both models to promote mammography behavior and Farhadifar et al. utilized them separately. In both studies, the use of these theories also promoted behavior.[32,33]
Education about breast cancer to be affected by the following factors ssuch as: (1) perceived susceptibility (perception of risk of being diagnosed with cancer); (2) perceived severity (perception of seriousness about cancer; (3) perceived benefits (effectiveness of way to detect cancer); (4) perceived barriers (such as don’t have money to obtain service); and (5) self-efficacy (perceived ability to do the behavior);[33] Subjective norms (perception that screening is considered important by others and family; Perceived Behavioral Control (perceptions of their ability to perform behavior); Behavioural intention (an indication of an individual's readiness to perform a given behavior).
It seems that a combination of the two models of health belief and planned behavior can be used to modify behavior by applying some of constructs. Therefore, because there is no study based on both models for promoting mammography and BSE, the present study was carried out to specify the effect of theory-based educational intervention on BSE and mammography behavior.
Materials and Methods
Study design and sampling method
The present experimental study was conducted in two randomly selected comprehensive health centers in Isfahan (2017). Finally, a center was considered as the intervention group and the other as control group based on the draw. Among those who were willing to participate in the study, 93 persons entered into the study after presenting the study objectives and having inclusion criteria. Among them, 46 persons were selected in the control group and 47 in the intervention group. In this study, inclusion criteria included existing an active file in the health center, aged 35 years and older, no history of disease, written informed consent, and willingness to participate in the study. Furthermore, exclusion criteria included not participating in at least a training session and unwillingness to continue participating at any time during the study or getting cancer.
Three months after the intervention, one subject from the control group and two subjects from the intervention group were excluded due to their unwillingness to cooperate, and eventually 45 individuals remained in each group [Figure 1].
Figure 1.
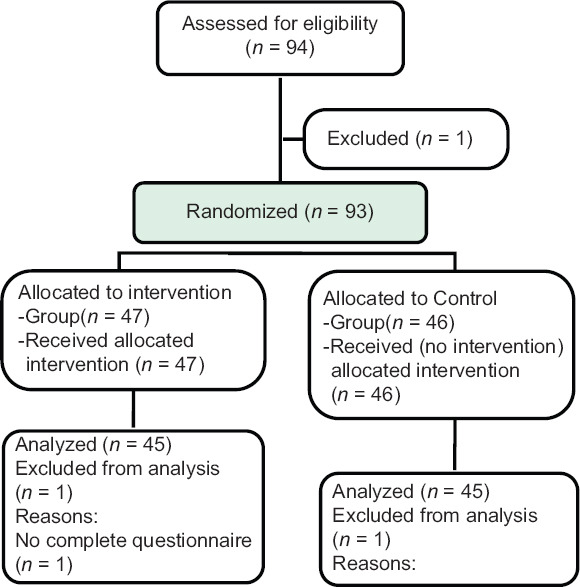
Flow diagram of the participants
Data collection instrument
A 4-part questionnaire was used for data collection in the present study. The first part included demographic information (age, education level, marital status, race, and family history of breast cancer problems). The second part covered breast cancer awareness questions (11 questions). Questions were scored as follows: correct answer: score 3; negative answer: score 1; and the “I don’t know” option: score 2 (score range: 12–36). The questions were derived from a study by Moodi et al.[28]
The third part included questions on the Champion's health belief model scale including perceived susceptibility (3 items), perceived severity (7 items), perceived benefits question about BSE (6 items), perceived benefits for mammography (6 Items), perceived barriers to BSE (9 Items), perceived barriers to mammography (10 items), and perceived self-efficacy (11 items). The susceptibility, severity, and perceived benefits and barriers were scored from strongly agree (5) to strongly disagree (1) according to 5-point Likert scale. Validity and reliability of the questionnaire were confirmed in Taymoori and Berry studies.[34] Taymoori's studies concluded that the Farsi version of the Champion health belief model Scale has the potential to measure beliefs related to BSE and mammography with Iranian women.
The fourth part comprised questions on the theory of planned behavior according to a questionnaire by Sargazi et al., containing behavioral intention constructs (3 items), subjective norms (6 items), perceived behavioral control (6 items), and behavior assessment (3 items). All constructs were scored based on a 5-point Likert scale. Of note, the validity and reliability of the questionnaire were confirmed by Sargazi et al.[30] Reliability of the questionnaire was obtained α > 0.94.
Educational intervention
The educational sessions based on the models was designed for educational interventions. Three sessions were set up in the program, and the educational goals and teaching method of each session were specified, the location of education was health centers, and the educational sessions were conducted by health educator and physician.
Educational sessions were then held for the intervention group as follows:
The first session aimed to introduce the breast structure, types of breast cancer and their risk factors, and the importance of early diagnosis by focusing on perceived susceptibility and severity. The educational content was provided through lecture (educational PowerPoint) and face-to-face training for 45 min. The goal of the second session was to introduce the benefits of BSE and to eliminate barriers such as being embarrassed about it (group discussion method), and the method of BSE was explained by a general practitioner according to a flip chart presented - for emproving self-efficacy on this field. The participants were able to perform individually the steps under the supervision of a physician (role playing) and answer the questions
The third training session focused on the related constructs of self-efficacy (mastery experiences, social modeling, social persuasion, and states of physiology) and perceived barriers performing mammography using instructional videos about mammography method and brainstorming to overcome the barriers. At the end of the final session, educational booklets containing scientifically trained content, which from reference books and approved by a health education and promotion specialist, were given to the individuals to be also studied by their spouses. It should be noted that mobile phone numbers were taken from participants if they had consent, and educational content and videos were provided for participants and their spouses via the Telegram app.
In the intervention group, the questionnaires were completed before intervention, right after, and 3 months following the intervention; however, in the control group, the questionnaires were collected before and 3 month after intervention and they received educational resources after interventions.
Data analysis
After completing the questionnaires, the obtained results were analyzed by the SPSS16 (SPSS Inc., Chicago, IL, USA). The descriptive analysis including mean, standard deviation, and percentage were utilized for data description; moreover, analytical tests such as independent t-test for comparing constructs between two groups in baseline and 3 month after intervention and repeated measures ANOVA were utilized for analyzing constructs of experimental group at three times; paired t-test was used to analyze the data of control group before and after the intervention. Significance level was considered to be 0.05.
Ethical considerations
The present study was approved by the Ethics Committee of Faculty of Medicine, Isfahan University of Medical Sciences, IR.MUI.REC.1396.3.565. To adhere to the principles of medical ethics, the implementation method and research were explained for the selected individual, and written consent to the participate in the research project was obtained after the full explanation. The study was registered on the website of clinical trial with an ID of IRCT20180830040907N1.
Results
The mean age (SD) was 43.69 (8.53) years in the intervention group and 44.02 (7.60) years in the control group (P = 0.845). There was no significant difference between the two groups in terms of race, education, occupational status, and breast cancer incidence [Table 1].
Table 1.
Demographic characteristics of participants in two groups (intervention and control)
| Variables | Intervention | Control | P |
|---|---|---|---|
| Age (mean±SD) | 43.69±8.35 | 44.02±7.60 | 0.845 |
| Education level, n (%) | |||
| Illiterate | 3 (6.7) | 2 (4.4) | 0.058 |
| Reading and writing literacy | 16 (35.6) | 14 (31.1) | |
| High school | 7 (15.6) | 14 (31.1) | |
| Diploma | 19 (42.2) | 11 (24.4) | |
| University | 0 (0.0) | 4 (8.9) | |
| Marital status, n (%) | |||
| Single | 1 (2.2) | 1 (2.2) | 0.329 |
| Married | 39 (86.7) | 43 (95.6) | |
| Divorced | 5 (11.1) | 1 (2.2) | |
| Tribe, n (%) | |||
| Fars | 39 (86.7) | 44 (97.8) | 0.070 |
| Tork | 2 (4.4) | 1 (2.2) | |
| Lor | 4 (8.9) | 0 (0.0) | |
| History of breast problem, n (%) | |||
| Yes | 12 (26.7) | 8 (17.8) | 0.720 |
| No | 32 (71.1) | 36 (80.00) | |
| Don’t know | 1 (2.2) | 1 (2.2) |
SD=Standard deviation
According to the results presented in Table 2, there were no significant differences between the intervention and control groups concerning all constructs except for perceived behavioral intention and self-efficacy and perceived benefits for mammography before the intervention.
Table 2.
The comparison of the mean±standard deviation of integrated model structures in intervention and control groups
| Groups | Baseline | Immediately after intervention | 3 months after intervention | P | |
|---|---|---|---|---|---|
| Knowledge | Intervention | 26.87±2.94 | 30.38±2.83 | 29.40±3.66 | <0.001 |
| Control | 26.27±3.06 | - | 27.22±2.72 | 0.017 | |
| P | 0.345 | 0.002 | |||
| Perceived susceptibility | Intervention | 9.49±2.49 | 9.49±2.48 | 9.72±2.91 | 0.819 |
| Control | 9.71±2.17 | - | 9.76±2.21 | 0.420 | |
| P | 0.653 | 0.935 | |||
| Perceived severity | Intervention | 25.64±5.13 | 26.02±4.69 | 25.71±4.72 | 0.463 |
| Control | 24.36±4.75 | - | 24.40±4.73 | 0.688 | |
| P | 0.219 | 0.192 | |||
| Perceived benefits of BSE | Intervention | 23.71±4.14 | 24.49±3.85 | 24.73±3.55 | 0.023 |
| Control | 22.78±2.89 | - | 22.80±2.90 | 0.710 | |
| P | 0.218 | 0.006 | |||
| Perceived barriers for BSE | Intervention | 30.23±4.51 | 31.57±4.35 | 31.59±4.44 | 0.037 |
| Control | 29.73±4.46 | - | 29.29±4.47 | 0.124 | |
| P | 0.572 | 0.017 | |||
| Self-efficacy for BSE | Intervention | 27.76±10.89 | 39.00±8.59 | 36.04±10.36 | <0.001 |
| Control | 22.84±8.28 | - | 22.58±7.97 | 0.411 | |
| P | 0.018 | <0.001 | |||
| Perceived benefits for mammography | Intervention | 18.04±3.07 | 19.02±3.16 | 19.07±2.93 | 0.001 |
| Control | 19.44±2.28 | - | 19.40±2.28 | 0.728 | |
| P | 0.016 | 0.549 | |||
| Perceived barriers for mammography | Intervention | 19.55±3.22 | 19.95±2.71 | 19.95±2.75 | 0.613 |
| Control | 19.04±4.67 | - | 19.24±4.43 | 0.512 | |
| P | 0.547 | 0.363 | |||
| Subjective norm | Intervention | 23.69±3.21 | 24.09±2.73 | 23.91±2.70 | 0.549 |
| Control | 24.55±3.22 | - | 24.64±3.02 | 0.577 | |
| P | 0.204 | 0.228 | |||
| Perceived behavioral control | Intervention | 22.49±2.47 | 23.18±2.43 | 22.76±2.31 | 0.070 |
| Control | 22.42±2.45 | - | 22.51±2.32 | 0.400 | |
| P | 0.898 | 0.618 | |||
| Intention of BSE | Intervention | 3.91±0.90 | - | 4.06±0.82 | 0.035 |
| Control | 3.46±0.94 | - | 3.42±0.92 | 0.160 | |
| P | 0.305 | 0.044 | |||
| Intention of mammography | Intervention | 3.80±0.97 | 3.93±0.89 | 0.452 | |
| Control | 3.21±1.32 | 3.31±1.35 | 0.852 | ||
| P | 0.512 | 0.011 |
BSE=Breast self-examination
The repeated measures analysis of variance indicated significant changes in the mean knowledge of the intervention group before, immediately after, and 3 months after the intervention; nonetheless, there were no significant changes regarding perceived susceptibility and severity in either groups after the intervention [Table 2].
In terms of BSE, the mean perceived benefits and barriers and self-efficacy of the intervention group changed significantly over time (P < 0.05); nevertheless, the changes were not significantly different in the control group before and after the intervention.
The ANOVA tests also showed that the mean perceived benefits of mammography were significantly different in the intervention group among the three times, but changes were not significant in the control group, and perceived barriers did not change significantly in either groups after the intervention.
In the field of theory of planned behavior, just behavioral intention construct for BSE significantly changed in the intervention group after the intervention; however, other constructs such as the subjective norms and perceived behavioral control were not significantly different in the intervention and control groups after the intervention.
According to Table 3, the percentage of BSE was not significantly different between the intervention and control groups before the intervention, but the difference between the two groups was significant 3 months after the intervention (P < 0.001). On the other hand, there was no significant difference between the two groups in terms of mammography percentages before and after the intervention (P = 0.107). Intragroup analyses revealed a significant increase in the percentages of BSE and mammography in the intervention group (P = 0.001 and 0.031, respectively); nonetheless, there was no significant difference between the two time points (before and after the intervention) in the control group.
Table 3.
Comparison of frequency of behaviors (mammography and breast self- examination) by time and group
| Behaviors | Groups | Baseline (%) | 3 months after intervention (%) | P |
|---|---|---|---|---|
| Breast self-examination | Intervention | 29 (64.4) | 40 (88.9) | 0.001 |
| Control | 23 (51.1) | 24 (53.3) | 0.089 | |
| P | 0.2 | <0.001 | ||
| Mammography | Intervention | 11 (24.4) | 17 (37.8) | 0.031 |
| Control | 9 (20.00) | 10 (22.2) | 0.078 | |
| P | 0.612 | 0.107 |
Discussion
The present study was conducted to determine the impact of theory-based educational intervention based on planned behavior theory and health belief model in order to promote screening behaviors such as mammography and BSE in women referred to Isfahan health centers.
The mean scores of knowledge significantly increased in the intervention group over time, which is consistent with studies by Glanz et al.[35] and Wu and Yu.[36] The slight increase in the mean score of knowledge in the control group might be due to the participants’ sensitivity for receiving information and it occurred because of completion of questionnaires by the group.
Concerning the constructs of health belief model, there was no significant increase in perceived susceptibility and severity in the intervention group, and it was inconsistent with a study by Ghaffari et al.[37] and Karimy et al.[38] In the field of perceived susceptibility, since there were few numbers of questions, the susceptibility was initially high in both the groups. However, the lack of significant changes in perceived severity can be attributed to the non-use of pictures and videos of those with advanced stages of breast cancer as it could increase perceived severity in them. Therefore, attention should be paid to this issue in future studies.
The results further also indicated that the mean perceived benefits significantly increased in the intervention group immediately after and 3 months after the intervention, which reveals the effectiveness of education. However, the control group alteration was not significant. This result was consistent with studies by Ghaffari et al.[37] and Momenyan et al.[39] The use of group discussion seems to have been a strong point in these studies. On the other hand, some studies reported that education was not efficient.[40,41] The cause of these differences is different population.
In addition, mammography-based education significantly increased the mean score of perceived benefit constructs over time, but the changes in the control group were not significant between the times points. These results are inconsistent with previous studies such as Hadizadehtalasaz and Latifnejade[42] and Ghaffari et al.[37] who reported that the mean perceived benefits of mammography were also high in women at the beginning of study. Thus, the changes over time in construct were not significant.
Despite the significant reduction over time was detected in perceived barriers to BSE in the intervention group, perceived barriers to mammography did not significantly decrease in the intervention group, which is consistent with Hadizadehtalasaz and Latifnejade.[42] One of the reasons is the high cost of mammography because it is not free in health national system, often addressed as a barrier by many researchers, for which there is unfortunately no solution. Consistent with other studies, the incremental changes in the perceived benefit score indicate the effectiveness of education.[28,36]
Educational interventions were able to effectively increase the mean self-efficacy scores in the intervention group in the three time points, which is in line with other interventional studies on self-efficacy.[41,43] This implies the role of self-efficacy in behavioral changes; therefore, effective steps can be taken toward it by proper educational method through applying constructs such as mastery experiences, social modeling, social persuasion, and states of physiology. The role of self-efficacy in this field has also been mentioned in the study of Pirzadeh.[44]
In the present study, subjective norms of the intervention group did not change significantly after education sessions, which is compatible with a study by Sargazi et al. The reason is due to the absence of participants’ spouses in the educational sessions. Given the role of spouses as individuals who play a key role in encouraging spouses to perform screening behaviors, as well as an important factor in providing mammography funding, this should be addressed in future studies. Hence, we suggest that effective individuals are trained more in future outlook. In the field of perceived behavioral control construct, the Sargazi et al.'s study reported significant changes in this construct in the intervention group.[30]
Behavioral intention is a construct of the theory of planned behavior in the field of BSE also increased significantly after the intervention, which is consistent with Ghaffari et al.,[37] Fletcher et al.,[45] and Juon et al.;[46] however, the behavioral intention for mammography did not change significantly, possibly due to the impact of perceived barriers on mammography behavioral intention.
Finally, the results showed that the education along with changes in constructs such as awareness, perceived benefits, self-efficacy, and behavioral intention could significantly increase the BSE in participants; on the other hand, the changes were not effective in regard to the mammography. These results were consistent with studies by Ghaffari et al.[37] and Nasir Isfahani et al.[47] Ghaffari et al. combined the above two models, the education changed behavior toward the BSE, but changes in mammography were not significant. Being simple and free, not requiring equipment, and doing lonely are the main reasons for significant impact on BSE, but mammography is costly and needs to visit centers and is time-consuming and costly. Furthermore, the lack of changes in perceived barriers to mammography is another reason for this issue.
Conclusion
The present study revealed that theory-based education by health belief model constructs and theory of planned behavior could promote breast cancer screening behaviors such as BSE; however, it did not affect the mammography behavior; barriers, especially financial, played significant roles in this field. Therefore, care givers are recommended to employ theory-based strategies in their education to promote the BSE behavior. Mammography costs and other barriers should also be reduced these behaviors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The present study was derived from a dissertation on medicine and registered with a number of 396,565. We are grateful to all participants in this project and the officials in the health centers.
References
- 1.Masoudiyekta L, Dashtbozorgi B, Gheibizadeh M, Malehi AS, Moradi M. Applying the health belief model in predicting breast cancer screening behavior of women. Jundishapur J Chronic Dis Care. 2015;4:e30234. [Google Scholar]
- 2.Harirchi I, Kolahdoozan S, Karbakhsh M, Chegini N, Mohseni SM, Montazeri A, et al. Twenty years of breast cancer in Iran: Downstaging without a formal screening program. Ann Oncol. 2011;22:93–7. doi: 10.1093/annonc/mdq303. [DOI] [PubMed] [Google Scholar]
- 3.Plummer M, de Martel C, Vignat J, Ferlay J, Bray F, Franceschi S. Global burden of cancers attributable to infections in 2012: A synthetic analysis. Lancet Glob Health. 2016;4:e609–16. doi: 10.1016/S2214-109X(16)30143-7. [DOI] [PubMed] [Google Scholar]
- 4.Khazaee-Pool M, Montazeri A, Majlessi F, Rahimi Foroushani A, Nedjat S, Shojaeizadeh D. Breast cancer-preventive behaviors: Exploring Iranian women's experiences. BMC Womens Health. 2014;14:41. doi: 10.1186/1472-6874-14-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nafissi N, Khayamzadeh M, Zeinali Z, Pazooki D, Hosseini M, Akbari ME. Epidemiology and histopathology of breast cancer in Iran versus other Middle Eastern countries. Middle East J Cancer. 2018;9:243–51. [Google Scholar]
- 6.Mousavi SM, Montazeri A, Mohagheghi MA, Jarrahi AM, Harirchi I, Najafi M, et al. Breast cancer in Iran: An epidemiological review. Breast J. 2007;13:383–91. doi: 10.1111/j.1524-4741.2007.00446.x. [DOI] [PubMed] [Google Scholar]
- 7.Sim HL, Seah M, Tan SM. Breast cancer knowledge and screening practices: A survey of 1,000 Asian women. Singapore Med J. 2009;50:132–8. [PubMed] [Google Scholar]
- 8.Yavari P, Pourhoseingholi MA. Socioeconomic factors association with knowledge and practice of breast self-examination among Iranian women. Asian Pac J Cancer Prev. 2007;8:618–22. [PubMed] [Google Scholar]
- 9.Doganer YC, Aydogan U, Kilbas Z, Rohrer JE, Sari O, Usterme N, et al. Predictors affecting breast self-examination practice among Turkish women. Asian Pac J Cancer Prev. 2014;15:9021–5. doi: 10.7314/apjcp.2014.15.20.9021. [DOI] [PubMed] [Google Scholar]
- 10.Smith RA, Andrews K, Brooks D, DeSantis CE, Fedewa SA, Lortet-Tieulent J, et al. Cancer screening in the United States, 2016: A review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. 2016;66:96–114. doi: 10.3322/caac.21336. [DOI] [PubMed] [Google Scholar]
- 11.Kashiwagi Y, Kakinohana S. Breast cancer knowledge and preventive behavior among Filipino women in a rural area: A cross-sectional study. Nurs Midwifery Stud. 2016;5:e34300. [Google Scholar]
- 12.Khazaee-pool M, Majlessi F, Foroushani AR, Montazeri A, Nedjat S, Shojaeizadeh D, et al. Perception of breast cancer screening among Iranian women without experience of mammography: A qualitative study. Asian Pac J Cancer Prev. 2014;15:3965–71. doi: 10.7314/apjcp.2014.15.9.3965. [DOI] [PubMed] [Google Scholar]
- 13.Rastad H, Khanjani N, Khandani BK. Causes of delay in seeking treatment in patients with breast cancer in Iran: A qualitative content analysis study. Asian Pac J Cancer Prev. 2012;13:4511–5. doi: 10.7314/apjcp.2012.13.9.4511. [DOI] [PubMed] [Google Scholar]
- 14.Smith RA, Manassaram-Baptiste D, Brooks D, Cokkinides V, Doroshenk M, Saslow D, et al. Cancer screening in the United States, 2014: A review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. 2014;64:30–51. doi: 10.3322/caac.21212. [DOI] [PubMed] [Google Scholar]
- 15.Kim JH, Menon U, Wang E, Szalacha L. Assess the effects of culturally relevant intervention on breast cancer knowledge, beliefs, and mammography use among Korean American women. J Immigr Minor Health. 2010;12:586–97. doi: 10.1007/s10903-009-9246-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Memis S, Balkaya NA, Demirkiran F. Knowledge, attitudes, and behaviors of nursing and midwifery students regarding breast self-examination in Turkey. Oncol Nurs Forum. 2009;36:E39–46. doi: 10.1188/09.ONF.E39-E46. [DOI] [PubMed] [Google Scholar]
- 17.Shamsi M, Neyestani H, Ebrahimipour H, Esmaeili H, Nosrati M. Using social marketing model to persuade the women to do mammography. J Sch Public Health Inst Public Health Res. 2014;12:85–96. [Google Scholar]
- 18.Lamieian M, Heydarnia AR, Ahmadi F, Faghihzadeh S, Aguilar VM. Women's prospect of breast cancer early detection behavior: A qualitative research. J Birjand Univ Med Sci. 2008;15:88–102. [Google Scholar]
- 19.Farshbaf KA, Shahnazi M, Ghahvehchi A, Torabi S. Performance conditions of breast cancer screening methods and its efficient factors among women referring to health centers of Tabriz. Iran J Nurs Res. 2009;4:27–38. [Google Scholar]
- 20.Reisi M, Javadzade SH, Sharifirad G. Knowledge, attitudes, and practice of breast self-examination among female health workers in Isfahan, Iran. J Educ Health Promot. 2013;2:46. doi: 10.4103/2277-9531.117417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salimi Pormehr S, Kariman N, Sheykhan Z, Alavi Majd H. Investigation of breast cancer screening tests performance and affecting factors in women referred to Ardebil's health and medical centers, 2009. J Ardabil Univ of Med Sci Health Serv. 2011;10:310–8. [Google Scholar]
- 22.Banaeian-Borujeni S, Kazemian A, Kheiri S. Knowledge, attitude and practice about breast cancer screening and related factors among women referred to health care centers in Boroujen in 2005. J Shahrekord Univ Med Sci. 2006;7:28–34. [Google Scholar]
- 23.Hatefnia E, Niknami S, Bazargan M, Mahmoodi M, Lamyianm M, Alavi N. Correlates of mammography utilization among working Muslim Iranian women. Health Care Women Int. 2010;31:499–514. doi: 10.1080/07399331003725507. [DOI] [PubMed] [Google Scholar]
- 24.Heidari Z, Mahmoudzadeh-Sagheb H, Sakhavar N. Breast cancer screening knowledge and practice among women in southeast of Iran. Acta Med Iran. 2008;46:321–8. [Google Scholar]
- 25.Kasgari KA, Yagoubi T. “Health believes of women about performing mammography among clients referred to health centers in Sari, Iran”. J Mazanderan Univ Med Sci. 2011;7:683–8. [Google Scholar]
- 26.Moodi M, Rezaeian M, Mostafavi F, Sharifirad GR. Determinants of mammography screening behavior in Iranian women: A population-based study. J Res Med Sci. 2012;17:750–9. [PMC free article] [PubMed] [Google Scholar]
- 27.Khalili S, Shojaiezadeh D, Azam K, Kheirkhah Rahimabad K, Kharghani Moghadam M, Khazir Z. The effectiveness of education on the health beliefs and practices related to breast cancer screening among women referred to Shahid Behtash Clinic, Lavizan area, Tehran, using health belief model. J Health. 2014;5:45–58. [Google Scholar]
- 28.Moodi M, Mood MB, Sharifirad GR, Shahnazi H, Sharifzadeh G. Evaluation of breast self-examination program using Health Belief Model in female students. J Res Med Sci. 2011;16:316–22. [PMC free article] [PubMed] [Google Scholar]
- 29.Rezaeian M, Sharifirad G, Mostafavi F, Moodi M, Abbasi MH. The effects of breast cancer educational intervention on knowledge and health beliefs of women 40 years and older, Isfahan, Iran. J Educ Health Promot. 2014;3:43. doi: 10.4103/2277-9531.131929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sargazi M, Mohseni M, Safar-Navade M, Iran-Pour A, Mirzaee M, Jahani Y. Effect of an educational intervention based on the theory of planned behavior on behaviors leading to early diagnosis of breast cancer among women referred to health care centers in Zahedan in 2013. Iran Q J Breast Dis. 2014;7:45–55. [Google Scholar]
- 31.Hatefnia E, Niknami S, Mahmoudi M, Lamieian M. The Effects of “Theory of Planned Behavior” based education on the promotion of mammography performance in employed women. J Birjand Univ Med Sci. 2010;17:50–8. [Google Scholar]
- 32.Farhadifar F, Molina Y, Taymoori P, Akhavan S. Mediators of repeat mammography in two tailored interventions for Iranian women. BMC Public Health. 2016;16:149. doi: 10.1186/s12889-016-2808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taymoori P, Molina Y, Roshani D. Effects of a randomized controlled trial to increase repeat mammography screening in Iranian women. Cancer Nurs. 2015;38:288–96. doi: 10.1097/NCC.0000000000000185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Taymoori P, Berry T. The validity and reliability of Champion's Health Belief Model Scale for breast cancer screening behaviors among Iranian women. Cancer Nurs. 2009;32:465–72. doi: 10.1097/NCC.0b013e3181aaf124. [DOI] [PubMed] [Google Scholar]
- 35.Glanz K, Rimer BK, Viswanath K. Health behavior and Health Education: Theory, Research, and Practice. San Francisco: John Wiley & Sons; 2008. [Google Scholar]
- 36.Wu TY, Yu MY. Reliability and validity of the mammography screening beliefs questionnaire among Chinese American women. Cancer Nurs. 2003;26:131–42. doi: 10.1097/00002820-200304000-00007. [DOI] [PubMed] [Google Scholar]
- 37.Ghaffari M, Rad TN, Mohammadi S, Rakhshanderou S. Effect of an Intervention on the Breast Cancer Screening Behavior in Women: Application of Integrated Behavioral Model. Int J Prev Med. 2018;9:99. doi: 10.4103/ijpvm.IJPVM_147_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Karimy M, Niknami S, Amin SF, Shamsi M, Hatami A. The relationship of breast self-examination with self-esteem and perceived benefits/barriers of self-efficacy in health volunteers of Zarandieh city. Iran J Breast Dis. 2009;2(2):41–48. [Google Scholar]
- 39.Momenyan S, Rangraz JM, Sanei IF, Adibi GZ, Sarvi F. Prediction of breast self-examination in a sample of nursing and midwifery students Qom city using health belief model, Iran. Q Univ Med Sci J. 2014;8:28–33. [Google Scholar]
- 40.Ebadifard Azar F, Rimaz S. Effects of training breast-cancer screening on female university students’ beliefs. Iran J Obstet Gynecol Infertil. 2012;15:10–7. [Google Scholar]
- 41.Tavafian SS, Hasani L, Aghamolaei T, Zare S, Gregory D. Prediction of breast self-examination in a sample of Iranian women: An application of the Health Belief Model. BMC Womens Health. 2009;9:37. doi: 10.1186/1472-6874-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hadizadehtalasaz F, Latifnejade R. The effect of health education based on health belife model on attitude female students towards breast self examination. J Birjand Univ Med Sci. 2004;1:25–30. [Google Scholar]
- 43.Aghamolaei T, Hasani L, Tavafian SS, Zare S. Improving breast self-examination: an educational intervention based on health belief model. Iran J Cancer Prev. 2011;4(2):82–87. [Google Scholar]
- 44.Pirzadeh A. Application of the health belief model in breast self-examination by Iranian Female University Students. Int J Cancer Manag. 2018;11:e7706. [Google Scholar]
- 45.Fletcher SW, Harris RP, Gonzalez JJ, Degnan D, Lannin DR, Strecher VJ, et al. Increasing mammography utilization: A controlled study. J Natl Cancer Inst. 1993;85:112–20. doi: 10.1093/jnci/85.2.112. [DOI] [PubMed] [Google Scholar]
- 46.Juon HS, Choi S, Klassen A, Roter D. Impact of breast cancer screening intervention on Korean-American women in Maryland. Cancer Detect Prev. 2006;30:297–305. doi: 10.1016/j.cdp.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 47.Nasiri Isfahani S, Rajabi N, Zakeri P. Predictive Factors of Mammography Based on Health Belief Model in Healthy Volunteers in Isfahan City Healthcare Centers. IJCA. 2019;1(3):38–45. [Google Scholar]


