Abstract
BACKGROUND:
To have a thorough understanding of epidemic surveillance, it is essential to broaden our knowledge of death tolls worldwide. This study aimed to determine the age-standardized mortality rate (ASMR) and predictors of mortality among coronavirus disease 2019 (COVID-19) patients.
MATERIALS AND METHODS:
In this cross-sectional design, all COVID-19 patients with a positive polymerase chain reaction test in the population covered by Arak University of Medical Sciences (AUMS) were entered to the study. Data collection was conducted by phone interview. The study variables comprised age, sex, coronary heart diseases, diabetes, and some symptoms at admission. The adjusted odds ratio (OR) and 95% confidence intervals (CIs) were obtained by logistic regression. The direct method was applied to calculate ASMR (per 100,000) of COVID-19. The analysis was applied by STATA software 12.0.
RESULTS:
A total of 208 cases of COVID-19 (out of 3050 total infected cases) were dead and 2500 cases were recovered. The mean age of dead patients was 70 years. The COVID-19 fatality rate in the population equaled 6.8%; in those patients who were 70 years old or more, however, the case fatality rate was 16.4%. The ASMR of COVID-19 was 12.9 (CI 95%: 11.2, 14.8). The odds of COVID-19-related death in the age over 60 were 10.87 (CI 95%: 6.30, 18.75) times than lower 45 years old. Moreover, it was observed that COVID-19 significantly increased the odds of COVID-19-related death in diabetes patients (OR = 1.45, CI 95%: 1.02, 2.06, P = 0.036).
CONCLUSION:
The ASMR of COVID-19 was relatively higher in males than females. In general, the COVID-19 fatality rate was relatively high. We found that older age and diabetes can have impact on the death of COVID-19, but the headache was found to have a negative association with the COVID-19-related death.
Keywords: Age-standardized, COVID-19, epidemiology, Iran, mortality
Introduction
The novel severe acute respiratory syndrome coronavirus 2 caused the coronavirus disease 2019 (COVID-19) and has resulted in a pandemic reported from nearly every country around the world.[1,2] On January 30, 2020, the World Health Organization (WHO) declared the outbreak of COVID-19 as a public health emergency of international concern.[3] The total number of identified COVID-19 infections has been 5,204,508 across the world and 133,521 cases in Iran at the time of writing this article (May 25, 2020).[4] Of all these patients, 337,687 cases have died worldwide and 7359 cases have died in Iran.[4] The community transmission of COVID-19 has occurred at the onset of the epidemic in Iran since February 20, 2020, including the study setting; the area covered by Arak University of Medical Sciences (AUMS). This region was also among the first to implement intensive public health interventions aiming to decrease the transmission of infection, including social distancing for all populations, establishing a “stay at home”’ campaign, closing all schools and universities, closing mosques and reducing working hours, evaluating infection symptoms of passengers at the entrances and exits of cities, conducting the mass screening, and banning vehicle movements within cities. Hence, it is crucially important to understand the impact of these interventions to inform health policymakers to control the epidemic. Although there are very vague points in the natural history of the infection, mortality as the endpoint is the most important outcome.
The rapid increase in the number of COVID-19 cases worldwide, including Iran, has persuaded researchers to pay attention to the trend of morbidity and predict the epidemic size and epidemiology of infection. In addition, it has been reported that considering the mortality has been lower than the morbidity. Hence, the epidemiology of COVID-19 in the world, including Iran, remains poorly described, especially mortality rates related to the patients’ age and sex and the predictors of mortality even though it has been predicted that the epidemic in autumn and winter may seriously challenge the community in terms of morbidity and mortality of COVID-19.
In order to have a clearer picture of the epidemic surveillance, it is of key importance to increase our information regarding the mortality of the infection. Mortality analysis should be employed for guidance in control of the pandemic.[5] Therefore, we aimed to determine the age-standardized mortality rate (ASMR) and the predictors of mortality among COVID-19 patients in the center area of Iran in 2020.
Materials and Methods
The study area covered by AUMS was located in the center of Iran. According to the 2016 census, this area has a population of 1,429,475.[6] In this analysis, we included all COVID-19 patients with a diagnosis of probable and confirmed cases based on the WHO case definition. All diagnosed and dead cases were registered in the Vice Presidency Department of Health of AUMS. This study was approved by the Ethics Committee of AUMS (Ethic Code: IR.ARAKMU.REC.1398.335).
Variables
All participants who had polymerase chain reaction (PCR) on oropharyngeal/nasopharyngeal swab specimens, in viral transport media, were referred to the Specialized Virology laboratory of Emam Reza clinic (AUMS, Arak, Iran). Viral RNA was extracted using the QIAamp DSP Virus Kit (Qiagen, Hilden, Germany) in QIAcube extractor machines (Qiagen), based on the standard protocol of the manufacturer. Reverse-transcription real-time PCR (RT-qPCR) assays were performed using the 2019-nCoV Nucleic Acid Diagnostic Kit (Sansure biotech, Changsha, China), according to the manufacturer's protocol.[7]
The study variables included the age group (<5, 5–15, 16–45, 46–60, 61–70, and ≥70 years old), sex (male/female), coronary heart diseases (CHDs) (yes/no), diabetes Type 2 (yes/no), symptoms at admission fever (yes/no), dry cough (yes/no), dyspnea (yes/no), fatigue (yes/no), skeletal pain (yes/no), sore throat (yes/no), diarrhea (yes/no), headache (yes/no), and chest pain (yes/no). The data were collected by self-reported forms from the patients and for dead patients from the nearest surrogate relatives. The outcome variable (death) was determined based on death certificates.
Statistical analysis
The statistical analyses of the study were done by STATA 12.0. Frequency distributions and percentages were calculated for all the study variables. The logistic regression was applied for univariate analysis. The adjusted odds ratio (OR) and 95% confidence interval (CI) were obtained by unconditional logistic regression. The criteria for inclusion in the final model were based on a P < 0.2. In order to determine the regression line of death number by days from the1s t day of the epidemic (February 20, 2020)[2] until May 9, 2020. Regression coefficients and the related figures were also observed [Figure 1]. Furthermore, the ASMR (per 100,000) of COVID-19 was obtained. The direct method was applied to calculate ASMRs. The ASMRs of COVID-19-related death per 100,000 population were adjusted to the world standard population.[6,8] ASMRs with 95% CI estimations were obtained by the provided command in STATA 12.0.[6,9] The significance level was assigned as a P < 0.05.
Figure 1.
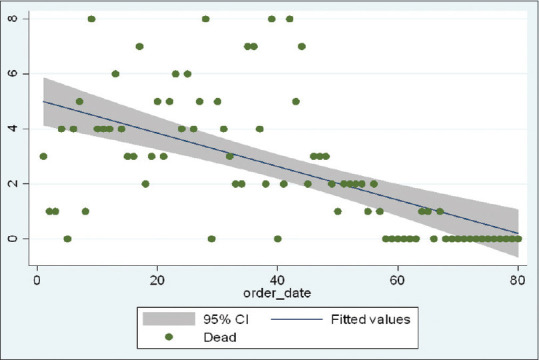
Trend of COVID-19 related death in Arak university of medical sciences, Iran, 2020
Results
The analysis was conducted on the probable and confirmed cases of COVID-19 from February 20 to May 9, 2020. A total of 3050 cases of COVID-19 infections were included. In this time period, 208 COVID-19-related deaths occurred in the study region. There was no statistically significant difference in the number of COVID-19-related deaths between males (n = 114) and females (n = 94) (P = 0.314). The mean age of dead patients was 70 years (standard deviation 15 and range 17, 99). The majority of dead patients (56.3%, n = 117) were over 70 years of age, and no death was observed in the patients who were 16 years old or younger. Mortality rates per 10,000 population in the different cities of the study region were 7.94 (Delijan), 4.01 (Tafresh), 3.33 (Khondab), 2.89 (Mahalat), 2.76 (Farahan), 2.47 (Komijan), 2.45 (Ashtian), 1.53 (Shazand), and 1.42 (Arak).
COVID-19 fatality rate in the population was found to be 6.8% in the study region: Mahalat (10.8%), Delijan (10.2%), Khondab (9.5%), Komijan (9.2%), Shazand (7.5%), Tafresh (7.5%), Arak (5.3%), Farahan (5.2%), and Ashtian (4.5%). Furthermore, in the category of age group, the case fatality rates (CFRs) were 16.4% (over 70 years old), 8.9% (61–70 years old), 5.6% (46–60 years old), and 1.3% (16–45 years old).
The number of COVID-19 deaths decreased in the study period time. From the 1st day of the epidemic onward, a statistically significant decrease (P = 0.001) was observed in the number of deaths [Figure 1]. According to Table 1, the calculated ASMR of COVID-19 for the population was 12.9 (CI 95%: 11.2, 14.8). In addition, it was observed that ASMR was higher among males (14.8 [CI 95%: 12.2, 17.9] per 100,000 population) than among females (11.1 [CI 95%: 8.9, 13.7] per 100,000 population).
Table 1.
Age-standardized rate (per 100,000) for coronavirus disease 2019-related death in Arak, Iran, 2020
| Sex | Number of death | Number of population | Crude rate | ASMR (95% CI) |
|---|---|---|---|---|
| Female | 94 | 703,724 | 13.4 | 11.1 (8.9-13.7) |
| Male | 114 | 725,751 | 15.7 | 14.8 (12.2-17.9) |
| Total | 208 | 1,429,475 | 14.6 | 12.9 (11.2-14.8) |
ASMR=Age-standardized mortality rate per 100,000 population, CI=Confidence interval
In order to determine of COVID-19 death-related factors in univariate analysis, the statistically significant associations were observed between COVID-19 death and age (P = 0.001), having CHD (P = 0.001), having diabetes (P = 0.001), having shortness of breath (P = 0.001), having headache (P = 0.003), and having chest pain at admission (P = 0.019) [Table 2].
Table 2.
Univariate analysis of the included variables for coronavirus disease 2019-related death in Arak University of Medical Sciences, 2020
| Variables | Death | OR (95% CI) | P | |
|---|---|---|---|---|
| No | Yes | |||
| Age, mean (SD) | 51 (21) | 70 (15) | 1.05 (1.04-1.06) | 0.001 |
| Age group | ||||
| 0-45 | 1223 | 15 | ||
| 46-60 | 620 | 37 | 4.87 (2.65-8.93) | 0.001 |
| >60 | 999 | 156 | 12.73 (7.45-21.77) | |
| Sex | ||||
| Male | 1455 | 114 | 1.16 (0.87-1.53) | 0.315 |
| Female | 1387 | 94 | 1 | |
| CHD | ||||
| No | 2295 | 133 | 1 | |
| Yes | 547 | 75 | 2.37 (1.76-3.19) | 0.001 |
| Diabetes | ||||
| No | 2504 | 157 | 1 | |
| Yes | 338 | 51 | 2.41 (1.72-3.37) | 0.001 |
| Symptoms at admission | ||||
| Fever | ||||
| No | 1336 | 103 | 1 | 0.48 |
| Yes | 1506 | 105 | 0.9 (0.68-1.20) | |
| Dry cough | ||||
| No | 1166 | 92 | 1 | 0.37 |
| Yes | 1676 | 116 | 0.88 (0.66-1.16) | |
| Dyspnea | ||||
| No | 1592 | 90 | 1 | 0.001 |
| Yes | 1250 | 118 | 1.67 (1.26-2.22) | |
| Fatigue | ||||
| No | 2300 | 159 | 1 | 0.12 |
| Yes | 542 | 49 | 1.31 (0.94-1.83) | |
| Skeletal pain | ||||
| No | 2253 | 172 | 1 | 0.24 |
| Yes | 589 | 36 | 0.8 (0.55-1.16) | |
| Sore throat | ||||
| No | 2324 | 178 | 1 | 0.17 |
| Yes | 518 | 30 | 0.76 (0.51-1.13) | |
| Diarrhea | ||||
| No | 2710 | 200 | 1 | 0.6 |
| Yes | 132 | 8 | 0.82 (0.4-1.7) | |
| Headache | ||||
| No | 2456 | 195 | 1 | 0.003 |
| Yes | 386 | 13 | 0.42 (0.24-0.75) | |
| Chest pain | ||||
| No | 2732 | 193 | 1 | 0.019 |
| Yes | 110 | 15 | 1.93 (1.1-3.38) | |
OR=Odds ratio, CI=Confidence interval
In the multiple logistic regression analysis, first, all variables were included in the model; next, the variables with P > 0.2 were excluded. Finally, in the final model, the odds of death in the age group ≥60 were 10.87 (CI 95%: 6.30, 18.75) and in the 45–60 age group were 4.38 (2.38, 8.08) times more than the <45 age group (P = 0.001). Males showed a positive association with COVID-19 death after adjusting the effects of other including variables (OR = 1.23, 95% CI: 0.92, 1.65, P = 0.16). Diabetes patients had a statistically significant increase in the odds of COVID-19 death (OR = 1.45, CI 95%: 1.02, 2.06, P = 0.036). Assuming adjustment for the studied variables, determining the association of having dyspnea at admission and COVID-19-related death, OR was found to be 1.33 (95% CI: 0.99, 1.78, P = 0.057). Having headache at admission was also associated with a decreased odd of COVID-19 death (OR = 0.59, 95% CI: 0.33, 1.07, P = 0.081). Finally, it was revealed that COVID-19 patients who had chest pain at admission were significantly more likely to experience death compared to those who did not have chest pain at admission (OR = 1.89, CI 95%: 1.05, 3.39, P = 0.033) [Table 3].
Table 3.
Factors related to death from coronavirus disease 2019 in adjusted logistic analysis
| Variables | OR (95% CI) | P |
|---|---|---|
| Age group | ||
| <45 | 1 | |
| 46-60 | 4.38 (2.38-8.08) | 0.001 |
| ≥60 | 10.87 (6.30-18.75) | 0.001 |
| Sex | ||
| Female | 1 | |
| Male | 1.23 (0.92-1.65) | 0.16 |
| Diabetes | ||
| No | 1 | |
| Yes | 1.45 (1.02-2.06) | 0.036 |
| Dyspnea | ||
| No | 1 | |
| Yes | 1.33 (0.99-1.78) | 0.057 |
| Headache | ||
| No | 1 | |
| Yes | 0.59 (0.33-1.07) | 0.081 |
| Chest pain | ||
| No | 1 | |
| Yes | 1.89 (1.05-3.39) | 0.033 |
OR=Odds ratio, CI=Confidence interval
Discussion
The results of the study showed that the ASMRs of COVID-19 were relatively higher in males than in females. The infection fatality rate was 6.8%. Moreover, age, diabetes, and chest pain had significant impacts on the odds of COVID-19 death. However, the dyspnea was an important symptom by considering the odds of COVID-19 death, but headache had a protective factor on the COVID-19 death. The other studied factors, including CHD, sex, fever, dry cough, fatigue, skeletal pain, sore throat, and diarrhea at admission, were not significantly associated with COVID-19-related death.
Li et al.[10] indicated that some CHD-related factors, such as hypertension, cardiac injury, and hyperglycemia, were associated with death in patients with severe COVID-19. However, in this study, CHD-related factors were not associated with COVID-19 death. One of the potential reasons may be our applied analysis among all patients with severe and nonsevere forms of COVID-19, whenever, Li et al.[10] reported the same findings only among severe types of the disease. Although, in this study, we analyzed the subgroups of severe and nonsevere patients, the sufficient sample size was not available in the study region. Furthermore, Li et al.[10] reported that male sex is an important factor for death resulting from COVID-19. Likewise, in our study, the calculated ASMR of COVID-19 in males was higher than in females, but in adjusted analysis for the OR, a statistically significant association was not observed. In addition, similar to this study, having diabetes has been emphasized as an important variable for the death of COVID-19 patients. It should be highlighted that because of the noncomparability of the study populations between this study and Li et al.'s study,[10] these interpretations should be interpreted with caution.
In line with the findings of this study, Zhou et al.[11] reported that older age was a potential risk factor for COVID-19-related death in Wuhan, China; moreover, they could not find any associations between CHD and death in COVID-19 patients. In another study in China, Du et al.[12] demonstrated that older age and CHD-related factors were predictors of mortality among the patients suffering from COVID-19. Besides, according to the study conducted in the U. S.,[13] a small increase in PM 2.5 could increase the county's COVID-19 mortality rate. On the other hand, Arak is an industrial city and is exposed to industrial pollutants including PM 2.5, and as seen in this study, the mortality of COVID-19 in Arak was lower than other cities where they have very low pollution. Nevertheless, Arak has higher access to medical facilities, such as medical care personnel, intensive care units, hospital beds, and medical equipment compared to other cities in the region; therefore, such facilities seem to be one of the reasons for the lower mortality and infection fatality rates of COVID-19 in Arak. Furthermore, Ji et al.[14] emphasized the role of substantial regional disparities in health-care resource availability and accessibility in COVID-19-related death.
According to Jordan et al.,[15] the CFR of COVID-19 could be as high as 1%; in this study, it was calculated as 6.8%. Considering severe and critical clinical symptoms for categorized confirmed cases, it was estimated that the infection fatality rates should be lower than 6.8%. In the Italian population,[16] the CFR was 7.2%, which was near to the estimation made in this study. In agreement with the findings of this study, the CFR was 16.3% among Italian individuals who were 70 years old or older.[16] There were broad differences in estimated CFR related to COVID-19 between and among countries and local levels. Furthermore, the estimated CFR may be misleading. One of the reasons for this may be more or less probability to find or report COVID-19 deaths. Other reasons may be various policies for case finding and PCR testing; because of insufficient accessibility and financial limitations of PCR kit that under-reported the number of cases or deaths. Moreover, accessibility to the PCR test varied at different time lags. In addition, there were many differences in the quality of provided swab specimens in local levels. Therefore, the estimated CFR may be overshadowed by these.[17]
This analysis supports the hypothesis proposed by Bhopal and Bhopal[18] that the number of cases in males versus women was not dissimilar, but the reason for the difference between deaths could be leading to a range of hypotheses, from lifestyles to differences in chromosomal structure. In addition, according to Bhopal and Bhopal,[18] it was indicated that differences in occupation, smoking, alcohol use, medical comorbidities, or use of medications and social and cultural factors between males and women were more explanatory than genetic structure. Moreover, Kadel and Kovats[19] suggested that respiratory viral infections are more prevalent among males than females.
Furthermore, air pollution is an important risk factor influencing COVID-19.[20] The region covered by AUMS is exposed to air pollution due to petrochemical industries and road traffic.[6] In addition, population with chronic exposure to high levels of air pollution, such as Arak, the center of Markazi province, are susceptible to develop respiratory infections that may be a potentially indirect or direct risk factor to affect COVID-19.
Similarly with this study, findings of a systematic review and meta-analysis[21] were indicated that older age and male gender were most prone to death related to COVID-19; likewise, diabetes Type 2 significantly increased the risk of mortality of COVID-19. Furthermore, in line with the findings of this study, headache had a negative association with mortality due to COVID-19. Similarly, diabetes patients had a 3-fold risk of mortality of influenza.[21] One of the reasons for this finding may be the importance of glycemic control in diabetes Type 2 patients, other reasons may be insufficient immunity due to a decrease in T cell counts, release of inflammatory mediators, especially, interleukin-1 β and tumor necrosis factor α, which stimulates insulin resistance and β-cell damage, and higher levels of various inflammatory factors.[22,23]
Based on our findings of the importance of diabetes and the risk of COVID-19, people with diabetes are recommended to regularly control glycemic values and to have pneumococcal and annual influenza vaccinations.[24] Valid and reliable measurements of cause-specific mortality is an important principle in epidemiologic studies.[5] As COVID-19-related deaths are increasing, mortality analysis can potentially be susceptible to information bias, including nondifferential and differential misclassification bias.[25,26] Therefore, these considerations were the limitations of this study. Furthermore, the definition of COVID-19-related death may be different among countries, and hence any comparisons should be made cautiously.[16] Moreover, it considered probable cases as COVID-19-related deaths because we could not run an RT-PCR test for dead patients. One of the strengths of this study, however, was a registry system recording deaths in the study area. In other words, the findings were population-based, whereas in another study,[20] the delay of ascertainment of COVID-19 deaths was a challenging problem. In the estimation of the mortality studies related to COVID-19, there are some limitations that they should be considered in the interpretation of the findings and even may be a source of potential biases. At the beginning of an outbreak, severe and fatal death cases are more likely to detect and report, and any delay in reporting of deaths may underestimate the CFR. Moreover, some deaths occurring in epidemic may attribute to other causes.[17] It is possible to record and report incorrectly all deaths that it led to information bias; this information bias may be adjusted by the use of methodological considerations on simulation of estimations. This requires knowing the sensitivity and specificity of the surveillance system in reporting of deaths.[25,26]
Thus, it is recommended that the findings of this study be updated in future months. Moreover, it is necessary to conduct more studies on survival analysis and the impact of other factors on the COVID-19 death in this area to optimize our understanding. The quality of the data collection procedure is the most important issue that is recommended to the health policymakers be considered.
This study indicated that some background characteristics such as age, gender, diabetes, other diseases and so on are effective on COVID-19 burden of disease and death. These factors are those that Primary Health Care (PHC) system of Iran have worked on them for more than 4 decades and has readiness to provide educational, preventive, referring, and follow-up patients to final recovery. This system has the required infrastructures, skilled human resource, equipment, and above all is widespread around the country from the farthest villages to cities and from the most mountainous places to deserts, and in the other words, from everywhere people live and work. So utilization of this system can reduce the burden of COVID-19 and decrease the number of severe cases visiting hospitals.[27,28]
Conclusion
It was concluded that the ASMRs of COVID-19 were relatively higher in males than females. The COVID-19 fatality rate was relatively high. We found that older age, diabetes, and having chest pain and dyspnea have had an impact on the death of COVID-19 patients, but the headache was a protective association with COVID-19-related death. The factors associated with mortality-related COVID-19 found in this study may help policymakers to consider them in future preventive strategies in order to support and more attention to the health status of the high-risk groups. These strategies can be focused on primary, secondary, and tertiary prevention levels to diminish mortality-related COVID-19.
Financial support and sponsorship
This study has been supported financially by AUMS, Arak, Iran (Grant number: 3608).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This study was supported by AUMS, Arak, Iran (Grant number: 3608, Ethic code: IR.ARAKMU.REC.1398.335). The authors thank the Research Deputy and Health Deputy of AUMS.
References
- 1.Lewnard JA, Liu VX, Jackson ML, Schmidt MA, Jewell BL, Flores JP, et al. Incidence, clinical outcomes, and transmission dynamics of severe coronavirus disease 2019 in California and Washington: Prospective cohort study. BMJ. 2020;369:m1923. doi: 10.1136/bmj.m1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moradzadeh R. The challenges and considerations of community-based preparedness at the onset of COVID-19 outbreak in Iran, 2020. Epidemiol Infect. 2020;148:e82. doi: 10.1017/S0950268820000783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sohrabi C, Alsafi Z, O’Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–6. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Technical Reports of World Health Organization; 25 May. 2020. [Last accessed on 2020 Nov 29]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200524-covid-19-sitrep-125.pdf?sfvrsn=80e7d7f0_2 .
- 5.Rao C. Medical certification of cause of death for COVID-19. Bull World Health Organ. 2020;98:298–298A. doi: 10.2471/BLT.20.257600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moradzadeh R, Anoushirvani AA. Trend of gastric cancer incidence in an area located in the Center of Iran: 2009-2014. J Gastrointest Cancer. 2020;51:159–64. doi: 10.1007/s12029-019-00227-8. [DOI] [PubMed] [Google Scholar]
- 7.Health Emergencies Preparedness and Response, WHO Global. Diagnostic Testing for SARS-CoV-2, Interim Guidance 11 September 2020. WHO REFERENCE NUMBER: WHO/2019-nCoV/laboratory/ 2020. [Last accessed on 2020 Sep 17]. p. 6. Available from: https://www.who.int/publications/i/item/diagnostic-testing-for-sars-cov-2 .
- 8.McGahan CE, Linn K, Guno P, Johnson H, Coldman AJ, Spinelli JJ, et al. Cancer in first nations people living in British Columbia, Canada: An analysis of incidence and survival from 1993 to 2010. Cancer Causes Control. 2017;28:1105–16. doi: 10.1007/s10552-017-0950-7. [DOI] [PubMed] [Google Scholar]
- 9.Consonni D, Coviello E, Buzzoni C, Mensi C. A command to calculate age-standardized rates with efficient interval estimation. Stata J. 2012;12:688–701. [Google Scholar]
- 10.Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146:110–118. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Du RH, Liang LR, Yang CQ, Wang W, Cao TZ, Li M, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: A prospective cohort study. Europ Resp J. 2020;55:2000524. doi: 10.1183/13993003.00524-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu X, Nethery RC, Sabath BM, Braun D, Dominici F. Exposure to air pollution and COVID-19 mortality in the United States: A nationwide cross-sectional study. Sci Adv. 2020;6:abd4049. doi: 10.1126/sciadv.abd4049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ji Y, Ma Z, Peppelenbosch MP, Pan Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Health. 2020;8:e480. doi: 10.1016/S2214-109X(20)30068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jordan RE, Adab P, Cheng KK. Covid-19: Risk factors for severe disease and death. BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- 16.Kazemi-Karyani A, Safari-Faramani R, Amini S, Ramezani-Doroh V, Berenjian F, Dizaj MY, Hashempour R, Dizaj JY. World one-hundred days after COVID-19 outbreak: Incidence, case fatality rate, and trend. J Educ Health Promot. 2020;9:1–10. doi: 10.4103/jehp.jehp_483_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization Team. Department of Communications, Global Infectious Hazard Preparedness, WHO Global. Estimating mortality from COVID-19. WHO REFERENCE NUMBER: WHO-2019-nCoV-Sci_Brief-Mortality-2020. COVID-19: Scientific Briefs; 1 August. 2020. [Last accessed on 2020 Sep 18]. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci-Brief-Mortality-2020.1 .
- 18.Bhopal SS, Bhopal R. Sex differential in COVID-19 mortality varies markedly by age. Lancet. 2020;396:532–3. doi: 10.1016/S0140-6736(20)31748-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kadel S, Kovats S. Sex hormones regulate innate immune cells and promote sex differences in respiratory virus infection. Front Immunol. 2018;9:1653. doi: 10.3389/fimmu.2018.01653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Michelozzi P, de’Donato F, Scortichini M, de Sario M, Noccioli F, Rossi P, et al. Mortality impacts of the coronavirus disease (COVID-19) outbreak by sex and age: Rapid mortality surveillance system, Italy, 1 February to 18 April 2020. Euro Surveill. 2020;25:1–5. doi: 10.2807/1560-7917.ES.2020.25.19.2000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mojtaba S, Maryam T, Yousef A, Sima A, Hadiseh H. Factors associated with mortality in COVID-19 patients: A systematic review and meta-analysis. Iran J Public Health. 2020;49:1211–1221. doi: 10.18502/ijph.v49i7.3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Odegaard JI, Chawla A. Connecting type 1 and type 2 diabetes through innate immunity. Cold Spring Harb Perspect Med. 2012;2:a007724. doi: 10.1101/cshperspect.a007724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guo L, Wei D, Zhang X, Wu Y, Li Q, Zhou M, et al. Clinical features predicting mortality risk in patients with viral pneumonia: The MuLBSTA score. Front Microbiol. 2019;10:2752. doi: 10.3389/fmicb.2019.02752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gupta R, Ghosh A, Singh AK, Misra A. Clinical considerations for patients with diabetes in times of COVID-19 epidemic. Diabetes Metab Syndr. 2020;14:211–2. doi: 10.1016/j.dsx.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moradzadeh R, Mansournia MA, Baghfalaki T, Nadrian H, Gustafson P, McCandless LC. The impact of maternal smoking during pregnancy on childhood asthma: Adjusted for exposure misclassification; results from the National Health and Nutrition Examination Survey, 2011-2012. Ann Epidemiol. 2018;28:697–703. doi: 10.1016/j.annepidem.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 26.Moradzadeh R, Mansournia MA, Ghiasvand R, Baghfalaki T, Nadrian H, Holakouie-Naieni K. Impact of age at menarche on breast cancer: The assessment of recall Bias. Arch Iran Med. 2019;22:65–70. [PubMed] [Google Scholar]
- 27.Koolivand A, Amini S. The importance of PHC-based measures in controlling COVID-19 outbreak: implications for global health system. Ethics, Med Public Health. 2020;14:1–3. doi: 10.1016/j.jemep.2020.100549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nazari J, Amini S, Amiresmaili M. Lessons learned to control COVID-19 to prevent a crisis: the case of Iran. Open Publ Health J. 2020;13:1–2. [Google Scholar]


