Summary
After the March–April 2020 coronavirus disease 2019 (COVID‐19) outbreak, a second contagion wave afflicted Europe in the autumn. The present study aimed to evaluate sleep health/patterns of Italians during this further challenging situation. A total of 2,013 Italians longitudinally participated in a web‐based survey during the two contagion peaks of the COVID‐19 outbreak. We investigated the risk factors for sleep disturbances during the second wave, and we compared sleep quality and psychological well‐being between the two assessments (March–April and November–December 2020). Female gender, low education, evening chronotype, being a high‐risk person for COVID‐19 infection, reporting negative social or economic impact, and evening smartphone overuse predicted a higher risk of poor sleep and insomnia symptoms during the second wave. Advanced age, living with a high‐risk person for COVID‐19 infection, and having a relative/friend infected with COVID‐19 before the prior 2 weeks were risk categories for poor sleep quality. Living with children, having contracted COVID‐19 before the prior 2 weeks, being pessimistic about the vaccine and working in healthcare, were risk factors for insomnia symptoms. The follow‐up assessment highlighted reduced insomnia symptoms and anxiety. Nevertheless, we found reduced sleep duration, higher daytime dysfunction, advanced bedtime and wake‐up time, and a shift to morningness, confirming the alarming prevalence of poor sleepers (~60%) and severe depression (~20%) in a context of increased perceived stress. The present study showed a persistent impact of the COVID‐19 pandemic on sleep and mental health. Large‐scale interventions to counteract the chronicity and exacerbation of sleep and psychological disturbances are necessary, especially for the at‐risk categories.
Keywords: insomnia, longitudinal, mental health, pandemic waves, sleep health
1. INTRODUCTION
From December 2019, coronavirus disease 2019 (COVID‐19) began to spread worldwide rapidly. The Italian government reacted to the first contagion wave (March–April 2020) implementing a total lockdown involving home confinement and social distancing for the entire population, and the closure of most business activities. The lockdown started on 9 March and lasted until 3 May 2020. Many studies reported a pervasive impact of the lockdown period during the first wave of the COVID‐19 outbreak on sleep and psychological health of the general population (Jahrami et al., 2020; Rajkumar, 2020; Salfi et al., 2020b). In the autumn, a second contagion outbreak occurred in Italy, leading the government to adopt new restraining measures to control the virus propagation. A regional approach was adopted this time: restrictions to freedom of movement, business and school activities were imposed according to the local infection diffusion and the pressure on the regional healthcare system. On 6 November 2020, Italian regions were classified across three risk levels (yellow, orange, and red, ordered in terms of the severity of the restrictions), periodically updated based on the COVID‐19‐related data monitoring. In the present study, we provide the first evaluation of sleep health of the general population during the second wave of the COVID‐19 emergency, identifying the at‐risk categories for sleep disturbances during this further challenging period. Moreover, we longitudinally compared the outcome of the current period in a large Italian sample with the situation of the first pandemic wave using a web‐based survey administered during 2 weeks around the two contagions peaks.
2. METHODS
2.1. Participants and procedure
The present study is part of a larger research project aimed at understanding the consequences of the COVID‐19 outbreak on the Italian population (Salfi et al., 2020a, 2020b). The study was approved by the Institutional Review Board of the University of L’Aquila (protocol n. 43066/2020). A total of 8,798 Italian citizens participated in a web‐based survey during the first wave of COVID‐19 (Test 1: 25 March–7 April 2020, the third and fourth week of lockdown; Figure 1). The survey evaluated sleep quality, insomnia symptoms, chronotype, depression symptoms, perceived stress, and anxiety using the following validated questionnaires: the Pittsburgh Sleep Quality Index (PSQI; Curcio et al., 2013), the Insomnia Severity Index (ISI; Castronovo et al., 2016), the reduced form of the Morningness–Eveningness Questionnaire (MEQr; Natale et al., 2006), the Beck Depression Inventory‐second edition (BDI‐II; Ghisi et al., 2006), the 10‐item Perceived Stress Scale (PSS‐10; Mondo et al., 2019), and the state–anxiety subscale of the State‐Trait Anxiety Inventory (STAI‐X1; Spielberger et al., 1970).
FIGURE 1.
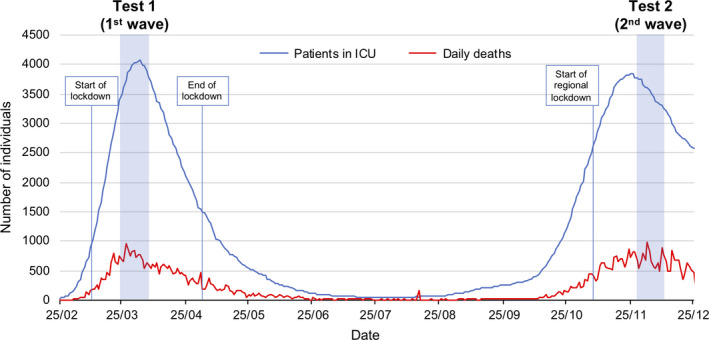
Italian national trend of daily deaths (blue line) and patients in the Intensive Care Unit (ICU; red line) due to COVID‐19 infection across the pandemic period (Protezione civile, 2020). The two assessment periods (Test 1: 25 March–7 April 2020, Test 2: 28 November–11 December 2020) are marked by the light blue areas
The Test 1 respondents were invited by Email to participate in a follow‐up assessment on 28 November 2020, corresponding to the contagion peak of the second wave of the COVID‐19 outbreak. A total of 2,013 individuals participated in the second measurement in a 2‐week time window (Test 2: 28 November–11 December 2020; Figure 1). The follow‐up measurement comprised the same questionnaires as Test 1. Additionally, we collected the following sociodemographic and COVID‐19‐related information as continuous or categorical variables: age, gender, education, occupation, geographical region used to derive the restraining measures in force (yellow, orange, or red zone), living with children, being a high‐risk person for COVID‐19 infection, living with a high‐risk person for COVID‐19 infection, COVID‐19 infection, forced quarantine, infection or death of a relative/close friend due to COVID‐19, perspective on vaccination, negative economic and social impact of the current situation, and mean exposure (min) to smartphone, personal computer (PC)/tablet, television, and e‐reader in the 2 hr before falling asleep during the previous 2 weeks. The available choices for each categorical variable along with the sociodemographic composition of the follow‐up sample, and the COVID‐related responses are reported in Table 1. The compilation of the last three questionnaires (BDI‐II, PSS‐10, STAI‐X1) was optional to ensure reliable unforced responses. A total of 1,847, 1,790, and 1,784 participants completed the BDI‐II, the PSS‐10, and the STAI‐X1, respectively, during Time 1 and Time 2. Online informed consent was obtained from participants.
TABLE 1.
Sociodemographic composition and COVID‐related responses of the Test 2 sample and results (B, odds ratio [OR], 95% confidence interval [CI], p) of the logistic regression analyses on PSQI (>5) and ISI (>14) scores. Numbers preceded by an asterisk (*) are mean values (SD)
| Poor sleep (PSQI >5) | Moderate/severe insomnia (ISI >14) | ||||||
|---|---|---|---|---|---|---|---|
| Predictor | N (%) or *mean (SD) | B | OR (95% CI) | p | B | OR (95% CI) | p |
| Intercept | −1.99 | 0.14 (0.06–0.32) | <.001 | −4.36 | 0.01 (0.002–0.07) | <.001 | |
| Age, years | *34.84 (12.37) | 0.02 | 1.02 (1.01–1.03) | <.01 | −0.01 | 0.99 (0.97–1.01) | .35 |
| Gender | |||||||
| Female | 1,648 (81.87) | Ref. | Ref. | ||||
| Male | 365 (18.13) | −0.39 | 0.68 (0.52–0.87) | <.01 | −0.45 | 0.64 (0.41–0.998) | <.05 |
| Education | |||||||
| Middle/High school | 586 (29.11) | Ref. | Ref. | ||||
| Graduate | 1,163 (57.77) | −0.22 | 0.80 (0.64–1.01) | .06 | −0.47 | 0.62 (0.45–0.87) | <.01 |
| Postgraduate | 264 (13.12) | −0.33 | 0.72 (0.51–0.99) | <.05 | −0.31 | 0.73 (0.44–1.21) | .22 |
| Occupation | |||||||
| Unemployed | 151 (7.50) | Ref. | Ref. | ||||
| Student | 521 (25.88) | −0.20 | 0.82 (0.53–1.28) | .38 | 0.13 | 1.13 (0.60–2.13) | .70 |
| Healthcare worker | 159 (7.90) | −0.36 | 0.70 (0.42–1.18) | .18 | 0.86 | 2.36 (1.15–4.83) | .02 |
| Self‐employed | 340 (16.89) | −0.33 | 0.72 (0.46–1.13) | .15 | 0.31 | 1.36 (0.71–2.60) | .35 |
| Employed | 772 (38.35) | −0.16 | 0.86 (0.56–1.30) | .46 | 0.43 | 1.53 (0.84–2.78) | .16 |
| Retired | 70 (3.48) | −0.26 | 0.77 (0.36–1.66) | .51 | 0.86 | 2.36 (0.76–7.37) | .14 |
| Restraining measures | |||||||
| Red zone | 1,046 (51.96) | Ref. | Ref. | ||||
| Orange zone | 451 (22.40) | −0.07 | 0.93 (0.73–1.20) | .58 | 0.11 | 1.12 (0.77–1.62) | .55 |
| Yellow zone | 516 (25.63) | 0.05 | 1.06 (0.83–1.34) | .66 | −0.08 | 0.92 (0.64–1.33) | .67 |
| Chronotype | |||||||
| Neither‐type | 1,289 (64.03) | Ref. | Ref. | ||||
| Morning‐type | 487 (24.19) | −0.44 | 0.65 (0.51–0.82) | <.001 | −0.48 | 0.62 (0.41–0.94) | .03 |
| Evening‐type | 237 (11.77) | 0.42 | 1.53 (1.10–2.13) | .01 | 0.71 | 2.03 (1.36–3.03) | <.001 |
| Living with children | |||||||
| No | 1,566 (77.79) | Ref. | Ref. | ||||
| Yes | 447 (22.21) | 0.12 | 1.13 (0.89–1.45) | .32 | 0.41 | 1.50 (1.06–2.13) | .02 |
| Being a high‐risk person for COVID‐19 infection | |||||||
| No | 1,812 (90.02) | Ref. | Ref. | ||||
| Yes | 201 (9.99) | 0.49 | 1.64 (1.13–2.38) | <.01 | 0.59 | 1.80 (1.16–2.81) | <.01 |
| Living with a high‐risk person for COVID‐19 infection | |||||||
| No | 1,493 (74.17) | Ref. | Ref. | ||||
| Yes | 520 (25.83) | 0.31 | 1.36 (1.07–1.71) | .01 | 0.01 | 1.01 (0.72–1.41) | .96 |
| COVID‐19 infection | |||||||
| No | 1,887 (93.74) | Ref. | Ref. | ||||
| Yes (prior 2 weeks) | 34 (1.69) | 0.92 | 2.50 (0.87–7.17) | .09 | 0.84 | 2.32 (0.78–6.86) | .13 |
| Yes (before the prior 2 weeks) | 92 (4.57) | 0.18 | 1.20 (0.71–2.02) | .50 | 0.66 | 1.94 (1.02–3.70) | .04 |
| Forced quarantine | |||||||
| No | 1,513 (75.16) | Ref. | Ref. | ||||
| Yes (prior 2 weeks) | 128 (6.36) | 0.12 | 1.13 (0.70–1.81) | .62 | 0.01 | 1.01 (0.51–2.01) | .98 |
| Yes (before the prior 2 weeks) | 372 (18.48) | −0.02 | 0.98 (0.74–1.30) | .89 | 0.05 | 1.05 (0.69–1.58) | .83 |
| COVID‐19 infection of a relative/close friend | |||||||
| No | 823 (40.88) | Ref. | Ref. | ||||
| Yes (prior 2 weeks) | 541 (26.88) | 0.17 | 1.19 (0.92–1.52) | .19 | −0.02 | 0.99 (0.68–1.44) | .94 |
| Yes (before the prior 2 weeks) | 649 (32.24) | 0.31 | 1.36 (1.06–1.74) | .01 | −0.10 | 0.90 (0.62–1.30) | .59 |
| Death of a relative/close friend due to COVID‐19 | |||||||
| No | 1,832 (91.01) | Ref. | Ref. | ||||
| Yes | 181 (8.99) | −0.04 | 0.96 (0.67–1.37) | .82 | 0.06 | 1.06 (0.64–1.77) | .81 |
| Perspective on vaccination | |||||||
| Optimistic | 853 (42.38) | Ref. | Ref. | ||||
| Undecided | 887 (44.06) | 0.19 | 1.21 (0.98–1.49) | .08 | 0.29 | 1.33 (0.95–1.86) | .09 |
| Pessimistic | 273 (13.56) | 0.20 | 1.22 (0.89–1.67) | .23 | 0.61 | 1.84 (1.20–2.81) | <.01 |
| Economic impact | |||||||
| None | 1,055 (52.41) | Ref. | Ref. | ||||
| Negative | 712 (35.37) | 0.47 | 1.60 (1.27–2.01) | <.001 | 0.57 | 1.78 (1.28–2.46) | <.001 |
| Positive | 246 (12.22) | −0.08 | 0.92 (0.68–1.26) | .61 | −0.17 | 0.85 (0.49–1.47) | .56 |
| Negative social impact | |||||||
| None | 74 (3.68) | Ref. | Ref. | ||||
| A little | 760 (37.76) | 0.79 | 2.21 (1.28–3.80) | <.01 | 0.85 | 2.35 (0.55–10.02) | .25 |
| A lot | 1,179 (58.57) | 1.46 | 4.29 (2.50–7.36) | <.001 | 1.59 | 4.93 (1.18–20.65) | .03 |
| Electronic device usage in the 2 hr before falling asleep, min | |||||||
| Smartphone | *55.25 (37.96) | 0.009 | 1.009 (1.006–1.012) | <.001 | 0.009 | 1.009 (1.005–1.013) | <.001 |
| PC and tablet | *37.02 (44.00) | 0.002 | 1.002 (1.00–1.005) | .11 | 0.001 | 1.001 (0.998–1.004) | .57 |
| Television | *50.11 (45.96) | −0.001 | 0.999 (0.996–1.001) | .27 | <0.001 | 0.999 (0.996–1.003) | .70 |
| E‐reader | *6.08 (19.53) | 0.003 | 1.003 (0.997–1.008) | .32 | 0.002 | 1.002 (0.996–1.009) | .51 |
ISI, Insomnia Severity Index; PC, personal computer; PSQI, Pittsburgh Sleep Quality Index; Ref., reference.
Bold values statistically significant at p < .05.
2.2. Statistical analysis
Prevalence of poor sleepers, moderate/severe insomnia, and severe depression symptoms were computed according to the conventional cut‐off scores: PSQI >5, ISI >14, BDI‐II >28, respectively. The MEQr scores were used to assign the respondents to three chronotype groups (Morning‐type: 19–25; Neither‐type: 11–18; Evening‐type: 4–10).
To provide a comprehensive overview of the sociodemographic and COVID‐related factors influencing the risk of poor sleep quality and moderate/severe insomnia during the second pandemic wave, we performed binomial logistic regressions on PSQI (>5) and ISI (>14) scores including the available sociodemographic and COVID‐19‐related variables as predictors.
The investigation on possible changes in sleep quality, insomnia symptoms, chronotype, depression, perceived stress, and anxiety between the two infection waves was performed contrasting the questionnaire scores (PSQI, ISI, MEQr, BDI‐II, PSS‐10, STAI‐X1, respectively) at the two time‐points by Wilcoxon signed‐rank tests, due to violation of the normality assumption. The analysis was replicated for specific items (bedtime and wake‐up time) and each sub‐component of the PSQI (“Subjective sleep quality”, “Sleep latency”, “Sleep duration”, “Habitual sleep efficiency”, “Sleep disturbances”, “Sleep medications”, and “Daytime dysfunction”) to further detail the specific dimensions of sleep habits/quality possibly changed between the two assessments. All p values were corrected for multiple comparisons by false discovery rate (FDR).
The prevalence of poor sleep quality, moderate/severe insomnia, and severe depression were compared between the two time‐points using the McNemar's test.
All tests were two‐tailed and statistical significance was set to p < .05. We excluded 153 respondents from the PSQI analyses due to compilation errors (they declared longer total sleep time than the reported total time in bed).
3. RESULTS
3.1. At‐risk categories for sleep disturbances during the second wave
The results of the logistic regression models are reported in Table 1. Female gender, evening chronotype, being a high‐risk person for COVID‐19 infection, reporting negative social or economic impact of the current situation, and higher smartphone usage in the 2 hr before falling asleep predicted a higher risk of poor sleep and moderate/severe insomnia symptoms during the second wave of COVID‐19. On the other hand, higher education level and morning chronotype emerged as protective factors against poor sleep quality and insomnia symptoms.
Advanced age, living with a high‐risk person for COVID‐19 infection, and having a relative/close friend infected with COVID‐19 were at‐risk categories for poor sleep quality, while living with children, having contracted COVID‐19 before the prior 2 weeks, being pessimistic about the vaccination prospective, and being a healthcare worker, were risk factors for developing moderate/severe insomnia symptoms.
3.2. Sleep and psychological differences between the waves
Results of the Wilcoxon signed‐rank tests between Test 1 and Test 2 are reported in Table 2. The sample went to bed and woke‐up earlier at Test 2. Notwithstanding the lack of significant changes on PSQI total score, the analyses on PSQI sub‐components highlighted several differences between the two measurements. Subjective sleep quality improved and was accompanied by a decrease in sleep latency and sleep disturbances. On the contrary, respondents slept less, tended to increase sleep medications use, and showed higher daytime dysfunction. Moreover, the participants reported reduced severity of insomnia symptoms and increased MEQr scores, pointing to a morning chronotype. Finally, depressive symptomatology remained stable, while perceived stress increased, and anxiety declined. The prevalence comparisons showed that the percentage of poor sleepers remained stable, insomniacs declined, and the individuals reporting severe depression symptoms remained unchanged over time.
TABLE 2.
Descriptive statistics (mean [SD]) of questionnaire scores assessing sleep/chronobiological habits and quality (bedtime and wake‐up time, PSQI total score and sub‐components, ISI, MEQr), and psychological condition (BDI‐II, PSS‐10, STAI‐X1) for Test 1 (25 March–7 April) and Test 2 (28 November–11 December), and the corresponding statistical comparisons (Wilcoxon signed‐rank test: Z, p). Prevalence (%) of sleep disturbances (poor sleep and moderate/severe insomnia) and severe depression at the two time‐points and the corresponding statistical comparisons (McNemar's test: chi square, p) are also reported
| Test 1 (1st wave) | Test 2 (2nd wave) | |||
|---|---|---|---|---|
| Sleep/chronotype features | mean (SD) | Z | p | |
| Bedtime, hr:min | 00:14 (1:25) | 23:38 (1:17) | 21.13 | <.001 |
| Wake‐up time, hr:min | 08:44 (1:38) | 07:50 (1:22) | 25.72 | <.001 |
| PSQI total score | 6.95 (3.67) | 6.90 (3.54) | 0.47 | .64 |
| Subjective sleep quality | 1.39 (0.78) | 1.34 (0.72) | 2.52 | .02 |
| Sleep latency | 1.43 (1.04) | 1.27 (1.02) | 6.60 | <.001 |
| Sleep duration | 0.70 (0.81) | 0.79 (0.78) | −5.21 | <.001 |
| Habitual sleep efficiency | 0.79 (1.00) | 0.81 (1.00) | −0.47 | .64 |
| Sleep disturbances | 1.41 (0.60) | 1.38 (0.57) | 2.25 | .03 |
| Sleep medications | 0.29 (0.80) | 0.33 (0.86) | −1.96 | .059 |
| Daytime dysfunction | 0.85 (0.71) | 0.92 (0.70) | −4.17 | <.001 |
| ISI score | 8.34 (5.45) | 7.73 (5.39) | 5.61 | <.001 |
| MEQr score | 15.31 (3.66) | 15.44 (3.68) | −2.36 | .03 |
| Psychological status | mean (SD) | Z | p | |
|---|---|---|---|---|
| BDI‐II score | 12.46 (8.96) | 12.35 (9.41) | 0.65 | .60 |
| PSS‐10 score | 17.99 (7.41) | 18.70 (3.74) | −4.16 | <.001 |
| STAI‐X1 score | 48.58 (9.17) | 46.78 (9.39) | 8.13 | <.001 |
| Sleep/psychological disturbance | N (%) | Chi square | p | |
|---|---|---|---|---|
| Poor sleep | 1,116 (60.16) | 1,110 (59.84) | 0.04 | .84 |
| Moderate/severe insomnia | 270 (13.41) | 226 (11.23) | 6.56 | .01 |
| Severe depression | 352 (19.06) | 370 (20.03) | 0.90 | .34 |
BDI‐II, Beck Depression Inventory‐second edition; ISI, Insomnia Severity Index; MEQr, Morningness–Eveningness Questionnaire reduced version; PSQI, Pittsburgh Sleep Quality Index; PSS‐10, 10‐item Perceived Stress Scale; STAI‐X1, state–anxiety subscale of the State‐Trait Anxiety Inventory.
Bold values statistically significant at p < .05.
4. DISCUSSION
Consistent with the literature about the first wave, we confirmed a higher predisposition of female gender (Cellini et al., 2020; Salfi et al., 2020b) and low education level (Kokou‐Kpolou et al., 2020) to develop sleep disturbances during our second‐wave assessment. The healthcare workers confirmed their vulnerability to insomnia symptomatology during the second wave (Pappa et al., 2020), while the elderly emerged as a risk factor for poor sleep quality.
The circadian preference was a crucial predictor of sleep outcome, consistent with the pre‐pandemic literature (Adan et al., 2012): evening‐type individuals showed a greater predisposition to poor sleep quality and moderate/severe insomnia symptoms, while morning chronotype emerged as a protective factor. The follow‐up assessment of our investigation took place during a period of lighter restraining measures. In Italy, during the second wave of contagion, a regional lockdown was adopted, and we failed to highlight any difference according to the rigidity of the restraining measures adopted. This result pointed to a detrimental effect of the pandemic period itself, regardless of the restrictions in force.
The present findings showed a higher risk of insomnia in individuals who lived with children. In‐person school activities were suspended in Italy during the follow‐up measurement, while working activities partially continued (especially in the orange and yellow zones). This may have created a difficult situation to manage for parents, explaining the present results.
Being a high‐risk person for COVID‐19 infection was associated with a higher predisposition to poor sleep quality and moderate/severe insomnia symptoms, while living with a high‐risk person for COVID‐19 infection predicted a higher probability of experiencing poor sleep quality. These results could reflect a greater fear of infection and worries experienced by these individuals, which triggered sleep disturbances. Having contracted the COVID‐19 or having a relative/close friend infected before the prior 2 weeks of the survey participation constituted a risk factor for insomnia and poor sleep quality, respectively, pointing to a long‐term impact of these events. Notably, optimism for the future due to the arrival of a vaccine emerged as a protective factor against the insomnia exacerbation. Therefore, it seems that the vaccination campaign prospective could be itself beneficial for sleep health.
The pandemic has lasted for many months, and the healthcare emergency has been accompanied by unprecedented economic and social crises. In this context, more than one‐third of the sample reported a negative economic impact of the current situation, and six out of ten of the respondents reported a consistent impairment of their social relationships. Both these outcomes turned out to be risk factors for exacerbation of sleep disturbances. Finally, smartphone overuse before sleep onset emerged as a risk factor for sleep disturbances. This finding is putatively ascribable to the well‐known detrimental effect of backlit screen exposure before sleep time on the circadian system, as well as to the alerting effects of digital engagement. Notably, the increased evening usage of electronic devices has already been proposed as a mediator of sleep deterioration during the March–April lockdown (Salfi et al., 2020a).
Comparisons between data from the two outbreak waves displayed an articulated framework.
We showed improved insomnia symptoms, reduced prevalence of moderate/severe insomnia conditions, and reduced anxiety. However, the present investigation confirmed the alarming situation highlighted during the first wave of COVID‐19 (Jahrami et al., 2020; Salfi et al., 2020b), as the majority of the sample consisted of poor sleepers and this prevalence (~60%) remained stable between the two pandemic waves.
Despite the invariance of sleep quality between the two assessments, we showed several differences as concerns the PSQI sub‐components. The subjective sleep quality, sleep latency, and sleep disturbances dimensions improved. However, the improvements were compensated by reduced sleep duration, more severe daytime dysfunction, and a trend to higher sleep medication use. Moreover, the participants went to bed more than half an hour earlier and woke‐up almost an hour earlier than during the March–April lockdown. These results were accompanied by a significant shift towards the morning chronotype. In light of these results, it should be acknowledged that the first lockdown period was characterised by a substantial reduction of the social jetlag due to weaker social and working obligations (Korman et al., 2020). The present findings suggest that the social jetlag returned to negatively influence Italians’ sleep, as the second assessment period was marked by a substantial resumption of daily working and activity routine.
Finally, we confirmed the severity of depressive symptomatology and the alarming prevalence of severe depression conditions (~20%) of the March–April lockdown. Remarkably, all these results were obtained in a context of increased perceived stress, putatively ascribable to the prolonged emergency period.
In conclusion, the present study found that the impact of the COVID‐19 pandemic persists on both sleep and mental health, although the second wave of contagion has been faced using lighter restraining measures. Therefore, vigilance is still required, and large‐scale interventions should be implemented to counteract the chronicity and exacerbation of sleep and psychological disturbances, especially for the categories identified as at‐risk in the present study.
CONFLICT OF INTEREST
None of the authors have potential conflicts of interest to be disclosed. All authors have seen and approved the manuscript.
AUTHOR CONTRIBUTIONS
FS: Conceptualisation, methodology, investigation, data curation, formal analysis, writing – original draft, writing – review and editing. ADA: Writing – original draft, writing – review and editing. DT: Writing – review and editing. MF: Conceptualisation, methodology, investigation, supervision, writing – review and editing.
Salfi F, D'Atri A, Tempesta D, Ferrara M. Sleeping under the waves: A longitudinal study across the contagion peaks of the COVID‐19 pandemic in Italy. J Sleep Res. 2021;30:e13313. 10.1111/jsr.13313
Funding information
This research did not receive any specific grant from funding agencies in the public, commercial, or not‐for‐profit sectors.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Adan, A. , Archer, S. N. , Hidalgo, M. P. , Di Milia, L. , Natale, V. , & Randler, C. (2012). Circadian typology: A comprehensive review. Chronobiology International, 29(9), 1153–1175. 10.3109/07420528.2012.719971 [DOI] [PubMed] [Google Scholar]
- Castronovo, V. , Galbiati, A. , Marelli, S. , Brombin, C. , Cugnata, F. , Giarolli, L. , Anelli, M. M. , Rinaldi, F. , & Ferini‐Strambi, L. (2016). Validation study of the Italian version of the Insomnia Severity Index (ISI). Neurological Sciences, 37(9), 1517–1524. 10.1007/s10072-016-2620-z [DOI] [PubMed] [Google Scholar]
- Cellini, N. , Conte, F. , De Rosa, O. , Giganti, F. , Malloggi, S. , Reyt, M. , Guillemin, C. , Schmidt, C. , Muto, V. , & Ficca, G. (2020). Changes in sleep timing and subjective sleep quality during the COVID‐19 lockdown in Italy and Belgium: Age, gender and working status as modulating factors. Sleep Medicine, 77, 112–119. 10.1016/j.sleep.2020.11.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curcio, G. , Tempesta, D. , Scarlata, S. , Marzano, C. , Moroni, F. , Rossini, P. M. , Ferrara, M. , & De Gennaro, L. (2013). Validity of the Italian version of the Pittsburgh sleep quality index (PSQI). Neurological Sciences, 34, 511–519. 10.1007/s10072-012-1085-y [DOI] [PubMed] [Google Scholar]
- Ghisi, M. , Flebus, G. , Montano, A. , Sanavio, E. , & Sica, C. (2006). Beck Depression Inventory‐II: Edizione Italiana. Giunti Editore. [Google Scholar]
- Jahrami, H. , BaHammam, A. S. , Bragazzi, N. L. , Saif, Z. , Faris, M. , & Vitiello, M. V. (2020). Sleep problems during COVID‐19 pandemic by population: A systematic review and meta‐analysis. Journal of Clinical Sleep Medicine, 10.5664/jcsm.8930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokou‐Kpolou, C. K. , Megalakaki, O. , Laimou, D. , & Kousouri, M. (2020). Insomnia during COVID‐19 pandemic and lockdown: Prevalence, severity, and associated risk factors in French population. Psychiatry Research, 290, 113128. 10.1016/j.psychres.2020.113128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korman, M. , Tkachev, V. , Reis, C. , Komada, Y. , Kitamura, S. , Gubin, D. , Kumar, V. , & Roenneberg, T. (2020). COVID‐19‐mandated social restrictions unveil the impact of social time pressure on sleep and body clock. Scientific Reports, 10, 22225. 10.1038/s41598-020-79299-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mondo, M. , Sechi, C. , & Cabras, C. (2019). Psychometric evaluation of three versions of the Italian perceived stress scale. Current Psychology, 10.1007/s12144-019-0132-8 [DOI] [Google Scholar]
- Natale, V. , Esposito, M. J. , Martoni, M. , & Fabbri, M. (2006). Validity of the reduced version of the Morningness‐Eveningness Questionnaire. Sleep and Biological Rhythms, 4, 72–74. 10.1111/j.1479-8425.2006.00192.x [DOI] [Google Scholar]
- Pappa, S. , Ntella, V. , Giannakas, T. , Giannakoulis, V. G. , Papoutsi, E. , & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID‐19 pandemic: A systematic review and meta‐analysis. Brain, Behavior, and Immunity, 88, 901–907. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Protezione civile (2020). Emergenza Coronavirus: La risposta nazionale. Retrieved from http://www.protezionecivile.gov.it/attivita‐rischi/rischio‐sanitario/emergenze/coronavirus [Google Scholar]
- Rajkumar, R. P. (2020). COVID‐19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52, 102066. 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salfi, F. , Amicucci, G. , Corigliano, D., D’Atri, A. , Viselli, L. , Tempesta, D. , & Ferrara, M. (2020a). Changes of evening exposure to electronic devices during the COVID‐19 lockdown affect the time course of sleep disturbances. medRxiv. 10.1101/2020.10.20.20215756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salfi, F. , Lauriola, M. , Amicucci, G. , Corigliano, D. , Viselli, L. , Tempesta, D. , & Ferrara, M. (2020b). Gender‐related time course of sleep disturbances and psychological symptoms during the COVID‐19 lockdown: A longitudinal study on the Italian population. Neurobiology of Stress, 13, 100259. 10.1016/j.ynstr.2020.100259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger, C. D. , Gorsuch, R. L. , & Lushene, R. E. (1970). The State‐Trait Anxiety Inventory (STAI) Test Manual for Form X. Consulting Psychologist Press. (tr. it.: Lazzari R, Pancheri P., 1980. S.T.A.I. Questionario di autovalutazione dell’ansia di stato e di tratto. Firenze, IT: Organizzazioni Speciali). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


