Abstract
Objectives
Without pharmaceutical measures available, endorsement of protective behaviours, such as hygiene behaviours, social distancing, and adherence to recommended behaviours in case of symptoms is of key importance to curb the ongoing COVID‐19 pandemic. Based on an extended version of the protection motivation theory, this study examined the role of perceived risks to oneself and to others, self‐efficacy, response efficacy, and perceived social norms for intentions to and the endorsement of several protective behaviours and alternative behaviours known to be ineffective. Further, it was hypothesised that effects of risk perceptions depended on high levels of self‐efficacy.
Design
Data were collected by telephone at the beginning of the lockdown in Switzerland with a large sample (N = 1,009) representative of the adult Swiss population.
Methods
All predictors (self‐efficacy, response efficacy, perceived social norms, intentions) but risk perceptions were assessed for hygiene behaviours, social distancing, adherence to recommended behaviours in case of symptoms, and alternative measures known to be ineffective.
Results
Across all analyses of intentions for and endorsement of protective and alternative behaviours, response efficacy and self‐efficacy emerged as the most important predictors. Social norms were mainly related to intentions, but not to behaviours. The different risk perceptions were rarely and inconsistently related to intentions and behaviours. No consistent pattern of interactions between self‐efficacy and risk perceptions emerged.
Conclusion
This study demonstrates that even in the face of a pandemic of an unknown virus, the resources (self‐efficacy, response efficacy) rather than the risk perceptions have the potential to promote protective behaviours.
Keywords: COVID‐19, protection motivation theory, protective behaviours, risk perception, self‐efficacy
Statement of contribution.
What is already known on this subject?
In the current COVID‐19 pandemic, behavioural protective measures are central for infection control.
Adopting or changing habitual behaviours such as washing hands more diligently is difficult.
Empirical evidence speaks in favour of the Protection Motivation Theory’s core assumptions in the context of pandemics
What does this study add?
Response efficacy and self‐efficacy were the most important predictors for intentions and behaviours.
Different risk perceptions were mostly unrelated to intentions and behaviours.
Alternative, ineffective measures are related to the same determinants as recommended protective behaviours.
Background
On 11 March, the World Health Organization, WHO, classified the current new coronavirus outbreak, SARS‐CoV‐2, and the resulting disease COVID‐19 as a pandemic (2020), that is a disease that spreads across wide geographic areas while affecting a large proportion of the population (Merriam Webster, 2020). Given that at the beginning of the pandemic, there were no pharmaceutical means available to prevent the transmission of the virus or to heal COVID‐19, non‐pharmaceutical, behavioural protective measures (e.g., hand hygiene, social distancing) are central for infection control (Nicolaides, Avraam, Cueto‐Felgueroso, González, & Juanes, 2019). It is therefore of crucial importance to examine the key factors for promoting the uptake of the recommended protective behaviours by as many individuals as possible. Thus, this study set out to examine theory‐guided key determinants of protective behaviours in the face of the current COVID‐19 pandemic in a sample representative of the general population of Switzerland during the first weeks of a country‐wide lockdown.
Predicting the uptake of protective behaviours
Protective behaviours for slowing the development of a pandemic can be classified as preventive behaviours (e.g., hand washing, using tissues when coughing or sneezing), avoidance behaviours (e.g., social distancing, compliance to quarantine regulations), and management behaviours (e.g., seeking professional medical advice) (Bish & Michie, 2010; Moran, Del Valle, & Nishiura, 2016). Behaviours from all these categories had been recommended by the WHO and the Federal Office of Public Health Switzerland for slowing the spread of SARS‐CoV‐2 (WHO, 2019). However, adopting new or changing habitual behaviours such as washing hands more diligently or keeping the recommended distance is very difficult (e.g., Davidson & Scholz, 2020).
Applying a theory‐based approach is essential for effectively identifying the key determinants for health behaviour change. Failure to do so may result in counterproductive interventions that might do more harm than good (Kok, Peters, Kessels, Hoor, & t., & Ruiter, R. A. C., 2018). One theory to identify key factors contributing to the adoption of preventive behaviours is Protection Motivation Theory (PMT; Bui, Mullan, & McCaffery, 2013; Floyd, Prentice Dunn, & Rogers, 2000; Maddux & Rogers, 1983). Core assumptions of the basic version of this theory are that a high threat appraisal, usually assessed as perceived risk (i.e., the severity of a disease and own vulnerability), will only translate into an intention to engage in protective behaviour (called here: protection motivation) when combined with a high coping appraisal (high response efficacy, i.e., the expectation that a protective behaviour will effectively reduce the risk, and high self‐efficacy, i.e., the optimistic belief that a person is capable of implementing the protective behaviour) (Kok et al., 2018). In turn, high levels of protection motivation are assumed to predict the adoption of protective behaviours.
Empirical evidence speaks in favour of the PMT’s assumptions in the context of pandemics. For example, perceived risk positively relates to intentions (Ferrer & Klein, 2015; Tooher, Collins, Street, Braunack‐Mayer, & Marshall, 2013; Williams, Rasmussen, Kleczkowski, Maharaj, & Cairns, 2015). Moreover, response efficacy for different protective measures during a pandemic predicts intentions specifically for these protective measures (Rubin, Potts, & Michie, 2010; Timpka et al., 2014), such as social distancing behaviour (Williams et al., 2015). Finally, self‐efficacy is associated with intentions to engage in protective behaviours (Lin et al., 2020; Timpka et al., 2014; Williams et al., 2015). For all determinants, there is also evidence not only for indirect effects via intentions, but also for effects on behaviour directly (e.g., Bish & Michie, 2010; Sheeran, Harris, & Epton, 2014).
However, there are several open questions with regard to determinants of intentions to adopt protective measures and the actual engagement in these behaviours during a pandemic. For example, during the ongoing new coronavirus pandemic everybody, even those who are at low risk of developing severe symptoms, might nevertheless transmit the virus. Thus, adopting preventive behaviours might be associated not only with the perceived risk for oneself but also with the perceived risk for others. This risk involves the vulnerability (i.e., contracting the virus) and severity (i.e., developing severe symptoms) of the disease for others as well as the risk for transmitting the virus to others (Lau, Kim, Tsui, & Griffiths, 2007; Rolison, Hanoch, & Freund, 2019). Therefore, the current study examined assumptions of the PMT with a more nuanced assessment of risk perceptions for oneself as well as for others. We also include subjectively perceived social determinants for intentions for adopting and endorsing recommended behaviours given the collective experience of the pandemic (e.g., Bish & Michie, 2010). Drawing on the theory of planned behaviour (Ajzen, 1991), this study examines the role of social norms, that is, the subjective perceptions of other people’s approval or disapproval of specific behaviours. Social norms had been shown to relate to intentions and behaviour during the H1/N1 pandemic (L. Lin, McCloud, Jung, & Viswanath, 2018) and also during the COVID‐19 pandemic (C.‐Y. Lin et al., 2020).
Studies on the change in health‐relevant behaviours typically only include the likelihood to adopt the health‐relevant behaviours targeted at but neglect behaviours people believe to be effective although there is no evidence supporting this belief. In the case of the new coronavirus pandemic, likely fuelled by the lack of knowledge about the new virus, social media floated numerous ‘alternative’ measures such as eating garlic or praying. In the current study, we included such ‘alternative’ behaviours to explore if their adoption is driven by the same factors as the adoption of the officially recommended preventive behaviours.
In sum, the study tested the following hypotheses (preregistered at Open Science Framework, OSF, DOI 10.17605/OSF.IO/G6EHD; for an overview, see Figure 1):
Figure 1.
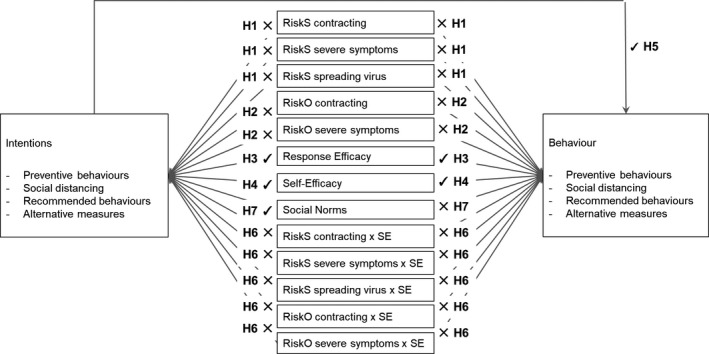
Hypotheses and results for predicting intentions and behaviours.
Note. RiskS self = Risk to oneself of contracting COVID‐19. RiskS severe symptoms = Risk to self of developing severe symptoms. RiskS spreading virus = Risk to self of spreading the virus. RiskO contracting = Risk to others of contracting COVID‐19. RiskO severe symptoms = Risk to others of developing severe symptoms; SE = Self‐efficacy; Recommended behaviour = recommended behaviours in case of symptoms.
Hypothesis 1
Higher perceived risk to oneself of (1) contracting COVID‐19, (2) developing severe symptoms, and (3) spreading the virus is related to (i) higher intentions to adopt and (ii) higher endorsement of (a) preventive behaviours, (b) social distancing, (c) recommended behaviours in case of symptoms, and (d) alternative measures known to be ineffective.
Hypothesis 2
Higher perceived risk to others of (1) contracting COVID‐19, and (2) developing severe symptoms is related to (i) higher intentions to adopt and (ii) higher endorsement of (a) preventive behaviours, (b) social distancing, (c) recommended behaviours in case of symptoms, and (d) alternative measures known to be ineffective.
Hypothesis 3
Higher response efficacy, that is, the perceived effectiveness of engaging in (a) preventive behaviours, (b) social distancing, (c) recommended behaviours in case of symptoms, and (d) alternative measures are related to (i) higher intentions to adopt (a), (b), (c), and (d), respectively, and (ii) higher self‐reported adherence to (a), (b),(c), and (d), respectively.
Hypothesis 4
Higher self‐efficacy of engaging in (a) preventive behaviours, (b) social distancing, (c) recommended behaviours in case of symptoms are related to (i) higher intentions to adopt (a), (b), and (c), respectively, and (ii) higher self‐reported adherence to (a), (b), and (c), respectively.
Hypothesis 5
Higher intentions to adopt (a) preventive behaviours, (b) social distancing, (c) recommended behaviours in case of symptoms, and (d) alternative measures are related to higher levels in these behaviours.
Another open question is the moderating role of self‐efficacy on the associations between the different risk perceptions and intentions for and endorsement of protective measures in that high levels of perceived risk are assumed to only translate into intentions and behaviour when coupled with high self‐efficacy (Kok et al., 2018). This has not yet been tested in the context of pandemics.
Hypothesis 6
Self‐efficacy is assumed to moderate the associations between risk perceptions and intention and behaviour: The positive associations as specified in Hypotheses 1 and 2 are stronger when self‐efficacy for the different behaviours is higher and weaker when self‐efficacy for the different behaviours is lower.
With regard to social norms, we were interested in effects of perceived disapproval from the social network on intentions and behaviours themselves, leading to the following hypothesis:
Hypothesis 7
Perceived social norms (i.e., disapproval of adopting (a) preventive behaviours, (b) social distancing, (c) recommended behaviours in case of symptoms, and (d) alternative measures) are negatively related to (i) intentions to adopt (a), (b), (c), and (d), respectively, and (ii) to engage in (a), (b),(c), and (d), respectively.
Methods
The cross‐sectional survey took place in the last week of March 2020 and first week of April 2020 in Switzerland. One week earlier, on 16 March 2020 the Swiss government declared the state of ‘extraordinary situation’ for the country and ordered a country‐wide lockdown with closing all facilities and businesses that were not of systemic importance (non‐food shops, bars, restaurants, entertainment and leisure facilities, hairdressers, etc.). Exceptions were food providers, pharmacies, petrol stations, railway stations, banks, post offices, hotels, public administrations, and social institutions. Medical services also remained open, but only for urgent or emergency treatments. Private and public events as well as gatherings of more than five people were legally prohibited, and educational institutions (schools, universities, etc.) were closed as were the country’s borders. At the time of data collection, the official communication from the Swiss Federal Office of Public Health for being at risk was being 65 years or older and/or having at least one of the following conditions: cardiovascular disorder, high blood pressure, immunodeficiency, cancer, chronic respiratory diseases, or diabetes. People belonging to such a risk group were urged to stay at and work from home. The general population was asked to avoid all unnecessary contact, to keep their distance from others, and to follow the recommended hygiene measures.
Data were collected by a market research bureau, sampling a total of N = 1,009 inhabitants of Switzerland. The survey was run by telephone in order to have the highest likelihood of unbiased coverage of the general population. Moreover, random digit dialling was implemented to allow inclusion of households not listed in the telephone book and of mobile phone numbers and thus avoid selection bias particularly in younger people who oftentimes do not have landline networks anymore. The study was carried out in accordance with the ethics regulations of the University of Zurich.
Participants’ mean age was 55.53 (SD = 18.77; range = 18–96 years) with 50.2% being female. The majority of participants were Swiss citizens (85.5%), with 50.2% living in the German‐speaking part, 29.9% living in the French‐speaking part, and 19.8% living in the Italian‐speaking part of Switzerland. Most participants reported to have undergone vocational training (33.5%), followed by 32.0% reporting to have a university degree, 13.9% having higher education, 10.5% had A‐Levels, and 9.3% had completed the mandatory 9 years of schooling. In terms of income, 18.4% reported to have a total household income of < 4,000 Swiss Francs (approx. 4,500 USD), 20.1% reported to have between 4,001 and 6,000 Swiss Francs (approx., 4,501–6,800 US), 27.3% reported a total household income between 9,001 and 12,000 Swiss Francs (approx.. 6,801–13,550 USD), 8.9% reported to have more than 12,000 Swiss Francs (> approx. 13,550 USD), and 13.6% preferred not to say. The majority (66.2%) was married or in a committed relationship, 18.9% of participants were single, and 13.5% were divorced or widowed.
A total of 42.3% of the participants self‐classified as being at risk for developing severe symptoms when acquiring SARS‐CoV‐2. More than a third (35.1%) reported to have regular close contact with people belonging to the risk group. Only 15 out of the 1,009 participants (1.5%) reported to have undergone testing for COVID‐19 during this early phase of the pandemic, and only one person had been tested positively.
Measures
Owing to the telephone survey, all constructs were measured using single items. Response efficacy items were adapted from Ling, Kothe, and Mullan (2019). Self‐efficacy, intention, and risk perception items were adapted from Scholz, Keller, and Perren (2009). The social norms items were generated based on recommendations provided by Ajzen (2020). The item wordings, response formats, means, and standard deviations displayed in Table 1 were assessed in German, French, and Italian. Items were presented in random order within blocks (e.g., all items of response efficacy).
Table 1.
Descriptive statistics for all variables of the analyses
| Variable | Item Wording | Response format | M | SD | Min. | Max. | n | |
|---|---|---|---|---|---|---|---|---|
| Cat. 0 | Cat. 1 | |||||||
| Risk perception | 0 = ‘not at all’ to 10 = ‘extremely likely’ | |||||||
| RiskS contracting a | How likely do you think it is that you will be infected with the virus in the future? | 4.15 | 2.45 | 0 | 10 | |||
| RiskS severe symptoms b | If you are infected, how likely do you think it is that you develop serious symptoms? | 4.43 | 2.51 | 0 | 10 | |||
| RiskS spreading virus c | If you are infected, how likely do you think it is that you pass on the corona virus to others? | 4.23 | 2.94 | 0 | 10 | |||
| RiskO contracting d | How likely do you think it is that others in your environment will be infected with the corona virus in the future? | 5.08 | 2.53 | 0 | 10 | |||
| RiskO severe symptoms e | How likely do you think it is that these persons will develop serious symptoms? | 4.67 | 2.37 | 0 | 10 | |||
| Response efficacy | How effective do you think the following measures are against a corona virus infection? | 0 = ‘not effective at all’ to 10 = ‘extremely effective’ | ||||||
| RE preventive behaviours f | the official hygiene recommendations, i.e. washing your hands thoroughly, sneezing or coughing into a handkerchief or the crook of your arm. | 8.47 | 1.74 | 0 | 10 | |||
| RE social distancing g | keep your distance from others, i.e. do not attend events with larger groups, avoid public transport, do not shake hands with others or hug or kiss them as a greeting. | 8.95 | 1.62 | 0 | 10 | |||
| RE recommended behaviours h | recommendations on what to do in case of symptoms, i.e. get medical advice by phone, stay at home and avoid contact with others | 8.76 | 1.69 | 0 | 10 | |||
| RE alternatives i | alternative measures, e.g. going out into the fresh air, eating garlic, praying | 3.29 | 3.23 | 0 | 10 | |||
| Self‐efficacy | I am sure that I can manage to… | 0 = ‘does not apply at all’ to 10 = ‘applies exactly’ | ||||||
| SE preventive behaviours j | … follow the hygiene recommendations, even if it is difficult (washing my hands thoroughly, sneezing or coughing in a handkerchief or crook of my arm) | 8.89 | 1.68 | 0 | 10 | |||
| SE social distancing k | … keep my distance from others, even if it is difficult (not attending events with larger groups, avoiding public transport, not shaking hands with others) | 8.71 | 1.98 | 0 | 10 | |||
| SE recommended behaviours l | … follow the recommendations on what to do in case of symptoms, even if it is difficult (get medical advice by phone, stay at home and avoid contact with others). | 8.95 | 1.65 | 0 | 10 | |||
| SE total score | Mean score of three self‐efficacy items (Cronbach’s Alpha =.69) | 8.85 | 1.39 | 0 | 10 | |||
| Social norms | My environment (friends, colleagues, family) would find it excessive if I … | 0 = ‘does not apply at all’ to 10 = ‘applies exactly’ | ||||||
| SN preventive behaviours m | …followed the hygiene recommendations (washing my hands thoroughly, sneezing or coughing in a handkerchief or crook of my arm) | 1.67 | 3.04 | 0 | 10 | |||
| SN social distancing n | … kept my distance from others (no attending events with larger groups, avoiding public transport, no shaking hands) | 1.84 | 3.08 | 0 | 10 | |||
| SN recommended behaviours o | … followed the recommendations on what to do in case of symptoms (get medical advice by phone, stay at home) | 1.69 | 3.06 | 0 | 10 | |||
| SN alternatives p | …took alternative measures (e.g. go out into the fresh air, eat garlic, pray) | 4.23 | 3.76 | 0 | 10 | |||
| Intentions | I have the intention to … | 0 = ‘does not apply at all’ to 10 = ‘applies exactly’ | ||||||
| Intent preventive behaviours q | … follow the hygiene recommendations (washing my hands thoroughly, sneezing or coughing in a handkerchief or crook of my arm) | 9.31 | 1.58 | 0 | 10 | |||
| Intent social distancing r | … keep my distance from others (no attending events with larger groups, avoiding public transport, not shaking hands) | 9.22 | 1.82 | 0 | 10 | |||
| Intent recommended behaviours s | … follow the recommendations on what to do in case of symptoms (get medical advice by phone, stay at home) | 9.33 | 1.64 | 0 | 10 | |||
| Intent alternatives t | …take alternative measures (e.g. go out into the fresh air, eat garlic, pray) | 3.98 | 3.79 | 0 | 10 | |||
| Behaviours | How often... | 0 = ‘never’ to 10 = ‘always’ | ||||||
| Preventive behaviours u | …do you follow the hygiene recommendations? (wash your hands thoroughly, sneeze or cough in a handkerchief or crook of your arm) | 9.22 | 1.15 | 0 | 10 | |||
| Social distancing v | …do you keep your distance from others? (do not attend events with larger groups, avoid public transport, do not shake hands with others or give a welcome hug or kiss) | 9.18 | 1.50 | 0 | 10 | |||
| Recommended behaviours x | If you had or have symptoms: do you follow the recommendations on what to do in case of symptoms? (get medical advice by phone, stay at home and avoid contact with others) | 9.29 | 1.43 | 0 | 10 | |||
| Alternative behaviours w | … do you use alternative measures? (e.g. going out into the fresh air, eating garlic, praying) | 3.93 | 3.64 | 0 | 10 | |||
| Dichotomous outcomes | ||||||||
| Intent preventive behaviours | .71 | .45 | 0 | 1 | 292 | 716 | ||
| Intent social distancing | .71 | .46 | 0 | 1 | 295 | 712 | ||
| Intent recommended behaviours | .72 | .45 | 0 | 1 | 283 | 724 | ||
| Intent alternatives | .32 | .47 | 0 | 1 | 679 | 322 | ||
| Preventive behaviours | .58 | .49 | 0 | 1 | 427 | 580 | ||
| Social distancing | .62 | .49 | 0 | 1 | 385 | 620 | ||
| Recommended behaviours | .66 | .47 | 0 | 1 | 303 | 594 | ||
| Alternative behaviours | .32 | .47 | 0 | 1 | 680 | 320 | ||
Min. = minimum, Max. = maximum, Cat. 1 = for all DVs except for intentions for alternative measures, and alternative behaviours highest category, Cat 0 = for all DVs except for intentions for alternative measures, and alternative behaviours all other categories of the 11‐point response scale. Cat 1 for intentions for alternative measures and alternative behaviours all answers from categories 6 to 10, and Cat 0 all answers from categories 0 to 5.
Risk to self of contracting COVID‐19.
Risk to self of developing severe symptoms.
Risk to self of spreading the virus.
Risk to others of contracting COVID‐19.
Risk to others of developing severe symptoms.
Response efficacy for preventive behaviours.
Response efficacy for social distancing.
Response efficacy for recommended behaviours in case of symptoms.
Response efficacy for alternative measures.
Self‐efficacy for preventive behaviours.
Self‐efficacy for social distancing.
Self‐ efficacy for recommended behaviours in case of symptoms.
Social norm for preventive behaviours.
Social norm for social distancing.
Social norm for recommended behaviours in case of symptoms.
Social norm for alternative measures.
Intention for preventive behaviours (not dichotomous).
Intention for social distancing (not dichotomous).
Intention for recommended behaviours in case of symptoms (not dichotomous).
Intention for alternative measures (not dichotomous).
Preventive behaviours (not dichotomous).
Social distancing (not dichotomous).
Alternative behaviours (not dichotomous).
Recommended behaviours (not dichotomous).
No self‐efficacy for alternative behaviours was assessed. For the analyses predicting intentions for and alternative behaviours themselves, the three self‐efficacy items of the other behaviours were collapsed to a mean score (Cronbach’s α = .69).
Data analysis
All dependent variables were severely skewed prohibiting to analyse the data with linear regression models. Thus, all DVs were dichotomized with 1 representing the response scale point 10 and 0 representing all other categories (0–9 of the response scale). Intentions for and adoption of alternative measures were less skewed, so dichotomization resulted in 1 comprising all answers ranging from 6 to 10, and 0 comprising all answers ranging from 0 to 5.
Data were analysed with hierarchical logistic regressions using SPSS version 26 separately for all four intentions and behaviours, with interaction terms introduced in the final step. For testing the interactions, variables were mean‐centred (e.g., Hayes, 2018), and interaction terms were computed by multiplying the mean‐centred variables. Significant interaction terms were probed by applying the Johnson‐Neyman technique for testing the region of significance and plotted and probed by testing the simple slopes one SD above and below the mean using the ModProbe Macro by Hayes and Matthes (2009). In case of univariate and multivariate outliers (Field, 2018), these were excluded from the respective analyses. Data and corresponding syntax are available at https://osf.io/g6ehd/.
For all models, sensitivity analyses were run by controlling for belonging to the risk group as well as for age, language region, and gender as these latter variables were oversampled with regard to the Swiss population (see Tables S2–S9). Due to significant associations with dependent variables, we also controlled for education, marital status, being in regular close contact with people belonging to the risk group, and income as an indicator of socioeconomic status. Because the latter two variables were unrelated to preventive behaviours, and income was also unrelated to intentions for preventive behaviours, and intentions to engage in recommended behaviours, they were not included in these specific analyses. For recommended behaviours, nationality was also added to the control variables.
Results
Descriptives
All risk perceptions showed moderate mean levels, indicating that the general population of Switzerland seemed to be moderately alert with regard to COVID‐19 (see Table 1). In contrast, mean levels of response efficacy and self‐efficacy demonstrated high confidence in the behavioural means available for fighting the pandemic and in one’s own competences to do so. Social norms (i.e., social disapproval for behaviours) had very low mean levels speaking in favour of subjectively shared beliefs about which behaviours to consider as effective across participants’ social networks. Intentions and self‐reported behaviours had very high mean levels speaking for high intended and self‐reported compliance with the recommended measures in Switzerland. Only the ‘alternative’ measures such as using garlic or prayer against getting infected were generally not strongly endorsed.
Intercorrelations between constructs were mainly low to moderate as displayed in Table S1.
Predicting intentions
Disconfirming H1 and H2, the perceived risk to others for developing severe symptoms was the only risk perception significantly associated with intentions for preventive behaviours (see Table 2, and for an overview of all results, see Figure 1). Counter to expectations, a one‐unit increase in this risk perception was related to a 9% decrease in the odds of holding an intention to use preventive behaviours for people with an average self‐efficacy. Confirming H3, a one‐unit increase in response efficacy resulted in a 39% increase in the odds of endorsing the intention. Confirming H4, a one‐unit increase in self‐efficacy resulted in a 121% increase in the odds of forming this intention for people with average perceptions of risk to self and to others for developing severe symptoms. In line with H7, a one‐unit increase in perceived social norms resulted in a 5% decrease in the odds of forming this intention. Contrary to H6, at levels of self‐efficacy lower than 0.12 the risk to others for developing severe symptoms related negatively to the odds of forming an intention (see Figure S1). At levels of self‐efficacy lower than −0.82, the risk to oneself for developing severe symptoms related negatively to the odds of forming an intention (see Figure S1).
Table 2.
Logistic regression results for intention to engage in preventive behaviours
| Variable | B | SE | OR | 95% CI for OR | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Intercept | −1.77 | .43 | .17** | ||
| RiskS contracting a | −.04 | .05 | .96 | .87 | 1.05 |
| RiskS severe symptoms b | −.03 | .04 | .97 | .90 | 1.04 |
| RiskS spreading virus c | −.03 | .04 | .97 | .90 | 1.04 |
| RiskO contracting d | .09 | .05 | 1.09 | .99 | 1.20 |
| RiskO severe symptoms e | −.10 | .04 | .91* | .83 | .99 |
| RE preventive behaviours f | .33 | .05 | 1.39** | 1.26 | 1.54 |
| SE preventive behaviours g | .79 | .08 | 2.21** | 1.91 | 2.56 |
| SN preventive behaviours h | −.06 | .03 | .95* | .89 | 1.00 |
| RiskS contracting*SE preventive behaviours | −.04 | .03 | .96 | .91 | 1.02 |
| RiskS severe symptoms*SE preventive behaviours | .07 | .03 | 1.07* | 1.01 | 1.14 |
| RiskS spreading virus*SE preventive behaviours | .05 | .03 | 1.05 | 1.00 | 1.04 |
| RiskO contracting*SE preventive behaviours | −.03 | .04 | .97 | .90 | 1.04 |
| RiskO severe symptoms*SE preventive behaviours | .08 | .03 | 1.08* | 1.01 | 1.15 |
The null model (M0) classified 69.4% of persons correctly, the main effects model (M1) classified 76% of persons correctly, and the full model (M2) classified 76.2% of persons correctly. Model fit improved with inclusion of main, and interaction effects: = 233.66 (df = 8), p < 0.001; = 261.81 (df = 13), p < 0.001. N = 891. CI = confidence interval; LL = lower level; UL = upper level.
Risk to self of contracting COVID‐19.
Risk to self of developing severe symptoms.
Risk to self of spreading the virus.
Risk to others of contracting COVID‐19.
Risk to others of developing severe symptoms.
Response efficacy for preventive behaviours.
Self‐efficacy for preventive behaviours.
Social norm for preventive behaviours.
p < .05,
p < .01.
Disconfirming H1, H2, and H7 neither risk perceptions nor social norms related to intentions to engage in social distancing (see Table 3). In line with H3, a one‐unit increase in response efficacy resulted in a 41% increase in the odds of endorsing this intention. Confirming H4, a one‐unit increase in self‐efficacy resulted in a 80% increase in the odds of forming this intention for people with average perceptions of risk to self of contracting the virus and of developing severe symptoms. Two interactions emerged (see Figure S2): higher risk to oneself for contracting the virus and higher risk to oneself for developing severe symptoms were positively related to the odds of endorsing the intention to socially distance when self‐efficacy was below −2.90 and above 0.25 for the risk to oneself for contracting the virus and below −0.77 for risk to oneself for developing severe symptoms. These results disconfirmed H6.
Table 3.
Logistic regression results for intention to engage in social distancing
| Variable | B | SE | OR | 95% CI for OR | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Intercept | −2.10 | .49 | .12** | ||
| RiskS contracting a | −.07 | .04 | .94 | .86 | 1.02 |
| RiskS severe symptoms b | .02 | .04 | 1.02 | .95 | 1.10 |
| RiskS spreading virus c | −.01 | .03 | .99 | .93 | 1.06 |
| RiskO contracting d | .07 | .05 | 1.07 | .98 | 1.17 |
| RiskO severe symptoms e | −.03 | .04 | .97 | .89 | 1.05 |
| RE social distancing f | .34 | .06 | 1.41** | 1.23 | 1.57 |
| SE social distancing g | .59 | .06 | 1.80** | 1.59 | 2.03 |
| SN social distancing h | −.04 | .03 | .96 | .91 | 1.01 |
| RiskS contracting*SE social distancing | −.08 | .03 | .92** | .88 | .97 |
| RiskS severe symptoms*SE social distancing | −.08 | .02 | .93** | .88 | .97 |
| RiskS spreading virus*SE social distancing | −.01 | .02 | 1.00 | .96 | 1.03 |
| RiskO contracting*SE social distancing | .04 | .03 | 1.04 | .99 | 1.10 |
| RiskO severe symptoms*SE social distancing | .01 | .03 | 1.01 | .96 | 1.06 |
The null model (M0) classified 69.2% of persons correctly, the main effects model (M1) classified 74.7% of persons correctly, and the full model (M2) classified 74.7% of persons correctly. Model fit improved with inclusion of main, and interaction effects: = 211.50 (df = 8), p < 0.001; = 236.21 (df = 13), p < 0.001. N = 889. CI = confidence interval; LL = lower level; UL = upper level.
Risk to self of contracting COVID‐19.
Risk to self of developing severe symptoms.
Risk to self of spreading the virus.
Risk to others of contracting COVID‐19.
Risk to others of developing severe symptoms.
Response efficacy for social distancing.
Self‐efficacy for social distancing.
Social norm for social distancing.
p < .05,
p < .01.
Confirming H2, H3, and H4, intention for engaging in recommended behaviours in case of symptoms was positively related to response efficacy, self‐efficacy, and the perceived risk to others of contracting COVID‐19 (see Table 4): A one‐unit increase in response efficacy resulted in a 22% increase in the odds of forming this intention, and a one‐unit increase in the risk to others of contracting the virus resulted in a 10% increase in the odds of forming this intention. A one‐unit increase in self‐efficacy resulted in 91% increase in the odds of endorsing this intention for people with average perception of risk to self of developing severe symptoms. Confirming H7 but contrasting H1 and H2, a one‐unit increase in social norms (H7), a one‐unit increase in perceived risk to oneself of contracting COVID‐19, and a one‐unit increase in perceived risk to others of developing severe symptoms resulted each in 9% decrease of the odds of forming this intention. Again disconfirming H6, only one interaction reached significance (see Figure S3): A higher risk to oneself for developing severe symptoms related negatively to the odds of forming an intention to adopt recommended behaviours at values of self‐efficacy below −5.40.
Table 4.
Logistic regression results for intention to engagen in recommended behaviours
| Variable | B | SE | OR | 95% CI for OR | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Intercept | −.67 | .43 | .51 | ||
| RiskS contracting a | −.10 | .04 | .91* | .83 | .99 |
| RiskS severe symptoms b | .01 | .04 | 1.01 | .94 | 1.09 |
| RiskS spreading virus c | −.03 | .03 | .97 | .91 | 1.03 |
| RiskO contracting d | .09 | .05 | 1.10* | 1.01 | 1.20 |
| RiskO severe symptoms e | −.10 | .04 | .91* | .83 | .98 |
| RE recommended behaviours f | .20 | .05 | 1.22** | 1.11 | 1.34 |
| SE recommended behaviours g | .65 | .07 | 1.91** | 1.66 | 2.20 |
| SN recommended behaviours h | −.08 | .03 | .93** | .88 | .98 |
| RiskS contracting*SE recommended behaviours | .01 | .03 | 1.01 | .94 | 1.07 |
| RiskS severe symptoms*SE recommended behaviours | .06 | .03 | 1.06* | 1.003 | 1.12 |
| RiskS spreading virus*SE recommended behaviours | .01 | .03 | 1.01 | .96 | 1.06 |
| RiskO contracting*SE recommended behaviours | .02 | .03 | 1.02 | .96 | 1.09 |
| RiskO severe symptoms*SE recommended behaviours | .04 | .03 | 1.04 | .98 | 1.11 |
The null model (M0) classified 69.9% of persons correctly, the main effects model (M1) classified 74.6% of persons correctly, and the full model (M2) classified 74.4% of persons correctly. Model fit improved with inclusion of main, and interaction effects: = 171.71 (df = 8), p < 0.001; = 187.11 (df = 13), p < 0.001. N = 889. CI = confidence interval; LL = lower level; UL = upper level.
Risk to self of contracting COVID‐19.
Risk to self of developing severe symptoms.
Risk to self of spreading the virus.
Risk to others of contracting COVID‐19.
Risk to others of developing severe symptoms.
Response efficacy for recommended behaviours in case of symptoms.
Self‐ efficacy for recommended behaviours in case of symptoms.
Social norm for recommended behaviours in case of symptoms.
p < .05,
p < .01.
Finally, disconfirming H1 and H2 perceived risks were unrelated to intentions for engaging in alternative measures except for a negative effect of perceived risk to others of developing severe symptoms on this intention (see Table 5). Confirming H3, a one‐unit increase in response efficacy resulted in 55% increase in the odds of endorsing this intention. Contrasting H4, self‐efficacy was unrelated to this intention. A one‐unit increase in social norms resulted in a 7% decrease in the odds of intending to use alternative measures, confirming H7. Disconfirming H6, only the interaction effect between perceived risk to others of contracting COVID‐19 and self‐efficacy was significant (see Figure S4): For values below −3.01 of self‐efficacy, the risk to others of contracting COVID‐19 was positively related to the intention to engage in alternative measures (Table 5).
Table 5.
Logistic regression results for intention to engage in alternatives measures
| Variable | B | SE | OR | 95% CI for OR | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Intercept | −2.34 | .20 | .10** | ||
| RiskS contracting a | .0002 | .05 | 1.00 | .91 | 1.10 |
| RiskS severe symptoms b | .05 | .04 | 1.05 | .97 | 1.14 |
| RiskS spreading virus c | .05 | .04 | 1.05 | .97 | 1.12 |
| RiskO contracting d | −.02 | .05 | .98 | .89 | 1.08 |
| RiskO severe symptoms e | −.12 | .05 | .88** | .81 | .97 |
| RE alternatives f | .44 | .03 | 1.55** | 1.45 | 1.65 |
| SE mean g | .14 | .08 | 1.15 | .99 | 1.33 |
| SN alternatives h | −.07 | .03 | .93* | .89 | .98 |
| RiskS contracting*SE mean | −.06 | .03 | .95 | .89 | 1.01 |
| RiskS severe symptoms*SE mean | −.02 | .03 | .98 | .93 | 1.04 |
| RiskS spreading virus*SE mean | .01 | .03 | 1.01 | .96 | 1.06 |
| RiskO contracting*SE mean | −.09 | .04 | .92* | .85 | .99 |
| RiskO severe symptoms*SE mean | .02 | .03 | 1.02 | .96 | 1.09 |
The null model (M0) classified 69.8% of persons correctly, the main effects model (M1) classified 80.8% of persons correctly, and the full model (M2) classified 80.3% of persons correctly. Model fit improved with inclusion of main, and interaction effects: = 279.98 (df = 8), p < 0.001; = 297.31 (df = 13), p < 0.001. N = 843. CI = confidence interval; LL = lower level; UL = upper level.0
Risk to self of contracting COVID‐19.
Risk to self of developing severe symptoms.
Risk to self of spreading the virus.
Risk to others of contracting COVID‐19.
Risk to others of developing severe symptoms.
Response efficacy for alternative measures.
Mean score of self‐efficacy for preventive behaviours, social distancing, and recommended behaviours in case of symptoms.
Social norm for alternative measures.
p < .05,
p < .01.
Table 6.
Logistic regression results for the endorsement of preventive behaviours
| Variable | B | SE | OR | 95% CI for OR | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Intercept | −2.23 | .45 | .11** | ||
| RiskS contracting a | −.02 | .04 | .98 | .91 | 1.07 |
| RiskS severe symptoms b | −.09 | .04 | .92* | .85 | .97 |
| RiskS spreading virus c | −.004 | .03 | 1.00 | .93 | 1.07 |
| RiskO contracting d | −.14 | .05 | .87** | .79 | .95 |
| RiskO severe symptoms e | −.08 | .04 | .93 | .85 | 1.01 |
| RE preventive behaviours f | .12 | .05 | 1.12* | 1.02 | 1.24 |
| SE preventive behaviours g | .54 | .08 | 1.72** | 1.48 | 1.99 |
| SN preventive behaviours h | −.02 | .03 | .98 | .93 | 1.04 |
| Intent preventive behaviours i | 1.99 | .21 | 7.33** | 4.91 | 10.95 |
| RiskS contracting* SE preventive behaviours | .05 | .03 | 1.05 | 1.00 | 1.11 |
| RiskS severe symptoms* SE preventive behaviours | .02 | .03 | 1.02 | .96 | 1.08 |
| RiskS spreading virus* SE preventive behaviours | −.01 | .03 | .99 | .93 | 1.04 |
| RiskO contracting* SE preventive behaviours | .13 | .04 | 1.14** | 1.06 | 1.22 |
| RiskO severe symptoms* SE preventive behaviours | .07 | .03 | 1.07* | 1.00 | 1.14 |
The null model (M0) classified 55.2% of persons correctly, the main effects model (M1) classified 75.3% of persons correctly, and the full model (M2) classified 76.6% of persons correctly. Model fit improved with inclusion of main, and interaction effects: = 293.45 (df = 9), p < 0.001; = 336.42 (df = 14), p < 0.001. N = 887.
CI = confidence interval; LL = lower level; UL = upper level.
Risk to self of contracting COVID‐19.
Risk to self of developing severe symptoms.
Risk to self of spreading the virus.
Risk to others of contracting COVID‐19.
Risk to others of developing severe symptoms.
Response efficacy for preventive behaviours.
Self‐efficacy for preventive behaviours.
Social norm for preventive behaviours.
Intention for preventive behaviours dichotomous).
p < .05,
p < .01.
Patterns of results remained the same in sensitivity analyses, with the effects of response efficacy and self‐efficacy as well as social norms if present being robust across all models.
Predicting self‐reported behaviours
Disconfirming H1, H2, and H7, most of the perceived risks and social norms were irrelevant for preventive behaviours (see Table 6, and Figure 1 for an overview). A one‐unit increase in perceived risk to oneself for developing severe symptoms resulted in a 8% decrease, and a one‐unit increase in perceived risk to others for contracting COVID‐19 resulted in a 13% decrease in the odds of engaging in preventive behaviours for people with average self‐efficacy. Confirming H3, H4, and H5, one‐unit increases in response efficacy (H3) and intentions (H5) resulted in 12% and 633% increase in the odds of endorsing preventive behaviours, and a one‐unit increase in self‐efficacy (H4) resulted in 72% increased odds of preventive behaviours for people with average risk to others of contracting the virus and of developing severe symptoms.
Disconfirming H6, the probing of the two significant interaction effects (see Figure S5) indicates that higher levels of perceived risk to others for contracting COVID‐19 related to lower odds for preventive behaviours at values of the self‐efficacy below 0.43. Higher levels of risk to others developing severe symptoms related to a lower odds for preventive behaviours at values below −0.14 of the mean‐centred self‐efficacy.
Disconfirming H1 and H2 for social distancing (see Table 7), the only risk perceptions relevant for social distancing were the risk to self for developing severe symptoms (positive association), and the risk to others for contracting COVID‐19 (negative association). Moreover, the odds of social distancing increased with higher intentions (confirming H5), higher self‐efficacy, and higher response efficacy (confirming H3 and H4). For self‐efficacy, a one‐unit increase in self‐efficacy resulted in 84% increase in the odds of social distancing at average levels for the risk to others for developing severe symptoms. Contrasting H7, perceived social norms were unrelated to social distancing. Again disconfirming H6, the association between the risk to others for developing severe symptoms and the odds for social distancing behaviour was significantly negative at levels below −.20 of self‐efficacy (see Figure S6).
Table 7.
Logistic regression results for social distancing
| Variable | B | SE | OR | 95% CI for OR | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Intercept | −2.45 | .53 | .09** | ||
| RiskS contracting a | .01 | .05 | 1.01 | .93 | 1.11 |
| RiskS severe symptoms b | .10 | .04 | 1.10* | 1.02 | 1.19 |
| RiskS spreading virus c | −.01 | .04 | .99 | .93 | 1.06 |
| RiskO contracting d | −.10 | .05 | .90* | .82 | .99 |
| RiskO severe symptoms e | −.07 | .05 | .93 | .85 | 1.02 |
| RE social distancing f | .13 | .06 | 1.14* | 1.02 | 1.28 |
| SE social distancing g | .61 | .08 | 1.84** | 1.59 | 2.13 |
| SN social distancing h | .02 | .03 | 1.02 | .96 | 1.08 |
| Intent social distancing i | 2.33 | .20 | 10.26** | 6.88 | 15.29 |
| RiskS contracting*SE social distancing | −.04 | .03 | .96 | .91 | 1.01 |
| RiskS severe symptoms*SE social distancing | −.05 | .03 | .95 | .90 | 1.00 |
| RiskS spreading virus*SE social distancing | .01 | .02 | 1.01 | .97 | 1.05 |
| RiskO contracting*SE social distancing | −.04 | .03 | .96 | .90 | 1.02 |
| RiskO severe symptoms*SE social distancing | .10 | .03 | 1.11** | 1.05 | 1.17 |
The null model (M0) classified 60.9% of persons correctly, the main effects model (M1) classified 80.3% of persons correctly, and the full model (M2) classified 81.2% of persons correctly. Model fit improved with inclusion of main, and interaction effects: = 392.57 (df = 9), p < 0.001; = 411.66 (df = 14), p < 0.001. N = 887.
CI = confidence interval; LL = lower level; UL = upper level.
Risk to self of contracting COVID‐19.
Risk to self of developing severe symptoms.
Risk to self of spreading the virus.
Risk to others of contracting COVID‐19.
Risk to others of developing severe symptoms.
Response efficacy for social distancing.
Self‐efficacy for social distancing.
Social norm for social distancing.
Intention for social distancing dichotomous).
p < .05,
p < .01.
Contrasting H1 and H2, risk perceptions were either not or negatively related to recommended behaviours in case of symptoms (see Table 8). Confirming H3, H4, and H5, the odds for recommended behaviours increased by 16% for a one‐unit increase in response efficacy, by 515% for a one‐unit increase in intentions (H5), and by 36% for a one‐unit increase in self‐efficacy for average levels in risk to self and others of contracting the virus and risk to others of developing severe symptoms. Perceived social norms were unrelated to recommended behaviours, disconfirming H7. Disconfirming H6, three interactions between risk perceptions and self‐efficacy were significant (see Figure S7): Higher levels of perceived risk to oneself of contracting COVID‐19 related to increased odds in recommended behaviours at levels of self‐efficacy below −.88. Again, only at levels of self‐efficacy below −.74 the higher perceived risk to others of contracting COVID‐19 resulted in lower odds for recommended behaviours. The same pattern emerged for the perceived risk to others of developing severe symptoms which resulted in higher odds in recommended behaviours in case of symptoms only at levels of self‐efficacy below −.61.
Table 8.
Logistic regression results for recommended behaviours
| Variable | B | SE | OR | 95% CI for OR | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Intercept | −1.78 | .47 | .17** | ||
| RiskS contracting a | .05 | .04 | 1.05 | .96 | 1.14 |
| RiskS severe symptoms b | −.001 | .04 | 1.00 | .93 | 1.08 |
| RiskS spreading virus c | −.11 | .03 | .90** | .84 | .96 |
| RiskO contracting d | −.04 | .05 | .96 | .88 | 1.05 |
| RiskO severe symptoms e | .06 | .04 | 1.06 | .97 | 1.15 |
| RE recommended behaviours f | .15 | .05 | 1.16** | 1.04 | 1.28 |
| SE recommended behaviours g | .31 | .06 | 1.36** | 1.21 | 1.54 |
| SN recommended behaviours h | .004 | .03 | 1.00 | .95 | 1.06 |
| Intent recommended behaviours i | 1.82 | .19 | 6.15** | 4.23 | 8.94 |
| RiskS contracting*SE recommended behaviours | −.06 | .03 | .94* | .89 | .99 |
| RiskS severe symptoms*SE recommended behaviours | −.04 | .03 | .97 | .92 | 1.02 |
| RiskS spreading virus*SE recommended behaviours | −.004 | .02 | 1.00 | .96 | 1.04 |
| RiskO contracting*SE recommended behaviours | .09 | .03 | 1.09* | 1.02 | 1.17 |
| RiskO severe symptoms*SE recommended behaviours | −.06 | .03 | .94* | .88 | 1.00 |
The null model (M0) classified 64.5% of persons correctly, the main effects model (M1) classified 76.2% of persons correctly, and the full model (M2) classified 76.6% of persons correctly. Model fit improved with inclusion of main, and interaction effects: = 214.13 (df = 9), p < 0.001; = 229.46 (df = 14), p < 0.001. N = 785.
CI = confidence interval; LL = lower level; UL = upper level.
Risk to self of contracting COVID‐19.
Risk to self of developing severe symptoms.
Risk to self of spreading the virus.
Risk to others of contracting COVID‐19.
Risk to others of developing severe symptoms.
Response efficacy for recommended behaviours in case of symptoms.
Self‐efficacy for recommended behaviours in case of symptoms.
Social norm for recommended behaviours in case of symptoms.
Intention for recommended behaviours in case of symptoms (dichotomous).
p < .05,
p < .01.
Finally, contrasting H1, H2, and H4, no effects emerged for risk perceptions and self‐efficacy for alternative behaviours (see Table 9). The odds for endorsing alternative behaviours were higher at higher levels of intentions and response efficacy, and for lower levels of social norms, confirming H3, H5, and H7. Moreover, but again disconfirming H6, higher levels of the perceived risk to self of developing severe symptoms were related to lower odds of self‐reported alternative behaviours at values of self‐efficacy higher than .03. (see Figure S8).
Table 9.
Logistic regression results for frequency alternative measures
| Variable | B | SE | OR | 95% CI for OR | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Intercept | −3.45 | .03 | .03** | ||
| RiskS contracting a | .08 | .06 | 1.08 | .96 | 1.22 |
| RiskS severe symptoms b | −.10 | .05 | .90 | .81 | 1.00 |
| RiskS spreading virus c | .06 | .05 | 1.06 | .96 | 1.17 |
| RiskO contracting d | −.07 | .06 | .94 | .83 | 1.06 |
| RiskO severe symptoms e | .01 | .06 | 1.01 | .90 | 1.14 |
| RE alternatives f | .33 | .04 | 1.39** | 1.28 | 1.51 |
| SE mean g | −.09 | .09 | .92 | .77 | 1.10 |
| SN alternatives h | −.10 | .04 | .91** | .85 | .97 |
| Intent alternatives i | 3.64 | .26 | 38.08** | 22.76 | 63.73 |
| RiskS contracting*SE mean | −.06 | .04 | .95 | .87 | 1.02 |
| RiskS severe symptoms*SE mean | −.08 | .04 | .92* | .86 | .99 |
| RiskS spreading virus*SE mean | .04 | .03 | 1.04 | .98 | 1.10 |
| RiskO contracting*SE mean | .01 | .05 | 1.01 | .92 | 1.10 |
| RiskO severe symptoms*SE mean | .03 | .04 | 1.03 | .95 | 1.12 |
The null model (M0) classified 70.4% of persons correctly, the main effects model (M1) 88.4% of persons correctly, and the full model (M2) classified 88.9% of persons correctly. Model fit improved with inclusion of main, and interaction effects: = 552.04 (df = 9), p < 0.001; = 560.91 (df = 14), p < 0.001. N = 829.
CI = confidence interval; LL = lower level; UL = upper level.
Risk to self of contracting COVID‐19.
Risk to self of developing severe symptoms.
Risk to self of spreading the virus.
Risk to others of contracting COVID‐19.
Risk to others of developing severe symptoms.
Response efficacy for alternative measures.
Mean score of self‐efficacy for preventive behaviours, social distancing, and recommended behaviours in case of symptoms.
Social norm for alternative measures.
Intention for alternative measures (dichotomous).
p < .05,
p < .01.
Patterns of results remained the same in sensitivity analyses, with the effects of response efficacy, self‐efficacy, and intentions, as well as social norms if present being robust across all models (see Tables S6–S9).
Discussion
Based on the PMT (Maddux & Rogers, 1983), this study set out to examine the associations between threat appraisals (different perceptions of risk to oneself and others), coping appraisals (response efficacy, self‐efficacy), and the interactions between self‐efficacy and risk perceptions with intentions for and the endorsement of preventive behaviours, social distancing, recommended behaviours in case of symptoms, and alternative measures during a nationwide lockdown in Switzerland in the face of the ongoing SARS‐CoV‐2 pandemic. The representative sample covered the three language regions and took place in the first phase of the (first) lockdown in Switzerland.
Across all different kinds of intentions and behaviours, response efficacy and self‐efficacy consistently emerged as the most important predictors. This supported our preregistered hypotheses and is in line with results from research on non‐pharmaceutical, behavioural measures in the context of epidemics (Lin et al., 2020; Timpka et al., 2014). It further confirms the important role of resources in contrast to the role of risk perceptions for behavioural change (Floyd et al., 2000; van Bavel et al., 2020).
The only exception of the consistent predictive power of self‐efficacy was the case of alternative measures. This was most likely due to the fact that the mean score of self‐efficacy did not match the specificity of the assessment of alternative behaviours, thus violating the principle of compatibility (Ajzen & Fishbein, 2005). Unfortunately, in this study we had not assessed self‐efficacy for alternative measures because it concerned behaviours that are not specific to facing the new coronavirus, such as praying or eating garlic, things that everybody can do if desired. Future studies should assess self‐efficacy for such behaviours as well in order to allow testing the interpretation offered above.
In sharp contrast to the consistent effects of response efficacy and self‐efficacy, the different kinds of risk perceptions were mostly unrelated to intentions and behaviour and, where present, pointed in the opposite direction than predicted. This result contradicts previous findings on the role of risk perception for behavioural decision making, behaviour change in general (e.g., Ferrer & Klein, 2015; Sheeran et al., 2014), and in the context of pandemics in particular (Bish & Michie, 2010; Niepel, Kranz, Borgonovi, Emslander, & Greiff, 2020). Context could be one potential explanation for the null effects of risk perception in the present study: People were in a nationwide lockdown with both public and private life being greatly reduced. Possibly, under these circumstances risk perceptions lost their relevance for intention formation and behaviours. Yet, the finding is consistent with other research on the PMT, indicating that risk perception is relatively less important for behaviour change than coping appraisals (Timpka et al., 2014).
Contrary to our hypotheses, some of the effects of risk perceptions on intentions and behaviour were negative: In this case, higher risk perception related to a lower likelihood of intentions and behaviour. Given the cross‐sectional nature of this study, one possible explanation is that of a reverse causation: People who already intend to or do engage in the protective behaviour perceive a lower risk. This has been called relative accuracy of risk perceptions (e.g., Brewer, Weinstein, Cuite, & Herrington, 2004; Renner, Schüz, & Sniehotta, 2008). The current results of risk perception speak to this hypothesis.
Interaction effects of risk perceptions with self‐efficacy were inconsistent: Most interactions turned out to be irrelevant, and where present, the pattern varied depending on the risk perceptions and outcomes. None of the interaction effects resulted in the hypothesized result that higher levels of risk perceptions are only positively related to intentions or behaviour at higher levels of self‐efficacy. To the contrary, some of the interaction effects indicated that lower levels of self‐efficacy together with higher levels of risk perceptions related to a lower likelihood of intentions and behaviour. This result might indicate a kind of ‘freezing’ in the face of high perceived risks when feeling unable to meet its challenges. This underscores the central role of self‐efficacy when perceiving high risks. Yet some interaction effects pointed in the opposite direction, in that lower self‐efficacy related positively to intentions and self‐reported behaviour when risk was perceived as higher. We refrain from speculating about these interaction effects given their unreliable nature across the eight different analyses. Future research is needed to clarify the interplay of risk perceptions and self‐efficacy when facing a situation like the beginning of a pandemic that is characterized by high uncertainty, little knowledge, and potentially also extreme harm.
We had hypothesized that social norms expressing disapproval of behaviours undermine the intentions and actual engagement in them. The hypothesis was supported for three of the four intentions, but not for most of the behaviours in this study. This latter result contradicts studies demonstrating social norms to relate to protective behaviours during pandemics (Bish & Michie, 2010). It might be that social norms expressing the approval for certain behaviours are more strongly related to people’s intentions and engagement in them. Social approval might be more rewarding than disapproval is punishing, leading to an asymmetry in the two kinds of social norms. Thus, an interesting question for future studies concerns the differences in effects of social approval and disapproval. Furthermore, other social determinants, such as social support (e.g., Scholz et al., 2016), might be more relevant for behavioural change, particularly given the increased levels of concern and worries (Lauri Korajlija & Jokic‐Begic, 2020; Yıldırım, Geçer, & Akgül, 2020) and loneliness (Luchetti et al., 2020) reported during the current pandemic.
One of the strengths of the current study is the representativeness of the sample and that it targeted a variety of theoretically important constructs hypothesized to contribute to intentions and behaviour to ward off potentially deadly health risks. However, the study also has several limitations. First, this study was a cross‐sectional survey preventing to draw causal inferences. Second, given the nature of the telephone‐based survey of the Swiss general population, the number of items had to be limited which resulted in single item assessments of the constructs. This has likely affected negatively the reliability of the measures. Moreover, we were unable to use validated measures as running a validation study was impossible given the sudden and quickly changing nature of the emerging pandemic requiring to launch the study as quickly as possible. In order to prepare for future research during unforeseen pandemics, it would be useful to develop a set of validated measures for behaviours commonly recommended during pandemics (Toussaint, Cheadle, Fox, & Williams, 2020). Finally, this survey allowed the assessment of self‐reported behaviours only. Although common in surveys aiming at a large sample representative for a country’s population, the likelihood of biased results due to over‐ or underreporting needs to be kept in mind.
In conclusion, this study provides important insights into the question which factors are of key relevance for behavioural change in the context of the worldwide COVID‐19 pandemic. Results indicate that interventions for promoting behavioural change in the general population during a nationwide lockdown to combat an ongoing pandemic should target people’s response efficacy and self‐efficacy rather than their risk perceptions. Moreover, this study emphasizes the importance to use behaviour change theories, such as the PMT, as a basis for investigations of factors affecting people’s behaviours during health crises such as this pandemic. Testing theoretically derived hypotheses allows to accumulate knowledge facilitating the development of campaigns for promoting behavioural measures in the general population for effectively countering the spread of pandemics.
Conflicts of interest
All authors declare no conflict of interest.
Author contributions
Urte Scholz, Ph.D. (Conceptualization; Formal analysis; Funding acquisition; Investigation; Methodology; Writing – original draft) Alexandra M. Freund (Conceptualization; Funding acquisition; Investigation; Methodology; Writing – review & editing).
Supporting information
Figure S1 Moderation of risk to others for developing severe symptoms (left panel) and moderation of risk to self for developing severe symptoms (right panel) with self‐efficacy for preventive behaviors on intention for preventive behaviors.
Figure S2 Moderation of risk to self of contracting Covid‐19 with self‐efficacy for social distancing (left panel) and moderation of risk to self for developing severe symptoms with self‐efficacy for social distancing (right panel) on intention for social distancing.
Figure S3 Moderation of risk to self for developing severe symptoms with self‐efficacy for recommended behaviors on intentions for recommended behaviors.
Figure S4 Moderation of risk to others of contracting Covid‐19 with self‐efficacy on intentions for alternative measures.
Figure S5 Moderation of risk to others for contracting Covid‐19 (left panel) and moderation of risk to others for developing severe symptoms (right panel) with self‐efficacy for preventive behaviors on preventive behavior.
Figure S6 Moderation of risk to others for developing severe symptoms with self‐efficacy on social distancing.
Figure S7 Moderation of risk to self for contracting Covid‐19 (upper left panel), moderation of risk to others for contracting Covid‐19 (upper right panel), and moderation of risk to others for developing severe symptoms (lower left panel) with self‐efficacy for recommended behaviors on recommended behaviors in case of symptoms.
Figure S8 Moderation of risk to self for developing severe symptoms with self‐efficacy on alternative behaviors.
Table S1 Correlations of all study variables.
Table S2 Logistic regression results for intention preventive behaviours with control variables.
Table S3 Logistic regression results for intention social distancing with control variables.
Table S4 Logistic regression results for intention recommended behaviours with control variables.
Table S5 Logistic regression results for intention alternatives measures with control variables.
Table S6 Logistic regression results for preventive behaviours with control variables.
Table S7 Logistic regression results for social distancing with control variables.
Table S8 Logistic regression results for recommended behaviours with control variables.
Table S9 Logistic regression results for frequency alternative measures with control variables.
Acknowledgements
The authors gratefully acknowledge the financial support provided by the University of Zurich for research related to the new Corona virus. The project was preregistered at DOI 10.17605/OSF.IO/G6EHD.
References
- Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50(2), 179–211. 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- Ajzen, I. (2020). Constructing a theory of planned behavior questionnaire. https://people.umass.edu/aizen/pdf/tpb.measurement.pdf [Google Scholar]
- Ajzen, I. , & Fishbein, M. (2005). The influence of attitudes on behavior. In Albarracín D., Johnson B. T. & Zanna M. P. (Eds.), The handbook of attitudes (pp. 173–221). Mahwah, NJ: Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Bish, A. & Michie, S. (2010). Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. British Journal of Health Psychology, 15(Pt 4), 797–824. 10.1348/135910710X485826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer, N. T. , Weinstein, N. D. , Cuite, C. L. , & Herrington, J. E. (2004). Risk perceptions and their relation to risk behavior. Annals of Behavioral Medicine, 27, 125–130. 10.1207/s15324796abm2702_7 [DOI] [PubMed] [Google Scholar]
- Bui, L. , Mullan, B. , & McCaffery, K. (2013). Protection motivation theory and physical activity in the general population: A systematic literature review. Psychology, Health & Medicine, 18, 522–542. 10.1080/13548506.2012.749354 [DOI] [PubMed] [Google Scholar]
- Davidson, K. W. , & Scholz, U. (2020). Understanding and predicting health behaviour change: A contemporary view through the lenses of meta‐reviews. Health Psychology Review, 14(1), 1–5. 10.1080/17437199.2020.1719368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer, R. A. , & Klein, W. M. (2015). Risk perceptions and health behavior. Current Opinion in Psychology, 5, 85–89. 10.1016/j.copsyc.2015.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field, A. (2018). Discovering statistics using IBM SPSS statistics (5th edn). London: SAGE. [Google Scholar]
- Floyd, D. L. , Prentice Dunn, S. , & Rogers, R. W. (2000). A meta‐analysis of research on protection motivation theory. Journal of Applied Social Psychology, 30, 407–429. 10.1111/j.1559-1816.2000.tb02323.x [DOI] [Google Scholar]
- Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis: A regression‐based approach (2nd edn). New York: Guilford Press. [Google Scholar]
- Hayes, A. F. , & Matthes, J. (2009). Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behavior Research Methods, 41, 924–936. 10.3758/BRM.41.3.924 [DOI] [PubMed] [Google Scholar]
- Kok, G. , Peters, G.‐J.‐ Y. , Kessels, L. T. E. , ten Hoor, G. A. , & Ruiter, R. A. C. (2018). Ignoring theory and misinterpreting evidence: The false belief in fear appeals. Health Psychology Review, 12, 111–125. 10.1080/17437199.2017.1415767 [DOI] [PubMed] [Google Scholar]
- Lau, J. T. F. , Kim, J. H. , Tsui, H. , & Griffiths, S. (2007). Perceptions related to human avian influenza and their associations with anticipated psychological and behavioral responses at the onset of outbreak in the Hong Kong Chinese general population. American Journal of Infection Control, 35(1), 38–49. 10.1016/j.ajic.2006.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauri Korajlija, A. , & Jokic‐Begic, N. (2020). Covid‐19: Concerns and behaviours in croatia. British Journal of Health Psychology, 25, 849–855. 10.1111/bjhp.12425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, C.‐Y. , Imani, V. , Majd, N. R. , Ghasemi, Z. , Griffiths, M. D. , Hamilton, K. , … Pakpour, A. H. (2020). Using an integrated social cognition model to predict COVID‐19 preventive behaviours. British Journal of Health Psychology, 25, 981–1005. 10.1111/bjhp.12465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, L. , McCloud, R. F. , Jung, M. , & Viswanath, K. (2018). Facing a health threat in a complex information environment: A national representative survey examining American adults' behavioral responses to the 2009/2010 A(H1N1) pandemic. Health Education & Behavior, 45(1), 77–89. 10.1177/1090198117708011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling, M. , Kothe, E. J. , & Mullan, B. A. (2019). Predicting intention to receive a seasonal influenza vaccination using protection motivation theory. Social Science & Medicine, 233, 87–92. 10.1016/j.socscimed.2019.06.002 [DOI] [PubMed] [Google Scholar]
- Luchetti, M. , Lee, J. H. , Aschwanden, D. , Sesker, A. , Strickhouser, J. E. , Terracciano, A. , & Sutin, A. R. (2020). The trajectory of loneliness in response to COVID‐19. American Psychologist, 75, 897–908. 10.1037/amp0000690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddux, J. E. , & Rogers, R. W. (1983). Protection motivation and self‐efficacy: A revised theory of fear appeals and attitude change. Journal of Experimental Social Psychology, 19, 469–479. 10.1016/0022-1031(83)90023-9 [DOI] [Google Scholar]
- Merriam Webster (2020). https://www.merriam‐webster.com/dictionary/pandemic
- Moran, K. R. , Del Valle, S. Y. , & Nishiura, H. (2016). A meta‐analysis of the association between gender and protective behaviors in response to respiratory epidemics and pandemics. PLoS One, 11, e0164541. 10.1371/journal.pone.0164541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolaides, C. , Avraam, D. , Cueto‐Felgueroso, L. , González, M. C. , & Juanes, R. (2020). Hand‐hygiene mitigation strategies against global disease spreading through the air transportation network. Risk Analysis, 40, 723–740. 10.1111/risa.13438 [DOI] [PubMed] [Google Scholar]
- Niepel, C. , Kranz, D. , Borgonovi, F. , Emslander, V. , & Greiff, S. (2020). The coronavirus (covid‐19) fatality risk perception of us adult residents in march and April 2020. British Journal of Health Psychology, 25, 883–888. 10.1111/bjhp.12438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renner, B. , Schüz, B. , & Sniehotta, F. F. (2008). Preventive health behavior and adaptive accuracy of risk perceptions. Risk Analysis, 28, 741–748. 10.1111/j.1539-6924.2008.01047.x [DOI] [PubMed] [Google Scholar]
- Rolison, J. J. , Hanoch, Y. , & Freund, A. M. (2019). Perception of risk for older adults: differences in evaluations for self versus others and across risk domains. Gerontology, 65, 547–559. 10.1159/000494352 [DOI] [PubMed] [Google Scholar]
- Rubin, G. J. , Potts, H. W. W. , & Michie, S. (2010). The impact of communications about swine flu (influenza A H1N1v) on public responses to the outbreak: Results from 36 national telephone surveys in the UK. Health Technology Assessment, 14, 183–266. 10.3310/hta14340-03 [DOI] [PubMed] [Google Scholar]
- Scholz, U. , Keller, R. , & Perren, S. (2009). Predicting behavioral intentions and physical exercise: A test of the health action process approach at the intrapersonal level. Health Psychology, 28, 702–708. 10.1037/a0016088 [DOI] [PubMed] [Google Scholar]
- Scholz, U. , Stadler, G. , Ochsner, S. , Rackow, P. , Hornung, R. , & Knoll, N. (2016). Examining the relationship between daily changes in support and smoking around a self‐set quit date. Health Psychology, 35, 514–517. 10.1037/hea0000286 [DOI] [PubMed] [Google Scholar]
- Sheeran, P. , Harris, P. R. , & Epton, T. (2014). Does heightening risk appraisals change people's intentions and behavior? A meta‐analysis of experimental studies. Psychological Bulletin, 140, 511–543. 10.1037/a0033065 [DOI] [PubMed] [Google Scholar]
- Timpka, T. , Spreco, A. , Gursky, E. , Eriksson, O. , Dahlström, Ö. , Strömgren, M. , … Holm, E. (2014). Intentions to perform non‐pharmaceutical protective behaviors during influenza outbreaks in Sweden: A cross‐sectional study following a mass vaccination campaign. PLoS One, 9, e91060. 10.1371/journal.pone.0091060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tooher, R. , Collins, J. E. , Street, J. M. , Braunack‐Mayer, A. , & Marshall, H. (2013). Community knowledge, behaviours and attitudes about the 2009 H1N1 Influenza pandemic: A systematic review. Influenza and Other Respiratory Viruses, 7, 1316–1327. 10.1111/irv.12103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toussaint, L. L. , Cheadle, A. D. , Fox, J. , & Williams, D. R. (2020). Clean and contain: Initial development of a measure of infection prevention behaviors during the COVID‐19 pandemic. Annals of Behavioral Medicine, 54, 619–625. 10.1093/abm/kaaa064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Bavel, J. J. V. , Baicker, K. , Boggio, P. S. , Capraro, V. , Cichocka, A. , Cikara, M. , … Willer, R. (2020). Using social and behavioural science to support COVID‐19 pandemic response. Nature Human Behaviour, 4, 460–471. 10.1038/s41562-020-0884-z [DOI] [PubMed] [Google Scholar]
- WHO (2019). Advice for public: Coronavirus disease (COVID‐19) advice for the public. https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/advice‐for‐public [Google Scholar]
- Williams, L. , Rasmussen, S. , Kleczkowski, A. , Maharaj, S. , & Cairns, N. (2015). Protection motivation theory and social distancing behaviour in response to a simulated infectious disease epidemic. Psychology Health & Medicine, 20, 832–837. 10.1080/13548506.2015.1028946 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2020). WHO Director‐General's opening remarks at the media briefing on COVID‐19 ‐ 11 March 2020. https://www.who.int/dg/speeches/detail/who‐director‐general‐s‐opening‐remarks‐at‐the‐media‐briefing‐on‐covid‐19–‐11‐march‐2020 [Google Scholar]
- Yıldırım, M. , Geçer, E. , & Akgül, Ö. (2020). The impacts of vulnerability, perceived risk, and fear on preventive behaviours against covid‐19. Psychology, Health & Medicine, 26(1), 35–43. 10.1080/13548506.2020.1776891 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Moderation of risk to others for developing severe symptoms (left panel) and moderation of risk to self for developing severe symptoms (right panel) with self‐efficacy for preventive behaviors on intention for preventive behaviors.
Figure S2 Moderation of risk to self of contracting Covid‐19 with self‐efficacy for social distancing (left panel) and moderation of risk to self for developing severe symptoms with self‐efficacy for social distancing (right panel) on intention for social distancing.
Figure S3 Moderation of risk to self for developing severe symptoms with self‐efficacy for recommended behaviors on intentions for recommended behaviors.
Figure S4 Moderation of risk to others of contracting Covid‐19 with self‐efficacy on intentions for alternative measures.
Figure S5 Moderation of risk to others for contracting Covid‐19 (left panel) and moderation of risk to others for developing severe symptoms (right panel) with self‐efficacy for preventive behaviors on preventive behavior.
Figure S6 Moderation of risk to others for developing severe symptoms with self‐efficacy on social distancing.
Figure S7 Moderation of risk to self for contracting Covid‐19 (upper left panel), moderation of risk to others for contracting Covid‐19 (upper right panel), and moderation of risk to others for developing severe symptoms (lower left panel) with self‐efficacy for recommended behaviors on recommended behaviors in case of symptoms.
Figure S8 Moderation of risk to self for developing severe symptoms with self‐efficacy on alternative behaviors.
Table S1 Correlations of all study variables.
Table S2 Logistic regression results for intention preventive behaviours with control variables.
Table S3 Logistic regression results for intention social distancing with control variables.
Table S4 Logistic regression results for intention recommended behaviours with control variables.
Table S5 Logistic regression results for intention alternatives measures with control variables.
Table S6 Logistic regression results for preventive behaviours with control variables.
Table S7 Logistic regression results for social distancing with control variables.
Table S8 Logistic regression results for recommended behaviours with control variables.
Table S9 Logistic regression results for frequency alternative measures with control variables.


