Abstract
To predict whether the COVID‐19 pandemic and transplant center responses could have resulted in preventable deaths, we analyzed registry information of the US end‐stage renal disease (ESRD) patient population awaiting kidney transplantation. Data were from the Organ Procurement and Transplantation Network (OPTN), the US Centers for Disease Control and Prevention, and the United States Renal Data System. Based on 2019 OPTN reports, annualized reduction in kidney transplantation of 25%–100% could result in excess deaths of wait‐listed (deceased donor) transplant candidates from 84 to 337 and living donor candidate excess deaths from 35 to 141 (total 119–478 potentially preventable deaths of transplant candidates). Changes in transplant activity due to COVID‐19 varied with some centers shutting down while others simply heeded known or suspected pandemic risks. Understanding potential excess mortality for ESRD transplant candidates when circumstances compel curtailment of transplant activity may inform policy and procedural aspects of organ transplant systems allowing ways to best inform patients and families as to potential risks in shuttering organ transplant activity. Considering that more than 700 000 Americans have ESRD with 100 000 awaiting a kidney transplant, our highest annual estimate of 478 excess total deaths from postponing kidney transplantation seems modest.
Keywords: COVID‐19, excess mortality, kidney transplant candidates, transplant program activity
1. INTRODUCTION
Novel coronavirus‐19 (COVID‐19), its resultant pandemic, and the feared viral SARS‐CoV‐2 infection risks, have led to various transformations in organ transplantation in the United States and worldwide. Withholding or postponing kidney transplantation for patients with end‐stage renal disease (ESRD) has occurred for manifold reasons including the need for hospital beds to treat COVID‐19 patients, uncertainty as to the transmission of virus from deceased organ donors, issues with testing for viral presence, limitations imposed on operating suites, concerns with professional staffing, the potential for substantial postoperative mortality risk from COVID‐19 infection in any patient, and other circumstances which have accompanied a most unpredictable and potentially lethal virus. 1 , 2 , 3 , 4 , 5 , 6 , 7 While the United Network for Organ Sharing has confirmed the decreased numbers of kidney transplants from both deceased and living donors, no analysis has emerged to estimate the number of patients who might be expected to die due to delay in receipt of a living or deceased donor kidney. 8
Estimates of US deaths due to delays and cancelations of kidney transplantation may not only shed light on lost opportunities to save lives, but also point to revisions of policies and planning which could address future interruptions in the practice of organ transplantation. Especially with ESRD transplant candidates, the ubiquitous asset of US dialysis may compel an unsubstantiated assessment that kidney transplantation can wait because no patient will suffer or die while waiting longer for a kidney. Other factors such as reduced social interactions, organ donation, and recovery imperatives, as well as the already‐stated program cancelations may support such a temporizing approach. While ESRD professionals understand the mortality risks associated with ongoing dialysis, there is little to enlighten patients, caregivers, or families about additive risks if kidney transplantation were partially or completely curtailed for some period of time.
This study seeks to predict the possible loss of US lives due to the delay and cancelation of kidney transplantation. The analyses are based on past measures of known mortality risks among different categories of patients receiving maintenance dialysis, those who are wait‐listed for a deceased donor kidney, those scheduling a living donor transplant, and kidney recipients already transplanted. We sought to estimate the number of excess deaths related to various levels of interruptions to kidney transplant care in circumstances such as the COVID‐19 pandemic.
2. METHODS
2.1. Data sources
Transplant and ESRD data including counts and characteristics of donors and recipients were taken from the US Department of Health and Human Services Organ Procurement and Transplantation Network (OPTN). 9 Mortality rates were obtained from the US Centers for Disease Control and Prevention and the United States Renal Data System. 10 , 11
2.2. Analysis
Calculations were performed to estimate the number of deaths which would result when considering two factors: (1) a baseline count of deceased and living donor transplants for 2019 from the OPTN and (2) the difference in the mortality rates that a typical patient on the deceased donor waiting list would experience if transplanted.
Calculations considered that a patient who is on the deceased donor waitlist and is subsequently transplanted exchanges one risk (dialysis mortality) for another typically lower risk (transplant mortality). The higher mortality estimates are based on the delta (Δ) loss rate where the former is the mortality for wait‐listed dialysis patients and the latter is the loss rate experienced if patients had been transplanted.
2.3. Outcomes
The Δ mortality rate is based on the reported values of mortality risk for wait‐listed patients in 2016 (5.3%/year), compared with the lower transplant mortality risk for a patient with a successfully functioning transplant (3.26%/year). 12 Therefore, the difference (5.30% − 3.26% = 2.04%) in mortality was rounded to 2 percentage points. Stated otherwise, the lower risk of dying with a kidney transplant was subtracted from the higher risk of dying while on dialysis but wait‐listed for a kidney, the difference being excess mortality. For completeness and comparison, mortality rates for the general population and Medicare beneficiaries over age 65 years were noted. Counts of excess mortality were estimated for a range of possible reductions in transplant services (25%–100%).
3. RESULTS
Mortality rates vary widely in the United States for the population at large and for persons suffering from ESRD (Figure 1) (figure results rounded to one‐tenth of 1%). 13 While the risk of dying for all Americans is 8.6 per 1000 per year (0.86%) that figure rises to 43.8 deaths annually per 1000 (4.38%) for persons over age 65 years and on Medicare. For all dialysis patients, the mortality rate is 178.9 deaths per thousand or 17.89%, and the mortality rate for all ESRD patients (inclusive of every dialysis and kidney transplant patient) is 137.6 deaths per 1000 patients per year, or 13.76%. Transplant wait‐listed dialysis patients, who may be younger and healthier than those not evaluated for transplant, have a mortality rate of 53.0 per 1000 patient years, or 5.3%, while patients with a functioning kidney transplant have a mortality rate of 32.6 per 1000 patients or 3.26% (Δ 2.04 percentage points). The mortality risk for the entire over age 65 US Medicare population is lower than that for the depicted ESRD categories and wait‐listed transplant candidates suffer an increasing mortality risk as they grow older, particularly beyond age 60 and 65 years. 13
FIGURE 1.
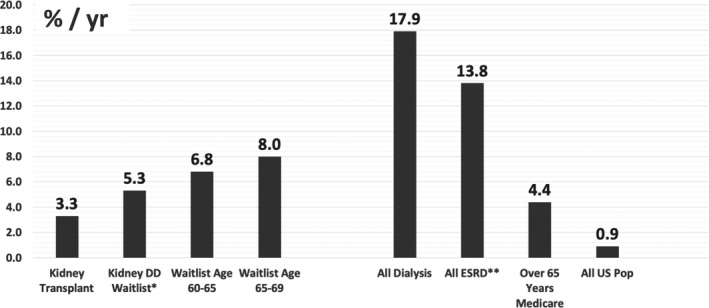
Annual mortality rate for kidney failure and all US populations, 2017. ESRD mortality rates from mortality reference tables US Renal Data System, National Institutes of Health, NIDDK, Bethesda, MD, 2018. 13 (Percentage rounded to one‐tenth of 1%). *Deceased donor (DD) waitlist data. **All End‐stage renal disease (ESRD) = dialysis + kidney transplant populations
This rounded 2 percentage point difference in mortality rates between remaining on dialysis and obtaining a kidney transplant differs in terms of real numbers for living donor and deceased donor candidates (Figure 2). 9 This is due to the two different sizes of the 2019 comparable potentially transplanted populations; that is, patients receiving a living donor kidney (6879 per study year), and those transplanted with a deceased donor organ (16 534 per study year). The calculated estimates of possible additional deaths of patients awaiting living donor kidneys and deceased donor kidneys are based on the annualized degree of transplant center disruptions. The stepwise degrees of transplant center postponement in the analysis range from 25% to 100% (complete closure of all US kidney transplant centers) over a period of one year.
FIGURE 2.
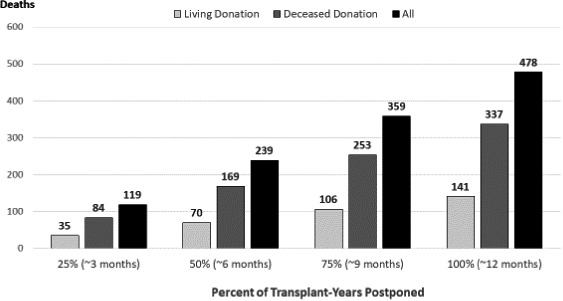
Annual number of predicted living and deceased donor kidney transplant candidate excess deaths due to disruptions in kidney transplant activity in the United States. Baseline: all Deceased Donor Transplants, 16 534 in 2019; https://optn.transplant.hrsa.gov/data/view‐data‐reports/national‐data/#. 9 Numbered deaths are the predicted increased differences between waitlisted and potentially transplanted patients if levels of kidney transplant postponement were to be realized
With a Δ death rate of 2 percentage points per year and a baseline of 6867 living donor transplants, additional deaths if living donor transplants were canceled would vary from 35 at a decrement of 25% in US transplant activity, to 141 deaths if 100% if all living donor transplant activities were to be curtailed for one year. With deceased donor kidney transplantation, considering a baseline of 16 534 deceased donor transplants in 2019, excess mortality would vary from 84 to 337 patients awaiting a deceased donor kidney depending on how many transplants were not performed because of the duration of inactivity. For example, if no deceased donor transplants were done for 9 months in the United States, the additional deaths in the following year would be 253 as depicted in the third column of Figure 2.
The number of estimated deaths assumes that the waiting living donor and deceased donor patients continue to remain transplant candidates while being subject to the dialysis‐associated mortality rate of 5.30% per year and not the lower 3.26% mortality had they been transplanted. The total calculated excess mortality for all United States suitable kidney transplant candidates would range from 119 to 478 persons with cancelation of 25% and 100% of kidney transplants, respectively. Importantly, the calculated actual decrement for the six months, March through August of 2020, does not appear to have been sustained, dropping overall a total of 6% for deceased donor kidney transplants and 26% for live donor kidney transplants when compared to February 2020 baseline activity (Table 1). 14
TABLE 1.
COVID‐19 impact on US kidney transplant (KXP) activity March through August 2020 a
| US Kidney transplants by month 2020 | Feb baseline | Mar | Apr | May | Jun | Jul | Aug | Total 6 mo. Mar‐Aug |
|---|---|---|---|---|---|---|---|---|
| Deceased donor | 1517 | 1323 | 1083 | 1262 | 1685 | 1649 | 1585 | 8587 |
| Live donor | 505 | 302 | 72 | 322 | 525 | 543 | 473 | 2237 |
| % Baseline (Feb) | ||||||||
| Deceased Donor KXP | 100 | 87 | 71 | 83 | 111 | 109 | 104 | 94 b |
| Live donor KXP | 100 | 60 | 14 | 64 | 104 | 108 | 94 | 74 b |
After: Hil, G, National Kidney Registry, Sept. 2020 14
Total percent calculation: total 6 month transplant activity ÷ 6 = Average monthly transplants. Average monthly transplants ÷ baseline (Feb) × 100 = Average monthly % for 6 month period.
4. DISCUSSION
The development of policy regarding organ donation and transplantation in the United States has taken numerous issues into account now and for nearly three decades. 1 , 8 , 15 , 16 , 17 , 18 Factors important in policy considerations have included patient‐centered (donor and recipient) features such as age, race, and immunologic status, as well as system‐related features such as organ procurement organization and transplant center performance measures or regulation‐driven aversions to accept less‐than‐perfect donor organs and transplant candidates. Donor and recipient infection have always been a primary consideration, especially if potential lethal outcomes might ensue. Early in 2020, the feared patient and system‐related risks posed by the COVID‐19 viral pandemic compelled the entire transplant enterprise to consider options which even included complete cessation of organ transplant activities.
Any analysis of survival or mortality based on past events or circumstances documented by a comprehensive long‐term database such as the USRDS 12 may seem a constant hazard or, if otherwise analyzed, a continuous or actuarial change in risk depending on the methods used in the referenced database. We employed calculations based on recent historic data to predict excess mortality in the US ESRD patient population awaiting kidney transplant if kidney transplantation was limited due to the COVID‐19 pandemic compared with usual levels of kidney transplant activity. Considering that over one‐half million Americans are on dialysis and that approximately 100 000 are actively awaiting a kidney transplant, our highest annual estimate of 478 excess total deaths seems modest, especially since total curtailment of US kidney transplantation for an entire year seems highly unlikely. And, the comparator dialysis mortality rate of 5.3% for patients awaiting transplant cannot account for possible COVID‐19 risks, as yet unknown, for kidney transplant candidates. Furthermore, the increased postoperative mortality associated with the COVID‐19 pandemic may have placed lives of both living kidney donors and newly transplanted patients at heightened risk if all centers had remained fully functional. 2 , 3 , 4 , 5 , 6 , 8 , 18
Our estimates of postponing or canceling kidney transplantation were different in deceased donor and living donor circumstances related to the COVID‐19 pandemic as depicted in Figure 2. In deceased donor kidney transplantation, the organs not transplanted would be lost for all time even if the kidneys were recovered, resulting in a decrement of the total resource which accounts for the majority of US kidney transplants. In the case of living donor transplants, the procedure may just be delayed. But, in some cases a living donor kidney transplant might never occur due to evolving clinical complications of either the donor or the recipient. In all cases where a prospective transplant is postponed, the potential recipient is subject to the higher dialysis mortality risk than if transplant were to be realized. Also, deaths on the waiting list could be more frequent for patients who have been listed longer, even if they are more likely to be selected for transplantation under current allocation algorithms. Thus, by delaying transplants, it is possible the kidney wait‐list mortality could be higher than can be reasonably calculated from database information available for analysis in this study. Moreover, it should be noted that any postponement of transplantation may adversely affect the improved quality of life accompanying a successful kidney transplant. 19
Changes in US kidney transplant efforts due to the COVID‐19 pandemic have been numerous and variable by region and by transplant center. Some centers shut down completely, while others changed little while heeding the known risks of COVID‐19. 1 , 8 , 18 , 20 Therefore, real outcomes as to number of excess kidney transplant candidate deaths cannot be known. And, mortality risk facing wait‐listed patients receiving dialysis might be increasing due to the insidious nature of the SARS‐CoV‐2 virus itself with its pathophysiologic features of multisystem organ perturbations. Despite the speculative nature of applying historic data to potential outcomes of the present, estimates we describe may serve a useful purpose not only to examine national transplant policies and procedures, but also to inform patients and families about possible outcomes of actions taken on their behalf due to the pandemic or other unforeseen exigencies. Cessation, curtailment, or full engagement of organ recovery and sharing, as well as all clinical transplantation activities must be predicated upon the best scientific analysis of the moment whenever unforeseen disaster strikes. While well researched best practices during the 2020–2021 COVID‐19 pandemic may not be known for some time, we trust that our analysis can provide some useful information regarding altered transplant center activity at various levels for varying periods of time.
Because the United States Renal Data System compiles information only for patients being treated for ESRD, the scope of our study is limited to kidney transplantation, although potential recipients awaiting other vital organs may have been similarly affected. And, our analysis cannot address transplant center wait‐listed patient health or actions taken by any center to offer any patient a particular kidney regardless of the pandemic. Most recent information discloses that during the COVID‐19 pandemic, there are over 700 000 Americans with ESRD 21 ; the approximately 100 000 patients awaiting kidney transplant may tend to be younger with fewer comorbidities that the US dialysis population at large. Thus, overall comparisons are of notably different patient groups. Add the unknowable complexities of the COVID‐19 virus to the disruptions at the hospital and transplant program level, and outcome predictions of all sorts become conjectural, at best. Yet, we believe that the calculated potential mortality rates for wait‐listed patients may provide guidance to transplant programs regarding a refrain from transplantation versus offering kidneys in the clinical circumstances which suggest both better patient survival as well as an improved quality of life.
Finally, the potential impact of COVID‐19‐related transplant center inactivity on ESRD mortality in the United States, while likely impossible to fully determine, may serve as a model in estimating effects of transplant center closure due to unanticipated catastrophic circumstances. There is little question that kidney transplantation activity diminished, at least for a while. Yet, the return to near normal activity seems to affirm the resiliency of the overall kidney transplant enterprise in the United States. Even if an annualized kidney transplant decrement of 25% were experienced, an additional 84 patients awaiting a deceased donor kidney might die on the waitlist while 35 potential living donor kidney recipients could perish—deaths in excess of anticipated mortality had kidney transplantation been performed. Conclusions derived from readily available ESRD mortality and kidney transplant outcome data may serve ESRD patients and families as well as transplant professionals to best determine how to respond to serious and unexpected infringements in providing optimal kidney transplantation services.
CONFLICTS OF INTEREST
The authors of this manuscript have no conflicts of interest to disclose.
AUTHORS’ CONTRIBUTIONS
Research idea and study design: TGP, JLB‐G, JPR, GC, and PJH; Data acquisition: JLB‐G, ACK, and PJH; Data analysis/interpretation: TGP, JLB‐G, ACK, FMcC, and PJH; Statistical analysis: JLB‐G and ACK; Supervision or mentorship: TGP and PJH; Manuscript preparation, editing, and review: All authors. Each author contributed to important intellectual content during manuscript drafting and its revisions, accepts personal accountability for the author's own contributions, and agrees to ensure that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Peters TG, Bragg‐Gresham JL, Klopstock AC, et al. Estimated impact of novel coronavirus‐19 and transplant center inactivity on end‐stage renal disease‐related patient mortality in the United States. Clin Transplant. 2021;35:e14292. 10.1111/ctr.14292
Funding information
There was no extramural support for this research. Each author contributed time and effort voluntarily. Except for the authors, no person or institution had a role in defining the content of the manuscript.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available at: 1. US Department of Health and Human Services: OPTN 2019 Annual Data Report: https://optn.transplant.hrsa.gov/data/view‐data‐reports/national‐data/#; 2. Centers for Disease Control and Prevention: National Center for Health Statistics. FastStats, Life Stages and Populations, Deaths. https://www.cdc.gov/nchs/fastats/deaths.htm; 3. US Renal Data System Chapter 3: Morbidity and Mortality in Patients with CKD. https://www.usrds.org/2017/view/v1_03.aspx; 4. US Renal Data System Chapter 5: Mortality. https://www.usrds.org/2018/view/v2_05.aspx; 5. Mortality Reference Tables USRDS 2018 Report United States Renal Data System. 2018 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2018; 6. Hil G. COVID assessment, National Kidney Registry. October 8, 2020. https://www.kidneyregistry.org/. Our respective manuscript reference numbers for the six numbered resources above: refs 9, 10, 11, 12, 13, 14. Our data were derived from the above resources available in the public domain.
REFERENCES
- 1. Boyarsky BJ, Po‐Yu Chiang T, Werbel WA, et al. Early impact of COVID‐19 on transplant center practices and policies in the United States. Am J Transplant. 2020;20:1809‐1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Doglietto F, Vezzoli M, Gheza F, et al. Factors associated with surgical mortality and complications among patients with and without coronavirus disease 2019 (COVID‐19) in Italy. JAMA Surg. 2020;155(8):691‐702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kates OS, Fisher CE, Stankiewicz‐Karita HC, et al. Earliest cases of coronavirus disease 2019 (COVID‐19) identified in solid organ transplant recipients in the United States. Am J Transplant. 2020;20:1885‐1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kumar D, Manuel O, Natori Y, et al. COVID‐19: A global transplant perspective on successfully navigating a pandemic. Am J Transplant. 2020;20:1773‐1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Myles PS, Maswime M. Mitigating the risks of surgery during the COVID‐19 pandemic. Lancet. 2020;396:2‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shah MB, Lynch RJ, El‐Haddad H, Doby B, Brockmeier D, Goldberg G. Utilization of deceased donors during a pandemic: an argument against using SARS‐CoV‐2–positive donors. Am J Transplant. 2020;20:1795‐1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Woloshin S, Patel B, Kesselheim AS. False negative teats for SARS‐CoV‐2 infection—challenges and implications. N Engl J Med 2020;383(6):e38 (1‐3). [DOI] [PubMed] [Google Scholar]
- 8. Cholankeril G, Podboy A, Alshuwaykh OS, et al. Early impact of COVID 19 on solid organ transplantation in the United States. Transplantation. 2020;104(11):2221‐2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. US Department of Health and Human Services . OPTN 2019 annual data report. https://optn.transplant.hrsa.gov/data/view‐data‐reports/national‐data/#. Accessed 1 December, 2020.
- 10. Centers for Disease Control and Prevention: National Center for Health Statistics . FastStats, life stages and populations, deaths. https://www.cdc.gov/nchs/fastats/deaths.htm. Accessed 1 December, 2020.
- 11. US renal data system chapter 3: morbidity and mortality in patients with CKD. https://www.usrds.org/2017/view/v1_03.aspx. Accessed 1 December, 2020.
- 12. US Renal Data System Chapter 5: Mortality. https://www.usrds.org/2018/view/v2_05.aspx. Accessed 1 December, 2020.
- 13. Mortality Reference Tables USRDS 2018 Report United States Renal Data System. 2018 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018. [Google Scholar]
- 14. Hil G. Personal communication: COVID assessment. National Kidney Registry. 2020. https://www.kidneyregistry.org/. Accessed 1 December, 2020.
- 15. Andreoni K. Now is the time for the organ procurement and transplantation network to change regulatory policy to effectively increase transplantation in the United States: Carpe Diem. Am J Transplant. 2020;20:2026‐2029. [DOI] [PubMed] [Google Scholar]
- 16. Klassen DK, Edwards LB, Stewart DE, Glazier AK, Orlowski JP, Berg CL. The OPTN deceased donor potential study: implications for policy and practice. Am J Transplant. 2016;16:1707‐1714. [DOI] [PubMed] [Google Scholar]
- 17. Sanfillppo FP, Vaughn WK, Peters TG, et al. Factors affecting the waiting time of cadaveric kidney transplant candidates in the United States. JAMA. 1992;267:247‐252. [PubMed] [Google Scholar]
- 18. Kataria A, Yakubu I, Winstead R, Gowda M, Gupta G. COVID‐19 in kidney transplantation: Epidemiology, management considerations, and the impact on kidney transplant practice. Transplantation Direct. 2020;6(8):e582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tonellia M, Wiebea N, Knollb G, et al. Systemic review: Kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11:2093‐2109. [DOI] [PubMed] [Google Scholar]
- 20. Mohamed IH, Chowdary PB, Shetty S, et al. Outcomes of renal transplant recipients with SARS‐CoV‐2 infection in the eye of the storm: a comparative study with waitlisted patients. Transplantation. 2021;105(1):115‐120. [DOI] [PubMed] [Google Scholar]
- 21. HHS reports progress on President Trump’s Advancing American Kidney Health Initiative. https://www.hhs.gov/about/news/2020/08/17/hhs‐reports‐progress‐on‐president‐trumps‐advancing‐american‐kidney‐health‐initiative.html. Accessed 1 December, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available at: 1. US Department of Health and Human Services: OPTN 2019 Annual Data Report: https://optn.transplant.hrsa.gov/data/view‐data‐reports/national‐data/#; 2. Centers for Disease Control and Prevention: National Center for Health Statistics. FastStats, Life Stages and Populations, Deaths. https://www.cdc.gov/nchs/fastats/deaths.htm; 3. US Renal Data System Chapter 3: Morbidity and Mortality in Patients with CKD. https://www.usrds.org/2017/view/v1_03.aspx; 4. US Renal Data System Chapter 5: Mortality. https://www.usrds.org/2018/view/v2_05.aspx; 5. Mortality Reference Tables USRDS 2018 Report United States Renal Data System. 2018 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2018; 6. Hil G. COVID assessment, National Kidney Registry. October 8, 2020. https://www.kidneyregistry.org/. Our respective manuscript reference numbers for the six numbered resources above: refs 9, 10, 11, 12, 13, 14. Our data were derived from the above resources available in the public domain.


